Abstract
Objective:
To assess changes in screening mammography cost-sharing and utilization before and after the Affordable Care Act (ACA) and the revised United States Preventive Services Task Force (USPSTF) guidelines. To compare mammography cost-sharing between women ages 40–49 and those 50–74.
Methods:
We used patient-level analytic files between 2004 and 2014 from Clinformatics™ Data Mart (OptumInsight, Eden Prairie, MN). We included women 40–74 years without a history of breast cancer or mastectomy. We conducted an interrupted time series analyses assessing cost-sharing and utilization trends before and after the ACA implementation and USPSTF revised guidelines.
Results:
We identified 1,763,959 commercially insured women ages 40– 74 years. Between 2004 and 2014, the proportion of women with zero cost-share for screening mammography increased from 81.9% in 2004 to 98.2% in 2014, reaching 93.1% with the 2010 ACA implementation. The adjusted median cost-share remained $0 over time. Initially at 36.0% in 2004, screening utilization peaks at 42.2% in 2009 with the USPSTF guidelines change, dropping to 40.0% in 2014. Comparing women ages 40–49, 50–64 and 65–74, the proportion exposed to cost-sharing declined over time in all groups.
Conclusions:
A substantial majority of commercially insured women had first dollar coverage for mammography prior to the ACA. After ACA, nearly all women had access to zero cost-share mammography. The lack of an increase in mammography use post-ACA can be partially attributed to a USPSTF guideline change, the high proportion women without cost-sharing prior to ACA, and the relatively low levels of cost-sharing prior to the policy implementation.
Summary statement:
The ACA did not change breast screening utilization despite more employed insured women experiencing zero cost-share, while the USPSTF 2009 guideline revision resulted in a significant utilization decrease.
INTRODUCTION:
The goal of the Affordable Care Act (ACA) is to “give more Americans access to affordable, quality health insurance and to reduce the growth in U.S. health care spending.”1 Obama describes several early achievements including a 16% reduction in the uninsured rate, a decline in the rate of growth in healthcare spending, and improvements in health care quality2 with continued need for improving affordability of health insurance and health care.
Value-Based Insurance Design (VBID) encourages consumers to use high value medical services, defined as having strong evidence to improve clinical outcomes and/or increase health system efficiency 3–6, by requiring reduction or elimination of out-of-pocket costs for these services. VBID has achieved particular success in aligning use of high value medications through cost-share reduction7, although cost reduction was not uniformly achieved 6,8,9. Nevertheless, women in particular continue to report unmet health care needs because of costs even after the passage of the ACA10. By eliminating out-of-pocket costs for high value services, the ACA has the potential to increase the affordability of women’s health care and subsequent use of high value services using VBID principles, including screening mammography.
The ACA required health plans to eliminate cost-sharing for preventive services rated by the United States Preventive Health Task Force (USPSTF) Grade A or B in 2010 to improve access, including screening11. However, in 2009, the USPSTF’s revised guidelines downgraded routine screening mammography among women ages 40–49 from Grade B to Grade C, potentially increasing the cost barrier to screening in this group while maintaining a Grade B for biennial screening in women ages 50–7412. The primary objective of this study was to correlate changes in cost-sharing for screening before and after implementation of the ACA and the revised USPSTF guidelines with screening utilization. The secondary objective was to compare screening mammography cost-sharing, defined as costs not covered by insurance typically including deductibles, coinsurance and copayments, between women ages 40–49 and women ages 50–74, before and after ACA implementation.
METHODS:
We used de-identified patient-level analytic files between January 2000 – December 2014 from The Clinformatics™ Data Mart Database (OptumInsight, Eden Prairie, Minnesota, U.S.). The Optum™ Clinformatics™ Data Mart includes member enrollment data including demographic variables, individual-level insurance claims, laboratory test results, hospital discharge information, and pharmacy claims. The advantages of this data source include its large size (over 140 million unique members included since 2000), its inclusion of race, income and household size, and the ability to follow individuals longitudinally as individuals are reported by employers not health plans. It also contains complete patient payment and charge information, including patient copayment, deductible, and coinsurance amounts, and standardized costs. This study was deemed exempt by our Medical School Institutional Review Board.
Our sample included women aged 40–74 years enrolled in employer-based health plans between 2004 and 2014 1) without a history of breast cancer or prior mastectomy with 2) at least 12 months of continuous enrollment in a given plan for the plan year and 3) were only enrolled in one plan for a given calendar year. We checked the eligible status annually and we excluded participants who were diagnosed with breast cancer in a given year from subsequent years’ samples. We reported annual mammography utilization rate, not biannual screening adherence. This sample included 50–64 (commercial insurance beneficiary age) and 65–74 (Medicare beneficiary age) year old women for whom the 2009 USPSTF guidelines recommended screening as a level B service. The ACA provides for cost sharing elimination for all preventive services deemed to be level A or B by the USPSTF. In this population, ACA requires screening be covered without any out-of-pocket costs. Inclusion of this population permits evaluation of the effect of ACA cost sharing elimination on the out-of-pocket costs experienced by these women undergoing screening and subsequent screening rates.
Among women 40–49 years, the USPSTF revised the 2002 screening mammography guidelines in 2009 from a level B service to a level C service. Inclusion of these women in our sample population allows evaluation of the effect of guideline revision on out of pocket costs experienced by these women undergoing screening. Of note, the ACA uses the 2002 guidelines for cost-share elimination. This further allows isolation of the effect of the cost-share elimination on screening utilization, compared to the effect of the 2009 guideline revision.
Analysis:
Patient cost-sharing (total out-of-pocket costs) at each calendar year was calculated as the sum of patient co-payments, co-insurance and deductible payments for each patient that underwent screening mammography. Patient-level analyses were used to examine changes in screening cost-sharing and utilization. All payments and cost estimates were adjusted to 2014 dollars using the Medical Consumer Price Index (CPI).
Screening mammography utilization was calculated as the proportion of all women with at least one claim for that service among all women enrolled for each year. Cost-sharing elimination, or first dollar coverage, of screening was defined as zero patient cost-sharing for the service date. The proportion of women without cost sharing for screening mammography each year was calculated as a proportion of those with first dollar coverage divided by all screening users. For women with more than one screening mammogram claim in a calendar year, only the first service claim was included in the analyses.
All analyses were performed and presented stratified by year of service. Demographic characteristics and levels of utilization are described by descriptive statistics such as medians and proportions. Low income women were defined as having household incomes at or below the 2015 poverty guidelines updated periodically in the Federal Register by the U.S. Department of Health and Human Services under the authority of 42 U.S.C. 9902(2)13. We anticipated that following the ACA, cost sharing for screening would fall rapidly as plans lost grandfathered status. Therefore, patient cost sharing was examined both among all patients that utilized service and among users with non-zero cost sharing each year. Reporting the adjusted median of the individual patient’s cost-sharing values provides a representation of the typical patient’s out of pocket cost per service visit that is robust to extreme cost values.
Median values and interquartile ranges were computed for all continuous measures. The above analyses were conducted for the whole population and for three age subpopulations, women 40–49, 50–64 and 65–74 years old. Interrupted time series analyses were run to assess cost-sharing trends before and after the ACA implementation, along with utilization trends before and after the USPSTF revised guidelines. These models were fit using generalized estimating equations (GEE) with robust standard errors, assuming a binomial distribution with a logit link function. Post-estimation commands were used to obtain the estimated trends over time (slope) in cost-sharing both before and after the ACA implementation, and also for utilization both before and after the USPSTF revised guidelines.
All analysis were conducted using Stata (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.)
RESULTS
We identified an average of 1,763,959 commercially insured women ages 40–74 years without a history of breast cancer or mastectomy with at least 12 months of continuous enrollment in a given plan per year. Characteristics of members and their health plans from 2004 to 2014 are shown in Table 1 and Appendix 1. Overall, the proportion of nonwhite women enrolled increased from 23% at the beginning of the observation period to 27% at the end. Similarly, the proportion of poor (less than 400% of the federal poverty level) enrollees increased over the time period from 25% to 27%.
Table 1:
Patient and plan characteristics of the study sample, by year.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | % | % | % | % | % | |
| Age group | |||||||||||
| 40–49 | 48.6 | 46.4 | 45.2 | 43.2 | 42.2 | 41.8 | 41.5 | 40.5 | 40.1 | 39.6 | 39.3 |
| 50–64 | 46.2 | 47.8 | 49.0 | 50.4 | 51.2 | 51.7 | 53.1 | 53.6 | 54.0 | 55.0 | 55.1 |
| 65–74 | 5.2 | 5.7 | 7.0 | 6.5 | 6.6 | 6.5 | 5.4 | 5.8 | 5.8 | 5.4 | 5.5 |
| Race/ Ethnicity | |||||||||||
| Asian | 2.5 | 2.6 | 2.6 | 2.7 | 3.0 | 3.1 | 3.2 | 3.3 | 3.5 | 3.7 | 4.0 |
| Black | 8.1 | 8.4 | 8.9 | 10.4 | 11.1 | 11.7 | 11.3 | 11.1 | 11.0 | 10.8 | 9.3 |
| Hispanic | 7.0 | 7.2 | 7.7 | 7.8 | 7.9 | 7.9 | 7.8 | 8.1 | 8.1 | 8.4 | 9.6 |
| Unknown | 5.3 | 4.9 | 4.5 | 4.1 | 3.9 | 3.8 | 3.8 | 3.9 | 3.9 | 4.0 | 4.2 |
| White | 77 | 77 | 76.2 | 75 | 74.1 | 73.5 | 73.8 | 73.7 | 73.7 | 73.1 | 72.8 |
| Poverty status | |||||||||||
| ≤400% FPL | 25.3 | 26.4 | 27.2 | 28.5 | 28.6 | 28.6 | 28.0 | 28.0 | 27.8 | 27.7 | 27.3 |
| > 400% FPL | 74.7 | 73.6 | 72.8 | 71.5 | 71.4 | 71.4 | 72.0 | 72.0 | 72.2 | 72.3 | 72.7 |
| Health plan type | |||||||||||
| Exclusive provider organization | 12.2 | 12.4 | 13.5 | 13.3 | 13.3 | 14.7 | 14.5 | 13.8 | 12.8 | 12.5 | 10.0 |
| Health maintenance organization | 19.5 | 14.7 | 12.5 | 9.9 | 10.8 | 10.0 | 9.0 | 9.2 | 9.3 | 9.0 | 8.9 |
| Indemnity | 2.5 | 2.9 | 2.7 | 2.4 | 2.2 | 18.5 | 1.6 | 1.3 | 1.1 | 0.8 | 0.9 |
| Other | 0.3 | 0.3 | 0.2 | 0.15 | 0.2 | 0.2 | 0.2 | 0.3 | 0.3 | 0.4 | 0.7 |
| Point of service | 51.5 | 60.1 | 63.1 | 67.1 | 67.9 | 68.5 | 71.6 | 72.6 | 74 | 74.7 | 77.6 |
| Preferred provider organization | 14.0 | 9.7 | 7.8 | 7.1 | 5.6 | 4.7 | 3.0 | 2.7 | 2.4 | 2.5 | 2.0 |
| Zero cost share for mammography service | 81.9 | 83.5 | 88 | 89.4 | 88.9 | 92.1 | 93.1 | 96.9 | 97.2 | 97.7 | 98.2 |
Between 2004 and 2014, the proportion of women with zero cost-share for screening increased from 81.9% (95% confidence interval (CI) 81.8–82.0) in 2004 to 98.2% (95%CI 98.2–98.3) in 2014 (p<0.001) (Figure 1). In 2010, the year that the ACA eliminated screening mammography cost-sharing for all non-grandfathered private insurance plans, the proportion of women without cost sharing reached 93.1%. The proportion of women with zero cost share increased over time (estimated slope=+0.014) in the years preceding 2010, when first dollar coverage of preventive services was implemented. The proportion of women with zero cost share continued to increase over time in the years after 2010 (estimated slope= +0.034), p<0.001).
Figure 1:
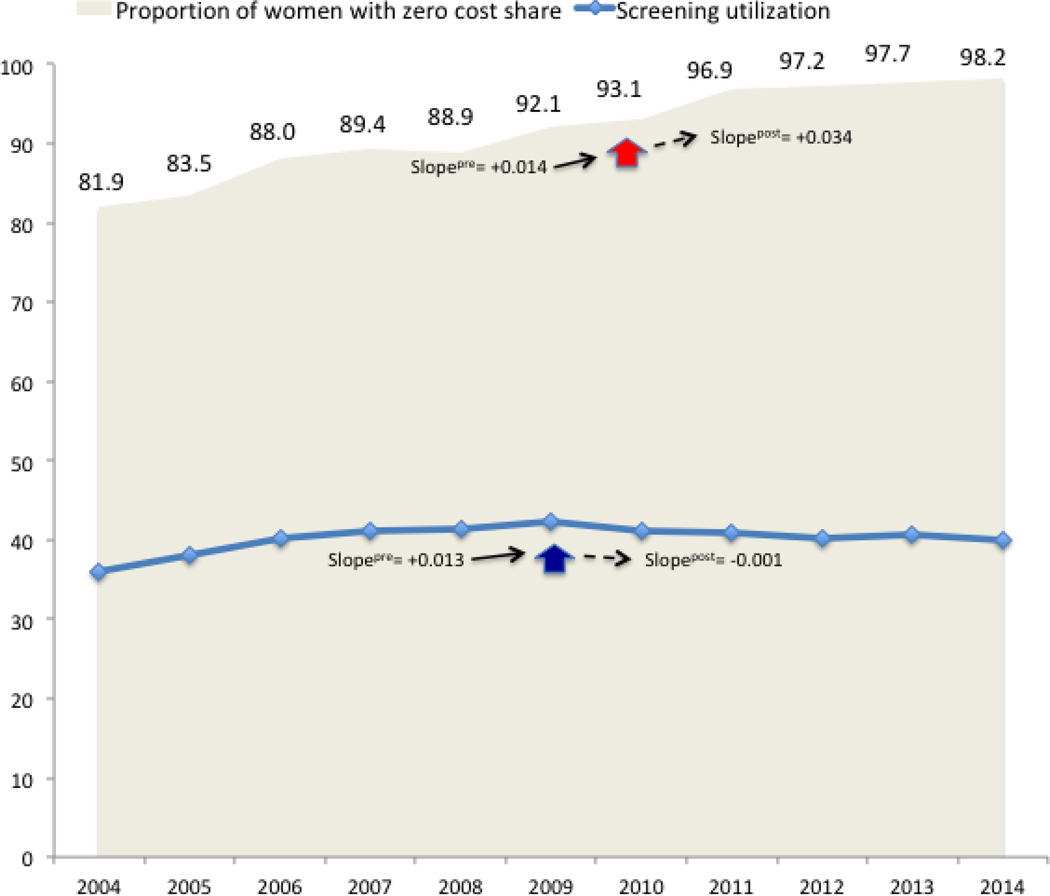
Patterns of cost sharing and utilization in screening mammography among privately insured women in the United States, 2004–2014. The gray area represents the proportion of patients with zero cost share over time. The proportion of patients with zero cost share rose before and after 2010 (red arrow), the year that the ACA provision for cost elimination for qualified preventive services was implemented. The blue line represents screening mammography utilization over time. Screening utilization increased until 2009, the year that the USPSTF revised its guideline for age of screening mammography initiation and frequency, flattening in the subsequent years.
Reflecting first dollar coverage for a large majority of the insured, the adjusted median cost-share over the entire screening population remained $0 (interquartile range (IQR) $0–0) across the whole population over the observation period. However, for women exposed to cost-sharing, 18.1% in 2004 down to 1.7% in 2014, adjusted median total out of pocket costs increased from $22 (IQR, $11–53) in 2004 to $46 (IQR, $16–104) in 2014 (Figure 2). Co-insurance represented the most frequent source of out-of-pocket costs. Adjusted median co-insurance for women required to share the cost of screening fluctuated over time (Figure 2).
Figure 2:
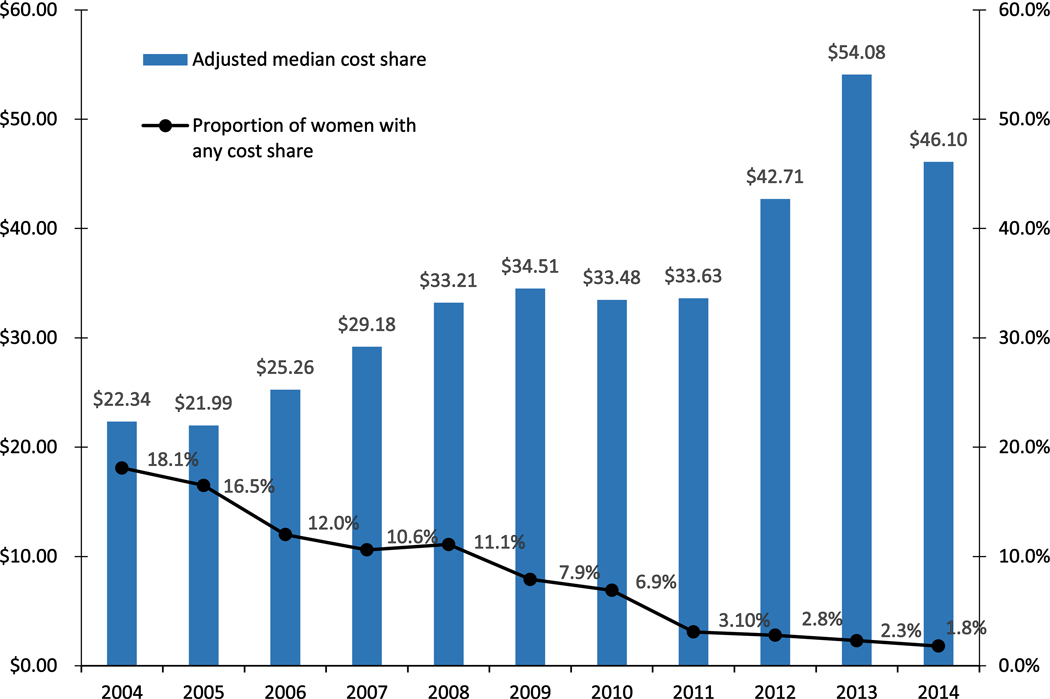
Median out-of-pocket costs for screening mammography among women with cost sharing, adjusted to 2014 dollars. The solid line describes the proportion of women for whom out-of-pocket costs have not been eliminated.
Patterns of cost-share elimination over time for all three age groups mirrored trends in the overall population (Figure 3). For women 40–49 years, 83.7% (95% CI 83.5–83.8) had first dollar coverage of screening mammography in 2004 rising to 98.6% (95% CI 98.5–98.6) by 2014 (Table 2). For those 50–64 years, 81.7% (95% CI 81.5–81.8) initially had first dollar coverage, rising to 98.1% (95% CI 98.0–98.1) by 2014. For those 65–74 years, 69.4% (95% CI 68.3–69.9), rising to 98.1 (95% CI 98.0–98.3). In all groups, the proportion of women with zero cost share increased over time before and after 2010 (Figure 3), (p<0.001).
Figure 3:
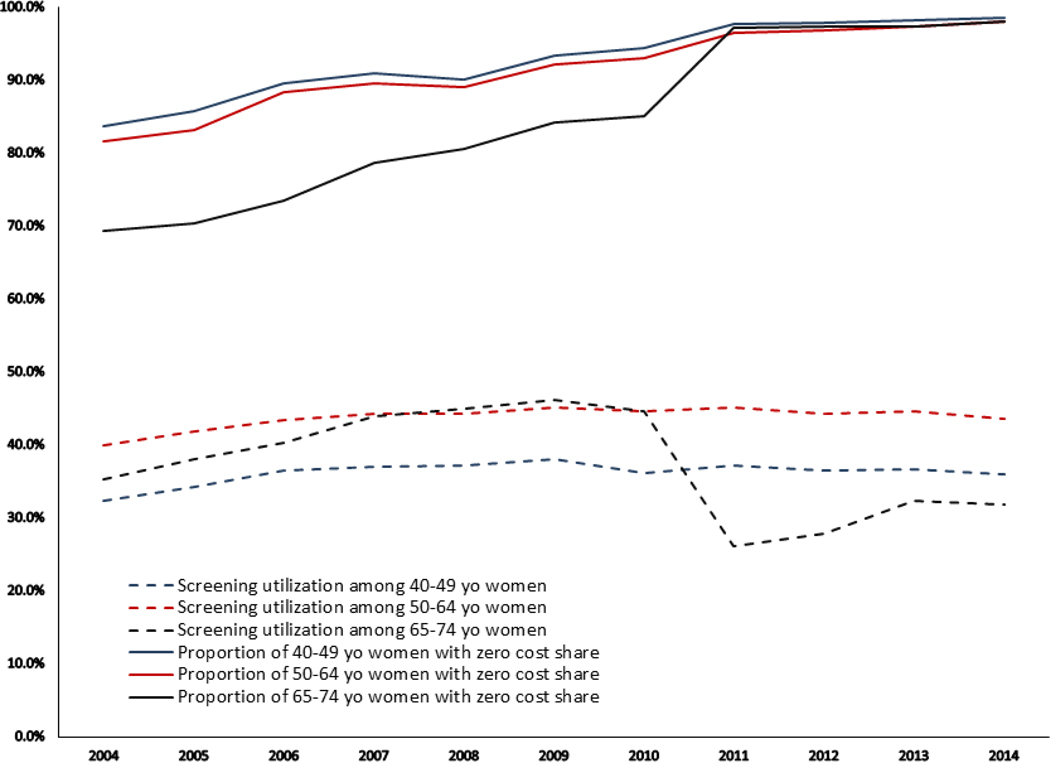
Patterns of cost sharing and utilization in screening mammography among privately insured women in the United States, 2004–2014, by age group. The solid lines represent the proportion of women with zero cost share, by age group. The dashed lines represent screening utilization, by age group. The patterns of cost share elimination and screening utilization over time among 40–49 year olds and 50–64 year olds mirror the overall population.
Table 2.
Mammography utilization and percent with zero cost share by age group.
| Year | Mammography Utilization % | Zero Cost Share % | ||||||
|---|---|---|---|---|---|---|---|---|
| All | 40–49 yo | 50–64 yo | 65–74 yo | All | 40–49 yo | 50–64 yo | 65–74 yo | |
| 2004 | 36.0 | 32.3 | 40.0 | 35.3 | 81.9 | 83.7 | 81.7 | 69.4 |
| 2005 | 38.1 | 34.3 | 41.9 | 38.1 | 83.5 | 85.8 | 83.1 | 70.4 |
| 2006 | 40.1 | 36.5 | 43.4 | 40.3 | 88.0 | 89.6 | 88.3 | 73.5 |
| 2007 | 41.1 | 37.0 | 44.3 | 44.0 | 89.4 | 90.9 | 89.6 | 78.7 |
| 2008 | 41.3 | 37.2 | 44.0 | 44.9 | 88.9 | 90.1 | 89.1 | 80.6 |
| 2009 | 42.2 | 38.0 | 45.1 | 46.1 | 92.1 | 93.3 | 92.2 | 84.2 |
| 2010 | 41.1 | 36.1 | 44.6 | 44.7 | 93.1 | 94.4 | 93.1 | 85.0 |
| 2011 | 40.8 | 37.2 | 45.2 | 26.2 | 96.9 | 97.7 | 96.4 | 97.1 |
| 2012 | 40.2 | 36.5 | 44.2 | 27.9 | 97.2 | 97.8 | 96.8 | 97.3 |
| 2013 | 40.7 | 36.6 | 44.6 | 32.3 | 97.7 | 98.2 | 97.4 | 97.3 |
| 2014 | 39.9 | 36.0 | 43.5 | 31.8 | 98.2 | 98.6 | 98.1 | 98.1 |
Initially at 36.0% (95% CI 36.0–36.1) in 2004, screening utilization peaked at 42.2% (95% CI 42.1–42.3) in 2009, the year that the USPSTF guidelines change, and drops to 39.9% (95% CI 39.8–40.0) in 2014. Screening utilization increased over time (estimated slope=+0.013) in the years preceding 2009, when the USPSTF revised their screening recommendations. Screening utilization flattened in the years after 2010 (estimated slope= −0.001), p<0.001) (Figure 1). Comparing women ages 40–49, 50–64 and 65–74, patterns of screening utilization for 40–49 and 50–64 years old women paralleled the trends in the overall population, peaking at 38.0% (95% CI 37.9–38.01) in 2009 for ages 40–49 and 45.2% (95% CI 45.1–45.3) in 2011 for ages 50–64 (Table 2). Peak screening utilization for ages 65–74 was 46.10% (95% CI 45.8–46.3) in 2009 followed by a sharp drop in 2011 (26.2%, 95% CI 25.9–26.5) then a slow increase thereafter (Figure 3).
DISCUSSION
Prior to the ACA, employer-provided health insurance plans granted first dollar coverage for screening mammography to a substantial majority of their beneficiaries. ACA implementation resulted in near universal elimination of cost-sharing. Despite USPSTF guideline revision in 2009, these health plans continued to provide the same level of screening coverage for women ages 40–49 as for those ages 50–74. Despite the ACA’s elimination of cost-sharing for qualified preventive services, screening utilization gradually declined immediately after 2009 suggesting that the expected increases in use due to lower out of pockets costs, were offset by reductions resulting from the USPSTF guideline revision. Similar trends in decreasing mammography utilization is noted among all three age groups (40–49, 50–64 and 65–74). This effect is most pronounced in the Medicare beneficiary age group, which experienced a precipitous drop in utilization immediately after the guideline change with a modest rebound in later years. Despite rising rates of screening in this age group after 2012, at the end of the observation period, the rates still lagged those in the younger age groups. The guideline change produced greater effects on both guideline-concordant utilization reduction among 40–49 year olds and guideline-discordant utilization reduction among those 50 and older.
Not previously reported, we observed that despite USPSTF guideline revision, employer-provided health plans continued to provide the same level of first dollar screening coverage for women ages 40–49 as for those ages 50–74. Utilization trends in 40–49 and 50–64 years old subpopulations mirror the overall trend for declining use of screening after USPSTF guideline revision. The fear that the USPSTF downgrading of the evidence quality for screening among 40–49 year olds leads to withdrawal of service coverage14 has not materialized, at least of our population, likely as ACA is required to use the 2002 screening mammography guidelines for cost-share elimination. However, continued and expanded first dollar coverage has not resulted in enhanced screening in either age group, perhaps due to other barriers to screening. Our results are in line with previous study by Jena et al. showing mammography utilization decreased in Medicare beneficiary age group in a large Medicare Advantage health maintenance organization15, however we observed a dramatically sharp drop in our study (from 46.1% in 2009 to 26.2% in 2011).
We observed annual mammography utilization rates decreased after ACA cost sharing elimination in 2010 in all age groups. As of October 2010, the ACA mandated elimination of cost sharing for USPSTF level A or B preventive services including screening11.This mandate applied to all private insurance plans, except for grandfathered plans which did not have to comply. Medicare had already eliminated deductibles for screening mammography for beneficiaries in 199716 and expanded first dollar coverage in January 201117. Comparing grandfathered plans to nongrandfathered plans offered by small businesses, approximately 90% of mammography services for 50–64 year olds were already fully covered by both plan types and mammography rates remained stable between October 2008 and May 2012. Despite elimination of a $20 copayment for screening among Medicare eligible beneficiaries, screening rates declined in a large MA health maintenance organization15. In studies that evaluated national samples of Medicare beneficiaries, screening mammography rates did not change after first dollar coverage18,19 or only modestly increased17. The initial effort to reduce out-of-pocket costs through deductible elimination in 1997 resulted in a 25% increase in screening rates up to four years afterward16 while early elimination of mammography deductibles in preferred provider organization (PPO) in 2002 resulted in increased utilization as of 2006. Our study among others demonstrate that ACA cost share elimination did not result in increased screening rates unlike much earlier efforts to reduce financial barriers to preventive services, likely due to the high proportion of employer-insured women who already had screening cost share eliminated prior to the ACA implementation. Our results are consistent with Trivedi et al who reported no increase in screening adherence in plans already had full coverage for screening mammography during the study duration20.
Extensive efforts to improve breast cancer screening predate the ACA, including the near complete elimination of financial barriers to breast screening in the employed insured population, suggesting that at least for this population, we may be experiencing a ceiling effect in further responses of screening rates to patient financial incentives to reduce screening cost. Improving breast cancer screening rates may require direct payments to women in addition to offering the test itself for free. Alternatively, shared financial incentives for physicians and patients may further increase screening over physician or patient incentives alone similar to cholesterol level reduction experienced by patients with elevated risk of a cardiac event or stroke who were on statin therapy21. Women concerned about downstream costs that they may incur from a positive screen may elect not to undergo the free mammogram22. Particularly for the employed insured, additional costs such the need to take time off work 23,24 or arrange for childcare25 have been cited as barriers to screening. Competing priorities such as other health concerns perceived as more salient than cancer screening predict nonadherence 26–28.
Another factor that may mitigate the ACA’s goal to increase consumers’ use of high value services is that it is difficult to know in advance how much a visit will cost among grandfathered plans. Predicting the total cost-share of a screening visit should be straightforward, it should be free. However, the challenge is knowing whether one’s insurance plan represents one of the few remaining grandfathered plans allowed to charge a cost share for breast cancer screening. For non-pharmacy related services, VBID may require better way to communicate insurance plan characteristics to consumers, including benefit coverage, coupled with communication of the clinical value of preventive services, independent of cost-share elimination.
Overall, the key lesson learned from this study and others evaluating the impact of the ACA on screening utilization is that the ACA achieved its goal to improve screening service utilization by eliminating cost share as a barrier in populations that had an existing cost share prior to ACA implementation. For our population insured in employer-provided plans, these plans already provided the full coverage of mammography screening for the vast majority of their insured women that the ACA had a muted effect on screening mammography utilization, outweighed by the effect of the USPSTF guideline change.
Limitations:
We expressed use of screening mammography services as annual utilization rate, rather than biennial adherence rate as reported by the Behavioral Risk Factors Screening Surveillance (BRFSS) and by the American Cancer Society, hence are approximately half of the rates we previously reported using the BRFSS29. As this is a descriptive cross sectional study, we cannot assess whether individual women experienced reductions in their cost sharing or changed their use of screening mammography in response. Future longitudinal studies should be conducted to clarify this question. Second, while using administrative data offers the opportunity to examine changes in large populations, it has inherent weaknesses. Variation in coding and billing likely contributes in part to the variation in cost sharing we observed. Further, the interrupted time series models that were used for significance testing did control for patient specific dependence but did not control for the potential dependence due to patients being nested within the same plan.
Conclusion
Few commercially insured women were subject to cost-sharing for mammography before the ACA was passed. The ACA mandated elimination of consumer out of pocket costs for mammography was successful in extending this removal of cost-sharing to nearly all women. The lack of a significant increase in mammography use post-ACA can be partially attributed by a guideline change that recommended less frequent screening intervals, the high proportion women who had no cost-sharing prior to ACA, and the relatively low levels of cost sharing prior to the policy implementation. As demonstrated for other high value services, the removal of out-of-pocket costs does guarantee that consumers will receive clinically indicated care, particularly where cost share existed prior to the ACA. Accordingly, targeted clinician and consumer-facing programs are warranted to enhance appropriate mammography utilization.
Take Home Points:
The ACA requires elimination of cost-sharing for high-value preventive services to decrease cost as a barrier to utilization and improve access.
In 2009, the USPSTF revised guidelines downgrading routine screening mammography among women 40–49 potentially increasing the barrier to screening this group.
Evaluation of claims data for employed insured women demonstrated that in the year prior to ACA implementation reached 92% and 98% four years after.
ACA implementation had no effect on breast screening utilization, while USPSTF guideline change resulted in a significant decrease.
The effects of the ACA and USPSTF on breast screening utilization was not significantly different between women ages 40–49 and those 50 and over.
Acknowledgments
This study was coordinated by the ECOG-ACRIN Cancer Research Group (Robert L. Comis, MD and Mitchell D. Schnall, MD, PhD, Group Co-Chairs) and supported by the National Cancer Institute of the National Institutes of Health under the following award numbers: CA189828, CA180801. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
APPENDIX
Appendix 1:
Patient and plan characteristics of the study sample by plan year (expanded).
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2,012 | 2,013 | 2,014 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total eligible women | 1,541,293 | 1,682,880 | 1,717,175 | 1,812,643 | 1,877,042 | 1,899,439 | 1,822,460 | 1,859,587 | 1,834,060 | 1,806,802 | 1,550,172 | |||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Age group | ||||||||||||||||||||||
| 40–49 | 748738 | 48.6 | 781201 | 46.4 | 776330 | 45.2 | 782,219 | 43.2 | 792520 | 42.2 | 793317 | 41.8 | 756609 | 41.5 | 753,605 | 40.5 | 735914 | 40.1 | 714790 | 39.6 | 610755 | 39.3 |
| 50–64 | 712430 | 46.2 | 805231 | 47.8 | 841223 | 49 | 912,690 | 50.4 | 961148 | 51.2 | 982932 | 51.7 | 968118 | 53.1 | 997,685 | 53.6 | 991603 | 54.0 | 994378 | 55.0 | 853726 | 55.1 |
| 65–74 | 80125 | 5.2 | 96448 | 5.7 | 99d622 | 7 | 117,734 | 6.5 | 123374 | 6.6 | 123190 | 6.5 | 97733 | 5.4 | 108,297 | 5.8 | 106543 | 5.8 | 97634 | 5.4 | 85691 | 5.5 |
| Race/ Ethnicity | ||||||||||||||||||||||
| Asian | 37238 | 2.5 | 41319 | 2.6 | 44,430 | 2.6 | 48950 | 2.7 | 54565 | 3 | 57346 | 3.1 | 58151 | 3.2 | 60169 | 3.3 | 63253 | 3.5 | 66434 | 3.7 | 61166 | 4 |
| Black | 119293 | 8.1 | 135118 | 8.4 | 149183 | 8.9 | 184593 | 10.4 | 204731 | 11.1 | 217844 | 11.7 | 203382 | 11.3 | 203142 | 11.1 | 194204 | 11 | 189518 | 10.8 | 143698 | 9.3 |
| Hispanic | 102636 | 7 | 117034 | 7.2 | 128774 | 7.7 | 138335 | 7.8 | 146347 | 7.9 | 148630 | 7.9 | 139647 | 7.8 | 147783 | 8.1 | 146298 | 8.1 | 149079 | 8.4 | 148393 | 9.6 |
| Unknown | 77716 | 5.3 | 78578 | 4.9 | 75769 | 4.5 | 72523 | 4.1 | 71977 | 3.9 | 71139 | 3.8 | 68864 | 3.8 | 70667 | 3.9 | 70794 | 3.9 | 70865 | 4.0 | 64498 | 4.2 |
| White | 1127103 | 77 | 1244468 | 77 | 1277982 | 76.2 | 1335906 | 75 | 1369492 | 74.1 | 1374358 | 73.5 | 1323619 | 73.8 | 1348028 | 73.7 | 1327896 | 73.7 | 1296616 | 73.1 | 1119535 | 72.8 |
| Poverty status | ||||||||||||||||||||||
| ≤ 400% FPL | 166484 | 25.3 | 216758 | 26.4 | 263015 | 27.2 | 351354 | 28.5 | 443456 | 28.6 | 484987 | 28.6 | 456895 | 28 | 467937 | 28 | 457793 | 27.8 | 446216 | 27.7 | 377226 | 27.3 |
| > 400% FPL | 490780 | 74.7 | 603230 | 73.6 | 704202 | 72.8 | 883257 | 71.5 | 1106552 | 71.4 | 1207793 | 71.4 | 1172272 | 72 | 1201347 | 72 | 1189682 | 72.2 | 1164497 | 72.3 | 1005723 | 72.7 |
| Health plan type | ||||||||||||||||||||||
| Exclusive provider organization | 188227 | 12.2 | 208464 | 12.4 | 231443 | 13.5 | 241,700 | 13.3 | 250424 | 13.3 | 278490 | 14.7 | 264555 | 14.5 | 257321 | 13.8 | 234274 | 12.8 | 225,590 | 12.5 | 152754 | 10 |
| Health maintenance organization | 300351 | 19.5 | 246983 | 14.7 | 213850 | 12.5 | 179418 | 9.9 | 203425 | 10.8 | 190703 | 10.0 | 164262 | 9.0 | 172422 | 9.2 | 170999 | 9.3 | 163472 | 9 | 138436 | 8.9 |
| Indemnity | 37795 | 2.5 | 48321 | 2.9 | 47184 | 2.7 | 42813 | 2.4 | 40668 | 2.2 | 35151 | 18.5 | 28570 | 1.6 | 24507 | 1.3 | 19967 | 1.1 | 15208 | 0.8 | 13294 | 0.9 |
| Other | 4764 | 0.3 | 4,566 | 0.3 | 2842 | 0.2 | 2720 | 0.15 | 3399 | 0.2 | 4060 | 0.2 | 4640 | 0.2 | 5043 | 0.3 | 6393 | 0.3 | 7974 | 0.4 | 11573 | 0.7 |
| Point of service | 793903 | 51.5 | 1011096 | 60.1 | 1084223 | 63.1 | 1216779 | 67.1 | 1273626 | 67.9 | 1301432 | 68.5 | 1304292 | 71.6 | 1348917 | 72.6 | 1356900 | 74 | 1349249 | 74.7 | 1202317 | 77.6 |
| Preferred provider organization | 216253 | 14.0 | 163450 | 9.7 | 137112 | 7.8 | 128813 | 7.1 | 105073 | 5.6 | 88964 | 4.7 | 55457 | 3.0 | 50751 | 2.7 | 44810 | 2.4 | 44475 | 2.5 | 31521 | 2 |
| Zero cost share for mammography service | 455037 | 81.9 | 535894 | 83.5 | 605499 | 88 | 666513 | 89.4 | 688749 | 88.9 | 737797 | 92.1 | 696861 | 93.1 | 735804 | 96.9 | 715723 | 97.2 | 718,904 | 97.7 | 607449 | 98.2 |
Footnotes
Conflict of interest
The authors declare that they do not have a conflict of interest.
References
- 1.ObamaCare Facts: Facts on the Affordable Care Act. 2017. https://obamacarefacts.com/obamacare-facts/. Accessed January 18, 2018.
- 2.Obama B United States Health Care Reform: Progress to Date and Next Steps. JAMA. 2016;316(5):525–532. doi: 10.1001/jama.2016.9797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choudhry NK, Fischer MA, Smith BF, et al. Five features of value-based insurance design plans were associated with higher rates of medication adherence. Health Aff (Millwood). 2014;33(3):493–501. doi: 10.1377/hlthaff.2013.0060. [DOI] [PubMed] [Google Scholar]
- 4.Frank MB, Fendrick AM, He Y, et al. The effect of a large regional health plan’s value-based insurance design program on statin use. Med Care. 2012;50(11):934–939. doi: 10.1097/MLR.0b013e31826c8630. [DOI] [PubMed] [Google Scholar]
- 5.Sepúlveda M-J, Roebuck MC, Fronstin P, Vidales-Calderon P, Parikh A, Rhee K. Elimination of the Out-of-Pocket Charge for Children’s Primary Care Visits: An Application of Value-Based Insurance Design. J Pediatr. 2016;175:195–200. doi: 10.1016/j.jpeds.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Hirth RA, Cliff EQ, Gibson TB, McKellar MR, Fendrick AM. Connecticut’s Value-Based Insurance Plan Increased The Use Of Targeted Services And Medication Adherence. Health Aff (Millwood). 2016;35(4):637–646. doi: 10.1377/hlthaff.2015.1371. [DOI] [PubMed] [Google Scholar]
- 7.Maeng DD, Pitcavage JM, Snyder SR, Davis DE. The value of value-based insurance design: savings from eliminating drug co-payments. Am J Manag Care. 2016;22(2):116–121. http://www.ncbi.nlm.nih.gov/pubmed/26885671. [PubMed] [Google Scholar]
- 8.Maciejewski ML, Wansink D, Lindquist JH, Parker JC, Farley JF. Value-based insurance design program in north Carolina increased medication adherence but was not cost neutral. Health Aff (Millwood). 2014;33(2):300–308. doi: 10.1377/hlthaff.2013.0260. [DOI] [PubMed] [Google Scholar]
- 9.Lee JL, Maciejewski M, Raju S, Shrank WH, Choudhry NK. Value-based insurance design: quality improvement but no cost savings. Health Aff (Millwood). 2013;32(7):1251–1257. doi: 10.1377/hlthaff.2012.0902. [DOI] [PubMed] [Google Scholar]
- 10.Health Care Costs Are a Barrier to Care for Many Women. Urban Institute Health Policy Center. http://hrms.urban.org/briefs/Health-Care-Costs-Are-a-Barrier-to-Care-for-Many-Women.html. 2015. Accessed January 18, 2018.
- 11.Coverage of Preventive Services. https://www.federalregister.gov/documents/2013/07/02/2013-15866/coverage-of-certain-preventive-services-under-the-affordable-care-act. Accessed January 18, 2018.
- 12.U.S. Preventive Services Task Force Recommendations. Breast Cancer Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening. Accessed January 18, 2018.
- 13.U.S. Federal Poverty Guidelines Used to Determine Financial Eligibility for Certain Federal Programs. Office of the Assistant Secretary for Planning and Evaluation. U.S. Department of Health and Human Services. https://aspe.hhs.gov/2015-poverty-guidelines. Accessed January 18, 2018. [Google Scholar]
- 14.17M Women Could Lose Mammogram Coverage Under Draft Recommendations From USPSTF. Society of Breast Imaging. 4/11/2017.28. Pearson CF: Updated Breast Cancer Screening Recommendation of Mammography for 17M Women; Avalere 2015. http://avalere.com/expertise/managed-care/insights/updated-breast-cancer-screening-recommendation-could-eliminate-guaranteed-c. Accessed January 18, 2018. [Google Scholar]
- 15.Jena AB, Huang J, Fireman B, et al. Screening Mammography for Free: Impact of Eliminating Cost Sharing on Cancer Screening Rates. Health Serv Res. 2017;52(1):191–206. doi: 10.1111/1475-6773.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goodwin SM, Anderson GF. Effect of cost-sharing reductions on preventive service use among Medicare fee-for-service beneficiaries. Medicare Medicaid Res Rev. 2012;2(1). doi: 10.5600/mmrr.002.01.a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sabatino SA, Thompson TD, Guy GP, de Moor JS, Tangka FK. Mammography Use Among Medicare Beneficiaries After Elimination of Cost Sharing. Med Care. 2016;54(4):394–399. doi: 10.1097/MLR.0000000000000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fedewa SA, Goodman M, Flanders WD, et al. Elimination of cost-sharing and receipt of screening for colorectal and breast cancer. Cancer. 2015;121(18):3272–3280. doi: 10.1002/cncr.29494. [DOI] [PubMed] [Google Scholar]
- 19.Jensen GA, Salloum RG, Hu J, Ferdows NB, Tarraf W. A slow start: Use of preventive services among seniors following the Affordable Care Act’s enhancement of Medicare benefits in the U.S. Prev Med (Baltim). 2015;76:37–42. doi: 10.1016/j.ypmed.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 20.Trivedi AN, Leyva B, Lee Y, Panagiotou OA, Dahabreh IJ. Elimination of Cost Sharing for Screening Mammography in Medicare Advantage Plans. N Engl J Med. 2018;378(3):262–269. doi: 10.1056/NEJMsa1706808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asch DA, Troxel AB, Stewart WF, et al. Effect of Financial Incentives to Physicians, Patients, or Both on Lipid Levels: A Randomized Clinical Trial. JAMA. 2015;314(18):1926–1935. doi: 10.1001/jama.2015.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Highfield L, Bartholomew LK, Hartman MA, Ford MM, Balihe P. Grounding evidence-based approaches to cancer prevention in the community: a case study of mammography barriers in underserved African American women. Health Promot Pract. 2014;15(6):904–914. doi: 10.1177/1524839914534685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gany FM, Herrera AP, Avallone M, Changrani J. Attitudes, knowledge, and health-seeking behaviors of five immigrant minority communities in the prevention and screening of cancer: a focus group approach. Ethn Health. 2006;11(1):19–39. doi: 10.1080/13557850500391394. [DOI] [PubMed] [Google Scholar]
- 24.Moy B, Park ER, Feibelmann S, Chiang S, Weissman JS. Barriers to repeat mammography: cultural perspectives of African-American, Asian, and Hispanic women. Psychooncology. 2006;15(7):623–634. doi: 10.1002/pon.994. [DOI] [PubMed] [Google Scholar]
- 25.Watson-Johnson LC, DeGroff A, Steele CB, et al. Mammography adherence: a qualitative study. J Womens Health (Larchmt). 2011;20(12):1887–1894. doi: 10.1089/jwh.2010.2724. [DOI] [PubMed] [Google Scholar]
- 26.Ahmed NU, Fort JG, Elzey JD, Bailey S. Empowering factors in repeat mammography: insights from the stories of underserved women. J Ambul Care Manage. 2004;27(4):348–355. http://www.ncbi.nlm.nih.gov/pubmed/15495747. [DOI] [PubMed] [Google Scholar]
- 27.Lopez EDS, Khoury AJ, Dailey AB, Hall AG, Chisholm LR. Screening mammography: a cross-sectional study to compare characteristics of women aged 40 and older from the deep South who are current, overdue, and never screeners. Womens Health Issues. 2009;19(6):434–445. doi: 10.1016/j.whi.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Makuc DM, Breen N, Meissner HI, Vernon SW, Cohen A. Financial barriers to mammography: who pays out-of-pocket? J Womens Health (Larchmt). 2007;16(3):349–360. doi: 10.1089/jwh.2006.0072. [DOI] [PubMed] [Google Scholar]
- 29.Dehkordy SF, Hall KS, Roach AL, Rothman ED, Dalton VK, Carlos RC. Trends in Breast Cancer Screening: Impact of U.S. Preventive Services Task Force Recommendations. Am J Prev Med. 2015;49(3):419–422. doi: 10.1016/j.amepre.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]


