Abstract
Introduction
Diabetes is a highly prevalent disease worldwide and represents a challenge for patients and healthcare systems. This population-based study evaluated diabetes burden in Italy in 2018 by assessing all aspects of outpatient and hospital care.
Research design and methods
We investigated data of 11 300 750 residents in local health districts contributing to ARNO Diabetes Observatory (~20% of Italian inhabitants). All administrative healthcare claims were analyzed to gather information on access to medical resources. Subjects with diabetes, identified by antihyperglycemic drug prescriptions, disease-specific copayment exemption and hospital discharge codes, were compared with age, sex and residency-matched non-diabetic individuals.
Results
We identified 697 208 subjects with ascertained diabetes, yielding a prevalence of 6.2% (6.5% in men vs 5.9% in women, p<0.001). Age was 69±15 (mean±SD). As compared with non-diabetic subjects, patients with diabetes received more prescriptions of any drugs (+30%, p<0.001), laboratory tests, radiologic exams and outpatient specialist consultations (+20%, p<0.001) and were hospitalized more frequently (+86%, p<0.001), with a longer stay (+1.4 days, p<0.001). Although cardiovascular diseases accounted for many hospital discharge diagnoses, virtually all diseases contributed to the higher rate of hospital admissions in diabetic subjects (235 vs 99 per 1000 person-years, p<0.001). Healthcare costs were >2-fold higher in subjects with diabetes, mainly driven by hospitalizations and outpatient care related to chronic complications rather than to glucose-lowering drugs, diabetes-specific devices, or metabolic monitoring.
Conclusions
The burden of diabetes in Italy is particularly heavy and, as a systemic disease, it includes all aspects of clinical medicine, with consequent high expenses in all areas of healthcare.
Keywords: hospitalization, health care and epidemiology, resource use, administrative data
Significance of this study.
What is already known about this subject?
Diabetes is a common disease frequently associated with macrovascular and microvascular complications which have a significant impact on healthcare expenditure worldwide.
What are the new findings?
Diabetes prevalence in Italy seems to have reached a plateau to approximately 6%.
Diabetes is associated with an increased access to any kind of medical resources (drugs, diagnostic procedures, outpatient and hospital care).
Diabetes is associated to an increased risk of virtually all diseases and not solely classic chronic complications.
Virtually all diseases occurring in a diabetic person might be regarded as an acute or chronic complication.
Diabetes is a systemic (‘all-in’) disease which generates a healthcare expenditure more than twofold higher than in gender and age-matched non-diabetic population.
How might these results change the focus of research or clinical practice?
Research might broaden to other kinds of organ damage beyond the classic macrovascular and microvascular complications.
Clinical practice might look at diabetes as the true origin of diseases currently considered just as incidental comorbidities.
Introduction
Diabetes mellitus has been identified as a medical emergency by the WHO due to its apparently relentless increase in all continents.1 According to the International Diabetes Federation diabetes currently afflicts almost half billion individuals worldwide, a number more than doubled as compared with 30 years ago.2
Diabetes conveys an increased risk of acute and chronic complications, such as infections of any type (eg, pneumonia, hepatitis, urinary tract infections), myocardial infarction, stroke, amputation, end-stage renal disease, and blindness.3 4 As a consequence, diabetes care contributes substantially to personal and social medical costs and overall healthcare expense of most countries.5 6
Italian residents, as well as residents of many other European countries, rely on a public National Health System (NHS), which offers a full coverage of medical assistance to people with diabetes free of charge: drugs, devices, laboratory exams, imaging, outpatient visits by specialists, hospital care, rehabilitation, and so on. All the assistance delivered to diabetic people by the Italian NHS generates claims, which are carefully recorded in administrative archives. Therefore, these archives can be examined and their data analyzed in order to understand which kind of assistance is delivered in terms of variety (eg, HbA1c assessment or ECG or admission to hospital for myocardial infarction) and numbers (eg, delivered to how many people or how many times per year). Standard costs can be used to investigate diabetes-related health expenses, based on diagnosis-related group (DRG) reimbursement system as well as national and regional price lists of outpatient diagnostic and therapeutic procedures, medications and devices.
Aims of this study were: (1) to provide updated information on the prevalence of diabetes in Italy; (2) to establish the burden of diabetes in Italy in terms of medical care (drugs, devices, outpatient care, hospital care) delivered in 2018; (3) to compare the use of medical resources and their costs in very large samples of subjects with and without diabetes. Our data support the view that diabetes is a systemic (‘all-in’) disease.
Research design and methods
Claims of all drugs, devices, outpatient diagnostic and therapeutic procedures, outpatient specialist consultations prescribed to Italian residents as well as hospital admissions for all causes are collected and filed in by all local health districts (LHD) composing the Italian NHS. Many of these LHDs contribute their data to a national consortium named CINECA, established by the Italian Ministry of University and Research to allow statistical analysis and reporting. Other LHDs contribute their data to the Research & Health Foundation for the same purposes. In calendar year 2018, these two institutions received individual data from 11 300 750 Italian residents of any age living in different areas of North (37.5% of the sample), Center (8.5% of the sample) and South of Italy (54% of the sample). All data referring to a given subject were linked by a unique anonymous identification code. Both institutions had also an available list of subjects who were exempted from paying a fee for some medical services (eg, copayment of drugs or outpatient care) due to the presence of diabetes. In this regard, it is important to emphasize that in Italy not all diabetic people apply for this exemption for a number of reasons and therefore the list of exempted people does not necessarily include all persons with diabetes.
In the present study, three sources were used to identify diabetic subjects from the general population: at least one prescription of an antihyperglycemic drug (oral or injectable), presence of exemption due to a diagnosis of diabetes or a discharge from hospital with a diagnosis of diabetes as primary or secondary cause. The three sources were merged in order to set up a single list of subjects with ascertained diabetes. This approach has been previously used by others and ourselves.7–17 Noteworthy, no clinical data (eg, body mass index, blood pressure HbA1c, lipids, renal function tests, type of diabetes, and so on) were available for these subjects. Only sex, age, residency and administrative claims related to access to medical services were available.
In order to compare the use of medical resources in subjects with or without diabetes a population-based case–control study was conducted. For every one case with diabetes, one subject who did not have diabetes was randomly selected as the control.18 Cases and the controls were matched in terms of gender, age and residency by using the package ‘Designmatch’ of R Foundation. After establishing two well-matched groups with the same number of subjects, we compared drugs, devices, outpatient diagnostic exams and specialist consultation prescriptions as well as information available in hospital discharge medical records (overall and disease-specific rates, duration of hospital stay) in those with and without diabetes in year 2018 (from 1 January to 31 December). All drugs, diagnostic procedures, consultations and admissions to hospital were compared, without a specific focus on those generally associated with diabetes diagnosing, monitoring and care.
Diagnoses reported in hospital discharge records (a maximum of six was allowed) were examined and analyzed. In particular, primary diagnosis (the first in the list) was taken as representative of the main reason for hospital stay. Diagnoses are those listed in International Classification of Diseases, Ninth Revision.19 Also, the DRG codes originated by diagnosis listed in the discharge medical reports were considered. We used DRG codes specific of Italy which sometimes differ from those used in other countries. In some analyses the occurrence of a diagnosis code in the hospital discharge record (eg, myocardial infarction) was linked to a single subject to achieve the number of subjects with at least one event (per 1000 persons). In other analyses all hospitalizations with a given diagnosis code were linked to a single individual in order to achieve the cumulative number of events (per 1000 persons).
Costs of all medical services delivered to patients were calculated according to Italian DRG reimbursement system, as well as national and regional price lists of outpatient diagnostic and therapeutic procedures, medications and devices. Costs were grouped into five expense items: (A) hospital care; (B) outpatient care (exams, specialist consultations, and so on); (C) diabetes-related devices (glucose strips, lancets, needles); (D) antihyperglycemic drugs; (E) any kind of other drugs (eg, antihypertensive, lipid lowering but also antibiotics, anti-inflammatory, and so on).
Continuous variables are reported as mean and SD or SE as indicated, whereas categorical variables were reported as percentage. Continuous variables were compared using unpaired Student’s t-test or analysis of variance. Categorical variables were compared using χ2 test. The statistical significance level was conventionally set at 0.05. R software was used to perform statistical analysis.
Results
Prevalence of diabetes
Diabetic subjects with the prescription of an antihyperglycemic drug were 619 849. An exemption due to diabetes was found in 485 452 subjects. The mention of diabetes in hospital discharge records (any position in the six allowed for listing) was retrieved in 51 085 subjects admitted to hospital. The combined use of the three sources allowed the identification of 697 208 subjects with ascertained diabetes out of 11 300 750 residents. This number corresponds to an overall prevalence of the disease of 6.2%.
Mean age was 69±15 years (mean±SD). Men were 51% and women 49%. Table 1 illustrates the distribution of subjects according to gender and age. Two-thirds of subjects (66.9%) aged ≥65 years but almost one-third were in the working age (20–64 years). As many as 23% of diabetic subjects were aged ≥80 years. Children or adolescents with diabetes (aged 0–19 years) accounted for less than 1% of subjects with diabetes (~5000 out of ~700 000).
Table 1.
Distribution of diabetic subjects according to gender and age
| Age classes (years) | Men | Women | All |
| 0–19 | 2376 (0.7%) | 2658 (0.8%) | 5034 (0.7%) |
| 20–34 | 4292 (1.2%) | 10 440 (3.1%) | 14 732 (2.1%) |
| 35–49 | 21 593 (6.1%) | 26 693 (7.8%) | 48 286 (6.9%) |
| 50–64 | 97 023 (27.3%) | 65 608 (19.2%) | 162 631 (23.3%) |
| 65–79 | 164 519 (46.2%) | 140 078 (41.0%) | 304 597 (43.7%) |
| ≥80 | 66 136 (18.6%) | 95 792 (28.1%) | 161 928 (23.2%) |
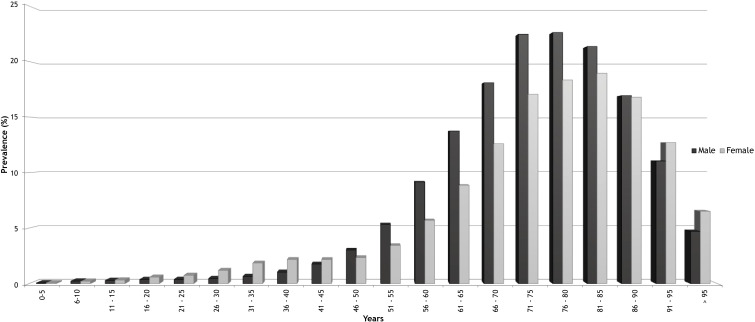
Figure 1 depicts the prevalence of diabetes according to gender and age. Prevalence steadily increased until the age of 75–80 in both genders, then it levels off before declining. Diabetes was more prevalent in men from the age of 50 to 85 years and in women when age was below 45 years or above 90. Overall prevalence was significantly higher in men than in women (6.5% vs 5.9%, p<0.001).
Figure 1.
Prevalence of diabetes according to gender and age.
Cases and controls
The matching procedures were successful and we were able to find a control identical to any single patient with diabetes for gender, age and residency. In particular, in both groups men were 51% and age was 69±15 years (mean±SD).
Drugs
As many as 96% of diabetic subjects received the prescription of a drug in year 2018 whereas the proportion was 74% in subjects without diabetes (p<0.001). Remarkably, the average number of drug packages prescribed in the year was 74±0.06 vs 31±0.04 (mean±SE), respectively, in the two groups (p<0.001), that is, twofold higher in diabetic subjects.
As many as 89% of diabetic subjects (n=619 849) received a prescription of an antihyperglycemic drug. Among them, 26% (n=161 085) were prescribed insulin and 88% (n=545 391) oral or injectable non-insulin medications, with (n=83 453) or without (n=461 276) an insulin prescription. Among subjects not treated with insulin (n=461 276), 316 675 (69%) were prescribed a single drug (monotherapy), 112 379 (24%) were prescribed two drugs (dual therapy, sometimes in a fixed combination pill) and 32 222 (7%) were prescribed three or more non-insulin drugs. Providing more details on antihyperglycemic drugs is beyond the scope of this paper.
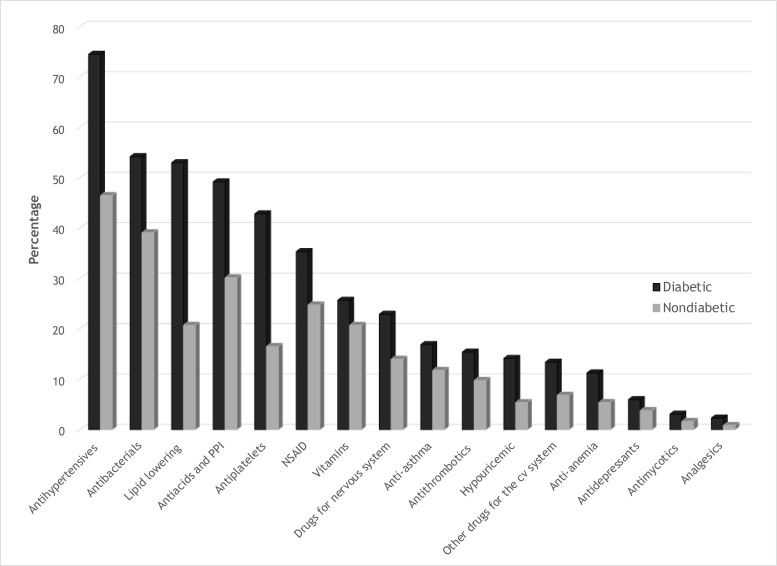
As shown in figure 2, diabetic subjects received more prescriptions of almost all drugs different from antihyperglycemic ones (any class +30%). In particular, ranking the Anatomical Therapeutic Chemical (ATC) classes, they received more prescriptions of analgesic +166%, hypouricemic +161%, lipid lowering +153%, antiplatelets +152%, antianemia +107%, other drugs for the cardiovascular system +95%, antimycotic +84%, drugs for nervous system +62%, antiacids and proton-pump inhibitors +61%, antihypertensive +59%, antithrombotic +55%, antidepressant +55%, antiasthma +42%, non-steroidal anti-inflammatory +41%, and antibiotics +37% (all comparisons p<0.001).
Figure 2.
Percentage of subjects receiving a prescription of drugs belonging to various Anatomical Therapeutic Chemical (ATC) classes (all comparisons p<0.001). cv, cardiovascular; NSAID, non-steroidal anti-inflammatory drug; PPI, proton-pump inhibitor.
Outpatient consultations, laboratory tests and imaging
As many as 83% of diabetic subjects received a prescription of at least one specialist consultation or diagnostic exam (laboratory test, imaging), or a therapeutic or rehabilitative procedure as outpatients, whereas the proportion was 69% in subjects without diabetes (p<0.001), with an average of 42±0.15 vs 29±0.1 (mean±SE) prescriptions in the two groups, respectively (p<0.001).
Subjects with diabetes received more prescriptions of specialist consultation visits of any type (+50%). Laboratory testing (+37%), ultrasonography (+48%), CT scan (+27%), MRI (+8%), standard radiography (+12%), histopathological assessment (+18%) and rehabilitation program (+76%) prescriptions were also more frequent in diabetic subjects (all p<0.001). Among laboratory tests, patients with diabetes received more frequently prescriptions of any type of blood or urine test and not necessarily only of those more directly related to diabetes monitoring (glucose, HbA1c, lipids, creatinine, microalbuminuria). As an example, they received more prescriptions of urate (+72%), aspartate aminotransferase (+72%), gamma-glutamyl transferase (+50%), ferritin (+34%), blood cell count (+32%), sodium (+32%), potassium (+32%), calcium (+27%), thyroid-stimulating hormone (+23%), and vitamin D (+8%) (p<0.001 for all comparisons).
Hospital admissions and discharges
Diabetic subjects admitted to hospital (ordinary hospitalization; day hospital excluded) were 14.1% vs 6.9% in non-diabetic subjects (p<0.001). The corresponding rates were 235 vs 99 per 1000 persons, respectively (p<0.001). Rates of admission to day hospital were 32 vs 21 per 1000 persons, respectively (p<0.001). Average number of admissions in those admitted was 1.6±0.002 (mean±SE) in diabetic subjects and 1.4±0.001 in non-diabetic subjects (p<0.001). The average duration of hospital stay was 11.3±0.02 days (mean±SE) in those with diabetes and 9.9±0.02 days in those without diabetes (p<0.001). Noteworthy, diabetic subjects admitted to hospital for an ordinary stay (day hospital excluded) were 98 369 but only 51 085 (52%) had diabetes mentioned in their discharge medical reports.
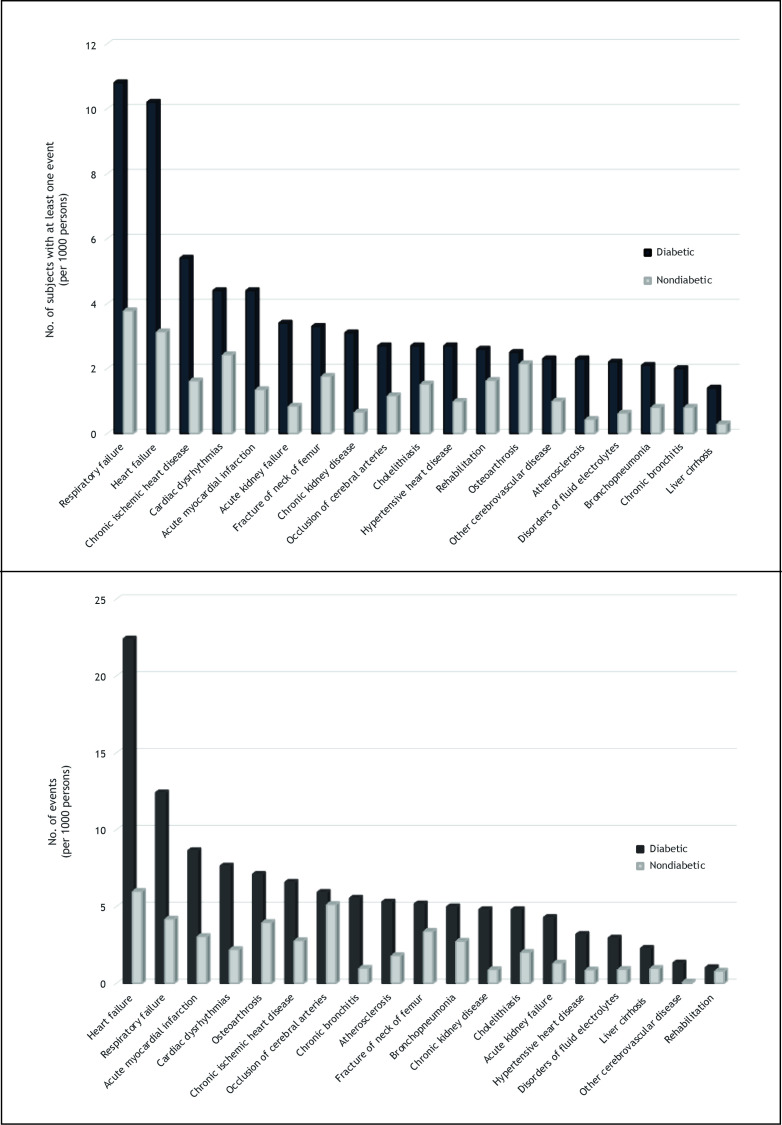
Figure 3 illustrates rates of discharges from (and therefore admission to) hospital in diabetic and non-diabetic subjects for diseases most frequently listed as primary diagnosis in the discharge medical reports. Several clinical manifestations of cardiovascular disease are among them but also kidney diseases, pulmonary diseases, gastrointestinal disease and bone diseases occurred frequently. Remarkably, all these rates were definitely higher in diabetic than in non-diabetic subjects (p<0.001). Quite often these rates were twofold higher or more in the presence of diabetes.
Figure 3.
Upper panel: number of subjects with at least one primary diagnosis of selected diseases in discharge medical reports. Lower panel: cumulative number of events (primary diagnosis of selected diseases in discharge medical reports). Data are presented per 1000 subjects with or without diabetes. All comparisons p<0.001.
The most common DRG code was heart failure/shock (n=10 490 discharges), followed by respiratory failure/pulmonary edema (n=9827) and kidney failure (n=5610). Among the top 20 DRG codes almost half (n=8) pertained to cardiovascular diseases, collectively accounting for 22% of all discharges. Remarkably, diabetes was not among the most common (No 18 in the ranking) and represented less than 1% of all DRG codes. This means that poorly controlled diabetes was rarely the cause of a hospital admission.
Consistent data were found when we calculated the cumulative number of events per 1000 persons. In this analysis the most frequent primary diagnosis was heart failure and other cardiovascular diseases ranked in the top 10. Also in this analysis, pulmonary, kidney, gastrointestinal and bone diseases occurred more commonly in sex, age and residency-matched subjects with diabetes (figure 3).
Sensitivity analyses were carried out after stratification of subjects according to age <65 or ≥65 years. This analysis confirmed the differences in drug prescriptions (pool of all ATC categories with the exception of antihyperglycemic drugs), outpatient diagnostic and therapeutic procedures (pool of all codes) and hospital admissions (any diagnosis) with higher figures in subjects with diabetes. Interestingly, the differences between subjects with and without diabetes were even more striking in younger subjects: drug prescriptions 50.2 vs 13.5 packages per year (p<0.001), diagnostic and therapeutic prescriptions 40.6% vs 23.1% exams or procedures per year (p<0.001), hospital admissions (ordinary and day hospital) 182 vs 70 per 1000 persons (p<0.001). In older subjects with and without diabetes the corresponding figures were: drugs 86.1% vs 39.3% (p<0.001), diagnostic and therapeutic prescriptions 44.1% vs 28.8% (p<0.001), hospital admission 307 vs 145 per 1000 person-years (p<0.001).
Costs for medical services
We compared costs for medical services delivered to subjects with and without diabetes (table 2). Rather than true cost, these should be regarded as prices (or fees). The DRG reimbursement methodology suffers from some limitation. In fact, despite the longer stay (+1.4 day), the mean DRG reimbursement for hospital admission was almost identical in subjects with and without diabetes (€4653 vs €4610). With this limitation in mind, the overall cost of medical services delivered to diabetic subjects was more than twofold higher. It amounted to €2833 as compared with €1268 in non-diabetic subjects. With the exception of the cost of devices, which are diabetes-specific, all costs were higher in subjects with diabetes: costs of drugs and hospital admissions were more than twofold higher, the cost for outpatient consultations and diagnostic/therapeutics was almost twofold higher. Among the costs of drugs, 22% were attributable to antihyperglycemic agents and 78% to any other drug. Therefore, even after restricting the comparison to non-diabetes-specific drugs, the cost attributable to drugs was definitely higher in subjects with versus without diabetes. The cost of hospital admissions represented 40% of overall costs, non-diabetes-specific drugs summed up to 31%, outpatient visits and diagnostic/therapeutics to 16%, antihyperglycemic drugs to 9%, and devices for diabetes to 4%.
Table 2.
Overall and specific costs in diabetic and non-diabetic subjects (in euros per subject in year 2018)
| Expense items | Diabetes (n=697 208) |
No diabetes (n=697 208) |
| Overall | €2833 | €1268 |
| All medications | €1116 (39.4%) |
€498 (39.3%) |
| Antihyperglycemic drugs | €249 (8.8%) |
€0 |
| Other drugs | €867 (30.6%) |
€498 (39.3%) |
| Devices (strips, lancets, needle, syringes) | €98 (3.4%) |
€0 |
| Outpatient care (exams, visits) | €467 (16.5%) |
€273 (21.5%) |
| Hospital care | €1152 (40.7%) |
€497 (39.2%) |
Percent of total cost is given in parenthesis. All differences p<0.001.
Discussion
Data presented in this paper depict the burden of diabetes in Italy by analyzing prevalence and healthcare resource utilization. Also differences between diabetic and non-diabetic populations are reported to emphasize how the presence of diabetes is associated with utilization of medical resources. A short description of the public health system in Italy and some considerations on how the ARNO Observatory might represent the entire country are instrumental to better understand the robustness of our data and the validity of our conclusions.
In Italy, each resident is registered with a single general practitioner (GP) (or family physician). No claim is produced for visits delivered by these family physicians. Only outpatient consultations delivered by specialist physicians working within the frame of the NHS yield claims. The same holds true for laboratory tests, imaging and other diagnostic or therapeutic procedures: only those prescribed by physicians working for the NHS in primary, secondary or tertiary care yield administrative claims, which are recorded by LHDs. Medical services delivered outside the frame of the NHS are not scrutinized in this study but they are a small fraction of total (about 10%).20
The number of subjects belonging to this very large database, which is fed by data collected in several regions of North, Center and South of Italy, corresponds approximately to 19% of people living in Italy in 2018,21 and therefore might be taken to represent the entire country, both in terms of prevalence and of resource use. Accordingly, the prevalence of diabetes we found in this very large database (ie, 6.2%) could be considered the most recent and robust information on prevalence of known diabetes in Italy. Interestingly, this prevalence is similar to the one observed in the ARNO Diabetes Observatory in years 2016 (6.3%) and 2014 (6.2%). This suggests that in Italy the prevalence of diabetes has probably reached a plateau, after a remarkable increase in the last 30 years.7 9 11 17 22 This is consistent with recent data from the USA and other Western countries.23 24 An explanation might be that a great effort was made in recent years in Western countries in order to identify cases of unknown diabetes and that the efficiency in detecting unknown diabetes reached a plateau. It should be noted, however, that this prevalence is probably a slight underestimate because a number of patients who are treated with diet only might not be in the list of those exempted for diabetes or might not be admitted to hospital in year 2018 (or, if admitted, the mention of diabetes might be missed). These subjects, however, are not expected to contribute substantially to diabetes prevalence. In fact, the prevalence of this ‘known but undetected’ diabetes should not exceed 5%–10% of total cases and therefore should minimally increase the overall prevalence of the disease. Therefore, it seems reasonably to conclude that in Italy (61 million of inhabitants) as many as 4 million people have diabetes, being aware of the disease.
For the reasons stated above, we feel that diabetic subjects identified in this study are reasonably representing diabetic subjects living in Italy. Therefore, their use of medical resources we described should be reasonably taken as the use of medical resources occurring in people with diabetes living in Italy, allowing a robust and reliable extrapolation to the entire country. Previous publications examined only subjects living in specific areas of Italy and/or focused on particular aspects of healthcare, with the major emphasis for costs.7–17
Almost 90% of diabetic subjects were treated with antihyperglycemic drugs and most of them also with other drugs. Remarkably, the use of drugs different from antihyperglycemic agents was definitely higher in diabetic than in non-diabetic subjects. Interestingly, these differences were observed also for drugs used for clinical conditions which are generally not considered a common finding in diabetes. This supports the concept that these conditions might be reasonably regarded as true complications of diabetes rather than just comorbidities. Noteworthy, the cost attributable to drugs different from antihyperglycemic agents was almost fourfold higher than the cost for antihyperglycemic drugs. Remarkably, the cost of drugs different from antihyperglycemic agents was almost twofold higher in subjects with diabetes.
The burden of diabetes is only modestly related to devices and drugs needed to control hyperglycemia or to treat acute and chronic complications. A substantial burden is represented by diagnostic and therapeutic procedures of outpatients and, most importantly, by hospital admissions. Many outpatient exams (laboratory, imaging) and specialist consultations were prescribed more frequently to diabetic subjects, and hospital admissions for most diseases were more common in subjects with diabetes. Noteworthy, several outpatient diagnostic and therapeutic procedures were not diabetes-specific and many admissions were generated by clinical conditions which are not generally listed among acute or chronic complications of diabetes. This further supports the concept that the list of diabetic complications might be definitely longer than the classic one, which includes cardiovascular disease, retinopathy, nephropathy, neuropathy and diabetes foot. Most, if not all, diseases occurred more frequently in diabetic than in non-diabetic subjects, requiring specific drugs, diagnostic procedures, outpatient follow-up and also hospital care. This is consistent also with data concerning the causes of death in diabetes in Italy and worldwide which quite often cannot be attributed to classic complications of the disease.25–28 In the past, diabetes was defined ‘a cardiovascular disease’29 but our data strongly support the concept that it could be indeed regarded as a ‘systemic disease’.
According to our data, the standard diabetes care, that is, antihyperglycemic drugs, diabetes-specific devices, outpatient consultations in diabetes clinics, and laboratory exams recommended for diabetes monitoring (HbA1c, blood glucose and lipid profile) collectively accounts for not more than 15% of costs. This proportion might be reduced to approximately 10% when considering that cost of hospital admissions of diabetic subjects is underestimated by the DRG reimbursement system because the duration of hospital stay is generally longer in the presence of diabetes than, for the same DRG, in the absence of diabetes. Therefore, the large proportion (85%–90%) of costs is attributable to chronic complications (including those which are generally regarded as comorbidities). The average cost of healthcare provided to diabetic subjects in 2018 (€2833) was definitely lower than the one calculated for patients living in Turin in 2003 (€3660),10 but higher than the one estimated for patients living in the Marche Region in 2008–2011 (€2318).16 In previous studies based on the ARNO Diabetes Observatory the overall cost ranged from €2589 in 20069 to €2791 in 2012,17 consistent with a modest trend to increase across years.
Considering the prevalence of the disease (6.2%), the number of affected people (around 4 million with known diabetes) and the individual cost (€2833), it turns out that diabetes care costs approximately €11 billion per year to the Italian NHS. This enormous amount of money, which is reasonably an underestimate because of the limits of the DRG reimbursement system, corresponds to 10% of the annual budget of the Italian NHS (€111 billion in year 2018).30 The burden of the disease is even greater when taking into account also direct personal costs (fee for private healthcare, copayments in not exempted subjects, income loss due to the disease, cost for assistance of not self-sufficient relatives with diabetes, and so on) and indirect social costs (eg, absenteeism, anticipated retirements, disability allowance, other public supports). These further costs were estimated to be collectively equivalent if not superior to the costs sustained by public health systems.31 32
The strengths of this population-based study are the extremely large number of subjects included and living in North, Center and South of Italy, which suggests the possibility to extrapolate our results to the entire country, the completeness in the collection of administrative claims from different sources, which allows to explore all aspects of medical resources used, the possibility to compare very large population-based samples of subjects with and without diabetes, and the timeliness of data presented which were collected in year 2018.
A potential limit of this study might be the lack of information on clinical aspects of diabetic subjects. However, the scope of this research was to investigate the burden of the disease and not the association between some clinical features (eg, HbA1c) and use of medical resources.
Another potential limit of this study, and of most studies based on administrative claims, might be the lack of a validation of the methodology used in case identification.33 However, a comprehensive and unquestionable validation is hard to implement. A validation by comparing administrative claims with lists of subjects attending diabetes clinics was recently successful34 but it excluded subjects not receiving secondary/tertiary care. A comparison of administrative claims with the medical records of GPs, searching for diabetes cases, would be more complete and appropriate. However, in a previous experience we found that this approach can be fallacious because lists of diabetic subjects provided by GPs did not include as many as 10% of subjects receiving prescriptions of antidiabetic medications.35 In this study, we used three sources of administrative claims and previous publications concluded that the three-source approach seems to be the most reliable.36 37
In conclusion, the burden of diabetes in Italy, which could be taken to well represent Western Europe, is very heavy and it is even heavier in younger people. Diabetes care is a true challenge for individuals, their families and the public health systems. Acute and chronic diseases occurring more frequently in people with diabetes are not limited to clinical manifestations of classic macrovascular and microvascular complications but they encompass virtually any kind of pathologic disorders. In this respect, diabetes might be regarded as a systemic (‘all-in’) disease. Standard care represents only 10%–15% of costs whereas medical services due to acute and chronic complications account for up to 85%–90% of costs. Therefore, a great effort should be devoted to an effective prevention of classic and non-classic clinical manifestations of diabetes and associated disorders. The best practice in diabetes care currently recommended by national and international guidelines should be extensively implemented in order to alleviate this burden.
Acknowledgments
The authors acknowledge the precious collaboration of the representatives of the LHDs contributing to the ARNO Observatory: R Roni (Trento), A De Marco (Dolomiti), S Zardo (Serenissima), E Salvatico (Veneto Orientale), A Ferrarese (Polesana), AM Grion (Euganea), M Giardino (Pedemontana), A Maroni (Berica), L Mezzalira (Scaligera), T Brocca (Florence), R Di Turi (Rome 3), I Senesi (Teramo), G La Bella (Naples 1), R Moscogiuri (Taranto). The authors thank the following members of the Research and Health Foundation: L Dondi, G Ronconi, A Pedrini, C Piccinni, S Calabria and A Maggioni.
Footnotes
Contributors: EB, SC and ER researched data and wrote the manuscript. GM, RM, OV, GPF and NM reviewed and edited the manuscript.
Funding: The Italian Diabetes Association is gratefully acknowledged for funding.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. All data relevant to the study are included in the article. All data are stored in an anonymized database at CINECA, Bologna, Italy.
References
- 1.World Health Organization Global report on diabetes. Geneva, Switzerland: WHO press, 2016. https://www.who.int/diabetes/global-report/en/ [Google Scholar]
- 2.International Diabetes Federation IDF diabetes atlas. 9 edn Brussels, Belgium, 2019. http://www.diabetesatlas.org [Google Scholar]
- 3.Carey IM, Critchley JA, DeWilde S, et al. . Risk of infection in type 1 and type 2 diabetes compared with the general population: a matched cohort study. Diabetes Care 2018;41:513–21. 10.2337/dc17-2131 [DOI] [PubMed] [Google Scholar]
- 4.Harding JL, Pavkov ME, Magliano DJ, et al. . Global trends in diabetes complications: a review of current evidence. Diabetologia 2019;62:3–16. 10.1007/s00125-018-4711-2 [DOI] [PubMed] [Google Scholar]
- 5.Peter P, Lipska K. The rising cost of diabetes care in the USA. Lancet Diabetes Endocrinol 2016;4:479–80. 10.1016/S2213-8587(15)00519-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bommer C, Sagalova V, Heesemann E, et al. . Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care 2018;41:963–70. 10.2337/dc17-1962 [DOI] [PubMed] [Google Scholar]
- 7.Brocco S, Visentin C, Fedeli U, et al. . Monitoring the occurrence of diabetes mellitus and its major complications: the combined use of different administrative databases. Cardiovasc Diabetol 2007;6:5–15. 10.1186/1475-2840-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gnavi R, Karaghiosoff L, Costa G, et al. . Socio-economic differences in the prevalence of diabetes in Italy: the population-based Turin study. Nutr Metab Cardiovasc Dis 2008;18:678–82. 10.1016/j.numecd.2007.11.004 [DOI] [PubMed] [Google Scholar]
- 9.Marchesini G, Forlani G, Rossi E, et al. . The direct economic cost of pharmacologically-treated diabetes in Italy-2006. The ARNO observatory. Nutr Metab Cardiovasc Dis 2011;21:339–46. 10.1016/j.numecd.2009.10.009 [DOI] [PubMed] [Google Scholar]
- 10.Bruno G, Picariello R, Petrelli A, et al. . Direct costs in diabetic and non diabetic people: the population-based Turin study, Italy. Nutr Metab Cardiovasc Dis 2012;22:684–90. 10.1016/j.numecd.2011.04.007 [DOI] [PubMed] [Google Scholar]
- 11.Monesi L, Baviera M, Marzona I, et al. . Prevalence, incidence and mortality of diagnosed diabetes: evidence from an Italian population-based study. Diabet Med 2012;29:385–92. 10.1111/j.1464-5491.2011.03446.x [DOI] [PubMed] [Google Scholar]
- 12.Bruno G, Bonora E, Miccoli R, et al. . Quality of diabetes care in Italy: information from a large population-based multiregional observatory (ARNO diabetes). Diabetes Care 2012;35:e64. 10.2337/dc12-0765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Valent F, Tillati S, Zanier L. Prevalence and comorbidities of known diabetes in northeastern Italy. J Diabetes Investig 2013;4:355–60. 10.1111/jdi.12043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Degli Esposti L, Saragoni S, Buda S, et al. . Glycemic control and diabetes-related health care costs in type 2 diabetes; retrospective analysis based on clinical and administrative databases. Clinicoecon Outcomes Res 2013;5:193–201. 10.2147/CEOR.S41846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bruno G, Pagano E, Rossi E, et al. . Incidence, prevalence, costs and quality of care of type 1 diabetes in Italy, age 0-29 years: the population-based CINECA-SID ARNO Observatory, 2002-2012. Nutr Metab Cardiovasc Dis 2016;26:1104–11. 10.1016/j.numecd.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 16.Marcellusi A, Viti R, Sciattella P, et al. . Economic aspects in the management of diabetes in Italy. BMJ Open Diabetes Res Care 2016;4:e000197. 10.1136/bmjdrc-2016-000197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pagano E, De Rosa M, Rossi E, et al. . The relative burden of diabetes complications on healthcare costs: the population-based CINECA-SID ARNO diabetes Observatory. Nutr Metab Cardiovasc Dis 2016;26:944–50. 10.1016/j.numecd.2016.05.002 [DOI] [PubMed] [Google Scholar]
- 18.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3 edn Wolters Kluver, Lippincot: Williams & Wilkins, 2008. [Google Scholar]
- 19.ICD-9-CM International classification of diseases, 9th revision,, 2002. Available: http://www.salute.gov.it [Accessed 9 Dec 2019].
- 20.Centre for Research on Health and Social Care Management (CERGAS) Private health care consumption in Italy - executive summary OCPS report. Available: http://www.cergas.unibocconi.eu/wps/wcm/connect/cdr/cergas/home/observatories/ocps [Accessed 9 Dec 2019].
- 21.National Institute of Statistics National demographic balance of year, 2018. Available: https://www.istat.it/it/files//2019/07/Bilancio-demografico_anno-2018_EN.pdf [Accessed 15 Dec 2019].
- 22.Gnavi R, Migliardi A, Maggini M, et al. . Prevalence of and secular trends in diagnosed diabetes in Italy: 1980-2013. Nutr Metab Cardiovasc Dis 2018;28:219–25. 10.1016/j.numecd.2017.12.004 [DOI] [PubMed] [Google Scholar]
- 23.Benoit SR, Hora I, Albright AL, et al. . New directions in incidence and prevalence of diagnosed diabetes in the USA. BMJ Open Diabetes Res Care 2019;7:e000657. 10.1136/bmjdrc-2019-000657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Magliano DJ, Islam RM, Barr ELM, et al. . Trends in incidence of total or type 2 diabetes: systematic review. BMJ 2019;366:l5003. 10.1136/bmj.l5003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Marco R, Locatelli F, Zoppini G, et al. . Cause-specific mortality in type 2 diabetes. The Verona diabetes study. Diabetes Care 1999;22:756–61. 10.2337/diacare.22.5.756 [DOI] [PubMed] [Google Scholar]
- 26.Zoppini G, Fedeli U, Gennaro N, et al. . Mortality from chronic liver diseases in diabetes. Am J Gastroenterol 2014;109:1020–5. 10.1038/ajg.2014.132 [DOI] [PubMed] [Google Scholar]
- 27.Zoppini G, Fedeli U, Schievano E, et al. . Mortality from infectious diseases in diabetes. Nutr Metab Cardiovasc Dis 2018;28:444–50. 10.1016/j.numecd.2017.12.007 [DOI] [PubMed] [Google Scholar]
- 28.Rao Kondapally Seshasai S, Thompson A, Thompson A, et al. . Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 2011;364:829–41. 10.1056/NEJMoa1008862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Candido R, Srivastava P, Cooper ME, et al. . Diabetes mellitus: a cardiovascular disease. Curr Opin Investig Drugs 2003;4:1088–94. [PubMed] [Google Scholar]
- 30.Gazzetta Ufficiale della Repubblica Italiana Ripartizione del fondo sanitario nazionale. Available: http://www.regioni.it/news/2019/02/28/riparto-fondo-sanitario-nazionale-2018-delibera-cipe-28-11-2018-gazzetta-ufficiale-n-49-del-27-febbraio-2019-595365/ [Accessed 15 Dec 2019].
- 31.Marcellusi A, Viti R, Mecozzi A, et al. . The direct and indirect cost of diabetes in Italy: a prevalence probabilistic approach. Eur J Health Econ 2016;17:139–47. 10.1007/s10198-014-0660-y [DOI] [PubMed] [Google Scholar]
- 32.Kanavos P, van den Aardweg P, Shurer W. Diabetes expenditure, burden of disease and management in 5 EU countries. LSE Health, London School of Economics, 2012. [Google Scholar]
- 33.Dalla Zuanna T, Pitter G, Canova C, et al. . A systematic review of case-identification algorithms based on Italian healthcare administrative databases for two relevant diseases of the endocrine system: diabetes mellitus and thyroid disorders. Epidemiol Prev 2019;43:17–36. 10.19191/EP19.4.S2.P008.089 [DOI] [PubMed] [Google Scholar]
- 34.Longato E, Di Camillo B, Sparacino G, et al. . Diabetes diagnosis from administrative claims and estimation of the true prevalence of diabetes among 4.2 million individuals of the Veneto region (North East Italy). Nutr Metab Cardiovasc Dis 2020;30:84–91. 10.1016/j.numecd.2019.08.017 [DOI] [PubMed] [Google Scholar]
- 35.Muggeo M, Verlato G, Bonora E, et al. . The Verona diabetes study: a population-based survey on known diabetes mellitus prevalence and 5-year all-cause mortality. Diabetologia 1995;38:318–25. 10.1007/BF00400637 [DOI] [PubMed] [Google Scholar]
- 36.Bruno G, LaPorte RE, Merletti F, et al. . National diabetes programs. Application of capture-recapture to count diabetes? Diabetes Care 1994;17:548–56. 10.2337/diacare.17.6.548 [DOI] [PubMed] [Google Scholar]
- 37.Verlato G, Muggeo M. Capture-recapture method in the epidemiology of type 2 diabetes: a contribution from the Verona diabetes study. Diabetes Care 2000;23:759–64. 10.2337/diacare.23.6.759 [DOI] [PubMed] [Google Scholar]