Abstract
The deleterious effects of diabetes in the heart are increasingly attributed to inflammatory signaling through the NLRP3 (NOD, LRR and PYD domains-containing protein 3) inflammasome. Thrombin antagonists reduce cardiac remodeling and dysfunction in diabetic mice, in part by suppressing fibrin-driven inflammation. The role of cellular thrombin receptor subtypes in this context is not known. We sought to determine the causal involvement of protease-activated receptors (PAR) in inflammatory signaling of the diabetic heart. Mice with diet-induced diabetes showed increased abundance of procaspase-1 and pro-interleukin (IL)-1β in the left ventricle (LV), indicating transcriptional NLRP3 inflammasome priming, and augmented cleavage of active caspase-1 and IL-1β, pointing to canonical NLRP3 inflammasome activation. Caspase-11 activation, which mediates non-canonical NLRP3 inflammasome signaling, was not augmented. Formation of the plasma membrane pore-forming protein N-terminal gasdermin D (GDSMD), a prerequisite for IL-1β secretion, was also higher in diabetic vs. control mouse LV. NLRP3, ASC and IL-18 expression did not differ between the groups, nor did expression of PAR1 or PAR2. PAR3 was nearly undetectable. LV abundance of PAR4 by contrast increased with diabetes and correlated positively with active caspase-1. Genetic deletion of PAR4 in mice prevented the diet-induced cleavage of caspase-1, IL-1β and GDSMD. Right atrial appendages from patients with type 2 diabetes also showed higher levels of PAR4, but not of PAR1 or PAR2, than non-diabetic atrial tissue, along with increased abundance of cleaved caspase-1, IL-1β and GSDMD. Human cardiac fibroblasts maintained in high glucose conditions to mimic diabetes also upregulated PAR4 mRNA and protein, and increased PAR4-dependent IL-1β transcription and secretion in response to thrombin, while PAR1 and PAR2 expressions were unaltered. In conclusion, PAR4 drives caspase-1-dependent IL-1β production through the canonical NLRP3 inflammasome pathway in the diabetic heart, providing mechanistic insights into diabetes-associated cardiac thromboinflammation. The emerging PAR4-selective antagonists may provide a feasible approach to prevent cardiac inflammation in patients with diabetes.
Keywords: Thrombin, Protease-activated receptor, Diabetes, Diabetic cardiomyopathy, Inflammation, Cardiac fibroblasts
Introduction
The heart is a major target for end-organ damage in metabolic disorders such as obesity and type 2 diabetes. The constellation of complications that characterize adiposity and diabetes includes a hypercoagulable state, with enhanced thrombin generation leading to a chronic low-grade thromboinflammation [11, 42, 47, 51]. Thrombin inhibition prevents diet-induced cardiac remodeling and dysfunction in mice [3, 4, 27, 28], consistently accompanied by reduced cardiac expression of the major thrombin receptors protease-activated receptor (PAR)1 and PAR4. Similarly, inhibition of activated factor X (FXa) with rivaroxaban blunted fibroinflammation in a mouse model of ischemic cardiomyopathy with high fat loading, in part by suppressing the expression of the major FXa-receptor PAR2 [31]. These findings suggest that coagulant proteases are present in the heart, and able to direct cellular signaling events that lead to adverse remodeling and inflammation. Extrahepatic prothrombin/thrombin distribution has been reported in various tissues including the myocardium, and seems to be identical to the plasma forms of the zymogen and active protease [24, 35]. Cardiac prothrombin/thrombin may therefore originate from the circulation, delivered by infiltrating immune cells, or from expression in situ. There is some evidence for a local coagulant system in the heart, encompassing the expression of tissue factor and prothrombin, with local activation to thrombin provided by proteases such as fibrinogen-like protein 2 (fibroleukin), mannose-binding lectin-associated serine proteases and matrix metalloproteinase-12, or by histones released from necrotic cells [10, 12, 39, 40]. Alternatively, PAR4 may not be in the first instance a receptor for thrombin, but rather for proteases such as cathepsin G released by neutrophils and mast cells, which are abundant in the diabetic heart [14].
Although causal involvement of PAR1 and PAR4 in the cardiac complications of metabolic disease is plausible, it has not yet been directly demonstrated. We have reported increased expression of PAR4 in whole heart lysates and isolated cardiac fibroblasts of mice fed a high-fat diet, and involvement of upregulated PAR4 in oxido-inflammatory stress in mouse cardiac fibroblast cultured under high glucose conditions [26]. By contrast, PAR1 and PAR3 are not upregulated under diabetic conditions [9, 26, 37]. Thus, selective PAR4 antagonists, which are currently in development as safer antithrombotics [22, 59], may exert unrecognized cardioprotective effects beyond platelet inhibition [14].
The NLRP3 (NACHT, LRR and PYD domains-containing protein 3) inflammasome is increasingly considered to be a driver of cardiac remodeling and diabetic cardiomyopathy [8, 33, 48, 49]. The NLRP3 inflammasome is essentially an activating platform for caspase-1, previously known as interleukin-converting enzyme given its primary function of proteolytic maturation of interleukin-1β (IL-1β) and IL-18 (reviewed in [20]). NLRP3 inflammasome-dependent caspase-1 activation and cytokine maturation are controlled at multiple levels: (1) transcriptional (NFKB-dependent) priming of the inflammasome components, and (2) triggering of the assembly of inflammasome components, with subsequent activation of caspase-1 through auto-cleavage. Besides pro-interleukin processing, a further function of caspase-1 is the cleavage of gasdermin D (GSDMD). This generates the plasma membrane pore-forming protein N-terminal (Nt) GSDMD, which enables the secretion of mature cytokines and hence transmission of inflammatory signaling to neighboring cells. Non-canonical NLRP3 activation and GDSMD pore formation are mediated through caspase-11 [20], but the relative contribution of this pathway to inflammatory signaling in the diabetic heart is not known. Numerous damage-associated molecular patterns (DAMPs) and other stress signals relevant to the diabetic state have been shown to drive canonical NLRP3 inflammasome priming and/or triggering, such as high glucose, endoplasmic reticulum (ER) stress and mitochondrial redox stress [13, 41, 58, 61]. Thrombin has been reported to activate the NLRP3 inflammasome in platelets and astroglia [44, 63], but no functional or regulatory interactions have to date been demonstrated in cardiac cells.
Here, we tested the hypothesis that upregulation of PAR4 thrombin receptors drives NLRP3 inflammasome-dependent caspase-1 activation in the diabetic heart.
Methods
High-fat diet (HFD) mouse model
PAR4−/− mice on C57Bl/6J background were generously provided by Dr. Justin Hamilton (Australian Centre for Blood Diseases, Melbourne, AUS) and bred heterozygously in-house. Male wild-type (WT) and PAR4−/− littermates aged 8 weeks received either control chow or high-fat diet (HFD, #S7200-E010, Ssniff Spezialdiäten GmbH, Soest, Germany) to induce obesity and glucose intolerance [19, 26]. Mice were weighed weekly during the 8-week treatment period. Body fat mass was determined using the Minispec NMR analyzer (Bruker Corporation, Billerica, MA, USA) after 2, 4 and 8 weeks. Oral glucose tolerance test (oGTT) was performed at 6 weeks, after a 6 h fasting period. Glucose (1 g/kg) was applied per os, and tail-vein blood glucose concentration was measured after 5, 15, 30, 60 and 120 min with the ACCU-CHEK Compact Plus device (Roche, Mannheim, Germany). After 8 weeks of feeding, mice were fasted for 6 h and then killed with CO2. Left ventricles (LV) were snap-frozen and stored for later analysis at − 80 °C. Body length was measured from nose to anus for determination of body mass index (BMI). The studies had the approval of the local animal experimentation ethics committee (Approval Number Az. 84–02.04.2012.A366, granted by the Landesamt für Natur, Umwelt und Verbraucherschutz Nordrhein-Westfalen).
Human atrial samples
Right atrial appendages were obtained from patients with type 2 diabetes mellitus (DM, n = 15) and non-diabetic control (Ctl, n = 13) patients undergoing open heart surgery for coronary bypass grafting or valve replacement. Each patient gave written informed consent. Tissue samples were collected immediately prior to atrial cannulation for extracorporeal circulatory bypass, stored in Tyrode’s solution and transferred to the laboratory for freezing. Diabetes was defined on the basis of an existing physician’s diagnosis of type 2 diabetes, BMI > 30 and use of oral antidiabetic drugs. Patient characteristics are depicted in Table 1. The studies were approved by the Human Ethics Committee of the Medical Faculty of the University Duisburg-Essen (Approval Number AZ: 12–5268-BO) and were performed in accordance with the Declaration of Helsinki.
Table 1.
Patient characteristics
| Characteristics | Control | Diabetes |
|---|---|---|
| Patients, n | 13 | 15 |
| Male gender, n (%) | 7 (54) | 9 (60) |
| Age (years), mean ± SD | 72 ± 7 | 70 ± 6 |
| BMI (kg/m2), mean ± SD | 25 ± 2 | 34 ± 3* |
| CAD, n (%) | 23 (0) | 4 (27) |
| AVD/MVD, n (%) | 5 (38) | 7 (47) |
| CAD + AVD/MVD, n (%) | 5 (38) | 4 (27) |
| Hypertension, n (%) | 10 (77) | 10 (67) |
| Hyperlipidemia, n (%) | 7 (54) | 13 (87)* |
| Smoker—current or ex, n (%) | 4 (31) | 6 (40) |
| Previous MI, n (%) | 3 (23) | 0 (0) |
| LV hypertrophy, n (%) | 5 (38) | 5 (33) |
| LVEF (%), mean ± SD§ | 57 ± 11 | 58 ± 9 |
| LA diameter (mm), mean ± SD§§ | 47 ± 13 | 44 ± 10 |
| Antidiabetic drugs, n (%)# | 0 (0) | 15 (100)* |
| ACEI/ARB, n (%) | 11 (85) | 12 (80) |
| Beta blockers, n (%) | 6 (46) | 10 (67) |
| Calcium channel blockers, n (%) | 0 (0) | 1 (6) |
| Digitalis, n (%) | 0 (0) | 1 (6) |
| Diuretics, n (%) | 6 (46) | 10 (67) |
| Lipid-lowering drugs, n (%) | 7 (54) | 10 (67) |
| Oral anticoagulants, n (%) | 1 (7) | 3 (20) |
| Platelet inhibitors, n (%) | 8 (62) | 9 (60) |
| CRP (mg/dL), mean ± SD | 0.57 ± 0.5 | 0.56 ± 0.5 |
| Leukocytes (/nL), mean ± SD | 7.8 ± 1.3 | 8.7 ± 2.7 |
Wilcoxon rank sum test used for continuous variables. Fisher’s exact test used for categorical values
ACEI angiotensin-converting enzyme inhibitors, AF atrial fibrillation, ARB angiotensin receptor blockers, AVD aortic valve disease, BMI body mass index, CAD coronary artery disease, CRP C-reactive protein, EF ejection fraction, LA left atrial, LV left ventricular, MI myocardial infarction, MVD mitral valve disease, SD standard deviation
P < 0.05
Insulin and/or metformin and/or sitagliptin, glibenclamide or dapagliflozin
Data missing from n = 2 control and n = 2 diabetes patients
Data missing from n = 4 control and n = 6 diabetes patients
Human ventricular cardiac fibroblasts
Adult human ventricular cardiac fibroblasts obtained from ScienCell (Provitro AG, Berlin Germany) at passage 1 were cultured in Fibroblast Growth Medium-2 containing 10% fetal bovine serum (FBS, both from ScienCell) and d-glucose (Sigma-Aldrich, Munich, Germany) at either 5.5 mmol/L (low glucose, LG) or 25 mmol/L (high glucose, HG). Cells were studied at passages 2–3. Cells were acclimatized to 2% FBS for 3 h prior to study, then stimulated for 24 h ± human alpha thrombin (3 U/mL, American Diagnostica GmbH, Pfungstadt, Germany) ± the PAR4 antagonist ML354 (200 nmol/L, added 15 min prior to thrombin). Supernatants and cell pellets were separately frozen at − 80 °C for analysis.
Western blot
Proteins of interest were quantified by Western blot and normalized to γ-tubulin, which was verified as a reliable loading control in prior experiments. Cell pellets were directly lysed in 1 × Laemmli sample buffer containing 0.01 M Tris, 2% sodium dodecyl sulfate (SDS) and 0.1 M dithiothreitol (DTT), and heated to 95 °C for 5 min. Frozen human or mouse tissues were crushed under liquid nitrogen and homogenized in Kranias lysis buffer, containing 1.5 M Tris (pH 8.8), 0.5 M EDTA (pH 8.0), 1 M NaF, 20% SDS and 10% glycerol. Kranias buffer was supplemented with 1:10 cOmplete™ Mini Protease Inhibitor Cocktail and 1:10 PhosSTOP™ Phosphatase Inhibitor Cocktail immediately prior to use. All chemicals were from Sigma-Aldrich. Homogenates were cleared by centrifugation (15 min, 900 × g at room temperature) and protein content was assessed with the Pierce BCA Protein Assay Kit (ThermoFisher Scientific, Dreieich, Germany). 100 μL aliquots of cleared lysates were supplemented with 20 μL of 6 × Laemmli buffer and heated to 95 °C for 5 min. Western blotting was performed as described [26]. Primary antibodies were purchased from: Santa Cruz Biotechnology (Dallas, USA: Caspase-1, Caspase-11, GSDMD, PAR1, PAR2, all diluted 1:500), Abcam (Berlin, Germany: PAR4, IL-1β, IL-18, TNFα, all diluted 1:1000), Novus Biologicals (Bio-Techne, Wiesbaden, Germany: NLRP3, diluted 1:1000) and ThermoFisher Scientific (γ-tubulin, diluted 1:1000). Infrared-coupled secondary antibodies were all obtained from LI-COR Biosciences (Bad Homburg, Germany) and diluted 1:1000. Band visualization and quantification were performed using the LI-COR Odyssey platform as described [19].
Quantitative real-time PCR (qPCR)
Total RNA was extracted from mouse LV and human cardiac fibroblasts for SYBR Green® qPCR assessment of mRNA expression levels as described [26]. Human and/or mouse Quantitect Validated Primer Assays for PAR1 (F2R), PAR2 (F2RL1), PAR3 (F2RL2), PAR4 (F2RL3), NLRP3, ASC (PYCARD), tumor necrosis factor α (TNFα), IL-1β and the housekeeping gene ribososmal 18S were purchased from Qiagen (Hilden, Germany).
IL-1β secretion
IL-1β secretion from human cardiac fibroblasts was assessed in media collected and frozen immediately after stimulation, using the Invitrogen Human IL-1beta Uncoated ELISA Kit (ThermoFisher Scientific) as instructed.
Statistical analysis
For animal and cell culture data, differences between two groups were determined by the unpaired t test or the Wilcoxon rank sum test as appropriate. Statistical testing of more groups utilized one-way or two-way analysis of variance, with Dunnet’s or Tukey’s post hoc multiple comparison procedure applied as appropriate. For clinical data, differences between the groups were determined using the Wilcoxon rank sum test for continuous variables, and twosided Fisher’s exact test for categorical values. Significance of correlations was determined as Pearson’s correlation coefficient. P < 0.05 was accepted as statistically significant.
Results
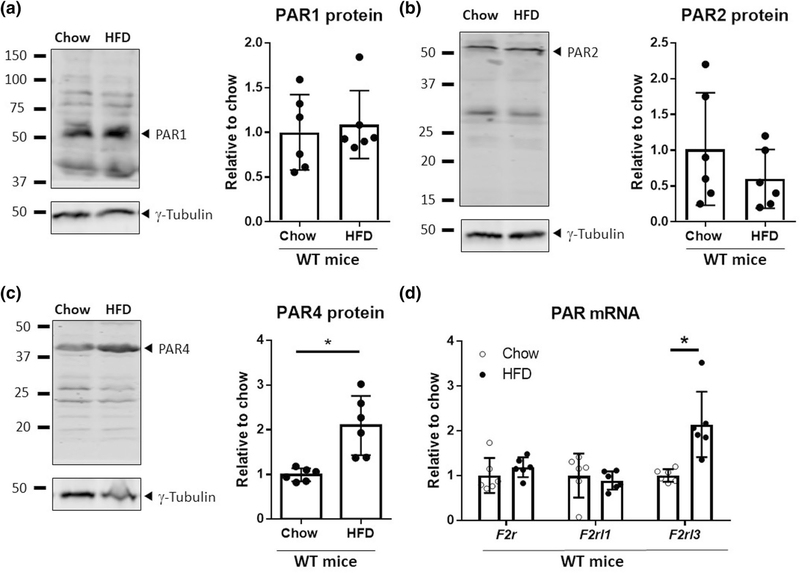
High-fat diet (HFD) increases cardiac PAR4 expression in mice
We previously found increased expression of PAR4, but not other PAR-subtypes, in LV of HFD-fed mice [26]. The same model was applied here to test the hypothesis that upregulation of PAR4 drives NLRP3 inflammasome signaling in the diabetic mouse heart. After 8 weeks of HFD, mice exhibited the typical sequelae of increased weight gain, body fat accumulation and BMI than chow-fed littermates, together with higher fasting blood glucose levels and impaired tolerance to oral glucose challenge (Suppl. Fig. S1, all n = 6). LV lysates of HFD-fed mice showed significantly increased abundance of F2rl3 mRNA and PAR4 total protein in comparison to LV from chow-fed mice, while gene and protein expressions of F2r/PAR1 and F2rl1/PAR2 were unaltered (Fig. 1). F2rl2 (PAR3) mRNA was barely detectable, with CT values > 37 (data not shown).
Fig. 1.
HFD upregulates cardiac PAR4. a PAR1, b PAR2 and c PAR4 protein expression, normalized to γ-tubulin, and d PAR1 (F2r), PAR2 (F2rl1) and PAR4 (F2rl3) mRNA expression, normalized to ribosomal 18S, in LV lysates of wild-type (WT) mice fed HFD or standard chow for 8 weeks (n = 6 each). Data show mean ± SD, relative to chow. *P < 0.05 vs. chow
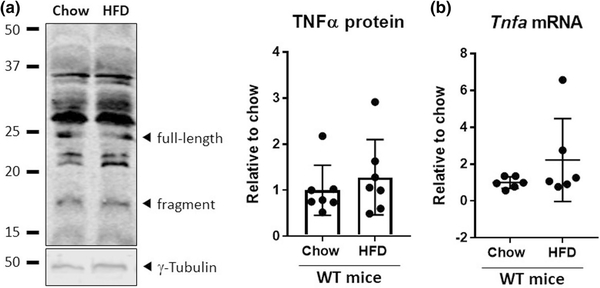
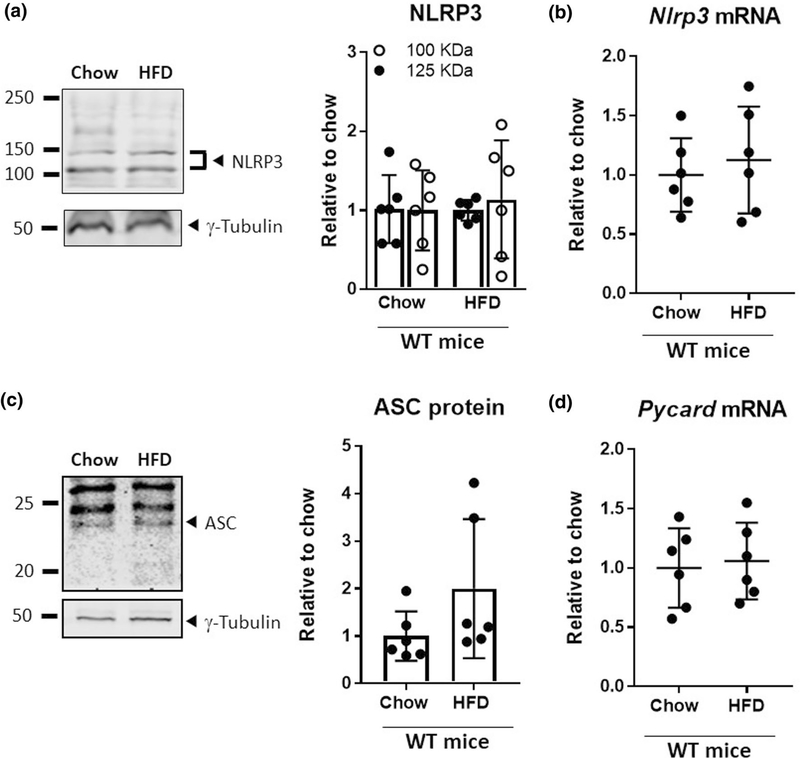
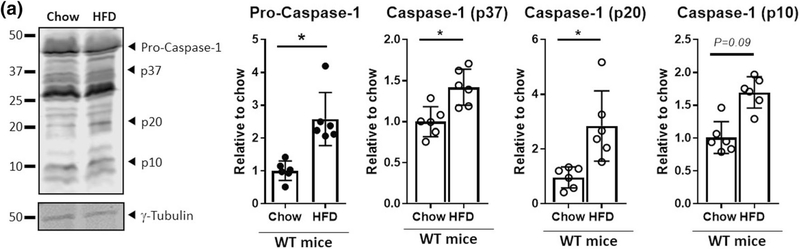
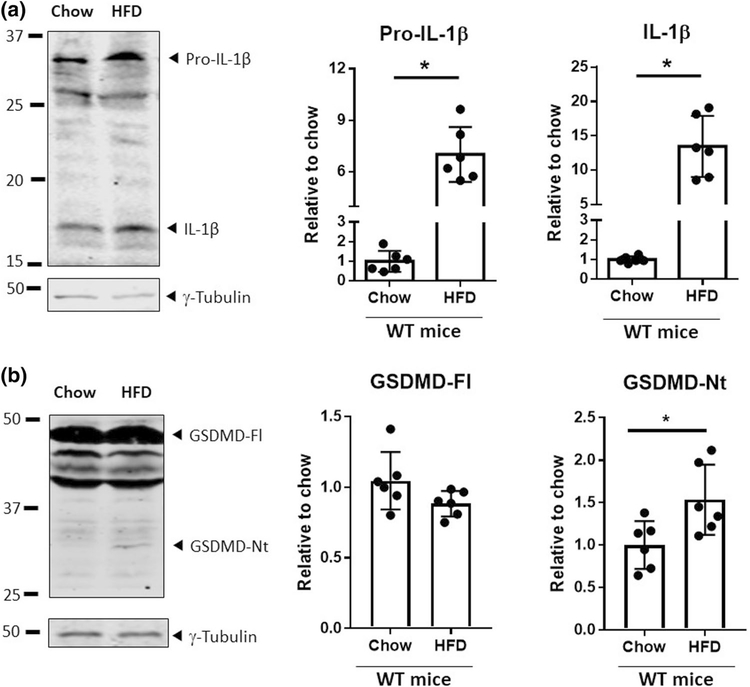
HFD drives caspase-1 expression and activation in LV of wild-type mice
We previously observed augmented PAR4-mediated expression of TNFα in human vascular smooth muscle cells maintained in high glucose conditions [9, 37]. We therefore examined if this also occurs in the hearts of HFD-fed mice, but found no significantly elevated TNFα protein or Tnfa mRNA levels in LV of mice fed HFD compared to chow (Fig. 2). Expression of the inflammasome components NLRP3 and ASC was comparable at both protein and mRNA levels in LV of mice fed HFD or chow for 8 weeks (Fig. 3) By contrast, the abundance of pro-caspase-1 and cleaved (active) forms of caspase-1 (p37, p20, p10) were increased in the HFD group (Fig. 4), Also augmented were the protein levels of pro-IL-1β and processed (active) IL-1β and the processing of full-length GSDMD to the pore-forming GSDMD-Nt. (Fig. 5). No difference was noted between the groups in the expression of pro-IL-18 or cleaved IL-18 (data not shown). Caspase-11, which mediates non-canonical NLRP3 inflammasome pathways [20], was reduced in the HFD group compared to chow-fed control mice (Fig. 6), so subsequent experiments focused on the canonical pathway involving caspase-1 only.
Fig. 2.
HFD does not significantly increase TNFα. a Expression of TNFα protein, normalized to γ-tubulin, and b Tnfa mRNA, normalized to ribosomal 18S, in LV lysates of wild-type (WT) mice fed an HFD or standard chow for 8 weeks (n = 6 each). Data show mean ± SD, relative to chow. *P < 0.05 vs. chow
Fig. 3.
HFD does not affect NLRP3 or ASC transcriptional priming. a Expression of NLRP3 protein, normalized to γ-tubulin, and b Nlrp3 mRNA, normalized to ribosomal 18S, and c expression of ASC protein and d Pycard (ASC) mRNA, in LV lysates of wild-type (WT) mice fed an HFD or standard chow for 8 weeks (n = 6 each). Data show mean ± SD, relative to chow. *P < 0.05 vs. chow
Fig. 4.
HFD drives caspase-1 expression and activation in mouse LV. a Abundance of pro-caspase-1 (p45) and cleaved caspase-1 (p37, p20, p10), in LV lysates of wild-type (WT) mice fed an HFD or standard chow for 8 weeks (n = 6 each). Protein expression is normalized to γ-tubulin. Data show mean ± SD, relative to chow. *P < 0.05 vs. chow
Fig. 5.
HFD augments IL-1β and gasdermin D activation in mouse LV. a Abundance of pro-IL-1β and mature IL-1β, and b full-length (FL) and N-terminal (Nt) gasdermin D (GSDMD), in LV lysates of wild-type (WT) mice fed an HFD or standard chow for 8 weeks (n = 6 each). Protein expression is normalized to γ-tubulin. Data show mean ± SD, relative to chow. *P < 0.05 vs. chow
Fig. 6.
HFD does not activate non-canonical inflammasome pathways. a Abundance of pro-caspase-11 and cleaved caspase-11, in LV lysates of wild-type (WT) mice fed an HFD or standard chow for 8 weeks (n = 6 each). Protein expression is normalized to γ-tubulin. Data show mean ± SD, relative to chow. *P < 0.05 vs. chow
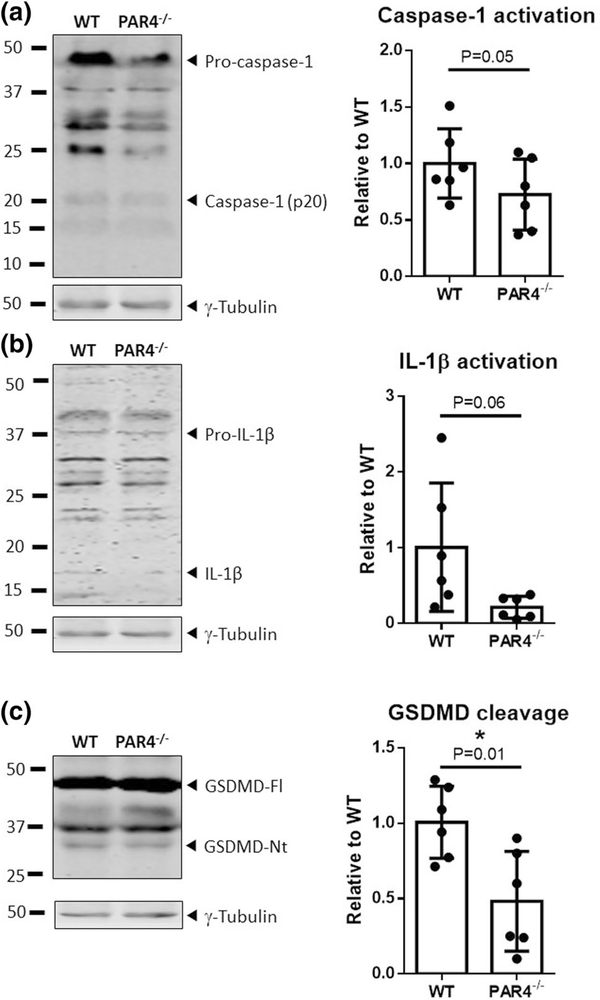
HFD-induced caspase-1 activation is attenuated in hearts from PAR4-deficient mice
The impact of PAR4 deletion on canonical NLRP3 inflammasome activation was assessed in WT and PAR4−/− littermates all fed the HFD for 8 weeks (n = 6 each). Nlrp3 and Pycard mRNA expressions were not significantly different in LV lysates of PAR4−/− compared to WT mice (Suppl. Fig. 2). By contrast, caspase-1 auto-cleavage, determined as the ratio of cleaved (p20) to uncleaved caspase-1 (p45), was nearly halved in LV from PAR4-deficient mice compared to HFD-fed WT controls. Accordingly, processing of pro-IL-1β and full-length GSDMD, to cleaved IL-1β and GSDMD-Nt, respectively, was also strongly attenuated in mice lacking PAR4 (Fig. 7). To assess if adaptive regulation of other PAR subtypes possibly contributes in the PAR4−/− mice, the gene expressions of PAR1 (F2r) and PAR2 (F2rl1) were determined in WT and PAR4-deficient littermates at baseline (prior to treatment with the HFD), and after 8 weeks of treatment. A modest but non-significant trend to lower F2r and F2rl1 mRNA expression in LV lysates of the knockout mice compared to WT mice was seen at baseline (n = 4), while after 8 weeks of HFD, gene expression of both receptor subtypes was comparable between the groups (Suppl. Fig. S3).
Fig. 7.
PAR4-deficiency blunts caspase-1 activation in LV of HFD-fed mice. a Ratios of cleaved (active) caspase-1 (p20) to procaspase-1 (p45), b mature IL-1β to pro-IL-β, and c pore-forming N-terminal (Nt) to full-length (Fl) GSDMD in LV lysates of WT and PAR4−/− mice fed an HFD for 8 weeks (n = 6 each). Protein expression is normalized to γ-tubulin. Data show mean ± SD, relative to WT. *P < 0.05 vs. WT
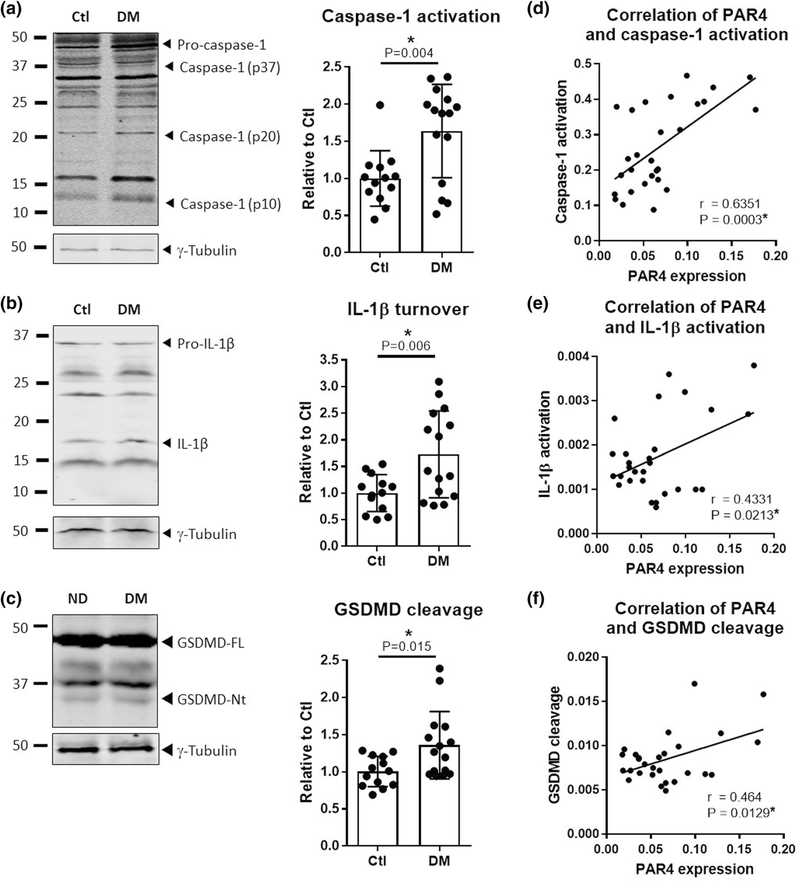
Increased caspase-1 activation in atria of patients with type 2 diabetes
To translate the observations made in murine hearts to the human setting, right atrial appendages from patients with type 2 diabetes mellitus (DM, n = 15) were compared with tissues from non-diabetic Ctl (n = 13) patients for expression levels of PAR and indices of caspase-1 activation. PAR1 and PAR2 expression levels were similar in atrial lysates from DM and Ctl patients, whereas PAR4 was significantly more abundant in the diabetic group (Fig. 8). Activation of caspase-1, determined as the ratio of cleaved (p20) to uncleaved (p45) caspase-1, was significantly higher in the diabetic group (Fig. 9a). Accordingly, cleavage of the caspase-1 targets IL-1β and GSDMD was also augmented, as demonstrated by increased ratios of processed IL-1β and GSDMD to their respective precursors (Fig. 9b, c). Atrial expression level of PAR4 correlated positively with cleavage of caspase-1, IL-1β and GSDMD (Fig. 9d–f, n = 28). Plasma levels of C-reactive protein (CRP) and leukocyte counts determined prior to surgery and tissue sampling were comparable between the two groups of patients (Suppl. Fig. S4), making a contribution of systemic inflammation unlikely.
Fig. 8.
Type 2 diabetes increases PAR4 expression in human atrial tissue. a PAR1, b PAR2 and c PAR4 protein expression, normalized to γ-tubulin, in lysates of right atrial appendages from non-diabetic control patients (Ctl, n = 13) and patients with type 2 diabetes mellitus (DM, n = 15). Data show mean ± SD, relative to Ctl. *P < 0.05 vs. Ctl
Fig. 9.
Type 2 diabetes increases caspase-1 activation in human atrial tissue. a Ratios of active caspase-1 (p20) to pro-caspase-1 (p45), b mature IL-1β to pro-IL-β, and c pore-forming N-terminal (Nt) to full-length (Fl) GSDMD, in lysates of right atrial appendages from non-diabetic control patients (Ctl, n = 13) and patients with type 2 diabetes mellitus (DM, n = 15). Data show mean ± SD, relative to Ctl. *P < 0.05 vs. Ctl. d Correlation between abundance of PAR4/γ-tubulin and ratio of caspase-1/pro-caspase-1, e ratio of IL-1β/pro-IL-1β and f ratio of GDSMD-Nt/full-length GSDMD, in human right atrial appendages (n = 28). r = Pearson’s coefficient of correlation (95% confidence interval)
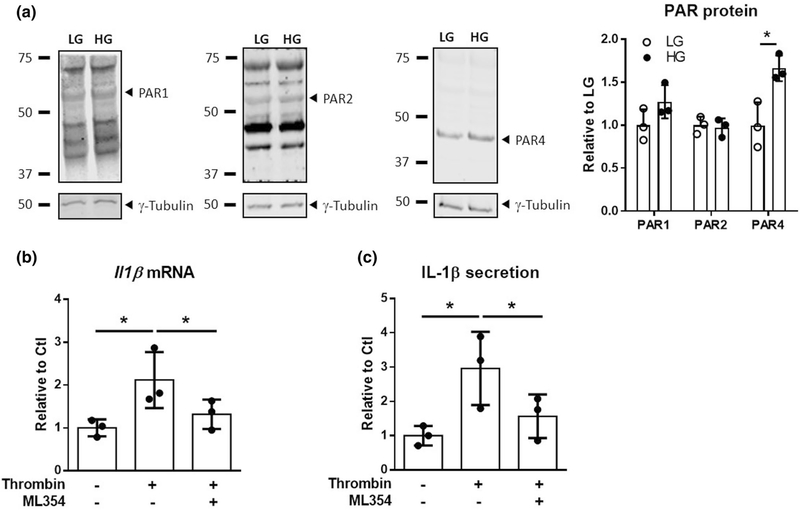
PAR4 mediates thrombin-stimulated IL-1β secretion from human ventricular fibroblasts
Finally, we aimed to establish a functional link between PAR4 and caspase-1-mediated IL-1β maturation and GSDMD-pore formation at the cellular level. Selective PAR4 induction is seen in cardiac fibroblasts obtained from diabetic mice, and in isolated mouse cardiac fibroblasts maintained under high glucose (HG) conditions in culture [26], but human cardiac cells have not been examined in this regard. We therefore cultured primary human ventricular fibroblasts in HG vs. LG medium for up to three passages. The HG environment significantly augmented constitutive expression of PAR4, but not of PAR1 or PAR2 (Fig. 10a; all n = 3), validating our observations in cardiac tissue of diabetic mice and patients. Thrombin significantly increased Il1b mRNA expression and IL-1β secretion in HG fibroblast cultures, and both effects were prevented by the PAR4 antagonist ML354 (n = 3, Fig. 10b, c). Neither thrombin nor ML354 elicited significant effects in LG fibroblast cultures (n = 3, data not shown).
Fig. 10.
PAR4 mediates thrombin-stimulated IL-1β secretion from human cardiac fibroblasts. a PAR1, PAR2 and PAR4 protein expression, normalized to γ-tubulin, in whole cell lysates of human ventricular fibroblasts maintained under low glucose (LG, 5.5 mmol/L) or high glucose (HG, 25 mmol/L) conditions (n = 3 individual experiments). b Il1b mRNA expression and c IL-1β secretion determined in HG-fibroblast cultures stimulated with thrombin (Thr, 3 U/mL) ± ML354 (PAR4 inhibitor, 200 nmol/L) for 24 h (n = 3 individual experiments). Data show mean ± SD, relative to control (Ctl). *P < 0.05 vs. corresponding LG, Ctl or Thr
Discussion
Our major new finding is that the PAR4 thrombin receptor provides a functional link between the hypercoagulant state and cardiac inflammatory signaling associated with obesity and diabetes.
Our previous work showed that glucose-driven, PAR4-mediated inflammatory signaling in human vascular smooth muscle cells largely involves induction of TNFα [9, 37]. This does not appear to be operative in LV of HFD-fed mice, since no significant upregulation of TNFα was found. Instead, the HFD appears to drive sterile inflammatory signaling through activation of caspase-1 and the production IL-1β. The contribution of caspase-1 to diabetes-driven cardiac remodeling and dysfunction was first reported over a decade ago [57]. The NLRP3 inflammasome has since been identified as the upstream activating platform of caspase-1, with a major role in the detrimental cardiac consequences of metabolic disease, and is intensely pursued as a therapeutic target in this context [30, 32, 33, 56, 64]. In LV from mice with mild adiposity and diabetes induced by 8 weeks of high-fat feeding, we detected no significant difference in the transcriptional priming of the inflammasome components NLRP3 or ASC. The increased abundance of both pro-caspase-1 and pro-IL-1β, however, indicates that some degree of priming does occur, while the augmented levels of active caspase-1 and mature IL-1β in the HFD group reflect triggering of NLRP3 inflammasome assembly and activation. A further consequence of caspase-1 activation is the cleavage of GSDMD to generate the pore-forming protein GSDMD-Nt, a prerequisite for cytokine secretion and autocrine/paracrine transmission of the inflammatory signal [20]. In keeping with the increased activation of caspase-1 in LV from HFD-fed mice, the turnover of the full-length precursor to GSDMD-Nt was also enhanced. We attribute the enhanced cleavage of pro-caspase-1, pro-IL-1β and GSDMD in the HFD group largely to the canonical pathway of NLRP3 inflammasome activation, since caspase-11 was not augmented but in fact reduced in LV from HFD vs. chow mice.
According to our working hypothesis, NLRP3 inflammasome activation in the heart is driven by PAR4, a low-affinity thrombin receptor normally expressed in very low levels in cells other than platelets, but showing a dynamic upregulation under conditions of inflammatory stress including diabetes [9, 14, 26, 37]. In the present study, mice that received the HFD for 8 weeks showed increased LV abundance of PAR4 transcript and total protein, compared to chow-fed controls, while other PAR subtypes were not regulated. Thus, PAR4 associates with indices of NLRP3 inflammasome priming and triggering in murine LV. This reflects findings from a recent study in a type 2 diabetic rat model, where treatment with a thrombin inhibitor led to concurrent reductions in inflammatory markers (NFKB phosphorylation, cyclooxygenase II induction) and PAR4 expression [3]. To prove the causal involvement of PAR4 in the canonical activation of caspase-1, IL-1β and GSDMD, these parameters were assessed in LV from WT and PAR4-deficient littermates all fed the HFD for 8 weeks. Consistent with our notion, genetic deletion of PAR4 reduced caspase-1 cleavage, IL-1β maturation and GSDMD-Nt formation. Transcriptional priming of Nlrp3 or Pycard was not influenced. The modestly reduced transcriptional expression of PAR1 and PAR2 in LV of PAR4-deficient mice compared to WT mice is unlikely to contribute significantly to this effect on caspase-1 and its downstream targets, since the reduction in PAR1 and PAR2 was not significant and observed only at baseline, and was no longer evident after 8 weeks of HFD. Our new findings extend our earlier observation that PAR4 deletion protects streptozotocin-diabetic mice from an excessive vascular remodeling and inflammatory response to injury [37], and support our concept of PAR4 as an inducible switch for diabetes-associated thromboinflammation [14].
We next sought to translate these mouse findings to the human heart. Although the NLRP3 inflammasome is a topic of intense cardiovascular research (for recent reviews see [8, 38]), surprisingly few studies have examined the NLRP3 signaling pathway in the human heart [62]. To our knowledge, this is the first study to directly link NLRP3 inflammasome signaling to cardiac-specific consequences of clinical diabetes. Right atrial appendages obtained from patients with type 2 diabetes showed increased cleavage of capase-1, IL-1β and GSDMD compared to atrial tissues from Ctl patients, validating the increased capacity for cardiac NLRP3 inflammasome activation, cytokine production and release that we observed in the HFD-fed mice. Mirroring what we noted in the HFD-fed mouse model, expression of PAR4 was significantly higher in atrial tissues from DM vs. Ctl patients, while expression of PAR1 and PAR2 was similar in both groups. Importantly, the differences in atrial markers of NLRP3 inflammasome activation, cytokine maturation and pore-forming GSDMD are not the consequence of a general systemic inflammatory burden in the diabetic group, since plasma CRP and blood leukocyte counts measured immediately prior to atrial tissue sampling were in the normal range and comparable between patients with and without diabetes.
A significant positive correlation was found between the abundance of PAR4 and the activation of caspase-1, IL-1β and GSDMD in human atria. We therefore proved the direct causal interaction between PAR4 and the NLRP3 inflammasome at the cellular level. Earlier studies have suggested a functional link between thrombin and the NLRP3 inflammasome in platelets and microglia [44, 63], and since PAR4 couples to Gq-signaling and the activation of NFkB in response to thrombin [9, 14], a direct thrombin/PAR4/NLRP3 inflammasome axis is conceivable. Components of the NLRP3 inflammasome and PAR subtypes including PAR4 are expressed in immune cells such as monocytes, macrophages and neutrophils [18, 21, 25, 34], and in cardiomyocytes and cardiac fibroblasts, at least in the mouse [26, 46, 55]. In this study, expression of the immune cell markers CD11b, CD45 and neutrophil elastase did not differ between LV lysates from HFD vs. chow mice, or between atrial tissues from diabetic vs. Ctl patients (data not shown). We therefore speculate that PAR4-associated caspase-1 activation occurs at least in part in cardiomyocytes and/or fibroblasts. Given our recent study highlighting the role of PAR4 in diabetic mouse cardiac fibroblasts [26], we here chose human ventricular fibroblasts as a model system to establish a functional link between PAR4 and the NLRP3 inflammasome. PAR4 was detectable in human ventricular fibroblasts and was strongly upregulated under conditions simulating hyperglycemia, unlike PAR1 and PAR2. Thrombin-stimulated Il1b mRNA expression and secretion of IL-1β, the latter serving as an index of both caspase-1-mediated cytokine processing and pore-forming GSDMD-Nt formation, were enhanced in the HG cultures, and this augmented responsiveness was attenuated by the PAR4 blocker ML354. Although a modestly upregulated PAR1 may also contribute, this receptor has been associated particularly with pro-fibrotic signaling in cardiac fibroblasts [1, 50, 52]. Taken together, we provide the first evidence that PAR4 contributes to thrombin-driven production and release of IL-1β in human cardiac fibroblasts under hyperglycemic conditions.
Our study has limitations. For instance, the influence of species differences in the relative distribution of PAR subtypes cannot be excluded. While human platelets express PAR1 and PAR4, murine platelets by contrast express PAR4 and PAR3 [16], and our present model of global PAR4 deletion does not allow us to specify the contribution of platelet PAR4 vs. PAR4 expressed by cardiac cells such as fibroblasts. Assessment of the platelet marker glycoprotein VI in murine LV lysates, however, showed comparably low, barely detectable, expression in all groups (data not shown), so the observed effects are likely to arise primarily from the lack of PAR4 in the heart, rather than on platelets. A further limitation of our study is the use of human atrial tissue to extrapolate our findings from murine LV to the diseased human heart, in the absence of available ventricular myocardial specimen. Ventricular and atrial remodeling differ quantitatively and qualitatively in many aspects [23], so the atrial appendage will not reflect all relevant mechanisms involved in diabetic cardiomyopathy which affects mainly the ventricular myocardium. However, the activation of the NLRP3 inflammasome appears to be one pathway that is common to remodeling of both atrial and ventricular myocardium [8, 33].
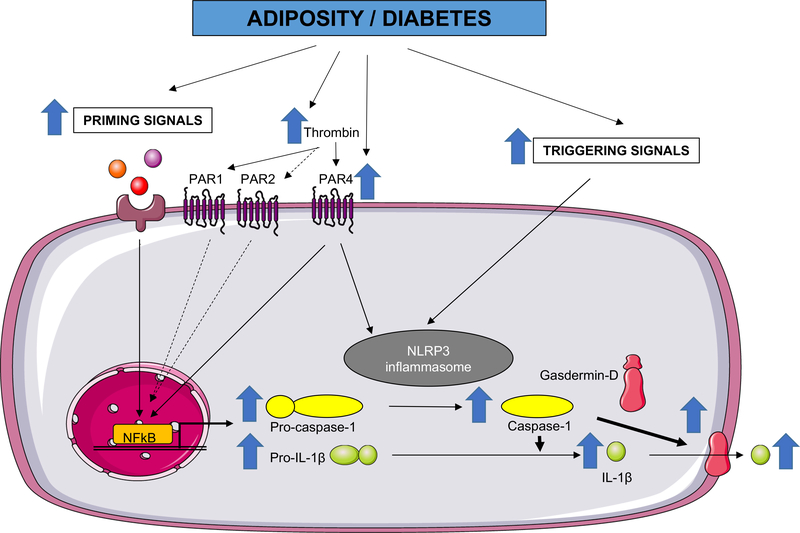
Our findings establish PAR4 thrombin receptors as relevant drivers of canonical NLRP3 inflammasome-dependent cytokine production and release in the diabetic heart, with cardiac fibroblasts likely to contribute substantially to PAR4-mediated sterile inflammatory signaling. A simplified schematic of our working model is provided in Fig. 11. How thrombin-derived peptides such as TP508, which signal independently of PAR, fit into this context is not known but warrants further study, given their prominent wound-healing effects in the settings of diabetes and ischemia [6, 15, 53]. We provide a mechanistic explanation for the chronic low-grade thromboinflammation that accompanies clinical and experimental metabolic disease [2, 4, 5, 7, 17, 27–29, 43, 45, 54], and for the protective effects of thrombin inhibition in experimental diabetic cardiomyopathy [3, 4]. The strong bleeding side effects of the direct thrombin inhibitors will limit their use to patients with a clear indication for anticoagulation, but the emerging PAR4-selective antagonists [59, 60] may provide a feasible alternative approach to blunt aberrant inflammatory signaling in the hearts of patients with diabetes and obesity.
Fig. 11.
Working model of PAR4-mediated cardiac inflammation. Metabolic disorders such as visceral adiposity and diabetes augment signals in the heart that (1) support NFkB-dependent transcriptional priming of pro-caspase-1 and pro-IL-1β, and (2) trigger NLRP3 inflammasome assembly and caspase-1 activation, leading to IL-1β maturation and secretion through the gasdermin D pore. A hypercoaguable state with increased thrombin generation together with upregulated PAR4 in diabetes contribute to caspase-1-dependent inflammatory signaling in the heart, originating at least in part in cardiac fibroblasts. PAR1 and PAR2, which are also activated by thrombin (PAR2 at supraphysiological levels only [36]) but which are not upregulated in the diabetic heart, might also contribute
Supplementary Material
Acknowledgements
We thank Bettina Mausa, Barbara Langer and Monika Hagedorn for excellent technical assistance. Financial support was provided by the Ernst und Berta Grimmke-Stiftung Düsseldorf (to ACF), an intramural grant from the medical faculty of the Heinrich-Heine-University Düsseldorf (to ACF) and by grants from the National Institutes of Health (R01-HL131517 and RO1-HL089598 to DD, R01-HL136389 to NL and DD) and the German Research Foundation (DFG, Do 769/4-1 to DD).
Footnotes
Compliance with ethical standards
Conflict of interest D. Dobrev is a member of the scientific advisory board of OMEICOS Therapeutics GmbH, a company developing small molecules mimicking the effects of omega-3 fatty acids, and of Acesion Pharma, a company developing selective blockers of small-conductance calcium-dependent potassium channels.
Ethical approval All human and animal studies were approved by the institutional ethics committees and were performed in accordance with the ethical standards laid down by the Declaration of Helsinki.
Informed consent All patients gave written informed consent prior to inclusion in the study.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s00395-019-0771-9) contains supplementary material, which is available to authorized users.
References
- 1.Altieri P, Bertolotto M, Fabbi P, Sportelli E, Balbi M, Santini F, Brunelli C, Canepa M, Montecucco F, Ameri P (2018) Thrombin induces protease-activated receptor 1 signaling and activation of human atrial fibroblasts and dabigatran prevents these effects. Int J Cardiol 271:219–227. 10.1016/j.ijcard.2018.05.033 [DOI] [PubMed] [Google Scholar]
- 2.Beijers HJ, Ferreira I, Spronk HM, Bravenboer B, Dekker JM, Nijpels G, ten Cate H, Stehouwer CD (2012) Impaired glucose metabolism and type 2 diabetes are associated with hypercoagulability: potential role of central adiposity and low-grade inflammation—the Hoorn Study. Thromb Res 129:557–562. 10.1016/j.thromres.2011.07.033 [DOI] [PubMed] [Google Scholar]
- 3.Bulani Y, Sharma SS (2017) Argatroban attenuates diabetic cardiomyopathy in rats by reducing fibrosis, inflammation, apoptosis, and protease-activated receptor expression. Cardiovasc Drugs Ther 31:255–267. 10.1007/s10557-017-6732-3 [DOI] [PubMed] [Google Scholar]
- 4.Bulani Y, Srinivasan K, Sharma SS (2019) Attenuation of type-1 diabetes-induced cardiovascular dysfunctions by direct thrombin inhibitor in rats: a mechanistic study. Mol Cell Biochem 451:69–78. 10.1007/s11010-018-3394-9 [DOI] [PubMed] [Google Scholar]
- 5.Campello E, Zabeo E, Radu CM, Spiezia L, Gavasso S, Fadin M, Woodhams B, Vettor R, Simioni P (2015) Hypercoagulability in overweight and obese subjects who are asymptomatic for thrombotic events. Thromb Haemost 113:85–96. 10.1160/th14-02-0156 [DOI] [PubMed] [Google Scholar]
- 6.Carney DH, Olszewska-Pazdrak B (2008) Could rusalatide acetate be the future drug of choice for diabetic foot ulcers and fracture repair? Expert Opin Pharmacother 9:2717–2726. 10.1517/14656566.9.15.2717 [DOI] [PubMed] [Google Scholar]
- 7.Chaudhary R, Bliden KP, Tantry US, Mohammed N, Mathew D, Gesheff MG, Franzese CJ, Gurbel PA (2016) Association of weight gain with coronary artery disease, inflammation and thrombogenicity. J Thromb Thrombolysis 41:394–403. 10.1007/s11239-015-1327-y [DOI] [PubMed] [Google Scholar]
- 8.Chen G, Chelu MG, Dobrev D, Li N (2018) Cardiomyocyte inflammasome signaling in cardiomyopathies and atrial fibrillation: mechanisms and potential therapeutic implications. Front Physiol 9:1115 10.3389/fphys.2018.01115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dangwal S, Rauch BH, Gensch T, Dai L, Bretschneider E, Vogelaar CF, Schror K, Rosenkranz AC (2011) High glucose enhances thrombin responses via protease-activated receptor-4 in human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 31:624–633. 10.1161/atvbaha.110.219105 [DOI] [PubMed] [Google Scholar]
- 10.de Ridder GG, Lundblad RL, Pizzo SV (2016) Actions of thrombin in the interstitium. J Thromb Haemost 14:40–47. 10.1111/jth.13191 [DOI] [PubMed] [Google Scholar]
- 11.Domingueti CP, Dusse LM, Carvalho M, de Sousa LP, Gomes KB, Fernandes AP (2016) Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complicat 30:738–745. 10.1016/j.jdiacomp.2015.12.018 [DOI] [PubMed] [Google Scholar]
- 12.Drake TA, Morrissey JH, Edgington TS (1989) Selective cellular expression of tissue factor in human tissues. Implications for disorders of hemostasis and thrombosis. Am J Pathol 134:1087–1097 [PMC free article] [PubMed] [Google Scholar]
- 13.Faria A, Persaud SJ (2017) Cardiac oxidative stress in diabetes: mechanisms and therapeutic potential. Pharmacol Ther 172:50–62. 10.1016/j.pharmthera.2016.11.013 [DOI] [PubMed] [Google Scholar]
- 14.Fender AC, Rauch BH, Geisler T, Schror K (2017) Protease-activated receptor par-4: an inducible switch between thrombosis and vascular inflammation? Thromb Haemost 117:2013–2025. 10.1160/th17-03-0219 [DOI] [PubMed] [Google Scholar]
- 15.Fossum TW, Olszewska-Pazdrak B, Mertens MM, Makarski LA, Miller MW, Hein TW, Kuo L, Clubb F, Fuller GM, Carney DH (2008) Tp508 (chrysalin) reverses endothelial dysfunction and increases perfusion and myocardial function in hearts with chronic ischemia. J Cardiovasc Pharmacol Ther 13:214–225. 10.1177/1074248408321468 [DOI] [PubMed] [Google Scholar]
- 16.French SL, Paramitha AC, Moon MJ, Dickins RA, Hamilton JR (2016) Humanizing the protease-activated receptor (par) expression profile in mouse platelets by knocking par1 into the par3 locus reveals par1 expression is not tolerated in mouse platelets. PLoS ONE 11:e0165565 10.1371/journal.pone.0165565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giordano P, Del Vecchio GC, Cecinati V, Delvecchio M, Altomare M, De Palma F, De Mattia D, Cavallo L, Faienza MF (2011) Metabolic, inflammatory, endothelial and haemostatic markers in a group of italian obese children and adolescents. Eur J Pediatr 170:845–850. 10.1007/s00431-010-1356-7 [DOI] [PubMed] [Google Scholar]
- 18.Gomides LF, Lima OC, Matos NA, Freitas KM, Francischi JN, Tavares JC, Klein A (2014) Blockade of proteinase-activated receptor 4 inhibits neutrophil recruitment in experimental inflammation in mice. Inflamm Res 63:935–941. 10.1007/s00011-014-0767-8 [DOI] [PubMed] [Google Scholar]
- 19.Gorski DJ, Petz A, Reichert C, Twarock S, Grandoch M, Fischer JW (2019) Cardiac fibroblast activation and hyaluronan synthesis in response to hyperglycemia and diet-induced insulin resistance. Sci Rep 9:1827 10.1038/s41598-018-36140-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Groslambert M, Py BF (2018) Spotlight on the nlrp3 inflammasome pathway. J Inflamm Res 11:359–374. 10.2147/jir.S141220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guarda G, Zenger M, Yazdi AS, Schroder K, Ferrero I, Menu P, Tardivel A, Mattmann C, Tschopp J (2011) Differential expression of nlrp3 among hematopoietic cells. J Immunol 186:2529–2534. 10.4049/jimmunol.1002720 [DOI] [PubMed] [Google Scholar]
- 22.Han X, Nieman MT (2018) Par4 (protease-activated receptor 4): particularly important 4 antiplatelet therapy. Arterioscler Thromb Vasc Biol 38:287–289. 10.1161/atvbaha.117.310550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hanna N, Cardin S, Leung TK, Nattel S (2004) Differences in atrial versus ventricular remodeling in dogs with ventricular tachypacing-induced congestive heart failure. Cardiovasc Res 63:236–244. 10.1016/j.cardiores.2004.03.026 [DOI] [PubMed] [Google Scholar]
- 24.Ito K, Date T, Ikegami M, Hongo K, Fujisaki M, Katoh D, Yoshino T, Anzawa R, Nagoshi T, Yamashita S, Inada K, Matsuo S, Yamane T, Yoshimura M (2013) An immunohistochemical analysis of tissue thrombin expression in the human atria. PLoS ONE 8:e65817 10.1371/journal.pone.0065817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jesmin S, Gando S, Zaedi S, Sakuraya F (2007) Differential expression, time course and distribution of four pars in rats with endotoxin-induced acute lung injury. Inflammation 30:14–27. 10.1007/s10753-006-9017-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kleeschulte S, Jerrentrup J, Gorski D, Schmitt J, Fender AC (2018) Evidence for functional par-4 thrombin receptor expression in cardiac fibroblasts and its regulation by high glucose: par-4 in cardiac fibroblasts. Int J Cardiol 252:163–166. 10.1016/j.ijcard.2017.10.019 [DOI] [PubMed] [Google Scholar]
- 27.Kopec AK, Abrahams SR, Thornton S, Palumbo JS, Mullins ES, Divanovic S, Weiler H, Owens AP 3rd, Mackman N, Goss A, van Ryn J, Luyendyk JP, Flick MJ (2017) Thrombin promotes diet-induced obesity through fibrin-driven inflammation. J Clin Investig 127:3152–3166. 10.1172/jci92744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kopec AK, Joshi N, Towery KL, Kassel KM, Sullivan BP, Flick MJ, Luyendyk JP (2014) Thrombin inhibition with dabigatran protects against high-fat diet-induced fatty liver disease in mice. J Pharmacol Exp Ther 351:288–297. 10.1124/jpet.114.218545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lagrange J, Didelot M, Mohamadi A, Walton LA, Bloemen S, de Laat B, Louis H, Thornton SN, Derby B, Sherratt MJ, Feve B, Challande P, Akhtar R, Cruickshank JK, Lacolley P, Regnault V (2017) Implication of free fatty acids in thrombin generation and fibrinolysis in vascular inflammation in zucker rats and evolution with aging. Front Physiol 8:949 10.3389/fphys.2017.00949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X, Ke X, Li Z, Li B (2019) Vaspin prevents myocardial injury in rats model of diabetic cardiomyopathy by enhancing autophagy and inhibiting inflammation. Biochem Biophys Res Commun 514:1–8. 10.1016/j.bbrc.2019.04.110 [DOI] [PubMed] [Google Scholar]
- 31.Liu J, Nishida M, Inui H, Chang J, Zhu Y, Kanno K, Matsuda H, Sairyo M, Okada T, Nakaoka H, Ohama T, Masuda D, Koseki M, Yamashita S, Sakata Y (2019) Rivaroxaban suppresses the progression of ischemic cardiomyopathy in a murine model of diet-induced myocardial infarction. J Atheroscler Thromb 26:915–930. 10.5551/jat.48405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luo B, Li B, Wang W, Liu X, Liu X, Xia Y, Zhang C, Zhang Y, Zhang M, An F (2014) Rosuvastatin alleviates diabetic cardiomyopathy by inhibiting nlrp3 inflammasome and mapk pathways in a type 2 diabetes rat model. Cardiovasc Drugs Ther 28:33–43. 10.1007/s10557-013-6498-1 [DOI] [PubMed] [Google Scholar]
- 33.Luo B, Li B, Wang W, Liu X, Xia Y, Zhang C, Zhang M, Zhang Y, An F (2014) Nlrp3 gene silencing ameliorates diabetic cardiomyopathy in a type 2 diabetes rat model. PLoS ONE 9:e104771 10.1371/journal.pone.0104771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahajan-Thakur S, Sostmann BD, Fender AC, Behrendt D, Felix SB, Schror K, Rauch BH (2014) Sphingosine-1-phosphate induces thrombin receptor par-4 expression to enhance cell migration and cox-2 formation in human monocytes. J Leukoc Biol 96:611–618. 10.1189/jlb.3AB1013-567R [DOI] [PubMed] [Google Scholar]
- 35.McBane RD 2nd, Miller RS, Hassinger NL, Chesebro JH, Nemerson Y, Owen WG (1997) Tissue prothrombin. Universal distribution in smooth muscle. Arterioscler Thromb Vasc Biol 17:2430–2436. 10.1161/01.atv.17.11.2430 [DOI] [PubMed] [Google Scholar]
- 36.Mihara K, Ramachandran R, Saifeddine M, Hansen KK, Renaux B, Polley D, Gibson S, Vanderboor C, Hollenberg MD (2016) Thrombin-mediated direct activation of proteinase-activated receptor-2: another target for thrombin signaling. Mol Pharmacol 89:606–614. 10.1124/mol.115.102723 [DOI] [PubMed] [Google Scholar]
- 37.Pavic G, Grandoch M, Dangwal S, Jobi K, Rauch BH, Doller A, Oberhuber A, Akhyari P, Schror K, Fischer JW, Fender AC (2014) Thrombin receptor protease-activated receptor 4 is a key regulator of exaggerated intimal thickening in diabetes mellitus. Circulation 130:1700–1711. 10.1161/circulationaha.113.007590 [DOI] [PubMed] [Google Scholar]
- 38.Pavillard LE, Marin-Aguilar F, Bullon P, Cordero MD (2018) Cardiovascular diseases, nlrp3 inflammasome, and western dietary patterns. Pharmacol Res 131:44–50. 10.1016/j.phrs.2018.03.018 [DOI] [PubMed] [Google Scholar]
- 39.Pawlinski R, Fernandes A, Kehrle B, Pedersen B, Parry G, Erlich J, Pyo R, Gutstein D, Zhang J, Castellino F, Melis E, Carmeliet P, Baretton G, Luther T, Taubman M, Rosen E, Mackman N (2002) Tissue factor deficiency causes cardiac fibrosis and left ventricular dysfunction. Proc Natl Acad Sci USA 99:15333–15338. 10.1073/pnas.242501899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pawlinski R, Tencati M, Hampton CR, Shishido T, Bullard TA, Casey LM, Andrade-Gordon P, Kotzsch M, Spring D, Luther T, Abe J, Pohlman TH, Verrier ED, Blaxall BC, Mackman N (2007) Protease-activated receptor-1 contributes to cardiac remodeling and hypertrophy. Circulation 116:2298–2306. 10.1161/circulationaha.107.692764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pei Z, Deng Q, Babcock SA, He EY, Ren J, Zhang Y (2018) Inhibition of advanced glycation endproduct (age) rescues against streptozotocin-induced diabetic cardiomyopathy: role of autophagy and er stress. Toxicol Lett 284:10–20. 10.1016/j.toxlet.2017.11.018 [DOI] [PubMed] [Google Scholar]
- 42.Pretorius L, Thomson GJA, Adams RCM, Nell TA, Laubscher WA, Pretorius E (2018) Platelet activity and hypercoagulation in type 2 diabetes. Cardiovasc Diabetol 17:141 10.1186/s12933-018-0783-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pruller F, Raggam RB, Posch V, Almer G, Truschnig-Wilders M, Horejsi R, Moller R, Weghuber D, Ille R, Schnedl W, Mangge H (2012) Trunk weighted obesity, cholesterol levels and low grade inflammation are main determinants for enhanced thrombin generation. Atherosclerosis 220:215–218. 10.1016/j.atherosclerosis.2011.09.035 [DOI] [PubMed] [Google Scholar]
- 44.Qiao J, Wu X, Luo Q, Wei G, Xu M, Wu Y, Liu Y, Li X, Zi J, Ju W, Fu L, Chen C, Wu Q, Zhu S, Qi K, Li D, Li Z, Andrews RK, Zeng L, Gardiner EE, Xu K (2018) Nlrp3 regulates platelet integrin alphaiibbeta3 outside-in signaling, hemostasis and arterial thrombosis. Haematologica 103:1568–1576. 10.3324/haematol.2018.191700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Romano M, Guagnano MT, Pacini G, Vigneri S, Falco A, Marinopiccoli M, Manigrasso MR, Basili S, Davi G (2003) Association of inflammation markers with impaired insulin sensitivity and coagulative activation in obese healthy women. J Clin Endocrinol Metab 88:5321–5326. 10.1210/jc.2003030508 [DOI] [PubMed] [Google Scholar]
- 46.Sabri A, Alcott SG, Elouardighi H, Pak E, Derian C, Andrade-Gordon P, Kinnally K, Steinberg SF (2003) Neutrophil cathepsin G promotes detachment-induced cardiomyocyte apoptosis via a protease-activated receptor-independent mechanism. J Biol Chem 278:23944–23954. 10.1074/jbc.M302718200 [DOI] [PubMed] [Google Scholar]
- 47.Sapkota B, Shrestha SK, Poudel S (2013) Association of activated partial thromboplastin time and fibrinogen level in patients with type ii diabetes mellitus. BMC Res Notes 6:485 10.1186/1756-0500-6-485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Scott L Jr, Li N, Dobrev D (2019) Role of inflammatory signaling in atrial fibrillation. Int J Cardiol 287:195–200. 10.1016/j.ijcard.2018.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sharma A, Tate M, Mathew G, Vince JE, Ritchie RH, de Haan JB (2018) Oxidative stress and nlrp3-inflammasome activity as significant drivers of diabetic cardiovascular complications: therapeutic implications. Front Physiol 9:114 10.3389/fphys.2018.00114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Snead AN, Insel PA (2012) Defining the cellular repertoire of gpcrs identifies a profibrotic role for the most highly expressed receptor, protease-activated receptor 1, in cardiac fibroblasts. FASEB J 26:4540–4547. 10.1096/fj.12-213496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Soma P, Swanepoel AC, Bester J, Pretorius E (2017) Tissue factor levels in type 2 diabetes mellitus. Inflamm Res 66:365–368. 10.1007/s00011-017-1030-x [DOI] [PubMed] [Google Scholar]
- 52.Sonin DL, Wakatsuki T, Routhu KV, Harmann LM, Petersen M, Meyer J, Strande JL (2013) Protease-activated receptor 1 inhibition by sch79797 attenuates left ventricular remodeling and profibrotic activities of cardiac fibroblasts. J Cardiovasc Pharmacol Ther 18:460–475. 10.1177/1074248413485434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sower LE, Payne DA, Meyers R, Carney DH (1999) Thrombin peptide, tp508, induces differential gene expression in fibroblasts through a nonproteolytic activation pathway. Exp Cell Res 247:422–431. 10.1006/excr.1998.4372 [DOI] [PubMed] [Google Scholar]
- 54.Stoppa-Vaucher S, Dirlewanger MA, Meier CA, de Moerloose P, Reber G, Roux-Lombard P, Combescure C, Saudan S, Schwitzgebel VM (2012) Inflammatory and prothrombotic states in obese children of European descent. Obesity (Silver Spring) 20:1662–1668. 10.1038/oby.2012.85 [DOI] [PubMed] [Google Scholar]
- 55.Takahashi M (2019) Cell-specific roles of nlrp3 inflammasome in myocardial infarction. J Cardiovasc Pharmacol. 10.1097/fjc.0000000000000709 [DOI] [PubMed] [Google Scholar]
- 56.Wang Y, Li H, Li Y, Zhao Y, Xiong F, Liu Y, Xue H, Yang Z, Ni S, Sahil A, Che H, Wang L (2019) Coriolus versicolor alleviates diabetic cardiomyopathy by inhibiting cardiac fibrosis and nlrp3 inflammasome activation. Phytother Res. 10.1002/ptr.6448 [DOI] [PubMed] [Google Scholar]
- 57.Westermann D, Van Linthout S, Dhayat S, Dhayat N, Escher F, Bucker-Gartner C, Spillmann F, Noutsias M, Riad A, Schultheiss HP, Tschope C (2007) Cardioprotective and anti-inflammatory effects of interleukin converting enzyme inhibition in experimental diabetic cardiomyopathy. Diabetes 56:1834–1841. 10.2337/db06-1662 [DOI] [PubMed] [Google Scholar]
- 58.Wilson AJ, Gill EK, Abudalo RA, Edgar KS, Watson CJ, Grieve DJ (2018) Reactive oxygen species signalling in the diabetic heart: emerging prospect for therapeutic targeting. Heart 104:293–299. 10.1136/heartjnl-2017-311448 [DOI] [PubMed] [Google Scholar]
- 59.Wilson SJ, Ismat FA, Wang Z, Cerra M, Narayan H, Raftis J, Gray TJ, Connell S, Garonzik S, Ma X, Yang J, Newby DE (2018) Par4 (protease-activated receptor 4) antagonism with bms-986120 inhibits human ex vivo thrombus formation. Arterioscler Thromb Vasc Biol 38:448–456. 10.1161/atvbaha.117.310104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wong PC, Seiffert D, Bird JE, Watson CA, Bostwick JS, Giancarli M, Allegretto N, Hua J, Harden D, Guay J, Callejo M, Miller MM, Lawrence RM, Banville J, Guy J, Maxwell BD, Priestley ES, Marinier A, Wexler RR, Bouvier M, Gordon DA, Schumacher WA, Yang J (2017) Blockade of protease-activated receptor-4 (par4) provides robust antithrombotic activity with low bleeding. Sci Transl Med 10.1126/scitranslmed.aaf5294 [DOI] [PubMed] [Google Scholar]
- 61.Yang L, Zhao D, Ren J, Yang J (2015) Endoplasmic reticulum stress and protein quality control in diabetic cardiomyopathy. Biochim Biophys Acta 1852:209–218. 10.1016/j.bbadis.2014.05.006 [DOI] [PubMed] [Google Scholar]
- 62.Yao C, Veleva T, Scott L Jr, Cao S, Li L, Chen G, Jeyabal P, Pan X, Alsina KM, Abu-Taha ID, Ghezelbash S, Reynolds CL, Shen YH, LeMaire SA, Schmitz W, Muller FU, El-Armouche A, Tony Eissa N, Beeton C, Nattel S, Wehrens XHT, Dobrev D, Li N (2018) Enhanced cardiomyocyte nlrp3 inflammasome signaling promotes atrial fibrillation. Circulation 138:2227–2242. 10.1161/circulationaha.118.035202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ye X, Zuo D, Yu L, Zhang L, Tang J, Cui C, Bao L, Zan K, Zhang Z, Yang X, Chen H, Tang H, Zu J, Shi H, Cui G (2017) Ros/txnip pathway contributes to thrombin induced nlrp3 inflammasome activation and cell apoptosis in microglia. Biochem Biophys Res Commun 485:499–505. 10.1016/j.bbrc.2017.02.019 [DOI] [PubMed] [Google Scholar]
- 64.Ye Y, Bajaj M, Yang HC, Perez-Polo JR, Birnbaum Y (2017) Sglt-2 inhibition with dapagliflozin reduces the activation of the nlrp3/asc inflammasome and attenuates the development of diabetic cardiomyopathy in mice with type 2 diabetes. Further augmentation of the effects with saxagliptin, a dpp4 inhibitor. Cardiovasc Drugs Ther 31:119–132. 10.1007/s10557-017-6725-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.