In April of 2002, the National Institute of Mental Health convened a workshop entitled “Mental Health Research Issues in HIV/AIDS and Aging.” The workshop convened to answer two broad questions: (1) “Do older adults infected with HIV differ from older uninfected adults or younger HIV-infected adults on a variety of factors related to HIV disease, such as natural course, risk factors, HIV-related comorbidities, neurocognitive, neuropsychiatric, and substance use complications, neuropathogensis, and response to treatment?”; and (2) “What is the nature of the relationships and the interaction of HIV infection with the aging process or with age-associated disease of the central nervous system (CNS) on the HIV-related variables of interest?”.1
Since the emergence of HIV more than three decades ago, but particularly within the past five years, a growing amount of research has sought to provide answers to these questions. As of May 2014, a search of the PubMed database using the terms “HIV and aging” yielded 1,701 articles. As shown in Figure 1, the number of studies examining HIV and aging issues has increased almost every year since 2002. Additional evidence of the burgeoning interest in HIV and aging is that, during the three-year period from 2011 to 2013 (or just 1,095 days), twice as many articles were published on “HIV and aging” than were published during the 15 year period from 1981 to 1999. Books examining HIV and aging that are written for both academic and larger lay audiences, such as Halkitis’ “The AIDS Generation: Stories of Survival and Resilience,”2 which chronicles the life histories of 15 HIV-infected gay men aging with HIV, are enjoying greater popularity and playing an increasingly important role in revealing what it is like to age with HIV in the United States.
Figure 1:
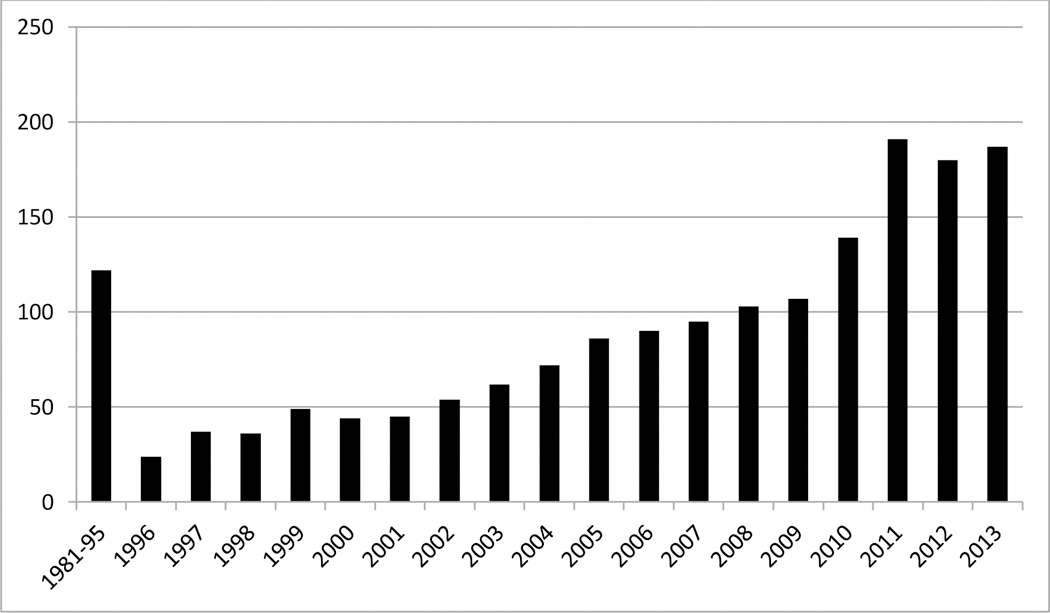
Number of Articles Published Each Year on the Topic of “HIV and Aging”
The intensified focus on how HIV impacts older adults is driven by the facts that (1) persons 50 years of age and older will soon account for more than one-half of all HIV cases in the United States,3 (2) persons infected with HIV in their 20s, 30s, and 40s are now living well into their 60s, 70s, and even longer, and (3) incidence rates of new HIV infections in older adults are steadily increasing.4 In certain geographic regions the United States (typically larger AIDS epicenters such as New York City and San Francisco), persons 50-plus years of age already account for more than half of all HIV cases.5 We are witnessing only the first cohort of aging HIV-positive individuals; with no cure or vaccine for HIV in sight and with some 50,000 new infections per year.6 Older adults living with HIV will continue to be a significant portion of our population for years to come, both in the United States and in other part of the world, including sub-Saharan Africa.7
During the first two decades of the AIDS epidemic, the overwhelming majority of research on HIV and aging was conducted in the United States. However, as life expectancies of people living with HIV/AIDS throughout the world continue to increase, many countries are paying greater attention to the impact of HIV on older adults, most notably Australia, Brazil, Canada, China, South Africa, and Uganda.
Studies investigating HIV and aging are indeed providing some answers to the questions posed by the NIMH “Mental Health Research Issues in HIV/AIDS and Aging” workshop that convened more than 10 years ago. Regarding the question of how older people living with HIV (OPLWH) differ from older uninfected adults or younger HIV-infected adults, research to date has revealed much about this population.
In terms of psychosocial burdens, rates of sex without condoms among sexually active OPLWH are comparable to those reported by younger and middle-aged persons living with HIV/AIDS.8–10 OPLWH report greater unhappiness, poorer attitudes about aging, experience a greater number of negative life events, and more perceived stress than their younger counterparts.11 Younger and older persons living with HIV report comparable rates of depressive disorders and depressive symptomatology.12–13 Consistent with a theory of syndemics, negative psychosocial burdens, sex with condoms, and mental health burdens are intimately linked in OPLWH.14
With regard to antiretroviral therapy (ART), adherence is greater in OPLWH than their younger counterparts, with a recent meta-analysis concluding that older age reduced non-adherence to ART by 27% in HIV-infected persons,15 a conclusion possibly corroborated by the fact that older adults indicate higher rates of viral suppression that younger individuals.16 OPLWH benefit just as much, if not more, from ART, suggesting that prompt ART treatment can significantly reduce mortality rates and enhance immunologic recovery in OPLWH and produce life expectancies that are comparable to those of their younger counterparts.17–19 Moreover, among all individuals living with HIV, older age is associated with lower HIV viral loads (perhaps due to more consistent ART adherence), being prescribed more HIV and non-HIV related medications, and more comorbid conditions. In fact, in addition to living with their HIV infection, many OPLWH live with more than three morbidities, with the most common being depression, coronary artery disease, hypertension, erectile dysfunction, diabetes, peripheral neuropathy, hepatitis C, and renal disease.20–25 Not surprisingly, polypharmacy is more common in OPLWH due to HIV-related treatments and medications for treating multimorbidities.26 Importantly, the long-term effects of polypharmacy on OPLWH remain largely unknown.
Moreover, and importantly, age and HIV interact to produce larger declines in verbal memory over time, with the largest declines found in OPLWH.11,27 In fact, the lowest rates of successful cognitive aging are found in OPLWH,28 and OPLWH demonstrate more cognitive “dispersion” (or intra-individual variability across a range of tests) than older HIV- and younger HIV+ individuals, suggesting greater cognitive dyscontrol29 --although some contradictory research exists suggesting that age and HIV-serostatus do not interact to affect neuropsychological performance.30
Taken together, these findings underscore the complexities of living and aging with HIV and once more point to the fact that HIV/AIDS is a disease, best understood and most effectively treated, using approaches informed by a biopsychosocial lens as opposed to a purely biomedical one. The demands of aging create stress in the lives of all individuals but for HIV-positive individuals, some of whom are long term survivors first detected to be living with the disease at the onset of the epidemic,2 these conditions are heightened by the demands of ongoing and near perfect adherence to ART, expectations of sex with condoms, psychosocial, social, and economic burdens, struggles delineating HIV vs. age-related morbidities, and navigating through a complex and changing health care system. In light of the aforementioned findings regarding cognitive decline, Herculean efforts are required of OPLWH to simply live their lives and manage their daily routines.
Highlighting these complexities of aging with HIV and the need for more robust understandings of issues faced by OPLWH, in 2012, the National Institutes of Health issued a funding opportunity announcement (FOA) entitled “Multidisciplinary Studies of HIV/AIDS and Aging.”31 This announcement invited grant applications to study “HIV infection, HIV-associated conditions, HIV treatment, and/or biobehavioral or social factors associated with HIV/AIDS in the context of aging and/or in older adults.” In particular, the FOA sought to stimulate research on clinical translational, observational, and intervention studies in domestic and international settings related to HIV and aging. Perhaps as a way of presaging the HIV and aging issues that will be of greatest importance in the future, the National Institutes of Health cited the following specific areas as being in need of additional research: (1) the role of innate and adaptive immune cells in eliminating senescent cells and maintaining normal tissue structures as one ages; (2) the extent to which comorbidities, such as cardiovascular disease, cancers, renal impairment, metabolic bone disease, liver disease, neurological diseases, and neuropsychiatric disorders develop or change in the context of long-term HIV treatment.; (3) the use of biomarkers to more effectively assess the severity, or progression, of one’s HIV status or HIV associated non-AIDS comorbidities in the context of treatment outcomes; (4) understanding frailty and vulnerability in OPLHW; (5) research on the adequacy of social supports, levels of social isolation, access to age-appropriate services, coping with HIV, the physical and psychological effects of HIV- and age-related stigmas, and the utilization of community-based services to meet the complex needs of OPLWH; and (6) interventions to reduce sex without condoms, improve psychological functioning, and enhance ART adherence in OPLWH. Unfortunately, many interventions targeting these outcomes currently administered to OPLWH are based on programs originally developed for younger persons living with HIV/AIDS, potentially limiting their efficacy. Moreover, the use of more innovative outcomes and clinical markers is needed to address whether interventions are truly helpful for OPLWH, such as maintaining or improving physical and cognitive functioning, reducing the number of HIV- and non-HIV-related medications OPLWH are taking, and the efficacious management of multimorbidities (constructs not routinely assessed in contemporary interventions for OPLWH).
Research on Disparities in Persons Aging with HIV Is Needed
The population of persons aging with HIV/AIDS displays remarkable diversity in terms of gender, race/ethnicity, and sexual self-identity. Among persons ages 55 and older who were newly infected with HIV in 2011, 48% were African American and 14% were Hispanic.32 In spite of considerable diversity among OPLWH, a search of the PubMed database that combined the terms of “HIV,” “aging,” and “disparities” yielded only 23 articles (or roughly just 1.3% of the 1,701 articles published on “HIV and aging” since 1981). To date, most research examining disparities in OPLWH has focused on gender and/or sexual orientation, with far less research investigating disparities related to race/ethnicity, socioeconomic status, culture, and differences that may emerge between those who were infected earlier in their lives (adolescence, young adulthood) versus those infected later (middle age, older adulthood).
This special issue of Behavioral Medicine seeks to address many of the initial questions posed by the 2002 NIMH Working Group,1 but with greater attention devoted to heath disparities in OPLWH. In this special issue, Ompad and colleagues examine how HIV clinical markers in older gay and bisexual men living with HIV/AIDS are related to smoking behaviors and smoking histories. Brennan-Ing and colleagues examine how substance use and sexual risk differ between older gay and bisexual men, two groups that have historically been combined into one larger and seemingly homogeneous group. Heckman and colleagues describe how older gay, bisexual, and other men who have sex with men (MSM) and older heterosexuals respond differently to telephone-administered psychotherapies for the treatment of depression. Lovejoy and colleagues examine how depressive symptoms moderate treatment outcomes in OPLWH who receive a telephone-administered sexual risk reduction intervention. Durvasula describes the physical, social, and emotional challenges that confront older women living with HIV/AIDS, a group that remains woefully understudied and whose physical and psychosocial needs appear to be very different than those of their male counterparts. Rivera-Mindt and colleagues characterize how age and ethnicity (Latino vs. non-Hispanic White) are related to neurocognitive impairment. This latter study is particularly important given HIV’s growing and disproportionate impact on the Latino/a community.
These six articles are intended to contribute to the still nascent inquiry of disparities among OPLWH and to attend to the diversity of this population and the intersectional identities individuals hold. Our approach to working with this population cannot be directed by an underlying premise that as a group, OPLWH are monolithic. Instead, identifying and addressing disparities within and across different groups of OPLWH is critical if the HIV research community is to develop age-appropriate and culturally-contextualized interventions capable of reducing sexual risk behavior, increasing ART adherence, improving psychological well-being, and reducing the impact of comorbid health conditions on the growing population of adults aging with HIV.
Acknowledgements:
This paper was supported by Grants RO1 MH078749 and RO1 MH087462 from the National Institute of Mental Health (NIMH) and the National Institute of Nursing Research (NINR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH, the NINR, or the NIH.
Contributor Information
Timothy G. Heckman, University of Georgia
Perry N. Halkitis, New York University
References
- 1.Stoff DM. Mental health research in HIV/AIDS and aging: problems and prospects. AIDS 2004; 18: S3–S10. [PubMed] [Google Scholar]
- 2.Halkitis P (2013). The AIDS Generation: Stories of Survival and Resilience Oxford University Press; New York, NY. [Google Scholar]
- 3.Justice A HIV and aging: Time for a new paradigm. Current HIV/AIDS Reports 2010; 7: 69–76. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (2006). HIV/AIDS Surveillance Report, 2005 (Vol. 17). Atlanta: U.S. Department of Health and Human Services. [Google Scholar]
- 5.Justice A, Falutz J. Aging and HIV: An evolving understanding. Curr Opin HIV AIDS 2014; 9: 291–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall HI et al. Estimation of HIV incidence in the United States. JAMA 2008; 300 (5): 520–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hontelez Jan AC, et al. “The impact of antiretroviral treatment on the age composition of the HIV epidemic in sub-Saharan Africa.” AIDS (London, England) 260 1 (2012).) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooperman NA, Arnsten JH, Klein RS. Current sexual activity and risky sexual behavior in older men with or at risk for HIV infection. AIDS Educ Prev 2007; 19: 321–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lovejoy TI, Heckman TG, Sikkema KJ, Hansen NB, Kochman A et al. Patterns and correlates of sexual activity and condom use behavior in persons 50-plus years of age living with HIV/AIDS. AIDS Behav 2008; 12: 943–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pappas MK & Halkitis PN (2011). Club drug use and unprotected sexual behavior in relation to age and number of years living with HIV in a sample of seropositive gay and bisexual men. AIDS Care, 23(11), 1410–1416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rueda S, Law S, Rourke SB. Psychosocial, mental health, and behavioral issues of aging with HIV. Curr Opin HIV AIDS 2014; 9: 325–31 [DOI] [PubMed] [Google Scholar]
- 12.Aljassem K, Raboud JM, Hart TA, Benoit A, Su D, Margolese SL, Rourke SB, Rueda S, Burchell A, Cairney J, Shuper P, Loutfy MR; and the OHTN Cohort Study Research Team. Gender differences in severity and correlates of depression symptoms in people living with HIV in Ontario, Canada. 2014. J Int Assoc Provid AIDS Care;June [Epub ahead of print] [DOI] [PubMed]
- 13.Do AN, Rosenberg ES, Sullivan PS, Beer L, Strine TW, Schulden JD, Fagan JL, Freedman MS, Skarbinski J. Excess burden of depression among HIV-infected persons receiving medical care in the United States: data from the medical monitoring project and the behavioral risk factor surveillance system. PLoS One 2014; 9(3): e92842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halkitis Perry N., et al. Evidence for a syndemic in aging HIV-positive gay, bisexual, and other MSM; Implications for a holistic approach to prevention and health care. Annals of Anthropological Practice 2012; 362: 365–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghidei L, Simone MJ, Salow MJ, Zimmerman KM, Paquin AM, Skarf LM, Kostas TR, Rudolph JL. Aging, antiretrovirals, and adherence: a meta analysis of adherence among older HIV-infected individuals. Drugs Aging 2013; 10: 809–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention, CDC Fact Sheet: HIV in the United States: The stages of Care, July, 2012. Retrieved at http://www.cdc.gov/hiv/pdf/research_mmp_stagesofcare.pdf
- 17.Davis DH, Smith R, Brown A, Rice B, Yin Z, Delpech V. Early diagnosis and treatment of HIV infection: magnitude of benefit on short-term mortality is greatest in older adults. Age Ageing 2013; 42: 520–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mutevedzi PC, Rodger AJ, Kowal P, Nyirenda M, Newell ML. Decreased chronic morbidity but elevated HIV associated cytokine levels in HIV-infected older adults receiving HIV treatment: benefit of enhanced access to care? PLoS One 2013; 8(10): e77379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sabin CA. Do people with HIV infection have a normal life expectancy in the era of combination antiretroviral therapy? BMC Med 2013; 11: 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vance DE, Fazeli PL, Gakumo CA. The impact of neuropsychological performance on everyday functioning between older and younger adults with and without HIV. J Assoc Nurses AIDS Care 2013; 24: 112–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodriguez-Penney AT, Iudicello JE, Riggs PK, Doyle K, Ellis RJ, Letendre SL, et al. Co-morbidities in persons infected with HIV: Increased burden with older age and negative effects on health-related quality of life. AIDS Patient Care ST 2013; 27(1): 5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salter ML, Lau B, Go VF, Mehta SH, Kirk GD, HIV Infection, immune suppression, and uncontrolled viremia are associated with increased multimorbidity among aging injection drug users. Clin Infect Dis 2011; 53: 1256–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Onen NF, Shacham E, Stamm KE, Overton ET. Comparisons of sexual behaviors and STD prevalence among older and younger individuals with HIV infection. AIDS Care 2010; 22: 711–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guaraldi G, Silva AR, Stentarelli C. Multimorbidity and functional status assessment. Curr Opin HIV AIDS 2014; 9:386–97 [DOI] [PubMed] [Google Scholar]
- 25.Havlik RJ, Brennan-Ing M, Karpiak SE. Comorbidities and depression in older adults with HIV. 2011. Sex Health; 8: 551–59. [DOI] [PubMed] [Google Scholar]
- 26.Edelman EJ, Gordon KS, Glover J, McNicholl IR, Fiellin DA, Justice AC. The next therapeutic challenge in HIV: polypharmacy. Drugs Aging 2013; 30: 613–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seider TR, Luo X, Gongvatana A, Devlin KN, de la Monte SM, Chasman JD et al. Verbal memory declines more rapidly with age in HIV infected versus uninfected adults. J Clin Exp Neuropsychol 2014; 36: 356–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moore RC, Fazeli PL, Jeste DV, Moore DJ, Grant I, Woods SP; HIV Neurobehavioral Research Program (HNRP) Group. Successful cognitive aging and health-related quality of life in younger and older adults infected with HIV. AIDS Behav 2014; 18: 1186–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morgan EE, Iudicello JE, Weber E, Duarte NA, Riggs PK, Delano-Wood L, Ellis R, Grant I, Woods SP. Synergistic effects of HIV infection and older age on daily functioning. J Acquir Immune Defic Syndr 2012; 61: 341–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valcour V, Paul R, Neuhaus J, Shikuma C. The effects of age and HIV on neuropsychological performance. J Int Neuropsychol Soc 2011; 17:190–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Multidisciplinary Studies of HIV/AIDS and Aging. National Institutes of Health http://grants.nih.gov/grants/guide/pa-fles/PAR-12-176.html. Retrieved May 24, 2014.
- 32.Centers for Disease Control and Prevention. HIV Surveillance Report, 2011; vol. 23 http://www.cdc.gov/hiv/topics/surveillance/resources/reports/. Published February 2013. Accessed June 1, 2014. [Google Scholar]


