Abstract
OBJECTIVES
To examine the longitudinal association between frequency of moderate physical activity (PA) and overall, physical, psychological, and social frailty among community‐dwelling older adults older than 70 years. Second, we assessed the association between a 12‐month change in frequency of moderate PA and frailty.
DESIGN
Longitudinal cohort study.
SETTING
Community settings in Spain, Greece, Croatia, the Netherlands, and the United Kingdom.
PARTICIPANTS
A total of 1735 participants (61.1% female; mean age = 79.6 years; SD = 5.5 years).
MEASUREMENTS
The frequency of self‐reported moderate PA was measured and classified into two categories: “regular frequency” and “low frequency.” The 12‐month change in frequency of moderate PA between baseline and follow‐up was classified into four categories: “continued regular frequency,” “decreased frequency,” “continued low frequency,” and “increased frequency.” The 15‐item Tilburg Frailty Indicator assessed overall, physical, psychological, and social frailty.
RESULTS
Participants who undertook moderate PA with a regular frequency at baseline were less frail at 12‐month follow‐up than participants with a low frequency. Participants who undertook moderate PA with a continued regular frequency were least frail at baseline and at 12‐month follow‐up. After controlling for baseline frailty and covariates, compared with participants with a continued regular frequency, participants with a decreased frequency were significantly more overall (B = 1.31; 95% confidence interval [CI] = 0.99‐1.63), physically (B = 0.80; 95% CI = 0.58‐1.03), psychologically (B = 0.43; 95% CI = 0.30‐0.56), and socially frail (B = 0.14; 95% CI = 0.04‐0.23) at 12‐month follow‐up; participants with a continued low frequency were significantly more overall (B = 1.16; 95% CI = 0.84‐1.49), physically (B = 0.73; 95% CI = 0.51‐0.96), psychologically (B = 0.42; 95% CI = 0.29‐0.55), and socially frail (B = 0.13; 95% CI = 0.04‐0.23) at 12‐month follow‐up; the 12‐month follow‐up frailty level of participants who undertook moderate PA with an increased frequency was similar to those with a continued regular frequency.
CONCLUSION
Maintaining a regular frequency of PA as well as increasing to a regular frequency of PA are associated with maintaining or improving overall, physical, psychological, and social frailty among European community‐dwelling older adults older than 70 years. J Am Geriatr Soc 68:1484‐1493, 2020.
Keywords: frailty, physical activity, physical frailty, psychological frailty, social frailty
Frailty is a multidimensional concept characterized by the loss of reserves, including energy, physical ability, cognition, and health. The prevalence of frailty strongly increases with age.1 According to the 2018 Ageing Report of the European Commission, the percentage of European citizens aged 65 years or older will rise from 19% in 2018 to 29% in 2070.2 This increase is predominantly caused by the percentage of citizens aged 80 years and older.2, 3 Hence, it is anticipated that frailty will pose a larger public health problem in the near future.3, 4, 5
Maintaining a healthy lifestyle in older age is associated with a lower level of frailty.3, 6, 7, 8 However, studies on the association between physical activity (PA) and frailty among older adults show contradictory results. Some studies4, 9, 10, 11 suggest that regular PA may delay the onset of frailty and reduce its severity, but others12 found that PA was not associated with a decreased risk for frailty among older adults. Second, most of the longitudinal studies on PA and frailty examine baseline PA only in relation to changes in frailty,11, 13 and evidence on the association between change in PA and frailty is limited. Additionally, most studies7, 11, 14, 15 on PA and frailty have been conducted in adults aged 50 to 70 years, and evidence on the longitudinal association between PA and frailty in adults older than 70 years is relatively scarce.
Due to the multidimensional nature of frailty, it has been suggested that the physical, psychological, and social dimensions of frailty should be considered.16 However, most previous studies on PA and frailty have focused on physical frailty only,4, 9, 11, 12, 13 and to date there has been little research into psychological and social frailty.
Therefore, the aim of our study was to examine the longitudinal association between frequency of moderate PA and overall, physical, psychological, and social frailty among community‐dwelling older adults older than 70 years. Second, we assessed the association between a 12‐month change in frequency of moderate PA and frailty.
1. METHODS
1.1. Participants
This study is part of the Urban Health Centres Europe (UHCE) project, which is aimed at promoting healthy aging in older adults by means of integrated care pathways covering the adherence to medication, prevention of falls and frailty, and loneliness.17, 18 Integrated care pathways were implemented in community settings at study sites in five European countries (Spain, Greece, Croatia, the Netherlands, and the United Kingdom). At each study site, adults older than 70 years, who lived independently and were expected to be able to participate in the study for at least 6 months, were invited to participate. A total of 2325 participants were recruited between May 2015 and June 2017; 1215 were included in an integrated care pathway intervention; 1110 were enrolled in the control group. Participants in the intervention group received care in accordance with the UHCE approach, which comprised three stages: risk assessment, shared decision making, and referral to care pathways aimed at reducing fall risk, inappropriate medication use, loneliness, and frailty by specific interventions.18 Further details on these interventions are described elsewhere.17, 18 Data were obtained from self‐reported questionnaires at baseline and at 12 months of follow‐up. Ethics committee procedures were followed at all study sites, and approval was obtained.17 Written informed consent was obtained from all participants.17, 18
The current study included participants in the UHCE project who had completed both baseline and follow‐up questionnaires (n = 1844).18 Participants in whom data on PA (N = 71) and frailty (N = 38) were missing were excluded. Thus, 1735 participants were included in the analyses of the current study.
Compared with the study population (n = 1735), the participants excluded from the study due to missing data on PA and frailty (N = 109) were younger (mean age = 77.1 years; SD = 6.1 years; P < .001), had less often completed tertiary education (P = .016), more often lived alone (P < .001), and were less often at risk for alcohol use (P = .045). No other significant differences between these two groups were found.
1.2. Measurements
1.2.1. Physical Activity
The frequency of moderate PA was measured by means of one question from the Frailty Instrument of the Survey of Health, Ageing and Retirement in Europe: “How often do you engage in activities that require a low or moderate level of energy such as gardening, cleaning the car, or taking a walk?”19, 20 Answer categories included (a) more than once a week, (b) once a week, (c) one to three times a month, and (d) hardly ever or never. For our study, we classified these into two categories: “regular frequency” (more than once a week) and “low frequency” (once a week or less). We classified the change in the frequency of moderate PA between baseline and follow‐up into four categories: (1) “continued regular frequency” (more than once a week), (2) “decreased frequency,” (3) “continued low frequency” (once a week or less), and (4) “increased frequency.”
1.2.2. Frailty
Frailty was measured with the Tilburg Frailty Indicator (TFI), which is a reliable and validated instrument to identify frailty in community‐dwelling older adults.21 The TFI comprises 15 self‐reported questions addressing three domains: physical frailty (eight items; score range = 0‐8), psychological frailty (four items; score range = 0‐4), and social frailty (three items; score range = 0‐3). An overall frailty score can be determined by adding up the 15 items (score range = 0‐15), with higher scores representing a higher level of frailty.22
1.2.3. Covariates
Some covariates were assessed at baseline, including age (in years), sex, country, educational level, living situation, smoking, alcohol risk, and multimorbidity. Educational level concerned the highest level of education completed by the participant and was categorized according to the 2011 International Standard Classification of Education (ISCED) into primary or less (ISCED 0‐1), secondary or equivalent (ISCED 2‐5), and tertiary or higher (ISCED 6‐8).23 Living situation was categorized as “not living with others” or “living with others” (a partner, child[ren], and/or others). Smoking was measured with one item that assessed whether a person currently smoked. Alcohol risk was measured with the Alcohol Use Disorder Identification Test (AUDIT‐C),24 which is a three‐item screener to grade high‐risk alcohol use on a scale from 0 (lowest risk) to 12 (highest risk). A score of at least four for men and three for women was regarded as hazardous drinking or active alcohol use disorder.24 Multimorbidity was defined as having at least two of the following 14 chronic conditions25: heart attack, hypertension, diabetes, stroke, high blood cholesterol, asthma, arthritis, osteoporosis, chronic lung disease, cancer or malignant tumor, stomach or duodenal ulcer, Parkinson's disease, cataract, and hip fracture or femoral fracture.26
1.3. Statistical Analysis
The longitudinal association between frequency of moderate PA and frailty was estimated with multivariate linear regression models. Four separate regression models were built for overall, physical, psychological, or social frailty at follow‐up as dependent variable and frequency of moderate PA at baseline as independent variable. The first set of models was adjusted for country and for frailty at baseline (crude model). The second set of models was additionally adjusted for age, sex, educational level, living situation, smoking, alcohol risk, and multimorbidity (adjusted model). Since the UHCE project was an intervention study and participants were divided over an intervention and a control group, intervention condition was also added to the adjusted mode as a covariate.
The association between the 12‐month change in frequency of moderate PA and overall, physical, psychological, or social frailty was assessed using the same crude and adjusted multivariate linear regression models as described above, taking change in frequency of moderate PA as the independent variable.
Furthermore, interactions between baseline frequency of moderate PA or 12‐month change in frequency of moderate PA and age, sex, country, educational level, living situation, and intervention on the frailty scores were assessed with UNIANOVA. Bonferroni correction was applied for multiple testing (P = .05/48 = .001). Apart from an interaction between country and change in frequency of moderate PA regarding psychological frailty, no statistically significant interaction was found. All P values of the interaction analyses are presented in Supplementary Table S1.
Finally, sensitivity analyses were performed where all analyses were repeated using the participants in the control group only; we found similar results.
All analyses were performed with SPSS version 23.0 (IBM SPSS Statistics for Windows; IBM Corp). The level of significance was P < .05.
2. RESULTS
2.1. Baseline Characteristics of Participants
Table 1 shows the general characteristics of the study population at baseline. The mean age of participants was 79.6 (SD = 5.5) years, and 61.1% were female. Compared with participants who undertook moderate PA with a regular frequency, participants with a low frequency of moderate PA were older (P < .001), were more often female (P < .001), had less often completed tertiary level education (P < .001), were less often at risk for alcohol use (P < .001), and more often experienced multimorbidity (P = .004).
Table 1.
Baseline Characteristics of Participants in the Analyses (n = 1735)
| Items | Total (n = 1735) | Baseline Frequency of Moderate PA | 12‐mo Change in Moderate PA | ||||
|---|---|---|---|---|---|---|---|
| Regular Frequency (n = 1272) | Low Frequency (n = 463) | Continued Regular Frequency (n = 1020) | Decreased Frequency (n = 252) | Continued Low Frequency (n = 302) | Increased Frequency (n = 161) | ||
| Age, y | 79.6 ± 5.5 | 79.1 ± 5.3a | 81.2 ± 5.8a | 78.8 ± 5.2b | 80.3 ± 5.6b | 81.9 ± 5.9b | 79.9 ± 5.4b |
| Sex | |||||||
| Male | 675 (38.9) | 532 (41.8)b | 143 (30.9)b | 430 (42.2)b | 102 (40.5)b | 84 (27.8)b | 59 (36.6)b |
| Female | 1060 (61.1) | 740 (58.2)b | 320 (69.1)b | 590 (57.8)b | 150 (59.5)b | 218 (72.2)b | 102 (63.4)b |
| Country | |||||||
| Spain | 394 (22.7) | 327 (25.7)c | 67 (14.5)c | 288 (28.2)c | 39 (15.5)c | 25 (8.3)c | 42 (26.1)c |
| Greece | 209 (12.0) | 149 (11.7)c | 60 (13.0)c | 101 (9.9)c | 48 (19.0)c | 44 (14.6)c | 16 (9.9)c |
| Croatia | 418 (24.1) | 255 (20.0)c | 163 (35.2)c | 185 (18.1)c | 70 (27.8)c | 128 (42.4)c | 35 (21.7)c |
| NL | 265 (15.3) | 203 (16.0)c | 62 (13.4)c | 161 (15.8)c | 42 (16.7)c | 30 (9.9)c | 32 (19.9)c |
| UK | 449 (25.9) | 338 (26.6)c | 111 (24.0)c | 285 (27.9)c | 53 (21.0)c | 75 (24.8)c | 36 (22.4)c |
| Educational level | |||||||
| Tertiary | 173 (10.0) | 147 (11.6)c | 26 (5.6)c | 110 (10.8)c | 37 (14.7)c | 15 (5.0)c | 11 (6.9)c |
| Secondary | 1125 (65.1) | 790 (62.4)c | 335 (72.7)c | 638 (62.9)c | 152 (60.6)c | 228 (75.5)c | 107 (67.3)c |
| Primary or less | 429 (24.8) | 329 (26.0)c | 100 (21.7)c | 267 (26.3)c | 62 (24.7)c | 59 (19.5)c | 41 (25.8)c |
| Living situation | |||||||
| Living with others | 1054 (60.9) | 790 (62.2) | 264 (57.4) | 631 (62.0) | 159 (63.1) | 170 (56.3) | 94 (59.5) |
| Living alone | 676 (39.1) | 480 (37.8) | 196 (42.6) | 387 (38.0) | 93 (36.9) | 132 (43.7) | 64 (40.5) |
| Smoking | |||||||
| No | 1601 (92.4) | 1166 (91.7) | 435 (94.4) | 941 (92.3) | 225 (89.3) | 284 (94.7) | 151 (93.8) |
| Yes | 131 (7.6) | 105 (8.3) | 26 (5.6) | 78 (7.7) | 27 (10.7) | 16 (5.3) | 10 (6.2) |
| Alcohol risk | |||||||
| No | 1198 (72.6) | 823 (68.5)c | 375 (83.7)c | 660 (68.1)c | 163 (70.0)c | 255 (87.3)c | 120 (76.9)c |
| Yes | 452 (27.4) | 379 (31.5)c | 73 (16.3)c | 309 (31.9)c | 70 (30.0)c | 37 (12.7)c | 36 (23.1)c |
| Multimorbidity | |||||||
| No | 162 (9.3) | 134 (10.5)d | 28 (6.0)d | 113 (11.1)d | 21 (8.3)d | 12 (4.0)d | 16 (9.9)d |
| Yes | 1573 (90.7) | 1138 (89.5)d | 435 (94.0)d | 907 (88.9)d | 231 (91.7)d | 290 (96.0)d | 145 (90.1)d |
Note: Data presented as mean ± SD or number (percentage). Missing items: age = 1; education level = 8; living situation = 5; smoking = 3; alcohol risk = 85.
Abbreviations: NL, the Netherlands; PA, physical activity; UK, the United Kingdom.
P < .001; P values are based on independent t test.
P < .001; P values are based on one‐way analysis of variance.
P < .001; P values are based on χ2 tests.
P < .01; P values are based on χ2 tests.
Figure 1 shows the frequency of moderate PA of participants at baseline and follow‐up as well as change in frequency of moderate PA. At baseline, 1272 participants reported undertaking moderate PA with a regular frequency. Of these participants, 1020 (58.8% of the study population) continued this regular frequency after 12 months of follow‐up and in 252 (14.5%) had decreased their exercise to low frequency. Of the 463 participants who undertook moderate PA with a low frequency at baseline, 302 (17.4%) continued this low frequency after 12 months of follow‐up, and 161 (9.3%) had increased their exercise to a regular frequency.
Figure 1.
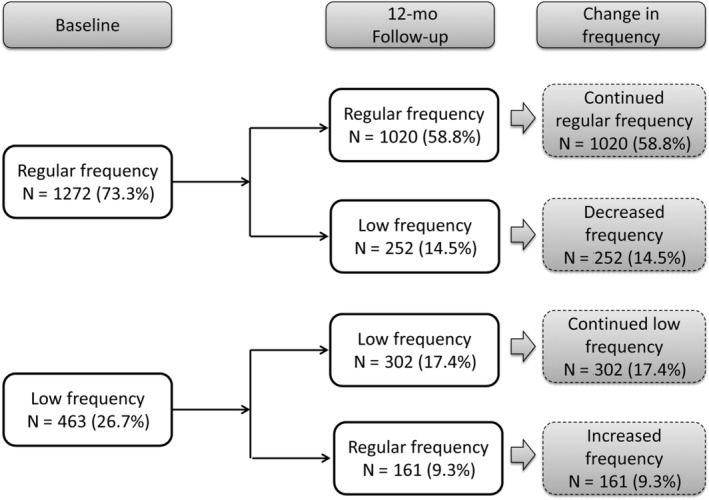
Frequency of moderate physical activity of participants.
2.2. Frailty at Baseline and Follow‐Up
Table 2 and Figure 2 show the overall, physical, psychological, and social frailty scores at baseline and follow‐up by (1) frequency of moderate PA at baseline and (2) 12‐month change in frequency of moderate PA. Compared with participants who undertook moderate PA with a regular frequency at baseline, participants who undertook moderate PA with a low frequency were significantly more overall (mean = 6.80; SD = 3.27; Figure 2A), physically (mean = 3.99; SD = 2.13; Figure 2C), psychologically (mean = 1.61; SD = 1.20; Figure 2E), and socially (mean = 1.21; SD = 0.89; Figure 2G) frail at follow‐up.
Table 2.
Overall, Physical, Psychological, and Social Frailty at Baseline and Follow‐Up
| Groups of PA | Baseline | Follow‐Up | P Valuea |
|---|---|---|---|
| Overall Frailty Score (Score Range = 0‐15) | |||
| Baseline frequency of PA | |||
| Regular frequency (n = 1272) | 4.45 ± 2.91b | 4.56 ± 3.16b | .122 |
| Low frequency (n = 463) | 6.96 ± 3.07b | 6.80 ± 3.27b | .165 |
| 12‐mo Change in PA | |||
| Continued regular frequency (n = 1020) | 4.18 ± 2.78c | 4.10 ± 2.95c | .337 |
| Decreased frequency (n = 252) | 5.57 ± 3.18c | 6.39 ± 3.34c | <.001 |
| Continued low frequency (n = 302) | 7.42 ± 2.93c | 7.67 ± 2.95c | .069 |
| Increased frequency (n = 161) | 6.10 ± 3.16c | 5.18 ± 3.22c | <.001 |
| Physical Frailty Score (Score Range = 0‐8) | |||
| Baseline frequency of PA | |||
| Regular frequency (n = 1272) | 2.51 ± 1.96b | 2.55 ± 2.16b | .409 |
| Low frequency (n = 463) | 4.20 ± 2.05b | 3.99 ± 2.13b | .009 |
| 12‐mo Change in PA | |||
| Continued regular frequency (n = 1020) | 2.33 ± 1.88c | 2.27 ± 2.04c | .313 |
| Decreased frequency (n = 252) | 3.26 ± 2.12c | 3.68 ± 2.67c | <.001 |
| Continued low frequency (n = 302) | 4.55 ± 1.91c | 4.54 ± 1.90c | .930 |
| Increased frequency (n = 161) | 3.56 ± 2.16c | 2.94 ± 2.17c | <.001 |
| Psychological Frailty Score (Score Range = 0‐4) | |||
| Baseline frequency of PA | |||
| Regular frequency (n = 1272) | 1.00 ± 1.00b | 1.06 ± 1.08b | .052 |
| Low frequency (n = 463) | 1.52 ± 1.10b | 1.61 ± 1.20b | .092 |
| 12‐mo Change in PA | |||
| Continued regular frequency (n = 1020) | 0.94 ± 0.97c | 0.92 ± 1.01c | .550 |
| Decreased frequency (n = 252) | 1.25 ± 1.06c | 1.60 ± 1.20c | <.001 |
| Continued low frequency (n = 302) | 1.64 ± 1.13c | 1.85 ± 1.21c | <.001 |
| Increased frequency (n = 161) | 1.30 ± 1.02c | 1.15 ± 1.05c | .103 |
|
Social Frailty Score (Score Range = 0‐3) |
|||
| Baseline frequency of PA | |||
| Regular frequency (n = 1272) | 0.94 ± 0.88b | 0.95 ± 0.88b | .601 |
| Low frequency (n = 463) | 1.24 ± 0.90b | 1.21 ± 0.89b | .485 |
| 12‐mo Change in PA | |||
| Continued regular frequency (n = 1020) | 0.91 ± 0.86c | 0.90 ± 0.87c | .898 |
| Decreased frequency (n = 252) | 1.05 ± 0.96c | 1.12 ± 0.91c | .197 |
| Continued low frequency (n = 302) | 1.23 ± 0.91c | 1.28 ± 0.88c | .266 |
| Increased frequency (n = 161) | 1.25 ± 0.89c | 1.08 ± 0.90c | .011 |
Note. Data presented as mean ± SD; a higher score represents a higher level of frailty.
Abbreviation: PA, physical activity.
Significant P values in bold; paired t test was used.
P < .001; P values are based on independent t test.
P < .001; P values are based on one‐way analysis of variance.
Figure 2.
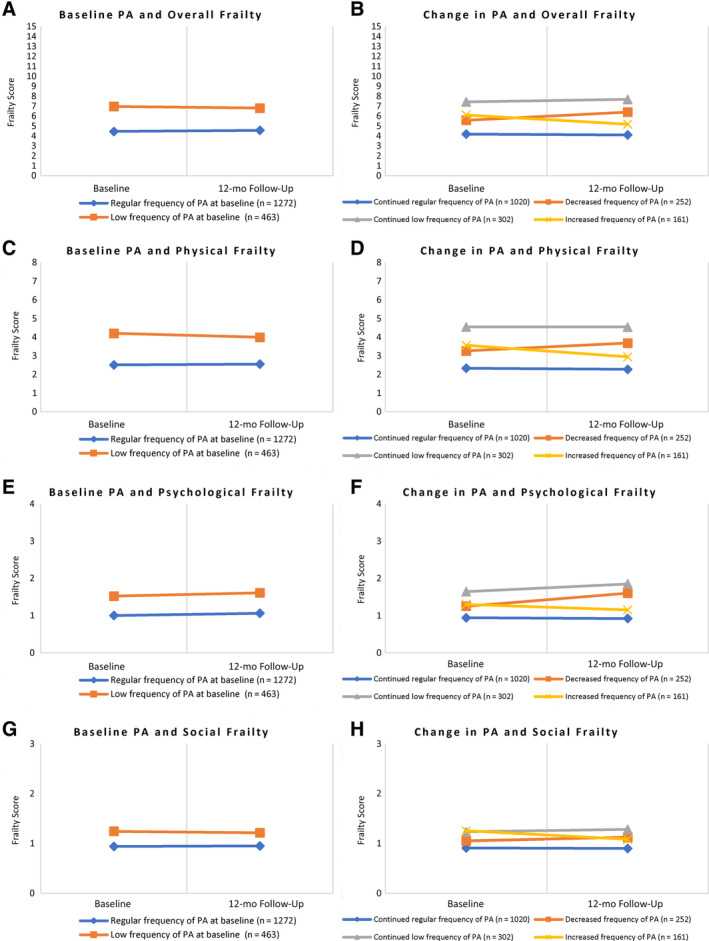
Frailty score at baseline and follow‐up of participants from the groups of frequency of moderate physical activity (PA). (A) Baseline PA and overall frailty, (B) Change in PA and overall frailty, (C) Baseline PA and physical frailty, (D) Change in PA and physical frailty, (E) Baseline PA and psychological frailty, (F) Change in PA and psychological frailty, (G) Baseline PA and social frailty, (H) Change in PA and social frailty.
Regarding change in frequency of moderate PA, those participants who undertook moderate PA with a continued regular frequency were least frail, and participants with a continued low frequency were most frail at follow‐up (Figure 2B,D,F,H). Participants who undertook moderate PA with a decreased frequency were more frail at follow‐up than at baseline (Figure 2B,D,F). However, the difference in social frailty was not significant. Conversely, participants who undertook moderate PA with an increased frequency were less frail at follow‐up than at baseline (Figure 2B,D,H), although the difference in psychological frailty was not significant.
2.3. Association Between Frequency of Moderate PA and Frailty
Supplementary Table S2 shows the multivariate linear regression models exploring the association between frequency of moderate PA at baseline and overall, physical, psychological, or social frailty at follow‐up. Compared with participants who undertook moderate PA with a regular frequency at baseline, participants with low exercise frequency were significantly more frail (B = 0.28; 95% confidence interval [CI] = 0.01‐0.55; P < .05) at follow‐up after controlling for overall frailty at baseline and the covariates.
2.4. Association Between 12‐Month Change in Frequency of Moderate PA and Frailty
Table 3 shows the multivariate linear regression models exploring the association between 12‐month change in frequency of moderate PA and overall, physical, psychological, or social frailty at follow‐up. Change in frequency of moderate PA was significantly associated with overall, physical, psychological, and social frailty at follow‐up.
Table 3.
Multivariate Linear Regression Models (12‐Month Change in Physical Activity and Follow‐Up Scores of Frailty)
| 12‐mo Follow‐Up Frailty Score | 12‐mo Change in Moderate Physical Activity | ||||
|---|---|---|---|---|---|
| Continued Regular Frequency | Decreased Frequency | Continued Low Frequency | Increased Frequency | Adjusted R2, % | |
| Overall frailty | |||||
| Crude modela | Reference | 1.34 (1.02 to 1.66) *** | 1.31 (1.00 to 1.63) *** | −0.25 (−0.64 to 0.13) | 56.6 |
| Adjusted modelb | Reference | 1.31 (0.99 to 1.63) *** | 1.16 (0.84 to 1.49) *** | −0.25 (−0.63 to 0.14) | 57.8 |
| Physical frailty | |||||
| Crude modelc | Reference | 0.83 (0.60 to 1.06) *** | 0.86 (0.63 to 1.09) *** | −0.15 (−0.42 to 0.12) | 51.6 |
| Adjusted modeld | Reference | 0.80 (0.58 to 1.03) *** | 0.73 (0.51 to 0.96) *** | −0.15 (−0.42 to 0.11) | 53.0 |
| Psychological frailty | |||||
| Crude modele | Reference | 0.45 (0.32 to 0.58) *** | 0.47 (0.35 to 0.60) *** | 0.02 (−0.13 to 0.18) | 39.2 |
| Adjusted modelf | Reference | 0.43 (0.30 to 0.56)*** | 0.42 (0.29 to 0.55)*** | 0.01 (−0.15 to 0.16) | 39.7 |
| Social frailty | |||||
| Crude modelg | Reference | 0.13 (0.03 to 0.23)* | 0.14 (0.05 to 0.24)** | −0.03 (−0.15 to 0.09) | 41.8 |
| Adjusted modelh | Reference | 0.14 (0.04 to 0.23)** | 0.13 (0.04 to 0.23)** | 0.02 (−0.09 to 0.13) | 48.5 |
Note: Data presented as B (95% confidence interval), unless otherwise indicated. More details can be found in Supplementary Table S3.
Adjusted for baseline overall frailty and country.
Adjusted for baseline overall frailty, country, age, sex, education level, living situation, smoking, alcohol risk, multimorbidity, and intervention condition.
Adjusted for baseline physical frailty and country.
Adjusted for baseline physical frailty, country, age, sex, education level, living situation, smoking, alcohol risk, multimorbidity, and intervention condition.
Adjusted for baseline psychological frailty and country.
Adjusted for baseline psychological frailty, country, age, sex, education level, living situation, smoking, alcohol risk, multimorbidity, and intervention condition.
Adjusted for baseline social frailty and country.
Adjusted for baseline social frailty, country, age, sex, education level, living situation, smoking, alcohol risk, multimorbidity, and intervention condition.
* P < .05, ** P < .01, *** P < .001, with significant effect estimates in bold.
Compared with participants who undertook moderate PA with a continued regular frequency, participants with a decreased frequency (B = 1.31; 95% CI = 0.99‐1.63; P < .001) and participants with a continued low frequency (B = 1.16; 95% CI = 0.84‐1.49; P < .001) were significantly more overall frail at follow‐up after the covariates and overall frailty at baseline were controlled. Regarding physical frailty, participants with a decreased frequency (B = 0.80; 95% CI = 0.58‐1.03; P < .001) and participants with a continued low frequency (B = 0.73; 95% CI = 0.51‐0.96; P < .001) were significantly more physically frail at follow‐up. Regarding psychological frailty, participants with a decreased frequency (B = 0.43; 95% CI = 0.30‐0.56; P < .001) and participants with a continued low frequency (B = 0.42; 95% CI = 0.29‐0.55; P < .001) were significantly more psychologically frail at follow‐up. Regarding social frailty, participants with decreased exercise frequency (B = 0.14; 95% CI = 0.04‐0.23; P < .01) and participants with a continued low frequency (B = 0.13; 95% CI = 0.04‐0.23; P < .01) were significantly more socially frail at follow‐up. There was no significant difference in overall, physical, psychological, and social frailty at follow‐up between participants who undertook moderate PA with an increased frequency and participants with a continued regular frequency. More details can be found in Supplementary Table S3.
3. DISCUSSION
Our study aimed to examine the longitudinal association between the frequency of moderate PA and frailty among community‐dwelling older adults older than 70 years. We found that participants who undertook moderate PA with a regular frequency at baseline were less overall frail at follow‐up than participants with a low frequency. Second, we assessed the association between a 12‐month change in frequency of moderate PA and frailty. Older adults who undertook moderate PA with an increased frequency were less overall frail at follow‐up than they were at baseline. Older adults who undertook moderate PA with a continued regular frequency were least overall frail at baseline and at 12‐month follow‐up. Interestingly, after controlling all the covariates and baseline overall frailty, the follow‐up overall frailty levels of participants who undertook moderate PA with an increased frequency were similar to those with a continued regular frequency. These findings indicate that maintaining a regular frequency of PA as well as increasing frequency of PA are associated with maintaining or improving overall frailty (multidimensional).
Previous observational studies3, 10, 15 also found that PA is associated with a delay in progression of frailty among older adults, but these studies focused on physical frailty. More studies on multidimensional frailty are still needed. Additionally, some randomized controlled trials (RCTs) on the effect of PA intervention on physical frailty showed conflicting results. An RCT among 424 older adults found that regular PA could reduce the presence and severity of physical frailty, especially in individuals at higher risk of disability.9 In contrast, a secondary analysis of an RCT among 1635 older adults reported that a structured, moderate‐intensity PA program was not associated with a reduction in the overall risk of physical frailty.12 These differing results may be due to the different characteristics of PA intervention methods (eg, the intensity, frequency, and duration of PA) as well as differing frailty criteria among studies.7, 12 RCTs that study the effect of various kinds of PA intervention (eg, moderate or vigorous activity or a combination of both with different frequency and duration) on frailty are needed to determine the optimal level of PA among older adults.
In addition to overall and physical frailty, our findings report on the longitudinal association between PA and psychological and social frailty. After controlling all the covariates and baseline frailty, we found that older adults who undertook moderate PA with a continued regular frequency were least psychologically and socially frail at baseline and follow‐up, and that the follow‐up psychological and social frailty levels of participants who undertook moderate PA with an increased frequency were similar to those with a continued regular frequency. Regarding psychological frailty, a controlled study of older adults aged 61 to 89 years in Canada found that PA training could improve cognitive functioning and psychological well‐being.27 A systematic review of 11 RCTs to assess the effect of PA on depression found that PA may reduce depression or depressive symptoms in adults older than 60 years.28 A qualitative study among older adults aged 80 to 91 years in Sweden reported that PA could help older adults to have the energy to be active and to improve their mood, because PA was able help them realize that their body was still working well enough to perform the activity.29 Regarding social frailty, an RCT in Spain found that a multicomponent exercise program was not only able to improve the physical aspects of frailty, but also to increase interaction with other people, which could reduce the level of social frailty.30, 31 However, studies to investigate the association between PA and psychological and social frailty among older adults are still scarce, and more studies are needed.27, 32
Finally, regarding psychological frailty, we found an interaction between 12‐month change in moderate PA and country; in the Netherlands, the results were different from the results from the other four countries (Supplementary Table S4). More studies are needed to clarify this finding.
3.1. Strengths and Limitations
One strength of our study is that we added longitudinal evidence on the association between PA and frailty among citizens aged 70 years or older from a diverse community‐based sample from five European countries. In addition, we used a validated instrument to consider frailty broadly from the physical, psychological, and social perspectives, and to add to the current literature on the association between change in PA and the three domains of frailty. Social frailty, in particular, is a rarely explored domain; and there is a dearth of studies on this subject.33, 34
However, our study also has some limitations. First, PA was measured by one self‐reported question, which is fairly crude and open to interpretation. This question does not differentiate between type of activity and does not take the duration of activity into account. Studies using a more comprehensive measurement of PA are needed to confirm our findings. However, some previous studies35, 36, 37 indicate that using a single question to measure PA is acceptable under certain conditions (eg, when the sample size is large, when more complex methods would add to respondent burden, and when collecting data from a broad range of settings). Gill et al also suggest that the reliability and validity of a single question to briefly classify PA levels is acceptable.38 Therefore, taking into account the large sample size, the response burden, and the aim of the study, we believe that using a single question to measure the frequency of PA is acceptable. Second, we transferred the ordinal variable of PA into a dichotomous one, which might cause information loss. However, we conducted additional analyses on the association between PA and frailty with the ordinal variable of PA (Supplementary Figure S1), and the results were similar to our primary findings. Third, we found statistically significant differences in frailty scores between baseline and follow‐up. This finding was based on statistical methods rather than on clinical examinations. Hence, we cannot draw conclusions on the clinical meaning of the TFI scores. Future studies should explore whether this statistical difference corresponds to a clinically meaningful change in frailty level. Fourth, participants in both the intervention and control groups were included in the analyses. The intervention may have led to improvement in health, which could result in the overestimation of the effect of PA on frailty. However, we controlled for the intervention condition by adding it to the regression models as a covariate. We also repeated the analyses for the control group only and found similar results. Additionally, we considered the results of those persons who had received specific UHCE interventions may have had an effect on the changes in the frequency of PA. Therefore, we conducted a sensitivity analysis to control for specific UHCE interventions that may promote PA. For this purpose, the intervention condition in the multivariable regression model was categorized into three categories instead of two: (1) control group, (2) intervention promoting PA group (participants who enrolled in the falls and/or frailty pathway), and (3) intervention not promoting PA group (participants who did not enroll in the falls and/or frailty pathway). The results of this sensitivity analysis were similar to our primary findings. Fifth, our observational study cannot confirm causality between PA and frailty. A decrease in frequency of PA might be the cause of the progression of frailty, or simply the epiphenomenon of a declining health status. In addition, a decrease in PA might also have been caused by external factors leading to frailty, such as an accident, stroke, or fall during the year. Adjusting for multimorbidity at baseline only partly reflects these variations of PA during 12‐month follow‐up. Sixth, overadjustment bias may exist because we adjusted for many covariates and some of these (eg, multimorbidity) may act partially as a confounder and partially as a mediator. Last, there may be overlap between PA and two items of the TFI (walking and balance), which could cause overestimation of the association. However, when we explored the association between PA and overall frailty, after deleting these two items, the results were similar. Hence, we do not expect that this limitation has changed our findings.
4. CONCLUSIONS
In conclusion, we found that both maintaining a regular frequency of PA and increasing to a regular frequency of PA are associated with maintaining or improving the level of frailty among European community‐dwelling older adults older than 70 years, not only in the physical domain, but also in the psychological and social domains of frailty. Our findings support the development of new public health strategies to encourage adults older than 70 years to maintain a regular frequency of PA to prevent and delay not only physical but also psychological and social frailty. More RCTs studying the effect of the frequency and intensity levels of PA are needed to determine the optimum level of PA required to prevent the progression of physical, psychological, and social frailty among older adults.
Supporting information
Supplementary Table S1: P Values for Interactions Between Baseline Frequency of Moderate PA or 12‐Month Change in Frequency of Moderate PA and Age, Sex, County, Education Level, Living Situation, and Intervention on the Frailty Scores
Supplementary Table S2: Multivariate Linear Regression Models (Frequency of Moderate Physical Activity at Baseline and Follow‐Up Scores of Frailty)
Supplementary Table S3: Multivariate Linear Regression Models (12‐Month Change in Physical Activity and Follow‐Up Scores of Frailty)
Supplementary Table S4: Multiple Linear Regression Models (12‐Month Change in Moderate Physical Activity and Psychological Frailty) Stratified by Country
Supplementary Figure S1: Frequency of moderate physical activity of participants (three categories of frequency of physical activity: “more than once a week”= [a] more than once a week; “one a week or less”= [b] once a week and [c] one to three times a month; “never” = [d] hardly ever or never).
ACKNOWLEDGMENT
We thank all participants and all organizations and professionals involved in the Urban Health Centres Europe project. We thank Ms Daphne Visser‐Lees from Meditrans Medical Editing and Translating for language editing of the manuscript.
Financial Disclosure
Urban Health Centres Europe is funded by the European Union, Consumers, Health, Agriculture and Food Executive Agency (CHAFEA), third health program, number 20131201. X.Z. is supported by a China Scholarship Council (CSC) PhD Fellowship for her PhD study in Erasmus MC, Rotterdam, The Netherlands. The scholarship file number is 201706010358, CSC (http://www.csc.edu.cn/).
Conflict of Interest
The authors have no conflicts.
Author Contributions
X.Z., A.G., and H.R.: study concept and design. C.F., L.B., T.A., J.G., A.V., G.W., G.C., T.R., R.S., A.V., and H.R.: acquisition of subjects and data. X.Z., C.F., S.S.T., A.G., and H.R.: analysis and interpretation of data. X.Z. and S.S.T.: preparation of manuscript. All authors: critical revision and final approval of manuscript.
Sponsor's Role
European Union and China Scholarship Council had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethics Approval and Consent to Participate
Ethics committee procedures were followed in all cities and institutions involved, and approval was obtained. The names of the review board and the approval references are: Manchester, United Kingdom: The National Research Ethics Service (NRES) Committee West Midlands–Coventry & Warwickshire; March 6, 2015; 15/WM/0080; NRES Committee South Central–Berkshire B; 29‐20‐2014; 14/SC/1349; Pallini, Greece: The Ethics and Scientific Board–Latriko Palaiou Falirou Hospital; March 4, 2015; 20150304‐01; Rijeka, Croatia: The Ethical Committee–Faculty of Medicine University of Rijeka; April 7, 2014; 2170‐24‐01‐14‐02; Rotterdam, The Netherlands: Medische Ethische Toetsings Commissie–Erasmus MC Rotterdam; January 8, 2015; MEC‐2014‐661; Valencia, Spain: Comisión de Investigación–Consorcio Hospital General Universitario de Valencia. January 29, 2015; CICHGUV‐January 29, 2015. Written consent is obtained from all participants.
The preliminary abstract of this study was presented at the International Society of Behavioral Nutrition and Physical Activity 2019 Annual Meeting held in Prague, Czech Republic, in June 2019 and was awarded the conference's best student abstract on aging.
REFERENCES
- 1. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community‐dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60:1487‐1492. [DOI] [PubMed] [Google Scholar]
- 2. The 2018 Ageing Report: Economic and Budgetary Projections for the EU Member States (2016‐2070). Brussels, Belgium: European Commission:2018. [Google Scholar]
- 3. McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016;17:567‐580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752‐762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu C, Smit E, Xue QL, Odden MC. Prevalence and correlates of frailty among community‐dwelling Chinese older adults: the China health and retirement longitudinal study. J Gerontol A Biol Sci Med Sci. 2017;73:102‐108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hamer M, Lavoie KL, Bacon SL. Taking up physical activity in later life and healthy ageing: the English longitudinal study of ageing. Br J Sports Med. 2014;48:239‐243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rogers NT, Marshall A, Roberts CH, Demakakos P, Steptoe A, Scholes S. Physical activity and trajectories of frailty among older adults: evidence from the English longitudinal study of ageing. PLoS One. 2017;12:e0170878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kehler DS, Theou O. The impact of physical activity and sedentary behaviors on frailty levels. Mech Ageing Dev. 2019;180:29‐41. [DOI] [PubMed] [Google Scholar]
- 9. Cesari M, Vellas B, Hsu FC, et al. A physical activity intervention to treat the frailty syndrome in older persons‐results from the LIFE‐P study. J Gerontol A Biol Sci Med Sci. 2015;70:216‐222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Peterson MJ, Giuliani C, Morey MC, et al. Physical activity as a preventative factor for frailty: the health, aging, and body composition study. J Gerontol A Biol Sci Med Sci. 2009;64:61‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Higueras‐Fresnillo S, Cabanas‐Sanchez V, Lopez‐Garcia E, et al. Physical activity and association between frailty and all‐cause and cardiovascular mortality in older adults: population‐based prospective cohort study. J Am Geriatr Soc. 2018;66:2097‐2103. [DOI] [PubMed] [Google Scholar]
- 12. Trombetti A, Hars M, Hsu FC, et al. Effect of physical activity on frailty: secondary analysis of a randomized controlled trial. Ann Intern Med. 2018;168:309‐316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yuki A, Otsuka R, Tange C, et al. Daily physical activity predicts frailty development among community‐dwelling older Japanese adults. J Am Med Dir Assoc. 2019;20:1032‐1036. [DOI] [PubMed] [Google Scholar]
- 14. de Vries NM, van Ravensberg CD, Hobbelen JS, Olde Rikkert MG, Staal JB, Nijhuis‐van der Sanden MW. Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community‐dwelling older adults with impaired mobility, physical disability and/or multi‐morbidity: a meta‐analysis. Ageing Res Rev. 2012;11:136‐149. [DOI] [PubMed] [Google Scholar]
- 15. Blodgett J, Theou O, Kirkland S, Andreou P, Rockwood K. The association between sedentary behaviour, moderate‐vigorous physical activity and frailty in NHANES cohorts. Maturitas. 2015;80:187‐191. [DOI] [PubMed] [Google Scholar]
- 16. Gobbens RJ, Luijkx KG, van Assen MA. Explaining quality of life of older people in the Netherlands using a multidimensional assessment of frailty. Qual Life Res. 2013;22:2051‐2061. [DOI] [PubMed] [Google Scholar]
- 17. Franse CB, Voorham AJJ, van Staveren R, et al. Evaluation design of Urban Health Centres Europe (UHCE): preventive integrated health and social care for community‐dwelling older persons in five European cities. BMC Geriatr. 2017;17:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Franse CB, van Grieken A, Alhambra‐Borras T, et al. The effectiveness of a coordinated preventive care approach for healthy ageing (UHCE) among older persons in five European cities: a pre‐post controlled trial. Int J Nurs Stud. 2018;88:153‐162. [DOI] [PubMed] [Google Scholar]
- 19. Romero‐Ortuno R, Walsh CD, Lawlor BA, Kenny RA. A frailty instrument for primary care: findings from the survey of health, ageing and retirement in Europe (SHARE). BMC Geriatr. 2010;10:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Romero‐Ortuno R. The frailty instrument of the survey of health, ageing and retirement in Europe (SHARE‐FI) predicts mortality beyond age, comorbidities, disability, self‐rated health, education and depression. European Geriatr Med. 2011;2:323‐326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gobbens RJ, Schols JM, van Assen MA. Exploring the efficiency of the Tilburg frailty indicator: a review. Clin Interv Aging. 2017;12:1739‐1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gobbens RJ, van Assen MA, Luijkx KG, Wijnen‐Sponselee MT, Schols JM. The Tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc. 2010;11:344‐355. [DOI] [PubMed] [Google Scholar]
- 23. Schneider SL. The international standard classification of education 2011. In: Elisabeth Birkelund G, ed. Class and Stratification Analysis (Comparative Social Research, Vol 30). Bingley: Emerald Group Publishing Limited; 2013:365‐379. [Google Scholar]
- 24. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT‐C): an effective brief screening test for problem drinking: ambulatory care quality improvement project (ACQUIP): alcohol use disorders identification test. Arch Intern Med. 1998;158:1789‐1795. [DOI] [PubMed] [Google Scholar]
- 25. Quah JHM, Wang P, Ng RRG, Luo N, Tan NC. Health‐related quality of life of older Asian patients with multimorbidity in primary care in a developed nation. Geriatr Gerontol Int. 2017;17:1429‐1437. [DOI] [PubMed] [Google Scholar]
- 26. Börsch‐Supan A. Ageing and Retirement in Europe (SHARE) Wave 5: Release Version: 5.0.0. [SHARE‐ERIC Data Set]. Survey of Health, 2015.
- 27. Langlois F, Vu TT, Chasse K, Dupuis G, Kergoat MJ, Bherer L. Benefits of physical exercise training on cognition and quality of life in frail older adults. J Gerontol B Psychol Sci Soc Sci. 2013;68:400‐404. [DOI] [PubMed] [Google Scholar]
- 28. Blake H, Mo P, Malik S, Thomas S. How effective are physical activity interventions for alleviating depressive symptoms in older people? a systematic review. Clin Rehabil. 2009;23:873‐887. [DOI] [PubMed] [Google Scholar]
- 29. Welmer AK, Morck A, Dahlin‐Ivanoff S. Physical activity in people age 80 years and older as a means of counteracting disability, balanced in relation to frailty. J Aging Phys Act. 2012;20:317‐331. [DOI] [PubMed] [Google Scholar]
- 30. Tarazona‐Santabalbina FJ, Gomez‐Cabrera MC, Perez‐Ros P, et al. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community‐dwelling frail elderly: a randomized clinical trial. J Am Med Dir Assoc. 2016;17:426‐433. [DOI] [PubMed] [Google Scholar]
- 31. Makizako H, Tsutsumimoto K, Shimada H, Arai H. Social frailty among community‐dwelling older adults: recommended assessments and implications. Ann Geriatr Med Res. 2018;22:3‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Landi F, Abbatecola AM, Provinciali M, et al. Moving against frailty: does physical activity matter? Biogerontology. 2010;11:537‐545. [DOI] [PubMed] [Google Scholar]
- 33. Dedeyne L, Deschodt M, Verschueren S, Tournoy J, Gielen E. Effects of multi‐domain interventions in (pre)frail elderly on frailty, functional, and cognitive status: a systematic review. Clin Interv Aging. 2017;12:873‐896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bunt S, Steverink N, Olthof J, van der Schans CP, Hobbelen JSM. Social frailty in older adults: a scoping review. Eur J Ageing. 2017;14:323‐334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rose SB, Elley CR, Lawton BA, Dowell AC. A single question reliably identifies physically inactive women in primary care. N Z Med J. 2008;121:U2897. [PubMed] [Google Scholar]
- 36. Weiss TW, Slater CH, Green LW, Kennedy VC, Albright DL, Wun CC. The validity of single‐item, self‐assessment questions as measures of adult physical activity. J Clin Epidemiol. 1990;43:1123‐1129. [DOI] [PubMed] [Google Scholar]
- 37. Milton K, Clemes S, Bull F. Can a single question provide an accurate measure of physical activity? Br J Sports Med. 2013;47:44‐48. [DOI] [PubMed] [Google Scholar]
- 38. Gill DP, Jones GR, Zou G, Speechley M. Using a single question to assess physical activity in older adults: a reliability and validity study. BMC Med Res Methodol. 2012;12:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: P Values for Interactions Between Baseline Frequency of Moderate PA or 12‐Month Change in Frequency of Moderate PA and Age, Sex, County, Education Level, Living Situation, and Intervention on the Frailty Scores
Supplementary Table S2: Multivariate Linear Regression Models (Frequency of Moderate Physical Activity at Baseline and Follow‐Up Scores of Frailty)
Supplementary Table S3: Multivariate Linear Regression Models (12‐Month Change in Physical Activity and Follow‐Up Scores of Frailty)
Supplementary Table S4: Multiple Linear Regression Models (12‐Month Change in Moderate Physical Activity and Psychological Frailty) Stratified by Country
Supplementary Figure S1: Frequency of moderate physical activity of participants (three categories of frequency of physical activity: “more than once a week”= [a] more than once a week; “one a week or less”= [b] once a week and [c] one to three times a month; “never” = [d] hardly ever or never).


