Abstract
Background: A bladder leiomyoma is a rare and benign bladder tumor. There are no established guidelines for the surgical treatment of this tumor. A transurethral approach for resection or surgical enucleation of the tumor is difficult, especially in patients with a large-sized leiomyoma. Therefore, a partial cystectomy is often indicated. In this case, we effectively performed a cystoscope-assisted laparoscopic enucleation of an intramural bladder leiomyoma.
Case Presentation: A 46-year-old female was incidentally found to have a large tumor on the left wall of her urinary bladder. The MRI and needle biopsy results confirmed that the tumor was a bladder leiomyoma. Despite its benign nature, the tumor was found to progressively increase in size in 6 months. Therefore, we chose to perform a laparoscopic enucleation of the tumor. Simultaneous intraoperative cystoscopy was utilized to observe the operative area from within the bladder, thus enabling us to perform the procedure relatively safely. Although there was a minor inadvertent injury to the bladder mucosa intraoperatively, the left ureteral orifice was preserved. As a result, the tumor was effectively enucleated. The postoperative course was uneventful, and no recurrence was observed at the 4-month follow-up.
Conclusion: We effectively accomplished the cystoscope-assisted laparoscopic enucleation of a large-sized leiomyoma of the urinary bladder. Based on our experience, we suggest that this combined technique is better and safer than an independent laparoscopic surgery. In addition, this surgery is now technically feasible and may have other applications in robotic surgery in the future.
Keywords: bladder tumor, bladder leiomyoma, enucleation, laparoscopic surgery, cystoscope
Introduction and Background
A bladder leiomyoma is a rare and benign mesenchymal tumor of the bladder, which constitutes 0.43% of all bladder tumors.1 Patients present with various symptoms in a spectrum that varies from being completely asymptomatic to having an irritable bladder.2 Although surgical management of these tumors is not always indicated, there are reports of procedures such as transurethral resection (TUR), partial cystectomy, or enucleation of the tumor being performed for treatment.2 When both TUR and enucleation are found to be technically challenging in a patient, a partial cystectomy, which is a more invasive procedure, is indicated.2
In this study, we report our experience in managing a patient with a large progressive bladder leiomyoma, which we effectively treated with a cystoscope-assisted laparoscopic enucleation. The procedure was technically more difficult than a TUR or an enucleation, but we managed to enucleate the tumor, while preserving the patient's bladder function.
Presentation of Case
A 46-year-old Japanese woman visited our urologic outpatient clinic for treatment of a bladder tumor. Although she was asymptomatic at the time, a large mass had been incidentally detected in her urinary bladder on an abdominal ultrasonography that had been advised by her family doctor, for cystitis. She had no significant medical or surgical history. She did not take any regular medications. Her height was 163 cm, and her weight was 69 kg. Her vital signs and physical examination findings were within normal limits. The patient's hematologic and biochemical test results were within normal parameters with a white blood cell count of 4800/μL, a hemoglobin level of 12.3 g/dL, a hematocrit of 37.4%, a platelet count of 233,000/μL, a blood urea nitrogen level of 10.9 mg/dL, and a creatinine level of 0.75 mg/dL.
During the patient's first visit, a cystoscopic examination confirmed the presence of a large submucosal pedunculated tumor. An MRI scan revealed that the tumor was located within the left wall of the bladder, which indicated the differential diagnosis of a bladder stromal tumor or solitary fibrous tumor. The tumor was 54 × 52 mm in diameter (Fig. 1A). A transvaginal needle biopsy of the tumor was performed, and the histopathologic examination revealed that the tumor was a leiomyoma of the bladder. Based on these findings, the tumor was diagnosed as an endovesical type of bladder leiomyoma.
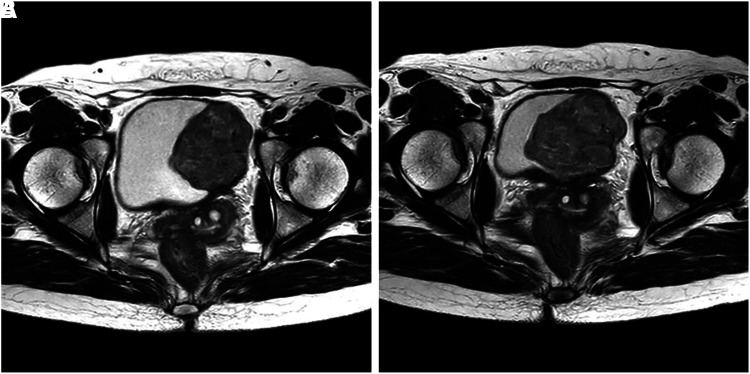
FIG. 1.
(A) An MRI showing a bladder tumor in the left wall. The tumor appeared mesenchymal, which was indicative of a bladder stromal tumor or a solitary fibrous tumor. (B) MRI repeated after 6 months showing tumor progression. The tumor had enlarged about 1.5 times as compared with its previous size.
Although the tumor was relatively large, as the patient was asymptomatic, we initially chose the method of expectant management. However, an abdominal MRI repeated 6 months after the initial visit revealed that the tumor had became larger and was now 76 × 70 mm in size (Fig. 1B). The rapid progression in size indicated a risk of the tumor becoming malignant in the future. In addition, there was a possibility that the growing tumor might adversely affect the patient's bladder voiding function, which may eventually lead to the development of a symptomatic neurogenic bladder. Therefore, we decided to proceed with a laparoscopic surgical removal of the tumor, as our hospital did not have a robotic surgical system. Moreover, the Japanese health insurance system did not offer coverage for the robotic procedure.
One month after the repeated MRI, we performed a laparoscopic enucleation of the leiomyoma. During the procedure, the patient was administered general anesthesia and draped, after being placed in the 30° Trendelenberg position. At the start of the operation, intravenous cefotiam (1 g) was administered. Total five ports were inserted during the procedure.
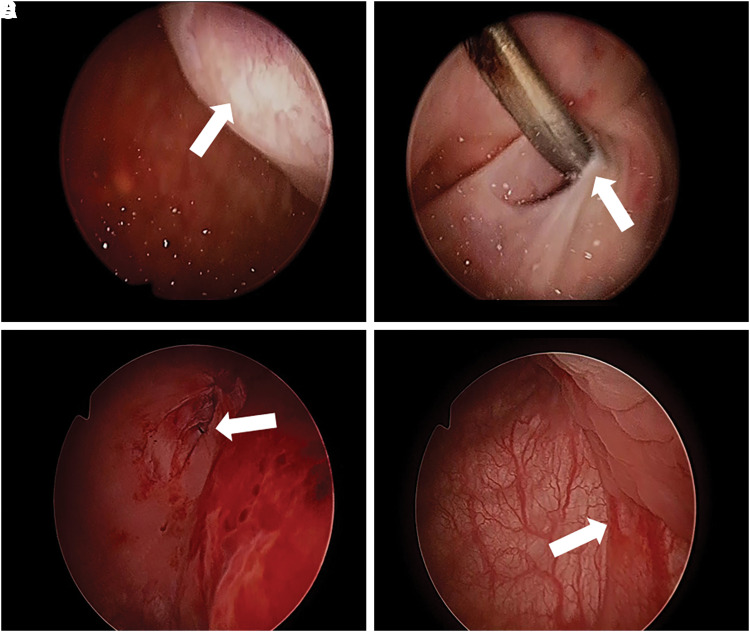
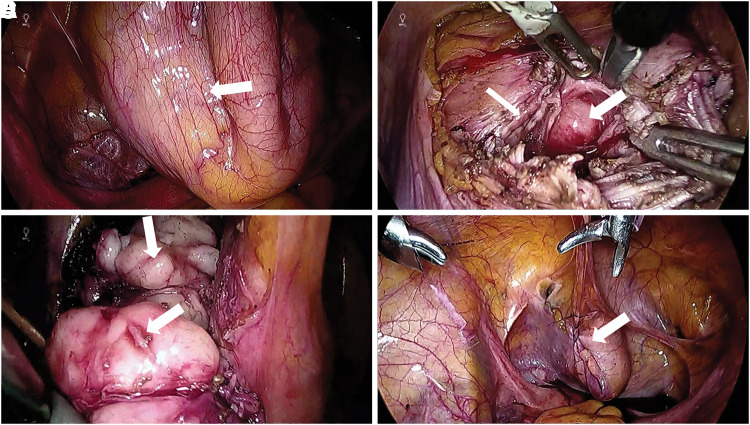
First, a laparoscope was introduced in the intraperitoneal cavity through the abdominal port. Second, a cystoscope was inserted through the urethra and the neck of the tumor was examined. Although the tumor was seen to be protruding into the bladder (Fig. 2A), the left ureteral orifice was found to be intact. Third, the tumor on the outside of the bladder was identified laparoscopically (Fig. 3A). Then, the peritoneum was dissected and the layer of the bladder muscle was sharply and bluntly split (Fig. 3B, C) under cystoscopic guidance, while keeping a check on the surgical margin and the ureteral orifices. The tumor was subsequently enucleated through the laparoscope. Although the bladder mucosa on the posterior wall suffered an accidental small puncture intraoperatively (Fig. 2B), the simultaneous cystoscopic examination confirmed that the left ureteral orifice was preserved.
FIG. 2.
(A) Through the cystoscope, a large submucosal tumor was protruded (arrow). (B) When enucleating the tumor, an inadvertent injury was observed (arrow). (C) After the approximation of bladder mucosa, the injury was repaired through cystoscope (arrow). (D) Lastly, the cystoscope confirmed that the left ureteral orifice was preserved (arrow).
FIG. 3.
(A) Through the laparoscope, a large tumor was identified through the peritoneum (arrow). (B) We dissected the peritoneum, split the bladder muscle (thin arrow), and identified the tumor (large arrow). (C) A large segmented tumor was enucleated (arrows). (D) After the enucleation, we repaired the bladder muscle using two-layer continuous sutures, and the peritoneum using 3-0 V-Loc sutures (arrow).
Next, we approximated the bladder mucosa using a continuous 4-0 Biosyn (Medtronic, Minneapolis, MN) suture. The defect within the bladder muscle was repaired using two layers of continuous 3-0 V-Loc (Medtronic) sutures, and the dissected peritoneum was closed with 3-0 V-Loc sutures (Fig. 3D). Lastly, a cystoscopic examination was performed to confirm both the repair of the incidental injury (Fig. 2C) and the continued integrity of the left ureteral orifice (Fig. 2D). The operative duration was 227 minutes, with an estimated 100 mL blood loss in total. There were no intraoperative complications, except for the minor puncture. On histopathologic examination, the enucleated tumor was confirmed as a bladder leiomyoma.
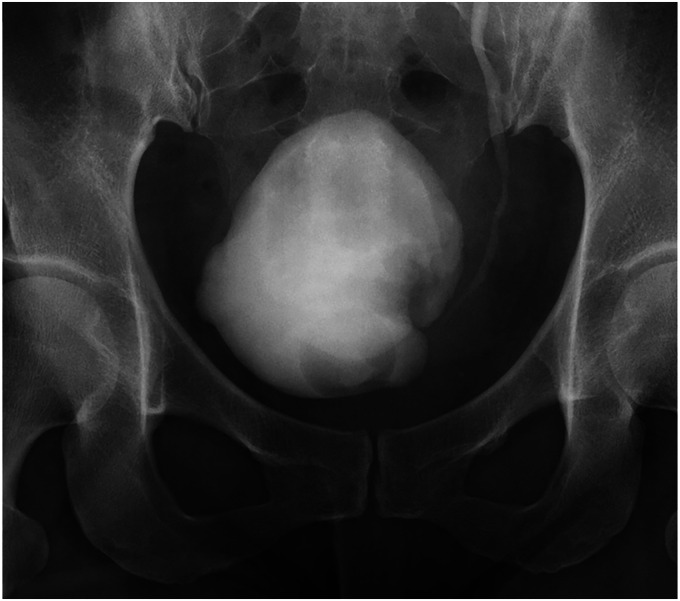
The postoperative course was uneventful. On postoperative day 7, we performed a cystographic examination, which showed a urinary bladder capacity of 250 mL. A vesicoureteral reflux (VUR) was observed when the bladder was filled to 200 mL (Fig. 4). However, after voiding, the resultant hydronephroureterosis was found to improve. Therefore, the VUR was not actively treated, and the patient was discharged the same day.
FIG. 4.
Retrograde cystography showing left hydronephroureterosis along with filling defect of the bladder at a capacity of 200 mL. Iatrogenic VUR was strongly suspected. VUR, vesicoureteral reflux.
The patient presented back to us with a complaint of urinary frequency. She was started on oral mirabegron at a dose of 50 mg/day, on an out-patient-department basis. The postoperative follow-up scheme was planned at 1-, 3-, 6-, and 18-month intervals after the surgery. No tumor recurrence was observed during the second visit, at 4 months after the surgery. Moreover, the long-term postoperative course was uneventful with no history of urinary tract infection reported during the follow-up. The patient continued to take mirabegron at a dose of 50 mg/day, with which her frequency of urination had reportedly decreased. Therefore, we continued with expectant management of the VUR.
Discussion
A leiomyoma of the urinary bladder is a rare type of tumor and accounts for <0.43% of all bladder tumors.1 The average age of presentation is reportedly 43 years, and a higher number of female patients are known to be affected.2 The bladder leiomyomas are divided into three types based on their exact location in the bladder wall as endovesical, extravesical, and the intramural leiomyomas.2,3 The commonest is the endovesical type (63%–86%), whereas the least common type is the intramural tumor (3%–7%).2,3
Our patient had the commoner endovesical leiomyoma. The endovesical bladder leiomyoma reportedly presents at various locations,3 and ∼80% of the patients affected are symptomatic.3,4 In one study conducted by Goluboff et al., 49% of patients with endovesical bladder leiomyomas presented with obstructive symptoms, because the protruding tumor blocked the bladder outlet.4 In addition, 30% of the patients presented with irritable bladder symptoms, associated with hematuria.4 Especially larger endovesical leiomyomas are known to cause symptoms of bladder irritation.3 The clinical presentation of our case was rare, because the patient was asymptomatic despite the relatively large size of the tumor (>50 mm).
There are no previous reports of a malignant transformation of a bladder leiomyoma.2,3 However, bladder leiomyomas often mimic malignant tumors, and a protocol of surgical removal and a diagnostic histopathologic examination of the extracted tumor was often preferred.3 Leiomyomas can be treated using various surgical modalities, such as open surgery, laparoscopic removal, TUR, hysteroscopic procedure, and robotic surgery.3 Tumors located in the bladder neck or large tumors (>70 mm) have been treated with partial cystectomy as reported in an earlier study.3 In our patient, the tumor was large, with a maximum diameter of 76 mm. An enucleation of the tumor through TUR was, therefore, difficult. For this reason, either laparoscopic or open surgery was indicated. We preferred to attempt an enucleation over a partial cystectomy, and achieved an effective outcome. To our knowledge, this is the first case in which a laparoscopic enucleation of bladder leiomyoma was performed for such a large tumor.
The patient was not subjected to a more invasive procedure such as an ureteroneocystostomy and her bladder capacity was conserved. As our procedure utilized simultaneous cystoscopy, we could visually delineate the surgical margin and could also confirm that the left ureteral orifice was not injured during the operative procedure. Although the bladder mucosa did sustain a minor incidental puncture intraoperatively, the defect was repaired straightforwardly during the same procedure. We believe that a cystoscope-assisted laparoscopic enucleation was the best treatment alternative, as it was less invasive and enabled us to preserve more of the bladder function than a partial cystectomy.
This case highlighted two clinically significant findings. First, a laparoscopic enucleation of a bladder leiomyoma was technically feasible, even for a large-sized tumor. Second, utilizing cystoscopy during the procedure enabled us to observe the surgical field from within the bladder, which assisted us in performing a safer laparoscopic enucleation of the leiomyoma. From these two findings, we suggest that a cystoscope-assisted robotic surgery can achieve as good an outcome as a plain laparoscopic procedure and may have other useful applications in the era of robotic surgery.
Conclusion
We reported an effective cystoscope-assisted laparoscopic enucleation of a large progressive bladder leiomyoma. The laparoscopic enucleation of a bladder leiomyoma is a technically feasible and less-invasive procedure. In addition, utilizing simultaneous cystoscopy during the operation can contribute toward a safer and a better surgical technique and improve the eventual outcome. A cystoscope-assisted robotic enucleation of the tumor can be offered as a better treatment option to the patient in the emerging era of robotic surgery.
Acknowledgment
We thank Editage for English language editing.
Abbreviations Used
- MRI
magnetic resonance imaging
- TUR
transurethral resection
- VUR
vesicoureteral reflux
Disclosure Statement
No competing financial interests exist.
Cite this article as: Yoshioka T, Kawakita M, Kameoka H (2019) Cystoscope-assisted laparoscopic enucleation of a large progressive bladder leiomyoma, Journal of Endourology Case Reports 5:3, 120–123, DOI: 10.1089/cren.2019.0015.
References
- 1. Cornella JL, Larson TR, Lee RA, et al. Leiomyoma of the female urethra and bladder: Report of twenty-three patients and review of the literature. Am J Obstet Gynecol 1997;176:1278–1285 [DOI] [PubMed] [Google Scholar]
- 2. Khater N, Sakr G. Bladder leiomyoma: Presentation, evaluation and treatment. Arab J Urol 2013;11:54–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Park JW, Jeong BC, Seo SI, et al. Leiomyoma of the urinary bladder: A series of nine cases and review of the literature. Urology 2010;76:1425–1429 [DOI] [PubMed] [Google Scholar]
- 4. Goluboff ET, O'Toole K, Sawczuk IS. Leiomyoma of bladder: Report of case and review of literature. Urology 1994;43:238–241 [DOI] [PubMed] [Google Scholar]