Abstract
Background: Filariasis is a tropical disease caused by infection with nematode parasites of the Filarioidea family. Filariasis is an endemic disease in parts of India, Sub-Saharan Africa, and Southeast Asia. Filariasis is a progressive disease predominantly affecting the lymphoreticular system, which can result in genitourinary complications (hydrocele, scrotal pain, and infertility), lymphedema, and elephantitis. Retroperitoneal fibrosis has a broad etiology, including secondary to chronic infection. Currently an estimated 25 million men are suffering from lymphatic filariasis with urogenital involvement worldwide.
Case Presentation: We present a rare case of a 40-year-old man presenting with fever, groin lymphadenopathy, and a history of infertility. Imaging confirmed significant hydronephrosis and retroperitoneal fibrosis. Filariasis serology was positive. Prior bilateral testicular biopsy demonstrated chronic inflammation and atrophy. Disease course was not improved by empirical eradication and supportive retrograde ureteral stenting. The patient developed elephantitis and progressive retroperitoneal fibrosis leading to a solitary functioning right kidney with nephrostomy.
Conclusion: Urologists should be aware of index presentations of filariasis and its associated urological complications, particularly in the travelling adult population in whom the etiology of renal impairment and infertility remains unclear.
Keywords: retroperitoneal fibrosis, filariasis, hydronephrosis, infertility, obstruction, renal failure
Introduction and Background
Filariasis is a tropical disease caused by nematode parasites of the Filarioidea family.1,2 Filarial parasites are classified broadly into cutaneous, lymphoreticular, and body cavity.1 Filariasis is an endemic disease in parts of India, Sub-Saharan Africa, and Southeast Asia.2 Lymphatic filariasis (Wuchereria bancrofti, Brugia malayi, and B. timori) is transmitted through mosquitoes.1,2 Adult filariae reside in lymphatics and cause damage to lymphatic vessels.1,2 Initial infection with filarial parasites is usually asymptomatic.2,3 However, in the acute adenolymphangitis phase patients present with fever, painful lymphadenopathy, and may have superimposed bacterial infection.2 Chronic infection leads to lymphedema, elephantitis, widespread fibrosis, and hydrocele formation.1,2 Currently an estimated 25 million men are suffering from lymphatic filariasis with urogenital involvement worldwide.2
Secondary retroperitoneal fibrosis has a broad etiology; common causes can be divided into drugs, malignancy, infection, radiotherapy, and intra-abdominal surgery.3 Extraluminal visceral obstruction colonic and ureteral are recognized complications of retroperitoneal fibrosis and have been reported in the literature.3 We present a rare case of a male patient presenting with significant hydronephrosis, renal failure, and infertility secondary to filariasis-driven retroperitoneal fibrosis.
Presentation of Case
A 40-year-old man of Indian origin presented to hospital with fever and a nontender lump in the left groin. Apart from a mildly raised erythrocyte sedimentation rate, his blood tests were unremarkable. An abdominal ultrasonography was performed, which demonstrated an inguinal mass and a dilated left renal pelvis.
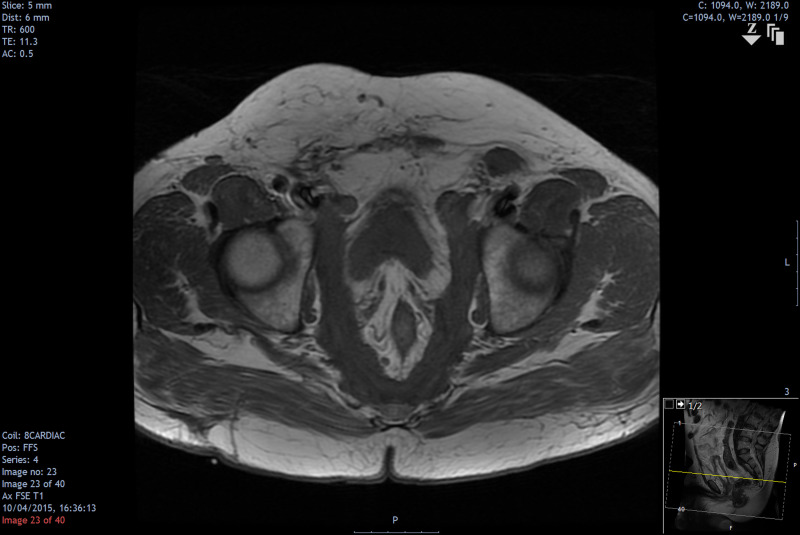
He underwent a CT-guided biopsy of his inguinal mass, which was reported as reactive lymphadenopathy, with no evidence of tuberculosis. A CT scan confirmed bilateral hydronephrosis and hydroureter to the level of the pelvic brim (Fig. 1). A pelvic MRI scan reported extensive fibrosis involving the presacral and pelvic regions (Fig. 2).
FIG. 1.
CT abdomen (noncontrast) demonstrating bilateral hydronephrosis with retroperitoneal fibrosis encasing ureters and vasculature.
FIG. 2.
MRI (T1-weighted) demonstrating extensive presacral and pelvic fibrosis and enlarged inguinal lymph nodes.
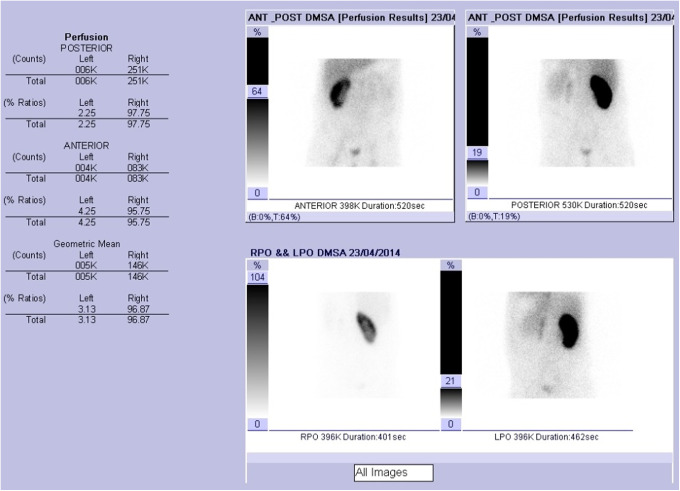
A working diagnosis of “atypical” retroperitoneal fibrosis was made and the patient was started on a trial of steroids. Bilateral Double-J stents were inserted, which improved renal function to baseline. The left kidney continued to deteriorate, the patient becoming nephrostomy dependent. A trial of steroids was stopped as the patient did not respond. Functional imaging with a dimercaptosuccinic acid scan demonstrated split renal function of 3.13% and 96.87% of the left and right kidney, respectively (Fig. 3).
FIG. 3.
DSMA scan with split renal function of 3.13% (left) and 96.87% (right). DSMA, dimercaptosuccinic acid; LPO, left posterior oblique; RPO, right posterior oblique.
The patient also complained of long-standing infertility. A prior testicular biopsy reported atrophy of the seminiferous tubules with chronic inflammation of unclear cause (Fig. 4). Semen analysis confirmed azoospermia. Owing to worsening lower urinary tract symptoms he had urodynamic studies that revealed a small capacity bladder with associated suprapubic pain on filling. His Pdet at 200 mL was 30 cm of water. His voiding phase showed a Qmax of 16 mL/s with a Pdet Qmax of 47 (>40 indicates obstruction). The findings were in keeping with a high-pressure bladder with loss of compliance. A cystoscopy performed demonstrated a conical-shaped bladder that was not suitable for ureteral implantation.
FIG. 4.
Testicular biopsy (A) Hematoxylin- and eosin-stained testicular tissue shows complete atrophy of the seminiferous tubules and chronic inflammation ( × 200). (B) Elastic-Van Gieson outlines of atrophic seminiferous tubules ( × 200).
Various specialties, including infectious diseases, hematology, and vascular, reviewed the patient to assist in diagnosis. Once tuberculosis and hematological malignancies were excluded, filariasis serology was performed and found positive. After multidisciplinary input, filariasis was felt the probable etiology of the patient's signs and symptoms.
The patient went on to develop mild elephantitis and was treated with ivermectin and an extended 6-week course of doxycycline without clinical improvement. In addition, the patient was listed for a clam cystoplasty.
Worsening retroperitoneal fibrosis resulted in severe compression off both common iliac veins and the lower inferior vena cava (Fig. 5). The patient's left kidney became atrophic and nonfunctioning, with renal function reliant on a solitary right kidney with nephrostomy. Sadly, after repeated multiresistant skin, urinary, and chest infections, the patient died as a result of multiorgan failure.
FIG. 5.
CT abdomen and pelvis demonstrating extensive retroperitoneal fibrosis. Abnormal soft tissue encasing the lower inferior vena cava. Fibrotic tissue thickening both pelvic sidewalls and invading the presacral space.
Discussion and Literature Review
Lymphatic filariasis is a debilitating tropical disease that has a devastating disease burden if untreated.1,2 An estimated 120 million people in 81 countries are currently infected and 1.34 billion are at risk of exposure in areas where the disease is endemic.1,2 Intrinsic renal involvement in filariasis can be caused by a range of pathologies and is noted in both acute, chronic, and coinfection with hepatitis B or malaria.1
Patients can present with a range of symptoms, including asymptomatic proteinuria, chyluria, hematuria, oliguria, nephrotic syndrome, and loin pain.1 Mesangioproliferative or membranoproliferative glomerulonephritis is a recognized manifestation of intrinsic renal filariasis. Research suggests that this is because of immune complex deposition (mainly immunoglobulin G and C3) as a reaction to parasitic antigens in the glomeruli and, therefore, an immune-pathogenetic process is felt to be the most likely mechanism. Retroperitoneal and perirenal lymphangiectasia consistent with lymphatic filariasis has been previously reported.4
Presentation of chronic lymphatic filariasis remains a rare cause of hydronephrosis and subfertility in the western world. However, as highlighted in this case, with increased travel to and from endemic countries, clinicians worldwide should be aware of infectious causes of secondary retroperitoneal fibrosis. These patients present a complex challenge to the primary attending urologist and involvement of colleagues from multiple specialties is needed to expedite diagnosis. An early diagnosis is of crucial importance as delay may lead to irreversible renal impairment and infertility, which hold a significant medical and psychological morbidity.2
We present a rare case of significant hydronephrosis, renal failure, and infertility secondary to filariasis-driven secondary retroperitoneal fibrosis. Clinicians should be aware of index presentations of filariasis and its associated nephrourological complications, particularly in travelling adult populations in whom the etiology of renal impairment and subfertility remains unclear.
Abbreviations Used
- CT
computed tomography
- MRI
magnetic resonance imaging
Disclosure Statement
All authors have declared no competing financial interests.
Cite this article as: Connor MJ, Habib A, Wen D, Kubba F, Raza A (2019) Filariasis an unusual cause of retroperitoneal fibrosis, hydronephrosis, and infertility in a young adult male, Journal of Endourology Case Reports 5:3, 113–116, DOI: 10.1089/cren.2019.0030.
References
- 1. Knopp S, Steinmann P, Hatz C, et al. Nematode infections: Filariases. Infect Dis Clin North Am 2012;26:359–381 [DOI] [PubMed] [Google Scholar]
- 2. World Health Organisation (WHO). Progress Report 2000–2009 and Strategic Plan 2010–2020 of the Global Programme to Eliminate Lymphatic Filariasis. Geneva, Switzerland: WHO, 2010 [Google Scholar]
- 3. Vaglio A, Salvarani C, Buzio C. Retroperitoneal fibrosis. Lancet 2006;21;367:241–251 [DOI] [PubMed] [Google Scholar]
- 4. Mount P, Thong M. Perirenal and lymphatic filariasis presenting with chyluria in pregnancy. Kidney Int 2006;69:2115. [DOI] [PubMed] [Google Scholar]