Abstract
Objective:
We applied the experimental therapeutics approach to test whether acute treatment outcomes for winter seasonal affective disorder (SAD) are mediated by a cognitive mechanism in cognitive-behavioral therapy (CBT-SAD) versus a chronobiologic mechanism in light therapy (LT).
Method:
Currently depressed adults with Major Depression, Recurrent with Seasonal Pattern (N = 177; 83.6% female, 92.1% non-Hispanic White, M age = 45.6) were randomized to 6 weeks of LT or group CBT-SAD. SAD symptoms were assessed weekly on the Structured Clinical Interview for the Hamilton Rating Scale for Depression-SAD Version. At pre-, mid-, and post-treatment, participants completed measures of general depressogenic cognitions (Dysfunctional Attitudes Scale; DAS); SAD-specific negative cognitions (Seasonal Beliefs Questionnaire; SBQ); chronotype (Morningness-Eveningness Questionnaire; MEQ), and depressive symptoms (Beck Depression Inventory-Second Edition).
Results:
Parallel-process growth models showed evidence for hypothesized mechanisms. For SAD-specific negative cognitions (SBQ), both symptom measures showed (1) an effect of treatment group on the slope of the mediator, with CBT-SAD demonstrating greater decreases, and (2) an effect of the slope of the mediator on the slope of the outcome. These effects held for the SBQ but not the broader measure of depressogenic cognitions (DAS). For the chronotype measure (MEQ), treatment assignment affected change whereby LT was associated with reduced “eveningness,” but this was unrelated to change in symptoms.
Conclusions:
CBT-SAD promoted decreases in SAD-specific negative cognitions, and these changes were related to decreases in symptoms. Consistent with the theory that LT corrects misaligned circadian rhythms, LT reduced eveningness, but this did not correspond to symptom improvement.
Public Health Significance:
This study suggests that cognitive-behavioral therapy for winter depression might exert its acute antidepressant effects though changing maladaptive beliefs about the seasons, light availability, and weather rather than through change in more generic depressogenic beliefs. In contrast, light therapy is associated with a change in chronotype (i.e., a change in diurnal preference towards less eveningness), but change in chronotype is not mechanistic of light therapy’s acute antidepressant effects.
Keywords: Experimental therapeutics, mediators, seasonal affective disorder, cognitive-behavioral therapy, light therapy
In its Strategic Plan for Research, the National Institute of Mental Health (NIMH, 2015) calls for an experimental medicine or therapeutics approach, whereby clinical trials are designed to test an intervention’s mechanisms of action as well as its efficacy. The experimental therapeutics approach assumes that modifying a target (i.e., a hypothesized mechanism of action) will cause improvement in symptoms, behaviors, and/or functional outcomes (NIMH, 2015). NIMH’s Funding Opportunity Announcements (FOAs) for clinical trials seek studies designed to provide evidence of “target engagement” (i.e., a significant difference in target change between the experimental and comparator treatments) and “target validation” (i.e., an association between changes in target and in outcome in the hypothesized direction). Regarding these FOAs, Insel and Gotay (2014) wrote, “Every trial will need to include a mediator that tests the mechanism of action…” (p. 746).
NIMH’s funding priority for experimental therapeutics is consistent with psychotherapy research’s longstanding focus on identifying key mechanisms driving symptom change during treatment (i.e., testing mediators). An intervening variable emerges as a mediator when a treatment first changes the intervening variable and then this change accounts for subsequent change in outcome, which requires assessing both the potential mediator and outcome at least three times (Kazdin, 2007; Kraemer, Wilson, Fairburn, & Agras, 2002). According to Kazdin (2007), demonstrating statistical mediation is a first step towards elucidating a treatment’s potential mechanism of action (i.e., the actual causal process responsible for change). Mediation is necessary but not sufficient to identify a mechanism, with additional requirements to establish a mediator as a mechanism (e.g., replication, experimental manipulation of the mediator, dose-response relationships between mediator and outcome; see Kazdin, 2007). Elucidating mediators of evidence-based interventions can improve treatment outcomes through enhanced attention towards the active ingredients responsible for change. Mediators of symptom improvement have been examined in various psychotherapies for depression (for a review, see Lemmens, Müller, Arntz, & Huibers, 2016). Here, we apply the experimental therapeutics approach and contribute to that literature by examining mediators of antidepressant effects in our recently completed randomized clinical trial comparing two first-line treatments for winter seasonal affective disorder (SAD): bright light therapy (LT; Golden et al., 2005) and cognitive-behavioral therapy (CBT-SAD; Rohan, 2008).
SAD, a recurrent subtype of depression wherein major depression emerges in the fall or winter months and remits in the spring or summer months annually (Rosenthal, 1984), is an important public health challenge. Data on over 600 SAD patients at the NIMH Seasonal Studies Program 1981-2001 suggest that an untreated fall/winter major depressive episode persists for an average 4.9±1.4 months before spontaneous springtime remission (N. E. Rosenthal, personal communication, May 24, 2005). A multisite study of 1,042 SAD patients reported a mean age for onset of 27.2 years and, on average, 13.4 past fall/winter major depressive episodes (Modell et al., 2005). Underscoring the cumulative burden of SAD, these data suggest that SAD patients spend over 40% of the year struggling with substantial depressive symptoms, beginning in young adulthood.
The integrative cognitive-behavioral model of SAD (Rohan, Roecklein, & Haaga, 2009) articulates the assumed targets and mechanisms of CBT-SAD and LT. The model assumes that CBT-SAD targets and improves psychological vulnerabilities to SAD, such as dysfunctional attitudes, rumination, and behavioral disengagement, whereas LT targets and improves physiological vulnerabilities to SAD (i.e., circadian phase shifts, retinal subsensitivity to light, and increased duration of nocturnal melatonin release). Despite these plausible and distinct pathways to antidepressant effects in CBT-SAD vs. LT, the mechanisms through which each treatment fosters symptom change are not well established. A better understanding of how each treatment facilitates change in seasonal depression symptoms has both clinical and scientific implications. In practice, knowing the mechanisms would allow clinicians to assess and monitor target engagement to maximize treatment effectiveness within particular patients. In research, a better understanding of mechanisms underlying effective treatments could inform studies testing refinements of the treatment protocols themselves to increase emphasis on those treatment components most robustly driving treatment effects.
Relative to the understudied mechanisms of CBT-SAD, there is a literature examining cognitive contents and processes as mediators of cognitive-behavioral therapy’s (CBT’s) acute effects on nonseasonal depression. According to Beck’s cognitive model of depression (Beck, Rush, Shaw, & Emery, 1979), depressed individuals possess maladaptive cognitive schemata containing dysfunctional attitudes that elicit negative emotional and behavioral reactions to stressful events. The model assumes that modifying dysfunctional attitudes causes the reduction in depressive symptoms in CBT (Hamilton & Dobson, 2002). Using designs that assessed both mediator and outcome at least three times to address the issue of temporal precedence, several studies have examined dysfunctional attitudes as a mediator of outcomes in CBT relative to various psychotherapies and pharmacological treatments for depression. For example, DeRubeis and colleagues (1990) found that dysfunctional attitudes mediated depressive symptom change in CBT, but not in pharmacotherapy, such that change in dysfunctional attitudes from pre- to mid-treatment predicted change in depression from mid- to post-treatment only in CBT.
Most studies designed to address the issue of temporal precedence have failed to support the mediational role of dysfunctional attitudes in CBT for depression. For example, although Vittengl, Clark, Thase, and Jarrett (2014) observed concurrent changes in dysfunctional attitudes and depressive symptoms; early (i.e., pre- to mid-treatment) change in dysfunctional attitudes did not significantly account for later (i.e., mid- to post-treatment) change in depression over acute CBT. Similarly, in both Interpersonal Psychotherapy (IPT) and CBT; Lemmens, Galindo-Garre, Arntz et al. (2017) reported a significant concurrent relation between change in dysfunctional attitudes and improvement in depressive symptoms during the second half of treatment. Although dysfunctional attitudes at mid-treatment were associated with mid- to post-treatment change in depression, Lemmens et al. (2017) failed to find a significant temporal relation between early change in dysfunctional attitudes and subsequent change in depression. Therefore, neither the Lemmens et al. (2017) nor the Vittengl et al. (2014) study supports dysfunctional attitudes as a mediator of depression change in CBT, according to the sophisticated definition of mediation we adopt here, wherein earlier dysfunctional attitudes change would need to account for later depressive symptom change. Warmerdam, van Straten, Jongsma, Twisk, and Cuijpers (2010) identified dysfunctional attitudes as mediators of depression symptom change in two online depression treatments, CBT and problem-solving therapy (PST). However, when dysfunctional attitudes were entered simultaneously with other mediators; worrying, perceived control, and a negative problem orientation predicted depressive symptoms in both treatments whereas dysfunctional attitudes did not. In addition, they observed a negative correlation between early (i.e., first 5 weeks) change in dysfunctional attitudes and later (i.e., last 3 weeks) change in depression in CBT, such that larger early reductions in dysfunctional attitudes were associated with smaller later improvements in depression. As Warmerdam et al. (2010) acknowledge, they were limited in their ability to draw case and effect inferences from their data because the majority of total change in depressive symptoms occurred between pre-treatment and the mid-point (i.e., 5-week) assessment, with relatively limited change between weeks 5 and 8 (i.e., post-treatment).
We recently developed a measure of SAD-specific cognitions about the seasons, light availability, and weather called the Seasonal Beliefs Questionnaire (SBQ; Rohan et al., 2019). The SBQ was inspired by our clinical observations of SAD patients endorsing negative thoughts about the winter season, short photoperiods, environmental cues signaling winter, and inclement weather conditions and positive thoughts about the summer season, long photoperiods, environmental cues signaling spring, and favorable weather conditions. Items were derived from a qualitative analysis of negative thoughts reported during CBT-SAD sessions, particularly during sessions where these thoughts are primed and elicited by presenting various scenarios (e.g., waking up on an overcast, cold, snowy winter day). Although CBT-SAD involves the traditional CBT for depression components of behavioral activation, cognitive restructuring, and relapse prevention, it is possible that change in seasonal beliefs is mechanistic of change in depression over CBT-SAD, more so than change in more generic depressogenic dysfunctional attitudes.
Studies testing LT’s mechanisms have primarily focused on the timing or “phase” of the circadian clock (i.e., the extent to which circadian rhythms are synchronized with the light/dark cycle and clock time), but have produced mixed results (Burgess, Fog, Young, & Eastman, 2004; Eastman, Gallo, Lahmeyer, & Fogg, 1993; Knapen, Gordijn, & Meester, 2016; Murray et al., 2005; Lewy, Lefler, Emens, & Bauer, 2006; Murray et al., 2006; Terman, Terman, Lo, & Cooper, 2001). Prior studies have correlated change in depression symptoms from pre- to post-LT with change in physiological indicators of circadian phase from pre- to post-LT, with physiological indicators such as dim light melatonin onset (DLMO; Lewy, Sack, Singer, Whate, & Hoban, 1988; Terman et al., 2001), time of core body temperature minimum (Tmin; Burgess et al., 2004; Eastman et al., 1993), and phase angle difference (PAD; calculated as the time between DLMO and mid-sleep or core-body temperature minimum; Lewy et al., 2006; Murray et al., 2006). Only the study by Terman and colleagues (2001) found a significant correlation between change in DLMO and improvement in depression severity across LT, and another study showed that change in the interval between Tmin to wake-time across LT to a “therapeutic window” of 3 hours correlated with better antidepressant response from pre- to post-LT (Burgess et al., 2004). We are not aware of any LT study that involves a true test of mediation, according to the definitions of Kazdin (2007) and Kraemer et al. (2002).
These chronobiological measures are reliable markers of the timing of the biological clock, but are not typically available in clinical practice due to expense and burden. For example, DLMO, the most established marker of circadian phase, is assessed via obtaining saliva or blood samples every 30 minutes beginning 6 hours before habitual bedtime under controlled, dim light conditions, and the melatonin assay is expensive (~U.S. $14.50 per sample). Certain self-report measures correlate with chronobiological indicators of circadian phase and are more practical to implement in clinical practice because they are relatively non-invasive and inexpensive. One such measure, the Horne-Östberg Morningness-Eveningness Questionnaire (MEQ; Horne & Östberg; 1976), includes questions about preferred sleep and wake times; preferred clock times for performing various tasks (e.g., exercise, physically demanding work, mentally demanding tests); alarm clock dependency; and perceptions of evening sleepiness and of morning alertness, tiredness, and hunger. MEQ scores correlated significantly and negatively with DLMO in various mixed samples of healthy controls and people with assumed circadian misalignment, e.g., r = −0.70 in healthy controls and patients with delayed sleep phase disorder (Kantermann, Sung, & Burgess, 2015) and r = −0.64 in peri- and post-menopausal depressed and nondepressed women (Meliska et al., 2011), such that greater morningness was associated with an earlier DLMO. In addition, Kantermann et al. (2015) found that MEQ score, another chronotype measure (the Munich ChronoType Questionnaire), and age emerged as significant predictors of DLMO and, together, accounted for 60% of the variance in DLMO. The two chonotype measures were the strongest predictors of DLMO and did not differ from each other. Goulet, Mongrain, Desrosiers, Paquet, and Dumont (2007) used MEQ responses to classify people as morning or evening chronotypes and found significantly earlier circadian phase in morning-types than in evening-types, with group differences of 2.4 hours in DLMO and 1.7 hours in Tmin.
The MEQ has been tested as a moderator of change in depression score from pre- to post-LT, but results were not significant and the study design was limited in that it pooled data across four different studies using different LT protocols (e.g., different durations and timing of administration of LT; Knapen, Gordijn, & Meesters, 2016). Additional research is needed to test whether change in chronotype mediates change in depression symptoms over LT and, thus, reflects a potential therapeutic mechanism of LT. Studies testing whether chronotype mediates the antidepressant effects of other (non-chronobiological) SAD treatments are also needed to elucidate whether change in chronotype is a potential mechanism underlying improvement across treatments or if offsetting other etiologies may be implicated in improving SAD.
This study is the first to test mediators underlying the acute antidepressant effects of CBT-SAD and LT in a mediation analysis that meets the requirements of Kazdin (2007) and Kraemer et al. (2002), with both mediator and outcome assessed at least three times to address the issue of temporal precedence. In the parent trial, CBT-SAD and LT did not differ on continuous depression scores during treatment or at treatment endpoint, and the proportions in remission at post-treatment were very similar (47.6% in CBT-SAD and 47.2% in LT; Rohan et al., 2015). We administered self-report measures of dysfunctional attitudes and maladaptive seasonal beliefs as well as self-reported chronotype at pre-, mid-, and post-treatment to test whether these constructs emerged as mediators of depression improvement. Importantly, we tested mediation using a parallel-process growth curve framework (Cheong, MacKinnon, & Khoo, 2003), incorporating repeated assessments of each candidate mediator and outcome over time to test whether treatment-group-related change in each mediator was associated with change in each outcome. Although the treatments have comparable acute outcomes, here, we test the hypothesis that CBT-SAD and LT exert their antidepressant effects through distinct cognitive vs. chronobiological mechanisms. We hypothesized that changes in both seasonal beliefs (as measured by the SBQ) and dysfunctional attitudes (as measured by the DAS) would mediate changes in depressive symptoms in CBT-SAD but not in LT. We further expected that maladaptive seasonal beliefs would emerge as the strongest mediator of depression improvement in CBT-SAD, relative to more modest mediational effects of dysfunctional attitudes. We hypothesized that self-reported chronotype (as measured with the MEQ) would mediate depression improvements in LT but not in CBT-SAD.
Method
Participants
Participants were recruited through the parent randomized clinical trial testing the comparative efficacy of two SAD treatments assumed to operate via distinct mechanisms of action: CBT-SAD and LT (Rohan et al., 2013). All study procedures were reviewed and approved by the University of Vermont’s Institutional Review Board, and all participants provided informed consent. Participants included 177 adults, aged 18 and older, who met Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision (DSM-IV-TR) criteria for major depression, recurrent, with a seasonal pattern. Potential participants were screened using the Structured Clinical Interview for DSM-IV Axis I Disorders–Clinician Version (First, Spitzer, Gibbon, & Williams, 1995) and were required to be in a current SAD episode to be eligible, defined as total score of 20 or higher (with a minimum score of 5 on the atypical subscale) on the Structured Interview Guide for the Hamilton Rating Scale for Depression—Seasonal Affective Disorder Version (Williams, Link, Rosenthal, Amira, & Terman, 1992). Participants were excluded from this study if they had past, present, or planned treatment with CBT or LT for SAD. Contraindications to participation included a comorbid psychiatric disorder requiring immediate treatment or active and serious suicidal intent, evidence of hypothyroidism on thyroid panel, or travel plans that conflicted with treatment schedules.
Eligible participants (N = 177) were randomly assigned to receive 6-weeks of either CBT-SAD (n = 88) or LT (n = 89) during the acute treatment phase (for a detailed description of all study procedures, including randomization procedures, see Rohan et al., 2013). The majority of participants were women (83.6%) and non-Hispanic White (92.1%), with a mean age of 45.6 years (SD = 12.7). Participants allocated to CBT-SAD and LT did not differ on any baseline characteristic, including demographic variables, antidepressant medication status (45/177; 25.4% taking stable antidepressants), or comorbid diagnosis status (47/177; 26.6% had a comorbidity; see Rohan et al. 2015). A breakdown of demographics and baseline characteristics by treatment condition and the CONSORT flow diagram covering screening through treatment endpoint appear in Rohan et al. (2015).
Treatments
Details of CBT-SAD and LT treatment procedures are reported elsewhere (Rohan et al., 2013, 2015; Rohan, Meyerhoff et al., 2016). Briefly, individuals randomized to CBT-SAD received six weeks of group CBT-SAD (Rohan, 2008), which was administered in 12 90-minute sessions (with a frequency of twice per week) during the winter months. CBT-SAD incorporates standard elements of CBT (e.g., cognitive restructuring, behavioral activation, and relapse prevention). However, in CBT-SAD, some cognitive restructuring targets dysfunctional seasonal beliefs (i.e., negative beliefs about the winter season, limited natural light availability, inclement weather, and cues that the seasons are changing to fall or winter); behavioral activation aims to identify and schedule pleasant activities in the winter to counteract “hibernation” (i.e., avoidance); and relapse prevention involves a plan to implement cognitive and behavioral coping strategies in the early fall.
Participants randomized to LT were each provided with a light box (SunRay by SunBox Company©, Gaithersburg, MD), producing 10,000-lux of cool-white fluorescent light filtered through an ultraviolet shield. LT participants were instructed to initiate LT for 30-minutes daily immediately after waking. After one week of 30 minutes of morning LT, dosage adjustments were recommended by a chronobiological psychiatrist according to a treatment algorithm designed to maximize response to treatment and minimize unintended side effects.
A random sample of 25% CBT-SAD sessions and LT orientation sessions were rated for treatment integrity using an adaptation of the National Institute of Mental Health’s Collaborative Study Psychotherapy Rating Scale (see Rohan et al., 2013). CBT-SAD and LT emerged as distinct treatments that were administered consistently across providers and over time (see Rohan et al., 2015).
Measures
Depression Outcome Measures.
Structured Interview Guide for the Hamilton Rating Scale for Depression—Seasonal Affective Disorder Version (SIGH-SAD).
The SIGH-SAD (Williams et al., 1992), the most commonly used outcome in SAD treatment research, is a 29-item structured interview adapted from the 21-item Hamilton Rating Scale for Depression (HAM-D; Williams, 1988). SIGH-SAD items are comprised of HAM-D items and 8 additional questions that assess atypical symptoms commonly associated with SAD (e.g., fatigue, hyperphagia, hypersomnia). The SIGH-SAD was administered at pre-treatment and after treatment weeks 1, 2, 3, 4, 5, and 6 (post-treatment). Inter-rater reliability and our scoring protocol are reported elsewhere (Rohan, Rough et al. 2016).
Beck Depression Inventory—Second Edition (BDI-II).
The BDI-II (Beck, Steer, & Brown, 1996) is a well-validated, 21-item, self-report symptom severity measure for depression. Each item on the BDI-II consists of a general content area, such as “Past Failure” and 4 statements that span the full range of symptom severity within that content area, where 0 signifies a complete absence of that symptom and 3 signifies the most extreme presentation of that symptom. The BDI-II was administered at pre-, mid- (after treatment week 3), and post-treatment.
Candidate Mediator Measures.
The following measures corresponding to the hypothesized cognitive mediators of CBT-SAD (DAS and SBQ) and the hypothesized chronobiological mediator of (MEQ) were administered at pre-, mid-, and post-treatment.
Dysfunctional Attitudes Scale-Form A (DAS).
The DAS (Weissman & Beck, 1978) is a 40-item self-report measure that assesses attitudes common amongst depressed individuals, assumed to represent the semantic content of depressive schemas. Each DAS item consists of a statement consistent with a dysfunctional attitude and is rated on a 7-point Likert scale ranging from 7 (totally agree) to 1 (totally disagree). The DAS has good psychometric properties, including internal and test-retest reliability (Dobson & Breiter, 1983; Weissman & Beck, 1978).
Seasonal Beliefs Questionnaire (SBQ).
The SBQ (Rohan et al., 2019) comprises 26 statements about the seasons, light availability, and weather conditions. As in the DAS, each item is rated on a 7-point Likert scale ranging from 7 (totally agree) to 1 (totally disagree), and higher scores indicate more rigid seasonal beliefs. The measure discriminates individuals with SAD from both individuals with non-seasonal depression and non-depressed individuals and has good internal and test-retest reliability and good convergent validity (Rohan et al., 2019). Exploratory and confirmatory factor analysis revealed five factors (i.e., subscales): Personal Deficiency Related to Winter (PD), Global Summer Positivism (GS), Global Winter Negativity (GW), Effects from Lack of Light (ELL), and Lack of Perceived Seasonal or Weather Effect (LPSEW). Example items from each subscale include: “I’m ineffective in the winter” (PD); “All is well if the sun is shining” (GS); “I’m not a winter person” (GW); “Dark, gloomy days are depressing” (ELL); and “The weather is irrelevant to how I feel” (LPSWE).
Horne-Östberg Morningness-Eveningness Questionnaire (MEQ).
The MEQ (Horne & Östberg, 1976) is a 19-item self-report measure that assesses an individual’s chronotype or diurnal preference towards morningness or eveningness, with higher and lower scores indicating a preference for morning and evening, respectively. See the introduction for correlations between MEQ scores correlate and indices of circadian phase. The MEQ has good internal consistency (Smith, Reilly, & Midkiff, 1989) and test-retest reliability (Neubauer, 1992).
Data Analytic Plan
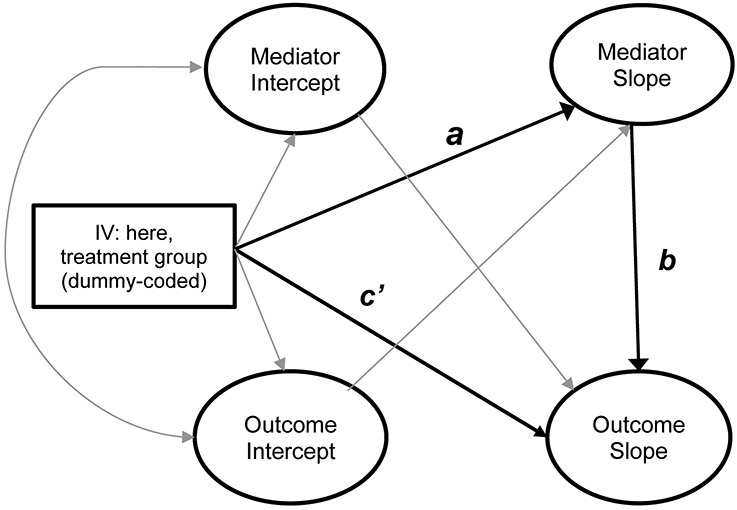
To examine the mechanisms of change that underlie the antidepressant effects of CBT-SAD and LT, we first conducted a series of single-construct growth models focusing in turn on each of the three mediators (DAS, SBQ, and MEQ) as well as our two outcome measures (SIGH-SAD and BDI-II) in order to screen for obvious modeling problems and to identify the appropriate form of change for use in subsequent parallel process models. After fitting individual growth models, we followed the procedures outlined in Cheong and colleagues (2003) to conduct a series of parallel-process growth curve models representing each combination of mediator and outcome measure, which allowed us to simultaneously examine the effect of treatment condition on change in the mediator and the effect of change in the mediator on change in the outcome. Figure 1 displays the core paths of the parallel-process mediation model, which improves upon single-variable tests of mediation by examining mediation via latent change factors. We then re-ran each of our parallel-process models including relevant covariates (i.e., gender, age, race/ethnicity, medication status, and comorbidity status, and days between baseline and first week of treatment). Finally, because the SBQ included subscales of theoretical interest, for models where an SBQ effect was indicated, we conducted follow-up analyses that separately tested each subscale. All modeling analyses were conducted using Mplus version 7.31 (Múthen & Múthen, 1998-2012).
Figure 1.
Key pathways of analytic model for parallel-process growth modeling; see Cheong et al. (2003) for further details. The independent variable (treatment group) is modeled as affecting linear change (slope) in the mediator, which in turn affects linear change (slope) in the outcome. Intercept factors represent starting points in order to anchor change from a particular baseline. Each intercept and slope factor is a latent variable specified by fixed factor loadings representing time lags for each observed data point.
a = effect of IV on mediator; b = effect of mediator on outcome; c’ = direct effect of IV on outcome; IV = independent variable.
Results
Table 1 shows descriptive statistics and correlations among key observed variables. To facilitate comparison with prior studies, descriptive statistics and correlations of observed difference scores between pre-, mid-, and post-treatment time points are available via the online Supplemental Materials.
Table 1:
Descriptive Statistics and Zero-Order Correlations Among Primary Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Gendera | - | ||||||||||||||||||||||||
| 2 Age | −0.095 | - | |||||||||||||||||||||||
| 3 Treatment Groupb | −0.013 | −0.099 | - | ||||||||||||||||||||||
| 4 Medicationc | 0.013 | 0.138 | −0.042 | - | |||||||||||||||||||||
| 5 Comorbidityd | −0.114 | −0.149 | −0.016 | 0.090 | - | ||||||||||||||||||||
| 6 Ethnicitye | −0.040 | −0.043 | 0.082 | −0.123 | 0.156 | - | |||||||||||||||||||
| 7 SIGH-SAD Baseline | 0.030 | −0.001 | −0.067 | 0.077 | 0.166 | 0.044 | - | ||||||||||||||||||
| 8 SIGH-SAD Tx Week 1 | 0.036 | −0.002 | −0.122 | 0.090 | 0.153 | 0.059 | 0.313 | - | |||||||||||||||||
| 9 SIGH-SAD Tx Week 2 | 0.065 | −0.080 | −0.048 | 0.054 | 0.082 | −0.053 | 0.425 | 0.642 | - | ||||||||||||||||
| 10 SIGH-SAD Tx Week 3 | 0.050 | 0.023 | −0.039 | 0.116 | 0.107 | −0.087 | 0.190 | 0.600 | 0.597 | - | |||||||||||||||
| 11 SIGH-SAD Tx Week 4 | 0.063 | −0.051 | −0.034 | −0.009 | 0.167 | −0.102 | 0.320 | 0.442 | 0.489 | 0.510 | - | ||||||||||||||
| 12 SIGH-SAD Tx Week 5 | 0.145 | −0.019 | −0.152 | −0.012 | 0.116 | −0.036 | 0.284 | 0.311 | 0.387 | 0.314 | 0.634 | - | |||||||||||||
| 13 SIGH-SAD Tx Week 6 | 0.034 | 0.046 | −0.112 | 0.059 | 0.116 | 0.001 | 0.266 | 0.361 | 0.416 | 0.400 | 0.455 | 0.431 | - | ||||||||||||
| 14 BDI-II Baseline | 0.063 | 0.015 | 0.046 | 0.099 | 0.159 | 0.080 | 0.407 | 0.371 | 0.358 | 0.267 | 0.272 | 0.231 | 0.296 | - | |||||||||||
| 15 BDI-II Tx Week 3 | 0.115 | −0.104 | −0.083 | 0.054 | 0.125 | −0.041 | 0.235 | 0.566 | 0.570 | 0.661 | 0.532 | 0.362 | 0.414 | 0.497 | - | ||||||||||
| 16 BDI-II Tx Week 6 | 0.022 | −0.042 | −0.080 | 0.056 | 0.171 | −0.016 | 0.283 | 0.243 | 0.310 | 0.263 | 0.320 | 0.329 | 0.699 | 0.352 | 0.476 | - | |||||||||
| 17 DAS Baseline | 0.132 | −0.224 | 0.010 | 0.006 | 0.269 | 0.117 | 0.192 | 0.193 | 0.247 | 0.082 | 0.200 | 0.033 | 0.137 | 0.418 | 0.306 | 0.153 | - | ||||||||
| 18 DAS Tx Week 3 | 0.158 | −0.232 | −0.078 | −0.027 | 0.301 | −0.028 | 0.187 | 0.196 | 0.320 | 0.247 | 0.254 | 0.146 | 0.230 | 0.304 | 0.435 | 0.276 | 0.707 | - | |||||||
| 19 DAS Tx Week 6 | 0.091 | −0.281 | −0.007 | −0.074 | 0.258 | −0.060 | 0.124 | 0.126 | 0.275 | 0.120 | 0.160 | 0.100 | 0.184 | 0.262 | 0.306 | 0.230 | 0.663 | 0.814 | - | ||||||
| 20 MEQ Baseline | 0.028 | 0.213 | 0.064 | −0.082 | −0.205 | 0.006 | −0.121 | −0.123 | −0.214 | −0.084 | −0.075 | −0.140 | −0.152 | −0.046 | −0.138 | −0.263 | −0.152 | −0.063 | −0.111 | - | |||||
| 21 MEQ Tx Week 3 | 0.088 | 0.223 | 0.119 | −0.076 | −0.196 | −0.064 | −0.093 | −0.047 | −0.131 | −0.035 | −0.087 | −0.213 | −0.107 | 0.020 | −0.174 | −0.286 | −0.152 | −0.145 | −0.189 | 0.860 | - | ||||
| 22 MEQ Tx Week 6 | −0.016 | 0.241 | 0.130 | −0.038 | −0.195 | −0.015 | −0.166 | −0.063 | −0.154 | −0.045 | −0.094 | −0.244 | −0.165 | −0.023 | −0.147 | −0.308 | −0.156 | −0.159 | −0.194 | 0.866 | 0.925 | - | |||
| 23 SBQ Baseline | 0.035 | 0.103 | −0.081 | 0.047 | 0.114 | −0.032 | 0.227 | 0.322 | 0.239 | 0.101 | 0.190 | 0.158 | 0.069 | 0.325 | 0.228 | 0.140 | 0.162 | 0.085 | 0.134 | −0.020 | −0.102 | −0.071 | - | ||
| 24 SBQ Tx Week 3 | −0.067 | 0.154 | 0.003 | −0.025 | 0.064 | −0.102 | 0.136 | 0.243 | 0.247 | 0.275 | 0.247 | 0.173 | 0.154 | 0.204 | 0.340 | 0.122 | 0.081 | 0.132 | 0.135 | −0.067 | −0.133 | −0.116 | 0.710 | - | |
| 25 SBQ Tx Week 6 | −0.062 | 0.065 | 0.140 | 0.006 | 0.065 | −0.049 | 0.179 | 0.200 | 0.312 | 0.258 | 0.275 | 0.195 | 0.234 | 0.254 | 0.354 | 0.295 | 0.137 | 0.165 | 0.239 | −0.095 | −0.201 | −0.165 | 0.562 | 0.734 | - |
| N | 177 | 177 | 177 | 177 | 177 | 177 | 177 | 154 | 153 | 154 | 149 | 149 | 173 | 177 | 164 | 172 | 176 | 164 | 173 | 167 | 158 | 171 | 175 | 163 | 171 |
| M | 0.836 | 45.638 | 0.503 | 0.254 | 0.266 | 0.079 | 27.746 | 22.968 | 19.582 | 17.857 | 14.866 | 13.785 | 12.197 | 23.95 | 13.15 | 7.9709 | 126.5 | 114.4 | 106.6 | 53.34 | 54.82 | 56.3 | 141.4 | 133.6 | 127.9 |
| SD | 0.371 | 12.742 | 0.501 | 0.437 | 0.443 | 0.271 | 5.485 | 7.856 | 7.790 | 7.381 | 7.603 | 6.913 | 6.795 | 9.094 | 7.122 | 6.488 | 33.62 | 31.17 | 28.85 | 11.18 | 10.91 | 11.29 | 16.02 | 16.79 | 21.4 |
Note: Italics = p < .05. Baseline = pre-treatment, Week 6 = post-treatment (treatment endpoint). SIGH-SAD = Structured Interview Guide for the Hamilton Rating Scale for Depression—Seasonal Affective Disorder Version., BDI-II = Beck Depression Inventory—Second Edition, DAS = Dysfunctional Attitudes Scale-Form A, MEQ = Horne-Östberg Morningness-Eveningness Questionnaire, SBQ = Seasonal Beliefs Questionnaire. Tx = treatment.
Gender was coded as 0 = male, 1 = female; therefore, the mean gender score of 0.836 indicates that 83.6% of the sample identified as female.
0 = CBT-SAD, 1 = light therapy.
0 = not taking antidepressant medication, 1 = taking antidepressant medication.
0 = no comorbid diagnosis, 1 = presence of at least one comorbid diagnosis.
0 = non-Hispanic White, 1 = all others.
Single-Construct Growth Models
All single-construct growth models converged and for three of the global fit indices, models showed adequate overall fit to the data: all CFIs exceeded .94, all TLIs exceeded .93, and all SRMRs were below .08. With two exceptions, the RMSEA also showed generally adequate overall fit with values below .08. Exceptions included the DAS linear change model (RMSEA = .096) and the SBQ linear model (RMSEA = .18). In each of these two instances, inspection of modification indices and residual correlation matrices did not suggest any interpretable additional parameters to estimate. These models had only a single degree of freedom, and prior simulation work suggests the poor RMSEA values are more common with low model degrees of freedom even for correctly specified models, leading the authors to discourage interpretation of RMSEA with low-df models (Kenny, Kaniskan, & McCoach, 2014).
With the exception of the SIGH-SAD, the best-fitting change model for each construct was a linear change model. For each, the observed change (slope factor) was statistically significant (all ps < .01) and in the expected direction (positive for the MEQ and negative for all other constructs). For the SIGH-SAD, a quadratic model showed better fit to the data via nested model comparison as compared to a linear model, Δχ2(4) = 12.49, p < .001. This model showed accelerating decrease in SIGH-SAD scores over the treatment period (negative linear plus negative quadratic change factors). In addition, based on modification index results, a residual covariance between treatment weeks 4 and 5 was modeled for the SIGH-SAD indicators. Additional details of the single-construct models are available from the authors on request.
Parallel Process Growth Models
Overview.
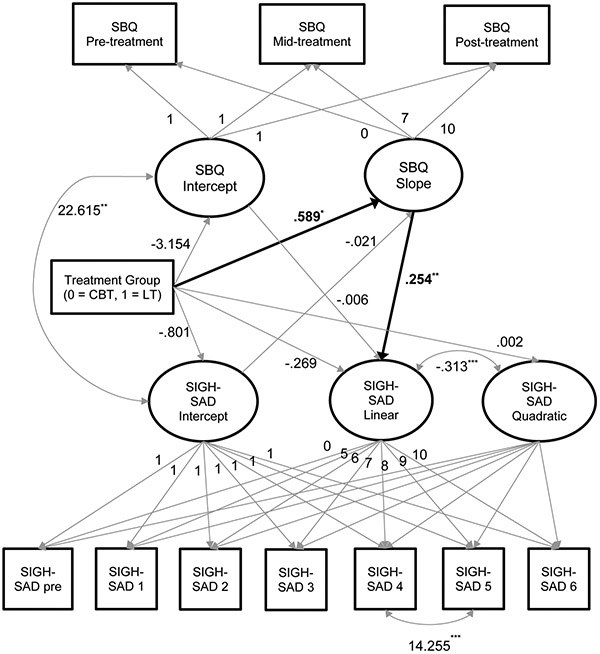
Parallel process growth models combined pairs of single-construct growth models—one mediator plus one outcome per model—while also modeling the effects of treatment group assignment (dummy-coded as 0 = CBT-SAD, 1 = LT) on intercept and slope of both mediator and outcome. In addition, these models estimated the key growth mediation path from slope of mediator to slope of outcome (for the SIGH-SAD models, this path was estimated leading to the linear component of change). All models followed the structure introduced by Cheong and colleagues (2003). Table 2 presents details of fit indices for these six key models. Overall model fit to the data was adequate (e.g., all CFIs > .90, all SRMRs < .08), with isolated exceptions, primarily in RMSEA. Figure 2 provides an example of such a model, showing the treatment effect on SIGH-SAD symptoms via SBQ scores. In text below, “estimate” refers to unstandardized model parameter estimates, with “β” reserved for standardized values.
Table 2:
Model Fit Statistics
| χ2 | RMSEA | CFI | TLI | SRMR | ||||
|---|---|---|---|---|---|---|---|---|
| Outcome (Mediator) | value | df | p | value | 90% CI | |||
| SIGH-SAD | ||||||||
| Model 1 (MEQ) | 67.028 | 44 | .0142 | .054 | [.025, .079] | .975 | 0.968 | .059 |
| Model 2 (SBQ) | 97.551 | 44 | <.0001 | .083 | [.061, .105] | .919 | 0.899 | .072 |
| Model 3 (DAS) | 78.076 | 44 | .0012 | .066 | [.041, .090] | .950 | 0.938 | .066 |
| BDI-II | ||||||||
| Model 1 (MEQ) | 20.305 | 11 | .0413 | .069 | [.014, .116] | .986 | 0.973 | .037 |
| Model 2 (SBQ) | 38.702 | 11 | <.0001 | .119 | [.080, .161] | .930 | 0.866 | .069 |
| Model 3 (DAS) | 29.278 | 11 | .0021 | .097 | [.055, .140] | .960 | 0.923 | .042 |
Note: See Table 1 for outcome measure abbreviations.
Figure 2.
Parallel process growth model: treatment effect on SIGH-SAD symptoms via SBQ scores. χ2(44) = 97.551, p < .001, CFI = .919, TLI = .899, RMSEA = .083, 90% CI [.061, .105], SRMR = .072. Unstandardized parameter estimates and fixed factor loadings from final model are presented. Fixed factor loadings for the SIGH-SAD quadratic term are the square of the presented loadings for the linear term. Slope/linear loadings represent the number of weeks of treatment. The primary mediation path is presented in bold. Residual variance arrows and estimates as well as mean structure parameters are not presented for space reasons. Full model details are available upon request.
* p < .05; ** p < .01; *** p < .001.
SIGH-SAD as outcome variable.
With the DAS as the mediator, neither the treatment-mediator slope path nor the mediator-outcome slope path was significantly different from zero. With the MEQ as the mediator, a marginal positive association was seen between treatment group assignment and mediator slope, estimate = 0.160, p = .083, β = 0.285; as expected, assignment to the LT group was associated with more positive MEQ slope, representing greater self-reported “morningness” over time. However, with the SBQ as the mediator, statistically significant effects were evident between treatment group and mediator slope (estimate = 0.589, p = .018, β = 0.275) as well as between mediator slope and outcome slope (estimate = 0.254, p = .002, β = 0.151). The overall indirect effect was marginal (p = .058). Thus, assignment to the CBT-SAD group resulted in a greater decrease in SBQ scores and consequent decrease in SIGH-SAD scores over the treatment period.1
BDI-II as outcome variable.
With the DAS as the mediator, the mediator-outcome slope path reached marginal significance level, estimate = .294, p= .083, β = 0.876, with no effect of treatment on mediator slope. With the MEQ as the mediator, the same marginal treatment group effect on mediator slope described in the preceding paragraph was observed, with no effect between mediator slope and outcome slope. With the SBQ as the mediator, effects were again observed for both the treatment-mediator slope path, estimate = 0.616, p = .012, β = 0.289, and the mediator-outcome slope path, estimate = 0.268, p = .003, β = 1.317. The overall indirect effect was again marginal (p = .057). Thus, assignment to CBT-SAD resulted in a greater decrease in SBQ scores and consequent decrease in BDI-II scores over the treatment period.
Models Including Covariates
We re-ran all core models adding covariates identified a priori as being of potential interest for ruling out alternative explanations for associations of change. These models were run in two stages due to a modest amount of missing data (N = 23) on one covariate: the “pre-treatment interval,” or the number of days between baseline assessment and first week of treatment (there were no missing data on any other covariates). Thus, the first set of covariate models added gender, age, dichotomized race/ethnicity (White non-Hispanic vs. all others), medication status, and comorbidity status simultaneously as predictors of change factors; the second set also added days between baseline and first week of treatment.
Although details differed somewhat by model, in general the analyses including covariates upheld our initial findings (detailed model results are available in the online Supplemental Materials). More specifically, with the SIGH-SAD as outcome, the SBQ mediator model showed the same significant effects and the marginal indirect effect became significant (p = .037) with inclusion of all covariates including the pre-treatment interval. With the BDI-II as outcome and DAS as mediator, the marginal mediator-outcome slope path became significant with inclusion of all covariates, estimate = 0.255, p = .034, β = 0.876. With the BDI-II as outcome and MEQ as mediator, the marginal treatment group to mediator slope path became significant with inclusion of all covariates, estimate = 0.228, p = .022, β = 0.681. All other model results were consistent with the original model runs.
Follow-up Analyses: Subscales of the SBQ
Based on the significant treatment-mediator and mediator-outcome path associations for the SBQ measure, we conducted exploratory follow-up analyses to determine whether we could isolate the effects to specific subscales of the SBQ. Thus, we ran an additional five models (using the SIGH-SAD outcome measure) replacing the SBQ total score with each of the five subscales in turn. These models showed generally poor fit with the exception of the Personal Deficiency Related to Winter subscale, and did not show evidence for statistically significant paths from treatment to mediator slope or from mediator slope to outcome slope. Thus, despite the relative robustness of SBQ effects across outcome measures and with and without inclusion of covariates, those effects seemed to stem from the responses to the total measure and were not driven by a particular subscale.
Discussion
This study provides an example of the experimental approach in clinical psychological science to test mechanisms of action underlying efficacious nonpharmacologic interventions. To our knowledge, this is the first true test of mediation in any SAD treatment, as defined by Kazdin (2007) and Kraemer et al. (2002), requiring that a change in the mediator precedes and accounts for a subsequent change in outcome. Our parent trial’s design lent itself to state-of-the-art mediation analyses (i.e., parallel-process growth curve models; Cheong et al., 2003) to examine change in both hypothesized mediators and outcome over time, even where one was assessed more frequently than the other (e.g., weekly SIGH-SAD outcome scores vs. candidate mediator assessments at pre-/mid-/post-treatment). The parent study found that CBT-SAD and LT are associated with large and comparable improvements in depressive symptoms at treatment endpoint (Rohan et al., 2015).
Although CBT-SAD and LT did not differ in acute outcomes, these findings suggest that CBT-SAD exerts its antidepressant effects through one potential mechanism that is distinct from LT: changing maladaptive seasonal beliefs. Seasonal beliefs emerged as a robust mediator of depression outcomes in CBT-SAD, with the statistical significance of the indirect effect improving after adjusting for covariates such as demographic factors, antidepressant medication and comorbidity statuses, and time before treatment initiation. In contrast, more generic depressogenic cognitions (i.e., dysfunctional attitudes) did not emerge as a mediator of depression outcomes in CBT-SAD, suggesting that modifying seasonal beliefs, but not changing dysfunctional attitudes, is potentially mechanistic of CBT-SAD’s acute effects. Although CBT-SAD represents a modification of CBT for depression (Beck et al., 1979) and retains the same basic treatment components, CBT-SAD might work through changing a distinct type of cognitive content relative to CBT for depression, i.e., seasonal beliefs or maladaptive thoughts about the seasons, light availability, and weather.
The hypothesis that seasonal beliefs is a central change mechanism in CBT-SAD could lead to further research aimed at refining the CBT-SAD intervention to have an increased emphasis on modifying seasonal beliefs. Change in seasonal beliefs appears relatively linear over the course of CBT-SAD. In the CBT-SAD protocol, behavioral activation is emphasized early and cognitive restructuring is the primary focus of the latter half of treatment. This highlights an empirical question that could be tested in further research: Are seasonal beliefs comparably modified by behavioral activation and cognitive restructuring? If change in seasonal beliefs is comparably effected via behavioral and cognitive interventions, one option may be to adapt CBT-SAD to spend more or less time on behavioral vs. cognitive CBT-SAD modules, as best matched to the individual case conceptualization. In individually-tailoring CBT-SAD, clinicians could repeatedly measure seasonal beliefs using the brief, freely available Seasonal Beliefs Questionnaire (SBQ; Rohan et al., 2019) to determine the extent to which particular intervention components are impacting this important mechanism. As a limitation, this study did not include a measure of behavioral activation as a candidate mediator of CBT-SAD, and future studies could examine seasonal beliefs and behavioral activation in relation to one another.
Alternatively, CBT-SAD could be modified to place greater emphasis on seasonal beliefs throughout the entire protocol. For example, the therapist could assess the effects of doing a pleasant activity on how the patient perceives him/herself during the winter months and his/her perceived degree of personal agency over mood state, regardless of the season or current light/weather conditions. Behavioral experiments could be developed in the context of activity scheduling to counter seasonal beliefs (e.g., to test the beliefs such as, “Watching TV is all I am capable of when it’s dark outside” and “If I wake up to overcast skies, my whole day will be awful”). In doing cognitive therapy, more time could be spent eliciting, challenging, and restructuring seasonal beliefs. Currently, the CBT-SAD protocol follows the patient’s lead, whereby they are encouraged to identify and work on seasonal beliefs, but not required to focus on them if more generic depressogenic thoughts are reported. More explicit use of visual imagery could be incorporated to elicit seasonal beliefs, as in CBT-SAD session 6 where scenarios are presented, such as watching the weather report leading up to the winter solstice and seeing fewer minutes of daytime each day, noticing the first signs of fall foliage, and waking up on a cold, snowy day. As homework, patients could be asked to complete thought diary entries while looking outside and noting their thoughts and emotions in response to any cues in the environment.
Although this study identified seasonal beliefs as a mediator of CBT-SAD’s effects, the candidate mediator of LT’s effects, chronotype, did not emerge as a mediator. To date, there are no true tests of mediation in LT, as prior studies have correlated pre- to post-LT differences in outcome with pre- to post-LT differences in a hypothesized mechanism. To our knowledge, ours is the first study that has the prerequisite number of timepoints (i.e., at least three) needed to test longitudinal mediation in LT. It is important to note that we replicated the prior finding that LT is associated with reduced “eveningness” over treatment (Murray et al., 2005); however, in our mediation analysis, change in chronotype was unrelated to change in SAD symptoms. Therefore, exactly how LT works, based on not only this study but the greater literature, remains unknown.
The current study has several limitations. Our methods could have been improved by including physiological indicators of LT’s hypothesized effect at pre-, mid- and post-treatment, such as Phase Angle Difference (PAD; the difference between timing of the dim light melatonin onset and the mid-point of sleep; Lewy et al., 2006). The parent study is a single-site trial with a relatively homogenous population, consisting predominantly of White, non-Hispanic women. The study’s pre-, mid-, and post-treatment assessment schedule afforded a test of longitudinal mediation, albeit with the minimal number of timepoints. More frequent assessments of candidate mediators would elucidate the shape of change in mediators over treatment. Our modest sample size and, in some cases, low degrees of model freedom (Kenny et al., 2014) likely contributed to less-than-ideal global model fit, which is an important limitation of this work. The high end of our RMSEA confidence interval ranges in particular fell outside typical cutoffs. Although close inspection of parallel-process model results did not suggest obvious reasons for this discrepancy in fit across indices, generally lower observed variable correlations tend to be associated with poorer RMSEA values. We were also unable to test for moderated mediation by comorbidity status due to highly unequal subgroup sizes, and we were unable to formally compare multiple mediators in a single model due to model complexity concerns; we see both areas as important directions for future research.
As an additional limitation, we focused on dysfunctional attitudes as a depressogenic cognitive mediator and did not examine other cognitive processes that have been explored as mediators of CBT outcomes, albeit to a lesser degree than the DAS. In DeRubeis et al. (1990), along with dysfunctional attitudes, automatic thoughts and hopelessness also mediated depression change in CBT but not in pharmacotherapy. A study testing an online CBT program for depressed adolescents supported rumination as a partial mediator of depressive symptom reductions (Smith et al., 2015). Cognitive distortions failed to emerge as a mediator in an adolescent depression randomized trial comparing CBT, systemic-behavioral family therapy, or nondirective supportive therapy (Kolko et al., 2000). However, Jacobs and colleagues (2014) identified cognitive distortions and three other cognitive processes—cognitive avoidance, positive outlook and solution-focused thinking—as partial mediators of depressive symptom change across CBT, pharmacotherapy, and combination CBT+pharmacotherapy in depressed adolescents. This finding was consistent across all three treatment modalities, with solution-focused thinking emerging as the strongest mediator. In a comparison of online depression treatment with CBT or problem-solved therapy relative to a waitlist control group, worrying, negative problem orientation, and perceived control were identified as mediators of outcome in both active treatments (Warmerdam et al., 2010). The current results suggest that CBT-SAD’s acute antidepressant effects are not mediated by change in dysfunctional attitudes, but it remains unknown whether these other constructs might function as mediators.
Although “experimental therapeutics” is a relatively new term in clinical psychological science, it is consistent with our field’s longstanding commitment to mechanisms-based research in treatment development and testing mediators. Applying the experimental therapeutics approach, this study provided evidence of both target engagement and validation for seasonal beliefs in CBT-SAD, as measured with a self-report questionnaire. Explicit in NIMH’s FOAs for clinical trials, “NIMH discourages reliance on self-reports and other subjective measures, in favor of using more objective measures, where possible.” Therefore, our newest randomized clinical trial in this programmatic line of work is responsive to this and is consistent with Lemmens et al.’s (2016) recommendation to include biological indicators as mediators. We are currently conducting an NIMH-funded, R01-level clinical trial aimed at identifying potential mechanisms of CBT-SAD’s vs. LT’s effects at the level of biomarkers. For CBT-SAD, our candidate mediators are sustained pupil dilation and sustained gamma-band EEG responses to winter words. In nonseasonal depression populations, both pupil dilation (Siegle, Granholm, Ingram, & Matt, 2001; Siegle, Steinhauer, Carter, Ramel, & Thase, 2003) and sustained gamma-band EEG (Siegle, Condray, Thase, Keshavan, & Steinhauer, 2010) to negatively-valenced emotional stimuli have been identified as critical biomarkers that distinguish depressed patients from controls. In response to emotional stimuli, sustained pupil dilation is believed to indicate prefrontal control in emotion regulation (Siegle, Steinhauer, Friedman, Thompson, & Thase, 2011), and sustained gamma-band EEG is thought to index sustained elaborative emotional processing (Siegle et al., 2010). For LT, our candidate mediators are PAD and the post-illumination pupil response (PIPR, Gamlin et al., 2007; Roecklein et al., 2013), which measures melanopsin-driven retinal subsensitivity to light.
In summary, modifying maladaptive beliefs about the seasons, light availability, and weather is one potential mechanism through which CBT-SAD exerts is acute antidepressant effects. Seasonal beliefs can be easily monitored with the SBQ during CBT-SAD to inform the extent to which treatment is engaging this possibly important change mechanism. Future studies should use more frequent, even session-by-session, measures of candidate mediators and explore refinements to the CBT-SAD protocol to maximize emphasis on active ingredients that effect the greatest change in those mechanisms that drive treatment efficacy. Given that CBT-SAD is superior to LT on outcomes following treatment, particularly lower risk for depression recurrence and less severe symptoms two winters after treatment (Rohan, Meyerhoff et al., 2016), studies should explore mediators of CBT-SAD’s enduring effects.
Supplementary Material
Acknowledgments
This work was supported, in part, by grant R01MH078982 from the National Institute of Mental Health to Kelly J. Rohan. Trial Registration: Cognitive-Behavioral Therapy vs. Light Therapy for Preventing SAD Recurrence; NCT01714050; http://clinicaltrials.gov/ct2/show/NCT01714050
Footnotes
Kelly J. Rohan receives book royalties from Oxford University Press for the treatment manual for the cognitive-behavioral therapy for SAD intervention. The authors have no other financial or nonfinancial competing interests.
Estimates of overall adjusted (i.e., reference-group) change in mediator and outcome variables in the parallel process models were similar in magnitude to those of the single growth curve models. However, these estimates were in general not significantly different from zero due to increased standard errors, which may indicate less stability of estimation due to sample size or other considerations.
References
- Beck AT, Rush AJ, Shaw BF, & Emery G (1979). Cognitive therapy of depression. New York, NY: Guilford Press. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II. Psychological Corporation (pp. 1–82). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Burgess HJ, Fogg LF, Young MA, & Eastman CI (2004). Bright light therapy for winter depression - Is phase advancing beneficial? Chronobiology International, 21(4–5), 759–775. 10.1081/CBI-200025979 [DOI] [PubMed] [Google Scholar]
- Cheong J, MacKinnon DP, & Khoo ST (2003). Investigation of Mediational Processes Using Parallel Process Latent Growth Curve Modeling. Structural Equation Modeling: A Multidisciplinary Journal, 10(2), 238–262. 10.1207/S15328007SEM1002_5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, Evans MD, Hollon SD, Garvey MJ, Grove WM, & Tuason VB (1990). How does cognitive therapy work? cognitive change and symptom change in cognitive therapy and pharmacotherapy for depression. Journal of Consulting and Clinical Psychology, 58(6), 862–869. 10.1037/0022-006X.58.6.862 [DOI] [PubMed] [Google Scholar]
- Dobson KS, & Breiter HJ (1983). Cognitive assessment of depression: Reliability and validity of three measures. Journal of Abnormal Psychology, 92(1), 107–109. 10.1037/0021-843X.92.1.107 [DOI] [PubMed] [Google Scholar]
- Eastman CI, Gallo LC, Lahmeyer HW, & Fogg LF (1993). The circadian rhythm of temperature during light treatment for winter depression. Biological Psychiatry, 34(4), 210–220. 10.1016/0006-3223(93)90074-n [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1995). Structured Clinical Interview for DSM-IV Axis I Disorders (Clinician Version). New York: NY: New York State Psychiatric Institute Biometrics Department. [Google Scholar]
- Gamlin PDR, Mcdougal DH, Pokorny J, Smith VC, Yau KW & Dacey DM (2007). Human and macaque pupil responses driven by melanopsin-containing retinal ganglion cells. Vision Research, 47(7), 946–954. 10.1016/j.visres.2006.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, … Nemeroff CB (2005). The efficacy of light therapy in the treatment of mood disorders: A review and meta-analysis of the evidence. The American Journal of Psychiatry, 162(4), 656–662. 10.1176/appi.ajp.162.4.656 [DOI] [PubMed] [Google Scholar]
- Goulet G, Mongrain V, Desrosiers C, Paquet J, & Dumont M (2007). Daily light exposure in morning-type and evening-type individuals. Journal of Biological Rhythms, 22(2), 151–158. 10.1177/0748730406297780 [DOI] [PubMed] [Google Scholar]
- Hamilton KE, & Dobson KS (2002). Cognitive therapy of depression: Pretreatment patient predictors of outcome. Clinical Psychology Review, 22(6), 875–894. 10.1016/S0272-7358(02)00106-X [DOI] [PubMed] [Google Scholar]
- Horne JA, & Östberg O (1976). A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. International Journal of Chronobiology, 4(2), 97–110. [PubMed] [Google Scholar]
- Insel TR, & Gotgay N (2014). National Institute of mental health clinical trials: New opportunities, new expectations. JAMA Psychiatry, 71(7), 745–746. 10.1001/jamapsychiatry.2014.426 [DOI] [PubMed] [Google Scholar]
- Jacobs RH, Becker SJ, Curry JF, Silva SG, Ginsburg GS, Henry DB, & Reinecke MA (2014). Increasing positive outlook partially mediates the effect of empirically supported treatments on depression symptoms among adolescents. Journal of Cognitive Psychotherapy, 28(1), 3–19. 10.1891/0889-8391.28.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantermann T, Sung H, & Burgess HJ (2015). Comparing the Morningness-Eveningness Questionnaire and Munich ChronoType Questionnaire to the Dim Light Melatonin Onset. Journal of Biological Rhythms, 30(5), 449–453. 10.1177/0748730415597520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kaniskan B, & McCoach DB (2014). The performance of RMSEA in models with small degrees of freedom. Sociological Methods & Research, 44(3), 486–507. 10.1177/0049124114543236 [DOI] [Google Scholar]
- Knapen SE, Gordijn MCM, & Meesters Y (2016). The relationship between chronotype and treatment outcome with light therapy on a fixed time schedule. Journal of Affective Disorders, 202, 87–90. 10.1016/j.jad.2016.05.009 [DOI] [PubMed] [Google Scholar]
- Kolko DJ, Brent DA, Baugher M, Bridge J, & Birmaher B (2000). Cognitive and family therapies for adolescent depression: Treatment specificity, mediation, and moderation. Journal of Consulting and Clinical Psychology, 68(4), 603–614. 10.1037/0022-006X.68.4.603 [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59(10), 877–883. 10.1001/archpsyc.59.10.877 [DOI] [PubMed] [Google Scholar]
- Lemmens LHJM, Galindo-Garre F, Arntz A, Peeters F, Hollon SD, Derubeis RJ, & Huibers MJH (2017). Exploring mechanisms of change in cognitive therapy and interpersonal psychotherapy for adult depression. Behaviour Research and Therapy, 94, 81–92. 10.1016/j.brat.2017.05.005 [DOI] [PubMed] [Google Scholar]
- Lemmens LHJM, Muller Viola N. L. S., Arntz A, & Huibers MJH (2016). Mechanisms of change in psychotherapy for depression: An empirical update and evaluation of research aimed at identifying psychological mediators. Clinical Psychology Review, 50, 95–107. 10.1016/j.cpr.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Lewy AJ, Lefler BJ, Emens JS, & Bauer VK (2006) The circadian basis of winter depression. PNAS, 103(19), 7414–7419. 10.1073/pnas.0602425103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewy AJ, Sack RL, Singer CM, Whate DM, & Hoban TM (1988). Winter depression and the phase-shift hypothesis for bright light's therapeutic effects: History, theory, and experimental evidence. Journal of Biological Rhythms, 3(2), 121–134. 10.1177/074873048800300203 [DOI] [PubMed] [Google Scholar]
- Meliska CJ, Martínez LF, López AM, Sorenson DL, Nowakowski S, & Parry BL (2011). Relationship of morningness-eveningness questionnaire score to melatonin and sleep timing, body mass index and atypical depressive symptoms in peri- and post-menopausal women. Psychiatry Research, 188(1), 88–95. 10.1016/j.psychres.2010.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modell JG, Rosenthal NE Harriett AE, Krishen A, Asgharian A, Foster VJ, Metz A, Rockett CB, & Wrightman DS (2005). Seasonal affective disorder and its prevention by anticipatory treatment with Buproprion XL. Biological Psychiatry, 58(8), 658–667. 10.1016/j.biopsych.2005.07.021 [DOI] [PubMed] [Google Scholar]
- Murray G, Michalak EE, Levitt AJ, Levitan RD, Enns MW, Morehouse R, & Lam RW (2005). Therapeutic mechanism in seasonal affective disorder: Do fluoxetine and light operate through advancing circadian phase? Chronobiology International, 22(5), 937–943. 10.1080/07420520500263292 [DOI] [PubMed] [Google Scholar]
- Murray G, Michalak EE, Levitt AJ, Levitan RD, Enns MW, Morehouse R, & Lam RW (2006). O sweet spot where art thou? Light treatment of seasonal affective disorder and the circadian time of sleep. Journal of Affective Disorders, 90, 227–231. 10.1016/j.jad.2005.10.010 [DOI] [PubMed] [Google Scholar]
- Múthen LK, & Múthen BO (1998-2012). Mplus user’s guide (7th edition). Los Angeles, CA: Múthen and Múthen. [Google Scholar]
- National Institute of Mental Health (2015). Strategic Plan for Research. Retrieved from http://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml
- Neubauer AC (1992). Psychometric comparison of two circadian rhythm questionnaires and their relationship with personality. Personality and Individual Differences, 13(2), 125–131. 10.1016/0191-8869(92)90035-N [DOI] [Google Scholar]
- Roecklein KA, Wong PM, Ernecoff N, Miller M, Donofry S, Kamarck M, Wood-Vasey WM, & Franzen P (2013).The post illumination pupil response is reduced in seasonal affective disorder. Psychiatry Research, 210(1), 150–158. 10.1016/j.psychres.2013.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ (2008). Coping with the seasons: A cognitive-behavioral approach to seasonal affective disorder: Therapist guide. Coping with the seasons: A cognitive-behavioral approach to seasonal affective disorder: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Rohan KJ, Evans M, Mahon JN, Sitnikov L, Ho S-Y, Nillni YI, … Vacek PM (2013). Cognitive-behavioral therapy vs. light therapy for preventing winter depression recurrence: Study protocol for a randomized controlled trial. Trials, 14, 82 10.1186/1745-6215-14-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ, Mahon JN, Evans M, Ho S-Y, Meyerhoff J, Postolache TT, & Vacek PM (2015). Randomized trial of cognitive-behavioral therapy versus light therapy for seasonal affective disorder: Acute outcomes. The American Journal of Psychiatry, 172(9), 862–869. 10.1176/appi.ajp.2015.14101293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ, Meyerhoff J, Ho S-Y, Evans M, Postolache TT, & Vacek PM (2016). Outcomes one and two winters following cognitive-behavioral therapy or light therapy for seasonal affective disorder. The American Journal of Psychiatry, 173(3), 244–251. 10.1176/appi.ajp.2015.15060773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ, Meyerhoff J, Ho S, Roecklein K, Nillni Y, Hillhouse J, … Vacek PM (2019). A measure of cognitions specific to seasonal depression: Development and validation of the Seasonal Beliefs Questionnaire. Psychological Assessment, 31(7), 925–938. 10.1037/pas0000715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ, Roecklein KA, & Haaga DAF (2009). Biological and psychological mechanisms of seasonal affective disorder: A review and integration. Current Psychiatry Reviews, 5(1), 37–47. 10.2174/157340009787315299 [DOI] [Google Scholar]
- Rohan KJ, Rough JN, Evans M, Ho S, Meyerhoff J, Roberts LM, & Vacek PM (2016). A protocol for the Hamilton Rating Scale for Depression: Item scoring rules, rater training, and outcome accuracy with data on its application in a clinical trial. Journal of Affective Disorders, 200, 111–118. 10.1016/j.jad.2016.01.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal NE, Sack DA, Gillin JC, Lewy AJ, Goodwin FK, Davenport Y … Wehr TA (1984). Seasonal affective disorder: A description of the syndrome and preliminary findings with light therapy. Archives of General Psychiatry, 41(1), 72–80. 10.1001/archpsyc.1984.01790120076010 [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Granholm E, Ingram RE, & Matt GE (2001). Pupillary response and reaction time measures of sustained processing of negative information in depression. Biological Psychiatry, 49(7), 624–636. 10.1016/S0006-3223(00)01024-6 [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Condray R, Thase ME, Keshavan M, & Steinhauer SR (2010). Sustained gamma-band EEG following negative words in depression and schizophrenia. International Journal of Psychophysiology, 75(2), 107–118. 10.1016/j.ijpsycho.2008.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegle GJ, Steinhauer SR, Carter CS, Ramel W, & Thase ME (2003). Do the seconds turn into hours? Relationships between sustained pupil dilation in response to emotional information and self-reported rumination. Cognitive Therapy & Research, 27(3), 365–382. 10.1023/A:1023974602357 [DOI] [Google Scholar]
- Siegle GJ, Steinhauer SR, Friedman ES, Thompson WS, & Thase ME (2011). Remission prognosis for cognitive therapy for recurrent depression using the pupil: Utility and neural correlates. Biological Psychiatry, 69(8), 726–733. 10.1016/j.biopsych.2010.12.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CS, Reilly C, & Midkiff K (1989). Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. Journal of Applied Psychology, 74(5), 728–738. 10.1037/0021-9010.74.5728 [DOI] [PubMed] [Google Scholar]
- Smith P, Scott R, Eshkevari E, Jatta F, Leigh E, Harris V, … Yule W (2015). Computerised CBT for depressed adolescents: Randomised controlled trial. Behaviour Research and Therapy, 73, 104–110. 10.1016/j.brat.2015.07.009 [DOI] [PubMed] [Google Scholar]
- Terman J Terman M, Lo E & Cooper TB (2001). Circadian time of morning light administration and therapeutic response in winter depression. Archives of General Psychiatry, 58(1), 69–75. 10.1001/archpsyc.58.L69 [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, & Jarrett RB (2014). Are improvements in cognitive content and depressive symptoms correlates or mediators during acute-phase cognitive therapy for recurrent major depressive disorder? International Journal of Cognitive Therapy, 7(3), 251–271. 10.1521/ijct.2014.7.3.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warmerdam L, van Straten A, Jongsma J, Twisk J, & Cuijpers P (2010). Online cognitive behavioral therapy and problem-solving therapy for depressive symptoms: Exploring mechanisms of change. Journal of Behavior Therapy and Experimental Psychiatry, 41(1), 64–70. 10.1016/j.jbtep.2009.10.003 [DOI] [PubMed] [Google Scholar]
- Weissman AN, & Beck AT (1978). Development and validation of the Dysfunctional Attitude Scale: A preliminary investigation. Paper presented at the annual meeting of the American Educational Research Association, Toronto, Ontario, Canada. [Google Scholar]
- Williams JB (1988). A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry, 45, 742–747. 10.1001/archpsyc.1988.01800320058007 [DOI] [PubMed] [Google Scholar]
- Williams JB, Link MJ, Rosenthal NE, Amira L, & Terman M (1992). Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version (SIGH-SAD). New York, New York State Psychiatric Institute. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.