Abstract
Background: There are limited data about urolithiasis in young infants, especially in class age younger than 2 years.
Case presentation: We report the case of a child <2 years old (13 months) affected by metabolic urolithiasis (cystinuria), and renal hypertension. He was admitted to our ward from the pediatric emergency room for fever, lack of appetite, irritability, and abdominal pain crisis. Ultrasonography (US) described a huge stone (15 mm) in dilated left renal pelvis (20 mm) associated with distal ureteral ectasia (7 mm). Urine and blood diagnostic assessments were performed. Hydropenic therapy and urine alkalization were started without success. The child underwent an ureteroscopy (URS) with a 4.5–6.5F rigid ureteroscope aiming to reach the renal pelvis and perform holmium: yttrium–aluminum–garnet laser stone disintegration. During the procedure, the ureter presented two unexpected stones in the distal portion (missed on US). A laser ureteral lithotripsy was effectively performed extracting smaller stone fragments. Ureteral kinking, confirmed by ascending pyelography, made it impossible to reach renal pelvis with the ureteroscope. The child was further studied with a CT scan that revealed a massive stone involvement of the left excretory pathway. Metabolic and urine assessment revealed a metabolic disease: cystinuria. To remove renal stones, an operative retroperitoneoscopy (RP) was performed. During the procedure was identified a lesion of the pelvis (secondary to stone decubitus) with urine tearing and massive perirenal inflammation. The stone was removed and pelvis was sutured. Postoperatively, the patient was stone free without major complications.
Conclusions: In particular cases (younger patients, ureteral kinking, and renal failure risk), a totally combinated minimally invasive access (URS, laser stone fragmentation, and RP) can be a valid alternative to micro percutaneous nephrolithotomy or to massive open treatment. In fact, rigid URS represents a valid minimally invasive approach either for examination or for laser treatment of pediatric urinary tract stones. With important ureteral kinking, RP must be considered by experienced pediatric urologists.
Keywords: urolithiasis, laser lithotripsy, ureteroscopy, retroperitoneoscopy, cystine stones, kidney
Introduction
Urolithiasis incidence in children is increasing; in the past 25 years, a 6%–10% increase every year was recorded. Incidence in pediatric age is ∼10% of adults. About 50:100.000 adolescents have at least one episode of renal colic. Urolithiasis can affect children of all age groups with males affected more in the first 10 years of age, females affected between 10 and 18 years. Totally, the prevalence is higher in females unlike the adult. Infantile urolithiasis represents 20% of the total pediatric urolithiasis research in the literature. The incidence of pediatric urolithiasis in the age group of children younger than 2 years is >20%, with a worldwide increase causing considerable morbidity.1 Extracorporeal shockwave lithotripsy (SWL) is still considered the first-line treatment of renal and upper ureteral calculi measuring <2 cm. In children, it is simple to perform, in general anesthesia, and does not require a long learning curve; it is also associated with few complications, most of which are minor. Over the past 20 years ureteroscopy, (URS) and percutaneous nephrolithotomy (PCNL) have also evolved significantly, thanks to major technological improvements: miniaturization of both semirigid and flexible endoscopes, improved imaging modalities, and the introduction of the holmium: yttrium–aluminum–garnet (Ho:YAG) laser for stone disintegration. Pediatric PCNL is efficient and has low complication rates. The Mini-Perc technique introduced by Jackman et al.2 results effective in 85% of cases in children with a mean age of 3.4 years. Many pediatric urologists currently use smaller endoscopes to reduce parenchymal damage and bleeding, as MicroPerc described by Caione et al.2 Although minimally invasive procedures are effective in the management of most renal and ureteral stones, particular cases of large calculi or stones resistant to either extra/intracorporeal lithotripsy need multiple treatment steps. With evolving pediatric laparoscopic renal surgery, initial experience with laparoscopic/retroperitoneoscopic or robotic pyelolithototmy has gained success, with reported stone-free rates (SFRs) of 95%–100%. Complications were minimal when expertise is available.3 We describe a 13-month-old boy with massive cystine urolithiasis involving the whole left excretory pathway with 15 mm kidney stone. We performed a combined endoscopic laser lithotripsy (Ho:YAG) using a 4.5/6.5F rigid ureteroscope in the left ureter combined with a retroperitoneoscopic stone asportation.
Case Report
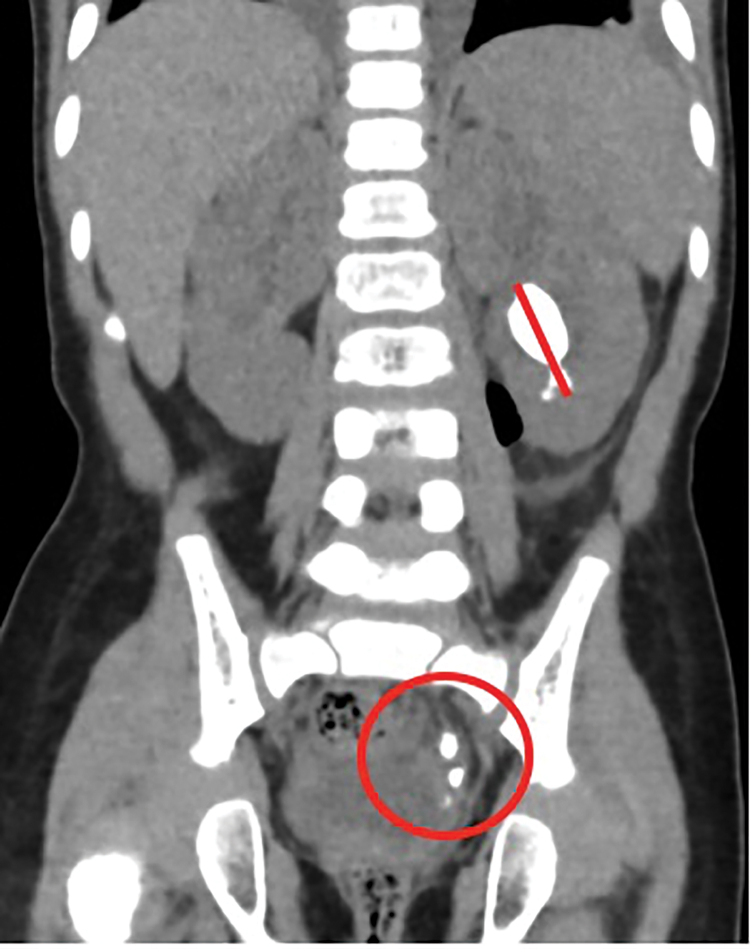
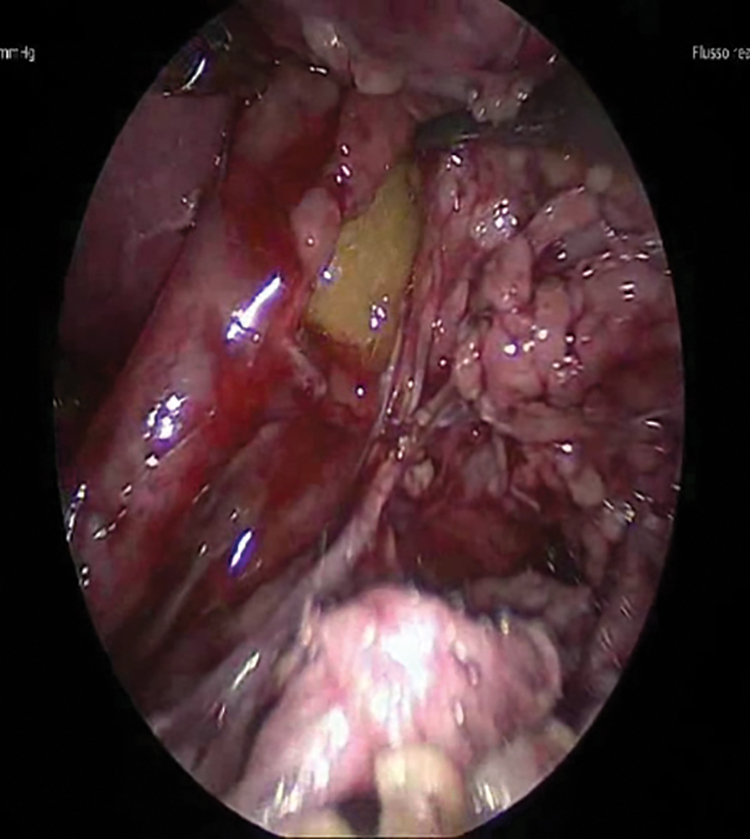
We report our challenging experience with a young boy of 13 months of life with multiple cystine kidney stones on the left excretory pathway. The boy (height, 90.5 cm; weight, 9.5 kg) had a medical history of kidney stone 3 months previously, discovered on ultrasonography (US) in a peripheral hospital. He was admitted to our ward from the pediatric emergency room for fever, lack of appetite, and irritability associated with abdominal pain crisis. On US, a 15 mm stone in the left dilated renal pelvis (20 mm) was described associated with 7 mm distal ureter ectasia. The right excretory pathway was stone free. Urine and blood assessments were started. The stone was monitored by imaging while the child was started on oral hydropenic therapy, urine alkalization (with potassium citrate), and antibiotic prophylaxis. We initially, having different US scans confirming only an intrarenal stone, did not perform a CT scan to avoid a huge X-ray exposure. We developed a strategy of minimally invasive treatment with miniature devices to reduce the patient's operative risk. We planned to perform retrograde intrarenal surgery (RIRS) using a 4.5–6.5F ultrathin rigid ureteroscope (R. Wolf, Germany) without ureteral stenting with the aim to treat the left kidney stone. During URS, we found in the distal segment of ureter (3–4 cm from the ureter–vesical junction), two unexpected big stones, missed at US. We started with Ho:YAG laser stone disintegration (Fig. 1). Ureteral laser lithotripsy was performed effectively. To avoid the difficulties of retrieval of fragment for the narrow ureter, we used a 6F-cystoscope, introducing it in the distal segment of the ureter. To exclude the presence of other ureteral stones, we performed intraoperatively an ascending pyelography, discovering a double kinking of the ureter (Fig. 2). To exclude the presence of other ureteral stones, an ascending pyelography was performed intraoperatively discovering a double kinking of the ureter so the insertion of a double-J ureteral stent with RIRS wasn't possible. We stopped the procedure and decided to study the child with CT scan using lower dose targeted noncontrast scanning, which revealed a massive stone involvement of the whole left excretory pathway (Fig. 3). Metabolic and urine assessment revealed a metabolic disease: cystinuria, confirmed by composition analysis. The child was so treated in two steps: (1) ureteral Ho:YAG laser lithotripsy for ureteral stones and (2) after 20 days, left retroperitoneoscopy (RP) (5 mm camera and 3 mm instruments), identifying a massive perirenal inflammation with a pelvis tearing extended from the proximal ureter, through the pelvis, just until the inferior calix. After stone removal and placing a 4.8F Double-J ureteral stent, we sutured the tear with a continuous suture in Polysorb 5/0. The procedures were effective. Operative time was 165 minutes. Postoperatively, the patient was stone free without major complications and was discharged on postoperative day 5. The Double-J stent was removed 1 month after RP. For blood hypertension, he was started on ACE-inhibitors therapy. At 2 and 3 months postoperatively, US and radiographs revealed no residual fragments or hydronephrosis. The patient was followed at our outpatient clinic by Holter-blood-pressure study, fundus-oculi, echocardiogram and renal scintigraphy. Hypertension was revealed and captopril was used. There was no flow asymmetry after ACE-inhibitor administration, no obstruction and symmetric renal function. US and radiographs revealed no residual fragments or hydronephrosis at the 2nd and 3rd months postoperatively.
FIG. 1.
Intraoperatively ascending pyelography discovering a double kinking of the ureter.
FIG. 2.
CT scan revealing a massive stone's involvement of the whole left excretory pathway. The red line indicates the intra-pyelic left kidney stone; the red circle indicates left ureteral stone.
FIG. 3.
Intraoperatory view: pyelic tear due to stone decubitus. The stone is visible inside the kidney pelvis.
Discussion and Literature Review
In this case we describe an effective combination of laser lithotripsy and mininvasive surgery, RP, using minimally invasive instruments, to treat a 13-month-old boy with large cystine kidney and ureter stones. Pediatric stone disease is a significant health problem, and is quite common in some parts of the world. Symptoms presentation is usually nonspecific when compared with adults. In pediatric age, urinary tract infection (UTI) and discomfort were the most frequent, whereas in 20%, diagnosis is incidental. Under 1-year-olds urolithiasis is diagnosed incidentally in 26% of patients, with UTI as the main presentation (27.5%). Long-term of medication is recognized as the first cause of metabolic abnormalities which cause urolithiasis, followed by hypocitraturia (19.4%), hypercalciuria (16.4%), hyperoxaluria (14.9%) and hyperuricosuria (13.4%). Cystinuria is rarer.4 According to the European Association of Urology/European Society for Pediatric Urology (EAU) guidelines, SWL represents the first-line treatment for upper urinary stones in children. The reported SFRs after SWL for kidney and ureteral stones are high, 83.4% and 94.8%, respectively, but with stones <2 cm. It is simple to perform, in general anesthesia, and does not require a long learning curve. Pediatric URS/RIRS is indicated for ureteral and kidney stones <2 cm in children of 2–3 years of age. These procedures associated with laser lithotripsy have become the techniques of choice for proximal stones treatment. Pediatric PCNL is efficient and has low complication rates. Jackman et al.2 introduced the MiniPerc technique with succesful results in 85% of cases in children with a mean age of 3.4 years. Caione et al. have reported Microperc with reduction of parenchymal damage and bleeding.5 Nowadays treatment of urolithiasis in children is challenging especially in first years of life. In past three decades, surgical management of urolithiasis has evolved, thanks to the evolution of the techniques and the new increasingly miniaturized instrumentation. This evolution allows to also treat small patients as reported by Inoue et al. They describe a 2-year-old boy with >2 cm bilateral cystine kidney stones treated with combined RIRS for the right kidney stone in the lithotomy position and super ultraminimally invasive endoscopy combined with intrarenal surgery for the left kidney stone under the Barts-modified Valdivia position.6 In our patient, affected by cystine stones, we performed endourologic Ho:YAG laser lithotripsy using first a 4.5/6.5F rigid ureteroscope in a narrow ureter, then a 6F cystoscope to complete lithotripsy and for fragments retrieval. According to EAU guidelines, removal of surgical stones may be considered as an option when SWL, URS, and percutaneous-URS fail or are unlikely to be effective. In particular, mininvasive surgery is indicated as the preferred option before open surgery when expertise is available. In our patients, age, ureter size, ureter kinking, and size of kidney stones have lead us to decide for retroperitoneal surgical removal. The patient was on lateral right decubitus. We use a 30° optic 5 mm camera and two 3 mm working port for thin instruments. The Gerota fascia and perirenal tissue were involved by a consolidated inflammatory process. Released the kidney from inflammatory adhesions we discovered an extended laceration from proximal ureter just until inferior calix caused by stone decubitus. After stone removal, we placed a Double-J stent and performed a continuous suture. The procedure was carried out safely. Treatment of urolithiasis represents a great problem in pediatric and urologic units. According to our experience, the combination of different approaches in difficult cases could represent the best choice of treatment but requires a management personalization considering age, anatomy, size, disposable instrumentations and expertise available.
Conclusions
URS and laser lithotripsy represent valid minimally invasive techniques for treatment of pediatric urolithiasis. According to us, our child was too young for MicroPerc treatment. RP was effective and the most appropriate choice, as surgical technique, in consideration of the perirenal inflammation and stone decubitus. In our patient, combination of URS with laser lithotripsy and RP was effective and minimally invasive.
Abbreviations Used
- ACE
angiotensin converting enzyme inhibitors
- CT
computed tomography
- EAU
European Association of Urology/European Society for Pediatric Urology
- Ho:YAG
holmium: yttrium–aluminum–garnet
- PCNL
percutaneous nephrolithotomy
- RIRS
retrograde intrarenal surgery
- RP
retroperitoneoscopy
- SFR
stone-free rate
- SWL
extracorporeal shockwave lithotripsy
- URS
ureteroscopy
- US
ultrasonography
- UTI
urinary tract infection
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Bleve C, Chiarenza SF (2020) Endourologic and retroperitoneoscopic combined mininvasive management of cystine urolithiasis in an infant of 13 months of life, Journal of Endourology Case Reports 6:1, 49–52, DOI: 10.1089/cren.2019.0072.
References
- 1. Naseri M. Urolithiasis in the first 2 months of life. Iran J Kidney Dis 2015;9:379–385 [PubMed] [Google Scholar]
- 2. Jackman SV, Hedican SP, Peters CA, Docimo SG. Percutaneous nephrolithotomy in infants and preschool age children: experience with a new technique. Urology 1998;52:697–701 [DOI] [PubMed] [Google Scholar]
- 3. Landau EH. Modern stone management in children. Eur Assoc Urol 2015;14:12–19 [Google Scholar]
- 4. Serdaroğlu E, Aydoğan M, Özdemïr K, Bak M. Incidence and causes of urolithiasis in children between 0–2 years. Minerva Urol Nefrol 2017;69:181–188 [DOI] [PubMed] [Google Scholar]
- 5. Caione P, Collura G, Innocenzi M, De Dominicis M, Gerocarni Nappo S, Capozza N. Percutaneous endoscopic treatment for urinary stones in pediatric patients: where we are now. Transl Pediatr 2016;5. [DOI] [PMC free article] [PubMed]
- 6. Inoue T, Watanabe M, Shimada S, Kinoshita H, Matsuda T. Successful ultra-minimally invasive endoscopic intrarenal surgery for 2-year-old boy with bilateral cystine kidney stones over 2 cm. J Endourol Case Rep 2018;4:101–104 [DOI] [PMC free article] [PubMed] [Google Scholar]