Abstract
Study Design:
A systematic review and meta-analysis.
Objectives:
The results from previous meta-analyses are limited by the small number of included studies. Moreover, the risk factors of heterotopic ossification (HO) have not been well studied. Therefore, this study aims to estimate the prevalence of HO after cervical total disc replacement (CTDR) at different follow-up time points and explore potential risk factors for HO.
Methods:
We searched databases to identify eligible studies that reported the rate of HO after CTDR. The pooled prevalence of HO, according to different grades of HO, length of follow-up and types of prosthesis, and 95% confidence intervals (CIs) were calculated. Multivariable meta-regression analyses were performed to identify factors that may contribute to the heterogeneity between estimates.
Results:
Of the 94 studies included, 82 studies reported an overall rate of HO, encompassing a total of 5861 cervical spinal levels that underwent CTDR. The overall pooled prevalence of HO was 32.5% (95% CI 26.7% to 38.4%). Single-level CTDR was associated with a higher overall rate of HO. When the rate of HO was stratified by McAfee/Mehren classification, the pooled prevalence of range of motion (ROM)–limiting HO was 11.0% (95% CI 9.2% to 12.8%). Latest publication, single-level CTDR, longer follow-up period, and studies published outside were associated with a higher rate of ROM-limiting HO.
Conclusions:
We provide a comprehensive overview of the prevalence of different grades of HO. This meta-analysis also identifies and rules out some risk factors for HO after CTDR.
Keywords: cervical total disc replacement, heterotopic ossification, risk factors, prevalence
Introduction
Anterior cervical discectomy and fusion (ACDF) is the gold-standard surgical treatment for cervical degenerative disc disease.1 One of the main complications of ACDF is the development of adjacent segment degeneration (ASD) and adjacent segment disease, which occurs when fusion of cervical spinal segments limits their range of motion (ROM) and increases intradiscal pressure of the adjacent intervertebral discs.2 One alternative procedure is cervical total disc replacement (CTDR), theoretically preserving the ROM of spinal segments and minimize the risk of ASD.
Nonetheless, heterotopic ossification (HO) has been reported as a complication of CTDR. HO is defined as the formation of bone tissue outside the skeletal system.3 Certain surgeries or trauma such as total hip replacement and spinal cord injury can also be complicated by HO.3 HO can be graded from 0 to IV by McAfee classification,4 which was further modified by Mehren et al.5 The severity of HO is graded based on the ROM of spinal segments and the degree of heterotopic bone invasion around the disc space. Although grade III and grade IV HO (ROM-limiting HO) reduce the ROM of surgical spinal segments, a recent meta-analysis of CTDR has not found any significant association between HO and clinical outcomes of patients.6
There is a need to estimate the prevalence of HO after CTDR. The period from CTDR to the development of HO indicates the longevity of the implanted prosthesis, which will aid clinicians’ and patients’ decision making. The prevalence of HO varies greatly among studies, ranging from 0% over a minimum of 5-year follow-up7 to 100% over 2-year follow-up.8 Although 2 meta-analyses, published in 20 129 and 2017,10 have explored the pooled prevalence of HO after CTDR, these 2 studies included only a small number of clinical trials, hindering an accurate estimate of the prevalence of HO. Furthermore, risk factors associated with the development of HO have not been well investigated in these meta-analyses.
Hence, the present systematic review and meta-analysis attempts to investigate the following research questions: (1) the pooled prevalence of HO after CTDR, (2) the pooled prevalence of HO based on different follow-up time points and types of prosthesis, and (3) the associations of demographic and surgical factors with the rate of HO.
Methods
Study Selection
A systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis protocols (PRISMA-P) guideline and the guidelines for academic neurosurgeons.11-13 We used the following medical subject headings (MeSH) and text words that were related to CTDR and HO: “heterotopic ossification,” “heterotopic bone,” “cervical,” “arthroplasty,” “total disc/disk replacement,” “artificial disc/disk replacement,” and “disc/disk prosthesis.” Literature published up to April 2018 in MEDLINE (OVID interface, 1948 onward), Embase (OVID interface, 1980 onward), the Cochrane Central Register of Controlled Trials (Wiley Interface, current issue), and PubMed databases were searched. Reference lists of all publications found in the initial literature search were manually reviewed for potential studies.
Two reviewers removed duplications and performed screening of title and abstract of articles. After screening, full-text articles would be assessed for compatibility with the inclusion and exclusion criteria. If more than 1 published article involved the same study population, the latest articles with the most comprehensive data was included in this meta-analysis. Any disagreement between the reviewers would first be resolved by discussion. If a consensus could not be reached, a senior author would be consulted.
The inclusion criteria were:
Clinical studies of CTDR reporting HO rates at the operative segment
Cervical disc degeneration disease or disc herniation as the surgical indication
Studies that included subjects aged ≥18 years
No limit placed on the number of radiologists/spine surgeons who diagnosed HO, or the type of prosthesis
The exclusion criteria were:
Subjects with bone diseases (such as osteoporosis or metabolic bone disease), malignancy, or systemic infection
Literature reviews, preclinical studies, case reports, cadaver tests, or editorials
Non-English or nonprospective studies
Absence of data on HO rates
TDR in the lumbar spine
Duplicated publications
Average or minimal follow-up shorter than 1 year
Rates of HO expressed in number of patients
Data Extraction
After screening and excluding ineligible articles, reviewers extracted the following data: year of publication, first author, study design, sample size, study location, age, type of prosthesis, spinal level of surgical segment, surgical indication, follow-up duration, and rates of HO.
Assessment of Methodological Quality
With regard to randomized controlled trials (RCTs), methodological quality was assessed in accordance with the guideline published by the Cochrane Back and Neck Group in the Cochrane Handbook for Systematic Review of Interventions.14 Item 11, which assesses compliance of intervention, was removed because CTDR is a single-session intervention. The Methodological Index for Non-Randomized Studies (MINORS) was used to assess the methodological quality of nonrandomized trials.15
Assessment of Publication Bias
Publication bias was assessed by funnel plot, Begg and Mazumdar rank correlation test and Egger’s regression test.
Statistical Analysis
Statistical analysis was conducted with Open Meta-Analyst and R, version 3.5.0 (“metafor” package 2.0-0). Results were considered statistically significant if P value was <.05.
Heterogeneity of included studies was calculated by I2 statistic and Q tests. The random-effects model was used to estimate the pooled prevalence of HO if I2 was larger than 50% or if P < .10. Otherwise, the fixed-effects model was used. Subgroup analysis was further conducted, according to grades of HO, length of follow-up and types of prosthesis.
Random-effects, multivariable, meta-regression analysis was conducted to identify the effect of the following demographic and surgical variables on rates of HO: year of publication, age, gender, length of follow-up, study design, study location, level of operation, and spinal level of surgical segment. Subgroup analysis was performed based on different grades of HO.
Results
Study Selection
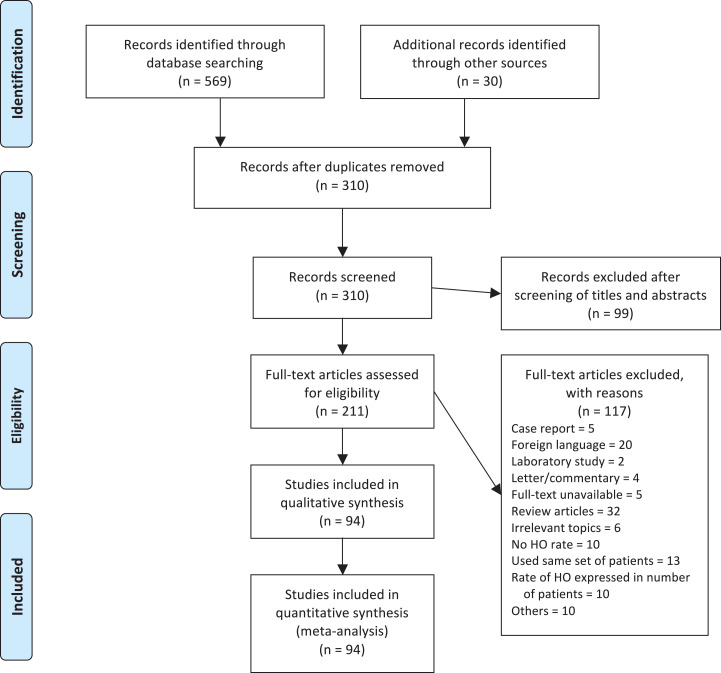
A total of 599 studies were identified, in which 569 studies were identified by searching in the databases, 28 studies from reference lists of the included studies and 2 from the US Food and Drug Administration clinical trial database. Removal of duplications and screening of titles and abstracts yielded 211 full-text articles to be examined for eligibility. A total of 94 studies were eligible for quantitative and qualitative analyses (Figure 1). Of all the studies included, 82 studies reported on the overall rate of HO, 59 on grade I, 60 on grade II HO, 70 on grade III HO, 76 on grade IV HO, and 75 on ROM-limiting HO.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) 2009 flow diagram.
Study Demographics
The average age of patients at the time of receiving CTDR was 44.6 years. More males (53.2%) on average received CTDR than females. The majority of patients received single-level CTDR (71.8%), followed by 2-level CTDR (18.6%). The most commonly operated spinal segments were C5C6 (52.6%), followed by C6C7 (23.2%) and C4C5 (16.5%). Other demographic, pre-operative and peri-operative variables were not well reported by the included studies. Mean operative time and hospitalization were 109 minutes and 3.8 days, respectively.
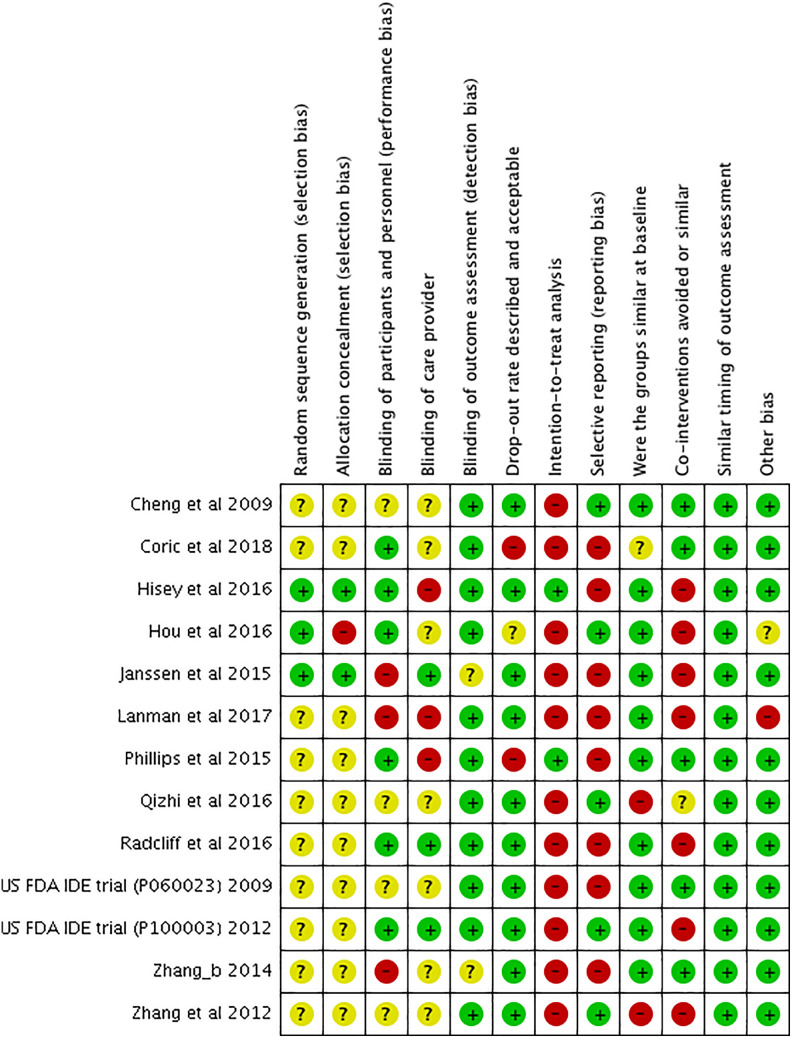
Methodological Quality
Figure 2 summarizes the risk of bias of 13 RCTs, which was assessed in accordance with Cochrane Back and Neck Group guidelines.14 The included RCTs demonstrated a low risk of bias in the majority of the criteria, except that there was potential reporting bias and a lack of intention-to-treat analysis across most included studies. Details of randomization methods were also absent in most studies.
Figure 2.
Risk of bias summary table. “?”: unclear risk of bias; “+”: low risk of bias; “−”: high risk of bias.
The methodological quality of non-RCT studies was assessed by MINORS.15 The means scores for noncomparative and comparative studies were 9.7 (out of 16) and 16.3 (out of 24), respectively.
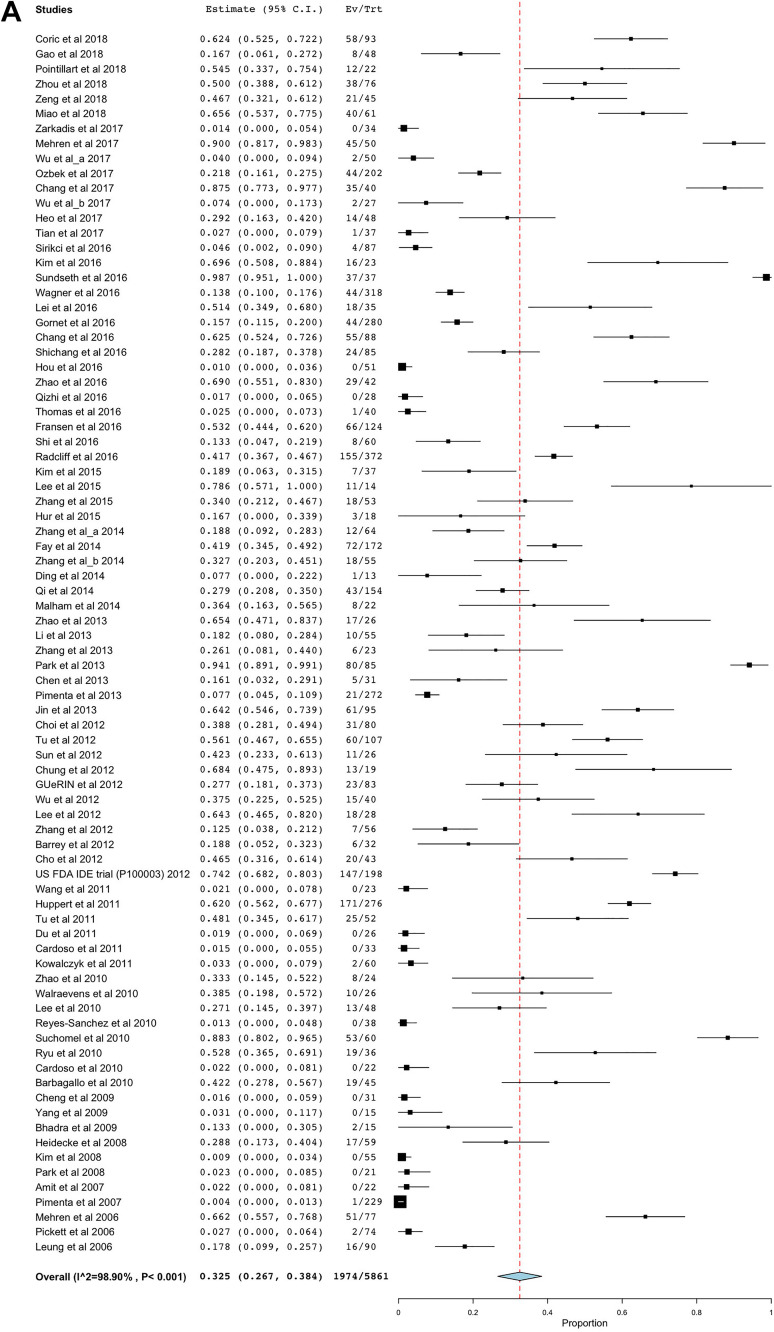
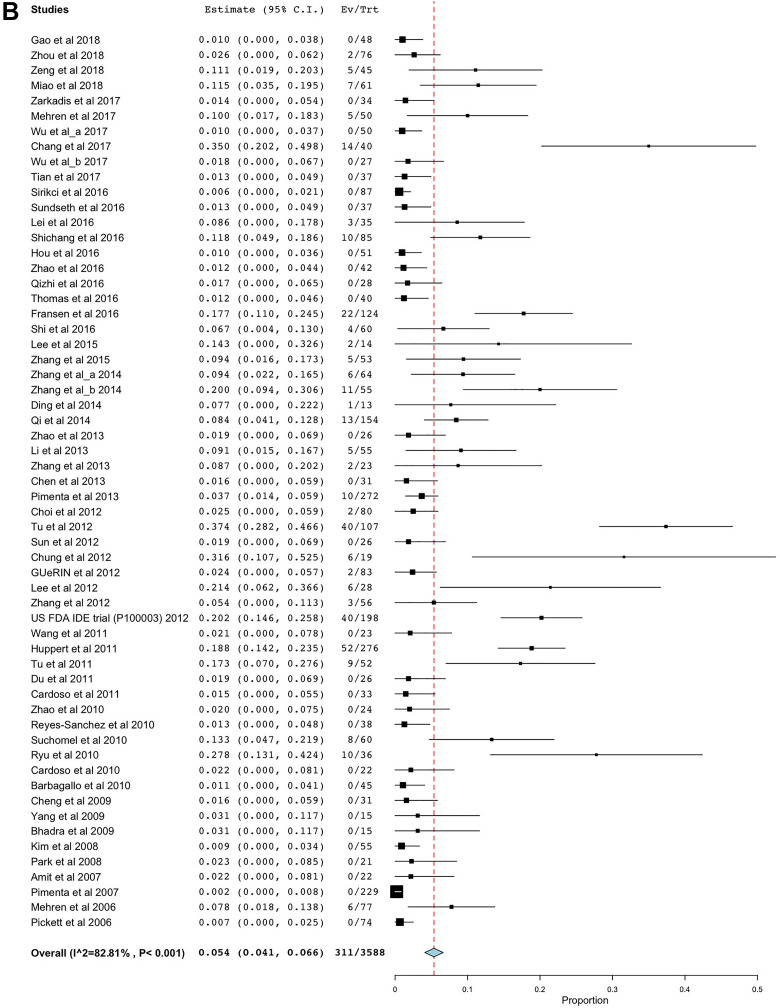
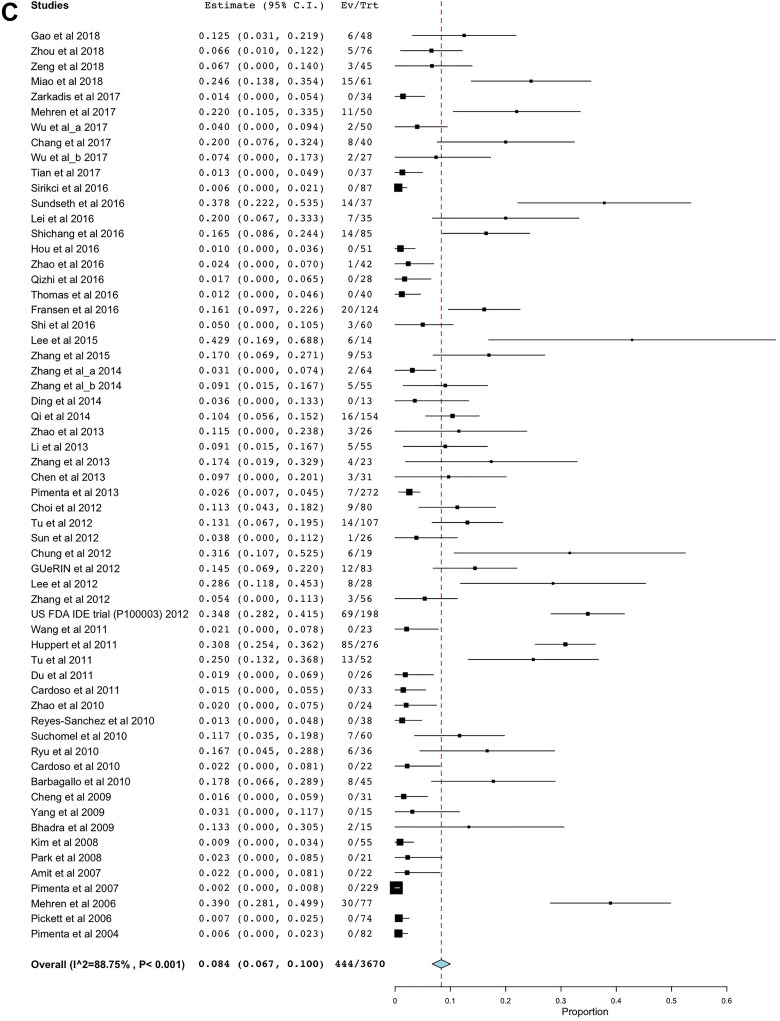
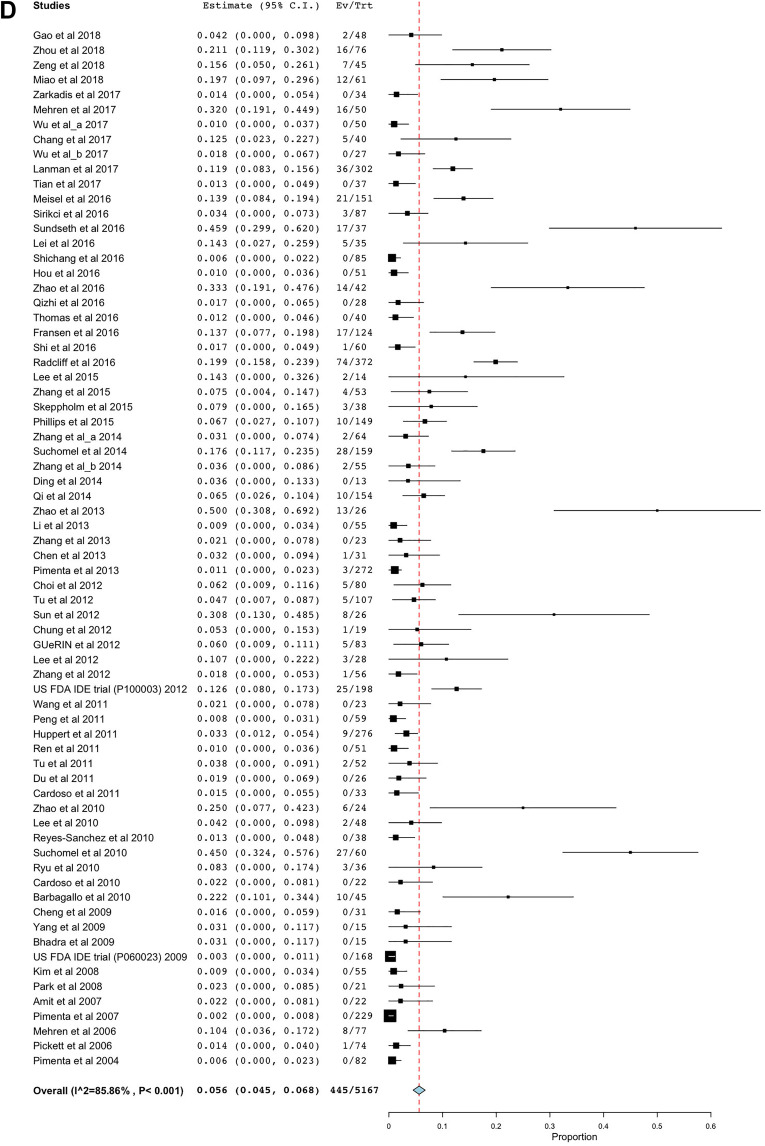
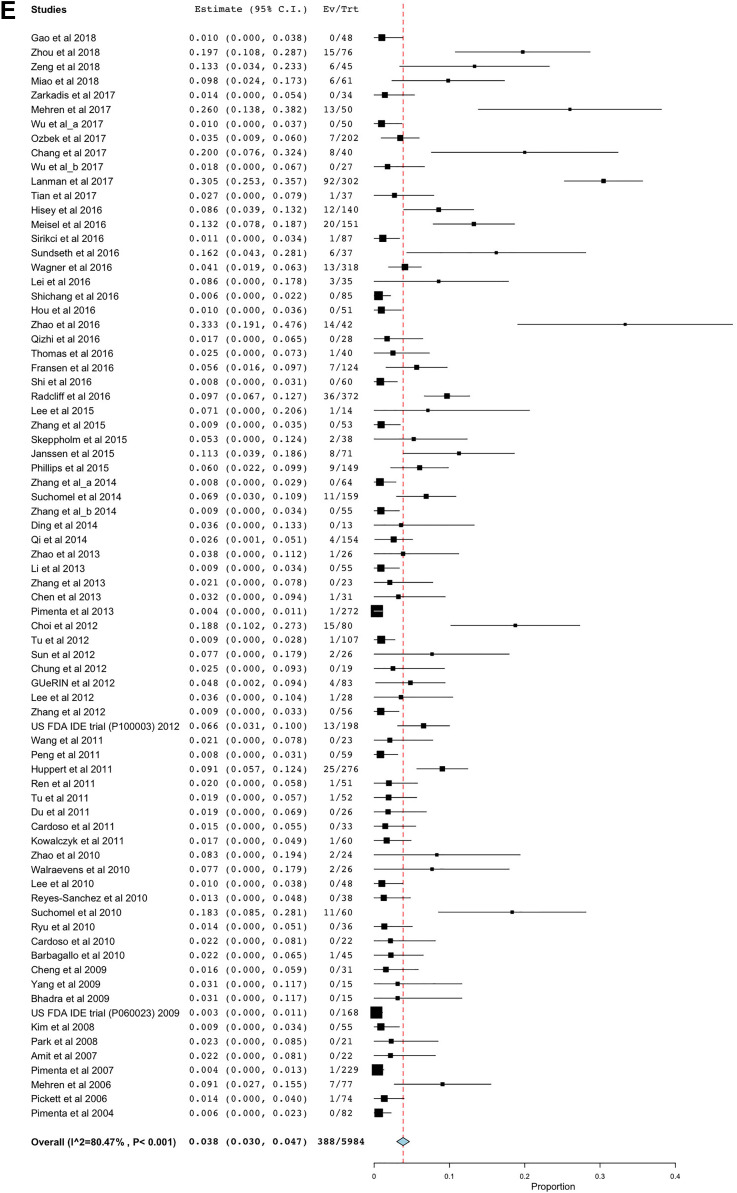
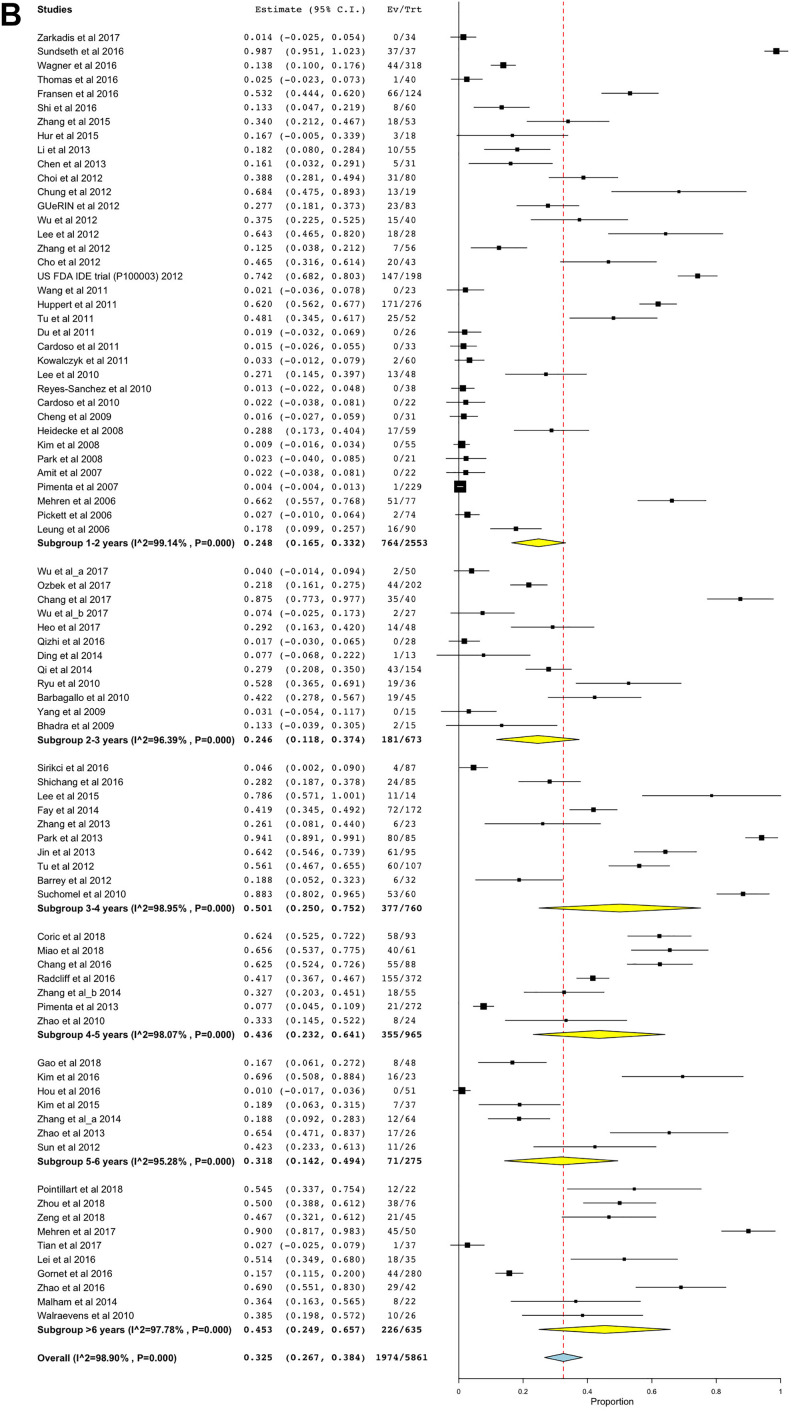
Overall HO
A total of 82 articles reported an overall rate of HO, composed of 5861 cervical spinal levels that underwent CTDR. The pooled prevalence of overall HO was 32.5% (95% confidence interval [CI] 26.7% to 38.4%; Figure 3A). Figure 3B-E shows the overall prevalence of grade I to grade IV HO. The pooled prevalence of grade I (pooled HO rate 5.4%, 95% CI 4.1% to 6.6%) and IV HO (pooled HO rate 3.8%, 95% CI 3.0% to 4.7%) was significantly lower than that of grade II HO (pooled HO rate 8.4%, 95% CI 6.7% to 10.0%).
Figure 3.
(A) The overall rate of heterotopic ossification (HO). (B) The rate of grade I HO. (C) The rate of grade II HO. (D) The rate of grade III HO. (E) The rate of grade IV HO.
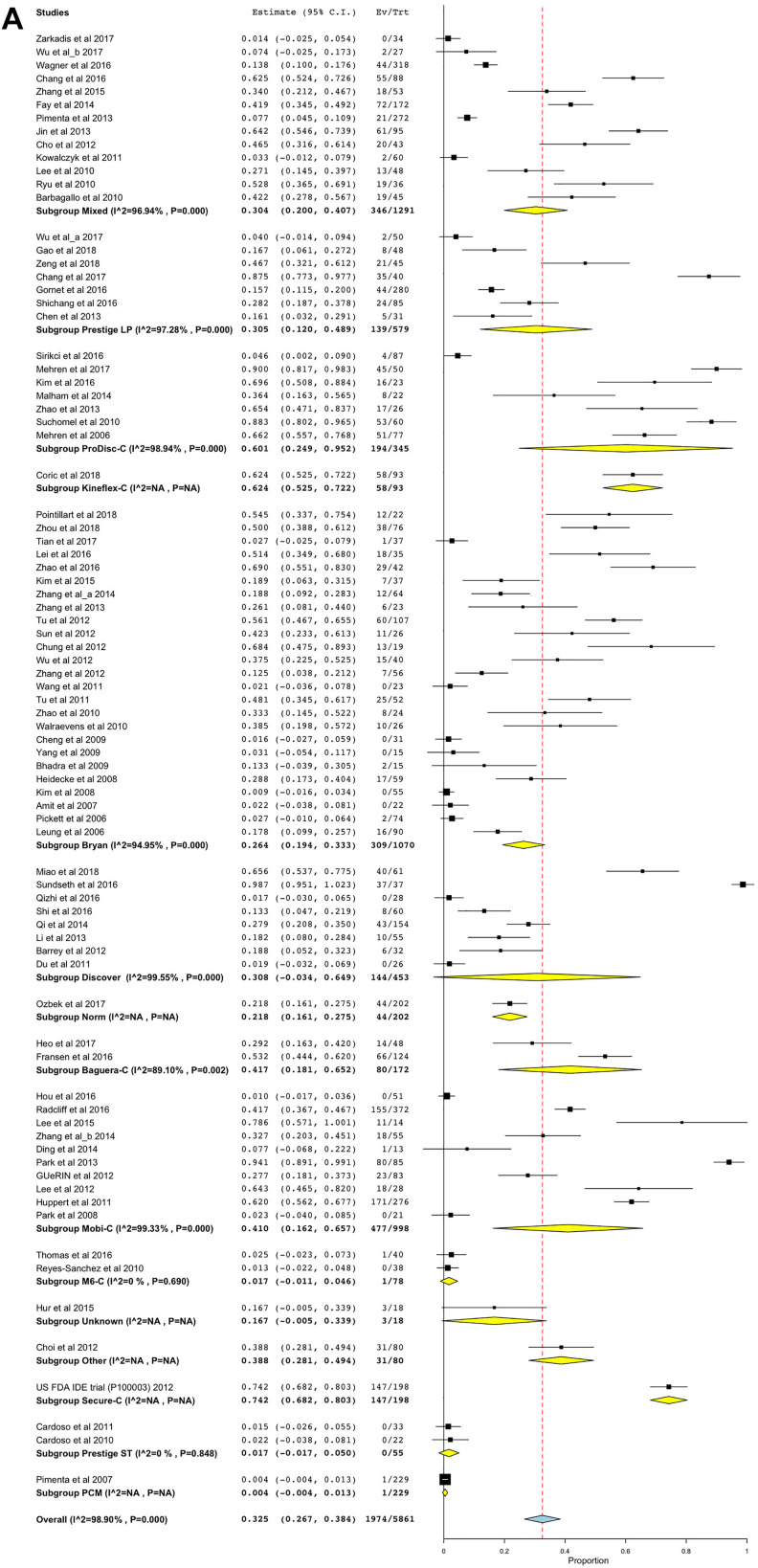
Subgroup analyses were conducted based on the types of prosthesis and the duration of follow-up. Kineflex-C (pooled HO rate 62.4%, 95% CI 52.5% to 72.2%) and Secure-C (pooled HO rate 74.2%, 95% CI 68.2% to 80.3%) prostheses demonstrated higher overall rates of HO, relative to the overall prevalence of HO (Figure 4A). In contrast, M6-C (pooled HO rate 1.7%, 95% CI 0% to 4.6%), Prestige ST (pooled HO rate 1.7%, 95% CI 0% to 5.0%), and PCM (pooled HO rate 0.4%, 95% CI 0% to 1.3%) exhibited lower rates of HO following CTDR than the overall prevalence of HO.
Figure 4.
(A) The overall rate of heterotopic ossification (HO) stratified by the types of prosthesis. (B) The overall rate of HO stratified by the length of follow-up.
When stratified according to the duration of follow-up, the overall prevalence of HO following CTDR was 24.8% (95% CI 16.5% to 33.2%) and 45.3% (95% CI 24.9% to 65.7%) in 1 to 2 years and >6 years follow-up subgroups, respectively (Figure 4B). The overall prevalence of HO was comparable across subgroups. There was a tendency for the overall HO rate to increase as the length of follow-up period increased.
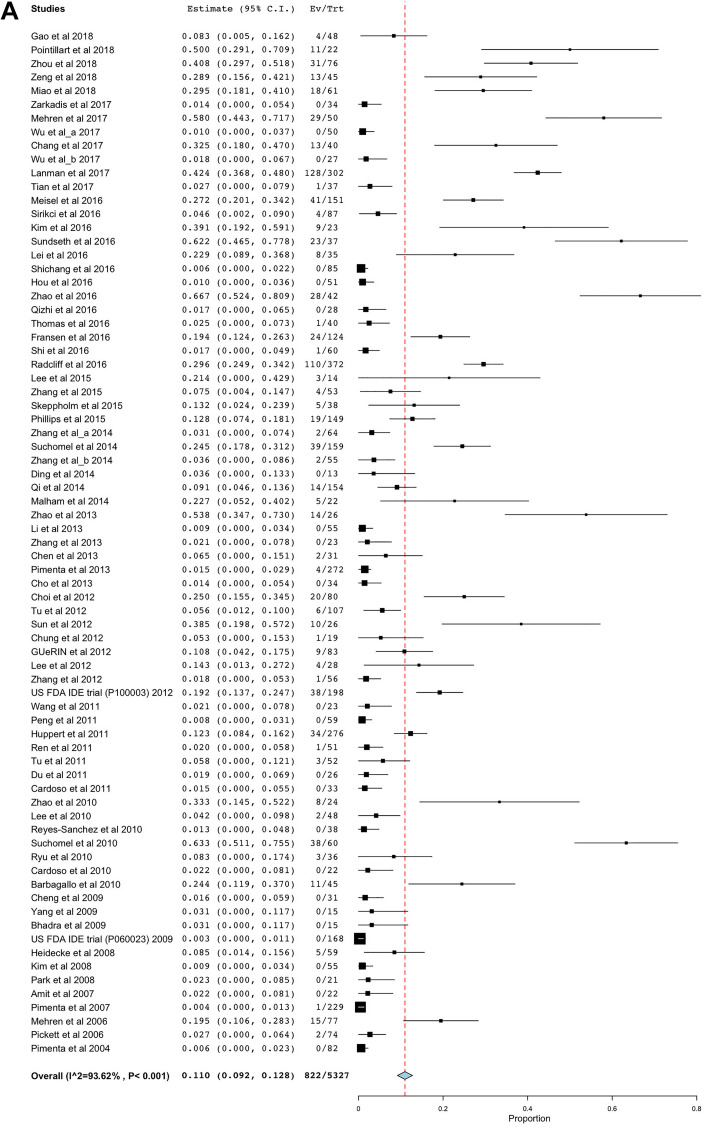
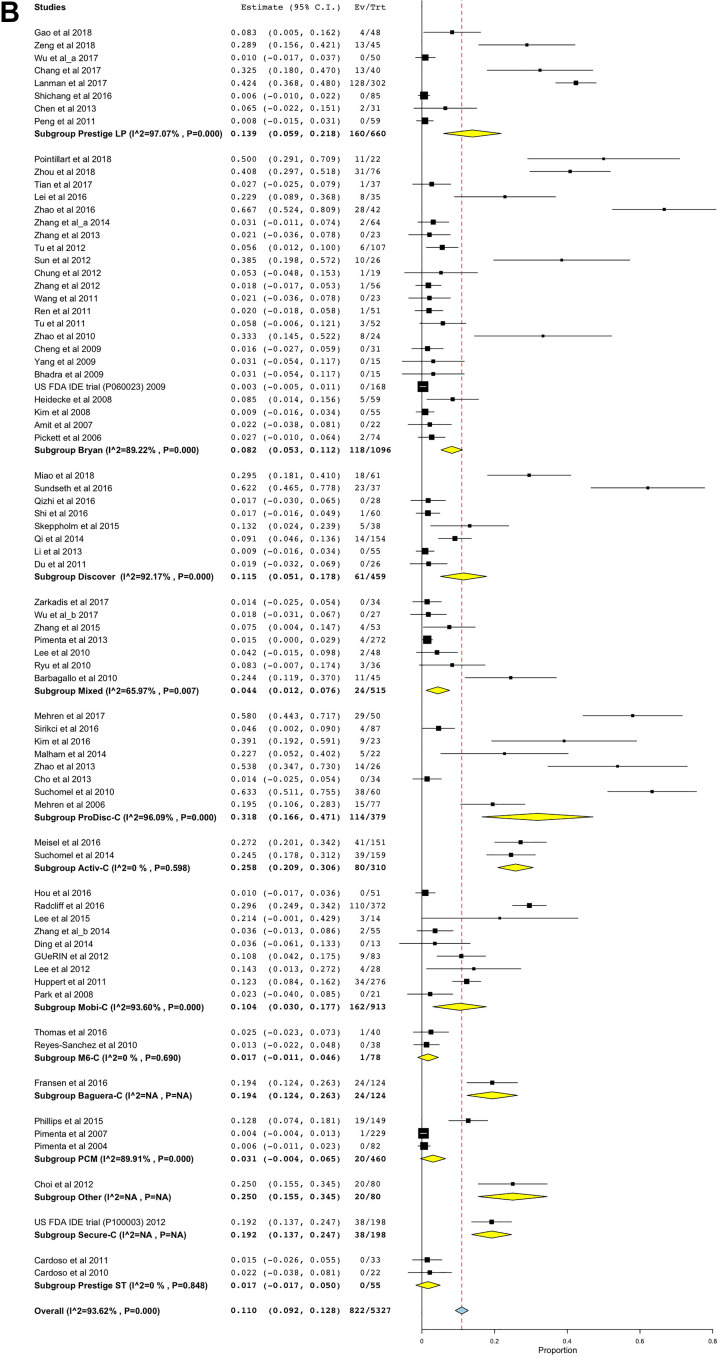
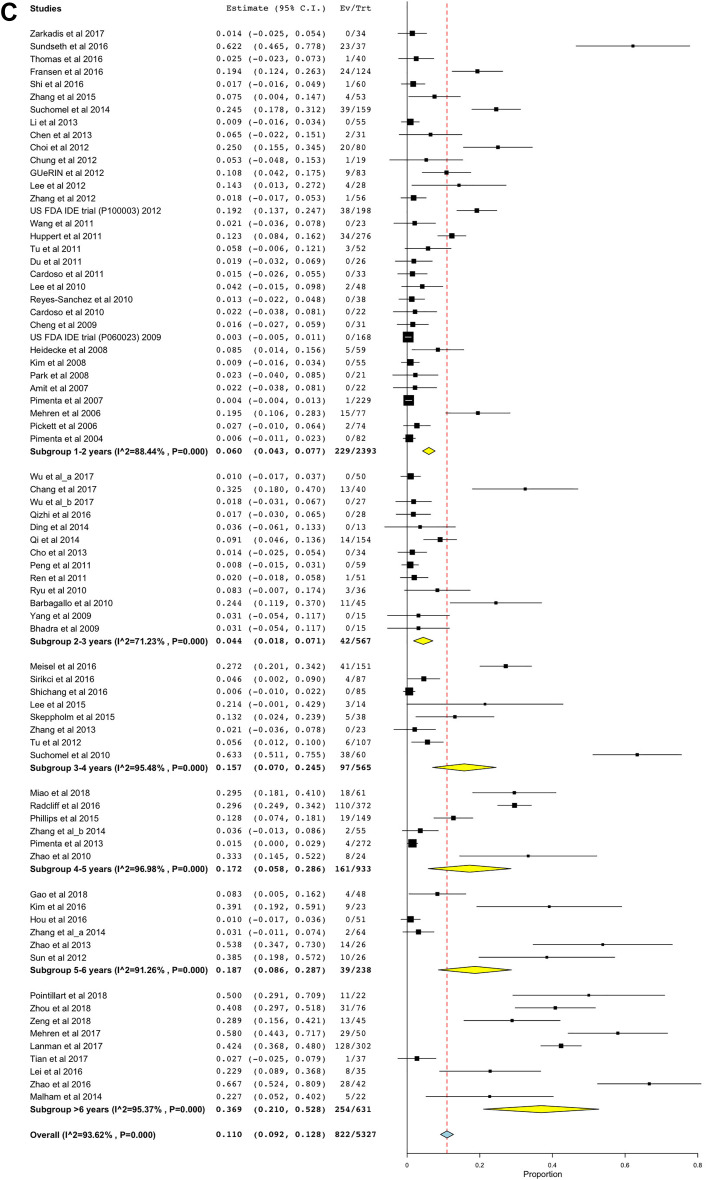
ROM-Limiting HO
A total of 75 studies reported the rates of ROM-limiting HO. The pooled prevalence of ROM-limiting HO was 11.0% (95% CI 9.2% to 12.8%; Figure 5A). When the analysis was stratified according to the types of prosthesis, ProDisc-C (pooled HO rate 31.8%, 95% CI 16.6% to 47.1%), Activ-C prosthesis (pooled HO rate 25.8%, 95% CI 20.9% to 30.6%), and Secure-C prostheses (pooled HO rate 19.2%, 95% CI 13.7% to 24.7%) had a significantly higher rate of ROM-limiting HO than the pooled prevalence of ROM-limiting HO (Figure 5B).
Figure 5.
(A) The rate of range of motion (ROM)–limiting heterotopic ossification (HO). (B) The rate of ROM-limiting HO stratified by the types of prosthesis. (C) The rate of ROM-limiting HO stratified by the length of follow-up.
Figure 5C shows the rates of ROM-limiting HO at various follow-up time points. The rate of ROM-limiting HO in >6 years of follow-up studies (pooled HO rate 36.9%, 95% CI 21.0% to 52.8%) was significantly higher than that in studies with 1 to 2 years (pooled HO rate 6.0%, 95% CI 4.3% to 7.7%) and 2 to 3 years (pooled HO rate 4.4%, 95% CI 1.8% to 7.1%) of follow-up.
Meta-Regression
Only single-level CTDR was associated with the overall rate of HO. When the rate of HO was stratified according to McAfee4 or Mehren classification,5 a number of factors were associated with the development of each subgrade of HO. Non-RCT study design and single-level CTDR were associated with a higher rate of grade I HO; latest publication, non-RCT study design, studies published outside Asia, male gender and single-level CTDR were associated with a higher rate of grade II HO; studies published outside Asia, male gender, single-level CTDR and longer follow-up period were associated with a higher rate of grade III HO; latest publication, studies published outside Asia and longer follow-up period were associated with a higher rate of grade IV HO; and latest publication, single-level CTDR, longer follow-up period and studies published outside Asia were associated with a higher rate of ROM-limiting HO. CTDR at C5C6 spinal level and age were not associated with the overall rate of HO or any subgrades of HO.
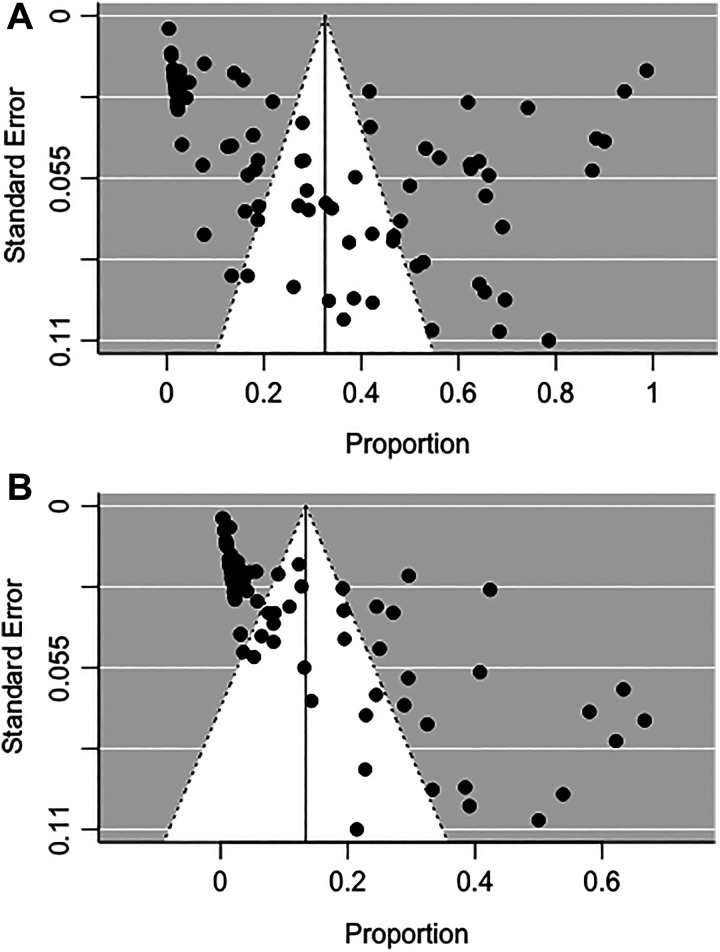
Publication Bias
In Figure 6A and B, there are asymmetries in both funnel plots. Results from the Begg and Mazumdar rank correlation test (overall HO P = .0001, Kendall’s tau = 0.29; ROM-limiting HO P < .0001, Kendall’s tau = 0.58) and Egger regression test (overall HO P < .0001; ROM-limiting HO P < .0001) also suggested potential publication bias.
Figure 6.
(A) Funnel plot of the meta-analysis of overall rate of heterotopic ossification (HO). (B) Funnel plot of the meta-analysis of rate of range of motion (ROM)–limiting HO.
However, the lack of studies in the bottom left side of the funnel plots in overall HO and ROM-limiting HO studies may not indicate possible publication bias. The prevalence of HO cannot be lower than zero, which may explain the asymmetry in the plots.
Discussion
The current systematic review and meta-analysis is composed of 94 clinical studies and is the most comprehensive assessment of the pooled prevalence of different grades of HO after CTDR to date. This meta-analysis is also the first to explore the associations between numerous risk factors and HO rates after CTDR by multivariable, meta-regression analysis.
Our study reported that the overall prevalence of HO 1 to 2 years post-CTDR was 24.8%. By contrast, Chen et al9 reported that the overall prevalence of HO ranged from 44.6% to 58.3% after 1 to 2 years of follow-up, while another recent meta-analysis reported the rate to be 38%.10 The discrepancy between our results and the results of previous meta-analyses can be explained by the inclusion of more clinical trials in our review. Some of our included studies with 1 to 2 years of follow-up reported a zero rate of HO, which were not included in the 2 previous meta-analyses.16-24 Moreover, the prevalence of HO was expressed in the number of spinal levels in our study, whereas previous meta-analyses expressed the prevalence of HO in the number of patients.
A number of risk factors of HO have been identified in our study. Our meta-analysis and another clinical trial have reported a significant positive association of single-level CTDR with the rate of HO.25 Yi et al26 suggested that the formation of HO is a dynamic process that is constantly affected by the environment, including biomechanical characteristics of the cervical spine. Since symptomatic patients with cervical disc degeneration often have pathologies in multiple cervical spinal segments,27 we infer that multilevel CTDR may restore the kinematics of the cervical spine of patients better than single-level CTDR. Therefore, the spine kinematics of patients who have received multilevel CTDR may exert less biomechanical disruption on their surgical spinal segments, thus reducing their rates of HO. One other risk factor of HO includes male gender.
Different prostheses have their distinct biomechanical characteristics, design, and implantation techniques.28 These variations have been postulated to contribute to the formation of HO.28 However, evidence is inconsistent as to which prosthesis is superior in reducing the rate of HO. In a nonrandomized study with an average 20 months of follow-up, the rate of HO was significantly lower in the Bryan disc group than that in the Mobi-C and ProDisc-C groups.28 By contrast, our meta-analysis showed that Kineflex-C and Secure-C prostheses had a higher rate of HO, whereas M6-C, Prestige ST, and PCM prostheses had a lower rate of HO, relative to the overall prevalence of HO. Of note, our findings were limited by the small number of included studies and the variation in the length of follow-up. Hence, the results should be interpreted with caution.
Despite the distinct biomechanical characteristics of the C5C6 spinal segment,29 CTDR at the C5C6 level was not correlated with the rate of HO. Besides surgical spinal segments, age was not a significant predictor of HO.
In addition to biological and surgical factors, the differences in study design were also associated with the rate of HO. Studies published in non-Asian countries were associated with higher rates of grade II to IV HO, which may be due to differences in ethnicities of subjects. Moreover, the latest publications tended to have higher rates of grade II and IV HO. The first grading system of HO in CTDR was first published in 2003.4 As radiologists and spine surgeons are gaining more experience in grading HO, the accuracy of diagnosing of HO may tend to improve over time. Last, non-RCT studies were associated with higher rates of grade I and II HO. Since nonrandomized studies cannot entirely exclude imbalances in prognostic factors,30 the biases in nonrandomized studies may lead to differences in the rate of HO between randomized and nonrandomized studies.
Furthermore, our meta-analysis has shown that a longer follow-up period was associated with higher rates of grade III and IV HO. The findings from our study were in congruent with another meta-analysis, which demonstrated a linear correlation between the length of follow-up and the prevalence of ROM-limiting HO in studies with 1 to 2 years and 2 to 5 years of follow-up.10 A retrospective study further showed that the second follow-up time point was significantly more likely to develop new and more severe HO than the first follow-up time point.26 However, whether there is any causal relationship between the length of follow-up and the rate of HO is unknown. HO has been suggested to be a progressive phenomenon in response to environmental factors.26 Constant dynamic load from nonphysiological motion of the cervical spine on the surgical spinal segments may stimulate bone remodeling and promote bone formation over time.31
Our meta-analysis has several limitations. First, although the statistical tests and funnel plots showed possible publication bias, it is impossible to have negative prevalence rates, and thus may explain the significant results in these tests. Second, we found significant heterogeneity across our included studies, and the residual heterogeneity remained significant after multivariate meta-regression analyses. We were unable to account for perioperative variables such as blood loss, because they were infrequently reported in the included studies. Third, the lack of studies with longer than 10 years of follow-up would not allow an accurate estimate of the point prevalence of HO in the long-term. Fourth, the number of studies of grade III, grade IV, and ROM-limiting HO is not equivalent because several studies reported the rate of one of these outcomes only. Last, interobserver bias exists, which may underestimate the rate and severity of HO, regardless of the type of imaging modality used. To minimize observer bias, most studies employed independent clinicians to review the images.
Conclusion
This meta-analysis shows that HO is prevalent in patients who received CTDR and the rate of HO was higher in studies with longer follow-up. The prevalence of HO varied according to the grades of HO, length of follow-up, and types of prosthesis. Moreover, studies published outside Asia, male gender, single-level CTDR, and longer follow-up period were risk factors of different subgrades of HO. The findings from our study may aid the understanding of the pathophysiology of HO and clinical decision making.
Supplemental Material
Supplemental Material, Summry_table_study_demographics for Prevalence of and Risk Factors for Heterotopic Ossification After Cervical Total Disc Replacement: A Systematic Review and Meta-Analysis by Nicholas Hui, Kevin Phan, Jack Kerferd, Meiyi Lee and Ralph J. Mobbs in Global Spine Journal
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Nicholas Hui  https://orcid.org/0000-0001-5625-4307
https://orcid.org/0000-0001-5625-4307
Supplemental Material: Supplemental material for this article is available online.
References
- 1. O’Neill KR, Wilson RJ, Burns KM, et al. Anterior cervical discectomy and fusion for adjacent segment disease: clinical outcomes and cost utility of surgical intervention. Clin Spine Surg. 2016;29:234–241. [DOI] [PubMed] [Google Scholar]
- 2. Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976). 2002;27:2431–2434. [DOI] [PubMed] [Google Scholar]
- 3. Garland DE. A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop Relat Res. 1991;(263):13–29. [PubMed] [Google Scholar]
- 4. McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 2003;16:384–389. [DOI] [PubMed] [Google Scholar]
- 5. Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976). 2006;31:2802–2806. [DOI] [PubMed] [Google Scholar]
- 6. Zhou HH, Qu Y, Dong RP, Kang MY, Zhao JW. Does heterotopic ossification affect the outcomes of cervical total disc replacement? A meta-analysis. Spine (Phila Pa 1976). 2015;40:E332–E340. [DOI] [PubMed] [Google Scholar]
- 7. Hou Y, Nie L, Pan X, et al. Effectiveness and safety of Mobi-C for treatment of single-level cervical disc spondylosis: a randomised control trial with a minimum of five years of follow-up. Bone Joint J. 2016;98:829–833. [DOI] [PubMed] [Google Scholar]
- 8. Sundseth J, Jacobsen EA, Kolstad F, et al. Heterotopic ossification and clinical outcome in nonconstrained cervical arthroplasty 2 years after surgery: the Norwegian Cervical Arthroplasty Trial (NORCAT). Eur Spine J. 2016;25:2271–2278. [DOI] [PubMed] [Google Scholar]
- 9. Chen J, Wang X, Bai W, Shen X, Yuan W. Prevalence of heterotopic ossification after cervical total disc arthroplasty: a meta-analysis. Eur Spine J. 2012;21:674–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kong L, Ma Q, Meng F, Cao J, Yu K, Shen Y. The prevalence of heterotopic ossification among patients after cervical artificial disc replacement: a systematic review and meta-analysis. Medicine (Baltimore). 2017;96:e7163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Phan K, Tian DH, Cao C, Black D, Yan TD. Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg. 2015;4:112–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Phan K, Mobbs RJ. Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg. 2015;1:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Furlan AD, Malmivaara A, Chou R, et al. 2015 updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976). 2015;40:1660–1673. [DOI] [PubMed] [Google Scholar]
- 15. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. [DOI] [PubMed] [Google Scholar]
- 16. Zarkadis NJ, Cleveland AW, Kusnezov NA, Dunn JC, Caram PM, Herzog JP. Outcomes following multilevel cervical disc arthroplasty in the young active population. Mil Med. 2017;182:e1790–e1794. [DOI] [PubMed] [Google Scholar]
- 17. Wang Q, Cheng H, Mao Z, Qi X, Zhang M, Chen Y. Clinical and radiographic results after treatment of cervical degenerative disc disease with the Bryan disc prosthesis: a prospective study with 2-year follow-up. Acta Orthop Belg. 2011;77:809–815. [PubMed] [Google Scholar]
- 18. Du J, Li M, Liu H, Meng H, He Q, Luo Z. Early follow-up outcomes after treatment of degenerative disc disease with the discover cervical disc prosthesis. Spine J. 2011;11:281–289. [DOI] [PubMed] [Google Scholar]
- 19. Cardoso MJ, Mendelsohn A, Rosner MK. Cervical hybrid arthroplasty with 2 unique fusion techniques. J Neurosurg Spine. 2011;15:48–54. [DOI] [PubMed] [Google Scholar]
- 20. Cardoso MJ, Rosner MK. Multilevel cervical arthroplasty with artificial disc replacement. Neurosurg Focus. 2010;28:E19. [DOI] [PubMed] [Google Scholar]
- 21. Cheng L, Nie L, Zhang L, Hou Y. Fusion versus Bryan cervical disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop. 2009;33:1347–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim SW, Shin JH, Arbatin JJ, Park MS, Chung YK, McAfee PC. Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J. 2008;17:20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Park JH, Roh KH, Cho JY, Ra YS, Rhim SC, Noh SW. Comparative analysis of cervical arthroplasty using Mobi-CÒ and anterior cervical discectomy and fusion using the SolisÒ-cage. J Korean Neurosurg Soc. 2008;44:217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Amit A, Dorward N. Bryan cervical disc prosthesis: 12-month clinical outcome. Br J Neurosurg. 2007;21:478–484. [DOI] [PubMed] [Google Scholar]
- 25. Huppert J, Beaurain J, Steib J, et al. Comparison between single-and multi-level patients: clinical and radiological outcomes 2 years after cervical disc replacement. Eur Spine J. 2011;20:1417–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yi S, Oh J, Choi G, et al. The fate of heterotopic ossification associated with cervical artificial disc replacement. Spine (Phila Pa 1976). 2014;39:2078–2083. [DOI] [PubMed] [Google Scholar]
- 27. Suzuki A, Daubs MD, Hayashi T, et al. Patterns of cervical disc degeneration: analysis of magnetic resonance imaging of over 1000 symptomatic subjects. Global Spine J. 2018;8:254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yi S, Kim KN, Yang MS, et al. Difference in occurrence of heterotopic ossification according to prosthesis type in the cervical artificial disc replacement. Spine (Phila Pa 1976). 2010;35:1556–1561. [DOI] [PubMed] [Google Scholar]
- 29. Holmes A, Wang C, Han ZH, Dang GT. The range and nature of flexion-extension motion in the cervical spine. Spine (Phila Pa 1976). 1994;19:2505–2510. [DOI] [PubMed] [Google Scholar]
- 30. Reeves B. Principles of research: limitations of non-randomized studies. Surgery (Oxford). 2008;26:120–124. [Google Scholar]
- 31. Cho HJ, Shin MH, Huh JW, Ryu KS, Park CK. Heterotopic ossification following cervical total disc replacement: iatrogenic or constitutional? Korean J Spine. 2012;9:209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Summry_table_study_demographics for Prevalence of and Risk Factors for Heterotopic Ossification After Cervical Total Disc Replacement: A Systematic Review and Meta-Analysis by Nicholas Hui, Kevin Phan, Jack Kerferd, Meiyi Lee and Ralph J. Mobbs in Global Spine Journal