Abstract
Burnout is one of the main chronic health problems with negative consequences on caregivers but also on the quality of care. This is a multidimensional occupational syndrome, characterized by three main criteria: emotional exhaustion (EE), depersonalization (DP), and low personal accomplishment (PA). Burnout is particularly identified in professionals working in caregiving and human services, especially the ones who are interpersonally stressed and emotionally vulnerable. Intensive care professionals seem to face a critical risk of burnout. This study aiming to evaluate the occurrence and the risk factors of burnout among Italian anesthesiologists and intensive care physicians. All members included in the mailing list of the Italian Society of Anesthesia, Analgesia, and Intensive Care were invited to participate in an online survey. An anonymous questionnaire was distributed via a specific website. Burnout was measured using the Maslach Burnout Inventory (MBI) questionnaire. All responses were evaluated through univariate and multivariable logistic regression. A total of 859 physicians out of 3,654 (23.5%) participated in this online survey. According to the MBI criteria for a high degree of burnout, 10.2% (88) of the respondents reported high EE, high DP, and low PA together; 79.9% (686) exhibited a moderate degree of burnout; and 9.9% (85) reported a low degree of burnout, with normal values in all three of the explored psychological dimensions. This study reported mostly a moderate level of burnout among Italian anesthesiologist and intensive care physicians since we found 10.2% incidence for high degree of burnout according to the MBI criteria.
Keywords: burnout syndrome, anesthesia, ICU, anesthesiologist, job stress
What do we already know about this topic?
Burnout is a common problem in intensive care medicine and anesthesiology.
How does your research contribute to the field?
This survey discovered a 10% rate for high degree of burnout among Italian anesthesiologists and intensive care physicians.
What are your research’s implications toward theory, practice, or policy?
Different interventions to reduce burnout are needed.
Background
Burnout is a work-related constellation of symptoms and signs that usually occurs in individuals with no history of psychological or psychiatric disorders.1,2 This term was first used in the 1970s by the psychoanalyst H.J. Freudenberger to describe a mental illness resulting in an impairing exhaustion, often observed in health care workers and caused by prolonged job-related stress.3 Burnout was later defined as a multidimensional occupational syndrome (burnout syndrome) characterized by three main criteria: emotional exhaustion (EE; feeling weak, tired, and worn out), depersonalization (DP; an increased feeling of distance toward the job and the patients), and reduced personal accomplishment (PA; a sense of ineffectiveness).
Burnout is particularly identified in professionals working in caregiving and human services, especially the ones who are interpersonally stressed and emotionally vulnerable.3-7 People affected by burnout may show early signs of stress arousal (eg, irritability, forgetfulness, and sleep disorders), may already attempt to compensate for stress (eg, social withdrawal, increased cynicism, and persistent tiredness), and suffer from exhaustion (eg, depression or anxiety symptoms, chronic pain syndromes, or functional disorders of the cardiovascular or gastrointestinal system).8-15
Burnout was observed in individuals in various medical subspecialties, including dentists, psychiatrists, and pediatricians; however, intensive care physicians and anesthesiologists were a special risk group.16-18 The prevalence of burnout syndrome among anesthesiologist and intensive care unit (ICU) physicians is relatively high.17 Intensive care physicians and anesthesiologists experienced significant amounts of stress in their work settings, having to directly deal with extreme working periods, high-risk patients, and an increasingly complex working environment.17,18
Since a previous Italian national survey to assess the burnout was conducted in cardiac anesthesiology subspecialty,19 we aimed to assess the occurrence of this syndrome among Italian anesthesiologists and intensive care physicians regardless of their subspecialties.
To address this issue, we conducted a national study of burnout using an online survey mailed to all members of the Italian Society of Anesthesia, Analgesia, and Intensive Care (SIAARTI).
Methods
The present survey was approved by the SIAARTI and sent twice by email from the secretariat to all members included in the mailing list of the society. At the time of the survey, the mailing list of the Italian society included 3,654 physicians. The survey was a free online survey that did not require ethical approval.
The questionnaire to assess burnout was composed of a first part comprising nine questions designed to capture basic sociodemographic and characteristic work-related information, and a second part including the Italian version of the Maslach Burnout Inventory (MBI),4 with legal permission from Mind Garden, Inc. (Menlo Park, CA, USA).4
We used the MBI because it is the most commonly used tool to diagnose burnout.1 The MBI contains subscales to separately assess different aspects of experienced burnout:
EE: assessing feelings resulting from the depletion of emotional resources.
DP: assessing personal and caring attitudes.
PA: assessing feelings of competence and successful achievement when working with people.
These three dimensions of psychological investigation are split into 22 items: 9 for EE, 5 for DP, and 8 for PA. All given answers are related to a 7-point Likert scale ranging from 0 (never) to 6 (every day) to express how frequently a person experiences the dimensions of burnout. These subscales are considered “high,” “average,” or “low” according to predetermined cut-off scores based on normative data. Scores are considered “high” if they are in the upper third of the normative distribution, “average” if they are in the middle one, “low” if they are in the lower third. Burnout is associated with high EE and DP values, as well as with a low PA score. Scores used to indicate the prevalence of burnout measured with the MBI have a wide range of variability, as reported by van Mol et al20; therefore, we used the normative Italian sample of 748 Italians working in the healthcare professions.21 The Italian validation of the MBI questionnaire established the following ranges: high EE ≥ 24, DP ≥ 9, PA ≤ 37, moderate: EE 16-23, DP 5-8, and PA 38-45.20,21 Cronbach’s coefficient was utilized to test the internal consistency reliability for each MBI subscale. The raw (standardized) values were .924 for EE, .690 for DP, and .788 for PA.
Data Entry and Statistical Analysis
The survey was conducted using a web-based survey instrument (MagNews© 2017, powered by Diennea S.r.l.). Microsoft Excel® and SPSS (IBM; Armonk, New York) were used for data entry and statistical analysis. Continuous data were reported as a mean or standard deviation, whereas categorical data were reported as a number or percentage.
A descriptive analysis was undertaken to determine the characteristics of the study population. Then, the associations between the burnout dimensions and the sociodemographic and work-related characteristic information were assessed through bivariate correlations; one-way analysis of variance was employed, separately, on each of the three dimensions of burnout: the dependent variable was the specific dimension of burnout. The regression coefficients with 95% confidence interval (CI) were presented. Post hoc tests (Tukey’s Honest Significant Difference [HSD] test) were conducted, if necessary.
Multivariate logistic regression analysis (backward stepwise) was performed to calculate the odds ratios (ORs), determining which variables were associated with high EE, high DP, and low PA. The variables with a P-value less than .1 in univariate analysis were included in multivariate analysis. The measures of association were expressed as ORs and corresponding 95% CIs. Univariate analysis was reported in the online Supplemental Material. A confirmatory factor analysis was performed using the lavaan e knitr packages of R software (version 3.6.0).
Results
A total of 859 physicians out of 3,654 (23.5%) participated in this online survey. Among the responders, 499 (58.1%) were above 40 years of age, 397 were males (46.2%), 522 (60.8%) were married, and 473 (55.1%) had at least one child. The overall population characteristics are synthesized in Table 1.
Table 1.
Baseline Demographic and Personal Characteristics of Respondents.
| Characteristics | Total (%) |
|---|---|
| Gender | |
| Male | 397 (46.2) |
| Female | 462 (53.8) |
| Age | |
| Under 40 | 360 (41.9) |
| Over 40 | 499 (58.1) |
| Marital status | |
| Married | 522 (60.8) |
| Single | 337 (39.2) |
| Offspring | |
| Yes | 473 (55.1) |
| No | 386 (44.9) |
| Type of institutions | |
| Public hospital | 764 (88.9) |
| Private hospital | 95 (11.1) |
| University hospital | 348 (40.5) |
| Main specialty area | |
| Intensive care | 472 (54.9) |
| Anesthesiology | 375 (43.7) |
| Pain therapy | 10 (1.2) |
| Hyperbaric therapy | 2 (0.2) |
| Pediatric specialty | |
| Yes | 137 (15.9) |
| No | 722 (84.1) |
| Geographic area | |
| North | 422 (49.1) |
| Center | 195 (22.7) |
| South | 157 (18.3) |
| Islands | 85 (9.9) |
Figure 1 shows the degree of burnout between the three domains of burnout separately. Low PA was reported by 31% of the respondents, and high scores for EE and DP were reported by 39.3% and 25.5% of the respondents. According to the MBI criteria for a high degree of burnout, 10.2% (88) of the respondents reported high EE, high DP, and low PA together; 79.9% (686) exhibited a moderate degree of burnout; and 9.9% (85) reported a low degree of burnout, with normal values in all three of the explored psychological dimensions.
Figure 1.
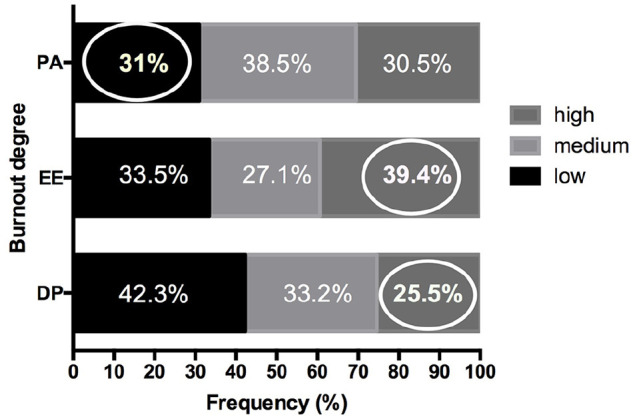
Frequency of burnout degree between EE, DP, and PA.
Note. The circles included high EE, High DP, and low PA that are the components of high degree of burnout. EE = emotional exhaustion; DP = depersonalization; PA = personal accomplishment.
Respondents above 40 years and working in ICU were significantly EE (OR: 1.47, CI: 1.07-2.03, P = .02; OR: 1.35, CI: 1.02-1.79, P = .04, respectively). Male respondents were significantly associated with high DP (OR: 1.61, CI: 1.20-2.15, P = .002). Physicians working in an ICU were significantly associated with a low PA score (OR: 1.68, CI: 1.18-2.38, P = .003).
The regression model (Supplementary Materials) showed that working in an intensive care setting (OR: 1.87, 95% CI: 1.15-3.03) and being an under-40 anesthetists (OR: 1.66, 95% CI: 1.00-2.76) cause one to be significantly more exposed to a diagnosis of burnout (Table 2).
Table 2.
Multivariate Logistic Regression Analysis Among Burnout Dimensions and Sociodemographic and Work-Related Characteristic Information.
| Characteristics | High emotional exhaustion OR (CI) | P | High depersonalization OR (CI) | P | Low personal accomplishment: OR (CI) | P |
|---|---|---|---|---|---|---|
| Male | 0.92 (0.7-1.22) | .56 | 1.6 (1.20-2.15) | .002 | 0.63 (0.43-0.93) | .02 |
| Over 40 | 1.47 (1.07-2.03) | .02 | 0.41 (0.30-0.57) | <.001 | 0.94 (0.67-1.32) | .12 |
| Married | 1.25 (0.87-1.79) | .24 | 1.31 (0.89-1.91) | .17 | 0.5 (0.32-0.77) | .002 |
| Offspring | 0.63 (0.43-0.91) | .01 | 0.73 (0.49-1.07) | .10 | 1.35 (0.86-2.10) | .19 |
| Public hospital | 1.04 (0.67-1.63) | .85 | 1.30 (0.81-2.08) | .28 | 1.90 (0.99-3.64) | .052 |
| University hospital | 1.26 (0.93-1.69) | .14 | 1.28 (0.94-1.74) | .12 | 0.68 (0.47-0.98) | .04 |
| Intensive care | 1.35 (1.02-1.79) | .04 | 0.87 (0.65-1.16) | .34 | 1.68 (1.18-2.38) | .003 |
| Pain therapy | 1.48 (0.41-5.35) | .55 | 0.61 (0.15-2.43) | .48 | 0.83 (0.13-5.32) | .85 |
| Hyperbaric therapy | 1.68 (0.10-27-58) | .72 | 0.41 (0.41-17.21) | .64 | 1.80 (0.04-77.8) | .76 |
Note. OR = odds ratio; CI = confidence interval. The bold face values refer to statistically significant results.
Discussion
In this survey, evaluating the occurrence of burnout among Italian anesthesiologists and intensive care physicians, we found that (1) according to the MBI criteria, 10.2% of the respondents reported a high degree of burnout, 79.9% showed a moderate degree of burnout, and 9.9% had no symptoms of burnout; and (2) according to our multivariate logistic regression, more than 40 years and working in ICU were significantly associated with EE, male respondents were significantly associated with high DP while working in ICU was significantly associated with low PA score. Three previous surveys investigated the incidence of burnout in the Italian contest of anesthesia;19,22,23 however, they had several differences when compared with this study. The survey by Capuzzo et al evaluated the incidence of burnout among anesthesiologists and anesthesia nurses working in four hospitals located in three North-Central Italian cities.22 This article reported an incidence of burnout for anesthesiologists and nurses of 22%.22 Orena et al assessed the incidence of burnout among 18 practitioners working at a neurological institute in the North of Italy.23 In this study, the high EE and DP scores were found in 22.2% of respondents while low PA in 66.7% of participants.23 Sanfilippo et al conducted an Italian nationwide survey involving anesthesiologists working primarily for cardiac surgery.19 A total of 382 cardiac anesthesiologists completed the survey and 54% of them scored a high risk of burnout.19 Our survey aimed to include each anesthesiologist working in the Italian setting without any geographical or subspecialty limitations. Although this, we had a participation of 23.5%.
Burnout deserves significant attention since the Critical Care Societies Collaborative, in partnership with the four major U.S. scientific societies in this field, published a document to focus attention on this topic.1 The MBI has been documented to be widely accepted in different countries.1 The current validation of the MBI has been established in health care workers by cross-sectional and longitudinal design with confirmatory factor analyses.24 In this survey, 90% of respondents scored a high or moderate risk of burnout. U.S. critical care and emergency medicine physicians reported the highest percentage of burnout (55%), whereas anesthesiologists scored slightly lower, with half of them at a significant risk.18,25 Our results reported a 10% incidence of burnout compared with the current literature. This result may have probably been influenced by the low response rate and the lengthy questionnaire we used. A recent report performed in the United Kingdom stated that burnout and depression deeply affected the physicians’ way of life.26 However, the most used strategies adopted by the physicians to reduce burnout were exercising, talking with family, sleeping, playing or listening to music, and eating junk food or drinking alcohol; nobody mentioned spending time on a personal computer or laptop.27
According to our multivariate logistic regression, working in ICU and being above 40 years were significantly associated with high EE, male respondents were significantly associated with high DP and working in ICU were significantly associated with low PA score. If different ages are risk factors for burnout is still matter of debate,28,29 actually no threshold age for burnout is established. In line with the current literature, male physicians are exposed to high risk of DP while working for years in ICU is a risk factor for burnout in the PA domain. The ICU is a complex environment because of end-of-life decisions, mortality, acutely ill patients with a poor prognosis, and working during the night and weekend.18 Improving the quality of work with adequate recovery after night shifts, psychological support for end-of-life decisions, and better communication within the ICU staff and with the family members of dying patients are modifiable factors that may reduce the risk of burnout.1
Limitations
This study suffers from some several limitations. First, the lower response rate might have affected the result of the multivariate regression. Second, this study is a survey and not a cross-sectional or observational study. Third, the questionnaire we included in this survey was sent to the mailing list of the SIAARTI members and not to all of the Italian anesthesiologists and ICU physicians. Fourth, we did not investigate the consequences of burnout. Fifth, in Italy, there are no differences between anesthesiologists and ICU physicians because they are the same professional figures. We were able to identify physicians working mainly as anesthesiologists, and physicians working mainly in the ICU. Sixth, we used the scoring system derived from the Italian validation of the MBI of 1993.
Conclusions
This study reported mostly a moderate level of burnout among Italian anesthesiologist and intensive care physicians since we found 10.2% incidence for high degree of burnout according to the MBI criteria.
Supplemental Material
Supplemental material, Supplemental_material for Burnout Among Anesthesiologists and Intensive Care Physicians: Results From an Italian National Survey by Maria Vargas, Gianmario Spinelli, Pasquale Buonanno, Carmine Iacovazzo, Giuseppe Servillo and Stefania De Simone in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
The authors wish to thank the President and the Secretary of the Italian Society of Anesthesia, Analgesia, and Intensive Care (SIAARTI) for their assistance with this article.
Footnotes
Authors’ Contributions: M.V., G.Sp., P.B., C.I., G.Se., and S.D.S. participated in writing the protocol, collecting data, analyzing results, and writing the manuscript. M.V., G.Sp., P.B., C.I., G.Se., and S.D.S. read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Maria Vargas  https://orcid.org/0000-0001-7652-970X
https://orcid.org/0000-0001-7652-970X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement-burnout syndrome in critical care health-care professionals: a call for action. Chest. 2016;150(1):17-26. [DOI] [PubMed] [Google Scholar]
- 2. Felton JS. Burnout as a clinical entity—its importance in health care workers. Occup Med (Lond). 1998;48(4):237-250. [DOI] [PubMed] [Google Scholar]
- 3. Freudenberger HJ. Staff burn-out. J Soc Issues. 1974;30(1):159-165. [Google Scholar]
- 4. Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99-113. [Google Scholar]
- 5. De Simone S. Conceptualizing the wellbeing in the workplace. Int J Bus Soc Sci. 2014;5(12):118-122. [Google Scholar]
- 6. De Simone S. Expectancy value theory: motivating healthcare workers. Am Int J Contemp Res. 2015. a;5(2):19-23. [Google Scholar]
- 7. De Simone S. Wellbeing at work: a survey on perception of health care workers. Rivista Internazionale di Scienze Sociali. 2015. b;4:395-412. [Google Scholar]
- 8. Maslach C, Jackson SE, Leiter M. The Maslach Burnout Inventory Manual. In: Zalaquett CP, Wood RJ, eds. A Book of Resources. The Scarecrow Press; 1997:191-218. [Google Scholar]
- 9. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995-1000. [DOI] [PubMed] [Google Scholar]
- 10. Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction. J Gen Intern Med. 2000;15(2):122-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jones JW, Barge BN, Steffy BD, Fay LM, Kunz LK, Wuebker LJ. Stress and medical malpractice: organizational risk assessment and intervention. J Appl Psychol. 1988;73(4):727-735. [DOI] [PubMed] [Google Scholar]
- 12. Guntupalli KK, Wachtel S, Mallampalli A, Surani S. Burnout in the intensive care unit professionals. Indian J Crit Care Med. 2014;18(3):139-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alexandrova-Karamanova A, Todorova I, Montgomery A, et al. Burnout and health behaviors in health professionals from seven European countries. Int Arch Occup Environ Health. 2016;89(7):1059-1075. [DOI] [PubMed] [Google Scholar]
- 14. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714-1721. [DOI] [PubMed] [Google Scholar]
- 15. Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54-62. [DOI] [PubMed] [Google Scholar]
- 16. Ciammella P, De Bari B, Fiorentino A, et al. The “BUONGIORNO” project: burnout syndrome among young Italian radiation oncologists. Cancer Invest. 2013;31(8):522-528. [DOI] [PubMed] [Google Scholar]
- 17. Sanfilippo F, Noto A, Foresta G, et al. Incidence and risk factors associated with burnout in anesthesiology: a systematic review. Biomed Res Int. 2017;2017:8648925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Milenovic M, Matejic B, Vasic V, Frost E, Petrovic N, Simic D. High rate of burnout among anaesthesiologists in Belgrade teaching hospitals: results of a cross-sectional survey. Eur J Anaesthesiol. 2016;33(3):187-194. [DOI] [PubMed] [Google Scholar]
- 19. Sanfilippo F, Noto A, Palumbo GJ, et al. Burnout in cardiac anesthesiologists: results from a national survey in Italy. J Cardiothorac Vasc Anesth. 2018;32(6):2459-2466. [DOI] [PubMed] [Google Scholar]
- 20. van Mol MM, Kompanje EJ, Benoit DD, Bakker J, Nijkamp MD. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PLoS One. 2015;10(8):e0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sirigatti S, Stefanile C. MBI—Maslach Burnout Inventory. Adattamento e taratura per l’Italia. 1993. [Google Scholar]
- 22. Capuzzo M, Gilli G, Paparella L, et al. Factors predictive of patient satisfaction with anesthesia. Anesth Analg. 2007;105(2):435-442. [DOI] [PubMed] [Google Scholar]
- 23. Orena EF, Caldiroli D, Cortellazzi P. Does the Maslach Burnout Inventory correlate with cognitive performance in anesthesia practitioners. Saudi J Anaesth. 2013;7(3):277-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Poghosyan L, Aiken LH, Sloane DM. Factor structure of the Maslach Burnout Inventory: an analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int J Nurs Stud. 2009;46(7):894-902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Medscape Lifestyle Report 2016: Bias and Burnout. http://www.medscape.com/slideshow/lifestyle-2016-overview-6007335#2. Accessed April 6, 2020.
- 26. Medscape UK Doctors’ Burnout & Lifestyle Survey 2018. https://www.medscape.com/slideshow/uk-burnout-report-6011058#1. Accessed April 6, 2020.
- 27. Medscape National Physician Burnout & Depression Report 2018. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235#1. Accessed April 6, 2020.
- 28. Chuang CH, Tseng PC, Lin CY, Lin KH, Chen YY. Burnout in the intensive care unit professionals. A systematic review. Medicine. 2016;95(50):e5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Merlani P, Verdon M, Businger A, et al. Burnout in ICU caregivers. Am J Respir Crit Care Med. 2011;184:1140-1146. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental_material for Burnout Among Anesthesiologists and Intensive Care Physicians: Results From an Italian National Survey by Maria Vargas, Gianmario Spinelli, Pasquale Buonanno, Carmine Iacovazzo, Giuseppe Servillo and Stefania De Simone in INQUIRY: The Journal of Health Care Organization, Provision, and Financing


