Abstract
People experiencing homelessness are at high risk for coronavirus disease 2019 (COVID-19). In March 2020, Boston Health Care for the Homeless Program, in partnership with city and state public health agencies, municipal leaders, and homeless service providers, developed and implemented a citywide COVID-19 care model for this vulnerable population. Components included symptom screening at shelter front doors, expedited testing at pop-up sites, isolation and management venues for symptomatic people under investigation and for people with confirmed disease, quarantine venues for asymptomatic exposed people, and contact investigation and tracing. Real-time disease surveillance efforts in a large shelter outbreak of COVID-19 during the third week of operations illustrated the need for several adaptations to the care model to better respond to the local epidemiology of illness among people experiencing homelessness. Symptom screening was de-emphasized given the high number of asymptomatic or minimally symptomatic infections discovered during mass testing; contact tracing and quarantining were phased out under the assumption of universal exposure among the sheltered population; and isolation and management venues were rapidly expanded to accommodate a surge in people with newly diagnosed COVID-19. During the first 6 weeks of operation, 429 of 1297 (33.1%) tested people were positive for COVID-19; of these, 395 people were experiencing homelessness at the time of testing, representing about 10% of the homeless adult population in Boston. Universal testing, as resources permit, is a focal point of ongoing efforts to mitigate the effect of COVID-19 on this vulnerable group of people.
Keywords: homelessness, COVID-19, emerging infectious diseases, public health practice, community health
On any given day, about 568 000 people are homeless in the United States.1 The high transmissibility of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, coupled with its variable and often subtle clinical presentation, makes homeless shelters and encampments especially susceptible to large outbreaks of coronavirus disease 2019 (COVID-19) among people with an already high likelihood of chronic heart2 and lung3 disease and accelerated aging.4 Early reports demonstrate the potential for widespread infection in this vulnerable population.5-7
Before the first known case of COVID-19 was identified in a homeless person, Boston Health Care for the Homeless Program (BHCHP)—a nonprofit, federally qualified health center serving more than 11 000 currently and formerly homeless people annually8—partnered with city and state public health agencies, municipal leaders, and homeless service providers to proactively develop a comprehensive response model for homeless and marginally housed people in Boston. In this case study, we describe the initial model of care, as well as adaptations, early outcomes, and lessons learned during the first 6 weeks of deploying this model.
Methods
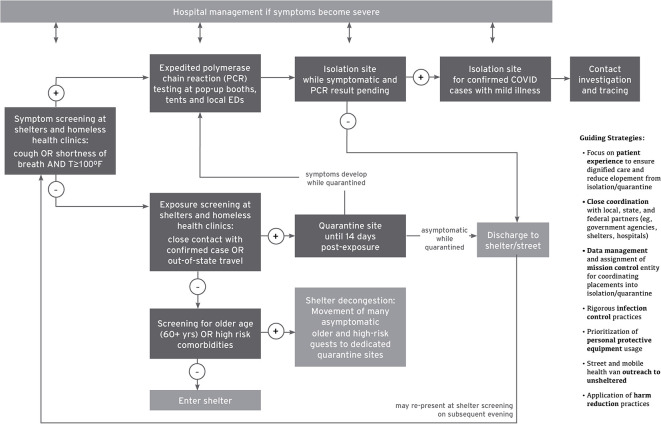
The initial COVID-19 care model (Figure 1) consisted of multiple interrelated components deployed across various venues, many of which were newly constructed or repurposed for COVID care (Table).
Figure 1.
COVID-19 response model for people experiencing homelessness in Boston, 2020. Abbreviations: COVID-19, coronavirus disease 2019; ED, emergency department; T, temperature.
Table.
Components of the original and adapted COVID-19 response model for people experiencing homelessness in Boston, 2020
| Venue Type | Original Model (first 3 weeks) | Adapted Model (week 4 and later) |
|---|---|---|
| Pop-up COVID-19 testing sites |
|
Format, staffing, and PPE unchanged |
| Isolation site for symptomatic people while COVID-19 test is pending |
|
|
| Isolation sites for management of people with confirmed COVID-19 | Site 1:
|
|
Site 2:
|
||
Site 3:
|
||
Site 4:
|
||
| Quarantine site for COVID-exposed people without symptoms |
|
|
Abbreviations: COVID-19, coronavirus disease 2019; PPE, personal protective equipment.
aData source: Boston Health Care for the Homeless Program.
Front-Door Symptom Screening
Staff members at local shelters and BHCHP clinical sites implemented front-door screening for cough or shortness of breath. If shelter guests reported either symptom, then clinical personnel measured their body temperature and triaged people with readings ≥100°F for expedited SARS-CoV-2 polymerase chain reaction (PCR) testing at local emergency departments or pop-up testing sites in areas of high homeless service density (Figure 2). For the pop-up sites, the Massachusetts Department of Public Health provided testing supplies and processed all specimens in the state public health laboratory.
Figure 2.

Pop-up booth for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) testing in Boston, Massachusetts. Photo taken March 20, 2020.
Isolation and Management Venues
To prevent viral spread while awaiting PCR results, BHCHP partnered with the City of Boston and a local construction company to rapidly build 2 tents: 1 tent for isolation of symptomatic patients with suspected COVID-19 and 1 tent for quarantine of COVID-exposed asymptomatic people. These tents, which were deployed in <1 week from conception to implementation, incorporated rigorous infection control elements. For the isolation tent, the guiding principle was that patients awaiting test results should not mix. Heavy vinyl panels partitioned the tent into 16 pods measuring approximately 52 sq ft (Figure 3), each with dedicated equipment for measuring vital signs and a portable toilet outside. The isolation tent incorporated negative pressure airflow, and staff members wore full personal protective equipment (PPE) consisting of an N95 respirator, face shield, gown, and gloves. Surface decontamination occurred at least every 4 hours. Patients with positive PCR test results were either hospitalized or transferred to a 17-bed homeless-specific COVID-19 care unit in a partitioned-off wing of BHCHP’s 104-bed medical respite program. More beds were eventually added to this inventory.
Figure 3.
Isolation tent pods for people with pending severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) tests in Boston, Massachusetts. Photo taken March 21, 2020.
Exposure Screening, Contact Tracing, and Quarantine
The second tent (Figure 4) was intended for quarantine of people who were asymptomatic but had been exposed to COVID-19, ascertained by 2 methods. First, shelter and clinic staff members deployed front-door exposure screening along with the symptom screening described previously to identify people reporting either (1) contact with someone known to have COVID-19 or (2) travel outside the state within the past 14 days. Second, BHCHP personnel conducted contact investigations of homeless people in Boston with confirmed COVID-19, and these contact investigations helped to identify people who may not have been aware of their exposure. Exposed people remained in the quarantine tent for 14 days after the estimated date of exposure. The quarantine tent had the same structure and layout as the isolation tent, but quarantine tent staff members used a lower level of PPE consisting of a surgical mask and gloves. People in the quarantine tent who developed symptoms were tested and isolated according to the algorithm previously described.
Figure 4.
Quarantine tent for asymptomatic people with coronavirus disease 2019 (COVID-19) exposure in Boston, Massachusetts. The tent was later repurposed for isolation of symptomatic people with pending severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) tests. Photo taken April 19, 2020.
Shelter-Based Infection Control
Concurrent efforts deployed by area shelters included emphasis on disinfection (eg, frequent cleaning, supporting hand and respiratory hygiene, ensuring adequate ventilation); environmental controls (eg, bed distancing, staggered showering schedules, staggered meals); and administrative controls (eg, ensuring clearly communicated sick-leave policies for staff members, reducing unnecessary assembly of staff members and guests). Ultimately, many shelters used a decongestion strategy to relocate people at highest risk for COVID-19 complications to vacated university dormitories.
Real-Time Surveillance
From the outset, BHCHP developed a COVID-19 surveillance strategy that incorporated data from multiple sources. BHCHP’s preexisting electronic health record spanning all clinical sites proved useful for tracking patients across various components of its COVID care model. BHCHP leadership established lines of communication with area hospitals to identify homeless people with COVID-19 or COVID-like illness in need of alternate care arrangements or post-discharge follow-up. Data analysts in the BHCHP Institute for Research, Quality, and Policy in Homeless Health Care cross-checked COVID-19 cases identified through testing at BHCHP or area hospitals with the Boston Homeless Management Information System, enabling a determination of the timing and location of recent shelter stays and the identification of shelters with rapid upticks in infections or high levels of sustained disease activity. A case tracking database served as a centralized repository of all known SARS-CoV-2 tests and results among people experiencing homelessness in Boston, allowing a real-time assessment of the scale and trajectory of COVID-19 in this population.
Command Structure and Organizational Dynamics
BHCHP established a command center early in the response to oversee the multiple components described previously. The command center was composed of senior leaders at BHCHP who met daily to design and implement programming specific to the crisis, enabling a centralized approach to decision-making and rapid deployment of resources when and where needed. In addition, a mission control team consisting of BHCHP nurses and case managers handled incoming patient referrals for isolation and quarantine, coordinated daily admissions to various care sites based on staffing and bed availability, facilitated transportation of patients from one venue to another, and coordinated care and discharge planning with area health care facilities for patients with confirmed or suspected COVID-19.
Staffing needs related to the COVID-19 response, combined with a general de-emphasis of in-person nonurgent aspects of health care (eg, routine health maintenance visits), required major shifts in other aspects of BHCHP operations. Under typical circumstances, BHCHP operates more than 40 clinics at shelters, day programs, and other community venues throughout greater Boston. Many of these clinic sites temporarily halted or cut back services to deploy staff members and resources for the COVID response. Where possible, clinics shifted to a telehealth approach for delivering medical, psychiatric, and addiction-oriented care that did not require in-person evaluation. The shift to telehealth was facilitated by regulatory waivers allowing reimbursement for such services from Medicaid and other payers. Early in the pandemic, BHCHP shifted nonclinical employees to remote work arrangements and limited meeting sizes in its facilities. As the situation evolved, many staff members were redeployed in other capacities to support COVID-related operations.
Transparent communication was emphasized early on. BHCHP leadership delivered daily organization-wide updates via online meeting platforms to ensure that all employees were informed of the latest developments. Dialogue was encouraged, and areas of uncertainty were openly discussed. These sessions also served to build and sustain community, foster a shared sense of purpose, and provide emotional support to staff members who were grappling with the uncertain and frightening realities of a rapidly evolving pandemic.
Outcomes
BHCHP and its community partners deployed the COVID-19 care model on March 12, 2020. In the first 2 weeks of operation, 118 homeless and marginally housed people underwent PCR testing for SARS-CoV-2. Of these, 8 (6.8%) were positive.
In the third week of the response, disease surveillance activities led to the identification of an emerging cluster of 22 people with COVID-19 at a single large shelter in Boston. This finding prompted universal PCR testing of 408 remaining shelter residents during a 2-day span that uncovered a 36% prevalence of SARS-CoV-2 infection, as described elsewhere.7 Most (88%) infected people identified through this universal testing reported no symptoms, and none had a positive symptom screen according to the algorithm previously described.
Overall, 1297 people underwent PCR testing for SARS-CoV-2 during the first 6 weeks of operations, of whom 429 (33.1%) had a positive test result (Figure 5). From March 20 to April 18, a total of 395 adults experiencing homelessness were diagnosed with COVID-19.
Figure 5.
Cumulative counts of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) polymerase chain reaction tests and positive results among homeless and marginally housed adults in Boston, March 12–April 18, 2020. The total number of tests (n = 1462) exceeds the number of unique people tested (n = 1297) because some people were tested more than once.
These surveillance efforts informed the need for several adaptations to the response model and COVID-specific care venues (Table):
De-emphasis on symptom screening: Symptom screening at community sites continued when possible to identify people meriting expedited testing; however, it was undertaken with an understanding of its limited sensitivity for identifying subclinical disease and was deprioritized in the overall care model to direct resources and efforts elsewhere. In its place, as of May 2020, mass PCR testing was being pursued at selected shelters with higher levels of confirmed COVID-19 activity and at other sites when resources permit.
Cessation of exposure screening and quarantining: Given the high prevalence of SARS-CoV-2 infection discovered during the shelter outbreak, BHCHP shifted from COVID-19 exposure screening to operating under the assumption of “universal exposure.” This shift obviated the need for quarantining exposed people and allowed the quarantine tent to be used as another isolation venue for symptomatic people awaiting PCR results.
Reduction of contact tracing efforts: As the number of new COVID-19 cases among homeless people rapidly increased, BHCHP scaled back its contact tracing efforts, again based on the assumption of universal exposure across large congregate living environments. This shift freed up considerable personnel time to focus on other aspects of the response.
Expansion of care sites: The surge in COVID-19 cases identified during the shelter outbreak required an immediate expansion of isolation and management sites, particularly for people with minimal or no symptoms who did not require hospitalization but were not allowed to stay in a shelter. In response, the original 17-bed COVID-19 care unit at BHCHP’s medical respite facility was quickly expanded to 52 beds. Simultaneously, dozens more beds became available in reopened segments of previously shuttered health care facilities, and funding from the city and state enabled the rapid construction of a field hospital inside the Boston Convention and Exhibition Center containing 500 additional beds for homeless and marginally housed people with COVID-19 (Figures 6 -8).
Figure 6.
Boston Hope field hospital for coronavirus disease 2019 (COVID-19)–positive people experiencing homelessness in Boston, Massachusetts. Photo taken April 10, 2020.
Figure 7.
Patient care corridor in Boston Hope field hospital for coronavirus disease 2019 (COVID-19)–positive people experiencing homelessness in Boston, Massachusetts. Photo taken April 9, 2020.
Figure 8.
Patient pods in Boston Hope field hospital for coronavirus disease 2019 (COVID-19)–positive people experiencing homelessness in Boston, Massachusetts. Photo taken April 10, 2020.
Lessons Learned
Our disease surveillance activities suggested that about 10% of Boston’s estimated homeless adult population contracted COVID-19 during a 4-week period.1 Private space to quarantine or recover from such an illness is a privilege not currently afforded to all. A community health center for people experiencing homelessness, working in close partnership with municipal leaders, public health agencies, and homeless service providers, rapidly deployed a COVID-19 care model that has reached a substantial number of people in the target population. This experience highlights a number of important lessons:
Homeless-tailored health centers are well-poised to serve as key agencies in collaborative municipal responses to COVID-19 among people experiencing homelessness.
Disease surveillance efforts deployed in parallel with clinical programming can play a crucial role in guiding community-based response efforts.
Given the fluidity of the COVID-19 pandemic, maintaining flexibility in the usage and staffing of various elements of the care model—while still adhering to the core principles of the response effort—is vital.
The high number of asymptomatic SARS-CoV-2 infections and the potential for rapid spread in congregate settings support the need for proactive, universal COVID-19 testing strategies in this population.
Widespread COVID-19 testing efforts in this population must be paired with sufficient spaces for isolation and management of newly discovered cases.
No illness more clearly illustrates the immense health risks of homelessness than COVID-19. Efforts to reduce widespread homelessness in the United States should remain a cornerstone of public health.
Acknowledgments
The authors thank Nora Sporn, MA, MPH, for her assistance with data compilation.
Footnotes
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Baggett receives royalties from UpToDate for authorship of a topic review on homeless health care.
Funding: The authors received no financial support with respect to the research, authorship, and/or publication of this article.
ORCID iD
Travis P. Baggett https://orcid.org/0000-0002-7032-2625
References
- 1. US Department of Housing and Urban Development 2019 AHAR: part 1—PIT estimates of homelessness in the U.S. Published 2020. Accessed April 4, 2020 https://www.hudexchange.info/resource/5948/2019-ahar-part-1-pit-estimates-of-homelessness-in-the-us
- 2. Baggett TP., Liauw SS., Hwang SW. Cardiovascular disease and homelessness. J Am Coll Cardiol. 2018;71(22):2585-2597. 10.1016/j.jacc.2018.02.077 [DOI] [PubMed] [Google Scholar]
- 3. Snyder LD., Eisner MD. Obstructive lung disease among the urban homeless. Chest. 2004;125(5):1719-1725. 10.1378/chest.125.5.1719 [DOI] [PubMed] [Google Scholar]
- 4. Brown RT., Hemati K., Riley ED. et al. Geriatric conditions in a population-based sample of older homeless adults. Gerontologist. 2017;57:757-766. 10.1093/geront/gnw011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mosites E., Parker EM., Clarke KEN. et al. Assessment of SARS-CoV-2 infection prevalence in homeless shelters—four U.S. cities, March 27-April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):521-522. 10.15585/mmwr.mm6917e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tobolowsky FA., Gonzales E., Self JL. et al. COVID-19 outbreak among three affiliated homeless service sites—King County, Washington, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):523-526. 10.15585/mmwr.mm6917e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baggett TP., Keyes H., Sporn N., Gaeta JM. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. Published online April 27, 2020. 10.1001/jama.2020.6887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. O’Connell JJ., Oppenheimer SC., Judge CM. et al. The Boston Health Care for the Homeless Program: a public health framework. Am J Public Health. 2010;100(8):1400-1408. 10.2105/AJPH.2009.173609 [DOI] [PMC free article] [PubMed] [Google Scholar]