Abstract
Objectives
Although research shows that public health is substantially affected during and after disasters, few studies have examined the health effects of Hurricane Harvey, which made landfall on the Texas coast in August 2017. We assessed disparities in physical health, mental health, and health care access after Hurricane Harvey among residents of the Houston–The Woodlands–Sugar Land, Texas, metropolitan statistical area (ie, Houston MSA).
Methods
We used structured survey data collected through telephone and online surveys from a population-based random sample of Houston MSA residents (n = 403) collected from November 29, 2017, through January 6, 2018. We used descriptive statistics to describe the prevalence of physical health/mental health and health care access outcomes and multivariable generalized linear models to assess disparities (eg, based on race/ethnicity, socioeconomic status, disability) in health outcomes.
Results
Physical health problems disproportionately affected persons who did not evacuate (odds ratio [OR] = 0.41; 95% confidence interval [CI], 0.19-0.87). Non-Hispanic black persons were more likely than non-Hispanic white persons to have posttraumatic stress (OR = 5.03; 95% CI, 1.90-13.10), as were persons in households that experienced job loss post-Harvey (vs did not experience job loss post-Harvey; OR = 2.89; 95% CI, 1.14-7.32) and older persons (OR = 1.04; 95% CI, 1.01-1.06). Health care access was constrained for persons whose households lost jobs post-Harvey (vs did not lose jobs post-Harvey; OR = 2.73; 95% CI, 1.29-5.78) and for persons with disabilities (vs without disabilities; OR = 3.19; 95% CI, 1.37-7.45).
Conclusions
Our findings underscore the need to plan for and ameliorate public health disparities resulting from climate change–related disasters, which are expected to occur with increased frequency and magnitude.
Keywords: health disparities, Hurricane Harvey, disaster, flooding
Hurricane Harvey made landfall on the Texas coast in August 2017. Harvey was an unprecedented tropical storm; total rainfall for the Houston, Texas, area was 36-48 inches.1 Rainfall caused flooding across the Houston–The Woodlands–Sugar Land metropolitan statistical area (ie, Houston MSA), resulting in about $125 billion in damages, making it the second costliest disaster in US history, after Hurricane Katrina in 2005.1 Although research shows that public health is substantially affected during and after disasters,2-9 few studies have examined the health effects of Harvey, none of which have been population based.
Persons in racial/ethnic minority groups, older persons, persons with disabilities or infirmities, and persons of low socioeconomic status (SES) disproportionately experience poor health outcomes after disasters occur.10-15 Research on Harvey found disparities in flood exposure based on race/ethnicity and SES.16-18 For example, after a flood event in El Paso, Texas, non–US citizens (vs US citizens) and persons of Hispanic ethnicity (vs non-Hispanic white persons) were more likely to have physical health problems such as allergies, headaches, coughing and wheezing, and throat, nose, eye, and skin irritations.10 A literature review published in 2012 concluded that men (vs women) and older persons (vs younger persons) tend to have a higher risk of physical health problems during and after flood events.2 In addition, women and persons of low SES had an increased risk of having posttraumatic stress (PTS) after Hurricane Ike, which occurred in 2008.19 In the El Paso study, non–US citizens were more likely to have mental health problems than US citizens.10
Public health issues resulting from Harvey have been inadequately documented in the literature. Studies have relied on small convenience samples of local residents. At a convention center in Houston, researchers found more than 200 evacuees seeking mental health treatment, many of whom had no access to needed medications.20 Another study found that many persons who relocated to shelters after Harvey had high levels of anxiety as a result.21 A survey of 41 persons in the Houston MSA found that hurricane exposure and property damage were associated with increased symptoms of PTS.22 Although these studies identified health effects resulting from Harvey, they were not based on representative, population-based samples but instead were based on convenience samples. To advance knowledge of Hurricane Harvey’s health effects, we conducted a population-based study based on a random sample of residents in the Houston MSA.
Our study addressed 2 research questions: (1) To what extent did Hurricane Harvey affect the physical health, mental health, and health care access of Houston MSA residents? and (2) How were factors of social vulnerability, disaster experiences, home site effects, and access to aid associated with physical health, mental health, and health care access outcomes among Houston MSA residents, during and soon after Hurricane Harvey?
Methods
Data Collection and Sample
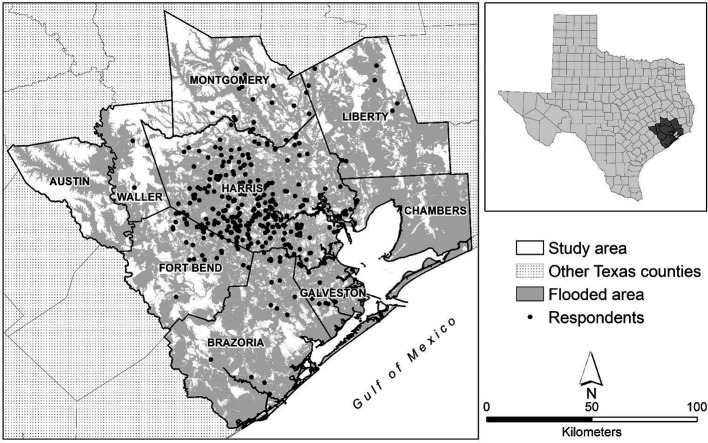
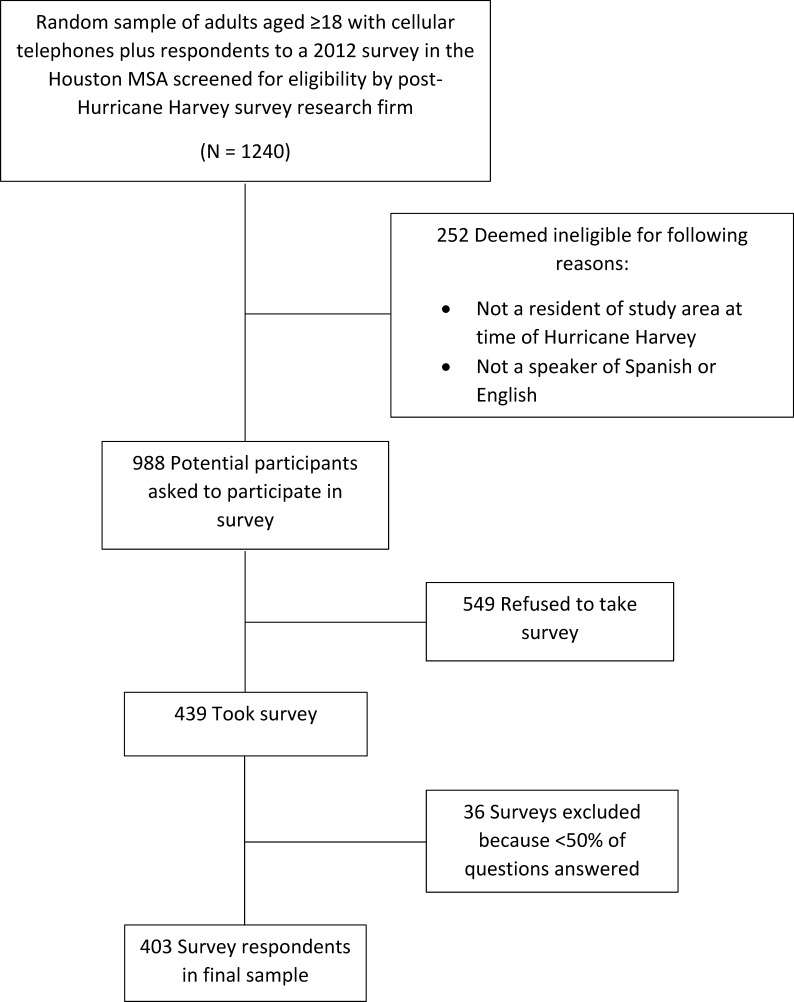
We collected data through telephone and online surveys of a random sample of Houston MSA residents from November 29, 2017, through January 6, 2018. The sampling frame consisted of adults aged ≥18 with cellular telephones in the Houston MSA (n = 1240). Using random-digit dialing within a random sample of cellular telephone numbers across this area, interviewers from a survey research firm screened respondents for eligibility, which was based on permanent residence in the Houston MSA at the time of Hurricane Harvey (August 25, 2017) and the ability to speak Spanish or English (Figure 1). Cellular telephone numbers were important because they allowed us to reach persons who had relocated (temporarily or permanently) because of Harvey.24 Respondents could take the survey by cellular telephone in English or Spanish; the average time for survey completion was 46 minutes. We augmented the sample with completed surveys from respondents to a representative, probability-based survey focused on flood hazards conducted in 2012; we updated their contact information and recontacted them as part of our 2017 post-Harvey survey.25,26
Figure 1.
Counties of the Houston–The Woodlands–Sugar Land, Texas, metropolitan statistical area, 2017. Data source: The flooded area is based on the Hurricane Harvey Inundation Footprint from the Federal Emergency Management Agency Region 6.23
Of 988 eligible respondents we contacted, 439 (44.4%) took the survey: 368 were new respondents from the cellular telephone sample and 71 were resurveyed respondents from the 2012 survey (Figure 2).25 This calculation follows the American Association for Public Opinion Research Cooperation Rate 2 guidelines.27 We excluded 36 respondents who did not complete at least 50% of the survey items relevant to this analysis, leaving a final sample of 403 survey respondents.
Figure 2.
Data collection process for a post–Hurricane Harvey survey in the Houston–The Woodlands–Sugar Land, Texas, metropolitan statistical area (ie, Houston MSA), 2017.
Survey respondents were generally representative of adult residents in the Houston MSA in terms of race/ethnicity, income, and age. The 2016 average annual household income for respondents was $66 400, whereas the 2016 median annual household income for Houston MSA residents was $61 708.28 The survey sample was 34% non-Hispanic white, 38% Hispanic/Latino, and 19% non-Hispanic black. In the Houston MSA in 2016, non-Hispanic white adults comprised approximately 36%, Hispanic/Latino adults comprised 37%, and non-Hispanic black adults comprised 17% of the adult population. The median age of survey respondents was 49.6; the average age for the adult population in the Houston MSA was 46.28
We adapted the survey instrument from previously administered post–flood disaster survey instruments.10,13,29-31 Through the survey, we collected data from participants on health problems experienced during and after Harvey, lack of access to health care during and after Harvey, and other domains (ie, social vulnerability, disaster experiences, home site effects, and access to aid). We geocoded data on respondents’ home addresses and integrated the data with Federal Emergency Management Agency (FEMA) estimates of the Harvey flood extent for areas surrounding their home sites.
Dependent Variables
We included 3 dichotomous dependent variables: physical health problems, PTS, and lack of access to health care. We assessed data on physical health problems based on respondents’ answers to 24 items about having physical health problems during or any time after Hurricane Harvey. We recoded the variable such that respondents who did not have any physical health problem were coded 0, and respondents who had at least 1 physical health problem were coded 1. We measured PTS by using the Post-Traumatic Stress Disorder Checklist-S (PCL-S),32 a 17-item self-reported measure that includes questions about experiences that occurred at any time since Harvey. Responses to each item were on a 5-point Likert-type scale, where 1 = not at all, 2 = a little bit, 3 = moderately, 4 = quite a bit, and 5 = very much. Overall scores can range from 17 to 85. Although various thresholds have been used to screen persons for PTS,32 we used a threshold of 40 based on previous studies assessing disaster-induced PTS.22,33 Respondents with a PTS score <40 were coded as 0 (no or low PTS), and respondents with a PTS score ≥40 were coded as 1 (high PTS). For the lack of access to health care variable, we coded respondents who had continuous access to health care during or soon after Harvey as 0 and respondents who went without access to health care during or soon after Harvey as 1.
Independent Variables
We classified independent variables into 4 domains: (1) social vulnerability, (2) disaster experiences, (3) home site effects, and (4) access to aid (Table 1).
Table 1.
Survey question and summary statistics for variables analyzed among adult respondents (N = 403) to a post–Hurricane Harvey survey in the Houston–The Woodlands–Sugar Land, Texas, metropolitan statistical area, 2017
| Variable | Survey Question | No. of Respondents | Mean Value | No. (%) of Respondents With Missing Information for This Question |
|---|---|---|---|---|
| Dependent variables | ||||
| Physical health problems | Respondent was asked if he/she experienced 24 health problems (Table 2) during or any time after Hurricane Harvey | |||
| 0 = No problems experienced | 177 | 0.56 | 0 | |
| 1 = ≥1 problem experienced | 226 | |||
| Posttraumatic stress | Respondent was asked 17 items related to posttraumatic stress symptoms from the Post-Traumatic Stress Disorder Checklist-S (PCL-S),32 and a composite score (on a scale of 17-85) was calculated (Table 3) | |||
| 0 = No, score <40 | 304 | 0.18 | 32 (8.0) | |
| 1 = Yes, score ≥40 | 67 | |||
| Lack of access to health care | Respondent was asked if he/she went without access to health care or medical services for some time during or soon after Hurricane Harvey | |||
| 0 = No | 305 | 0.22 | 10 (2.5) | |
| 1 = Yes | 88 | |||
| Social vulnerability | ||||
| Age | In what year were you born? | 377 | 49.6 | 26 (6.4) |
| Sex | Are you male or female? | |||
| 0 = Female | 220 | 0.44 | 7 (1.7) | |
| 1 = Male | 176 | |||
| Ethnicity | Are you Hispanic, Latino, or of Spanish origin? | |||
| 0 = No | 245 | 0.38 | 5 (1.2) | |
| 1 = Yes | 153 | |||
| Black or African American | Which of the following best describes your race? | |||
| 0 = No, if not black or African American | 319 | 0.20 | 8 (2.0) | |
| 1 = Yes, if black or African American | 76 | |||
| Multiple/other races | Which of the following best describes your race? | |||
| 0 = No, if not multiple/other races | 357 | 0.09 | 9 (2.2) | |
| 1 = Yes, if not multiple/other races | 37 | |||
| US born | Were you born in the United States? | |||
| 0 = No | 131 | 0.67 | 10 (2.5) | |
| 1 = Yes | 262 | |||
| Income | What was your total annual household income for the year 2016 before taxes? | |||
| 1 = <$10 000 2 = $10 000-$19 999 3 = $20 000-$29 999 4 = $30 000-$39 999 5 = $40 000-$49 999 6 = $50 000-$74 999 7 = $75 000-$99 999 8 = $100 000-$149 999 9 = $150 000-$249 999 10 = ≥$250 000 |
367 | 4.89 | 36 (8.9) | |
| Disaster experiences | ||||
| Evacuation disability | Because of a physical, mental, or emotional health condition, did you need any special assistance during Hurricane Harvey to evacuate your home and get to a safe place? | |||
| 0 = No | 364 | 0.07 | 10 (2.5) | |
| 1 = Yes | 29 | |||
| Evacuated | Did you evacuate your home? | |||
| 0 = No | 302 | 0.23 | 13 (3.0) | |
| 1 = Yes | 88 | |||
| Lost job | Did you or anyone else in your household lose a job because of Hurricane Harvey? | |||
| 0 = No | 357 (0) | 0.09 | 9 (2.2) | |
| 1 = Yes | 37 (1) | |||
| Unmet needsa | Which of the following happened to you during or soon after Hurricane Harvey? | |||
| Sum of 10 measures (range, 0-10)a | 393 | 2.73 | 10 (2.5) | |
| Adverse eventsb | Which of the following happened to you during or soon after Hurricane Harvey? | |||
| Sum of 12 measures (range, 0-12)b | 393 | 3.04 | 10 (2.5) | |
| Personal exposuresc | Which of the following happened to you during or soon after Hurricane Harvey? | |||
| Sum of 5 measures (range, 0-5)c | 393 | 1.13 | 10 (2.5) | |
| Home site effects | ||||
| Flood extentd | Proportion of area surrounding respondents’ home (100-m radius) that floodedd | 357 | 0.16 | 46 (11.4) |
| Level of home damage | Was the home you were living in at the time of Hurricane Harvey “not damaged at all,” “damaged to a minor degree,” “damaged to a limited degree,” “seriously damaged,” or “completely destroyed”? | |||
| 1 = Not damaged at all 2 = Minor damage 3 = Limited damage 4 = Serious damage 5 = Completely destroyed |
392 | 1.84 | 11 (2.7) | |
| Square feet of mold | How much surface area in the home you lived in was covered by mold after Hurricane Harvey? | |||
| 1 = 0 2 = <10 square feet 3 = 10-25 square feet 4 = 25-100 square feet 5 = >100 square feet |
389 | 1.72 | 14 (3.5) | |
| Access to aid | ||||
| Cleanup | After Hurricane Harvey, did you help clean or repair any flooded home sites? | |||
| 0 = No | 100 | 0.74 | 21 (5.2) | |
| 1 = Yes | 282 | |||
| Received social supporte | Since Hurricane Harvey, how often did family members, friends, neighbors, or coworkers . . . ? | |||
| Sum of 8 measures (range, 8-32)e | 394 | 15.4 | 9 (2.2) | |
aUnmet needs items were as follows: you went without a comfortable place to sleep for some time; you went without adequate drinking water for some time; you went without adequate clothing for some time; you went without a bathroom for some time; you went without running hot water for some time; you went without electricity for some time; you went without adequate food for some time; you went without adequate transportation for some time; you lacked money for living expenses for some time; or you went without clean piped water for some time.
bAdverse events items were as follows: you saw someone drowning or in danger of drowning; you lost a pet or had to abandon one; you worried about crime; you had to perform a dangerous activity; you were stranded in an unsafe place during the disaster; you lost irreplaceable items such as photographs, family mementos; you thought at least once that you might be injured or killed; you worried about family members or friends; you had to split up from household members; you were separated from your children; you experienced unsanitary living conditions; or you experienced crowded living conditions.
cPersonal exposure items were as follows: you were present when major flooding or hurricane damage occurred; you were a victim of a crime; you smelled unpleasant chemical odors; you inhaled smoke from chemical fires; or you made physical or skin contact with chemicals or contaminants.
dDerived using the Federal Emergency Management Agency estimates of Harvey flood extent for areas surrounding respondents’ home sites.23
eSocial support items were as follows: suggest some action that you should take; give, loan, or offer you money or something else you needed; comfort you with a hug or another sign of affection; let you know they would be around if you needed them; express interest and concern in your well-being; offer or provide you with a place to stay; help you with cleaning up or improving your property; or bring you food or cook for you.
Social vulnerability
We treated age as a continuous variable. Female respondents were the reference category (0), and male respondents were the response category (1). We operationalized race/ethnicity as a construct including dichotomous variables for Hispanic, non-Hispanic black, and non-Hispanic multiple/other race (nonwhite); in the multivariable models, results for those variables are interpretable in reference to the non-Hispanic white group. We coded respondents born outside the United States as 0 and respondents born in the United States as 1. Annual household income in 2016 was a 10-category measure (<$10 000, $10 000-$19 999, $20 000-$29 999, $30 000-$39 999, $40 000-$49 999, $50 000-$74 999, $75 000-$99 999, $100 000-$149 999, $150 000-$249 999, ≥$250 000).
Disaster experiences
We coded respondents without a disability as 0 and respondents with a physical or emotional disability that influenced their ability to evacuate as 1. We coded respondents who did not evacuate as 0 and respondents who did evacuate as 1. Losing a job because of Harvey was a dichotomous variable: we coded respondents whose households did not experience job loss as 0 and respondents whose households did experience job loss as 1. We created a variable for unmet needs by summing responses to 10 checklist-type items (with yes = 1 and no = 0): you went without a comfortable place to sleep for some time; you went without adequate drinking water for some time; you went without adequate clothing for some time; you went without a bathroom for some time; you went without running hot water for some time; you went without electricity for some time; you went without adequate food for some time; you went without adequate transportation for some time; you lacked money for living expenses for some time; or you went without clean piped water for some time. We determined the extent of adverse events experienced by summing 12 checklist-type items: you saw someone drowning or in danger of drowning; you lost a pet or had to abandon one; you worried about crime; you had to perform a dangerous activity; you were stranded in an unsafe place during the disaster; you lost irreplaceable items such as photographs, family mementos or heirlooms, jewelry, or documents; you thought at least once that you might be injured or killed; you worried about family members or friends; you had to split up from household members; you were separated from your children; you experienced unsanitary living conditions; or you experienced crowded living conditions. We assessed personal exposures by summing 5 checklist-type items: you were present when major flooding or hurricane damage occurred; you were a victim of a crime; you smelled unpleasant chemical odors; you inhaled smoke from chemical fires; or you made physical or skin contact with chemicals or contaminants.
Home site effects
We derived the flood extent by using Harvey’s Inundation Footprint, a cartographic product developed by the FEMA Region 6 Mitigation Division.23 This raster map layer contains flood depth values for each grid pixel (3×3 m) in the study area and was used in recent Harvey studies.16-18 Using ArcGIS Desktop version 10.5.1,34 we generated a flood extent value for each survey respondent by creating a circular buffer (100-m radius) around each geocoded home location and summing all flooded pixels (nonzero depth) areas within the buffer. Next, we divided the flooded area sum by the area of the circular buffer (square meters) to derive the proportion of the area surrounding the respondent’s home that was flooded because of Harvey. The level of home damage was a self-reported measure ranging from 0 (not damaged at all) to 5 (completely destroyed). The square footage of mold present in the respondent’s home was a self-reported measure ranging from 1 (none) to 5 (>100 ft2).
Access to aid
We coded respondents who did not help clean or repair flooded homes as 0 and respondents who did help clean or repair flooded homes as 1. We measured social support by summing respondents’ answers to 8 questions about how often they received the following types of help from family, friends, neighbors, or coworkers: suggest some action that you should take; give, loan, or offer you money or something else you needed; comfort you with a hug or another sign of affection; let you know they would be around if you needed them; express interest and concern in your well-being; offer or provide you with a place to stay; help you with cleaning up or improving your property; or bring you food or cook for you.
Data Analysis
To answer research question 1, we used descriptive statistics for the dependent variables and individual indicators comprising the physical health problems and PTS measures. To answer research question 2, we began by using multiple imputation, which is a best practice for reducing bias when analyzing data with missing values.35,36 We tabulated the percentage of missing values for each variable in the original data set; the percentage of respondents with missing information for our analysis variables ranged from 0% for physical health problems to 11.4% for flood extent (Table 1). As is recommended, we performed multiple imputation to create 20 data sets with imputed values for all missing data points.10,18,37,38 We specified all ordinal variables as continuous variables, which is recommended in the multiple imputation literature, because rounding imputed values to conform to discrete ordinal variable specifications results in more biased parameter estimates than treating ordinal variables as continuous in multivariable models.37,39-41
We used the multiple imputation data in binary logistic generalized linear modeling10 to predict the 3 dichotomous dependent variables. The physical health model did not include social support as an independent variable because social support has not been previously linked to postdisaster physical health outcomes. Social support was included in the PTS model because evidence indicates that social support protects against mental health problems (eg, depression, PTS) after disasters.42,43 The PTS model did not include cleaning activities because these activities are not known to predict PTS. The access to health care model included only social vulnerability variables and having an evacuation disability. For each model, we used Akaike information criterion values to assess goodness of fit. Diagnostic testing indicated that the models were not affected by multicollinearity. We report pooled results from analyses of the 20 multiply imputed data sets for each of the 3 dependent variables. We conducted all analyses by using SPSS version 25.44
Results
Research Question 1
More than half of respondents (226 of 403, 56.1%) had ≥1 physical health problem (Table 1). On average, respondents had 3 physical health problems, and 45 (11.2%) respondents had ≥10 physical health problems. The most common physical health problems were allergies or hay fever (n = 132, 32.8%), headaches (n = 114, 28.3%), nose irritation (n = 110, 27.3%), and throat irritation (n = 107, 26.6%; Table 2). Sixty-seven of 371 (18.1%) respondents had PTS scores ≥40. Of the 17 items on the PCL-S, having repeated, disturbing memories, thoughts, or images of Harvey was the most reported experience (n = 194 of 400, 48.5%; Table 3). Eighty-eight of 393 (22.4%) respondents reported going without access to health care during or soon after Harvey.
Table 2.
Physical health problems experienced by respondents to a post–Hurricane Harvey survey (N = 403) in the Houston–The Woodlands–Sugar Land, Texas, metropolitan statistical area, 2017
| Physical Health Problem | No. (%) Affected |
|---|---|
| Allergies or hay fever | 132 (32.8) |
| Headaches | 114 (28.3) |
| Nose irritation | 110 (27.3) |
| Throat irritation | 107 (26.6) |
| More allergies or hay fever than before Hurricane Harvey | 106 (26.3) |
| Eye irritation | 88 (21.8) |
| More coughing or wheezing than before Hurricane Harvey | 78 (19.4) |
| Lung or airway irritations or inflammation | 60 (14.9) |
| Dizziness | 52 (12.9) |
| Skin irritation | 50 (12.4) |
| Missed work or school because of coughing or wheezing | 48 (11.9) |
| Fever | 46 (11.4) |
| Blurred vision | 46 (11.4) |
| Diarrhea | 44 (10.9) |
| Nausea | 43 (10.7) |
| Asthma | 36 (8.9) |
| More asthma attacks than before Hurricane Harvey | 30 (7.4) |
| Vomiting | 30 (7.4) |
| Athlete’s foot | 29 (7.2) |
| Gastrointestinal infection | 15 (3.7) |
| Any other infectious disease | 11 (2.7) |
| Food poisoning | 7 (1.7) |
| West Nile virus | 4 (1.0) |
| Hepatitis A | 3 (0.7) |
Table 3.
Posttraumatic stress symptoms experienced by respondents to a post–Hurricane Harvey survey (N = 403) in the Houston–The Woodlands–Sugar Land, Texas, metropolitan statistical area, 2017
| Posttraumatic Stress Symptoms | No. of Respondents for This Question | No. (%) Affected “a Little Bit,” “Moderately,” “Quite a Bit,” or “Very Much” |
|---|---|---|
| Having repeated, disturbing memories, thoughts, or images of Hurricane Harvey | 400 | 194 (48.5) |
| Being “super-alert,” watchful, or on guard | 400 | 163 (40.8) |
| Feeling very upset when something reminded you of Hurricane Harvey | 395 | 160 (40.5) |
| Avoiding thinking about or talking about Hurricane Harvey or avoiding having feelings related to it | 397 | 148 (37.3) |
| Having repeated, disturbing dreams of Hurricane Harvey | 398 | 122 (30.7) |
| Suddenly acting or feeling as if Hurricane Harvey was happening again—as if you were reliving it | 401 | 120 (29.9) |
| Feeling jumpy or easily startled | 401 | 116 (28.9) |
| Having trouble falling or staying asleep | 397 | 114 (28.7) |
| Having difficulty concentrating | 399 | 114 (28.6) |
| Feeling distant or cut off from other people | 397 | 100 (25.2) |
| Feeling irritable or having angry outbursts | 401 | 100 (24.9) |
| Having a loss of interest in activities that you used to enjoy | 401 | 96 (23.9) |
| Having physical reactions—that is, heart pounding, trouble breathing, sweating—when something reminded you of Hurricane Harvey | 397 | 95 (23.9) |
| Avoiding activities or situations because they reminded you of Hurricane Harvey | 400 | 90 (22.5) |
| Having trouble remembering important parts of Hurricane Harvey | 399 | 84 (21.1) |
| Feeling as if your future will somehow be cut short | 399 | 82 (20.6) |
| Feeling emotionally numb or being unable to have loving feelings for those close to you | 397 | 81 (20.4) |
aPosttraumatic stress was measured by using the Post-Traumatic Stress Disorder Checklist-S (PCL-S),32 a 17-item self-reported measure that includes questions about experiences that occurred at any time since Harvey. Responses to each item were on a 5-point Likert-type scale, where 1 = not at all, 2 = a little bit, 3 = moderately, 4 = quite a bit, and 5 = very much.
Research Question 2
Respondents who evacuated after Harvey had 59% lower odds than those who did not evacuate of having ≥1 physical health problem (odds ratio [OR] = 0.41; 95% confidence interval [CI], 0.19-0.87). For each additional adverse event experience, respondents had 36% greater odds of reporting ≥1 physical health problem (OR = 1.36; 95% CI, 1.15-1.60). In addition, each scale unit increase in square feet of mold in the home resulted in a 39% increase in the odds of experiencing ≥1 physical health problem (OR = 1.39; 95% CI, 1.05-1.86; Table 4).
Table 4.
Generalized linear models predicting physical health problems, posttraumatic stress, and lack of access to health care among respondents to a post-Hurricane Harvey survey (N = 403) in the Houston–The Woodlands–Sugar Land, Texas, metropolitan statistical area, 2017a
| Variable | Has ≥1 Physical Health Problem | Posttraumatic Stress ≥40b | Lack of Access to Health Care |
|---|---|---|---|
| Social vulnerability | |||
| Age | 1.01 (0.99-1.03) [.22] | 1.04 (1.01-1.06) [.002] | 1.00 (0.98-1.01) [.71] |
| Sex | |||
| Female | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Male | 0.74 (0.46-1.19) [.21] | 0.80 (0.41-1.54) [.50] | 0.83 (0.50-1.39) [.49] |
| Race/ethnicity | |||
| Non-Hispanic white | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Hispanic | 0.76 (0.35-1.64) [.48] | 1.94 (0.65-5.80) [.24] | 1.26 (0.56-2.84) [.58] |
| Non-Hispanic black | 0.88 (0.43-1.79) [.73] | 5.03 (1.93-13.13) [<.001] | 1.57 (0.79-3.12) [.20] |
| Multiple/other races | 1.34 (0.60-3.00) [.47] | 1.11 (0.37-3.38) [.85] | 2.04 (0.92-4.53) [.08] |
| Nativity | |||
| Non–US-born | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| US-born | 1.31 (0.66-2.59) [.45] | 0.83 (0.33-2.08) [.69] | 1.79 (0.86-3.73) [.12] |
| Annual household income (2016) | 0.98 (0.88-1.08) [.68] | 0.96 (0.82-1.12) [.57] | 0.95 (0.85-1.06) [.31] |
| Disaster experiences | |||
| Needed assistance in evacuating because of a disability | |||
| No | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Yes | 1.35 (0.34-5.33) [.67] | 0.70 (0.22-2.25) [.55] | 3.19 (1.37-7.45) [.01] |
| Evacuated from home | |||
| No | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Yes | 0.41 (0.19-0.87) [.02] | 0.69 (0.26-1.79) [.44] | — |
| Persons in household experienced job loss post-Harvey | |||
| No | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Yes | 1.11 (0.45-2.74) [.82] | 2.89 (1.14-7.32) [.03] | 2.73 (1.29-5.78) [.01] |
| Unmet needs | 1.02 (0.91-1.15) [.72] | 1.11 (0.96-1.28) [.15] | — |
| Adverse event experiences | 1.36 (1.15-1.60) [<.001] | 1.28 (1.08-1.53) [.01] | — |
| Personal exposures | 1.31 (0.95-1.81) [.10] | 0.97 (0.63-1.48) [.88] | — |
| Home site effects | |||
| Flood extent | 0.38 (0.08-1.87) [.23] | 0.68 (0.06-8.20) [.76] | — |
| Level of home damage | 1.23 (0.88-1.71) [.23] | 0.83 (0.55-1.25) [.37] | — |
| Square feet of mold | 1.39 (1.05-1.86) [.02] | 1.55 (1.19-2.03) [<.001] | — |
| Access to aid | |||
| Helped clean up | |||
| No | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Yes | 1.63 (0.95-2.79) [.08] | — | — |
| Received social support | — | 1.06 (0.99-1.12) [.09] | — |
Abbreviation: —, not included in the model.
aAll values are odds ratio (95% CI) [P value]. The Wald χ2 test was used to determine significance; P < .05 was considered significant. Results are for analyses of multiply imputed data.
bPosttraumatic stress scores ranged from 17 (did not experience any symptoms at all) to 85 (experienced all symptoms very much).
Each additional year in age was associated with a 4% increase in the odds of having a PTS score ≥40 (OR = 1.04; 95% CI, 1.01-1.06; Table 4). Being non-Hispanic black versus non-Hispanic white was associated with a 403% increase in the odds of having a PTS score ≥40 (OR = 5.03; 95% CI, 1.93-13.13). Having a household member experience job loss because of Hurricane Harvey was associated with a 189% increase in the odds of having a PTS score ≥40 (OR = 2.89; 95% CI, 1.14-7.32). Each additional adverse event experience during or soon after Hurricane Harvey resulted in a 28% increase in the odds of having a PTS score ≥40 (OR = 1.28; 95% CI, 1.08-1.53). A scale-unit increase in square feet of mold present in the home was associated with a 55% increase in the odds of having a PTS score ≥40 (OR = 1.55; 95% CI, 1.19-2.03).
Having a disability that interfered with evacuation was associated with a 219% increase in the odds of going without access to health care after Harvey (OR = 3.19; 95% CI, 1.37-7.45; Table 4). Also, having a household member experience job loss because of Harvey was associated with a 173% increase in the odds of going without access to health care (OR = 2.73; 95% CI, 1.29-5.78).
Discussion
Descriptive statistics indicated the prevalent effects of Hurricane Harvey on the physical health, mental health, and lack of access to health care among residents of the Houston MSA. Physical health problems were prevalent in more than half of the sample. PTS affected approximately one-fifth of the population, which manifested most frequently in having repeated or disturbing memories of the hurricane. Nearly one-quarter of respondents reported going without adequate health care services during or after Harvey. These results align with previous findings after Hurricane Katrina.45-47
Our multivariable statistical models clarified important predictors of the 3 health-related outcomes. Evacuating at any time was protective, whereas more adverse event experiences (vs fewer adverse event experiences) and greater mold exposure (vs less mold exposure) increased the odds of having physical health problems after Harvey. The protective effect of evacuation was likely due to the evacuated residents’ absence during flooding, which reduced their odds of experiencing physical harm, highlighting the importance of evacuating during high-magnitude flood events. Adverse event experiences were also risk factors in the odds for greater severity of PTS, aligning with previous literature.10 Increased surface area of mold present in one’s home after Harvey was another substantial risk factor for greater severity of PTS. Studies have tested the relationship between mold exposure and mental health, but few have found significant relationships.48 Exposure to mold may induce physical discomfort or respiratory distress, which could exacerbate the stress response. Also, exposure to mold can impair cognitive function.49 Having a household member experience job loss because of Harvey played a substantial role in respondents’ mental health, significantly increasing their odds of having PTS. Older age also had a significant effect on respondents’ risk for PTS, which contradicts findings from most, but not all, postdisaster studies on PTS.13 Non-Hispanic black persons were disproportionately affected by PTS, highlighting environmental justice issues associated with flooding in the Houston MSA. These findings are also consistent with previous studies on mental health and disasters.8,19,50,51 Respondents whose households experienced job loss because of Harvey (vs households that did not experience job loss) and respondents whose disabilities made it difficult to evacuate (vs respondents without disabilities) faced greater odds of lacking access to health care after the event. These findings are concerning from a public health perspective. Disparate risks for populations with disabilities in the Houston MSA were also highlighted in a study that showed neighborhoods with higher (vs lower) proportions of residents with disabilities had more extensive flooding because of Harvey.17
Limitations
Although our sample was generally representative of the Houston MSA population, the data had some limitations. First, measurement error inevitably propagates in self-reported data, which were the basis for this study.52 Second, our analysis lacked the reference frame needed to attribute the health effects we documented directly to Harvey. For example, because we did not account for pre-Harvey health care access, we could not infer that Harvey exacerbated preexisting disparities in health care access. Thus, future postdisaster health research should seek to strengthen casual inferences using pre- and postevent designs and/or appropriate control groups. Finally, our PTS variable was not a diagnostic measure. It was a screening measure of PTS symptomatology based on a conventionally applied threshold.
Conclusion
To our knowledge, this study is the first to use a population-based random sample to analyze the physical health, mental health, and health care access outcomes among residents in the Houston MSA after Hurricane Harvey. Using structured survey data allowed us to determine which residents were disadvantaged in physical health, mental health, and access to health care. Our results indicate that Harvey had substantial effects on Houston MSA residents, highlighting racial/ethnic, age, and socioeconomic disparities, aligning with previous findings on environmental justice in the region.16,17,25,53-56 This study indicates a need to enhance knowledge of the role of race/ethnicity and SES in creating population health vulnerabilities in order to improve public health interventions, as some residents’ social disadvantages were associated with post-disaster health disparities. Our findings also indicate the need for improvements to flood hazard mitigation and public health response efforts in the Houston MSA. Public health officials can use this information to provide health services to disadvantaged populations in future flood events to ameliorate disparities. These efforts have become essential as similar events are more likely to occur now rather than 20 years ago in the Houston MSA because of climate change.57
Acknowledgments
The authors thank Mark English, the Hazard and Performance Analysis’s Geospatial Unit Lead with FEMA under Disaster Operations within the Mitigation Branch, for contributing to the creation of Harvey’s Inundation Footprint, a data product used in our analysis.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the US National Science Foundation (award no. 1841654). Any opinions, conclusions, or recommendations expressed in this article are those of the authors and do not necessarily reflect the views of the National Science Foundation.
ORCID iD
Aaron B. Flores https://orcid.org/0000-0003-0933-1386
References
- 1. Blake ES., Zelinsky DA. National Hurricane Center tropical cyclone report: Hurricane Harvey. 2018. Accessed March 30, 2020 https://www.hsdl.org/?view&did=807581
- 2. Alderman K., Turner LR., Tong S. Floods and human health: a systematic review. Environ Int. 2012;47:37-47. 10.1016/j.envint.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 3. Azuma K., Ikeda K., Kagi N., Yanagi U., Hasegawa K., Osawa H. Effects of water-damaged homes after flooding: health status of the residents and the environmental risk factors. Int J Environ Health Res. 2014;24(2):158-175. 10.1080/09603123.2013.800964 [DOI] [PubMed] [Google Scholar]
- 4. Rath B., Young EA., Harris A. et al. Adverse respiratory symptoms and environmental exposures among children and adolescents following Hurricane Katrina. Public Health Rep. 2011;126(6):853-860. 10.1177/003335491112600611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Murray KO., Kilborn C., DesVignes-Kendrick M. et al. Emerging disease syndromic surveillance for Hurricane Katrina evacuees seeking shelter in Houston’s Astrodome and Reliant Park complex. Public Health Rep. 2009;124(3):364-371. 10.1177/003335490912400304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Galea S., Tracy M., Norris F., Coffey SF. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. J Trauma Stress. 2008;21(4):357-368. 10.1002/jts.20355 [DOI] [PubMed] [Google Scholar]
- 7. Greenough PG., Lappi MD., Hsu EB. et al. Burden of disease and health status among Hurricane Katrina-displaced persons in shelters: a population-based cluster sample. Ann Emerg Med. 2008;51(4):426-432. 10.1016/j.annemergmed.2007.04.004 [DOI] [PubMed] [Google Scholar]
- 8. Goldmann E., Galea S. Mental health consequences of disasters. Annu Rev Public Health. 2014;35:169-183. 10.1146/annurev-publhealth-032013-182435 [DOI] [PubMed] [Google Scholar]
- 9. Marshall EG., Lu S-E., Williams AO., Lefkowitz D., Borjan M. Tree-related injuries associated with response and recovery from Hurricane Sandy, New Jersey, 2011-2014. Public Health Rep. 2018;133(3):266-273. 10.1177/0033354918766871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Collins TW., Jimenez AM., Grineski SE. Hispanic health disparities after a flood disaster: results of a population-based survey of individuals experiencing home site damage in El Paso (Texas, USA). J Immigr Minor Health. 2013;15(2):415-426. 10.1007/s10903-012-9626-2 [DOI] [PubMed] [Google Scholar]
- 11. Elliott JR., Pais J. Race, class, and Hurricane Katrina: social differences in human responses to disaster. Soc Sci Res. 2006;35(2):295-321. 10.1016/j.ssresearch.2006.02.003 [DOI] [Google Scholar]
- 12. Lowe D., Ebi KL., Forsberg B. Factors increasing vulnerability to health effects before, during and after floods. Int J Environ Res Public Health. 2013;10(12):7015-7067. 10.3390/ijerph10127015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Norris FH., Friedman MJ., Watson PJ., Byrne CM., Diaz E., Kaniasty K. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65(3):207-239. 10.1521/psyc.65.3.207.20173 [DOI] [PubMed] [Google Scholar]
- 14. Marmot M., Wilkinson RG. Social Determinants of Health. 2nd ed Oxford University Press; 2005. [Google Scholar]
- 15. Wilkinson RG. Unhealthy Societies, the Afflictions of Inequalities. Routledge; 1996. [Google Scholar]
- 16. Chakraborty J., Collins TW., Grineski SE. Exploring the environmental justice implications of Hurricane Harvey flooding in greater Houston, Texas. Am J Public Health. 2019;109(2):244-250. 10.2105/AJPH.2018.304846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chakraborty J., Grineski SE., Collins TW. Hurricane Harvey and people with disabilities: disproportionate exposure to flooding in Houston, Texas. Soc Sci Med. 2019;226:176-181. 10.1016/j.socscimed.2019.02.039 [DOI] [PubMed] [Google Scholar]
- 18. Collins TW., Grineski SE., Chakraborty J., Flores AB. Environmental injustice and Hurricane Harvey: a household-level study of socially disparate flood exposures in greater Houston, Texas, USA. Environ Res. 2019;179(Pt A):108772. 10.1016/j.envres.2019.108772 [DOI] [PubMed] [Google Scholar]
- 19. Ruggiero KJ., Gros K., McCauley JL. et al. Mental health outcomes among adults in Galveston. Disaster Med Public Health Prep. 2012;6(1):26-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shah AA., Valles N., Banu S., Storch EA., Goodman W. Meeting the mental health needs of Hurricane Harvey evacuees. Am J Psychiatry. 2018;175(1):13-14. 10.1176/appi.ajp.2017.17101108 [DOI] [PubMed] [Google Scholar]
- 21. Taioli E., Tuminello S., Lieberman-Cribbin W. et al. Mental health challenges and experiences in displaced populations following Hurricane Sandy and Hurricane Harvey: the need for more comprehensive interventions in temporary shelters. J Epidemiol Community Health. 2018;72(10):867-870. 10.1136/jech-2018-210626 [DOI] [PubMed] [Google Scholar]
- 22. Schwartz RM., Tuminello S., Kerath SM., Rios J., Lieberman-Cribbin W., Taioli E. Preliminary assessment of Hurricane Harvey exposures and mental health impact. Int J Environ Res Public Health. 2018;15(5):974. 10.3390/ijerph15050974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Federal Emergency Management Agency Harvey flood depths grid. 2018. Accessed April 13, 2020 https://www.hydroshare.org/resource/165e2c3e335d40949dbf501c97827837
- 24. Blumberg SJ., Luke JV. Wireless substitution: early release of estimates from the National Health Interview Survey, July–December 2016. 2017. Accessed April 8, 2020 https://www.cdc.gov/nchs/data/nhis/earlyrelease/wireless201705.pdf
- 25. Collins TW., Grineski SE., Chakraborty J., Montgomery MC., Hernandez M. Downscaling environmental justice analysis: determinants of household-level hazardous air pollutant exposure in greater Houston. Ann Assoc Am Geogr. 2015;105(4):684-703. 10.1080/00045608.2015.1050754 [DOI] [Google Scholar]
- 26. Grineski SE., Flores AB., Collins TW., Chakraborty J. Hurricane Harvey and Greater Houston households: comparing pre-event preparedness with post‐event health effects, event exposures, and recovery. Disasters. 2020;44(2):408-432. 10.1111/disa.12368 [DOI] [PubMed] [Google Scholar]
- 27. American Association for Public Opinion Research Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys . 9th ed AAPOR; 2016. [Google Scholar]
- 28. US Census Bureau 2016 American Community Survey 1-year estimates. Accessed February 22, 2019 https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2016/1-year.html
- 29. Kunii O., Nakamura S., Abdur R., Wakai S. The impact on health and risk factors of the diarrhoea epidemics in the 1998 Bangladesh floods. Public Health. 2002;116(2):68-74. 10.1016/S0033-3506(02)00506-1 [DOI] [PubMed] [Google Scholar]
- 30. Rath B., Donato J., Duggan A. et al. Adverse health outcomes after Hurricane Katrina among children and adolescents with chronic conditions. J Health Care Poor Underserved. 2007;18(2):405-417. 10.1353/hpu.2007.0043 [DOI] [PubMed] [Google Scholar]
- 31. Chen AC., Keith VM., Leong KJ. et al. Hurricane Katrina: prior trauma, poverty and health among Vietnamese-American survivors. Int Nurs Rev. 2007;54(4):324-331. 10.1111/j.1466-7657.2007.00597.x [DOI] [PubMed] [Google Scholar]
- 32. US Department of Veterans Affairs. National Center for Posttraumatic Stress Disorder Using the PTSD Checklist (PCL). 2012. Accessed April 8, 2020 https://sph.umd.edu/sites/default/files/files/PTSDChecklistScoring.pdf
- 33. DeSalvo KB., Hyre AD., Ompad DC., Menke A., Tynes LL., Muntner P. Symptoms of posttraumatic stress disorder in a New Orleans workforce following Hurricane Katrina. J Urban Health. 2007;84(2):142-152. 10.1007/s11524-006-9147-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. ArcGIS . Version 10.5.1. Esri; 2018.
- 35. Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons; 2004. [Google Scholar]
- 36. Sterne JA., White IR., Carlin JB. et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. 10.1136/bmj.b2393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Enders CK. Applied Missing Data Analysis. Guilford Press; 2010. [Google Scholar]
- 38. Maldonado A., Collins TW., Grineski SE., Chakraborty J. Exposure to flood hazards in Miami and Houston: are Hispanic immigrants at greater risk than other social groups? Int J Environ Res Public Health. 2016;13(8):775. 10.3390/ijerph13080775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Allison PD. Imputation of categorical variables with PROC MI. Sugi. 2005;30(1):1-14. [Google Scholar]
- 40. Horton NJ., Lipsitz SR., Parzen M. A potential for bias when rounding in multiple imputation. Am Stat. 2003;57(4):229-232. 10.1198/0003130032314 [DOI] [Google Scholar]
- 41. Rodwell L., Lee KJ., Romaniuk H., Carlin JB. Comparison of methods for imputing limited-range variables: a simulation study. BMC Med Res Methodol. 2014;14:57. 10.1186/1471-2288-14-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kaniasty K., Norris FH. Mobilization and deterioration of social support following natural disasters. Curr Dir Psychol Sci. 1995;4(3):94-98. 10.1111/1467-8721.ep10772341 [DOI] [Google Scholar]
- 43. Kaniasty K., Norris FH. In search of altruistic community: patterns of social support mobilization following Hurricane Hugo. Am J Community Psychol. 1995;23(4):447-477. 10.1007/BF02506964 [DOI] [PubMed] [Google Scholar]
- 44. IBM SPSS Statistics for Windows. Release 25. IBM Corp; 2017. [Google Scholar]
- 45. Norris FH, Speier A, Henderson AK, Centers for Disease Control and Prevention (CDC) Assessment of health-related needs after Hurricanes Katrina and Rita, Orleans and Jefferson Parishes, New Orleans area, Louisiana, October 17-22, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(2):38-41. [PubMed] [Google Scholar]
- 46. Rudowitz R., Rowland D., Shartzer A. Health care in New Orleans before and after Hurricane Katrina. Health Aff (Millwood). 2006;25(Suppl 1):W393-W406. 10.1377/hlthaff.25.w393 [DOI] [PubMed] [Google Scholar]
- 47. Madrid PA., Grant R. Meeting mental health needs following a natural disaster: lessons from Hurricane Katrina. Prof Psychol. 2008;39(1):86-92. 10.1037/0735-7028.39.1.86 [DOI] [Google Scholar]
- 48. Shenassa ED., Daskalakis C., Liebhaber A., Braubach M., Brown MJ. Dampness and mold in the home and depression: an examination of mold-related illness and perceived control of one’s home as possible depression pathways. Am J Public Health. 2007;97(10):1893-1899. 10.2105/AJPH.2006.093773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Crago BR., Gray MR., Nelson LA., Davis M., Arnold L., Thrasher JD. Psychological, neuropsychological, and electrocortical effects of mixed mold exposure. Arch Environ Health. 2003;58(8):452-463. 10.3200/AEOH.58.8.452-463 [DOI] [PubMed] [Google Scholar]
- 50. Chen L., Liu A. The incidence of posttraumatic stress disorder after floods: a meta-analysis. Disaster Med Public Health Prep. 2015;9(3):329-333. 10.1017/dmp.2015.17 [DOI] [PubMed] [Google Scholar]
- 51. Lieberman-Cribbin W., Liu B., Schneider S., Schwartz R., Taioli E. Self-reported and FEMA flood exposure assessment after Hurricane Sandy: association with mental health outcomes. PLoS One. 2017;12(1):e0170965. 10.1371/journal.pone.0170965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Crossley TF., Kennedy S. The reliability of self-assessed health status. J Health Econ. 2002;21(4):643-658. 10.1016/S0167-6296(02)00007-3 [DOI] [PubMed] [Google Scholar]
- 53. Sexton K., Linder SH., Marko D., Bethel H., Lupo PJ. Comparative assessment of air pollution–related health risks in Houston. Environ Health Perspect. 2007;115(10):1388-1393. 10.1289/ehp.10043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Linder SH., Marko D., Sexton K. Cumulative cancer risk from air pollution in Houston: disparities in risk burden and social disadvantage. Environ Sci Technol. 2008;42(12):4312-4322. 10.1021/es072042u [DOI] [PubMed] [Google Scholar]
- 55. Bullard RD. Solid waste sites and the black Houston community. Sociol Inq. 1983;53(2-3):273-288. 10.1111/j.1475-682X.1983.tb00037.x [DOI] [PubMed] [Google Scholar]
- 56. Chakraborty J., Collins TW., Grineski SE., Montgomery MC., Hernandez AM. Comparing disproportionate exposure to acute and chronic pollution risks: a case study in Houston, Texas. Risk Anal. 2014;34(11):2005-2020. 10.1111/risa.12224 [DOI] [PubMed] [Google Scholar]
- 57. Emanuel K. Assessing the present and future probability of Hurricane Harvey’s rainfall. Proc Natl Acad Sci U S A. 2017;114(48):12681-12684. 10.1073/pnas.1716222114 [DOI] [PMC free article] [PubMed] [Google Scholar]