Abstract
Background
Periodontal regeneration can change tooth prognosis and represents an alternative to extraction in teeth compromised by severe intra‐bony defects. The aim of this study was to compare periodontal regeneration (PR) with tooth extraction and replacement (TER) in a population with attachment loss to or beyond the apex of the root in terms of professional, patient‐reported and economic outcomes.
Methods
This was a 10‐year randomized controlled clinical trial. 50 stage III or stage IV periodontitis subjects with a severely compromised tooth with attachment loss to or beyond the apex were randomized to PR or TER with either an implant‐ or a tooth‐supported fixed partial denture. Subjects were kept on a strict periodontal supportive care regimen every 3 months and examined yearly. Survival and recurrence analysis were performed.
Results
88% and 100% survival rates were observed in the PR and TER groups. Complication‐free survival was not significantly different: 6.7–9.1 years for PR and 7.3–9.1 years for TER (p = .788). In PR, the observed 10‐year attachment gain was 7.3 ± 2.3 mm and the residual probing depths were 3.4 ± 0.8 mm. Recurrence analysis showed that the 95% confidence interval of the costs was significantly lower for PR compared with TER throughout the whole 10‐year period. Patient‐reported outcomes and oral health‐related quality‐of‐life measurements improved in both groups.
Conclusions
Periodontal regeneration can change the prognosis of hopeless teeth and is a less costly alternative to tooth extraction and replacement. The complexity of the treatment limits widespread application to the most complex cases but provides powerful proof of principle for the benefits of PR in deep intra‐bony defect.
Keywords: dental implants, fixed partial dentures, health economics, periodontal regeneration, randomized controlled clinical trial, recurrence analysis, survival analysis
Clinical Relevance.
Scientific rationale for the study: The boundaries of periodontal regeneration as a tool to change the prognosis of severely compromised teeth are unclear and so is its cost‐effectiveness compared with the treatment alternative represented by extraction and tooth replacement with a fixed partial denture.
Principal findings: Periodontal regeneration in the context of complex inter‐disciplinary treatment led to large amounts of clinical attachment‐level gains and 88% tooth survival over a 10‐year period. Survival and complication‐free survival were similar for regenerated teeth and for extraction and tooth replacement. Periodontal regeneration was more cost‐effective. Sustained improvements in patient‐reported outcomes and quality‐of‐life measures were observed for both groups.
Practical implications: Periodontal regeneration is the treatment of choice for compromised teeth with deep vertical intra‐bony defects. More research by additional groups should confirm the results obtained for “hopeless teeth.”
1. INTRODUCTION
Periodontal regeneration of intra‐bony defects is a highly predictable treatment modality that enables long‐term maintenance of severely compromised teeth in subjects with well‐controlled stage III and stage IV periodontitis (Cortellini & Tonetti, 2004). Over the years, the introduction of novel, biologically guided surgical approaches and biomaterials has resulted in a continuous expansion of the indications in terms of severity and morphology of the defects. A recent 20‐year follow‐up of a randomized controlled clinical trial has shown the long‐term health benefits and lower cost of managing periodontal recurrence of regeneration compared with access flap treatment (Cortellini, Buti, Pini Prato, & Tonetti, 2017). In the quest to expand the application of regeneration to the retention of teeth with complex and severe periodontal breakdown reaching the apex, we have designed a randomized clinical trial comparing the clinical and economic outcomes of regeneration with tooth extraction and appropriate prosthetic replacement (Cortellini, Stalpers, Mollo, & Tonetti, 2011). The 5‐year follow‐up has indicated that highly relevant attachment‐level gains can be achieved in teeth with a hopeless prognosis along with resolution or drastic reductions in tooth hypermobility. These improvements led to the possibility to retain 92% of teeth with hopeless prognosis beyond the one‐year follow‐up. The study also documented in the control group the complexity of tooth replacement with both implant‐ and tooth‐supported fixed partial prostheses.
The present manuscript reports the 10‐year outcomes of the study and (a) documents the stability of the regenerated clinical attachment‐level gain and shallow probing pocket depths in the test group; (b) compares survival, complication‐free survival and expected mean cumulative cost of recurrence between regeneration of hopeless teeth and their replacement with implant‐ or tooth‐retained fixed partial dentures; and (c) describes oral health‐related quality of life and patient‐centred outcomes.
2. MATERIALS AND METHODS
2.1. Study Design
This manuscript reports the 10‐year follow‐up of a parallel group, independent examiner, randomized controlled clinical trial comparing clinical, patient‐centred and economic outcomes of periodontal regeneration with extraction and replacement of teeth with “hopeless periodontal prognosis.” The test arm was also designed to explore the potential of periodontal regenerative therapy in changing the prognosis of hopeless teeth. The original population and study design have been described in the 5‐year report (Cortellini et al., 2011). In brief, 50 subjects with stage III or stage IV periodontitis (Tonetti, Greenwell, & Kornman, 2018) presenting with at least a tooth with a deep intra‐bony component and CAL/bone loss extending to or beyond the apex or a chronic perio‐endo lesion but with clearly detectable peaks of attachment/alveolar bone at the adjacent teeth were enrolled. Inclusions and exclusions criteria have been reported in detail. Subjects were randomly assigned to either test (periodontal regeneration) or control (extraction and tooth replacement) using computer‐generated codes and random permuted blocks with a block size of 4 and minimization for cigarette smoking (<20/day) to ensure balanced groups. The study was approved by the ATRO (Accademia Toscana di Ricerca Odontostomatologica) ethical board on 27 April 1998 and performed in accordance with the Helsinki Declaration on experimentation involving human subjects. All participants gave informed consent. Sample size was based on logistic considerations given the pilot nature of the study. Subjects were recruited between June 1998 and June 2003. All 10‐year patient follow‐up was completed by the end of 2014. The study is registered on Clincialtrials.gov (NCT04227964).
2.2. Initial assessment and pre‐treatment
All teeth were assessed in the context of a full periodontal examination and diagnosis. Given the complexity of the local condition characterized by high degrees of tooth hypermobility, migration and the possible presence of perio‐endo lesions as a consequence of retrograde pulpitis, teeth were frequently splinted to control hypermobility. Root canal treatment was performed for teeth with necrotic pulp and for vital teeth whenever instrumentation of the root apex was expected during the regenerative surgery. All subjects received a cycle of cause‐related periodontal therapy consisting of behavioural modification, risk factor control and root debridement with or without systemic antibiotic therapy (amoxicillin 500 mg tid and metronidazole 500 mg tid for 7 days).
2.3. Study interventions
Test subjects received periodontal regenerative microsurgery (Cortellini & Tonetti, 2001) consisting of papilla preservation flaps (Cortellini, Prato, & Tonetti, 1995, 1999) and application of a regenerative material (enamel matrix derivative, non‐resorbable e‐PTFE barrier membranes, bioresorbable barrier membranes and bone replacement grafts to optimize wound stability [Cortellini & Tonetti, 2005]). Local treatment of the regenerated sites was completed after 12 months of healing, if required, with minor orthodontic tooth movement, bonding or other restorative procedures to improve both function and aesthetics.
Control subjects received tooth extraction and replacement with either an implant‐ or tooth‐supported fixed partial denture in the context of comprehensive treatment planning. To ensure acceptable aesthetics and function, appropriate soft‐tissue and/or hard‐tissue augmentation was performed according to standard care before implant or final bridge positioning. All surgical procedures were performed by PC.
Both test and control subjects were enrolled in a professional supportive periodontal care programme in a specialist environment with a recommended frequency of 3 months.
2.4. Outcome assessment
The primary outcome of the study was tooth or tooth replacement retention according to pre‐specified criteria. These included patient comfort, masticatory function and improvement of clinical parameters contributing to the assessment of tooth prognosis according to McGuire and Nunn (1996a, 1996b) and Kwok and Caton (2007). Secondary outcomes included the following: (a) the assessment of periodontal parameters including full‐mouth plaque score (FMPS), full‐mouth bleeding on probing (FMBS), probing pocket depths (PPDs), recession of the gingival margin (Rec), tooth mobility and assessment of tooth vitality (cold test and electric pulp testing; Cortellini, Cortellini, & Tonetti, 2019; Cortellini et al., 2011); (b) biological or technical complications at the experimentally treated teeth or at the abutments of tooth‐ or implant‐supported bridges; and (c) health economic measures. Outcomes were evaluated yearly over the 10‐year follow‐up period by a single examiner (MST) not involved in the delivery of treatment.
2.5. Definition of events for survival analyses
Tooth, implant or fixed partial denture survival was defined as its presence in a state of comfort and function. A survival analysis was performed using time to tooth loss as the event or the time of complication‐free survival (time until the first technical or biological complication requiring intervention). Biological complications were defined as CAL loss, PPD deepening or radiographic bone loss of 2 mm or more compared with the 1‐year outcome, loss of tooth vitality or onset of caries. Technical complications were defined as broken splint, bridge/abutment failure, chipped ceramic requiring replacement or repair. Patients lost to follow‐up were censored at the date of the last examination. All analyses were performed using a Kaplan–Meir method.
2.6. Definition of events and costs for recurrence analyses
Onset of complications and the cost for their management were assessed essentially as described (Cortellini et al., 2017). All complications experienced over the 10‐year follow‐up period which required treatment were included in the analysis; these included tooth loss. Their total cumulative cost was determined by the actual cost of the necessary procedures using a fee scheduled derived as an average from a representative sample of 9 practices providing periodontal care and located in different regions in Italy (Cortellini et al., 2017). The cost of composite splinting and repair was set accordingly to the same schedule at 238 Euro.
2.7. Patient‐reported outcomes
Patient preference with regard to treatment of the compromised tooth was evaluated with a questionnaire indicating the preference for maintenance of the tooth, its extraction or no preference. Patient concerns in terms of aesthetics and masticatory function were evaluated with a 5‐point Likert‐type scale at baseline, and 1, 5 and 10 years after treatment using no concern, some concern, concerned, clearly concerned and very concerned as the points in the scale. Satisfaction with treatment of the hopeless tooth was assessed at 1 year using a 5‐point Likert‐type scale with the following definitions for the points in the scale: unsatisfied, moderately satisfied, satisfied, very satisfied and extremely satisfied. Oral health‐related quality of life was assessed with a validated Italian translation of the OHIP‐14 at baseline, and 1, 5 and 10 years after treatment and with reference to the perception in the recent period (Slade, 1997; Tonetti, Cortellini, et al., 2018).
2.8. Data analysis
Data were entered in a personal computer and proofed for entry errors. The locked database was exported in SPPS and Jump format. Descriptive statistics of the periodontal clinical parameters over time are presented as means and standard deviations. Survival analyses were performed in SPPS (Version 25) using the Kaplan–Meier method. 95% confidence intervals of survival time were calculated, and the null hypothesis of equality in the survival function was assessed with the Mantel–Cox log‐rank test. Recurrence analyses were performed in Jump (Version 14.3). Mean cumulative costs for the treatment of recurrences (biological/technical complications and tooth loss) were expressed in Euro and calculated yearly. The analysis takes into account both the actual occurrence of the event and censoring. 95% confidence intervals of the mean cumulative costs over the 10‐year follow‐up were plotted. All statistical comparisons were conducted at the 0.05 level of significance.
3. RESULTS
3.1. Subject accountability
A total of 50 subjects were enrolled in the study. Baseline characteristics and lack of significant differences in the test and control groups have been included in the 5‐year report of the study. Three subjects in the test group exited the study due to extraction of the experimental tooth (2 at year 1 for inadequate improvement following regeneration, and 1 at year 8 due to trauma on the experimental tooth). Four subjects (2 in the test and 2 in the control groups) were lost to follow‐up after 6 and 7 years: 3 were unavailable to continue participation and 1 subject died for study unrelated reasons.
3.2. Survival analysis
The survival curves for the test and control groups are displayed in Figure 1a. The 10‐year survival of regenerated teeth was 88%, while the 10‐year survival of implant‐ or tooth‐retained fixed partial dentures to replace the extracted teeth was 100%. There was no statistically significant difference comparing test and control treatments (p = .08, Mantel–Cox log‐rank test).
FIGURE 1.
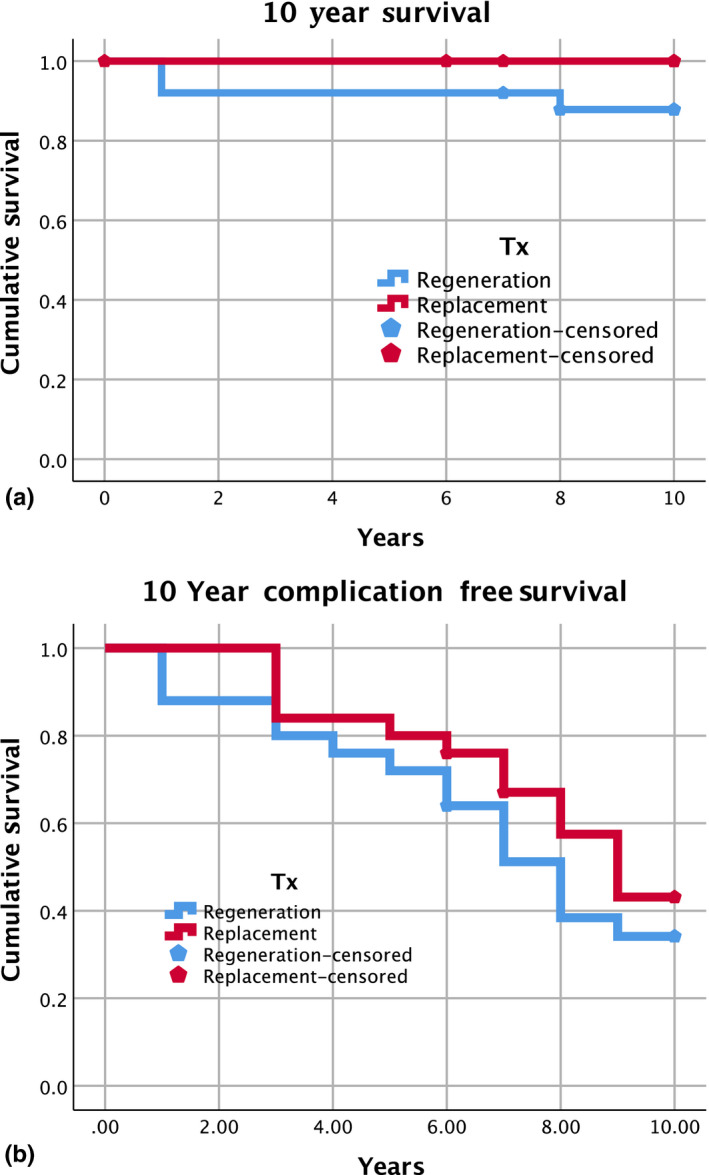
10‐year survival of regenerated teeth and tooth replacement. Kaplan–Maier 10‐year survival plot (a) and complication‐free survival plot (b) of regenerated teeth (blue line) and prosthetic tooth replacement after extraction (red line). Events and censored observations (loss to follow‐up is displayed for each curve)
Figure 1b illustrates the time until the occurrence of the first biological or technical complication. The 95% confidence interval for the complication‐free survival time was 6.7–9.1 years for the regeneration group and 7.3–9.1 years for the extraction and tooth replacement group. The difference was statistically not significant (p = .788, Mantel–Cox log‐rank test).
3.3. Stability of clinical improvements after periodontal regeneration
Table 1 shows improvements in clinical periodontal parameters and prognosis at 1‐, 5‐ and 10‐year follow‐up after regenerative periodontal surgery. No differences were observed over time for CAL gain or residual PPD after the first 12 months of healing, indicating good stability of the obtained clinical outcome in the successful cases.
TABLE 1.
Clinical improvements after periodontal regeneration and tooth prognosis in the test group (mean ± SD)
| Outcomes | 1‐year | 5‐year | 10‐year |
|---|---|---|---|
| CAL gain (mm) | 7.7 ± 2.8 | 7.6 ± 2.7 | 7.3 ± 2.3 |
| Residual PPD (mm) | 4 ± 1.7 | 3.4 ± 0.8 | 3.4 ± 0.8 |
| Tooth prognosis (hopeless/favourable) | 2/23 | 0/23 a | 0/22 b |
2 teeth with hopeless prognosis at the 1‐year follow‐up were extracted shortly thereafter.
1 tooth was extracted at year 8 as a consequence of trauma.
3.4. Recurrence analysis and cost of treatment
Figure 2a illustrates the 10‐year mean cumulative cost of recurrence for the test and control treatments. While the regeneration group seems to have greater costs at the beginning and the tooth extraction and replacement group shows more costs in the later years, substantial overlap in the 95% confidence interval exists for the whole observation period indicating that there was no significant difference in costs. The total mean cost of treatment (cost of the initial treatment and the management of the recurrences over the 10‐year observation period) is displayed in Figure 2b along with the 95% confidence interval. The total cost of treatment for the regeneration group (which includes the cost for the replacement of the 3 teeth that were lost) is significantly lower over the whole observation period.
FIGURE 2.
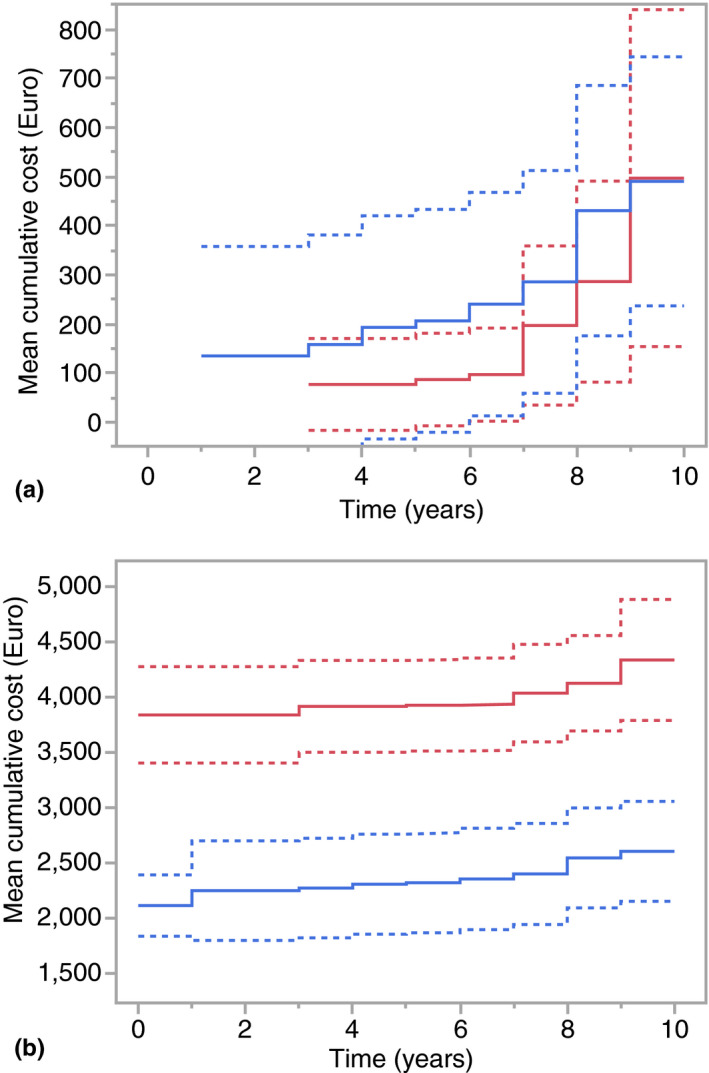
(a and b) Recurrence during the 10‐year follow‐up. Panel 2a illustrates the mean cumulative cost (Euro) of managing recurrences during the 10‐year follow‐up of regenerated teeth (blue line) and prosthetic tooth replacement (red line). Amounts do not include the initial cost of treatment and the costs of regular supportive periodontal care. The 95% confidence intervals (dashed lines) of the two groups overlap for the entire observation period. Panel 2b displays the mean cumulative cost (Euro) of initial treatment and managing recurrences during the 10‐year follow‐up of regenerated teeth (blue line) and prosthetic tooth replacement (red line). Figures do not include the costs of regular supportive periodontal care. Dashed lines represent the 95% confidence intervals
3.5. Patient‐reported outcomes
At baseline, 44 patients (88%) expressed their preference to keep their hopeless tooth, if possible. Three would have liked to have it extracted, and 3 patients did not express a preference. The formulation of the 14 questions of the OHIP‐14 questionnaire is displayed in Table 2. Baseline OHIP‐14 scores are shown in Figure 3a,b. Data show a significant impact of the oral health condition on the functional limitation, physical pain, psychological discomfort, physical disability and psychological disability domains. No differences were observed at baseline in terms of average total score (23.8 ± 3.9 vs., 24 ± 3.9 OHIP‐14 units, for test and control, respectively) or frequency of responses. 1 year after treatment, OHIP‐14 scores were 6.6 ± 2.4 for test and 11.9 ± 3 for controls. Improvements from baseline were highly significant for both groups; the inter‐group difference at 1 year was also significantly different (p = .013) with greater improvements observed in the regeneration group.
TABLE 2.
OHIP‐14 Questionnaire
| Q1 | Have you had trouble pronouncing any words because of problems with your teeth or mouth? |
| Q2 | Have you felt that your sense of taste has worsened because of problems with your teeth or mouth? |
| Q3 | Have you had painful aching in your mouth? |
| Q4 | Have you found it uncomfortable to eat any foods because of problems with your teeth or mouth? |
| Q5 | Have you been self‐conscious because of your teeth or mouth? |
| Q6 | Have you felt tense because of problems with your teeth or mouth? |
| Q7 | Has your diet been unsatisfactory because of problems with your teeth or mouth? |
| Q8 | Have you had to interrupt meals because of problems with your teeth or mouth? |
| Q9 | Have you found it difficult to relax because of problems with your teeth or mouth? |
| Q10 | Have you been a bit embarrassed because of problems with your teeth or mouth? |
| Q11 | Have you been a bit irritable with other people because of problems with your teeth or mouth? |
| Q12 | Have you had difficulty doing your usual jobs because of problems with your teeth or mouth? |
| Q13 | Have you felt that life in general was less satisfying because of problems with your teeth or mouth? |
| Q14 | Have you been totally unable to function because of problems with your teeth or mouth? |
FIGURE 3.
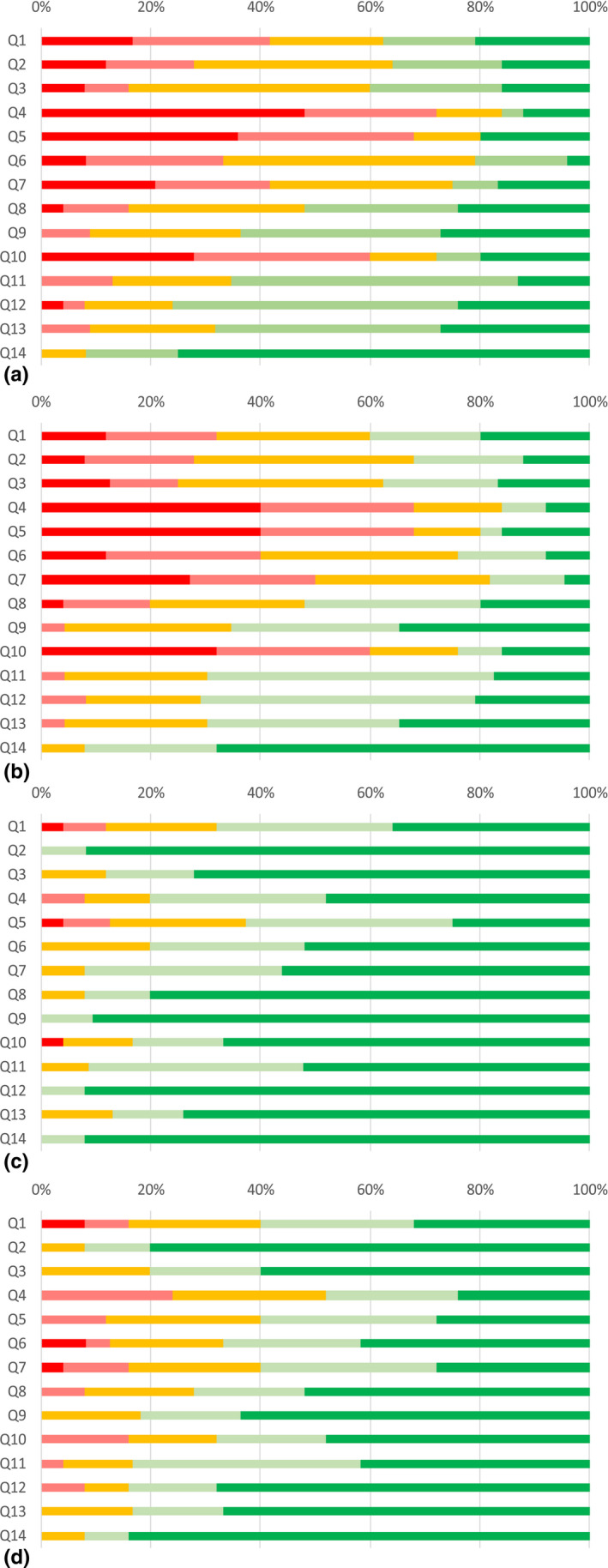
(a–d) Frequency distribution of OHIP scores group at baseline. Frequency of response for the 14 questions of the OHIP‐14 questionnaire for the regeneration group (a) and the extraction and tooth replacement group (b) at baseline and the 1‐year follow‐up (C for regeneration and D for extraction and tooth replacement groups). Colour keys: dark red = very often, light red = fairly often, yellow = occasionally, light green = hardly ever, dark green = never
At 1 year, treatment satisfaction was high for both test and control treatments with no inter‐group differences (p = .464, NS).
Likert‐scale level of concern in terms of masticatory function and aesthetics over time is illustrated in Figure 4a,b, respectively. At baseline, subjects expressed high levels of concerns for masticatory function with no significant difference between groups (p = .674, NS). One year after treatment, a highly significant decrease in the concerns for masticatory function (p < .001) was observed in both groups and the improvement was maintained over time until the 10‐year follow‐up. Interestingly, no difference was observed comparing the test and control groups at 1, 5 and 10 years (p > .1). Similar outcomes were observed for aesthetic concerns (Figure 5a,b): highly significant improvements between baseline and 1 year (p < .001) in both groups; stability in the improvement until the 10‐year follow‐up; and no difference comparing test and control over time (p > .10). Overall patient satisfaction with treatment is shown in Figure 6. No significant difference was observed between the test and control groups (p = .464).
FIGURE 4.
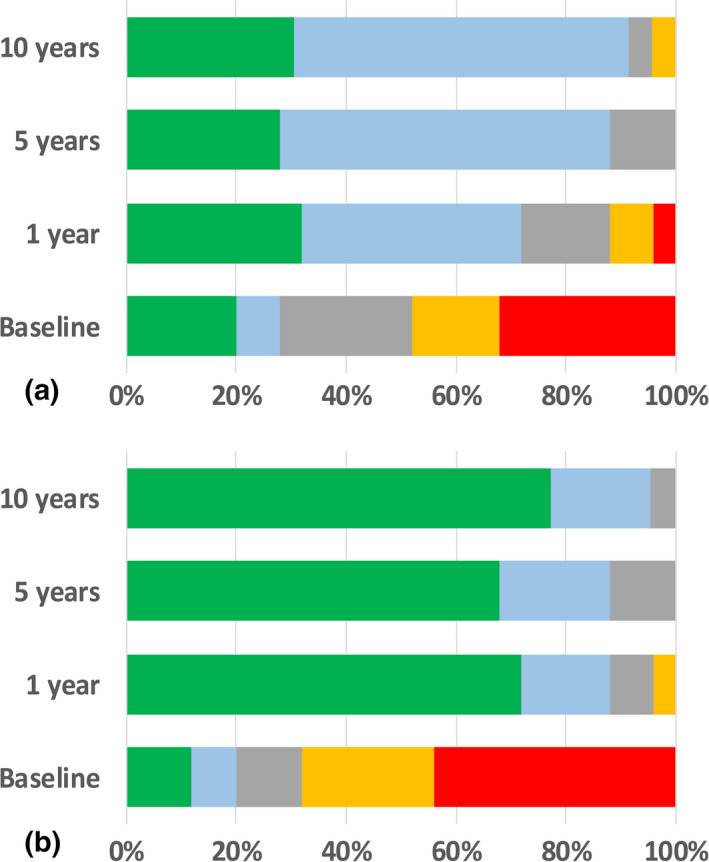
(a and b) Frequency distribution of patient‐reported outcomes in terms of concerns for masticatory function over the 10‐year observation. Data are expressed as frequency distribution of the responses across the five points of the Likert scale for the regeneration group (a) and the extraction and tooth replacement group (b). Green = no concern, light blue = some concern, grey = concerned, yellow = clearly concerned, red = very concerned
FIGURE 5.
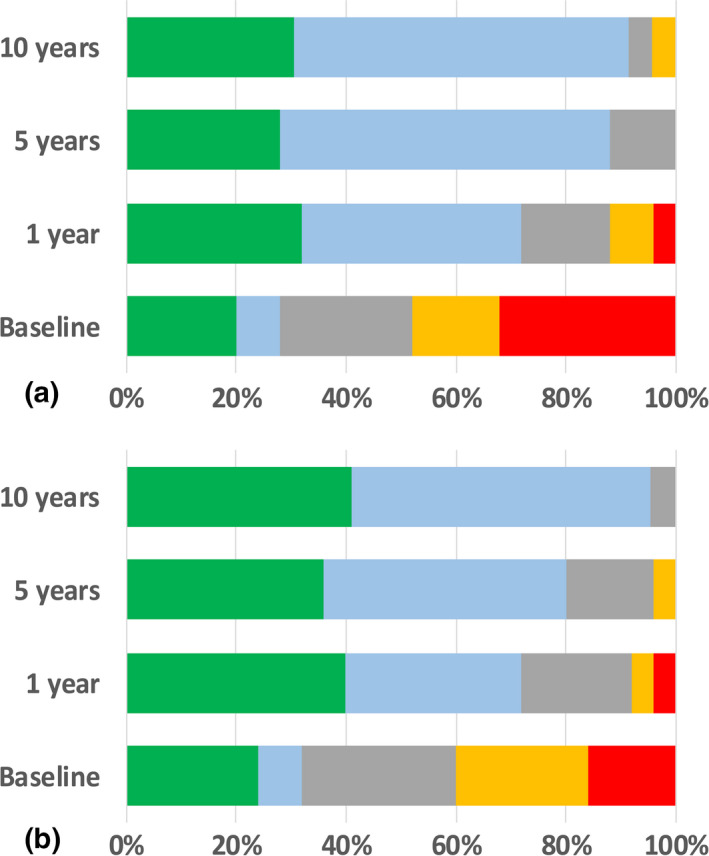
(a and b) Frequency distribution of patient‐reported outcomes in terms of concerns for aesthetics over the 10‐year observation. Data are expressed as frequency distribution of the responses across the five points of the Likert scale for the regeneration group (a) and the extraction and tooth replacement group (b). Green = no concern, light blue = some concern, grey = concerned, yellow = clearly concerned, red = very concerned
FIGURE 6.
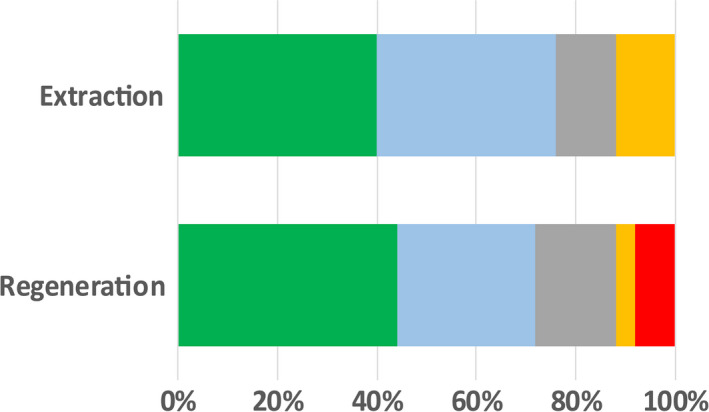
Frequency distribution of patient satisfaction with treatment at 1 year. Data are expressed as frequency distribution of the responses across the five points of the Likert scale. Green = extremely satisfied, light blue = very satisfied, grey = satisfied, yellow = moderately satisfied, red = not satisfied. No significant differences were observed between the two groups (p = .464, NS)
4. DISCUSSION
This manuscript extends the previously reported results of this randomized controlled clinical trial to the 10‐year follow‐up and indicates that periodontal regeneration is a clinically viable and more economical alternative to extraction and replacement for teeth severely compromised by the presence of an intra‐bony defect involving the apical portion of the root. While implant‐ or tooth‐supported fixed partial dentures perform well for the replacement of missing teeth complications occur, it is generally expected that they will not last for a lifetime (Pjetursson, Bragger, Lang, & Zwahlen, 2007; Pjetursson et al., 2004; Schmidlin et al., 2010). Cause of tooth loss and/or having suffered from periodontitis is considered to be risk indicators for implant failure (Ong et al., 2008; Sousa et al., 2016). The ability to preserve compromised teeth through powerful treatment modalities able to change tooth prognosis is a critical component of modern dentistry as it makes the goal of lifelong preservation of function possible even for subjects with severe conditions such as periodontitis.
Extension of periodontal regeneration to teeth with CAL and bone loss to or beyond the apex is a complex and inter‐disciplinary treatment modality: the ability to effectively control periodontitis, the management of tooth hypermobility and secondary occlusal trauma, and the control of the pulp/endodontic status of the affected tooth are pre‐requisites to a successful treatment. Specific algorithms to improve local characteristics at the regenerated sites have been previously reported (Cortellini & Tonetti, 2015). Case selection is also critical: all cases were characterized by the presence of good peaks of bone/attachment on the adjacent teeth, essentially providing good coronal anchorage to ensure stability of the flap and the clot as well as limiting soft‐tissue recession. Such characteristic is critical for both the test and the control treatments, and it is important not to generalize the results to cases without such specific morphology (Cortellini et al., 2019).
After periodontal regeneration of intra‐bony defects, the ability to preserve compromised teeth and stabilize attachment medium term to long term is well established (Cortellini & Tonetti, 2004; Nygaard‐Ostby, Bakke, Nesdal, Susin, & Wikesjo, 2010; Pretzl et al., 2009; Sculean et al., 2008). This study shows 88% survival of teeth with a hopeless prognosis at 10 years. Failures consisted of two teeth that did not improve after periodontal regeneration and were extracted shortly after the 1‐year follow‐up and a third tooth that was lost at year 8 after a traumatic injury. These pilot results compare well with those reported in systematic reviews and meta‐analyses of 10‐year survival of implant‐ or tooth‐supported fixed partial dentures (Pjetursson, Thoma, Jung, Zwahlen, & Zembic, 2012; Tan, Pjetursson, Lang, & Chan, 2004).
Complication‐free survival of regenerated hopeless teeth and tooth replacement was not significantly different in this small population. This aspect may, together with cost, be an important factor in assessing the merits of regeneration against replacement. A more in‐depth analysis assessing complication‐free survival from technical or biological complications showed no differences in terms of periodontal or cariologic/endodontic complications between the two groups. Technical complications, consisting mostly of broken splints or need for filling for cervical root abrasion, were more frequent and happened earlier in the periodontal regeneration group. These observations are not unexpected and may guide future clinical practice. The present data are unsuitable to gain further insight into the relative performance of implant‐ or tooth‐supported fixed partial dentures: the choice between the two options was based on expert opinion with the aim to maximize patient satisfaction and thus included both technical difficulty and the expected complication/failures.
Complication‐free survival or survival analyses are biased as they censor the subject at the time of the first event. Indeed, a single subject may suffer multiple complications, and these may range in severity from something relatively mild all the way to the loss of the tooth or the tooth replacement. In a recent study, we have addressed this potential problem by using recurrence analysis. This tool has been used extensively in medicine and surgery to describe changes in health status and to be able to introduce multiple events occurring in the same subject and also to quantify the cost for their management over time. This approach has been recently applied to the analysis of complications, their management and associated costs in a 20‐year follow‐up study of periodontal regeneration (Cortellini et al., 2017). In that study, less recurrences, better tooth retention and lower costs were observed for periodontal regeneration compared with the access flap control. In the present study, cost for recurrence had a tendency to occur earlier in the regeneration group than in the tooth replacement group. This is not unexpected as tooth extraction and replacement was a more radical solution and implant‐ or tooth‐retained partial dentures required more time to show complications and incur costs for their management. Of great importance, however, is the analysis that includes the baseline costs of therapy that were significantly lower for the regeneration group. When these are inserted in the recurrence analysis, the scale of the difference in actual costs becomes fully apparent: the biological saving represented by tooth preservation was accompanied by an important financial saving making it the more economic option over the 10‐year follow‐up of this study.
Results of patient‐reported outcomes are notable in several ways. In these subjects with hopeless teeth, oral health‐related quality‐of‐life measurements are strongly affected and show a significant impact across most of the domains of the OHIP‐14 instrument. Significant improvements in quality‐of‐life measurements were observed for both groups indicating that, in general, both treatments were successful in addressing patient concerns. Unexpectedly, better improvements in the OHIP‐14 scores were observed in the test group. This observation needs to be confirmed, and additional research is needed to properly assess the impact of tooth replacement with implants or conventional fixed partial dentures in subjects who have lost hopeless teeth. Improvements in quality of life and decreased aesthetic and functional concerns were reported throughout the 10‐year follow‐up. Patient‐reported outcomes further strengthen the potential of periodontal regenerative therapy for the management of severely compromised (or hopeless) teeth.
This study shows promising options for tooth retention that go beyond the current standard of care. The data need to be confirmed by independent studies by different clinicians and settings for this level of severity of the intra‐bony lesions. The results of this study, however, represent an important proof of principle as they compare for the first time, in a 10‐year trial, regeneration with extraction and tooth replacement in terms of professional, patient and economic outcomes. These results on hopeless teeth represent a powerful illustration of the benefits of periodontal regeneration in less severe cases: the economic advantages and the obvious patient preference for tooth retention are important arguments for periodontal regeneration as first‐choice treatment for teeth compromised by the presence of deep intra‐bony defects.
CONFLICT OF INTEREST
The authors report no conflict of interest in this study.
Cortellini P, Stalpers G, Mollo A, Tonetti MS. Periodontal regeneration versus extraction and dental implant or prosthetic replacement of teeth severely compromised by attachment loss to the apex: A randomized controlled clinical trial reporting 10‐year outcomes, survival analysis and mean cumulative cost of recurrence. J Clin Periodontol. 2020;47:768–776. 10.1111/jcpe.13289
Trial registration: NCT04227964
Funding information
This study was funded in part by the European Research Group on Periodontology, a Swiss public good foundation.
REFERENCES
- Cortellini, P. , Buti, J. , Pini Prato, G. , & Tonetti, M. S. (2017). Periodontal regeneration compared with access flap surgery in human intra‐bony defects 20‐year follow‐up of a randomized clinical trial: Tooth retention, periodontitis recurrence and costs. Journal of Clinical Periodontology, 44, 58–66. 10.1111/jcpe.12638 [DOI] [PubMed] [Google Scholar]
- Cortellini, P. , Cortellini, S. , & Tonetti, M. S. (2019). Papilla preservation flaps for periodontal regeneration of molars severely compromised by combined furcation and intrabony defects: Retrospective analysis of a registry‐based cohort. Journal of Periodontology, 91(2), 165–173. 10.1002/JPER.19-0010 [DOI] [PubMed] [Google Scholar]
- Cortellini, P. , Prato, G. P. , & Tonetti, M. S. (1995). The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. Journal of Periodontology, 66, 261–266. [DOI] [PubMed] [Google Scholar]
- Cortellini, P. , Prato, G. P. , & Tonetti, M. S. (1999). The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. International Journal of Periodontics & Restorative Dentistry, 19, 589–599. [PubMed] [Google Scholar]
- Cortellini, P. , Stalpers, G. , Mollo, A. , & Tonetti, M. S. (2011). Periodontal regeneration versus extraction and prosthetic replacement of teeth severely compromised by attachment loss to the apex: 5‐year results of an ongoing randomized clinical trial. Journal of Clinical Periodontology, 38, 915–924. [DOI] [PubMed] [Google Scholar]
- Cortellini, P. , & Tonetti, M. S. (2001). Microsurgical approach to periodontal regeneration. Initial evaluation in a case cohort. Journal of Periodontology, 72, 559–569. [DOI] [PubMed] [Google Scholar]
- Cortellini, P. , & Tonetti, M. S. (2004). Long‐term tooth survival following regenerative treatment of intrabony defects. Journal of Periodontology, 75, 672–678. [DOI] [PubMed] [Google Scholar]
- Cortellini, P. , & Tonetti, M. S. (2005). Clinical performance of a regenerative strategy for intrabony defects: Scientific evidence and clinical experience. Journal of Periodontology, 76, 341–350. 10.1902/jop.2005.76.3.341 [DOI] [PubMed] [Google Scholar]
- Cortellini, P. , & Tonetti, M. S. (2015). Clinical concepts for regenerative therapy in intrabony defects. Periodontology 2000, 68, 282–307. [DOI] [PubMed] [Google Scholar]
- Kwok, V. , & Caton, J. G. (2007). Commentary: Prognosis revisited: a system for assigning periodontal prognosis. Journal of Periodontology, 78(11), 2063–2071. [DOI] [PubMed] [Google Scholar]
- McGuire, M. K. , & Nunn, M. E. (1996a). Prognosis versus actual outcome. III. The effectiveness of clinical parameters in accurately predicting tooth survival. Journal of Periodontology, 67(7), 666–674. [DOI] [PubMed] [Google Scholar]
- McGuire, M. K. , & Nunn, M. E. (1996b). Prognosis versus actual outcome. II. The effectiveness of clinical parameters in developing an accurate prognosis. Journal of Periodontology, 67(7), 658–665. [DOI] [PubMed] [Google Scholar]
- Nygaard‐Ostby, P. , Bakke, V. , Nesdal, O. , Susin, C. , & Wikesjo, U. M. (2010). Periodontal healing following reconstructive surgery: Effect of guided tissue regeneration using a bioresorbable barrier device when combined with autogenous bone grafting. A randomized‐controlled trial 10‐year follow‐up. Journal of Clinical Periodontology, 37, 366–373. 10.1111/j.1600-051X.2010.01532.x [DOI] [PubMed] [Google Scholar]
- Ong, C. T. , Ivanovski, S. , Needleman, I. G. , Retzepi, M. , Moles, D. R. , Tonetti, M. S. , & Donos, N. (2008). Systematic review of implant outcomes in treated periodontitis subjects. Journal of Clinical Periodontology, 35, 438–462. [DOI] [PubMed] [Google Scholar]
- Pjetursson, B. E. , Bragger, U. , Lang, N. P. , & Zwahlen, M. (2007). Comparison of survival and complication rates of tooth‐supported fixed dental prostheses (FDPs) and implant‐supported FDPs and single crowns (SCs). Clinical Oral Implants Research, 18(Suppl. 3), 97–113. [DOI] [PubMed] [Google Scholar]
- Pjetursson, B. E. , Tan, K. , Lang, N. P. , Bragger, U. , Egger, M. , & Zwahlen, M. (2004). A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clinical Oral Implants Research, 15, 667–676. [DOI] [PubMed] [Google Scholar]
- Pjetursson, B. E. , Thoma, D. , Jung, R. , Zwahlen, M. , & Zembic, A. (2012). A systematic review of the survival and complication rates of implant‐supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clinical Oral Implants Research, 23(Suppl. 6), 22–38. [DOI] [PubMed] [Google Scholar]
- Pretzl, B. , Kim, T. S. , Steinbrenner, H. , Dorfer, C. , Himmer, K. , & Eickholz, P. (2009). Guided tissue regeneration with bioabsorbable barriers III 10‐year results in infrabony defects. Journal of Clinical Periodontology, 36, 349–356. [DOI] [PubMed] [Google Scholar]
- Schmidlin, K. , Schnell, N. , Steiner, S. , Salvi, G. E. , Pjetursson, B. , Matuliene, G. , … Lang, N. P. (2010). Complication and failure rates in patients treated for chronic periodontitis and restored with single crowns on teeth and/or implants. Clinical Oral Implants Research, 21, 550–557. [DOI] [PubMed] [Google Scholar]
- Sculean, A. , Kiss, A. , Miliauskaite, A. , Schwarz, F. , Arweiler, N. B. , & Hannig, M. (2008). Ten‐year results following treatment of intra‐bony defects with enamel matrix proteins and guided tissue regeneration. Journal of Clinical Periodontology, 35, 817–824. [DOI] [PubMed] [Google Scholar]
- Slade, G. D. (1997). Derivation and validation of a short‐form oral health impact profile. Community Dentistry and Oral Epidemiology, 25, 284–290. [DOI] [PubMed] [Google Scholar]
- Sousa, V. , Mardas, N. , Farias, B. , Petrie, A. , Needleman, I. , Spratt, D. , & Donos, N. (2016). A systematic review of implant outcomes in treated periodontitis patients. Clinical Oral Implants Research, 27, 787–844. [DOI] [PubMed] [Google Scholar]
- Tan, K. , Pjetursson, B. E. , Lang, N. P. , & Chan, E. S. (2004). A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clinical Oral Implants Research, 15, 654–666. [DOI] [PubMed] [Google Scholar]
- Tonetti, M. S. , Cortellini, P. , Pellegrini, G. , Nieri, M. , Bonaccini, D. , Allegri, M. , … Zuhr, O. (2018). Xenogenic collagen matrix or autologous connective tissue graft as adjunct to coronally advanced flaps for coverage of multiple adjacent gingival recession: Randomized trial assessing non‐inferiority in root coverage and superiority in oral health‐related quality of life. Journal of Clinical Periodontology, 45, 78–88. 10.1111/jcpe.12834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonetti, M. S. , Greenwell, H. , & Kornman, K. S. (2018). Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. Journal of Clinical Periodontology, 45(Suppl. 20), S149–S161. [DOI] [PubMed] [Google Scholar]


