Abstract
Background
Tooth wear is a multifactorial condition, leading to the loss of dental hard tissues. Physiological tooth wear is a slow process that normally does not lead to any subjective symptoms. When the condition progresses, it can become pathological, and several signs and symptoms may occur. The Tooth Wear Evaluation System (TWES) was described to implement a systematic diagnostic and management approach. Recently, management guidelines were presented in a European Consensus Statement (ECS) as well.
Objectives
To evaluate the TWES in practice and to integrate the principles described in the ECS in order to compose a renewed TWES 2.0 and a new taxonomy.
Methods
The TWES and the recommendations of the ECS were used by dental clinicians, in order to test its applicability in practice.
Results
Agreement was reached that the TWES 2.0 will use a stepwise approach, with a straightforward Tooth Wear Screening part and a more detailed Tooth Wear Status part. Also, the assessment of pathology from the ECS is incorporated in the TWES 2.0 (both classification and taxonomy).
Conclusions
In the TWES 2.0 is described that tooth wear is pathological if moderate/severe/extreme tooth wear is present, in combination with one or several described signs and symptoms. Aetiology can be assessed by findings that indicate a chemical and/or a mechanical cause. The taxonomy may help to identify situations in which preventive (restorative) interventions in early stages of tooth wear can be indicated. The reliability and validity of the adapted parts must be proven.
Keywords: classification, diagnosis, European Consensus Statement (ECS), management, pathological, physiological, taxonomy, tooth wear, Tooth Wear Evaluation System (TWES)
1. INTRODUCTION
Besides dental caries, tooth wear is the most frequent cause of damage of dental hard tissues. While the incidence of caries is declining, the frequency and severity of tooth wear seems to increase. 1 For example, a recent study among Dutch adults showed that mild to moderate tooth wear is a common phenomenon; its prevalence and severity increase with age, as determined in a previous survey. 2 A similar finding was revealed in the United Kingdom, where a 2009 survey 3 reported a higher prevalence of tooth wear than a 1998 survey. 4 The results of studies on children and adolescents, who exhibited a prevalence of 30% for tooth wear in permanent teeth, also indicate that tooth wear is on the rise. 5 , 6 The incidence of these severe levels of tooth wear in a study of 15‐year‐old adolescents was 25%. 7 By comparison, the prevalence among 70‐year‐olds was only 15%, according to another study. 8 One would normally expect the opposite: the prevalence of tooth wear should increase with the time the permanent teeth have been in function. It would therefore be desirable to recognise tooth wear at an early stage and to determine the causes so that preventive measures can be taken.
The causes of tooth wear can be chemical or mechanical. Chemical tooth wear (erosion) can be caused by extrinsic factors (acidic diet) or by intrinsic factors (acidic content of the stomach). Mechanical tooth wear can also be extrinsic or intrinsic. Extrinsic factors include the chewing of abrasive food components and the use of highly abrasive dental care products, which causes abrasion. Intrinsic factors include tooth grinding, which causes attrition. It is necessary that clinicians and researchers use the same nomenclature, in order make communication easier, and comparison of research possible. 9
It is a must to detect increased levels of tooth wear at an early stage to avoid necessary costly treatments. In the past, various indices have therefore been proposed for grading tooth wear. The most recent consensus statement 10 on the management of severe tooth wear therefore states that priority should be given to early detection of (severe) tooth wear and to identify the underlying aetiology. Indices such as the Tooth Wear Index (TWI), 11 the Basic Erosive Wear Examination (BEWE), 5 and the Tooth Wear Evaluation System (TWES) 12 have been recommended in the European Consensus Statement. These different indices make comparison of studies difficult. Hence, there is a strong need to formulate recommendations for the development of a broadly applicable Tooth Wear Evaluation System. 13 The European Consensus Statement proposed a differentiation between severe tooth wear and pathological tooth wear, defining the corresponding entities. Therefore, in daily practice, an examination protocol is required that combines the assessment of the severity of tooth wear with an evaluation of whether the tooth wear is pathological and thus forms the basis for clinical decision‐making. The present article proposes such a system, called the Tooth Wear Evaluation System (TWES 2.0).
2. TOOTH WEAR EVALUATION
The Tooth Wear Evaluation System (TWES) 12 , 14 , 15 introduced the principle of multi‐stage sequential (modular) evaluation of tooth wear in dentistry. The TWES consists of ten modules, four for basic diagnostics, three for extended diagnostics and three for management/treatment. After the initial phases of practical testing of the system by the authors themselves and feedback from many users, adjustments of the TWES in order to improve seem necessary. Feedback from the users revealed that the high number (ten) of modules could lead to confusion, and the grading scales led to discussion of applicability.
By combining the adapted TWES (TWES 2.0) with the concepts for differentiating pathological tooth wear of the European Consensus Statement (ECS), the authors propose a cascading procedure for future diagnoses of tooth wear.
3. TOOTH WEAR ASSESSMENT
At the time of its publication, the TWES Module Quantification used two ordinal grading scales for screening. A 5‐point ordinal scale for occlusal/incisal surfaces is used, in the adapted TWES 2.0 this grading remains the same (see Table 1).
TABLE 1.
Tooth Wear Screening, grading scales of the TWES 2.0
| Five‐point ordinal scale for occlusal and incisal grading 16 |
|
Grade 0 = no (visible) wear Grade 1 = visible wear within the enamel Grade 2 = visible wear with dentin exposure and loss of clinical crown height ≤ 1/3 Grade 3 = loss of clinical crown height > 1/3 but < 2/3 Grade 4 = loss of clinical crown height ≥ 2/3 |
| Five‐point ordinal scale for non‐occlusal and non‐incisal (= oral and vestibular) grading 13 : |
|
Grade 0 = No (visible) wear Grade 1 = Wear within the enamel Grade 2 = Wear with dentin exposure (less than 50% of the area) Grade 3 = Wear with dentin exposure (50% or more of the area) Grade 4 = Wear with dentin exposure (complete‐tooth loss of enamel or pulp exposure) |
| Tooth Wear Screening, Grading Document (redesign of Wetselaar & Lobbezoo 12 ) |
|
For the assessment of non‐occlusal/non‐incisal (or oral/vestibular) tooth wear, a 3‐point ordinal scale is used (Grade 0 = No (visible) wear; Grade 1 = Wear confined to the enamel; Grade 2 = Wear with exposed dentin). During Tooth Wear Screening in the TWES, grading is limited to the palatal surfaces of the second sextant, while the more detailed follow‐up examination inspected all oral and vestibular surfaces. However, users experienced that this screening grading cannot adequately represent oral and vestibular findings of advanced loss of dental hard tissues. Therefore, in the TWES 2.0, a 5‐point ordinal scale is incorporated for the assessment of the palatal surfaces during screening, based on comparison of existing grading scales 13 (see Table 1).
The evaluation of tooth wear in the original TWES was limited to natural teeth, as it was for all other existing indices as well. However, tooth wear can also affect direct and indirect restorative materials. Since the prevalence of tooth wear was increasing during the last decade, also more often, already restored dentitions will be present in the daily clinical practice. Tooth wear in connection with restorations allows conclusions to be drawn about the aetiology of tooth wear, because chemical tooth wear affects the dental hard tissues more severely than restorative materials. For teeth with restorations, the amount of substance lost is judged in comparison to the adjacent teeth or to unrestored teeth. Therefore, to assess the relevant wear on restorative materials and since no existing grading scale was detected in the literature, a 5‐point ordinal scale was suggested by the authors. By means of a Delphi process, all members of the working group commented until consensus was achieved (Wetselaar, Wetselaar‐Glas, Katzer, Ahlers, 2019). The resulting scale is as follows: Grade 0 = No (visible) wear; Grade 1 = Wear within the ceramic/resin composite material (“at enamel level”); Grade 2 = Wear within the ceramic/resin composite material (“at dentin level”); Grade 3 = Wear with metal/hard dental tissue exposure; Grade 4 = Wear with complete destruction of the ceramic/resin composite material. This new scale must and will be tested extensively, before implementation can occur. In the meantime, the two above‐mentioned scales can be used.
4. CLASSIFICATION OF TOOTH WEAR
As mentioned in the first version of the TWES, 12 the occlusal/incisal and non‐occlusal/non‐incisal (oral/vestibular) wear levels are leading to the following severity classification:
Grade 0 = No wear
Grade 1 = Mild tooth wear
Grade 2 = Moderate tooth wear
Grade 3 = Severe tooth wear
Grade 4 = Extreme tooth wear
As part of the diagnosis, these terms are combined with other information (see below).
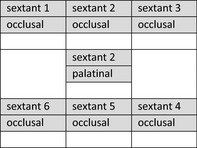
5. TOOTH WEAR SCREENING
The first step of the diagnostic process remains the Tooth Wear Screening. The goal of this examination is to identify patients with increased levels of tooth wear. Patients with prominent findings can or will undergo a more detailed examination, as the basis for possible treatment decisions. The screening is designed in such a way that it can be carried out quickly. No additional instruments are required for Tooth Wear Screening except for a mouth mirror and a documentation form. The highest grade for each sextant is entered in this documentation form, supplemented by an additional grade for the palatal surfaces of the maxillary anterior teeth (sextant 2). The five‐point ordinal scales mentioned in Table 1 are used to record the highest gradings. The individual grades obtained from the Tooth Wear Screening are interpreted as standalone values, no summation is performed.
The results of the Tooth Wear Screening are documented in the form provided for that purpose, in which the individual grades are entered (see Table 1).
The indication for a more detailed Tooth Wear Status depends on the highest individual grades, according to the following rules:
-
Grade 0 in all sextants and the anterior palatal sextant
→ No tooth wear → No action required
-
Grade 1 in any or all sextants and/or the anterior palatal sextant
→ Mild tooth wear → No action required
-
Grade 2 in any or all sextants and/or the anterior palatal sextant
→ Moderate tooth wear → Detailed Tooth Wear Status can be performed
Grade 3 or 4 in any or all sextants
> Severe or extreme tooth wear → Detailed Tooth Wear Status should be performed, if the patient and/or the dentist have reason to assume that the tooth wear might be pathological.
In contrast to the TWES 1.0, additional information regarding medical and dental history taking, and assessment of individual morphological characteristics (TWES Module Qualification), should be reserved for the extended diagnostics. This deliberately keeps the screening straightforward and limits the time and effort.
6. TOOTH WEAR STATUS
In accordance with the stepwise concept, a more detailed and therefore more complex examination is carried out at the second diagnostic stage.
It is indicated in the following situations:
Optional when the Tooth Wear Screening has indicated moderate tooth wear (TWES 1.0), obligatory when severe or extreme tooth wear are revealed
To assess tooth wear progression in detail, in order to evaluate preventive measurements (TWES 1.0)
When a detailed treatment plan is required (TWES 1.0)
A brief visual inspection reveals severe/extreme tooth wear (TWES 2.0)
Oral history taking/questionnaires indicating pathological tooth wear (TWES 2.0)
In case of situations 4 and 5, the Tooth Wear Status can be obtained directly (step one, the Tooth Wear Screening, can be skipped).
In the first version of the TWES (TWES 1.0), this examination was mentioned the “finer‐grained module” and included a much more detailed survey of all teeth and all surfaces. In the extended Tooth Wear Status are incorporated: 1. a detailed grading; 2. an adapted qualification to reveal etiological factors; and 3. recording of pathological symptoms.
6.1. Grading of tooth wear
In order to determine the Tooth Wear Status, one grade is recorded for each tooth surface (occlusal/incisal, vestibular and oral). The individual values are entered in a graphical diagnostic form (Table 2) based on the above‐mentioned five‐point ordinal scales 14 , 16 ; optionally, the 8‐point occlusal/incisal ordinal scale can be used. 12 , 17 In contrast to the Tooth Wear Screening, where the highest grade per sextant determines the overall evaluation, in the Tooth Wear Status, the highest grade per tooth is relevant for this determination.
TABLE 2.
Tooth Wear Status, Grading Document
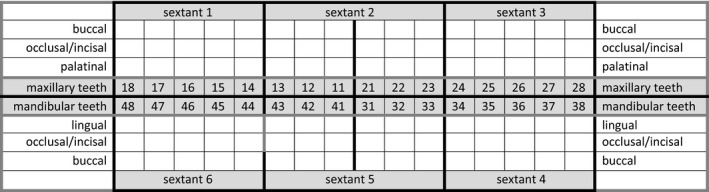
‐ The grading document of the Tooth Wear Status is a redesign of that of the TWES 1.0 12
‐ Use the two 5‐point ordinal scales of the Tooth Wear Screening (TWES 2.0) (see Table 1) or for occlusal/incisal grading, optional, the finer‐grained 8‐point ordinal scale from the TWES 1.0 can be used (Wetselaar et al, 2009)
For each tooth, the grade is determined as follows:
0 = no (visible) wear
1a = (within the enamel) minimal wear of cusps or incisal tips
1b = (within the enamel) facets parallel to the normal planes of contour
1c = (within the enamel) noticeable flattening of cusps or incisal edges
2 = wear with dentin exposure and loss of clinical crown height ≤ 1/3
3a = wear with dentin exposure and loss of clinical crown height 1/3 −1/2
3b = wear with dentin exposure and loss of clinical crown height ≥ 1/2 ‐ 2/3
4 = wear with dentin exposure and loss of clinical crown height of ≥ 2/3
6.2. Determining aetiology
A further component of the Tooth Wear Status is the recording of clinical signs that allows an aetiological classification. The TWES 1.0 12 had included in the “Module Qualification,” a cumulative list of 18 different clinical signs, divided in three sections (clinical signs of erosion, attrition and abrasion) on the basis of earlier research. 18 , 19 This list has been tested for clinical feasibility. It was found, by many users of the TWES, that three clinical signs were poorly reproducible (“usually located at cervical areas of the teeth,” “buccal/cervical lesions more wide than deep,” and “cervical areas of premolars and cuspids commonly affected”). However, since there is no evidence that any of the 18 clinical signs is valid, these three signs are still incorporated in the list. Further research is needed before a more reliable and valid list can be composed. Based on the results from two studies published recently, two findings have been added, “cracks within the enamel" 20 —not to be confused with cracked teeth—and the "torus mandibulae.” 21 Furthermore, we added the description non‐carious cervical lesions (NCCL). 22 The new table of clinical signs thus comprises 20 items and is divided only into two sections, one indicating chemical tooth wear and the other one indicating mechanical tooth wear (Table 3). The Tooth Wear Status assesses the individual clinical signs; subsequently, the number of clinical signs is registered as a percentage of the maximum number of possible clinical signs per section. It is of paramount importance to perform future research towards this topic. For now, we only can conclude that the existing clinical signs are not supported by solid evidence. Therefore, we skipped the quantification in the Tooth Wear Screening part and added this to the Tooth Wear Status part; in our taxonomy, it is mentioned last.
TABLE 3.
Tooth Wear Status, determining aetiology and pathology
| Tooth Wear Status, determining aetiology by clinical signs (Wetselaar, Wetselaar‐Glas, Katzer, Ahlers, 2019) | ||
|
Clinical signs indicating the influence of chemical factors ◯ 1. occlusal “cupping,” incisal “grooving,” ‘cratering’ [*], rounding of cusps and grooves [**] ◯ 2. wear on non‐occluding surfaces [*], non‐carious cervical lesions, NCCL [*****] ◯ 3. “raised” restorations [*] [**] ◯ 4. broad concavities within smooth surface enamel [*], convex areas flatten, or concavities become present, width exceed depth [**] ◯ 5. increased incisal translucency [*] ◯ 6. clean, non‐tarnished appearance of amalgams [*] ◯ 7. preservation of enamel “cuff” in gingival crevice [*] [**] ◯ 8. no plaque, discoloration or tartar [**] ◯ 9. hypersensitivity [*] ◯ 10. smooth silky‐shining, silky‐glazed appearance, dull surface [**] Clinical signs indicating the influence of mechanical factors ◯ 1. shiny facets [*], flat and glossy [**] ◯ 2. enamel and dentin wear at the same rate [*] ◯ 3. matching wear on occluding surfaces [*] corresponding features at the antagonistic teeth [**] ◯ 4. fracture of cusps or restorations [*] ◯ 5. impressions in cheek, tongue and/or lip [***] ◯ 6. located at cervical areas of the teeth [*], non‐carious cervical lesions, NCCL [*****] ◯ 7. buccal/cervical lesions more wide than deep [*], non‐carious cervical lesions, NCCL [*****] ◯ 8. cervical areas of premolars and cuspids are affected [*] ◯ 9. cracks within the enamel [****] ◯ 10. torus mandibulae [*****] | ||
|
[*] according to Gandara and Truelove 1999; [**] according to Ganss and Lussi 2014 (***) according to Wetselaar and Lobbezoo 2016; (****) according to Turssi et al 2019 (*****) according to Hammoudi et al 2019; [*****] according to Bhundia et al, 2019 The term “sometimes” (in item 10 Clinical signs indicating the influence of chemical factors), as well as the terms “possible,” “usually” and “commonly” (in item 4, 6 and 8, respectively, of the clinical signs indicating the influence of mechanical factors) are deleted, although they were mentioned in the original text of the respective authors; the answer options are now: yes or no | ||
|
In a small (theoretically) number of cases, one or more items cannot be assessed because of absence. These several possibilities are as follows: A. item 3 (Clinical signs indicating the influence of chemical factors), if there are no restorations; B. item 6 (Clinical signs indicating the influence of chemical factors), if there are no amalgam fillings; C. item 3 (Clinical signs indicating the influence of mechanical factors) if there are no antagonists; and D. item 8 (Clinical signs indicating the influence of mechanical factors) if there are no premolars or cuspids. So in both subgroups, two items can be “no scored.” So in both subgroups, two items can be “no scored.” If this is the case, the additional cut‐off criteria are as follows: with a minimum of four items, it still must be considered as “mainly (chemical or mechanical)”. | ||
| Tooth Wear Status, detection of pathological signs and symptoms (Wetselaar, Wetselaar‐Glas, Katzer, Ahlers, 2019) | ||
|
Tooth wear with dentin exposure (moderate, severe or extreme) Independent of distribution (localised or generalised) Tooth wear with dentin exposure (moderate, severe or extreme) Independent of distribution (localised or generalised) |
AND at least one of the following criteria: |
sensitivity and/or pain [*] [**] functional problems (difficulties chewing and eating) [*] [**] deterioration of aesthetic appearance (compromised dental attractiveness) [*] [**] fast progress of the tooth wear process after a period of monitoring [*] [**] wear atypical for the age of the patient [*] [**] crumbling of dental hard tissue and restorations, threatening the integrity of teeth [*] etiological factors not influenceable [*] surfaces that are involved in occlusion and articulation, leading to the loss of VDO [*] the condition of the saliva [*] phonetic impairment [***] |
|
[*] according to Wetselaar and Lobbezoo 2016; [**] according to Loomans et al, 2017; [***] according to Burnett and Clifford, 1999. | ||
6.3. Detection of pathological signs and symptoms
As a new part of the taxonomy, the signs (criteria assessed by the examiner) and symptoms (complaints of the patient) that are considered indicative for pathological tooth wear are assessed. 10 These symptoms are revealed through an oral history taking and a clinical observation. For evaluation purposes, it is first checked whether there are any signs of tooth wear with dentin exposure (moderate, severe or extreme; either localised or generalised) and any symptoms of pathogenicity. If positive, the characteristics are added up, with each of the characteristics indicating the presence of pathological tooth wear (Table 3).
7. TAXONOMY OF TOOTH WEAR DIAGNOSIS
Finally, the various individual findings are combined to form a structured diagnosis in order to guide towards the proper treatment/management option. Following the reassessment within the framework of the consensus statement, the amount of tooth wear as established by the application of an index should not be the decisive factor and certainly not the only basis for that decision. The various decision criteria were already specified in the original TWES publication. 12 The new taxonomy presented here simplifies the process by integrating the presence of pathological characteristics directly into the diagnosis. The synopsis in Table 4 is based on the following individual guidelines:
In line with the new classification of periodontal diseases, 23 the principle of indicating the distribution of tooth wear (generalised or localised tooth wear) as a first step of the process remains. This information is combined with the predominant severity of tooth wear (mild/ moderate/ severe/ extreme).
In patients with increased levels of tooth wear, this wear will not be uniformly present on all teeth; for example, a generalised level of severity can co‐occur with a different localised level of severity (higher or lower). Therefore, the diagnosis is made in two stages (eg generalised mild and localised severe tooth wear).
A new question is whether the tooth wear observed is pathological or not. The new taxonomy provides that pathology requires to be moderate, severe or extreme tooth wear, combined with at least one of the signs and symptoms mentioned in Table 3. Any additional symptom reinforces the classification of tooth wear as pathological. The classification as pathological tooth wear is placed immediately before the noun (eg “generalised mild and localised severe pathological tooth wear”) (Tables 4 and 5).
Finally, the evaluation of the findings on aetiology is included in the diagnosis. As specified in the evaluation of the clinical signs, the only subdivision is that of chemical and mechanical origin. The relevance of the respective factor is evaluated according to the number of actual positive findings as a percentage of the maximum number of possible positive findings. If 50% or more of the possible clinical signs are present, the origin is considered “mainly” (chemical or mechanical). If less than half of the possible clinical signs are present, the classification refers to “partially” (chemical or mechanical) origin (eg “generalised mild and localised severe pathological tooth wear, mainly mechanical and partially chemical”). If 50% or more of the possible characteristics are present for chemical and mechanical clinical signs, the classification refers to “both.” The combination of “mainly,” “partially” or “both” can thus result in various possible combinations for the assignment of mechanical or chemical origin (Tables 4 and 5). It is of paramount importance, in order to find cooperation and compliance in daily practice, to keep the “rules” as simple and straightforward as possible.
TABLE 4.
Taxonomy of tooth wear diagnosis, according to TWES 2.0
| Category | Description | Example |
|---|---|---|
|
1. Generalised severity no/mild/moderate/severe/extreme |
The most severe generalised grade comes first | Generalised mild tooth wear |
|
2. Localised severity no/mild/moderate/severe/extreme |
It is subsequently combined, if applicable, with a different localised grade | Generalised mild tooth wear and localised severe tooth wear |
|
3. Pathology no/yes |
Tooth wear is “pathological” if it is moderate, severe or extreme AND at least one of the criteria from Table 3 | Generalised mild tooth wear and localised severe pathological tooth wear |
|
4. Origin
|
The origin is either “mainly” or “partially” mechanical or chemical, depending if ≥ 50% or < 50% of the clinical signs of Table 3 indicate the cause respectively; and “both” in case of mechanical and chemical being both ≥ 50% |
Mild generalised tooth wear and severe localised pathological tooth wear, mainly mechanical and partially chemical |
TABLE 5.
Classification system of tooth wear, according to TWES 2.0
| Generalised | Mild | Tooth wear, |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
|
| Moderate | Pathological |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
||
| Severe | Pathological |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
||
| Extreme | Pathological |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
||
| Localised | Mild |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
||
| Moderate | Pathological |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
||
| Severe | Pathological |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
||
| Extreme | Pathological |
Both chemical and mechanical Mainly chemical/mechanical Partially chemical/mechanical |
||
|
Generalised = 3 to 6 sextants; localised = 1 or 2 sextants; mild = grade 1; moderate = grade 2; severe = grade 3; extreme = grade 4; pathological: see Table 3 mainly/partially/both: see Table 4 | ||||
8. TREATMENT/MANAGEMENT DECISIONS
The dental clinician has two options:
counselling/monitoring/taking preventive measurements and
restorative treatment. 24
The main goal of counselling/monitoring/taking preventive measurements is the attempt to detect signs of progressive wear in order to avoid further loss of hard dental tissues as much as possible. By doing this, the start of a restorative treatment can be postponed or even avoided. Recent research has revealed that yearly counselling/ monitoring is favourable towards counselling/ monitoring every five years. 25 It is beyond the scope of this article to discuss this in detail.
Advantages of a restorative treatment can be the reduction of sensitivity and/or pain, the improvement of function and mastication, the improvement of oro‐facial aesthetics and the prevention of further loss of hard dental tissues and/or restorations. Disadvantages of restorative procedures are often overlooked and include the failure and/or fracture of the restorations and/or of the teeth their selves. As soon as the restorative cycle is started, it is always necessary to re‐restore the dentition, since restorations will not last for decades. 26 , 27 Therefore, it is important to postpone the start to an older age of the patient as much as possible.
To guide the dental clinician with the decision‐making when to start a restorative treatment, in the TWES 1.0, an approach was suggested based on primary and secondary criteria. Primary criteria were the amount of tooth surface loss, which surfaces are affected, and the number of teeth that are affected; secondary criteria were the speed of the tooth wear process, age of the patient and aetiological factors (Module “Start of treatment/management” 12 ). At that time it was already stated, that starting a restorative treatment is really only acceptable if a patient has complaints (Module “Complaints of the patient versus reasons for the clinician to start treatment/management” 12 ). This basic starting point was acquired in the European consensus statement as well, in that document appointed as “pathological.” 10 In the TWES 2.0, both starting points are combined, adapted, and reformulated in the Tooth Wear Status, detection of pathological signs and symptoms.
Of most importance in decision‐making was and still is the severity (grade) of the tooth wear. The other signs and symptoms that need to be assessed and evaluated are: sensitivity and/or pain, functional problems (difficulties chewing and eating), deterioration of aesthetic appearance (compromised dental attractiveness), fast progress of the tooth wear process, wear atypical for the age of the patient, crumbling off dental hard tissue and restorations, threatening the integrity of teeth, aetiological factors not influenceable, surfaces that are involved in occlusion and articulation, leading to the loss of vertical dimension of occlusion (VDO), the condition of saliva and phonetic impairment, causing alterations of speech 28 (see Table 3 Tooth Wear Status, detection of pathological symptoms and signs).
9. DISCUSSION
Adopted from the original TWES is the stepwise diagnostic process. This is a proven approach in other areas of medicine as well, including periodontology and craniomandibular dysfunction. In the original TWES (TWES 1.0), seven separated diagnostic modules are available. 12 In the adapted TWES (2.0), two separated diagnostic parts are available, the Tooth Wear Screening and the Tooth Wear Status (Table 6). The above‐mentioned changes of the TWES will be discussed.
TABLE 6.
Tooth Wear Evaluation System, TWES 2.0
| Tooth Wear Screening: |
|
| Tooth Wear Status, obligatory: |
|
| Tooth Wear Status, optional: |
|
| Treatment/management Status: |
|
9.1. Tooth Wear Screening
The goal of the Tooth Wear Screening is to obtain in a relative short amount of time, an overall impression of the wear of the given dentition. In the TWES 2.0 two changes are made compared with the TWES 1.0:1. only grading (quantification) is incorporated, and 2. the grading uses two grading scales, one of them is adapted; a third scale is needed and suggested, but must be tested for reliability. The grading of occlusal/incisal tooth wear with a 5‐point ordinal scale was adopted from the TWES 1.0. With this grading scale, the transitions from Grade 0 to Grade 1 can be clearly defined with corresponding optical magnification. The exposure of dentin cores through the loss of the enamel cover can also be clearly delimited. The loss of one‐third of the crown length sometimes appears less clear, however, studies 14 , 16 , 17 have shown that the evaluation of tooth wear is reproducible at this level of differentiation. The original 5‐point ordinal scale had been developed in Amsterdam as early as in 2001. 16 Reproducibility has also been demonstrated for the 8‐point ordinal scale, which includes further subdivisions of Grades 1 and 3. 12 , 17 It is helpful that this evaluation is reproducible not only clinically (intra‐orally), but also if intra‐oral photographs and/or dental casts are used instead. 17 In the (near) future, the use of intra‐oral scanners will become standard in daily practice, it is likely that they can be used for recording the progression of tooth wear as well. The use is related to the available imaging resolution and especially the precision of the various scanners. 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 The average loss rate of dental hard tissue substances per year should also be taken into account, both for physiological 37 , 38 and for pathological loss rates. 39 So far, the average physiological loss rate is below the level of precision of intra‐oral scanners, improvement of the scanners will solve this shortcoming. Nevertheless, digital measurement data might support the evaluation of tooth wear but will never be able to replace an evaluation in the sense of the taxonomy presented here. The adapted 5‐point ordinal scale for non‐occlusal and non‐incisal (oral and vestibular) grading makes the evaluation of these surfaces more distinctive, because now the severity of these surfaces can also “reach” the levels “severe” and “extreme,” as is the same with the occlusal/incisal surfaces. Especially grading of the palatal surfaces of the second sextant (being involved in occlusion and articulation) can be performed in a more distinctive way. The distinction thus allows to discriminate by the size and depth of the defects, if palatal wear is “minimal” or “moderate”—and thus requires no or only non‐invasive treatment—or if wear is severe or extreme. With the additional information on pathology of wear this provides a broader basis for the decision regarding restorative treatment.
Adding the 5‐point ordinal scale for grading of restored teeth after testing can be an improvement as well, since already nowadays more because of tooth wear restored dentitions will be present in daily practice, this will increase in the future. The grades for the respective sextants remain separate, no summation is performed. This distinguishes the procedure from the BEWE, 5 where a summation is performed with the risk of masking important information.
9.2. Tooth Wear Status
The Tooth Wear Status consists of three parts, a more detailed grading (quantification), determining aetiology by clinical signs (qualification), and register possible pathological signs and symptoms. The goal of the Tooth Wear Status is to obtain a straightforward but more detailed impression of the wear of the given dentition. All surfaces of all teeth are evaluated, using the same grading scales of the Tooth Wear Screening. Optional is a finer‐grained 8‐point ordinal scale for the occlusal/incisal surfaces, to monitor in more detail. This evaluation is more in line with the Tooth Wear Index (Smith & Knight, 1984), in contrast to the BEWE, no summation is performed either.
After the grading, also incorporated in the Tooth Wear Status is the adapted qualification of the observed tooth wear characteristics. The clinical signs are adapted based on findings performed by other researchers. 20 , 21 These findings are organised in a different way than in the TWES 1.0. In the TWES 1.0, three different subgroups of clinical signs were determined (clinical signs of erosion, attrition, and abrasion). In the TWES 2.0, two subgroups are used, namely “clinical signs indicating the influence of chemical factors” and “clinical signs indicating the influence of mechanical factors.” The term “indicating” is important, since no evidence is available regarding their validity. This change was based on the experience of the users that often, or even always, many clinical signs do coexist, remaining differentiation difficult. Nevertheless, a proposal of cut‐off criteria is incorporated, to differentiate between “mainly,” “partially” and “both.”
Subsequently, detection of pathological symptoms is performed, based on those that are mentioned in the European Consensus Statement 10 and already mentioned in the TWES 1.0 (Module Complaints of the patient versus reasons for the clinician to start treatment/management). 24 This detection is necessary for the new taxonomy.
9.3. Taxonomy and classification
The taxonomy and diagnostic classification follow the principle of generalised severity before local severity of the new classification of periodontal diseases. 23 This should make adaptation to the new taxonomy easier for dentists in daily practice. As with the periodontal classification, this new taxonomy for tooth wear offers the possibility of forming decision trees based on the findings. 40 In contrast to the periodontal classification, however, the tooth wear taxonomy aimed to be simple and straightforward to make it self‐explanatory. The signs and symptoms of pathological tooth wear are now fully integrated into the diagnostic decision tree for the first time. The present proposal is thus the first concept that combines the evaluation of the severity of tooth wear with the detection of pathological tooth wear. As mentioned in the European Consensus Statement, it is not the amount of tooth wear loss alone that is the determining factors for any restorative decisions, 10 but its combination with factors of pathological tooth wear. What is relevant here is not absolute measurement data, but their clinical classification, which can be derived from the present taxonomy.
10. CONCLUSION
The following overall conclusions can be drawn:
According to the new TWES 2.0, the evaluation of tooth wear should take place in two stages, with a compact Tooth Wear Screening and a more detailed Tooth Wear Status.
In both cases, grading is performed based on two different 5‐point ordinal scales; additional an 8‐point ordinal scale for a more detailed grading of the occlusal/incisal surfaces is optional.
Tooth wear is only pathological if moderate/severe/extreme tooth wear is present, in combination with one or several described signs and symptoms.
Causality can be clarified by searching for findings that indicate a chemical and/or a mechanical cause.
The taxonomy may help to identify situations in which preventive (restorative) interventions in early stages of tooth wear can be indicated as the tooth wear cannot be influenced otherwise and restorations can prevent further destruction.
CONFLICT OF INTEREST
None of the authors has any conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
All co‐authors actively took part in the conceptualisation and preparation of this manuscript.
Wetselaar P, Wetselaar‐Glas MMJ, Katzer LD, Ahlers MO. Diagnosing tooth wear, a new taxonomy based on the revised version of the Tooth Wear Evaluation System (TWES 2.0). J Oral Rehabil. 2020;47:703–712. 10.1111/joor.12972
The peer review history for this article is available at https://publons.com/publon/10.1111/joor.12972
REFERENCES
- 1. Lussi A, Carvalho TS. Erosive tooth wear: a multifactorial condition of growing concern and increasing knowledge. Monogr Oral Sci. 2014;25:1‐15. [DOI] [PubMed] [Google Scholar]
- 2. Wetselaar P, Vermaire JH, Visscher CM, Lobbezoo F, Schuller AA. The prevalence of tooth wear in the Dutch adult population. Caries Res. 2016;50(6):543‐550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Steele JG, O'Sullivan I. Adult Dental Health Survey 2009. The NHS Information Centre for Health and Social Care. Part of the Government Statistical Service. Published March 2011. ISBN 978‐1‐84636‐492‐1.
- 4. Kelly M, Steele JG, Nuttall N, et al. Adult Dental Health Survey ‐ Oral Health in the United Kingdom 1998. London, UK: Stationery Office; 2000. [Google Scholar]
- 5. Bartlett D, Ganss C, Lussi A. Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Invest. 2008;12(Suppl 1):S65‐S68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Salas MM, Nascimento GG, Huysmans MC, Demarco FF. Estimated prevalence of erosive tooth wear in permanent teeth of children and adolescents: an epidemiological systematic review and meta‐regression analysis. J Dent. 2015;43(1):42‐50. [DOI] [PubMed] [Google Scholar]
- 7. El Aidi H, Bronkhorst EM, Huysmans MC, Truin GJ. Dynamics of tooth erosion in adolescents: a 3‐year longitudinal study. J Dent. 2010;38(2):131‐137. [DOI] [PubMed] [Google Scholar]
- 8. Van't Spijker A, Rodriguez JM, Kreulen CM, Bronkhorst EM, Bartlett DW, Creugers NH. Prevalence of tooth wear in adults. Int J Prosthodont. 2009;22(1):35‐42. [PubMed] [Google Scholar]
- 9. Wetselaar P, Lobbezoo F, Beddis H. Restorative dentistry: tooth wear terms. Br Dent J. 2018;225(2):94. [DOI] [PubMed] [Google Scholar]
- 10. Loomans B, Opdam N, Attin T, et al. Severe Tooth Wear: European consensus statement on management guidelines. J Adhes Dent. 2017;19(2):111‐119. [DOI] [PubMed] [Google Scholar]
- 11. Smith BG, Knight JK. An index for measuring the wear of teeth. Br Dent J. 1984;156(12):435‐438. [DOI] [PubMed] [Google Scholar]
- 12. Wetselaar P, Lobbezoo F. The tooth wear evaluation system: a modular clinical guideline for the diagnosis and management planning of worn dentitions. J Oral Rehabil. 2016;43(1):69‐80. [DOI] [PubMed] [Google Scholar]
- 13. Wetselaar P, Faris A, Lobbezoo F. A plea for the development of an universally accepted modular tooth wear evaluation system. BMC Oral Health. 2016;16(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wetselaar P, Lobbezoo F, Koutris M, Visscher CM, Naeije M. Reliability of an occlusal and nonocclusal tooth wear grading system: clinical use versus dental cast assessment. Int J Prosthodont. 2009;22(4):388‐390. [PubMed] [Google Scholar]
- 15. Wetselaar P, van der Zaag J, Lobbezoo F. Tooth wear, a proposal for an evaluation system. Ned Tijdschr Tandheelkd. 2011;118(6):324‐328. [DOI] [PubMed] [Google Scholar]
- 16. Lobbezoo F, Naeije M. A reliability study of clinical tooth wear measurements. J prosthet Dent. 2001;86(6):597‐602. [DOI] [PubMed] [Google Scholar]
- 17. Wetselaar P, Wetselaar‐Glas MJ, Koutris M, Visscher CM, Lobbezoo F. Assessment of the amount of tooth wear on dental casts and intra‐oral photographs. J Oral Rehabil. 2016;43(8):615‐620. [DOI] [PubMed] [Google Scholar]
- 18. Gandara BK, Truelove EL. Diagnosis and management of dental erosion. J Contemp Dent Pract. 1999;1(1):16‐23. [PubMed] [Google Scholar]
- 19. Ganss C, Lussi A. Diagnosis of erosive tooth wear. Monogr Oral Sci. 2014;25:22‐31. [DOI] [PubMed] [Google Scholar]
- 20. Turssi CP, Algarni AA, Eckert GJ, Hara AT. Enamel crack association with tooth age and wear severity: an optical coherence tomography study. Am J Dent. 2019;32(1):3‐8. [PubMed] [Google Scholar]
- 21. Hammoudi W, Trulsson M, Smedberg JI, Svensson P. Phenotypes of patients with extensive tooth wear‐A novel approach using cluster analysis. J Dent. 2019;82:22‐29. [DOI] [PubMed] [Google Scholar]
- 22. Bhundia S, Bartlett D, O'Toole S. Non‐carious cervical lesions ‐ can terminology influence our clinical assessment? Br Dent J. 2019;227(11):985‐988. [DOI] [PubMed] [Google Scholar]
- 23. Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri‐implant diseases and conditions ‐ Introduction and key changes from the 1999 classification. J Periodontol. 2018;89(Suppl 1):S1‐S8. [DOI] [PubMed] [Google Scholar]
- 24. Wetselaar P, Lobbezoo F. The Tooth Wear Evaluation System (TWES): a modular clinical guideline for the diagnosis and management planning of worn dentitions Part 2: treatment/management modules and discussion. J Craniomandibular Function. 2017;9(1):27‐38. [Google Scholar]
- 25. Wetselaar P, Lobbezoo F, de Jong P, Choudry U, van Rooijen J, Langerak R. A methodology for evaluating tooth wear monitoring using timed automata modelling. J Oral Rehabil. 2020;47(3):353‐360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lambrechts P, Meerbeek B, Perdigão J, Gladys S, Braem M, Vanherle G. Restorative therapy for erosive lesions. Eur J Oral Sci. 1996;104(2 (Pt 2)):229‐240. [DOI] [PubMed] [Google Scholar]
- 27. Peutzfeldt A, Jaeggi T, Lussi A. Restorative therapy of erosive lesions. Monogr Oral Sci. 2014;25:253‐261. [DOI] [PubMed] [Google Scholar]
- 28. Burnett CA, Clifford TJ. The mandibular speech envelope in subjects with and without incisal tooth wear. Int J Prosthodont. 1999;12(6):514‐518. [PubMed] [Google Scholar]
- 29. Ender A, Mehl A. Full arch scans: conventional versus digital impressions–an in‐vitro study. Int J Comput Dent. 2011;14(1):11‐21. [PubMed] [Google Scholar]
- 30. Ender A, Mehl A. Accuracy of complete‐arch dental impressions: a new method of measuring trueness and precision. J Prosthet Dent. 2013;109(2):121‐128. [DOI] [PubMed] [Google Scholar]
- 31. Ender A, Mehl A. In‐vitro evaluation of the accuracy of conventional and digital methods of obtaining full‐arch dental impressions. Quintessence Int. 2015;46(1):9‐17. [DOI] [PubMed] [Google Scholar]
- 32. Ender A, Zimmermann M, Mehl A. Accuracy of complete‐ and partial‐arch impressions of actual intraoral scanning systems in vitro. Int J Comput Dent. 2019;22(1):11‐19. [PubMed] [Google Scholar]
- 33. Bocklet C, Renne W, Mennito A, et al. Effect of scan substrates on accuracy of 7 intraoral digital impression systems using human maxilla model. Orthod Craniofac Res. 2019;22(Suppl 1):168‐174. [DOI] [PubMed] [Google Scholar]
- 34. Keul C, Guth JF. Accuracy of full‐arch digital impressions: an in vitro and in vivo comparison. Clin Oral Invest. 2020;24(2):735‐745. [DOI] [PubMed] [Google Scholar]
- 35. Mennito AS, Evans ZP, Nash J, et al. Evaluation of the trueness and precision of complete arch digital impressions on a human maxilla using seven different intraoral digital impression systems and a laboratory scanner. J Esthet Restor Dent. 2019;31(4):369‐377. [DOI] [PubMed] [Google Scholar]
- 36. Skramstad MJ. Welcome to Cerec Primescan AC. Int J Comput Dent. 2019;22(1):69‐78. [PubMed] [Google Scholar]
- 37. Xhonga FA. Bruxism and its effect on the teeth. J Oral Rehabil. 1977;4(1):65‐76. [DOI] [PubMed] [Google Scholar]
- 38. Lambrechts P, Braem M, Vuylsteke‐Wauters M, Vanherle G. Quantitative in vivo wear of human enamel. J Dent Res. 1989;68(12):1752‐1754. [DOI] [PubMed] [Google Scholar]
- 39. Seligman DA, Pullinger AG. The degree to which dental attrition in modern society is a function of age and of canine contact. J Orofac pain. 1995;9(3):266‐275. [PubMed] [Google Scholar]
- 40. Tonetti MS, Sanz M. Implementation of the new classification of periodontal diseases: decision‐making algorithms for clinical practice and education. J Clin Periodontol. 2019;46(4):398‐405. [DOI] [PubMed] [Google Scholar]


