Abstract
The triangular fibrocartilage complex (TFCC) is a well defined anatomical entity located on the ulnar aspect of the wrist joint functioning primarily to stabilize the distal radio –ulnar joint (DRUJ) and also to act as a shock absorber across the ulno-carpal joint.
Palmer and Werner were first to explain the anatomic details of the TFCC and to describe its biomechanical role at the wrist. The TFCC comprises of the fibro-cartilagenous disc, the dorsal and palmar ligaments spanning across radius and ulna, the ulno-carpal ligaments, a meniscal homolog, and the sub sheath of ulnar extensor of the wrist. The intricate anatomy of this area and complex load transmission kinematics renders it vulnerable to injury and attrition. Both traumatic and degenerative insults produce specific injury patterns which can present as vague ulnar-sided wrist pain particularly during forearm rotation.
These injuries are managed initially by modification of daily activities to avoid aggravation of pain and injury, by complete abstinence from sporting/gym/yoga maneuvers which involve stressing the wrist joints, temporary splint or cast immobilisation are also used along with non-steroidal anti-inflammatory medication.
Corticosteriod injection are also used in conjunction with physical therapy in grossly symptomatic patients.
Surgical treatment is advocated if conservative management fails to provide relief, or in cases presenting initially with frank instability of the DRUJ or with unstable and displaced fractures. Choice of operative treatment is guided by type and extent of injury and may include debridement, repair and in TFCC injuries associated with degenerative changes, ulnar unloading procedures like shortening or Wafer procedure. With current understanding of arthroscopic anatomy of the wrist, availability of instrumentation as well as familiarity of surgeons with this tool, arthroscopic management can be instituted successfully in most if not all conditions afflicting the TFCC.
Keywords: TFCC tear, Palmer classification, Arthroscopic repair
1. Introduction
The triangular fibrocartilage complex (TFCC) is a well defined anatomical entity located on the ulnar aspect of the wrist joint functioning primarily to stabilize the distal radio –ulnar joint (DRUJ) and also to act as a shock absorber across the ulno-carpal joint.
Palmer and Werner were first to explain the anatomic details of the TFCC and to describe its biomechanical role at the wrist. The TFCC comprises of the fibro-cartilagenous disc, the dorsal and palmar ligaments spanning across radius and ulna, the ulno-carpal ligaments, a meniscal homolog, and the sub sheath of ulnar extensor of the wrist. The intricate anatomy of this area and complex load transmission kinematics renders it vulnerable to injury and attrition. Both traumatic and degenerative insults produce specific injury patterns which can present as vague ulnar-sided wrist pain particularly during forearm rotation.
These injuries are managed initially by modification of daily activities to avoid aggravation of pain and injury, by complete abstinence from sporting/gym/yoga maneuvers which involve stressing the wrist joints, temporary splint or cast immobilisation are also used along with non-steroidal anti-inflammatory medication.
Corticosteriod injection are also used in conjunction with physical therapy in grossly symptomatic patients.
Surgical treatment is advocated if conservative management fails to provide relief, or in cases presenting initially with frank instability of the DRUJ or with unstable and displaced fractures. Choice of operative treatment is guided by type and extent of injury and may include debridement, repair and in TFCC injuries associated with degenerative changes, ulnar unloading procedures like shortening or Wafer procedure. With current understanding of arthroscopic anatomy of the wrist, availability of instrumentation as well as familiarity of surgeons with this tool, arthroscopic management can be instituted successfully in most if not all conditions afflicting the TFCC.
2. Etiology
Injury to the triangular fibrocartilage usually occurs due to axial loading of an ulnar deviated wrist. This is often the situation during a fall over an outstretched hand as well as during swing of a racquet or a bat when the wrist is loaded in ulnar deviation along with a progressive pronation force.
The other common cause of injury of the TFCC is the disruption of normal ulnar variance, most likely secondary to previous trauma, which renders the distal ulna to be longer than articular margin of the lunate fossa of the radius at the wrist. This positive variance has been shown to make the TFCC susceptible to injury and degeneration as a result of ulno-carpal impingement.
3. Anatomy
TFCC is formed by following components, the triangular fibrocartilage disc proper, the thick subsheath of extensor carpi ulnaris tendon, ulno-triquetral and ulno-lunate ligaments, the radio-ulnar ligaments, meniscal homolog, and the ulno-carpal collateral ligament. The triangular fibrocartilage disc attaches firmly to bony fovea on the ulnar side and to the hyaline cartilage on the radial side which is weaker compared to ulnar sided TFCC.1
Wrist with positive ulnar variance are vulnerable to TFCC injury. Palmer and Werner demonstrated that ulnar variance decreases with supination and increases with pronation. Substantial changes in amount of ulnar load have been observed small changes of ulnar length.2 The extensor carpi ulnaris sub-sheath which is a component of the TFCC, is important as pulley for wrist ulnar extensors, and thus any deviation of vector of pull of extensor carpi ulnaris tendon can put abnormal forces across the dorsal aspect of the TFCC, predisposing same to injury.3
Semisch M4 and colleagues have described the histopathology of TFCC describing the type and orientation of collagen fibers. They found that the disc is vascular on its periphery only, otherwise it is largely avascular. It is composed of fibrocartiagenous tissue. The ulnotriquetral, ulnolunate ligaments and the ECU subsheath are composed of loose as well as tightly packed, parallely oriented bundles of collagen fibers. The ligaments connecting the distal radius to ulna on volar and dorsal aspect are strong and contain tightly packet bundles of collagen and are important stabilizers of the distal radio-ulnar joint. The meniscal homolog is composed of loose connective tissue.
4. Clinical presentation
Patients with TFCC injury complain of activity related ulnar-sided wrist pain. Movements which involve rotation of wrist like rotating the door knobs, opening the lid of a jar or a bottle produce varying degree of symptoms ranging from moderate discomfort to sharp pain on the ulnar aspect of the wrist. Pain may also be accompanied with weakness in the grip, instability, or clicking at presentation. Weakness in pronation & supination due to underlying DRUJ instability is a common feature reported with TFCC injury.5
Examination of a suspected TFCC injured patient requires careful palpation and application of few provocative tests. The patient must be seated in a relaxed environment and should be explained to report any discomfort or reproduction of symptoms during the process of examination. All tests must be performed on the uninjured limb first, this serves in two ways. One, it acts as a control for comparision, two, it alleviates apprehension in an anxious patient.
The best place to palpate the TFCC is the soft spot on the volar aspect of wrist distal to ulnar head between the ulnar styloid, FCU and pisiform. Tay et al.6 described the “ulna fovea sign” which is positive when pain is elicited on plapation of this critical area labelled as fovea. When positive, it is a reliable test to diagnose tear of the ulno-triquetral ligament tear or disruption of the foveal attachment of the TFCC. This test has high sensitivity of 95.2% and a specificity of 86.5%.
The TFCC compression test is performed by ulnar deviating the forearm in neutral rotation. Reproduction of symptoms indicates that the test is positive In the TFCC stress test an axial load is applied to a ulnar-deviated wrist which produces pain and discomfort. The piano key test is done to assess the stability of the DRUJ. It is done in pronated position of forearm. With the hand being stabilized, the dorsal ulnar prominence relative to radius is observed and the ulnar head in pushed volarly. A positive piano key sign is noted when minimal amount of resistance is felt againt volar displacement of ulnar head, suggesting the presence of underlying DRUJ instability. The test should be repeated with the forearm in supination. Comparision of the amount of ulnar displacement must be done with contralateral side because patients with generalized ligamentous laxity may have a substantial amount of abnormal baseline displacement.
Another simple and reliable test to assess DRUJ laxity is the ballottement test.7 This test involves antero-posterior and postero-anterior translation of the ulna on the radius passively in a neutrally rotated forearm. Abnormal translation of the ulnar head suggests a complete TFCC disruption. While repeating the test in full supination, comptence of dorsal component of DRUJ ligaments, and in pronation, of the volar components can be tested separately.
The Grind test is performed by compressing the distal forearm and having the patient pronate and supinate. Presence of pain suggests DRUJ arthritis.
5. Evaluation
Initial workup typically starts with a radiograph to detect any fracture and assess the ulnar variance. The next step will often be to get an MRI with or without an arthrogram. Boer and colleagues have recently demonstrated that an arthrogram is only slightly better and arguably not worth advising in all suspected cases of TFCC given the increased discomfort and cost associated with MRA.8 A non-contrast MRI is usually sufficient to detect a TFCC tear. It has been shown to have high sensitivity of 92%, a specificity of 89% and accuracy of 91% by Zlatkin et al.9 For radial side tear Oneson et al. found that sensitivity and specificity of MRI was 100% and 86% though values for diagnosis of ulnar-sided tear were not so high.10 They concluded that peripheral ulnar tears, both styloid and foveal disruptions, were difficult to diagnose with low field MRI. Haims et al. also found low sensitivity (17%), specificity (79%) and accuracy (64%) for diagnosing peripheral ulnar tear using MRI.11 Arthroscopy is the most accurate means by which to diagnose TFCC injury irrespective of location.
6. Classification
The Palmer12 classification is the most widely used scheme. It classifies tears as traumatic or degenarative.
Type 1 lesion which occur secondary to trauma are further subclassified according to location of tear. On the other hand, Type 2 or the degenerative tears are subgrouped depending upon the extent of attritional process.
6.1. Type 1A
These are the commonest type of tears caused by trauma and are located in the central portion of fibrocartilage disc (Fig. 1). These lesions do not cause DRUJ instability or alter its kinematics.13,14 They are present typically as sagittal tears involving a portion of the disc within 2–3 mm of its radial attachment. Involvement of entire disc, however, can be seen in complex tears.
Fig. 1.
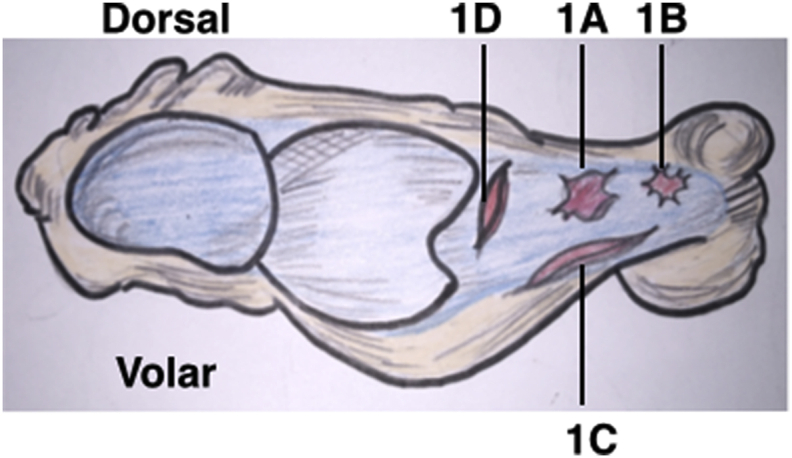
Palmer Classification of traumatic TFCC tears.
6.2. Type 1B
This sub-group represent traumatic peripheral tears of TFCC from it ulnar insertion (Fig. 1). These injuries are either soft tissue avulsion of ligaments from the fovea or bony fractures of the ulnar styloid base. They are commonly associated with instability of the DRUJ and require careful evaluation. These injuries are most amenable to repair and healing as blood supply is more in the periphery as previously discussed, which makes it conducive to repartative process.
6.3. Type 1C
These are uncommon high-energy injuries that involve the volar ulnar extrinsic ligament complex, including the ulno-lunate, ulno-triquetral, and/or ulno-capitate ligaments. These ligaments resist disruption due to their good strength and it requires a large amount of rapidly applied force to cause tears and avulsion such as in high velocity road traffic accidents or falls from significant height. As a consequence, these lesions are usually associated with DRUJ instability as well as gross ulno-carpal and inter-carpal dissociative instabilities. Fractures of the distal radius and its margins causing ligamentous disruption are also associated and often contribute to cause instability of the DRUJ.
6.4. Type 1D
These are avulsion injuries (bony/pure soft tissue) from the sigmoid notch of the radius. These lesions occur most often through bone, and are often due to fracture of the margins of the sigmoid notch causing disruption of and the insertion sites of the dorsal and palmar radio-ulnar ligaments. Because of this, they have high incidence of instability of the DRUJ associated with them.
6.5. Type 2
These are degenerative tears caused due to abnormal loading of ulnar side of wrist representing ulnar impaction syndrome. Positive ulnar variance is a common feature and pathognomonic. Attritional changes within this classification advance progressively as depicted in Table 1. Beginning with loss of thickness of TFCC along with its wear, catrilage erosion on the ulnar head and ulnar articular surface of lunate is seen in advancing stage. Perforation in the TFCC ensues which is then followed by the ulno-triquetral ligament tear and finally it progresses to ulno-carpal arthritis.
Table 1.
Palmer Classification of TFCC tear.
| TYPE 1 | TRAUMATIC |
|---|---|
| 1A | Isolated central TFCC articular disk perforation |
| 1B | Peripheral ulnar-sided TFCC tear (with or without ulnar styloid fracture) |
| 1C | Distal TFCC disruption |
| 1D | Radial TFCC disruption |
| TYPE 2 | DEGENERATIVE |
| 2A | TFCC wear |
| 2B | TFCC wear with lunate and/or ulnar chondromalacia |
| 2C | TFCC perforation with lunate and/or ulnar chondromalacia |
| 2D | TFCC perforation with lunate and/or ulnar chondromalacia and with lunotriqetral ligament perforation |
| 2E | TFCC perforation with lunate and/or ulnar chondromalacia, lunotriquetral ligament perforation and ulnocarpal arthritis |
Palmer classification indicates that occurence of one type of tear takes place in isolation. However some tears occur not in isolation but in combination where disruption may occur at more than one site.15 Also some tear patterns do not confirm to any sub-groups. Further, it is possible to find an acute traumatic tear associated with underlying degenerative pathology.
More recently Atzei16 and colleagues have proposed as new classification system for peripheral TFCC tear with algorithm to decide appropriate treatment for each class of peripheral TFCC lesion. Their algorithm of treatment is based on clinical assessment of DRUJ instability by ballottement test classified as negative (stable), mild instability (hard end point, sever instability (soft end point),radiographic presence of ulnar styloid fracture (tip or basilar). The third component in evaluation and classification is by arthroscopy (both radio-carpal and DRUJ) and it findings are summarized according to the following four parameters:
-
1.TFCC disruption extent
-
•Only distal tear evident from by positive trampoline and negative hook test
-
•Both distal & Proximal tear showing positive trampoline and hook test
-
•Proximal tear only seen on DRUJ arthroscopy though both hook test and trampoline test are positive on radio-carpal arthroscopy
-
•
-
2.
Potential to heal (vascularity of debrided edge)
-
3.
Triangular Fibrocartilage Complex Tear reducibility (small vs massive tear)
-
4.
DRUJ cartilage (evidence of arthritis)
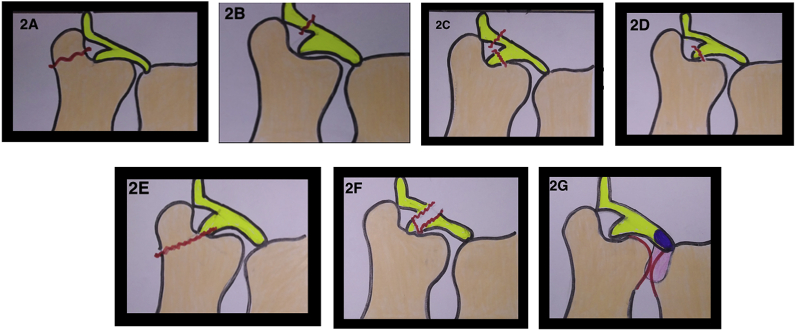
Based on above clinical, radiological and arthroscopic parameters a comprehensive classification and treatment algorithm has been proposed. A summarized version is presented in Table 2 and Fig. 2.
Table 2.
Summarized Atzei’s classification of TFCC peripheral tear (from Douglass, Nathan & Yao, Jeffrey. (2016). Biomechanics and Classification (Diagnosis and Imaging for TFCC Injuries, Instability).
| Class | 0 | 1 | 2 | 3 | 3a | 4 | 5 |
|---|---|---|---|---|---|---|---|
| Description | Ulnar styloid tip fracture | Distal TFCC tear | Distal & Proximal tear | Proximal TFCC tear | Ulnar Styloid base fracture | Irreparable proximal TFCC tear | Advanced DRUJ arthritis |
| Clinical DRUJ instability | Stable | Stable | Mild to severe instability | Variable | |||
| Distal TFCC | Intact | Torn | Torn | Normal | Normal | Irreparable tear | Variable |
| Proximal TFCC | Intact | Intact | Torn | Torn | Intact | Irreparable tear | Variable |
| Hook Test | Negative (taut) | Positive (Abnormal Laxity) | Variable | ||||
| Treatment | Immobilisation | TFCC suture repair | Fixation of proximal TFCC to fovea | Ulnar Styloid fixation | TFCC reconstruction | Salvage | |
Fig. 2.
A summarized version of Atzei’s classification of foveal TFCC tears.(2A-Class 0, 2B-Class 1, 2C-Class 2, 2D-Class 3, 2E-Class 3a, 2F-Class 4, 2G-Class 5.
7. Treatment/management
For management purposes we follow the Palmer classification. Initial treatment of all types of TFCC injury includes rest, activity modification, splint, physical therapy, and corticosteroid injections. In case of failure of conservative treatment to give relief or in tears with joint instability early surgical intervention is recommended. Choice of treatment is based on type of lesion and may include open or arthroscopic repair, arthroscopic debridement, ulnar shortening, and the Wafer procedure.
A debridement is a procedure in which the tear edge is trimmed to remove scar and reach a bleeding margin of the TFCC to stimulate healing. Debridement has been reported to be beneficial for central tears, however it has been shown to give worse outcomes for Class 2 lesions and tears in patients with positive variance of ulna.17 Repair techniques have continuously evolved over years. Last two decades have witnessed huge advancement in understanding of arthroscopic anatomy of wrist and its ligaments. Both open and arthroscopic repair techniques have been utilized to treat the torn TFCC. Till date both methods have given good results in terms of pain relief, failure rates or range of motion without significance difference.18
7.1. Non –operative treatment
As mentioned earlier, the initial treatment of all types of TFCC injury is conservative. This modality of treatment is expected to produce symptomatic relief in about one-third of patient population. The result of treatment is highly dependent on compliance of patient with therapy. Complete abstinence from sports, activity modification, splints or casts, pharmacological agents which reduce pain and inflammation, cold packs to reduce swelling are suggested to achieve healing and reduce pain.
Corticosteroid injections or platelet rich plasma therapy can also be utilized in recalcitrant cases. Physical therapy to prevent stiffness and gain range of motion is instituted once discomfort due to acute trauma or inflammation has subsided. Strengthening exesices are usually begun after 6 weeks of successful recovery.
Duration of conservative trial varies according to symptoms and class of injury. Usually a 6 months trial of non-operative treatment may be done in absence of gross DRUJ instability or a fracture requiring immediate intervention.
8. Surgical management
8.1. Type 1A
Type 1A tears that do not respond to conservative trial are the lesions most suited to be managed by arthroscopic debridement. Unstable flaps created by central disc tear can catch within the joint similar to locking caused by meniscal tear of the knee. Also, tear causes synovitis at its edge and is a source of considerable pain. The aim of debridement is to shave off all loose flaps and create a stable rim of TFCC similar to meniscal debridement and partial meniscectomy. Adams et al. in their study on biomechanics have shown that up to 80% of the disc substance can be removed without creating iatrogenic instability.19
8.1.1. Technique of arthroscopic debridement
Visualization of the TFCC is performed through a standard wrist arthroscopy technique using the dorsal 3–4 portal. Examination of the articular disc tension and rebound ability (trampoline test) is performed using a small arthroscopy probe. Any laxity or a negative trampoline test must alert the surgeon of possible detachment at one or more insertion sites. A hook test to evaluate integrity of foveal insertion of deep fibers of radio-ulnar ligaments on the fovea must also be performed to rule out peripheral avulsions. Debridement is then performed through the 4–5 or 6R portal. This can be achieved using arthroscopic instruments including 2.0-mm or 3.0-mm shavers, radiofrequency ablation probes, or arthroscopic knives/punches.
Good success rates have been reported in literature for the debridement of Type 1A TFCC tears ranging from 66% to 87%.20, 21, 22, 23, 24 However similar success has not been observed when the central tear is associated with ulnar positive variance.20,23,25 The most likely cause of the failure to achieve amelioration of symptoms in these case has been postulated to be due to an underlying degenerative TFCC present along with an acute central disc tear. Addition of ulnar shortening along with debridement of the tear has shown to improve overall success rates from 87% to 99%.26 The recognition of mild, symptomatic degenerative changes in association with Type 1A tears may alter outcomes of arthroscopic debridement in all patients.
8.2. Type 1B
This is the type of tear where most efforts to refine repair techniques have focused. These are, by virtue of being vascular, most amenable to successful repair and healing.
Partial tears do not involve radioulnar ligament injury and thus are stable and can be treated with peripheral capsular sutures arthroscopically. If the TFCC is avulsed from the foveal insertion then a reattachment procedure to re-fix the foveal insertion of radio-ulnar ligaments to the bone is the treatment of choice to restore DRUJ stability and function. For chronic and massively retracted tears, where a healthy edge of TFCC cannot be approximated to capsule or foveal insertion site or tears with severe fraying of margins (irreparable tears, Atzei Class 4), then a tendon graft may be required to bridge the gap during repair.
8.3. Technique of open repair of TFCC
Open repair of the TFCC has been performed over past 30 years with reasonable success. After anaesthesia and tourniquet inflation, a skin longitudinal incision about 5 cm in length, with slight ulnar curvature is made. Superficial dissection involves isolation and protection of transverse branch of the dorsal sensory ulnar nerve. The extensor retinaculum is incised over the fifth compartment and the tendon of extensor digiti minimi is retracted ulnar-wards. The joint is then exposed using a rectangular ulnar based capsular flap carefully protecting the dorsal radio-ulnar ligaments. The attachment of TFCC is evaluated and depending upon whether superficial tear or foveal detachment is found, the repair is done. The attachment site of TFCC is curetted at the fovaea and a small anchor with 2–0 suture (either ethibond or fiberwire) is inserted. One suture limb is then passed lateral to the edge of tear piercing the dorsal ligament and the knot is then tied inside the joint. If the tear is large another suture anchor is inserted into distal ulna and sutures are passed through the disc of TFCC and tied in neutral forearm rotation. The capsular flap is closed and skin is sutured with a 3-0 monocryl.
8.4. Technique of arthroscopic repair of TFCC
8.4.1. Capsular repair
Routine diagnostic arthroscopy is performed with a 30° small joint arthroscope through standard 3–4 and 4–5, portals. Once the tear has been identified and clearly visualized with the scope in the 3–4 portal and with the assistance of a probe (in the 4–5 portal), the trampoline and hook tests are performed. The scar tissue from margin is cleaned with a motorised shaver (in the 4–5 portal) to create a new bleeding margin for proper healing.
A small longitudinal incision is made on the ulnar side of the wrist just anterior to extensor carpi ulnaris tendon, and blunt dissection is used to protect any branches of the dorsal ulnar sensory nerve within the field. The dissection is further carried down to the retinaculum.
With the arthroscope in the 3–4 portal, a 20G needle loaded with no. 2-0 PDS (polydioxanone monofilament) suture is passed into the ulno-carpal joint. The needle is then directed distally and laterally to penetrate the articular disc radial to the edge of the tear. The 2-0 PDS is then advanced into the joint and pulled with small artery forceps or arthroscopy grasper outside the joint through the 4–5 portal to be shuttled later onto the loop from second needle. It is important to withdraw the needle slowly under vision before pulling the suture out, as the sharp beveled tip of the needle and angle of the suture pull can lacerate and weaken the suture. A second needle is then loaded with a loop of no. 2-0 Prolene suture and inserted into ulnocarpal joint and is directed laterally to pierce the TFCC disc dorsal to the PDS entry with a tissue bridge of at least 2 mm in between, and the loop is advanced through the needle into the joint and withdrawn with small artery forceps outside the joint through the 4–5 portal. The 2-0 PDS is carefully shuttled through the loop and withdrawn with the 2-0 PDS from within the joint, creating the first horizontal mattress suture. Same steps are repeated for passing more sutures, usually two or three horizontal mattress suture or a modified Mason-Allen suture configuration is utilized depending upon the size and reducibility of tear (Fig. 3A, Fig. 3B, Fig. 3C, Fig. 3Da,3b,3c and 3d). Both ends of each paired suture are routed such that the knot lies directly on the retinaculum with no interposed subcutaneous tissue or potential nerve branches. The sutures are sequentially tied after releasing the traction (Table 2, Table 3) (Fig. 3A, Fig. 3B, Fig. 3C, Fig. 3Da and b3c,3d).
Fig. 3A.
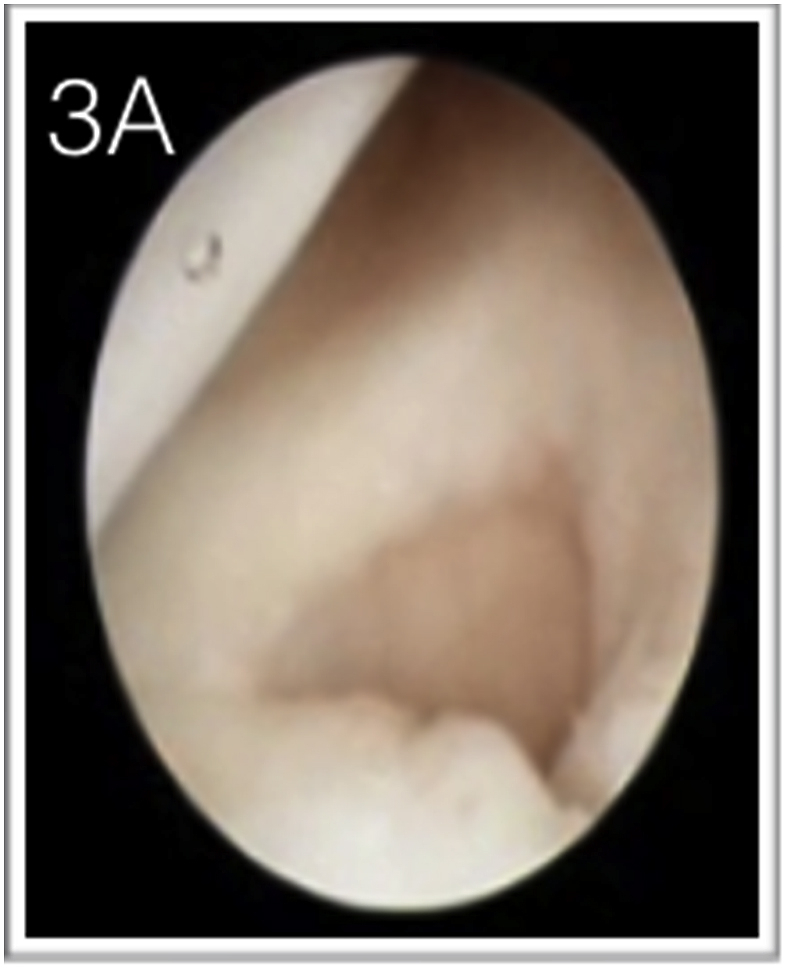
Peripheral TFCC tear being cleared of synovitis and being prepared for repair.
Fig. 3B.
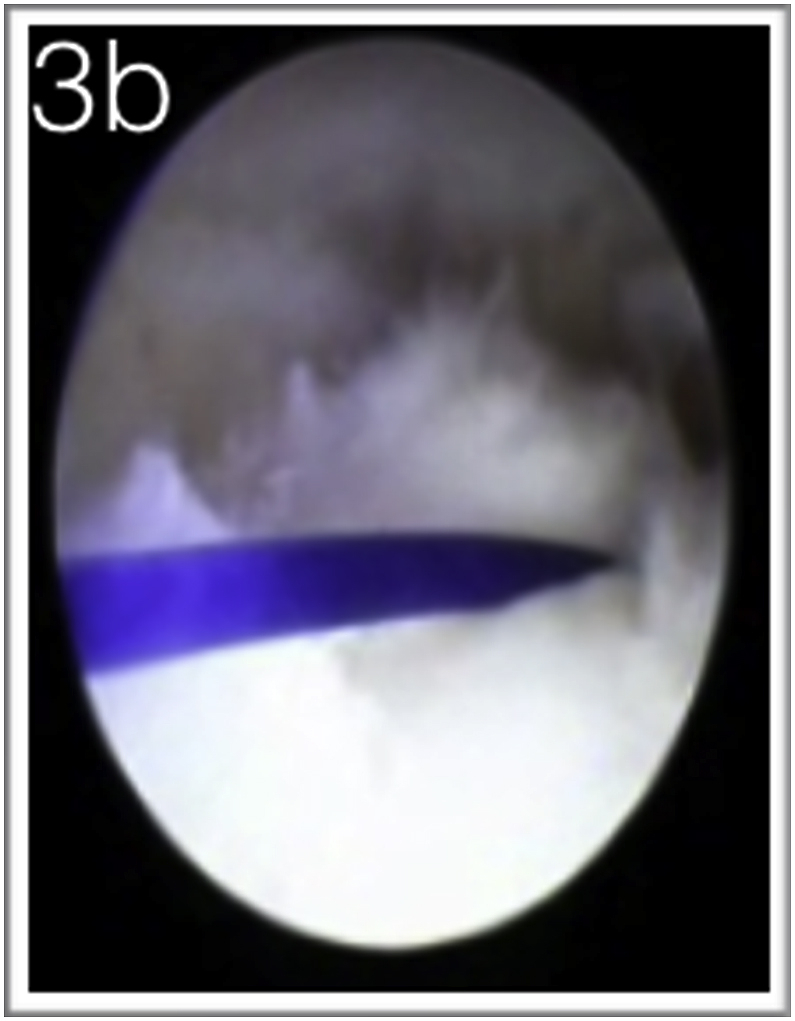
First ulnar sided horizontal mattress suture passed.
Fig. 3C.
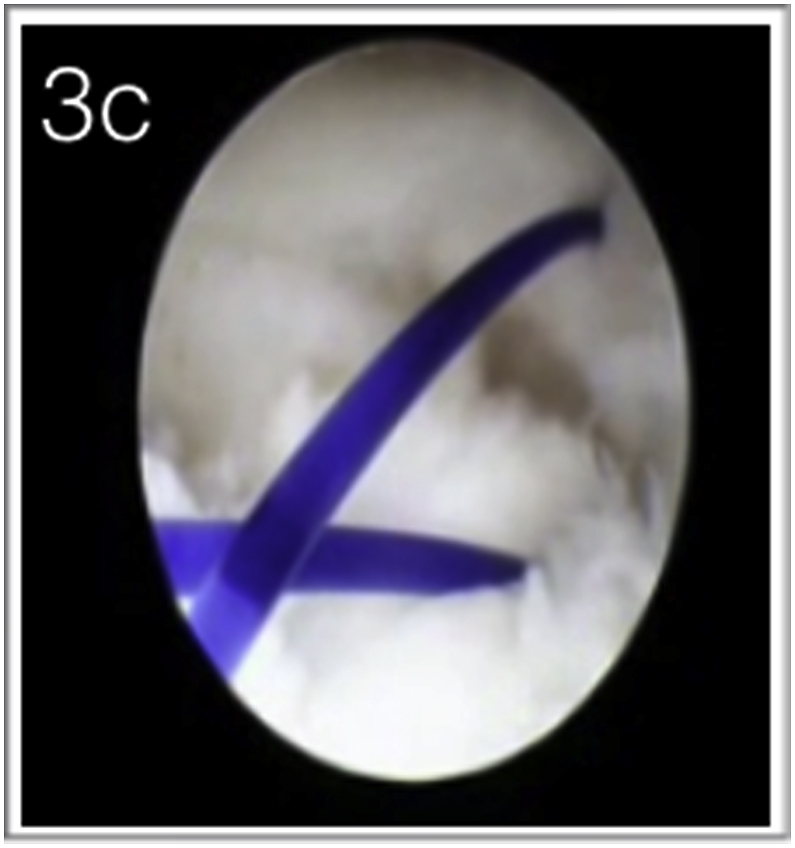
The second simple capsular suture passed radial to the horizontal mattress suture completing the modified Mason-Allen Configuration.
Fig. 3D.
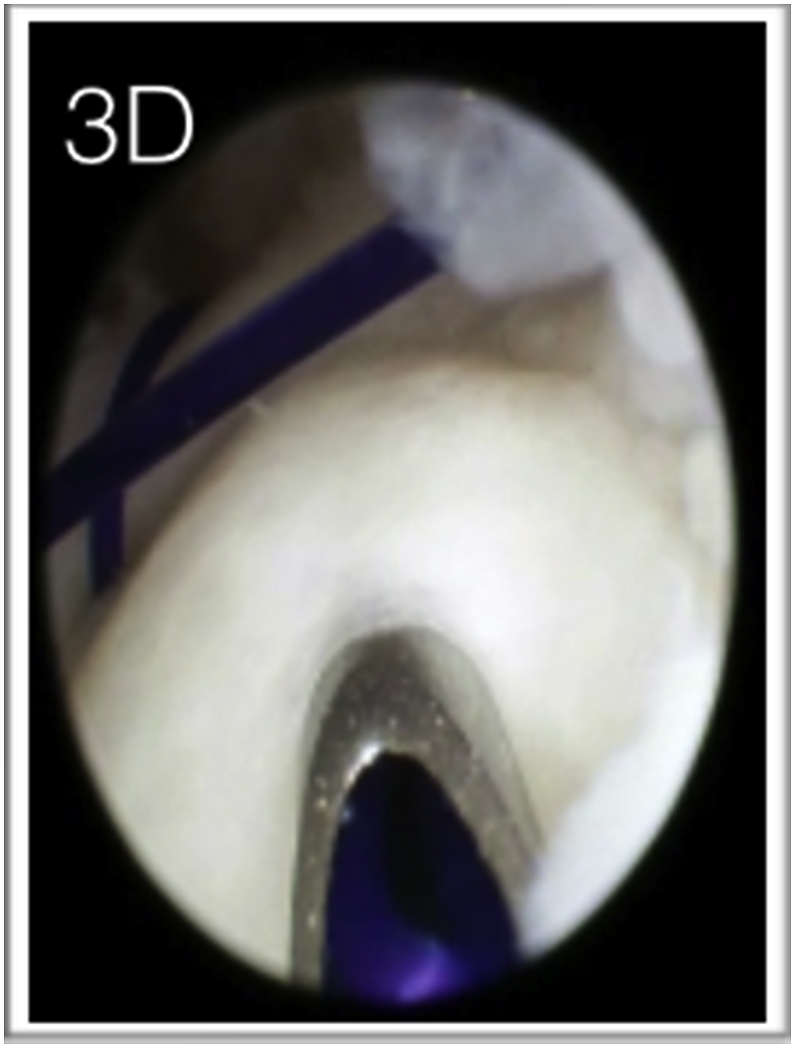
Second Capsular horizontal mattress suture being taken more dorsally to the first completed (not tied) suture assembly.
Table 3.
Pearls in capsular repair of TFCC.
| Pearls in capsular repair |
|---|
| Avoid multiple attempts to pierce the TFCC as it may cause an iatrogenic tear |
| Using a horizontal mattress prevents suture cut through |
| If the TFCC is pierced too radially, then this cause discomfort to the patient |
| Beware of any tendon getting incarcerated in the suture limbs during passing the PDS through loop. This can be avoided by bringing out both the tying suture (PDS) as well as the shuttling suture (Prolene loop) together from the 6R portal to ensure no tissue is caught between the suture limb. |
| Liberal incision to expose and protect dorsal sensory ulnar nerve branches before tying the knot must be made |
8.5. Arthroscopic foveal reattachment using transosseous tunnel
Before the patient is painted and draped, a thorough examination for assessment of DRUJ instability by performing the ballottement test under anaesthesia is done on both limbs. A routine arthroscopic evaluation of the wrist is then performed through the 3–4 and 4–5 & 6R portals under vertical traction. The integrity of TFCC foveal insertion is assessed with the TFCC trampoline sign and the hook test. The TFCC foveal detachment is confirmed by the positive hook test. Direct visualization of fovea through DRUJ portal has been suggested and can be utilized. A skin incision is made along the ulnar border of the distal ulna. The subcutaneous tissue is carefully dissected protecting the superficial ulnar nerve branches. Foveal refreshing, which is a necessary step for cases presenting late, is done to produce a vascular bed that allows the torn TFCC to heal back at its original footprint. A shaver or curette is used from the 4–5 or the 6R portal through the prestyloid recess or through the tear to reach the fovea. The torn or avulsed ligament is also debrided, removing only small rim of tissue to preserve as much as tissue to allow tension free repair. In acute injuries foveal refreshing can be minimal as the foveal bed is not covered with fibrous scar yet. Next, the transosseous tunnel is drilled with a 1.6-mm wire. The drilling is begun about 1 inch proximal to the ulnar styloid tip while keeping the forearm in the neutral rotation. We routinely use a small joint arthroscopy targeting device to aid in penetration of the TFCC at desired point. The targeting device helps in avoiding multiple attempts to create ideal tract for the suture and also prevents injury to cartilage of the carpal bones. The ulnar head is stabilized during drilling by holding it between the thumb and index fingers. Either one or two bony parallel bony tunnels are created (Fig. 4A, Fig. 4B, Fig. 4C, Fig. 4D, Fig. 4Ea,4b,4c and 4d).
Fig. 4A.
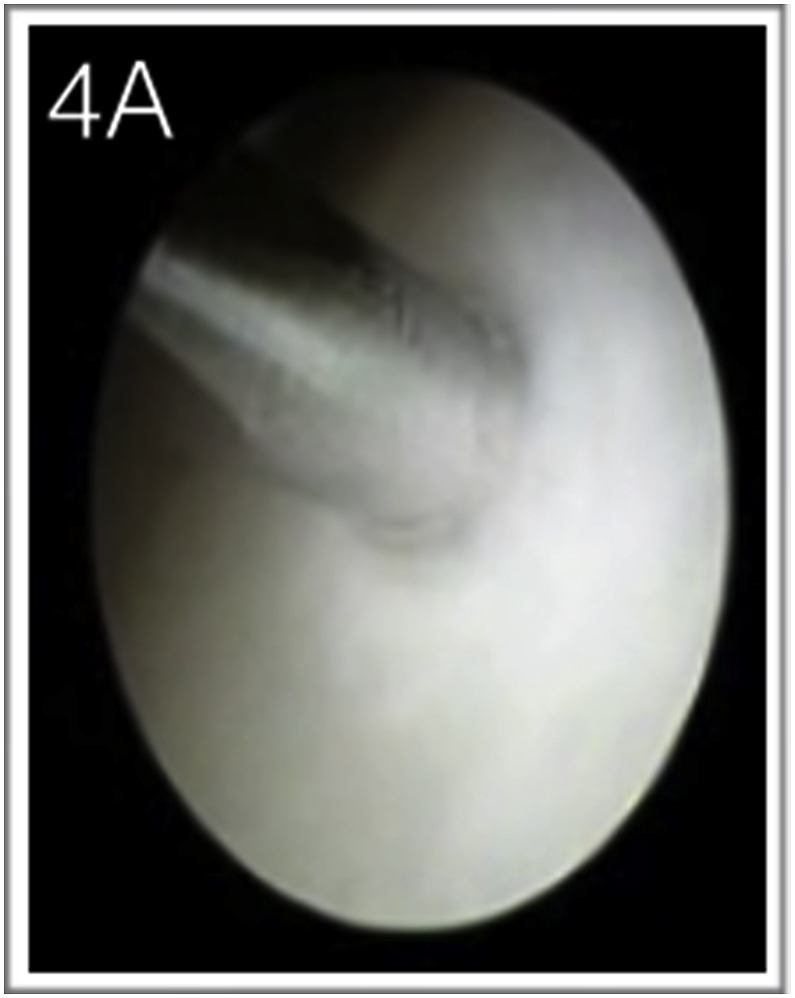
Penetration of the TFCC with a trans-osseous K wire.
Fig. 4B.
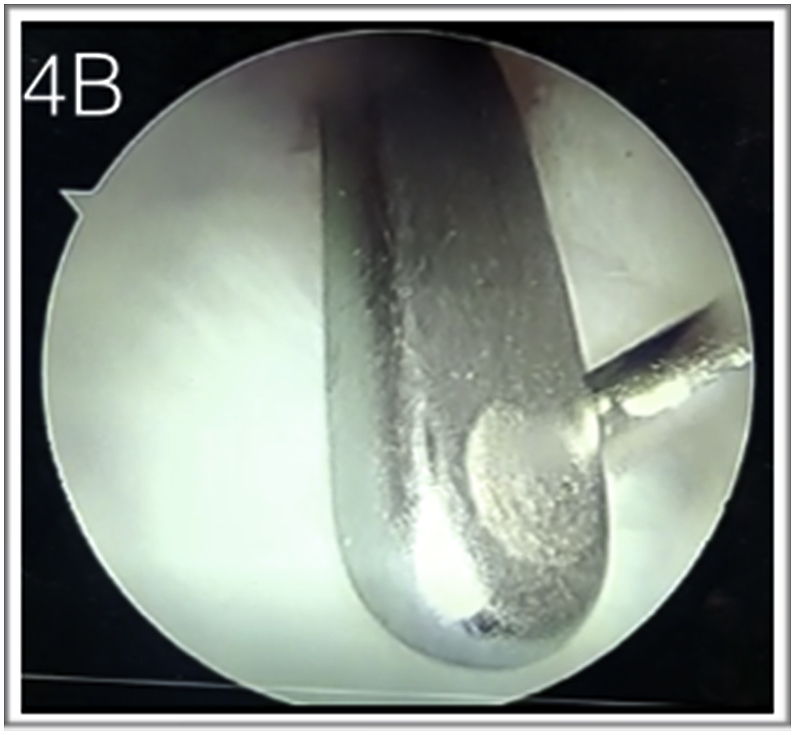
Arthroscopic view of creating the trans-osseous tunnel using a targeting device.
Fig. 4C.

Targeting device with 2 trans-osseous wires inserted.
Fig. 4D.

Sutures (Here 2-0 fibre-wire) being passed through the trans-osseous tunnels.
Fig. 4E.
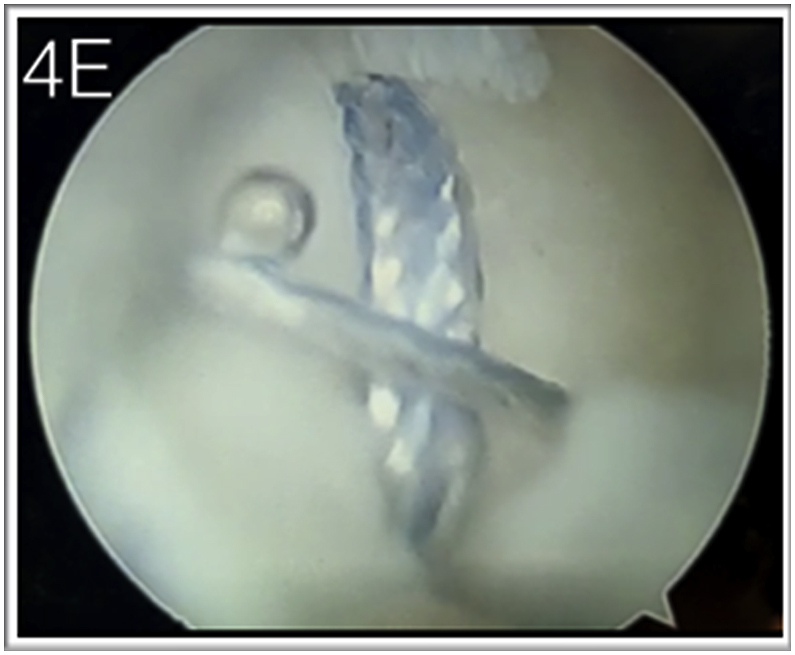
Arthroscopic view of same.
A 2-0 fiber-wire suture is passed into through the bony tunnel using a 16 G needle passed over the K-wire. Under the arthroscopic view from the 3–4 portal, the needle inserted into the ulnar osseous tunnel is pierced through the TFCC, while the DRUJ is properly reduced and the forearm is maintained in the neutral position. Once the suture has passed through the TFCC, it is pulled through the 4–5 portal using a small straight hemostat. This suture is shuttled out through TFCC ulnar edge from the capsule in similar fashion as described for capsular repair. A second suture through another bony tunnel may be passed and retrieved similarly or one or two horizontal mattress capsular sutures are passed in addition. After sutures have been passed, the traction is released, maintaining DRUJ reduction and neutral rotation of forearm, the knots are tied sequentially. The hook test is performed again which should be negative and good trampoline effect of the normal TFCC must be restored to indicate that the TFCC has been well reduced and compressed to its footprint. Skin is closed using an absorbable suture and an above elbow slab is applied in neutral forearm rotation (see Table 4 for pearls).
Table 4.
Pearls in transosseous repair of TFCC.
| Pearls in trans-osseous repair |
|---|
| Avoid making the bony tunnel too vertical as it may cause suture to pass to ulnarly. |
| Use of targeting device helps in piercing the wire into the TFCC at a desirable place |
| Keeping the forearm in neutral rotation while drilling helps in aiming the mid-portion of the ulnar head |
| To prevent laceration of suture from the needle, the needle is withdrawn prior to pulling the suture |
8.6. Outcome of arthroscopic repair
Arthroscopic treatment by repair of oeripheral tears has shown good to excellent results ranging from 60% to 90% in various studies.27, 28, 29, 30, 31 Corso27 used an arthroscopic outside –in technique in 45 patients. He reported good to excellent outcome in 41 patients after an average follow up og 37 months. He concluded that arthroscopic repair was helpful in earlier recovery with minimal soft tissue trauma and improved cosmesis. Degreef and colleagues28 also reported significant amelioration of pain in 47 of 52 wrists treated with arthroscopic repiair. When lesser satisfactory outcome factors were analyzed, Ruch and Papadonikolakis32 found a significant correlation with poorer outcomes and advancing age as well as ulnar-positive variance. More recently Sinohara33 et al. in their study of transossoeus stabilisation of foveal disrupted TFCC showed excellent to good result in 10 out of 11 patients with good restoration of grip strength (84%–98% of unaffected side), no DRUJ instability in 9 patients. Skin irritation at the ulnar neck caused by the suture thread was recognized as a postoperative complication in 3 patients. Atzei et al.34 reported results of 48 patients undergoing arthroscopy for foveal tear and DRUJ instability. After a mean follow-up of 33 months, pain improved significantly but remained moderate in four patients, severe in one. DRUJ instability resolved in 44 (out of 48) patients. Range of motion of wrist, Grip strength, MMWS, and DASH score improved significantly. Excellent and good MMWS equaled 83.3%. Forty-one patients (85.5%) resumed previous work and sport activities. Five patients in their study had neuroapraxia of the dorsal sensory branch of the ulnar nerve (DSBUN) which resolved spontaneously.
Wysocki35 and colleagues also found that arthroscopic capsular repair for peripheral tears with competent foveal attachment had good resolution of pain from 5 to 1 (VAS) and DASH from 38 to 9 at 1 year follow up. However they concluded that return to sport was variable and appeared worse for those who bear weight through the hands during playing.
The single trans-osseous tunnel technique is a reliable method for restoration of DRUJ stability and function as shown by Park et al.36 They reported results in 18 wrist with foveal disruption treated by this method and found that twelve patients had normal stability of the DRUJ and six patients showed mild laxity compared with the contralateral side. The mean VAS for pain perception decreased from 3.7 to 0.8 (P = 0.001). The modified Mayo wrist (P = 0.001) and Quick DASH (P = 0.001) scores showed significant functional improvement. No surgery-related complications occurred.
That, arthroscopic repair of the injured TFCC is a reliable method with long term resolution of pain and disability has also been reported. Soreide E and colleagues37 in their twenty years follow up of arthroscopically treated peripheral tears showed persistent good results in 10 out of 11 patients with no DRUJ instability or repeat surgery in the same wrist.
8.7. Type 1C & 1D
These two sub classes can also be treated by arthroscopic repair,38, 39, 40 but we have limited experience of repairing them. Trumble and colleagues39 have published thier technique of repair of radial sided tear arthroscopically. Thet utilized a modified technique of open repair of 1D tears described by Cooney and colleagues.41
They described the technique as follows. After identifying and refreshing the tear on the radial side of the disc utilizing a standard 3–4 portal for visualization and 6R portal as working portal. The TFCC attachment site on the sigmoid notch is also freshened using a shaver placed in the woking portal. A needle is then placed into the ulno-carpal joint just close to the proximal aspect of the triquetrum. The trajectory for passing the suture across the tear into radius is determined. An arthroscopic cannula is then inserted through a vertical incision along the path of needle. The cannula is utilized to pierce the double armed meniscal repair suture through the radial margin of the disc. The sutures are then passed across the radius in a horizontal mattress manner to exit on its dorso-lateral aspect protecting the sensory branches of radial nerve and the extensor tendons of wrist and thumb. The traction is released before tying the know while wrist is maintained in neutral rotation.
These authors have published their results of repair of radial tears. They found improvement in grip strength and range of motion of 89% and 87% that of the contralateral side, respectively. Eleven of 13 patients had complete relief of pain with all activities, whereas 2 had continued mild pain with moderate activity. Sagerman and Short40 repaired 1D tears in a cohort of 12 patients, and at an average of 17 months reported a 67% good or excellent clinical result.
Edgerton MT & Kollmorgen RC42 have described a novel all - inside arthroscopic technique of radial sided TFCC repair, in a single case report with promising results. More recently Cho et al.43 have also shown that all inside arthroscopic repair of radial sided TFCC is an effective, reliable and safe method of treating this class of tear.
8.8. Type 2
Type 2A, 2B, and 2C lesions are initially treated conservatively. If conservative management is unsuccessful, then a Wafer procedure (described later), which is resection of the distal aspect of the ulnar head, can be performed. Type 2E lesions are also treated by resection of the ulnar head. Type 2D lesions can be treated via ulnar shaft-shortening with osteotomy.1.
8.9. Arthroscopic wafer procedure
Standard arthroscopy portals (3–4, 4–5 and or 6R) are established and the arthroscope is placed through the 3–4 portal, with outflow being obtained using a 18 G needle introduced in the 6U portal. The 4–5 or the 6R portal is utilized for debridement of scapholunate ligament as well as for luno-triquetral ligament if necessary. We always excise large portion of the TFCC central disc to facilitate exposure of ulnar head cartilage but care is taken to prevent breaching the volar or dorsal radio-ulnar ligaments or the TFCC insertion at the base of the styloid. Ulnar head cartilage is removed along with subchondral bone using a small 2 mm burr. Ulnar head is removed first from the radial aspect roughly equal to the diameter of the burr from distal margin of sigmoid notch. This is followed by more ulnar resection (Fig. 5A, Fig. 5Ba and Fig. 5b).
Fig. 5A.
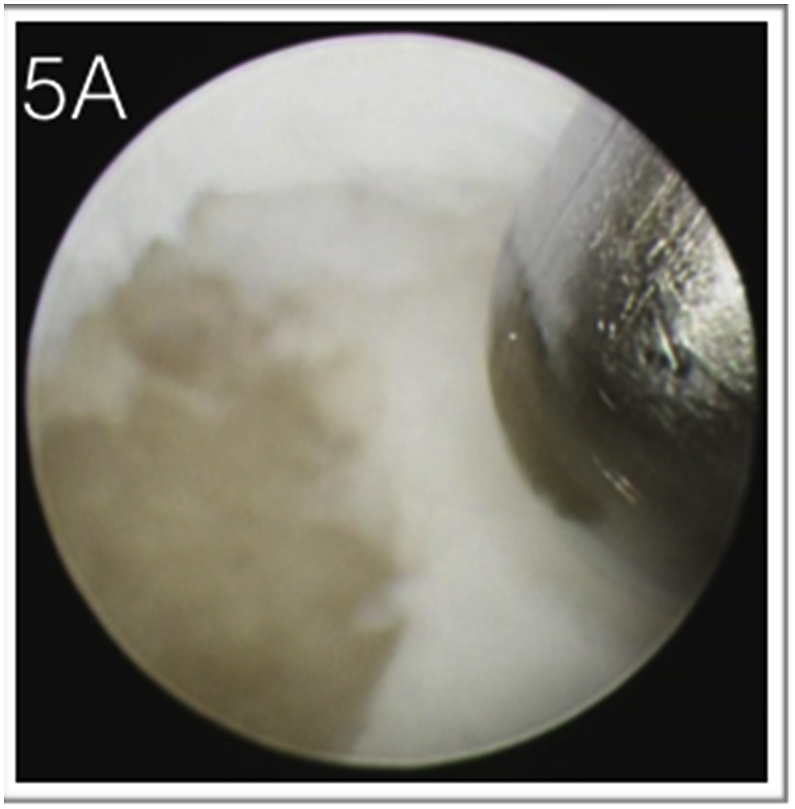
Arthroscopic Wafer with starting point being the radial side.
Fig. 5B.
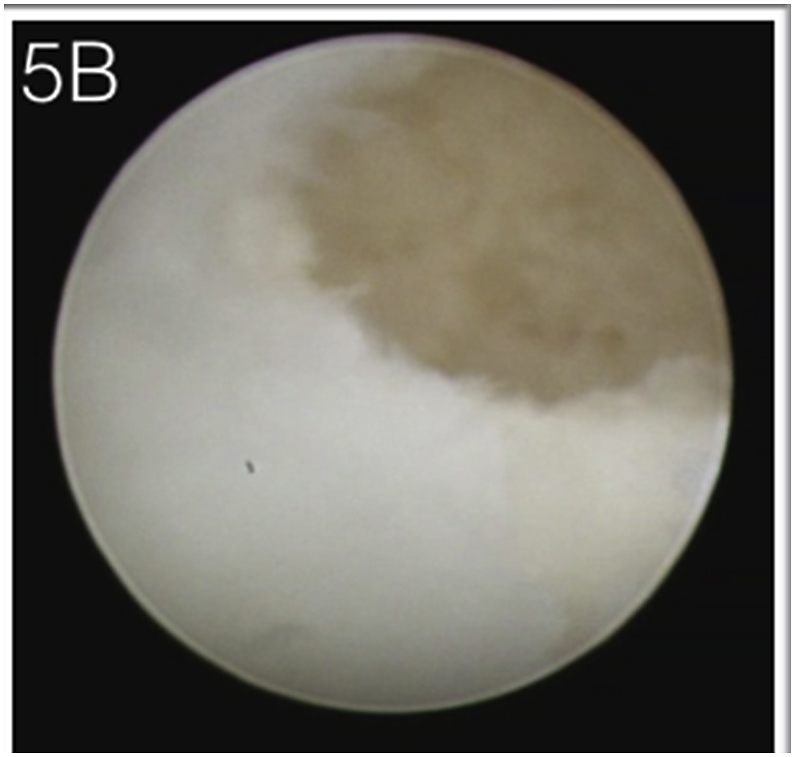
The procedure being advanced more ulnarly gradually taking care not to breach the radio-ulnar ligaments.
With the scope in 3–4 portal and the burr/shaver in 4–5 or 6R portal most of the procedure can be completed. Passive forearm rotation with maintained traction facilitates adequate and uniform removal of subchondral bone. All rough edges of the bone should be trimmed either by burr or using arthroscopic punch. At each stage of the procedure diligent care to avoid violation of radio-ulnar ligaments in the periphery region as well as at the foveal insertion must be taken. The arthroscope should be strategically switched between the 3–4 and 4–5/6R portal to ensure adequate excision at the styloid of ulna and adjacent to lunate fossa respectively.
Skin in closed with absorbable sutures and a slab is applied for 2 weeks. Range of motion is begun within first week and grip strengthening exercises are started over next 2 weeks.
8.10. Complications of arthroscopic management of TFCC
Post-operative complications like infections, hypertrophic scar, tendon injury, nerve injury, reflex sympathetic dystrophy, and joint stiffness can occur with arthroscopic management. Another major risk is of iatrogenic instability following aggressive debridement and during wafer’s procedure.
One of the serious complications is potential injury to the dorsal sensory branch of ulnar nerve. It can be prevented by careful dissection techniques and handling of the nerve after exposure. Knowledge of variation of position of the nerve with forearm rotation reduces the risk of nerve injury. Neuro-praxia of the dorsal sensory branch of ulnar nerve is usually transient and recovers spontaneously in 3–4 months.
The surgical scar of the ulnar side of the wrist can get adhered to deeper tissues and become tender during the early stages of physical therapy.
As in other arthroscopic procedures, infection remains a risk, which is usually prevented by a prophylactic dose of parenteral antibiotics before initiating the procedure.
The dry arthroscopy technique of joint exploration can be utilized to reduce soft tissue infiltration and swelling by the continuous leaking of saline through the portals.
Iatrogenic instability can be prevented by using the shaver/burr in a manner that avoids violating three important anatomical regions, the fovea, the sigmoid notch and the deep fibers of radio-ulnar ligaments. Strategically switching scope between the portals and rotating the lens to improve visualization of all corners and periphery of the joint and to minimize the blind spot is beneficial.
9. Summary
Tears of TFCC are a common cause of ulnar sided wrist pain and varying degree of DRUJ instability. Clinical examination aided by MRI helps in formulating a diagnosis and plan treatment. Most patients with acute tears can initially be managed conservatively if there is no gross instability. Chronic tears can result from previous trauma causing disturbance in ulnar variance. Arthroscopic techniques have evolved over past two decades and can be used as gold standard for evaluating and classifying and treating the TFCC tears. With refinement of surgical techniques and instrumentation, most of the lesion can be treated arthroscopically with very few complications which are self recovering and good to excellent result can be expected in majority of the patients.
Arthroscopic debridement, capsular repair, transosseous repair or a wafer procedure can be employed depending upon type of lesion in most adult patients with predictable outcome.
Acknowledgements
Nil.
Funding statement
The authors received no financial support for research, authorship, and/or publication of this article.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Skalski M.R., White E.A., Patel D.B., Schein A.J., RiveraMelo H., Matcuk G.R. The traumatized TFCC: an illustrated review of the anatomy and injury patterns of the triangular fibrocartilage complex. Curr Probl Diagn Radiol. 2016 Jan-Feb;45(1):39–50. doi: 10.1067/j.cpradiol.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Palmer A.K., Werner F.W. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984 Jul-Aug;(187):26–35. [PubMed] [Google Scholar]
- 3.Tang J.B., Ryu J., Kish V. The triangular fibrocartilage complex: an important component of the pulley for the ulnar wrist extensor. J Hand Surg Am. 1998 Nov;23(6):986–991. doi: 10.1016/S0363-5023(98)80004-X. [DOI] [PubMed] [Google Scholar]
- 4.Semisch M., Hagert E., Garcia-Elias M., Lluch A., Rein S. Histological assessment of the triangular fibrocartilage complex. J Hand Surg Eur. 2016 Jun;41(5):527–533. doi: 10.1177/1753193415618391. [DOI] [PubMed] [Google Scholar]
- 5.Andersson J.K., Axelsson P., Strömberg J., Karlsson J., Fridén J. Patients with triangular fibrocartilage complex injuries and distal radioulnar joint instability have reduced rotational torque in the forearm. J Hand Surg Eur. 2016 Sep;41(7):732–738. doi: 10.1177/1753193415622342. [DOI] [PubMed] [Google Scholar]
- 6.Tay S.C., Tomita K., Berger R.A. The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg. 2007;32A:438–444. doi: 10.1016/j.jhsa.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 7.Moriya T., Aoki M., Iba K. Effect of triangular liga- ment tears on distal radioulnar joint instability and evaluation of three clinical tests: a biomechanical study. J Hand Surg Eur. 2009;34:219–223. doi: 10.1177/1753193408098482. [DOI] [PubMed] [Google Scholar]
- 8.Boer B.C., Vestering M., van Raak S.M., van Kooten E.O., Huis In ’t Veld R., Vochteloo A.J.H. MR arthrography is slightly more accurate than conventional MRI in detecting TFCC lesions of the wrist. Eur J Orthop Surg Traumatol. 2018 Dec;28(8):1549–1553. doi: 10.1007/s00590-018-2215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zlatkin M.B., Rosner J. MR imaging of ligaments and triangular fibrocartilage complex of the wrist. Radiol Clin. 2006;44:595–623. doi: 10.1016/j.rcl.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Oneson S.R., Scales L.M., Timins M.E., Erickson S.J., Chamoy L. MR imaging interpretation of the Palmer classification of triangular fibrocartilage complex lesions. Radiographics. 1996;16:97–106. doi: 10.1148/radiographics.16.1.97. [DOI] [PubMed] [Google Scholar]
- 11.Haims A.H., Schweitzer M.E., Morrison W.B. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol. 2002;178:419–422. doi: 10.2214/ajr.178.2.1780419. [DOI] [PubMed] [Google Scholar]
- 12.Palmer A.K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 13.Palmer A.K., Werner F.W., Glission R.R. Partial excision of the triangular fibrocartilage complex. J Hand Surg Am. 1988;13:391–394. doi: 10.1016/s0363-5023(88)80015-7. [DOI] [PubMed] [Google Scholar]
- 14.Adams B.D. Partial excision of the triangular fibrocar- tilage complex articular disk: a biomechanical study. J Hand Surg Am. 1993;18:334–340. doi: 10.1016/0363-5023(93)90371-9. [DOI] [PubMed] [Google Scholar]
- 15.Melone C.P., Jr., Nathan R. Traumatic disruption of the triangular fibrocartilage complex: pathoanatomy. Clin Orthop. 1992;275:65–73. [PubMed] [Google Scholar]
- 16.Atzei A., Luchetti R. Foveal TFCC tear classification and treatment. Hand Clin. 2011 Aug;27(3):263–272. doi: 10.1016/j.hcl.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 17.Roh Y.H., Hong S.W., Gong H.S., Baek G.H. Prognostic factors of arthroscopic debridement for central triangular fibrocartilage complex tears in adults younger than 45 Years: a retrospective case series analysis. Arthroscopy. 2018 Nov;34(11):2994–2998. doi: 10.1016/j.arthro.2018.05.044. [DOI] [PubMed] [Google Scholar]
- 18.Anderson M.L., Larson A.N., Moran S.L., Cooney W.P., Amrami K.K., Berger R.A. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am. 2008 May-Jun;33(5):675–682. doi: 10.1016/j.jhsa.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 19.Adams B.D., Holley K.A. Strains in the articular disk of the triangular fibrocartilage complex: a biomechanical study. J Hand Surg Am. 1993;18:919–925. doi: 10.1016/0363-5023(93)90066-C. [DOI] [PubMed] [Google Scholar]
- 20.Minami A., Ishikawa J., Suenaga N. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg Am. 1996;21(3):406–411. doi: 10.1016/s0363-5023(96)80353-4. [DOI] [PubMed] [Google Scholar]
- 21.Westkawmper J.G., Mitsionis G., Giannakopoulous P.N. Wrist arthroscopy for the treatment of ligament and triangular fibrocartilage complex injuries. Arthroscopy. 1998;14:479–483. doi: 10.1016/s0749-8063(98)70075-1. [DOI] [PubMed] [Google Scholar]
- 22.Whipple T.L., Geissler W.B. Arthroscopic management of wrist triangular fibrocartilage complex injuries in the athlete. Orthopedics. 1993;16:1061–1067. doi: 10.3928/0147-7447-19930901-16. [DOI] [PubMed] [Google Scholar]
- 23.Miwa H., Hashizume H., Fujiwara K. Arthroscopic surgery for traumatic triangular fibrocartilage complex injury. J Orthop Sci. 1994;9:354–359. doi: 10.1007/s00776-004-0796-1. [DOI] [PubMed] [Google Scholar]
- 24.Blackwell R.E., Jemison D.M., Foy B.D. The holmium:yttrium-aluminum garnet laser in wrist arthroscopy: a five-year experience in the treatment of central triangular fibrocartilage complex tears by partial excision. J Hand Surg Am. 2001;26:77–84. doi: 10.1053/jhsu.2001.20157. [DOI] [PubMed] [Google Scholar]
- 25.Bernstein M.A., Nagle D.J., Martinez A. A comparison of combined arthroscopic triangular fibrocartilage complex debridement and arthro- scopic wafer distal ulna resection versus arthro- scopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ul- nocarpal abutment syndrome. Arthroscopy. 2004;20:392–401. doi: 10.1016/j.arthro.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 26.Hulsizer D., Weiss A.P., Akelman E. Ulna-shortening osteotomy after failed arthroscopic debridement of the triangular fibrocartilage complex. J Hand Surg Am. 1997;22A:694–698. doi: 10.1016/S0363-5023(97)80130-X. [DOI] [PubMed] [Google Scholar]
- 27.Corso S.J., Savoie F.H., Geissler W.B. Arthroscopic repair of peripheral avulsions of the triangular fibrocartilage complex of the wrist: a multicenter study. Arthroscopy. 1997;13:78–84. doi: 10.1016/s0749-8063(97)90213-9. [DOI] [PubMed] [Google Scholar]
- 28.Degreef I., Welters H., Milants P. Disability and function after arthroscopic repair of ulnar avulsions of the triangular fibrocartilage complex of the wrist. Acta Orthop Belg. 2005;71:289–293. [PubMed] [Google Scholar]
- 29.Estrella E.P., Hung L.K., Ho P.C. Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy. 2007;23:729–737. doi: 10.1016/j.arthro.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 30.Millants P., De Smet L., Van Ransbeeck H. Outcome study of arthroscopic suturing of ulnar avulsions of the triangular fibrocartilage complex of the wrist. Chir Main. 2002;21:298–300. doi: 10.1016/s1297-3203(02)00135-x. [DOI] [PubMed] [Google Scholar]
- 31.Anderson M.L., Larson A.N., Moran S.L. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am. 2008;33A:675–682. doi: 10.1016/j.jhsa.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 32.Ruch D.S., Papadonikolakis A. Arthroscopically assisted repair of peripheral triangular fibrocartilage complex tears: factors affecting outcome. Arthroscopy. 2005;21:1126–1130. doi: 10.1016/j.arthro.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 33.Shinohara T., Tatebe M., Okui N., Yamamoto M., Kurimoto S., Hirata H. Arthroscopically assisted repair of triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2013 Feb;38(2):271–277. doi: 10.1016/j.jhsa.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 34.Atzei A., Luchetti R., Braidotti F. Arthroscopic foveal repair of the triangular fibrocartilage complex.52. J Wrist Surg. 2015 Feb;4(1):22–30. doi: 10.1055/s-0035-1544226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wysocki R.W., Richard M.J., Crowe M.M., Leversedge F.J., Ruch D.S. Arthroscopic treatment of peripheral triangular fibrocartilage complex tears with the deep fibres intact. J Hand Surg Am. 2012 Mar;37(3):509–516. doi: 10.1016/j.jhsa.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 36.Park J.H., Kim D., Park J.W. Arthroscopic one-tunnel transosseous foveal repair for triangular fibrocartilage complex (TFCC) peripheral tear. Arch Orthop Trauma Surg. 2018 Jan;138(1):131–138. doi: 10.1007/s00402-017-2835-3. [DOI] [PubMed] [Google Scholar]
- 37.Soreide E., Husby T., Haugstvedt J.R. A long-term (20 years’) follow-up after arthroscopically assisted repair of the TFCC.) J Plast Surg Hand Surg. 2017 Oct;51(5):296–300. doi: 10.1080/2000656X.2016.1256296. [DOI] [PubMed] [Google Scholar]
- 38.Jantea C.L., Baltzer A., Ruther W. Arthroscopic repair of radial-sided lesions of the triangular fibrocartilage complex. Hand Clin. 1995;11:31–36. [PubMed] [Google Scholar]
- 39.Trumble T.E., Gilbert M., Vedder N. Isolated tears of the triangular fibrocartilage: management by early arthroscopic repair. J Hand Surg Am. 1997;22:57–65. doi: 10.1016/S0363-5023(05)80180-7. [DOI] [PubMed] [Google Scholar]
- 40.Sagerman S.D., Short W. Arthroscopic repair of radial-sided triangular fibrocartilage complex tears. Arthroscopy. 1996;12:339–342. doi: 10.1016/s0749-8063(96)90071-7. [DOI] [PubMed] [Google Scholar]
- 41.Cooney W.P., Linscheid R.L., Dobyns J.H. Triangular fibrocartilage tears. J Hand Surg Am. 1994;19:143–154. doi: 10.1016/0363-5023(94)90238-0. [DOI] [PubMed] [Google Scholar]
- 42.Edgerton M.T., Kollmorgen R.C. A novel all-inside arthroscopic technique for radial-sided triangular fibrocartilage complex tears: a case report and review of literature. Hand. 2017 Sep;12(5):NP166–NP169. doi: 10.1177/1558944717715138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cho C.H., Lee Y.K., Sin H.K. Arthroscopic direct repair for radial tear of the triangular fibrocartilage complex. Hand Surg. 2012;17(3):429–432. doi: 10.1142/S0218810412970076. [DOI] [PubMed] [Google Scholar]