Abstract
This study retrospectively estimated costs for a convenience sample of school-located vaccination (SLV) clinics conducted in Maine during the 2009–2010 influenza season. Surveys were developed to capture the cost of labor including unpaid volunteers as well as supplies and materials used in SLV clinics. Six nurses from different school districts completed a clinic day survey on staff time; four of the six also provided data for materials and supplies. For all clinics, average per-dose labor cost was estimated at $5.95. Average per-dose material cost, excluding vaccine, was $5.76. From the four complete clinic survey responses, total per-dose cost was estimated to be an average of $13.51 (range = $4.91–$32.39). Use of donated materials and uncompensated volunteer staff could substantially reduce per-dose cost. Average per-dose cost could also be lowered by increasing the number of doses administered in a clinic.
Keywords: influenza vaccination, 2009 H1N1, pandemic, influenza, school nurse, cost evaluation, school-located vaccination clinics
Introduction
Schools have been proposed as a potentially viable venue to reach school-age children for vaccinations routinely recommended for children and adolescents, including influenza vaccination (Lindley et al., 2008; Mazyck, 2010). School-located vaccination (SLV) clinics are defined as clinics designed to vaccinate school-age children. These clinics are usually held at school, before, during, or after school hours (Centers for Disease Control and Prevention, 2010a). Growing interest in SLV clinics has been prompted in part by the expansion of the influenza vaccination recommendations, recent vaccination recommendations for adolescents, and by the fact that SLV clinics were held widely in 2009–2010 for pandemic monovalent 2009 H1N1 (2009 H1N1) vaccination (Hull & Ambrose, 2011; Jenlink, Kuehnert, & Mazyck, 2010). Reductions in school absenteeism among students make SLV clinics program more promising (Graitcer et al., 2012; King et al., 2012). Given that resources are limited, the cost of conducting this activity is an important factor influencing the ability of local health departments and schools to run SLV clinics.
This study focuses on the cost of SLV clinics held in the state of Maine during the 2009–2010 pandemic influenza season. Over 95% of the more than 600 schools statewide either conducted or participated in SLV clinics (Lorick et al., 2011). However, schools and school districts used different SLV clinic approaches to address local needs and challenges. For example, some school districts partnered with local healthcare organizations (e.g., Visiting Nurses Associations [VNA] or hospital systems) or in some cases, implemented SLV independently with limited support from the state or local health department. Most SLV clinics were held onsite during school hours and the majority of SLV clinics offered both trivalent seasonal (seasonal) and 2009 H1N1 influenza vaccines (Lorick et al., 2011). Decisions about how to implement the SLV clinics were made at the local level by communities and school districts depending on the preferences and circumstances of each school district and community. 2009–2010 vaccination coverage for 2009 H1N1 vaccine in Maine was estimated at 60% for children and adolescents 6 months to 17 years, which was substantially higher than the national median coverage, 37% (Centers for Disease Control and Prevention, 2010b).
In this study, we present estimates of the cost of staff time and materials (excluding vaccine), including volunteer time and donated materials, related to conducting SLV clinics among a nonrepresentative, convenience sample of schools in Maine. The clinic-level SLV costs are compared by resource type - paid and unpaid staff and material cost - and clinic size. The data were collected after the SLV clinics were completed; thus, the study is retrospective in nature. While this evaluation was designed to characterize the cost-driving or cost-saving factors related to conducting clinics, costs related to outside clinic activities were also gathered but are being reported in a separate manuscript (Beeler-Asay et al., 2012).
Method
This study was determined to be nonresearch, public health practice and program evaluation by the Centers for Disease Control and Prevention (Personal communication with Micah H. Milton, MPH, CIP, NCIRD Human Subject Advisor of CDC). To obtain general information and inform survey instrument development, in May 2010, we interviewed in-person or by phone, a convenience sample of 10 “lead nurses” or “health services coordinators” who played a leading role in planning and implementation of the 2009–2010 SLV clinics in their school districts. Survey instrument drafts were reviewed and updated based on comments provided by a sample of two nurses. To obtain a sample representing varying approaches and partnerships (vaccination by the school nurse or vaccination performed by a VNA or hospital) and location (rural or urban), in early June 2010 we first invited a group of 12 school nurses representing 11 different school districts to participate. This initial group was based upon recommendations by Maine CDC and DOE leadership and evaluators from the University of Southern Maine, Muskie School of Public Service. To increase sample size, in July 2010, we invited an additional 11 nurses from eight districts to participate.
The survey consists of two parts: (1) staff time and role and (2) supplies and material information.1 Most schools held more than one SLV clinic. However, we collected information about the first 2009 H1N1 vaccine clinic held in each school district; some schools had already conducted a seasonal influenza vaccination clinic by the time their first H1N1 vaccination clinic was held in late October 2009. We asked participants to consult records related to the H1N1 clinics such as vaccine dose reports to the Maine Center for Disease Control, written personal records, and other electronic records available whenever possible. Participants faxed or e-mailed completed surveys or study team members completed surveys via phone interviews.
For the labor cost analysis, staff time spent and the associated cost was categorized according to clinic roles. The three roles included were (1) lead nurse; (2) vaccinator; and (3) non-vaccinator. Under the vaccinator and non-vaccinator categories, staff were grouped as paid or nonpaid volunteer staff. Time spent by each category was measured in person-hours. In order to estimate the value for staff time, we used the 2009 median wage for the state of Maine by occupation (e.g., registered nurse, school educators, physicians, secretaries) from the Bureau of Labor Statistics of U.S. Department of Labor (U.S. Bureau of Labor Statistics, 2010). For lead nurses, we used 75th percentile wages, as there is no wage data for lead school nurses. A median wage for all occupations was used for volunteers as we do not have any information about volunteers’ occupation. We assumed a 30% of fringe benefit rate for all employees.
Supplies and materials used were grouped by their source: new purchase, existing stock, or donation. Newly purchased materials include only newly acquired materials for the SLV clinics. Existing stock refers to materials already being used or purchased for replenishing stock for school year. Donated materials were provided free of charge to the school by nonschool entities such as local charities or local pharmacies. We collected price data from several school clinic supply vendors’ websites and used the average price for each item for year 2009. For all durable goods or assets such as TVs or tables, instead of purchase price, we used a depreciated value of the durable goods-the value lost due to its use. We depreciated products after 3 years with a fixed rate of depreciation (3%) assuming 15 total years of useful life of capital goods (e.g., televisions, tables, or other multi-use goods). We excluded the costs of H1N1 vaccine, needles, syringes, and sharps containers provided at no cost by the U.S. federal government, and seasonal vaccines provided by the state of Maine. The cost of additional syringes or sharps disposal containers acquired either by purchase or by donation was included in the cost estimation.
Survey data were de-identified and entered into a spreadsheet and tabulated for cost analyses. The clinic cost is the sum of labor and material cost. We calculated per dose clinic cost of vaccination by dividing the clinic cost by the total number of doses administered. For the clinics that offered both 2009 H1N1 and seasonal influenza vaccines, the sum of both 2009 H1N1 and seasonal influenza vaccines doses was used. All labor and materials costs are in constant 2009 U.S. dollars.
Since we did not collect information about second dose clinics or ask responders to break down the number of doses given by vaccine type (inactivated or live-attenuated vaccine), we could not estimate the average cost per dose by these factors. Because of the small sample size and convenience sampling, we compare the individual clinic cost by clinic instead of summary statistics such as variance or 95% confidence interval.
Results
Of the 19 school districts invited to participate, six lead nurses from different school districts completed all surveys for their school district’s first H1N1 clinic. Among six clinics, three SLV clinics vaccinated students with both H1N1 and seasonal influenza vaccines at the same visit and the rest of the clinics with H1N1 influenza vaccine only (Table 1). Clinics were held between October 26, 2009, and November 12, 2009. Of the six school districts, one school district is located in a city, two in suburbs, one in a town, and two in rural areas according to the school locale type definition (National Center for Education Statistics, 2006). The number of doses administered including both 2009 H1N1 and seasonal influenza vaccines ranged from 115 to 598 (mean = 386 doses). On average, 22 person-hours of the vaccinators (range = 15–30) and 42 person-hours of the non-vaccinators (range = 21–83) were spent per clinic. The ratio of vaccinator time to non-vaccinator time ranged from 0.22 to 1.46 (mean = 0.68). In 2009 H1N1 vaccination only clinics, more vaccinators and person-hours were used than in 2009 H1N1 and seasonal vaccination clinics. However, average time spent by non-vaccinators in both settings was similar. On average, one vaccinator administered 17 doses of vaccines per hour (range = 6–40). However, doses per vaccinator-hour in 2009 H1N1 and seasonal vaccination clinics are higher than in 2009 H1N1 vaccine only clinic: 21 doses versus 12 doses (Table 1).
Table 1.
Description of Sampled School-Located Vaccination Clinics
| 2009 H1N1 Vaccine Only Clinics | 2009 H1N1 and Seasonal Vaccine Clinics | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall Mean | Mean | Clinic 3 | Clinic 5 | Clinic 6 | Mean | Clinic 1 | Clinic 2 | Clinic 4 | |
| School locale typea | Rural | Suburb | Town | Suburb | City | Rural | |||
| Doses administered (A)b | 386 | 313 | 115 | 320 | 503 | 458 | 407 | 598 | 370 |
| Vaccinator | |||||||||
| Number of staff (B) | 6 | 8 | 3 | 12 | 8 | 5 | 5 | 5 | 4 |
| -Paid staff | 4 | 5 | 0 | 10 | 4 | 2 | 1 | 4 | 2 |
| -Unpaid staff | 3 | 3 | 3 | 2 | 4 | 2 | 4 | 1 | 2 |
| Person-hours spent (C) | 22 | 25 | 18 | 30 | 26 | 18 | 16 | 15 | 24 |
| Non-vaccinator | |||||||||
| Number of staff (D) | 12 | 11 | 16 | 8 | 9 | 13 | 17 | 12 | 9 |
| -Paid staff | 7 | 5 | 6 | 5 | 3 | 9 | 16 | 6 | 5 |
| -Unpaid staff | 5 | 6 | 10 | 3 | 6 | 4 | 1 | 6 | 4 |
| Person-hours spent (E) | 42 | 42 | 83 | 21 | 24 | 41 | 43 | 33 | 47 |
| Vaccinator/Non-vaccinator ratio | |||||||||
| Number of staff (=B/D) | 0.62 | 0.86 | 0.19 | 1.50 | 0.89 | 0.39 | 0.29 | 0.42 | 0.44 |
| Person-hours spent (=C/E) | 0.68 | 0.92 | 0.22 | 1.46 | 1.09 | 0.45 | 0.37 | 0.45 | 0.51 |
| Dose administered per vaccinator time (=A/C) | 17 | 12 | 6 | 11 | 19 | 21 | 33 | 40 | 15 |
School locale type is based on the definition by National Center for Education statistics.
Doses include both 2009 H1N1 and seasonal influenza vaccine doses.
Average labor cost for all six clinics is estimated at $1,458 (range = $1,117–$2,312; Table 2). In most SLV clinics, school nurses vaccinated the students with the help of either volunteer vaccinators or vaccinators from the local health department or the VNA. Most of the labor cost is associated with vaccinators including volunteer vaccinators, followed by non-vaccinators including school support staff. Among the six respondents, two were not able to provide data about supplies and materials used in SLV clinics so results are presented for the remaining four clinics. For supplies and material, an average of $1,369 (range= $1,237–$1,565) was spent. Material costs (50% of total cost) were covered by donations from either public health agencies or local communities.About 25% of material costs were from purchases for the SLV clinic program (e.g., Band-Aid, gauze, coolers for vaccine storage, etc.) and 25%of cost was from the use of existing supplies. For the four clinics with labor and materials data, the average total clinic cost is estimated to be $2,987 (range = $2,469–$3,724) with $ 1,618 of labor cost (54%), and $1,369 of material cost (46%). Approximately, 42% of clinic cost was covered through donations and volunteer time (approximately 20% for volunteers and 22% for donated materials). For all six clinics, the per-dose average labor cost is estimated to be $5.95 (range = $ 1.87–$ 20.11; Table 2). The average materials cost for the four clinics with available data is $5.76 per dose (range= $2.51–$12.28). The average total clinic cost per dose is $13.51 (range=$4.91–$32.39) for the four clinics with labor and materials data.
Table 2.
School-Located Vaccination Clinic Cost in Maine (2009–2010 Pandemic Influenza Season, 2009 US$)
| 2009 H1N1 vaccine only clinics | 2009 H1 N1 and seasonal vaccine clinics | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall mean | Mean (%) | Clinic 3 (%) | Clinic 5 (%) | Clinic 6 (%) | Mean (%) | Clinic 1 (%) | Clinic 2 (%) | Clinic 4 (%) | |
| Labor cost total (A) | $1,458 | $1,582 (100) | $2,312 (100) | $1,227 (100) | $1,207 (100) | $1,333 (100) | $1,156 (100) | $1,117 (100) | $1,726 (100) |
| Lead nurse | $259 | $231 (15) | $344 (15) | $143 (12) | $206 (17) | $286 (21) | $172 (15) | $344 (31) | $344 (20) |
| Vaccinators | $623 | $694 (44) | $516 (22) | $829 (68) | $737 (61) | $551 (41) | $555 (48) | $412 (37) | $687 (40) |
| Nonvaccinator | $576 | $657 (42) | $1,453 (63) | $255 (21) | $264 (22) | $496 (37) | $430 (37) | $362 (32) | $695 (40) |
| Supplies and material cost totala (B) | $1,369 | $1,413 (100) | $1,412 (100) | $1,565 (100) | $1,262 (100) | $1,237 (100) | –e | –e | $1,237 (100) |
| New purchase | $362 | $406 (29) | $250 (18) | $144 (9) | $824 (65) | $230 (19) | –e | –e | $230 (19) |
| Existing stock | $338 | $269 (19) | $303 (21) | $170 (11) | $335 (27) | $544 (44) | –e | –e | $544 (44) |
| Donation | $669 | $738 (52) | $860 (61) | $1,251 (80) | $103 (8) | $463 (37) | –e | –e | $463 (37) |
| Clinic cost total (=A + B) | $2,987 | $2,995 (100) | $3,724 (100) | $2,793 (100) | $2,469 (100) | $2,963 (100) | N/A | N/A | $2,963 (100) |
| Labor Costb | $1,618 | $1,582 (53) | $2,312 (62) | $1,227 (44) | $1,207 (49) | $1,944 (66) | N/A | N/A | $1,726 (58) |
| Paid staff time | $1,039 | $981 (33) | $1,859 (50) | $354 (13) | $728 (30) | N/A | N/A | N/A | $1,214 (41) |
| Volunteer timec | $579 | $602 (20) | $453 (12) | $874 (31) | $479ssss (l9) | N/A | N/A | N/A | $512 (17) |
| Material Cost | $1,369 | $1,413 (47) | $1,412 (38) | $1,565 (56) | $1,262 (51) | $1,237 (42) | N/A | N/A | $1,237 (42) |
| Purchased materialsd | $700 | $675 (23) | $553 (15) | $314 (11) | $1,159 (47) | $774 (26) | N/A | N/A | $774 (26) |
| Donated materials | $669 | $738 (25) | $860 (23) | $1,251 (45) | $103 (4) | $463 (16) | N/A | N/A | $463 (16) |
| Per-dose labor cost (6 clinics) | $5.95 | $8.78 | $20.11 (62) | $3.84 (44) | $2.40 (49) | $3.12 | $2.84 | $1.87 | $4.66 (58) |
| Per-dose material cost (4 clinics) | $5.76 | $6.56 | $12.28 (38) | $4.89 (56) | $2.51 (51) | $3.34 | N/A | N/A | $3.34 (42) |
| Per-dose clinic cost (4 clinics) | $13.51 | $15.34 | $32.39 (100) | $8.73 (100) | $4.91 (100) | $8.01 | N/A | N/A | $8.01 (100) |
Note. N/A = not applicable. Percentages may not add up to 100% due to rounding.
Both H1N1 and seasonal influenza vaccines, syringes, and needles are not included. Only four clinics with complete data were used.
Labor costs used to calculate the total clinic cost include only the clinic whose data about supplies and materials were provided.
Volunteer time includes medical volunteers, emergency medical services, and parents and others time.
Purchase materials include new purchase and existing stock.
Clinics 1 and 2 were not able to provide data about supplies and materials used for their clinics.
Figure 1 shows the cost per-dose for labor for six clinics and material and total clinic costs for four clinics. The inverse relationship between the average costs and the number of doses administered is heavily influenced by the cost per dose administered in Clinic 3 where the fewest number of doses were administered. However, even without Clinic 3, the average cost appears to decrease with increasing number of doses.
Figure 1.
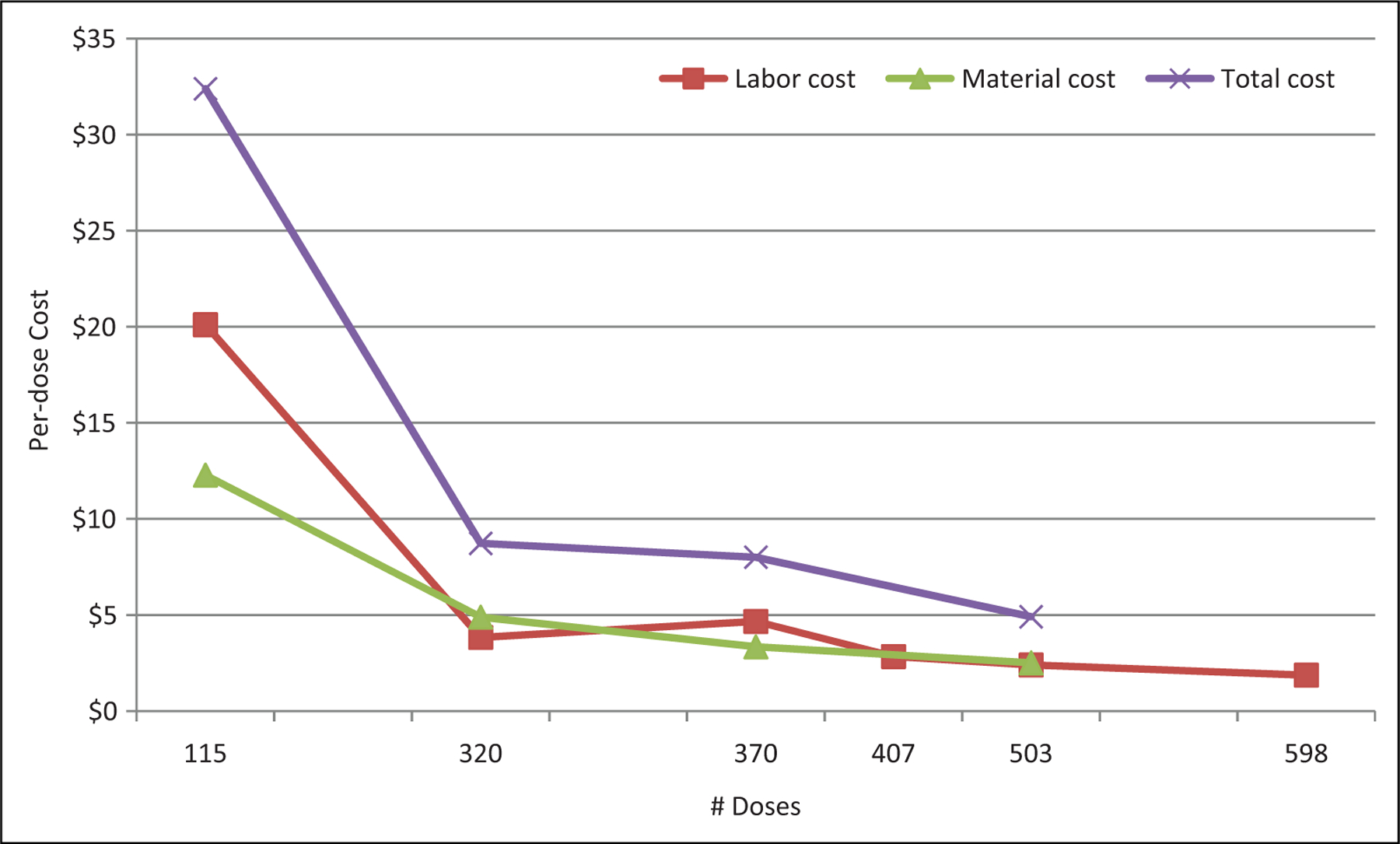
Per-dose labor, material, and total (labor plus material) cost by total doses per clinic. Note. Six clinics provided labor cost and only four clinics provided material cost
Discussion
We estimated that on average SLV clinics conducted in the state of Maine in 2009–2010 cost approximately $3,000 (comprised of 54% of labor cost and 46% of material cost) excluding the cost of vaccine, needles, and syringes. Of note is that 42% of the clinic cost was attributable to volunteer time and donated supplies and materials. An average per-dose vaccination cost, including labor and materials, of four individual clinics is estimated to be $13.51.
A literature review identified several SLV programs held in the United States, with some programs having been conducted over multiple years (Hull & Ambrose, 2011). These programs were organized at either the state or local level (Effler et al., 2010; Hull, 2010; Hull, Frauendienst, Gundersen, Monsen, & Fishbein, 2008; King et al., 2006; Mazyck, 2010; Schmier, Li, King, Nichol, & Mahadevia, 2008). Also, during the 2009–2010 H1N1 pandemic influenza season, SLV clinics were widely held across the United States to vaccinate school-age children, one of the initial target groups for 2009 H1N1 influenza vaccination (Centers for Disease Control and Prevention, 2009; Hull & Ambrose, 2011). SLV clinic cost analyses have been conducted and reported for Hawaii, Minnesota (MN), New York City (NYC), and Alachua County in Florida and the reported cost per vaccination ranges from $10 to $79 excluding vaccine prices (Carpenter et al., 2007; Effler et al., 2010; Hull et al., 2008; Kansagra et al., 2011; Tran et al., 2010; Yoo, 2011). This wide range reflects various factors including the differences in the approaches to conducting SLV clinics and in the factors included in determining total cost. For example, some do not account for the monetary value of volunteer time and donated materials, or planning costs.
However, as in other SLV cost studies (Effler et al., 2010; Hull et al., 2008; Kansagra et al., 2011; Tran et al., 2010; Yoo, 2011), the calculation with aggregated data may not capture the effect of the variation in the cost over individual clinics. For example, per-dose cost based on the aggregated cost ($11,949) and dose (1,308 doses) of four clinics with complete data is estimated to be $9. It is lower than our average of clinic-level per-dose cost ($13.51).
Average per-dose cost of these SLV clinics is less than the per-dose cost of SLV clinics in NYC (Kansagra et al., 2011) and more than the per-dose cost in MN (Hull et al., 2008). We found the range of clinic-level per-dose cost estimates of Maine SLV clinics (range = $5-$32) to be wider than expected but primarily related to one clinic. Excluding that clinic narrows the ranges to $5-$9. This clinic had the highest cost mostly because of the combination of lowest number of doses administered and highest number of non-vaccinator staff. Although our study valued the time of volunteers, in reality, no entity bore those costs. The number of staff present at any given clinic depended on many factors such as the school’s ability to recruit volunteers and availability of partners in the geographic area. Additionally, our study did not measure outcomes from other perspectives (i.e., children, parent, or educators) such as waiting time, school activity disruption, or satisfaction.
The inverse relationship between the average costs and the size of the clinic implies that as the number of doses per clinic increases, average costs falls; stated differently, additional doses spread the one-time or fixed costs (e.g., clinic setup and breakdown time, rental costs, transportation for staff, minimum number of staff per clinic, etc.) associated with conducting a clinic out over more doses of vaccine, reducing the overall cost to vaccinate each individual. In general, economic theory suggests that fixed (clinic) costs will not vary with the number of doses (Folland, Goodman, & Stano, 2004). For instance, a minimum number of people must be present to run the clinic, regardless of how many people will be vaccinated. Thus, with declining average costs, while total cost of a clinic may increase, the cost to vaccinate each individual person will decrease. The implication of this result is that SLV clinics probably could have reduced their average cost by increasing the number of students vaccinated at a clinic.
Finally, if the monetary value of volunteer time and donated materials were not included, the clinic-level per-dose cost would be lower (range = $2–$21) and the average clinic cost per dose would be $8.As suggested by Bobo, Etkind, and Talkinton (2011), the use of volunteer time and donated materials significantly reduces clinic cost (Tran et al., 2010). That is, volunteers and donations from the community are helpful to SLV sustainability in an economic sense. Therefore, in planning SLV clinics, assessing the availability of volunteers and donated supplies will ensure better cost estimates.
School Nursing Implications
Our findings suggest that school nurses should engage community stakeholders to help recruit both medical and nonmedical volunteers and solicit donations. In addition, nurses are encouraged to take part in local data collection efforts or larger studies to gain a better perspective on the true costs of conducting and sustaining SLV and their role in improving access and reducing disparities. School nurses can play a key role in providing school influenza vaccination opportunities to help meet the goal of educational continuity through improved student health and decreased absenteeism.
Limitations
This study is subject to several limitations. First, we evaluated SLV clinics during a pandemic year. Thus, issues related to H1N1 influenza prevention, such as more media/public attention, could have affected the cost of SLV clinic program (e.g., more attention during a pandemic could lead to higher student turnout for SLV clinics and increase donations and volunteer support). Second, as with other retrospective surveys, our data were subject to recall bias. Third, as lead nurses reported staff time and materials used for other staff members, this method was likely to be less accurate than if other staff members had reported the time and materials themselves. Fourth, because we used a convenience sampling scheme and examined a small number of school districts’ first H1N1 vaccination clinics, our results are not necessarily representative of all SLV clinics held in Maine in 2009–2010. Fifth, our per-dose clinic cost does not include overhead cost and the cost associated with outside clinic activities. Finally, we were not able to ascertain at what point adding doses of vaccine would no longer reduce average costs.
Conclusions
Despite the limitations, this study provides planners, policy makers, and school nurses with a range of SLV clinic costs for school districts of varying sizes. To our knowledge, this is the first study to assess clinic-level cost from various localities utilizing different approaches during a pandemic. Also, the monetary value of volunteer time and donated materials were estimated to provide a better understanding of the SLV cost structure. This information can provide a budget estimate for SLV clinic programs and plan for personnel and job tasks to lower costs. Further studies are needed to determine SLV clinics costs for different implementation approaches, and costs and revenues of billing health insurers.
Acknowledgments
The authors would like to thank the school survey participants and interviewees for their valuable time and input. Also, special thanks for the guidance, support, and information provided by Dr. Dora A. Mills, former Director of Maine Center for Disease Control and Prevention (CDC), Kristine L. Perkins, and Dr. Peter F. Smith, both were previously with Maine CDC and other Maine CDC staff, Maine school nurses and school administrators, staff from the VNA Home Health and Hospice, Home Health Visiting Nurses, City of Portland’s Health and Human Services Department, and Bangor’s Department of Health & Community Services, and Kay Dutram and Dr. Teresa Hubley from the University of Southern Maine, Muskie School and Dr. Ricardo Basurto-Davila, previously at CDC. The authors would also like to thank their CDC colleagues Drs. Pascale Wortley and Tara Vogt for their input on the analysis. The preliminary results were presented at Eastern Economics Association Annual Meeting in New York, 2011 and 45th National Immunization Conference in Washington, DC, 2011.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Bios
Bo-Hyun Cho, PhD, is a Health Economist with Carter Consulting Inc., assigned to the Centers for Disease Control and Prevention, Atlanta, GA, USA.
Garrett R. Beeler Asay, PhD, is a Health Economist at Health Services Research and Evaluation Branch, Immunization Services Division, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Suchita A. Lorick, DO, MPH, is a Medical Epidemiologist at Health Services Research and Evaluation Branch, Immunization Services Division, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Meredith L. Tipton, PhD, MPH, is the President of Tipton Enterprizes, Inc., ME, USA.
Nancy L. Dube, RN, MPH, is the School Nurse Consultant at the Maine Department of Education, Augusta, ME, USA.
Mark L. Messonnier, PhD, MS, is the Economics Team Lead at Immunization Services Division and Lead Economist, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Footnotes
Authors’ Note
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of Centers for Disease Control and Prevention.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The survey instrument is available upon request.
References
- Beeler Asay GR, Cho BH, Lorick SA, Tipton ML, Dube NL, & Messonnier ML (2012). Coordination costs for school-located influenza vaccination clinics, Maine, 2009 H1N1 Pandemic. The Journal of School Nursing, Advance online publication. Retrieved from http://jsn.sagepub.com/content/early/2012/06/11/1059840512448676.full.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobo N, Etkind P, & Talkinton K (2011). School-Located Vaccination Clinics: NASN, NACCHO, ASTHO Summit-Meeting Summary.
- Carpenter LR, Lott J, Lawson BM, Hall S, Craig AS, Schaffner W, & Jones TF (2007). Mass distribution of free, intranasally administered influenza vaccine in a public school system. Pediatrics, 120, e172–e178. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2009). Use of influenza A (H1N1) 2009 monovalent vaccine-recommendations of the advisory committee on immunization practices (ACIP), 2009. Morbidity and Mortality Weekly Report, 58, 1–8. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2010a). Influenza school-located vaccination (SLV): Information for planners Centers for Disease Control and Prevention Influenza (flu) website [On-line]. Retrieved from http://www.cdc.gov/flu/school/planners.htm
- Centers for Disease Control and Prevention. (2010b). Interim results: State-specific Influenza A (H1N1) 2009 monovalent vaccination coverage-United States, October 2009-January 2010. Morbidity and Mortality Weekly Report [Online]. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5912a2.htm [PubMed] [Google Scholar]
- Effler PV, Chu C, He H, Gaynor K, Sakamoto S, Nagao M, … Park SY(2010). Statewide school-located influenza vaccination program for children 5–13 years of age, Hawaii, USA. Emerging Infectious Diseases, 16, 244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folland S, Goodman AC, & Stano M (2004). Microeconomic Tools for Health Economics In The economics of health and health care (4th ed., p. 43). Upper Saddle River, NJ: Pearson Prentice Hall. [Google Scholar]
- Graitcer SB, Dube NL, Basurto-Davila R, Smith PF, Ferdinands J, Thompson M, … Shay DK (2012). Effects of immunizing school children with 2009 influenza A (H1N1) monovalent vaccine on absenteeism among students and teachers in Maine. Vaccine, 30, 4835–4841. [DOI] [PubMed] [Google Scholar]
- Hull HF (2010). A survey of physician-led influenza immunization programs in schools. Clinical Pediatrics, 49, 439–442. [DOI] [PubMed] [Google Scholar]
- Hull HF, & Ambrose CS (2011). Current experience with school-located influenza vaccination programs in the United States-A review of the medical literature. Human Vaccines, 7, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull HF, Frauendienst RS, Gundersen ML, Monsen SM, & Fishbein DB (2008). School-based influenza immunization. Vaccine, 26, 4312–4313. [DOI] [PubMed] [Google Scholar]
- Jenlink CH, Kuehnert P, & Mazyck D (2010). Influenza vaccinations, fall 2009: Model school-located vaccination clinics. The Journal of School Nursing, 26, 7S–13S. [DOI] [PubMed] [Google Scholar]
- Kansagra SM, McGinty MD, Morgenthau BM, Marquez ML, Rosselli-Fraschilla A, Zucker JR, & Farley TA (2011). Cost comparison of 2 mass vaccination campaigns against influenza a H1N1 in New York city. American Journal of Public Health, 102, e1–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King JC Jr., Beckett D, Snyder J, Cummings GE, King BS, & Magder LS (2012). Direct and indirect impact of influenza vaccination of young children on school absenteeism. Vaccine, 30, 289–293. [DOI] [PubMed] [Google Scholar]
- King JC Jr., Stoddard JJ, Gaglani MJ, Moore KA, Magder L, McClure E, … Neuzil K (2006). Effectiveness of school-based influenza vaccination. The New England Journal of Medicine, 355, 2523–2532. [DOI] [PubMed] [Google Scholar]
- Lindley MC, Boyer-Chu L, Fishbein DB, Kolasa M, Middleman AB, & Wilson T (2008). The role of schools in strengthening delivery of new adolescent vaccinations. Pediatrics, 121, S46–S54. [DOI] [PubMed] [Google Scholar]
- Lorick SA, Goldberg L, Birkhimer N, Dube N, Dutram K, Hubley T, … Mills DA (2011). Maine’s Success Story - H1N1 School Influenza Vaccination Efforts, 2009–2010. 45th National Immunization Conference, Washington, DC. [Google Scholar]
- Mazyck D (2010). School-located vaccination clinics. The Journal of School Nursing, 26, 3S–6S. [DOI] [PubMed] [Google Scholar]
- National Center for Education Statistics. (2006). Identification of rural locales. Institute of Education Sciences, U.S. Department of Education [Online]. Retrieved from http://nces.ed.gov/ccd/rural_locales.asp
- Schmier J, Li S, King JC Jr., Nichol K, & Mahadevia PJ (2008). Benefits and costs of immunizing children against influenza at school: An economic analysis based on a large-cluster controlled clinical trial. Health Affairs, 27, w96–w104. [DOI] [PubMed] [Google Scholar]
- Tran CH, McElrath J, Hughes P, Ryan K, Munden J, Castleman J, … Morris JG (2010). Implementing a community-supported school-based influenza immunization program. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, 8, 331–341. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. (2010). May 2009 State occupational employment and wage estimates, Maine. Occupational Employment Statistics. US Bureau of Labor Statistics, US Department of Labor [Online]. Retrieved from http://www.bls.gov/oes/current/oes_me.htm [Google Scholar]
- Yoo BK (2011). Cost-effectiveness analysis of school influenza vaccination program. 45th National Immunization Conference, Washington, DC, March 28–31, 2011. [Google Scholar]


