Abstract
Objectives
Evidence is needed for designing interventions to address health literacy–related issues among adults with prediabetes to reduce their risk of developing type 2 diabetes. This study assessed health literacy and behaviors among US adults with prediabetes and the mediating role of health literacy on health behaviors.
Methods
We used data from the 2016 Behavioral Risk Factor Surveillance System (BRFSS) (N = 54 344 adults). The BRFSS health literacy module included 3 questions on levels of difficulty in obtaining information, understanding health care providers, and comprehending written information. We defined low health literacy as a response of “somewhat difficult” or “very difficult” to at least 1 of these 3 questions. Respondents self-reported their prediabetes status. We included 3 health behavior indicators available in the BRFSS survey—current smoking, physical inactivity, and inadequate sleep, all measured as binary outcomes (yes/no). We used a path analysis to examine pathways among prediabetes, health literacy, and health behaviors.
Results
About 1 in 5 (19.0%) adults with prediabetes had low health literacy. The rates of physical inactivity (31.0% vs 24.6%, P < .001) and inadequate sleep (38.8% vs 33.5%, P < .001) among adults with prediabetes were significantly higher than among adults without prediabetes. The path analysis showed a significant direct effect of prediabetes and health literacy on health behaviors. The indirect effect of prediabetes through health literacy on health behaviors was also significant.
Conclusion
BRFSS data from 2016 showed that rates of low health literacy and unhealthy behaviors were higher among adults with prediabetes than among adults without prediabetes. Interventions are needed to assist adults with prediabetes in comprehending, communicating about, and managing health issues to reduce the risk of type 2 diabetes.
Keywords: prediabetes, health behaviors, health literacy, path model
More than 88 million US adults aged ≥18 (1 in 3) have prediabetes,1 but 80% of them do not know they have it.2 Adults with prediabetes are at high risk of type 2 diabetes (the most common type of diabetes), heart disease, and stroke.2 To prevent prediabetes from progressing to type 2 diabetes, maintaining a healthy weight and adopting healthy behaviors are critical. One determinant of self-care behavior in type 2 diabetes is health literacy.3 Adequate health literacy may increase individuals’ capacity to take responsibility for their health and the health of their family members.4
Health literacy is defined as the degree to which a person has the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.5 Thus, health literacy includes not only the components of general literacy—such as oral literacy, print literacy, and numeracy—but also the ability to obtain and use information for health-related decision making. Health literacy depends not only on the skills of a person but also on the communication skills of others, especially health care workers, and on the values of health care systems, such as whether intervention programs are in place to help those with low levels of health literacy.6
Health literacy is a national priority because limited health literacy costs the US health care system $106 to $238 billion each year.7 Healthy People 2020 goals called for substantial improvements in levels of health literacy to advance the health of the US population.8 The US Department of Health and Human Services released the National Action Plan to Improve Health Literacy in 2010 with a goal to provide all persons in the United States with access to accurate and actionable health information, deliver person-centered health information and services, and support lifelong learning and skills to improve health status.9
A growing body of literature shows that a low level of health literacy is associated with an increase in the number of hospitalizations and emergency department visits, poor self-care and adherence to medications, poor comprehension of medical terminology, poor communication with health care providers, unhealthy behaviors, and poor health outcomes.3,10,11 One study in China showed that the prevalence of low health literacy was higher among adults with prediabetes than among adults without prediabetes, especially among adults with low education levels.12 However, little research has been conducted to understand the role of health literacy among adults with prediabetes in the United States. Thus, the potential link between health literacy and health behaviors among adults with prediabetes is unclear. Health care providers and researchers have little evidence with which to design interventions (eg, improving communication for better understanding of medical instructions) to address health literacy–related issues among adults with prediabetes to reduce their risk of developing type 2 diabetes. The aim of this study was to describe health literacy and health behaviors among adults with prediabetes and assess the mediating role of health literacy on health behaviors.
Methods
Data Source
We used data for this analysis from the 2016 Behavioral Risk Factor Surveillance System (BRFSS).13 The BRFSS is a random-digit–dialed telephone survey of adults aged ≥18 residing in the United States. The BRFSS collects self-reported information on various health behaviors and preventive health practices. The survey instrument includes core questions (administered in every state and US territory) and optional modules (administered in some states and territories). The variables of interest in this analysis were from 2 optional modules: (1) the health literacy module, in which 14 states and territories participated, and (2) the prediabetes module, in which 27 states and territories participated. Among them, 8 states (Alabama, Alaska, Illinois, Iowa, Louisiana, Mississippi, Nebraska, and Virginia), as well as the District of Columbia and Puerto Rico, participated in both modules. The study sample included 54 344 adults who participated in both modules. Because this study was a secondary analysis of a publicly available data set, it did not require institutional review board review.
Measurement
Prediabetes status (independent variable)
Prediabetes status was defined by the response to the question, “Have you ever been told by a doctor or other health professional that you have prediabetes or borderline diabetes?” We classified respondents as having prediabetes if they answered yes; otherwise, we classified respondents as not having prediabetes. Respondents with diabetes were not asked the prediabetes question and were excluded from this analysis.
Health literacy (mediator variable)
The Centers for Disease Control and Prevention developed a 3-question health literacy module,14 which was offered as an optional module in the 2016 BRFSS. The 3 questions were (1) “How difficult is it for you to get advice or information about health or medical topics if you need it?” (indicated as “difficulty in obtaining information” hereinafter); (2) “How difficult is it for you to understand information that doctors, nurses, and other health professionals tell you?” (indicated as “difficulty in understanding doctors” hereinafter); and (3) “In general, how difficult is it for you to understand written health information?” (indicated as “difficulty in understanding written information” hereinafter).
We first coded the 3 health literacy variables as binary outcomes by combining the responses “somewhat difficult” and “very difficult” into 1 category—having difficulty (yes)—and by combining “very easy” and “somewhat easy” into 1 category—not having difficulty (no). We treated other responses—“don’t know/not sure” and “refused”—as missing. In addition, we also treated the responses “I don’t look for health information” in Question 1 and “I don’t pay attention to written health information” in Question 3 as missing. Our preliminary analysis showed a significant correlation among these 3 measures of health literacy (all P < .001). Given the study objective, we decided to combine the 3 variables into 1 variable: a respondent was classified as having low health literacy if a yes answer was recorded to any of the 3 questions; the respondent was classified as not having low health literacy if a no answer was recorded to all 3 questions.
Health behaviors (outcome/dependent variables)
We included 3 health behavior–related variables available in the 2016 BRFSS core questionnaire as binary outcome variables—current smoking, physical inactivity, and inadequate sleep. We selected these variables because smoking,15 physical inactivity,16 and inadequate sleep17,18 are all risk factors for type 2 diabetes. We categorized smoking status as current smokers (ie, everyday smoker or some-day smoker) vs not current smokers (ie, former smoker or never smoker). We coded physical inactivity according to the following yes/no question: “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” We coded inadequate sleep according to the question, “On average, how many hours of sleep do you get in a 24-hour period?” We classified respondents who reported <7 hours as having inadequate sleep.17 Otherwise, we classified respondents as not having inadequate sleep. We did not include variables on dietary intake because the 2016 BRFSS did not include questions on these topics.
Covariates
Consistent with previous research,19-21 we included the following variables as covariates: age, sex (male/female), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), formal education (<high school graduate, high school graduate, ≥some college), and annual household income (<$15 000, $15 000-$24 999, $25 000-$34 999, $35 000-$49 999, ≥$50 000). We also included marital status (married or living with a partner vs other [divorced, widowed, separated, or never married]) as an indicator of social support and having health insurance (yes/no) as an indicator of health care access.
Statistical Analysis
We used Pearson χ2 and t tests where appropriate to test for associations between sample characteristics and prediabetes status and between low health literacy and health behaviors. Then, using path analysis,22 we assessed pathways among prediabetes, health literacy, and the 3 health behaviors. A single path analysis model included prediabetes as the independent variable, low health literacy as the mediator variable, the 3 health behaviors as the dependent variables, and covariates. We calculated the total effect of prediabetes on the 3 health behaviors as the sum of direct and indirect effects. We converted the coefficients to adjusted odds ratios (aORs) for easy interpretation.
The BRFSS survey uses dual sampling frames and disproportionate stratified sampling to achieve a population-based probability sample. Thus, we used survey procedures in analysis to account for geographic and telephone number stratification and analysis weights. We conducted data analyses by using Stata version 14.23 Significance was set at P < .05.
Results
Adults with prediabetes were significantly older than adults without prediabetes (mean age, 53.3 vs 45.3; P < .001) (Table 1). Adults with prediabetes were also significantly more likely than adults without prediabetes to have health insurance (P = .04) and to be married or living with a partner (P = .02). Non-Hispanic black adults and Hispanic adults were significantly more likely than non-Hispanic white adults to have prediabetes (P < .001); adults with an annual household income <$35 000 were also significantly more likely to have prediabetes than adults with higher incomes (P < .001). Overall, adults with prediabetes were significantly more likely than adults without prediabetes to have low health literacy (19.0% vs 14.9%; P < .001). The proportions of adults who had difficulty in obtaining information (7.9% vs 5.4%; P < .001), understanding health care professionals (10.1% vs 7.0%; P < .001), and understanding written information (9.3% vs. 7.3%; P < .001) were significantly higher among adults with prediabetes than among adults without prediabetes.
Table 1.
Descriptive statistics of the study sample (54 344 adults aged ≥18), by prediabetes status, 2016 Behavioral Risk Factor Surveillance System (BFRSS) surveya
| Variables | Has Prediabetes (n = 5701) | Does Not Have Prediabetes (n = 48 643) | P Valueb |
|---|---|---|---|
| Age, weighted mean, y | 53.3 (52.6-54.1) | 45.3 (45.1-45.6) | <.001 |
| Female | 53.6 (51.2-55.9) | 51.8 (51.0-52.6) | .16 |
| Race/ethnicity | <.001 | ||
| Non-Hispanic white | 57.0 (54.7-59.3) | 61.6 (60.8-62.3) | |
| Non-Hispanic black | 19.9 (18.1-21.9) | 16.5 (15.9-17.1) | |
| Hispanic | 18.2 (16.4-20.2) | 16.6 (16.0-17.2) | |
| Other | 4.9 (3.8-6.2) | 5.4 (5.0-5.9) | |
| Has health insurance | 90.5 (88.8-91.9) | 88.6 (88.0-89.1) | .04 |
| Education level | .11 | ||
| <High school graduation | 13.9 (12.2-15.8) | 13.3 (12.7-14.0) | |
| High school graduation | 30.9 (28.8-33.2) | 28.8 (28.0-29.5) | |
| ≥Some college | 55.2 (52.8-57.5) | 57.9 (57.1-58.7) | |
| Annual household income, $ | <.001 | ||
| <15 000 | 13.7 (12.2-15.4) | 12.4 (11.9-13.0) | |
| 15 000-24 999 | 20.3 (18.2-22.5) | 17.8 (17.1-18.4) | |
| 25 000-34 999 | 11.3 (9.7-13.1) | 9.6 (9.1-10.1) | |
| 35 000-49 999 | 13.4 (11.8-15.0) | 13.3 (12.7-13.9) | |
| ≥50 000 | 41.4 (38.9-43.9) | 47.0 (46.1-47.8) | |
| Married/living with a partner | 52.4 (50.1-54.7) | 49.3 (48.5-50.1) | .02 |
| Low health literacyc | 19.0 (17.0-21.2) | 14.9 (14.3-15.6) | <.001 |
| Difficulty in obtaining information | 7.9 (6.5-9.5) | 5.4 (5.0-5.8) | <.001 |
| Difficulty in understanding health care professionals | 10.1 (8.6-11.8) | 7.0 (6.6-7.5) | <.001 |
| Difficulty in understanding written information | 9.3 (7.9-11.1) | 7.3 (6.9-7.8) | <.001 |
aVariables of interest were from 2 optional modules in the 2016 BRFSS survey: (1) the health literacy module, in which 14 states and territories participated, and (2) the prediabetes module, in which 27 states and territories participated. All values are weighted percentage (95% CI) unless otherwise indicated. Data source: Centers for Disease Control and Prevention.13
bDetermined by χ2 or t test; P < .05 was considered significant.
cThe BRFSS health literacy module included 3 questions on levels of difficulty in obtaining information, understanding health care providers, and comprehending written information. Low health literacy was defined as a response of “somewhat difficult” or “very difficult” to at least 1 of these 3 questions.
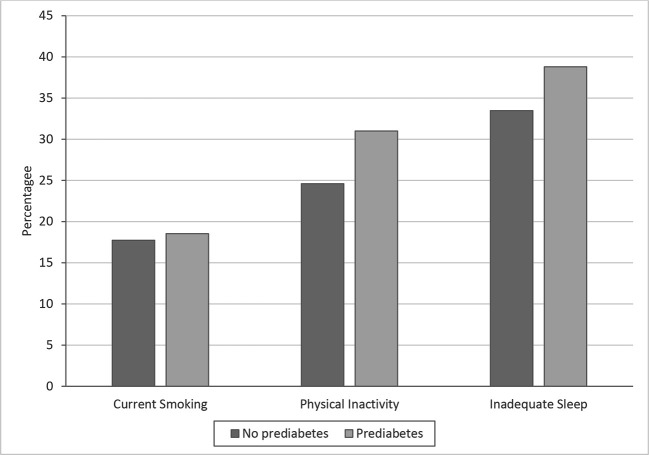
The proportion of adults who were physically inactive was significantly higher among adults with prediabetes than among adults without prediabetes (31.0% vs 24.6%; P < .001) (Figure 1). The proportion of adults who reported inadequate sleep was also significantly higher among adults with prediabetes (38.8% vs 33.5%; P < .001). We found no difference in smoking status (18.5% vs 17.7%; P = .44) by prediabetes status.
Figure 1.
Health behaviors reported by respondents (54 344 adults aged ≥18), by prediabetes status, 2016 Behavioral Risk Factor Surveillance System survey.13 Current smokers were defined as everyday smokers or some-day smokers; not current smokers were defined as former smokers or never smokers. Physical inactivity was coded according to the following yes/no question: “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Inadequate sleep was coded according to the question, “On average, how many hours of sleep do you get in a 24-hour period?” Those who reported <7 hours were classified as having inadequate sleep.17
Path Analysis
The path analysis generated information on direct effects, indirect effects, total effects, and coefficients for covariates. The direct effect of prediabetes on low health literacy was significant (ß = 0.034; P = .003 for all) in all 3 models (Figure 2A-C). The direct effect of low health literacy on current smoking was significant (ß = 0.059; P < .001), and the direct effect of prediabetes on current smoking was also significant (ß = 0.028; P < .001) (Figure 2A).
Figure 2.
Results of path analysis in a study (N = 54 344 adults aged ≥18) on health literacy and health behaviors among adults with prediabetes, 2016 Behavioral Risk Factor Surveillance System survey.13 (A) Relationship among prediabetes, low health literacy, and current smoking. (B) Relationship among prediabetes, low health literacy, and physical inactivity. (C) Relationship among prediabetes, low health literacy, and inadequate sleep. Low health literacy was defined as answering “somewhat difficult” or “very difficult” to any of the 3 questions on obtaining information, understanding physicians, and understanding written information. Current smokers were defined as everyday smokers or some-day smokers; not current smokers were defined as former smokers or never smokers. Physical inactivity was coded according to the following yes/no question: “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Inadequate sleep was coded according to the question, “On average, how many hours of sleep do you get in a 24-hour period?” Those who reported <7 hours were classified as having inadequate sleep.17 Arrows indicate a direct effect.
The direct effect of prediabetes on physical inactivity was significant (ß = 0.031; P = .02), as was the direct effect of low health literacy on physical inactivity (ß = 0.064; P < .001) (Figure 2B). Lastly, the direct effects of both prediabetes (ß = 0.070; P < .001) and low health literacy (ß = 0.075; P < .001) on inadequate sleep were significant (Figure 2C).
The indirect effect of prediabetes (ie, through low health literacy) on all 3 health behavior variables was also significant: current smoking (ß = 0.002; P < .001), physical inactivity (ß = 0.002; P = .01), and inadequate sleep (ß = 0.003; P < .001).
In the analysis of the total effects of prediabetes on the 3 health behaviors from the path model, we found that adults with prediabetes, compared with adults without prediabetes, were more likely to be current smokers (aOR = 1.03; 95% CI, 1.01-1.05), to be physically inactive (aOR = 1.03; 95% CI, 1.01-1.06), and to get inadequate sleep (aOR = 1.08; 95% CI, 1.05-1.11) (Table 2).
Table 2.
Results from the total effects path model in a study (N = 54 344 adults aged ≥18) on health literacy and health behaviors among adults with prediabetes, 2016 Behavioral Risk Factor Surveillance System surveya
| Variables | Model I (Dependent Variable Is Current Smokingb) | Model II (Dependent Variable Is Physical Inactivityc) | Model III (Dependent Variable Is Inadequate Sleepd) |
|---|---|---|---|
| Diabetes status | |||
| Has prediabetes | 1.03 (1.01-1.05) [.01] | 1.03 (1.01-1.06) [.01] | 1.08 (1.05-1.11) [<.001] |
| Does not have prediabetes | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Health literacy levele | |||
| Does not have low health literacy | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Has low health literacy | 1.06 (1.04-1.09) [<.001] | 1.07 (1.04-1.09) [<.001] | 1.08 (1.05-1.11) [<.001] |
| Age | 1.00 (0.998-0.999) [<.001] | 1.00 (1.002-1.003) [<.001] | 1.00 (0.998-0.999) [<.001] |
| Sex | |||
| Male | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Female | 0.96 (0.95-0.97) [<.001] | 1.04 (1.03-1.06) [<.001] | 0.99 (0.98-1.01) [.46] |
| Race/ethnicity | |||
| Non-Hispanic white | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Non-Hispanic black | 0.94 (0.92-0.96) [<.001] | 1.02 (1.00-1.04) [.06] | 1.10 (1.07-1.13) [<.001] |
| Hispanic | 0.83 (0.81-0.85) [<.001] | 1.03 (1.00-1.05) [.04] | 1.00 (0.97-1.03) [.89] |
| Other | 0.96 (0.93-1.00) [.03] | 1.02 (0.99-1.06) [.25] | 0.99 (0.95-1.04) [.65] |
| Health insurance status | |||
| Does not have health insurance | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Has health insurance | 0.92 (0.90-0.95) [<.001] | 0.97 (0.94-1.00) [.08] | 0.99 (0.96-1.02) [.45] |
| Education | |||
| <High school graduation | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| High school graduation | 0.95 (0.92-0.98) [<.001] | 0.94 (0.90-0.97) [<.001] | 1.01 (0.97-1.04) [.77] |
| ≥Some college | 0.89 (0.86-0.92) [<.001] | 0.86 (0.84-0.90) [<.001] | 1.01 (0.97-1.05) [.64] |
| Annual household income, $ | |||
| <15 000 | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| 15 000-24 999 | 0.98 (0.96-1.01) [.26] | 0.96 (0.93-0.99) [.005] | 0.99 (0.96-1.03) [.75] |
| 25 000-34 999 | 0.96 (0.93-0.99) [.01] | 0.92 (0.89-0.96) [<.001] | 0.98 (0.95-1.02) [.43] |
| 35 000-49 999 | 0.95 (0.92-0.98) [<.001] | 0.88 (0.85-0.91) [<.001] | 0.97 (0.93-1.00) [.06] |
| ≥50 000 | 0.89 (0.86-0.91) [<.001] | 0.82 (0.79-0.84) [<.001] | 0.96 (0.93-0.99) [.02] |
| Marital status | |||
| Divorced, widowed, separated, or never married | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Married/living with a partner | 0.96 (0.95-0.98) [<.001] | 1.01 (1.00-1.03) [.08] | 0.98 (0.96-1.00) [.02] |
| R2 | 16.3 | 17.6 | 12.3 |
| Standardized root mean squared residual | <.001 | <.001 | <.001 |
aAll values are adjusted odds ratio (95% CI) [P value] unless otherwise indicated. Variables of interest were from 2 optional modules in the 2016 Behavioral Risk Factor Surveillance System (BRFSS) survey: (1) the health literacy module, in which 14 states and territories participated, and (2) the prediabetes module, in which 27 states and territories participated. Data source: Centers for Disease Control and Prevention.13
bCurrent smokers were defined as everyday smokers or some-day smokers; not current smokers were defined as former smoker or never smokers.
cPhysical inactivity was coded according to the following yes/no question: “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?”
dInadequate sleep was coded according to the question, “On average, how many hours of sleep do you get in a 24-hour period?” Those who reported <7 hours were classified as having inadequate sleep.17
eThe BRFSS health literacy module included 3 questions on levels of difficulty in obtaining information, understanding health care providers, and comprehending written information. Low health literacy was defined as a response of “somewhat difficult” or “very difficult” to at least 1 of these 3 questions.
The significant results for the covariates were similar to significant results for the 3 health behavior outcomes (Table 2). Women were less likely to be current smokers (aOR = 0.96; 95% CI, 0.95-0.97) and more likely to be physically inactive (aOR = 1.04; 95% CI, 1.03-1.06) than men; adults with health insurance (aOR = 0.92; 95% CI, 0.90-0.95) were less likely than adults without health insurance to be current smokers; non-Hispanic black adults (aOR = 0.94; 95% CI, 0.92-0.96) and Hispanic adults (aOR = 0.83; 95% CI, 0.81-0.85) were less likely than non-Hispanic white adults to be current smokers; and Hispanic adults were more likely than non-Hispanic white adults to be physically inactive (aOR = 1.03; 95% CI, 1.01-1.05). As education levels increased, adults were less likely to be current smokers and less likely to be physically inactive (P < .001), and adults with an annual household income ≥$25 000 were less likely than adults with an annual household income <$15 000 to be current smokers and less likely to be physically inactive (P < .001).
In summary, the path analysis results confirmed the mediating role of low health literacy: (1) prediabetes status among adults was significantly associated with the 3 health behaviors (total effect); (2) prediabetes status was significantly associated with low health literacy levels among adults; (3) controlling for prediabetes, low health literacy was significantly associated with the 3 health behaviors among adults; and (4) the relationship between prediabetes and the 3 health behaviors among adults was reduced (ie, the direct effect) when we controlled for low health literacy (ie, the indirect effect), with a significant indirect effect.
Discussion
To our knowledge, our study is the first to use population-based national survey data to assess health literacy and health behaviors among adults with prediabetes and to examine the pathways among prediabetes, low health literacy, and health behaviors. Our results showed that, compared with adults without prediabetes, adults with prediabetes had lower health literacy and were more likely to be current smokers, to get inadequate sleep, and to be physically inactive.
We showed that almost 1 in 5 adults with prediabetes had low health literacy. The rate of low health literacy among adults with prediabetes (19.0%) was 4.1 percentage points higher than among adults without prediabetes (14.9%). These findings indicate that many adults with prediabetes may not be able to read and comprehend essential health-related materials (eg, prescription bottles, appointment slips, self-care protocols) and may lack the capacity to take responsibility for their health and their family’s health.
Health literacy is not just the result of individual capacities but also the health literacy–related demands and complexities of the health care system.6,24 Potential communication barriers between patients and health care providers created by low health literacy may lead to poor self-care and adherence to medications.25,26 To assist persons with low health literacy, programs and interventions such as visual aids and counseling could be implemented to increase comprehension of prescription labels and ensure medication safety and adherence.
The BRFSS survey first included the health literacy module as an optional module in 2016; these data will provide a baseline for tracking the prevalence of low health literacy. Because of differences in defining and measuring health literacy,27,28 it is difficult to directly compare our results with the results of other studies. In addition, few population-based studies on health literacy exist, and it is difficult to compare results from populations that differ by geography, health status, and demographic characteristics. To our knowledge, the only other existing national study of health literacy is the 2003 National Assessment of Adult Literacy,29 which found that more than one-third of US adults had basic (22%) or below-basic (14%) health literacy and would have difficulty managing common health-related tasks.
One might expect that adults with prediabetes would engage in healthy lifestyles because of their risk of developing type 2 diabetes. However, our study results showed that a larger proportion of adults with prediabetes than adults without prediabetes were physically inactive (31.0% vs. 24.6%) and got inadequate sleep (38.8% vs 33.5%). To prevent prediabetes from developing into type 2 diabetes, adults with prediabetes should be encouraged to exercise, quit smoking, and get adequate sleep.15-18 The National Diabetes Prevention Program has been proven to help persons make the lifestyle changes needed to prevent or delay type 2 diabetes. A loss of a modest amount of body weight (ie, 5%-7%) and regular physical activity (ie, ≥150 minutes per week of brisk walking or similar activity) greatly reduce the risk of type 2 diabetes.30
The path analysis results showed important direct and indirect effects of having prediabetes on low health literacy and then unhealthy behaviors. Low health literacy is consistently associated with increases in hospitalizations and use of emergency care, decreases in use of preventive care, and a poor ability to interpret labels and health messages.3,10 As such, programs that target improvements in health literacy could help to promote positive health behaviors among adults with prediabetes. Medical instructions and patient education material should be written at a sixth-grade or lower reading level, preferably including pictures and illustrations. Health care providers should be mindful that most patients are unwilling to admit that they do not understand medical instructions.31
Limitations
This study had several limitations. First, health literacy data were self-reported, and self-reported data can be subject to bias (eg, social desirability bias). Respondents to the BRFSS survey may have had undiagnosed prediabetes, which would have led to misclassification. Also, we treated data from respondents who answered “I don’t look for health information” in Question 1 and “I don’t pay attention to written health information” in Question 3 as missing. These respondents may have had limited health literacy. Second, we could not assess other health behaviors, such as dietary intake, because these data were not available in the BRFSS. Third, health behaviors were treated as outcomes in our study. Therefore, we could not test whether unhealthy behaviors might lead to prediabetes; that pathway was beyond the scope of this study. Fourth, the 3-item health literacy questionnaire was administered as an optional module, thereby limiting generalizability of findings to other states and territories. Finally, having low health literacy did not completely mediate the relationship between prediabetes and health behaviors—the ratio of indirect effect to total effect was small. Other factors, such as self-efficacy, likely contributed to this relationship.32
Conclusion
We found that adults with prediabetes had lower levels of health literacy and were more likely to practice unhealthy behaviors than adults without prediabetes. Health literacy plays an important role in the relationship between prediabetes and health behaviors. Intervention programs can target this modifiable factor to improve health behaviors and prevent prediabetes from developing into type 2 diabetes. Adults with low levels of health literacy, particularly those in low-resource communities, may not understand that physical inactivity and inadequate sleep can lead to type 2 diabetes. It is of public health importance to improve the health literacy level of these adults so that this population can adequately comprehend, communicate about, and manage health issues to reduce the risk of type 2 diabetes.
Acknowledgments
We presented the results of our study at the annual meeting of the 2019 American Public Health Association in Philadelphia, Pennsylvania, November 2-6, 2019.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Huabin Luo https://orcid.org/0000-0002-5144-3210
References
- 1. Centers for Disease Control and Prevention National diabetes statistics report: estimates of diabetes and its burden in the United States. 2020. Accessed March 29, 2020 https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
- 2. Centers for Disease Control and Prevention Prediabetes: your chance to prevent type 2 diabetes. Accessed November 22, 2019 https://www.cdc.gov/diabetes/basics/prediabetes.html
- 3. Bailey SC., Brega AG., Crutchfield TM. et al. Update on health literacy and diabetes. Diabetes Educ. 2014;40(5):581-604. 10.1177/0145721714540220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sørensen K., Van den Broucke S., Fullam J. et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. 10.1186/1471-2458-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Institute of Medicine Health Literacy: A Prescription to End Confusion . National Academic Press; 2004. [Google Scholar]
- 6. Brach C., Keller D., Hernandez L. et al. Ten Attributes of Health Literate Health Care Organizations. Vol. 2 National Academy of Sciences; 2012. Accessed January 25, 2019 https://nam.edu/wp-content/uploads/2015/06/BPH_Ten_HLit_Attributes.pdf 10.31478/201206a [DOI] [Google Scholar]
- 7. Vernon J., Trujillo A., Rosenbaum S., DeBuono B. Low health literacy: implications for national health policy. Accessed June 20, 2019 http://hsrc.himmelfarb.gwu.edu/sphhs_policy_facpubs/172/
- 8. US Department of Health and Human Services Healthy People 2020 topics & objectives: improve the health literacy of the population. Accessed June 1, 2019 https://www.healthypeople.gov/2020/topics-objectives
- 9. US Department of Health and Human Services, Office of Disease Prevention and Health Promotion National Action Plan to Improve Health Literacy. US Department of Health and Human Services; 2010. [Google Scholar]
- 10. Berkman ND., Sheridan SL., Donahue KE., Halpern DJ., Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97-107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- 11. Friis K., Vind BD., Simmons RK., Maindal HT. The relationship between health literacy and health behaviour in people with diabetes: a Danish population-based study. J Diabetes Res. 2016;2016:7823130. 10.1155/2016/7823130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Qin L., Xu H. A cross-sectional study of the effect of health literacy on diabetes prevention and control among elderly individuals with prediabetes in rural China. BMJ Open. 2016;6(5):e011077. 10.1136/bmjopen-2016-011077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention BRFSS survey data and documentation. 2016. Accessed April 3, 2020 https://www.cdc.gov/brfss/annual_data/annual_2016.html
- 14. Baur C., Rubin D. Putting health literacy questions on the nation’s public health report card. Health Literacy Annual Research Conference; October 13, 2016; Bethesda, MD. Accessed March 30, 2019 www.bumc.bu.edu/healthliteracyconference/files/2016/06/Baur_Cynthia.pdf
- 15. US Department of Health and Human Services The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General . US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 16. Centers for Disease Control and Prevention Diabetes: who’s at risk? 2019. Accessed January 24, 2019 https://www.cdc.gov/diabetes/basics/risk-factors.html
- 17. Knutson KL., Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287-304. 10.1196/annals.1417.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Touma C., Pannain S. Does lack of sleep cause diabetes? Cleve Clin J Med. 2011;78(8):549-558. 10.3949/ccjm.78a.10165 [DOI] [PubMed] [Google Scholar]
- 19. Brega AG., Ang A., Vega W. et al. Mechanisms underlying the relationship between health literacy and glycemic control in American Indians and Alaska Natives. Patient Educ Couns. 2012;88(1):61-68. 10.1016/j.pec.2012.03.008 [DOI] [PubMed] [Google Scholar]
- 20. Osborn CY., Bains SS., Egede LE. Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Technol Ther. 2010;12(11):913-919. 10.1089/dia.2010.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Luo H., Patil SP., Cummings DM. et al. Health literacy, self-management activities, and glycemic control among adults with type 2 diabetes: a path analysis. J Public Health Manag Pract. 2020;26(3):280-286. 10.1097/PHH.0000000000000984 [DOI] [PubMed] [Google Scholar]
- 22. Hayes AF., Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. Br J Math Stat Psychol. 2014;67(3):451-470. 10.1111/bmsp.12028 [DOI] [PubMed] [Google Scholar]
- 23.Stata [statistical software] Release 14. StataCorp LLC; 2015.
- 24. Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21(8):878-883. 10.1111/j.1525-1497.2006.00540.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ngoh LN. Health literacy: a barrier to pharmacist-patient communication and medication adherence. J Am Pharm Assoc (2003). 2009;49(5):e132-e149. 10.1331/JAPhA.2009.07075 [DOI] [PubMed] [Google Scholar]
- 26. Baker DW., Gazmararian JA., Williams MV. et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92(8):1278-1283. 10.2105/AJPH.92.8.1278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Altin SV., Finke I., Kautz-Freimuth S., Stock S. The evolution of health literacy assessment tools: a systematic review. BMC Public Health. 2014;14:1207. 10.1186/1471-2458-14-1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jordan JE., Osborne RH., Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J Clin Epidemiol. 2011;64(4):366-379. 10.1016/j.jclinepi.2010.04.005 [DOI] [PubMed] [Google Scholar]
- 29. Kutner M., Greenburg E., Jin Y., Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy. Report No: NCES 2006-483. US Department of Education, National Center for Education Statistics; 2006. [Google Scholar]
- 30. Centers for Disease Control and Prevention The surprising truth about prediabetes. 2020. Accessed March 23, 2020 https://www.cdc.gov/features/diabetesprevention/index.html
- 31. Safeer RS., Keenan J. Health literacy: the gap between physicians and patients. Am Fam Physician. 2005;72(3):463-468. [PubMed] [Google Scholar]
- 32. Lee YJ., Shin SJ., Wang RH., Lin KD., Lee YL., Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns. 2016;99(2):287-294. 10.1016/j.pec.2015.08.021 [DOI] [PubMed] [Google Scholar]