Abstract
This study aimed to validate the accuracy of the Omron HEM‐9601T, an automatic wrist‐type device for self‐blood pressure (BP) measurement with a timer function for automatic measurement of nocturnal BP, in the sitting position according to the American National Standards Institute/Association for the Advancement of Medical Instrumentation/International Organization for Standardization (ANSI/AAMI/ISO) 81060‐2:2013 guidelines, and to assess its performance in the supine position by applying the same protocol as conducted in the sitting position. The mean differences between the reference BPs and HEM‐9601T readings were 1.2 ± 6.9/1.1 ± 5.5 mmHg, 2.2 ± 6.5/1.8 ± 5.7 mmHg, 0.1 ± 6.6/1.5 ± 6.2 mmHg, and −0.8 ± 7.2/0.5 ± 6.4 mmHg for systolic BP/diastolic BP for criterion 1 in the sitting position, supine with sideways palm position, supine with upward palm position, and supine with downward palm position, respectively. In addition, the mean differences and their standard deviations for systolic BP and diastolic BP calculated according to criterion 2 in the ANSI/AAMI/ISO 81060‐2:2013 guidelines were acceptable in all four positions. In conclusion, the Omron HEM‐9601T fulfilled the validation criteria of the ANSI/AAMI/ISO81060‐2:2013 guidelines when used in the sitting position with the wrist at heart level, and its accuracy in the supine position was acceptable and roughly equivalent to that in the sitting position. The wrist‐type home BP monitor could be a more suitable tool for repeated nocturnal BP measurements at home than upper‐arm devices, and could improve the reliability of diagnosis and management of nocturnal hypertension.
Keywords: ANSI/AAMI/ISO81060‐2:2013, blood pressure, home nocturnal blood pressure, self‐measurement, validation, wrist‐type blood pressure monitor
1. INTRODUCTION
Several studies have reported that night‐time ambulatory blood pressure (ABPM), which is the nocturnal blood pressure (BP) obtained by a conventional arm‐cuff BP monitoring system at fixed intervals (eg, every 30 minutes), is a stronger predictor of cardiovascular events and prognosis of hypertension than either daytime ABPM or office BP 1 , 2 , 3 , 4 . Thus, ABPM has historically been the gold standard for measuring night‐time BP. In 2001, the first results of a clinical study on night‐time BP measurement by a validated oscillometric upper‐arm cuff home BP monitor were reported by a Japanese research group 5 . Since then, clinical data on nocturnal BP measurement by home BP monitoring have been accumulating globally 6 , 7 . Several studies have reported that the BP level of home nighttime BP measured by a home BP monitor is comparable to that of nighttime BP measured by ABPM 8 , 9 , 10 , 11 , 12 , 13 , and the home BP monitor and ABPM measurements show similar associations with target organ damage 9 , 12 , 13 . Recently, Kario et al. first demonstrated that nighttime systolic BP (SBP) obtained using a home device is a predictor of cardiovascular disease (CVD) events, independent of in‐office, and morning in‐home SBP measurement in patients with a history of or risk factors for CVD 14 . Based on these results, it is expected that nocturnal home BP measurements could be a reliable and practical alternative to ABPM for the evaluation of BP during sleep 15 . However, miscellaneous issues related to nocturnal BP measurement by an upper‐arm cuff home BP monitor remain to be addressed.
One major issue is that the accuracy of BP measurement by an upper arm‐cuff device during sleep might be adversely affected by the increased arousal and wakefulness induced by cuff inflation 16 . In addition, upper‐arm cuff inflation could lead to decreasing sleep quality due to disturbance of sleep 17 , 18 , 19 . To overcome this problem, there has been demand for a reliable wrist‐cuff‐type BP measurement device, since such a device would presumably cause less discomfort and muscle compression, and thus would be preferable for daily nocturnal BP monitoring 20 . Imai et al. were the first to develop a wrist‐type home nocturnal BP monitor (Omron HEM‐6310F‐N; Omron Healthcare; not yet on the market) and demonstrated based on a questionnaire administered to their participants that the wrist‐type cuff‐based device provided information on BP throughout the night with less sleep disturbance and discomfort compared to an upper arm cuff‐based device 21 . However, in the same study they also found that the SBP and diastolic BP (DBP) values obtained in the supine position using the wrist‐cuff device were higher than those obtained using the arm‐cuff device by 5.6 and 6.4 mmHg, respectively. 21
Meanwhile, we developed another wrist‐type home BP device which has a timer function for automatic nocturnal BP measurement (Omron HEM‐9600T; Omron Healthcare; not yet on the market), and conducted validation studies for the device in the sitting position with the wrist at heart level, the supine with sideways palm position, the supine with upward palm position and the supine with downward palm position 22 according to the American National Standards Institute/Association for the Advancement of Medical Instrumentation/ International Organization for Standardization (ANSI/AAMI/ISO) 81060‐2:2013 guidelines 23 . We experienced a similar problem—namely, that the SBP and DBP values obtained by the wrist‐type device in the supine with sideways palm position were higher than those measured by a mercury sphygmomanometer by 6.6 and 5.5 mmHg, respectively. Consequently, only the sitting position and supine with downward palm position fulfilled the validation criteria of the ANSI/AAMI/ISO81060‐2:2013 guidelines. We therefore developed a new wrist‐type home BP device with a timer function for automatic nocturnal BP measurement (Omron HEM‐9601T; Omron Healthcare) (Figure 1) and algorithms for both the sitting and supine positions, and improved the cuff. The purpose of this study was to validate the performance of the HEM‐9601T in the sitting position with the wrist at heart level according to the ANSI/AAMI/ISO81060‐2:2013 guidelines. In addition, to assess the performance of the Omron HEM‐9601T in the supine position, the wrist device was tested in the supine with sideways palm position, the supine with upward palm position and the supine with downward palm position according to same protocol as used for the sitting position, since there is currently no established validation protocol for the supine position.
Figure 1.
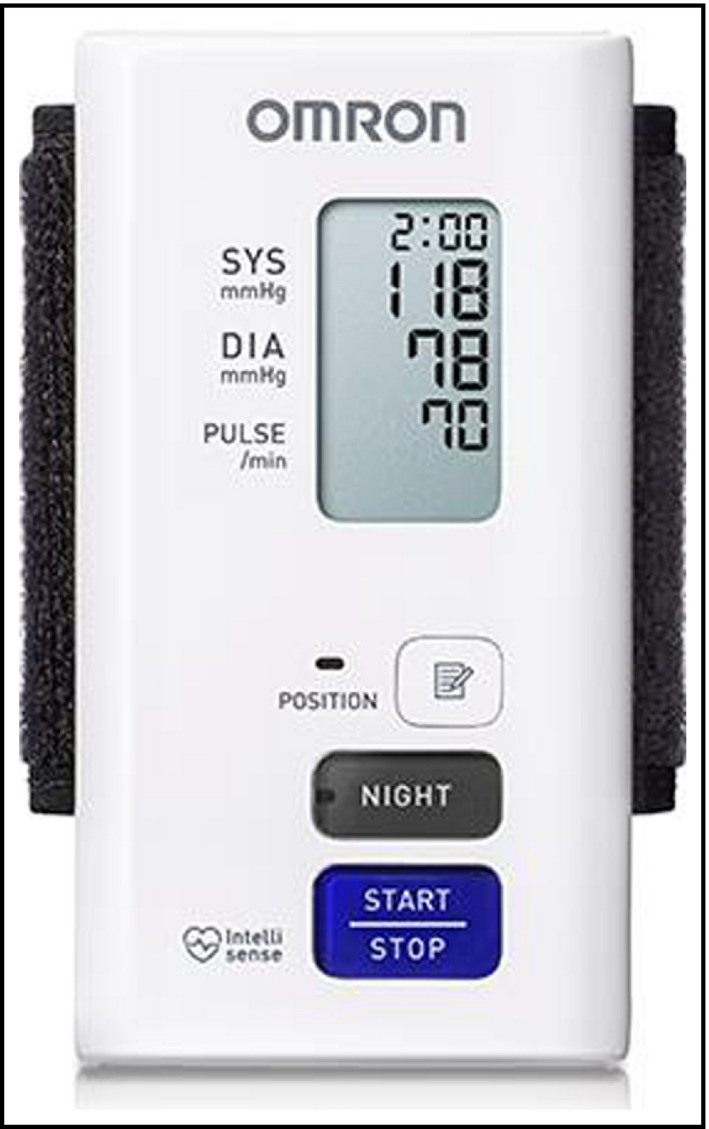
The Omron HEM‐9601T wrist‐type nocturnal home BP monitor
2. MATERIALS AND METHODS
2.1. Features of the Omron HEM‐9601T
The Omron HEM‐9601T is an automatic oscillometric device for measuring BP at the wrist, with a SBP range of 60–260 mmHg, DBP range of 40–215 mmHg and pulse rate (PR) range of 40–180 beats per min. The device measures SBP, DBP, and PR during the cuff‐inflation period. The cuff is inflated automatically by an electric pump and then deflated by a mechanical valve. The cuff can be used for wrist circumferences in the range 13.5–21.5 cm. The device has a timer function for automatic BP measurement during sleep. After entering nocturnal BP measurement mode by pushing the “NIGHT” button of the device (see Figure 1), BP measurements are automatically started using preset time points according to different timer functions: a fixed time function (eg, 2:00 am, 3:00 am), a time‐interval function (eg, every 30 minutes in the manner of ABPM), and a timer function providing BP measurements relative to the user's bedtime (eg, at 2, 3, and 4 hours after the user goes to bed).
2.2. Development of novel technology for the HEM‐9601T
Because we expected that the accuracy would be higher in the supine position, we newly developed an algorithm to determine SBP and DBP in the supine position. We optimized the parameters of this algorithm by using a dataset of SBPs and DBPs measured by a mercury sphygmomanometer at the upper arm in the supine position and those measured by the Omron HEM‐9601T in the supine position with the participant’s wrist at heart height level. The device determines SBP and DBP by using the algorithm for the supine position if the BP measurement is initiated in nocturnal BP measurement mode. In contrast, in normal BP measurement mode the device determines SBP and DBP by using the conventional algorithm for the sitting position; the normal BP measurement mode is activated by pushing the “START/STOP” button of the device (Figure 1). In addition, the HEM‐9601T has a bladder with a two‐layer structure, known as a “Sigma cuff” structure (Figure 2), and the cuff is “pre‐formed” with a plastic curler inside.
Figure 2.

Cross‐sectional diagram of a conventional cuff with a single‐layer bladder (A) and the Sigma cuff with a two‐layer bladder (B). In the case of the Sigma cuff, the flat section length of arterial occlusion is greater than in the conventional cuff due to the two‐layer bladder structure, which would lead to more adequate sensing of the cuff pressure pulse wave
2.3. Participant selection
The study design, approved by the Institutional Review Board (approval no. IRB‐1926), was organized by Omron Healthcare together with physicians from institutions unaffiliated with Omron Healthcare. All participants in this study were Japanese who were recruited as volunteers. All of them provided their written informed consent to participate in the study. The inclusion criterion was age ≥ 20 years. The exclusion criteria were arrhythmias based on the interview sheet, a DBP with an unclear Korotkoff sound, a wrist circumference smaller than 13.5 cm, and a wrist circumference larger than 21.5 cm.
2.4. Sitting and supine measurement procedures
In the supine position, we evaluated the device under three different conditions—that is, with the sideways palm position, upward palm position, and downward palm position. As a matter of course, the wrist will each rotate 90 degrees when the palm is rotated from upwards to sideways and another 90 degrees when the palm rotates from sideways to downward. The validation studies in the sitting position with the palm upward and the wrist at heart level, and in the supine with the sideways palm position were performed on the first day for each participant. The validation studies in the supine with the upward palm position and the supine with the downward palm position were performed on the second day for each participant. In the validation study of the sitting position, participants were seated in a quiet room at a comfortable room temperature, with their back supported, their legs uncrossed, and their measurement arm supported at the heart level. The participant’s arm was supported with pillows in order to keep the wrist at the heart level and the arm relaxed during BP measurement. In all the supine‐position studies, participants were lying on a bed in a relaxed position with their arms lying comfortably at their sides, and their wrists on the bed; in other words, the wrist was not adjusted to heart height level. In each study, the BP measurements were started after a 5‐min rest.
2.5. Blood pressure measurements
The device was validated on the same arm, using the sequential method described in the ANSI/AAMI/ISO 81060‐2:2013 guidelines. The manufacturer (Omron Healthcare) provided standard production device models for the sitting and supine studies. The validation team consisted of two nurses and one supervisor, who were hired by the manufacturer. The nurses were experienced in performing BP measurements and were trained by the British and Irish Hypertension Society online program (http://www.bihsoc.org). The wrist circumference was measured. All measurements in the sitting position were made on the left wrist at the heart level. All measurements in the supine position were made on the arm on the bed. For the BP measurement by the HEM‐9601T, in the validation study in the sitting position, SBP and DBP were determined by using the algorithm for the sitting position. On the other hand, SBP and DBP were determined by using the algorithm for the supine position in the validation studies in the supine positions. For the BP measurement by a mercury sphygmomanometer, two observers simultaneously measured BP using a Y tube and a calibrated mercury sphygmomanometer. SBP was determined based on phaseⅠ of the Korotkoff sound. DBP was determined based on phase Ⅴof the Korotkoff sound, except when the Korotkoff sound was still audible with the cuff deflated, in which case phase Ⅳ was used. The BP measurements for each participant were alternately performed using the mercury sphygmomanometer and the automatic device. The time interval between each set of BP measurements was ≥60 sec. Two of the observers were blinded to each other's readings, and the third observer served as a supervisor who checked the BP readings of the other two. BPs measured by the mercury sphygmomanometer were determined as the average value of BPs measured by the two observers. All data from participants were excluded as cases of “Reference BP variation” if any two reference SBP determinations differed by more than 12 mmHg or if any two reference DBP determinations differed by more than 8 mmHg.
2.6. Analysis of the BP data
In each study, the BP and other data were analyzed according to the ANSI/AAMI/ISO81060‐2:2013 guidelines. The first BP measurements taken with the mercury sphygmomanometer and the automatic device were not applied in the analysis. In each study, analysis was performed according to criteria 1 and 2 as follows.
For criterion 1, we calculated the differences defined as the SBP or DBP value measured by the HEM‐9601T minus the mean value of SBP or DBP measured by the mercury sphygmomanometer before and after BP measurement by the HEM‐9601T. Three difference values were calculated for each participant. The mean value and standard deviation (SD) of these difference values were calculated in each study.
For criterion 2, the reference SBP or DBP value was defined as the mean value of SBP or DBP measured by the mercury sphygmomanometer at the current and previous measurement sessions. We calculated the differences defined as the mean value of three SBPs or DBPs measured by the HEM‐9601T minus the mean value of three reference SBPs or DBPs. The mean value and SD of these difference values were calculated in each study.
3. RESULTS
Table 1 summarizes the participant recruitment details for each study. After excluding participants for the reasons shown in Table 1, a group of 85 participants common to all four studies were selected for the analysis in each study. The characteristics of these 85 study participants are shown in Table 2. All the percentages of participants with wrist circumferences of 13.5–15.4 cm, 13.5–17.4 cm, 17.5–21.5 cm, and 19.5–21.5 cm fulfilled the criteria of ISO81060‐2:2013 (≥20%, ≥40%, ≥40%, and ≥20%, respectively). Table 3 shows reference SBP and DBP values for the participants in each validation study (n = 255). Figure 3 and Figure 4 show Bland‐Altman plots for the differences between the Omron HEM‐9601T readings and the observer measurements for SBP and DBP, respectively.
Table 1.
Recruitment details for each validation study
| Screening and recruitment | Validation for HEM‐9601T | |||
|---|---|---|---|---|
| Sitting | Supine with sideways palm | Supine with upward palm | Supine with downward palm | |
| Total screened, n | 99 | 102 | 91 | 91 |
| Total excluded, n | 14 | 17 | 6 | 6 |
| Poor quality sounds | 0 | 1 | 0 | 0 |
| Body movements, n | 0 | 0 | 1 | 1 |
| Reference blood pressure variation, n | 3 | 7 | 2 | 4 |
| Incorrect wearing of the cuff | 1 | 1 | 1 | 0 |
| Excluded from the sitting position study | 0 | 1 | 0 | 0 |
| Excluded from the supine with sideways palm position study | 3 | 0 | 0 | 0 |
| Excluded from the supine with upward palm position study | 1 | 1 | 0 | 1 |
| Excluded from the supine with downward palm position study | 2 | 2 | 2 | 0 |
| Participant was unavailable for the supine with upward and/or downward palm position study | 4 | 4 | 0 | 0 |
| Total recruited, n | 85 | 85 | 85 | 85 |
Table 2.
Characteristics of the study participants (n = 85)
| Age, y (range) | 54.6 ± 13.3 (21‐82) |
| Men : women, n (%) | 44 : 41 (51.8, 48.2) |
| Wrist circumstance, cm (range) | 17.2 ± 2.2 (13.5‐21.4) |
| Percentage of the participants with 13.5‐15.4 cm, % | 28.2 |
| Percentage of the participants with 13.5‐17.4 cm, % | 56.5 |
| Percentage of the participants with 17.5‐21.5 cm, % | 43.5 |
| Percentage of the participants with 19.5‐21.5 cm, % | 20.0 |
Data are expressed as the means ± standard deviation or percentages or number.
Table 3.
Reference SBP and DBP of the participants in each validation study (n = 255)
| Validation for HEM‐9601T | ||||
|---|---|---|---|---|
| Sitting | Supine with sideways palm | Supine with upward palm | Supine with downward palm | |
| Reference SBP, mmHg (range) |
125.2 ± 22.0 (85.3‐188.5) |
125.3 ± 22.5 (86.0‐189.0) |
124.4 ± 21.1 (90.0‐179.8) |
125.9 ± 22.3 (87.5‐187.5) |
| Percentage with high SBP (≥160 mmHg), % | 8.6 | 9.8 | 7.1 | 9.4 |
| Percentage with medium SBP (≥140 mmHg), % | 25.9 | 28.6 | 22.7 | 23.5 |
| Percentage with low SBP (≤100 mmHg), % | 11.4 | 12.5 | 14.1 | 12.9 |
| Reference DBP, mmHg (range) |
79.7 ± 14.6 (51.5‐118.0) |
76.8 ± 14.4 (45.8‐109.5) |
74.7 ± 13.8 (44.5‐110.5) |
76.6 ± 13.9 (50.3‐114.3) |
| Percentage with high DBP (≥100 mmHg), % | 11.4 | 7.5 | 2.4* | 5.5 |
| Percentage with medium DBP (≥85 mmHg), % | 34.5 | 29.4 | 28.2 | 28.6 |
| Percentage with low DBP (≤60 mmHg), % | 8.2 | 11.8 | 13.3 | 10.2 |
Data are expressed as the means ± standard deviation or percentages.
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
Limitation: The percentage of participants with high DBP (≥100 mmHg) in the study of the supine with upward palm position did not fulfill the criteria of ISO81060‐2:2013 (≥5%).
Figure 3.

Bland‐Altman plots of the differences between the Omron HEM‐9601T readings and the observer measurements for systolic blood pressure in the sitting position (A), the supine position with sideways palm (B), the supine position with upward palm (C), and the supine position with downward palm (D) (N = 255)
Figure 4.

Bland‐Altman plots of the differences between the Omron HEM‐9601T readings and the observer measurements for diastolic blood pressure in the sitting position (A), the supine position with sideways palm (B), the supine position with upward palm (C), and the supine position with downward palm (D) (N = 255)
The differences in absolute BP value between the two observers ranged from 0 mmHg to 4 mmHg both for SBP and DBP in all four positions. Therefore, there were no reference BP readings which were repeated due to disagreement between observers in all four positions (a criterion of less than 4 mmHg disagreement was used). The mean differences between the reference BPs and HEM‐9601T readings for SBP and DBP according to criterion 1 and criterion 2 are shown in Table 4. These results indicate the HEM‐9601T fulfilled the validation criteria of the ISO81060‐2:2013 (≤5 ± ≤8.0 mmHg for criterion 1; the SD should be less than the threshold shown in Table 4) in all four positions.
Table 4.
Results of each validation study
| Validation for HEM‐9601T | ||||
|---|---|---|---|---|
| Sitting | Supine with sideways palm | Supine with upward palm | Supine with downward palm | |
| Difference in SBP for criterion 1, mmHg |
1.2 ± 6.9 (passed) |
2.2 ± 6.5 (passed) |
0.1 ± 6.6 (passed) |
−0.8 ± 7.2 (passed) |
| Difference in SBP for criterion 2, mmHg |
1.2 ± 5.9 (6.8) (passed) |
2.2 ± 5.6 (6.5) (passed) |
0.1 ± 6.0 (6.9) (passed) |
−0.8 ± 6.1 (6.8) (passed) |
| Difference in DBP for criterion 1, mmHg |
1.1 ± 5.5 (passed) |
1.8 ± 5.7 (passed) |
1.5 ± 6.2 (passed) |
0.5 ± 6.4 (passed) |
| Difference in DBP for criterion 2, mmHg |
1.1 ± 4.9 (6.8) (passed) |
1.8 ± 5.1 (6.7) (passed) |
1.5 ± 5.6 (6.7) (passed) |
0.5 ± 5.9 (6.9) (passed) |
Data are expressed as the means ± standard deviation and the means ± standard deviation (threshold of the standard deviation) for criterion 1 and criterion 2, respectively.
4. DISCUSSION
In this study, we demonstrated that the Omron HEM‐9601T device, a wrist‐type home nocturnal BP monitor, fulfilled the validation criteria of the ANSI/AAMI/ISO81060‐2:2013 guidelines in the sitting position. Additionally, we demonstrated that the accuracies of the HEM‐9601T device in the supine with downwards palm position, in the supine with upward palm position and in the supine with downward palm position were acceptable and roughly equivalent to those in the sitting position.
4.1. Accuracy improvement of the mean differences between the reference BPs and HEM‐9601T readings
Compared to those in the previous validation study for a wrist‐type nocturnal BP monitor (HEM‐9600T) 22 , the mean differences between the reference BPs and BP readings in the present validation study of the HEM‐9601T were dramatically improved in three supine positions, with a maximum improvement of 4.4 mmHg for SBP in the case of the supine with sideways palm position. These results might be attributable to our newly developed algorithm for the supine position, because the algorithm was developed by using a dataset of BPs obtained by a mercury sphygmomanometer and the HEM‐9601T, both in the supine position. In the case of conventional wrist‐type BP devices, the parameters of the algorithm used to determine SBP and DBP were optimized by using BP datasets from several participants obtained by a mercury sphygmomanometer and a wrist device, both in the sitting position. Therefore, the accuracy of the wrist device is only guaranteed in the case of BP measurement conducted in the sitting position—specifically, in the sitting position with the wrist and palm in the same angle and posture as for the BP data collection conducted to develop the algorithm. By changing the position from sitting to supine, the degree of amplification between the brachial artery and radial or ulnar artery might differ. In addition, the positional relationships between the radial artery or ulnar artery and radius or tendon in the supine position, especially with the sideways palm position, might differ from those in the sitting position with palm upward, which was the position used for the BP data collection when developing the algorithm. These differences in the measurement conditions might be the cause of the large differences in the mean differences between the reference BPs and wrist device readings. In this study, although we used the algorithm for the supine position, mean differences of 2.2 mmHg for SBP and 1.8 mmHg for DBP remained between the reference BPs and HEM‐9601T readings in the supine with sideways palm position. This might have been due to the difference in the height from the bed between the wrist and upper arm in the supine position. Some previous studies demonstrated that BP differs by 7 mmHg if the height difference between the heart level and cuff position is 10 cm 24 , 25 due to hydrostatic pressure. In this study, the mean height difference between the height from the bed at the middle of the upper arm and the height from the bed at the middle of the wrist in the supine position was 1.7 cm. Based on this result, it is estimated that 1.2 mmHg, which is almost half of the total difference of 2.2 mmHg for SBP, could be attributed to the height difference between the arm and wrist in the supine position. Because the supine‐position algorithm cannot automatically compensate for the height difference between the wrist and the upper arm, it will be necessary to develop technologies that can automatically detect this height difference and adjust the BP values accordingly. Such technologies will be especially crucial for night‐time BP measurement under real‐world sleeping conditions.
4.2. Accuracy improvement of the SD of the mean differences
In this study, the SD of the mean differences between the reference BPs and HEM‐9601T readings were relatively improved in all three supine positions compared to those in the previous validation study for the HEM‐9600T 22 . These results might be attributable to an improvement of the cuff for the HEM‐9601T. The HEM‐9601T has a bladder with a two‐layer “Sigma cuff” structure, and the cuff is “pre‐formed” with a plastic curler inside. In the case of the Sigma cuff, due to the two‐layer structure of the bladder, the flat section length of arterial occlusion could be greater than in a conventional cuff of the same width. This advantage is expected to lead to more adequate sensing of the cuff pressure pulse wave. For the pre‐formed cuff, it is expected that the structure of the plastic curler will function as a backboard to the bladder, which would lead to an increase in the stroke volume, and thereby an increase in the cuff inflation to press the blood vessels vertically. Such an increase in the stroke volume of the cuff would help the cuff to occlude the artery effectively, resulting in adequate sensing of the cuff pressure pulse wave. These phenomena might have contributed to the observed decrease in the SD of the mean differences between the reference BPs and HEM‐9601T readings.
4.3. Limitation and future perspectives
For now, there are no established validation protocols and no requirements for an automatic oscillometric BP monitor in the supine position. Therefore, in a strict sense, the results of this study in the supine position should be regarded as a reference for clinical practice. In this study, to compare the accuracy performance of the HEM‐9601T in the sitting position, the supine with sideways palm position, the supine with upward palm position and the supine with downward palm position, a group of 85 participants common to all four studies were selected for the analysis in each study. The distribution of the reference SBP and DBP in the sitting position fulfilled the criteria of the ISO81060‐2:2013 guidelines. However, in the analyses of the three supine positions, although the distribution of the reference SBP in all three supine positions and those of the reference DBP in the supine with sideways palm position and supine with downward palm position fulfilled the criteria of the guidelines, the distribution of the reference DBP in the supine with upward palm position did not fulfill the criteria. This may have been attributable to day‐by‐day BP variability and/or the difference of body position between sitting and supine. Moreover, this study was conducted under laboratory conditions by well‐trained nurses. Therefore, the accuracy of HEM‐9601T demonstrated in this study can only be guaranteed under laboratory conditions. The accuracy of the wrist device should be further evaluated under real‐world conditions. In particular, a future study evaluating the difference between nighttime BP measured by a wrist‐type BP monitor and that measured by an upper‐arm BP monitor under real‐world sleeping conditions will be needed in order to assess how the wrist‐type BP monitor is adopted and experienced by users for monitoring night‐time BP.
5. CONCLUSION
The Omron HEM‐9601T fulfilled the validation criteria of the ANSI/AAMI/ISO81060‐2:2013 guidelines when used in the sitting position with the wrist at heart level, and its accuracy in the supine position was acceptable and roughly equivalent to that in the sitting position. These results indicate that the accuracy of the Omron HEM‐9601T, a wrist‐type home nocturnal BP monitor, is acceptable not only in the sitting position but also in the supine position when the algorithm for the sitting or supine position is appropriately chosen depending on the position of the patient. A wrist‐type home BP monitor could be a more suitable tool for repeated nocturnal BP measurements at home than an upper‐arm device, and could improve the reliability of diagnosis and management of nocturnal hypertension.
DISCLOSURE
Y Imai, T Ohkubo and K Kario received research grants from Omron Healthcare, and are consultants for Omron Healthcare.
AUTHOR CONTRIBUTIONS
1) Conception: Mitsuo Kuwabara PhD, 2) Drafting of the manuscript or critical revision for important intellectual content: Mitsuo Kuwabara PhD, 3) Final approval of the submitted manuscript: Mitsuo Kuwabara PhD, Kanako Harada MPH, Yukiko Hishiki BA, Takayoshi Ohkubo MD, PhD, Kazuomi Kario MD, PhD, and Yutaka Imai MD, PhD.
ACKNOWLEDGMENTS
We gratefully acknowledge the volunteers who agreed to have their BP measured for the purpose of this study.
Kuwabara M, Harada K, Hishiki Y, Ohkubo T, Kario K, Imai Y. Validation of a wrist‐type home nocturnal blood pressure monitor in the sitting and supine position according to the ANSI/AAMI/ISO81060‐2:2013 guidelines: Omron HEM‐9601T. J Clin Hypertens. 2020;22:970–978. 10.1111/jch.13864
Funding information
This research was conducted by research funds from Omron Healthcare.
References
- 1. Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA. 1999;282:539–546. [DOI] [PubMed] [Google Scholar]
- 2. Kikuya M, Ohkubo T, Asayama K, et al. Ambulatory blood pressure and 10–year risk of cardiovascular and noncardiovascular mortality: the Ohasama study. Hypertension. 2005;45:240–245. [DOI] [PubMed] [Google Scholar]
- 3. Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–1229. [DOI] [PubMed] [Google Scholar]
- 4. Investigators T‐H, Roush GC, Fagard RH, et al. Prognostic impact from clinic, daytime, and night‐time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014;32:2332–2340. [DOI] [PubMed] [Google Scholar]
- 5. Chonan K, Kikuya M, Araki T, et al. Device for the self‐measurement of blood pressure that can monitor blood pressure during sleep. Blood Press Monit. 2001;6:203–205. [DOI] [PubMed] [Google Scholar]
- 6. Kollias A, Ntineri A, Stergiou GS. Association of night‐time home blood pressure with night‐time ambulatory blood pressure and target organ damage: a systematic review and meta‐analysis. J Hypertens. 2017;35:442–452. [DOI] [PubMed] [Google Scholar]
- 7. Kario K. Nocturnal Hypertension: New Technology and Evidence. Hypertension. 2018;71:997–1009. [DOI] [PubMed] [Google Scholar]
- 8. Ushio H, Ishigami T, Araki N, et al. Utility and feasibility of a new programmable home blood pressure monitoring device for the assessment of night‐time blood pressure. Clin Exp Nephrol. 2009;13:480–485. [DOI] [PubMed] [Google Scholar]
- 9. Ishikawa J, Hoshide S, Eguchi K, et al. Japan Morning Surge‐Home Blood Pressure Study Investigators Group. Night‐time home blood pressure and the risk of hypertensive target organ damage. Hypertension. 2012;60:921–928. [DOI] [PubMed] [Google Scholar]
- 10. Stergiou GS, Nasothimiou EG, Destounis A, Poulidakis E, Evagelou I, Tzamouranis D. Assessment of the diurnal blood pressure profile and detection of non‐dippers based on home or ambulatory monitoring. Am J Hypertens. 2012;25:974–978. [DOI] [PubMed] [Google Scholar]
- 11. Ishikawa J, Shimizu M, Sugiyama Edison E, et al. Assessment of the reductions in night‐time blood pressure and dipping induced by antihypertensive medication using a home blood pressure monitor. J Hypertens. 2014;32:82–89. [DOI] [PubMed] [Google Scholar]
- 12. Andreadis EA, Agaliotis G, Kollias A, Kolyvas G, Achimastos A, Stergiou GS. Night‐time home versus ambulatory blood pressure in determining target organ damage. J Hypertens. 2016;34:438–444. [DOI] [PubMed] [Google Scholar]
- 13. Lindroos AS, Johansson JK, Puukka PJ, et al. The association between home vs. ambulatory night‐time blood pressure and end‐organ damage in the general population. J Hypertens. 2016;34:1730–1737. [DOI] [PubMed] [Google Scholar]
- 14. Kario K, Kanegae H, Tomitani N, et al. Nighttime blood pressure measured by home blood pressure monitoring as an independent predictor of cardiovascular events in general practice. Hypertension. 2019;73(6):1240–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Asayama K, Fujiwara T, Hoshide S, et al. International Expert Group of Nocturnal Home Blood Pressure. Nocturnal blood pressure measured by home devices: evidence and perspective for clinical application. J Hypertens. 2019;37(5):905–916. [DOI] [PubMed] [Google Scholar]
- 16. Dimsdale JE, Coy TV, Ancoli‐Israel S, Clausen J, Berry CC. The effect of blood pressure cuff inflation on sleep. A polysomnographic examination. Am J Hypertens. 1993;6:888–891. [DOI] [PubMed] [Google Scholar]
- 17. Alessi A, Alessi CR, Piana ER, Assis M, Oliveira LR, Cunha CL. Influence of quality of sleep on the nocturnal decline in blood pressure during ambulatory blood pressure monitoring. Arq Bras Cardiol. 2002;78:212–223. [DOI] [PubMed] [Google Scholar]
- 18. Beltman FW, Heesen WF, Smit AJ, May JF, Lie KI, Meyboom‐de JB. Acceptance and side effects of ambulatory blood pressure monitoring: evaluation of a new technology. J Hum Hypertens. 1996;10(Suppl 3):S39–S42. [PubMed] [Google Scholar]
- 19. Mallion JM, de Gaudemaris R, Baguet JP, et al. Acceptability and tolerance of ambulatory blood pressure measurement in the hypertensive patient. Blood Press Monit. 1996;1:197–203. [PubMed] [Google Scholar]
- 20. Veerman DP, van Montfrans GA, Wieling W. Effects of cuff inflation on self‐recorded blood pressure. Lancet. 1990;335:451–453. [DOI] [PubMed] [Google Scholar]
- 21. Imai Y, Asayama K, Fujiwara S, et al. Development and evaluation of a home nocturnal blood pressure monitoring system using a wrist‐cuff device. Blood Press Monit. 2018;23(6):318–326. [DOI] [PubMed] [Google Scholar]
- 22. Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of a wrist‐type home nocturnal blood pressure monitor in the sitting and supine position according to the ANSI/AAMI/ISO81060‐2:2013 guidelines: Omron HEM‐9600T. J Clin Hypertens (Greenwich). 2019;21(4):463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Association for the Advancement of Medical Instrumentation . American National Standard: Non‐invasive sphygmomanometers – part 2: Clinical validation of automated measurement type; ANSI/AAMI/ISO. 81060–2. 2013. http://my.aami.org/store/detail.aspx‐?id=8106002. Accessed August 1st, 2019.
- 24. Kikuya M, Chonan K, Imai Y, Goto E, Ishii M. Research Group to Assess the Validity of Automated Blood Pressure Measurement Devices in Japan. Accuracy and reliability of wrist‐cuff devices for self‐measurement of blood pressure. J Hypertens. 2002;20:629–638. [DOI] [PubMed] [Google Scholar]
- 25. Yarows SA. Comparison of the Omron HEM‐637 wrist monitor to the auscultation method with the wrist position sensor on or disabled. Am J Hypertens. 2004;17:54–58. [DOI] [PubMed] [Google Scholar]


