Abstract
Background: Aggressive large tumors of the bladder are not always malignant or invasive. Inflammatory myofibroblastic tumor (IMT) of the bladder, a typically benign lesion, is challenging to diagnose as it presents similarly to other malignant disease processes. Awareness of the specific pathological features of these rare tumors is necessary to promote accurate diagnosis and avoid unnecessary treatment.
Case Presentation: We discuss a case of a 51-year-old Caucasian man who presented with gross hematuria. Cystoscopy demonstrated a large, sessile bladder mass concerning for bladder cancer. After an aggressive transurethral resection of this mass, pathology demonstrated an IMT. Lesions of this nature are extremely rare in the bladder and present similarly to an invasive bladder tumor.
Conclusion: IMT is a rare typically benign tumor in the urinary bladder with a presentation concerning for malignant disease. Transurethral resection of the tumor is the standard for diagnosis; however, immunohistochemistry can be useful in distinguishing IMT from other spindle cell malignancies. After initial treatment with transurethral resection, patients have an ∼1.6% chance of lesion recurrence within 6 months. Given these findings, treatment with transurethral resection of bladder tumor in combination with routine cystoscopy and CT urogram every 3 to 6 months is adequate and reasonable for monitoring for local recurrences in the majority of cases.
Keywords: bladder cancer, bladder tumor, myofibroblast, pseudotumor, urinary bladder
Introduction and Background
Inflammatory myofibroblastic tumor (IMT) is highly rare in the genitourinary tract and represents a diagnostic challenge to physicians because of its significant overlap in clinical presentation and gross findings. There are currently no known risk factors for lesion formation and occurrences in both genders of all ages have been documented in past literature.1 Despite this, there remains uncertainty regarding definitive treatment and disease management. This article discusses adequate treatment and management of inflammatory myofibroblastic lesions in the urinary bladder to characterize best practices for this rare pathology.
Presentation of Case
A 51-year-old man presented to urology clinic with complaints of dysuria, lower urinary tract symptoms (LUTS), and gross hematuria with passing tissue fragments in his urine since previous 2 weeks. He denied any prior or recent history of urologic instrumentation, fever, trauma, urinary tract infections, and sexually transmitted diseases. He was a nonsmoker and had no relevant surgical history or history of malignancy. His family history was negative for genitourinary cancer. Urologic history included benign prostatic hyperplasia with LUTS and erectile dysfunction treated with a combination of tamsulosin and tadalafil. He had a body mass index of 22.8 and worked in the airline industry as a career pilot.
All blood and urine investigations of his work-up were generally unremarkable. His renal function was within normal limits with a serum creatinine of 0.84 mg/dL and an estimated glomerular filtration rate of 102 mL/min/1.73. His urine culture was negative for significant growth. Sexually transmitted infection panel was negative as well.
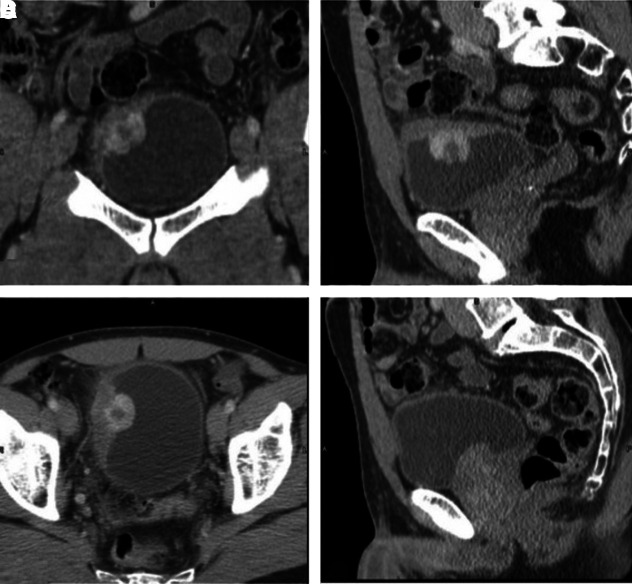
After consultation, the patient was investigated through CT urogram, which revealed a 3.5 × 3.5 × 4 cm right-side bladder wall mass ∼13 mm in depth with extravesical invasion into the musculature and perivesicular space. These findings were concerning for an invasive bladder tumor (Fig. 1). No metastatic lesions were identified on CT imaging.
FIG. 1.
CT Urogram demonstrating a polypoid mass in the right posterior bladder wall protruding into bladder lumen. Lesion is ∼13 mm in depth with extravesical spread (A: coronal, B: sagittal, C: axial with IV contrast, D: sagittal).
A partial cystectomy was offered to the patient; however, after an extensive literature review and discussion on options with the patient, he opted instead for resection of the lesion with close follow-up. A cystoscopy with aggressive transurethral resection of bladder tumor (TURBT) was performed. Intraoperative findings revealed a large sessile smooth-walled bladder lesion involving the right posterior bladder wall, clear of the ureteral orifices (Fig. 2). No satellite lesions were identified at that time.
FIG. 2.

(A) Intraoperative appearance of bladder tumor. Patient had a large sessile mass in right posterior aspect of bladder; (B) intraoperative appearance of bladder after treatment with aggressive transurethral resection of bladder tumor. No residual tumor or regrowth was seen at the time of 3-month cystoscopy.
Subsequent histological examination revealed IMT, a spindle cell tumor with invasion into both the lamina propria and muscularis propria (Fig. 3). On immunohistochemical evaluation, the tumor was found to express anaplastic lymphoma kinase, a known marker specific for IMT.2
FIG. 3.
(A) Normal bladder mucosa; (B) spindle cell tumor invading muscular propria; (C) high power view of spindle cell tumor; (D) anaplastic lymphoma kinase immunohistochemistry.
A follow-up cystoscopy was performed 3 months after initial treatment with TURBT. Follow-up cystoscopy demonstrated no evidence of regrowth or residual tumor. He was asymptomatic at that time and so repeat TURBT or partial cystectomy was not indicated. Patient will be subsequently seen in follow-up at 3 months.
Discussion
IMT in the urinary bladder is uncommon and has historically been recognized as having an unknown neoplastic potential. Lesions of this nature were first described in 1937 by Brunn from a section of lung tissue, the most frequently affected anatomical site to date.3 IMT is highly rare in the genitourinary tract; Roth documented the first case of IMT in the urinary bladder in 1980, which he described as a solid tumor composed of inflammatory cells and myofibroblasts.1 The presence of lymphocytic infiltrate and spindle myoepithelial cell proliferation remain the essential criteria for diagnosis.2
Unfortunately, IMT shares a significant overlap in clinical presentation, gross findings, morphology, and immunoprofile between benign and malignant spindle cell processes, providing a set of challenges for diagnosticians.
Clinical presentation and gross findings
Currently, there are no known predisposing factors for developing IMT in the bladder; however, previous literature has found associations between infection, autoimmunity, trauma, and recent surgical instrumentation. IMT occurrences have been well described in both genders in all age groups, spanning from infancy to age 88.2 Cystoscopic evaluation typically reveals a polypoid mass or submucosal nodule with a firm whirled pattern and texture. Typical vesical IMTs are <2 cm in size with predilection for the posterior wall of the bladder.
Treatment
Typical IMTs can be locally aggressive and thus complete surgical resection is the treatment of choice. Of the 182 patients in Teoh et al.'s systematic review, 60.8% were treated with TURBT, 29.2% with partial cystectomy, and 9.2% with radical cystectomy.4 Despite a typically benign course, 5 of these 182 patients developed local recurrences, representing an overall 2.7% rate of local recurrence. Two of these five recurrences occurred within a 6-month window after the primary excision and required treatment with a second TURBT. Only one single case of metastases related to IMT was reported in a 71-year-old man with a remote history of radiation related to prostate cancer. Despite only a single documented case of metastases, Teoh et al. concede that close follow-up is indicated because of the possibility of IMT presenting concurrently with sarcomatoid urothelial carcinomas.4 Therefore, most cases can be adequately treated with transurethral resection. In rare cases involving the majority of the bladder, however, partial cystectomy may be indicated.
Conclusion
In conclusion, IMT is a rare, mainly benign tumor in the urinary bladder that presents similarly to malignant disease processes. Transurethral resection of the tumor is the standard for diagnosis and immunohistochemistry can be used to further distinguish IMT from other spindle cell malignancies. Assuming no early recurrences, specifically within 6 months of initial resection, patients have an ∼1.6% chance of lesion recurrence. Given these findings, treatment with TURBT in combination with routine follow-up, cystoscopy, and CT urogram every 3 to 6 months is adequate and reasonable for monitoring both local recurrences and distant metastases for the majority of cases.
Abbreviations Used
- CT
computed tomography
- IMT
inflammatory myofibroblastic tumor
- LUTS
lower urinary tract symptoms
- TURBT
transurethral resection of bladder tumor
Disclosure Statement
No competing financial interests exist.
Cite this article as: Gass J, Beaghler M, Kwon M (2019) Inflammatory myofibroblastic tumor of the urinary bladder: a case report, Journal of Endourology Case Reports 5:2, 31–33, DOI: 10.1089/cren.2018.0096.
References
- 1. Roth JA. Reactive pseudosarcomatous response in urinary bladder. Urology 1980;16:635–637 [DOI] [PubMed] [Google Scholar]
- 2. Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: Where are we now? J Clin Pathol 2008;61:428–437 [DOI] [PubMed] [Google Scholar]
- 3. Brunn H. Two interesting benign lung tumors of contradictory histopathology, remarks on the necessity for maintaining chest tumor registry. J Thorac Surg 1939;9:119 [Google Scholar]
- 4. Teoh JY, Chan NH, Cheung HY, Hou SS, Ng CF. Inflammatory myofibroblastic tumors of the urinary bladder: A systematic review. Urology 2014;84:503–508 [DOI] [PubMed] [Google Scholar]