Abstract
Objective
Controlling or prescriptive support styles (e.g., pressure) often hinder weight loss, but can sometimes be beneficial. This secondary analysis of data from a randomized controlled trial examined persuasion, pressure, and indirect social control among cohabitating couples and the effect of these supports on weight loss.
Methods
Couples (NCouples = 130) were randomized to either Weight Watchers (WW) or a self-guided control condition (SG). Only one member of each couple received the intervention, the other member of the couple was untreated. Couples were weighed and completed study measures at baseline, three, and six months.
Results
Dyadic multilevel models examined BMI change and differences across role (treated participant/untreated spouse) and condition (WW/SG). Prescriptive support predicted BMI change for treated participants in the WW condition only. For treated WW participants, there was no significant decrease in BMI when pressure was high (+1SD), B = −.25, p = .22, but a significant decrease when pressure was low (0), B = 1.06, p < .001. Additionally, high levels of indirect social control (+1SD) predicted greater decreases in BMI compared to low (−1SD) indirect social control, B = −.91, p < .001, and, B = −.41, p < .01.
Conclusions
Considering both the type and context of support for weight management is worthwhile. Intervention participants had access to treatment resources that may have engendered more effective responses to spouses’ concerns or a sense of obligation to their spouse (indirect social control), whereas pressures to lose weight—while engaged in treatment—may have undermined behavior-change efforts.
Keywords: weight loss, couples, intervention, prescriptive support, social control
The links between social support and successful weight management have long been recognized (Elfhag, & Rössner, 2005; Kiernan et al., 2012; McLean, Griffin, Toney, & Hardeman, 2003; Wing & Jeffery, 1999). More recently, studies have attempted to understand the complexities of how different types of support might uniquely influence weight loss outcomes (e.g., Gabriele, Walker, & Gill, 2005; Gabriele, Carpenter, Tate, & Fisher, 2011; Gorin, Powers, Koestner, & Wing, 2014. For example, supporting individual autonomy and providing encouragement can be beneficial for weight loss, whereas more prescriptive forms of support, such as directive support or social control, may hinder weight loss efforts (Gabriele et al., 2005; Gorin et al., 2014), suggesting that people realize better outcomes when they are making healthy decisions for themselves rather than when they “don’t want to let others down” (McSpadden et al., 2016). In contrast, some have also found that offering more structured, concrete, and directive support—as opposed to flexible, less directive support—may increase weight loss when offered as part of an intervention (e.g., Gabriele et al., 2011). This raises the possibility that both the context of the weight loss (e.g., a structured intervention vs. self-directed) and the type of support interact to predict weight loss outcomes.
Eating, activity and weight loss are among the most common things that spouses attempt to influence (Lewis & Butterfield, 2007; Tucker & Anders, 2001). Spousal involvement and support can significantly enhance health outcomes such as weight loss (Gorin et al., 2014), but can also prove to be detrimental if spousal or family involvement is undermining in nature (Henry, Rook, Stephens, & Frank, 2013; Wang et al., 2014). Specifically, social control and directive forms of social support can hinder weight loss and related behaviors, including physical activity and healthy eating (Gabriele et al., 2005; Gorin et al., 2014; McSpadden et al., 2016). There are a number of reasons this may occur. For example, internally motivated behavior (i.e., behavior that is not due to felt pressures from a partner, etc.) promotes sustained engagement in behavior change (Deci & Ryan, 2008; Ryan, Patrick, Deci, & Williams, 2008; Teixeira, Carraca, Markland, Silva, & Ryan, 2012; Teixeira, Silva, Mata, Palmeira, & Markland, 2012). By contrast, if an individual is externally motivated, for example being active solely to satisfy his or her partner, he/she may be less likely to maintain this exercise long term. If controlling styles of social support, geared towards pressuring someone to lose weight, engage in physical activity, or make eating changes, are perceived as stigmatizing, this can undermine positive health behaviors, weaken perceptions of social support (Brewis, 2014; Hunger, Major, Blodorn, & Miller, 2015; Wang, Pbert, & Lemon, 2014), and may further erode weight loss efforts. Social directives may be especially stigmatizing if the recipient is not actively trying to lose weight. For example, if an individual is actively engaged in weight management treatment, he/she may understand why a partner attempts to influence him/her to be active, or may even welcome additional reminders and motivation. If the individual is not currently engaged in weight management treatment, the same directives may be experienced as more shaming or stigmatizing. The role of such context in shaping the effects of social control or directive support is not well understood.
Although social control and directive supports are often seen as detrimental, they can be beneficial under some circumstances (e.g., Gabriele et al., 2014; Koestner, Powers, Carbonneau, Milyavskaya, & Chua, 2012). Apparent discrepancies in the effects of more controlling or directive forms of support on weight loss may be a result of the way these supports have been defined. Some types may be coercive and confrontational (e.g., a partner restricting foods in the home or criticizing behavior), whereas others may be a straightforward request (e.g., a partner asking for behavior change), or more insidious (e.g., a sense of guilt or obligation to one’s partner). In a three-part study of goal progress and attainment, Koestner et al. (2012) found that directive support, such as partner reminders or calling attention to unhealthy behaviors and opportunities for goal attainment, was positively related to progress towards attaining health-related goals. Furthermore, Gabriele et al. (2014) found that women achieved greater weight loss and reductions in waist circumference when e-coaching was delivered in a directive support style (providing a structured, non-adaptive intervention and behavioral suggestions), compared to e-coaching delivered in a nondirective style (a more flexible and collaborative approach, providing multiple behavioral/goal options and promoting participant choice). Both of these studies therefore operationalized directive supports in a relatively non-stigmatized, non-pressured way.
Beginning to break down different types of directive support and social control within a single study, Novak and Webster (2011) found that spousal support in the form of eating healthier foods together and restricting access to unhealthy foods could facilitate positive health behaviors, whereas criticism or direct pressure to lose weight had the opposite effect. Social control, or attempts to influence and/or regulate one another’s health behaviors and exert influence on health-behavior change, independent of being perceived as supportive, validating, or reassuring (Lewis & Rook, 1999; Lewis & Butterfield, 2005), can also been defined in multiple ways, and the effects of social control vary depending on study operationalization. Health-related social control, including reinforcement, modeling, and encouragement, has been associated with better adherence to diabetic dietary recommendations and positive emotional reactions, whereas social control using persuasion and warnings has been associated with poorer adherence to dietary recommendations and pretending to make necessary behavior change (Lewis & Rook, 1999; Okun, Huff, August, & Rook, 2007; Stephens et al., 2010; Thorpe, Lewis, & Sterba, 2008).
Studies have yet to examine these nuances prospectively in the context of a weight loss intervention, and none have explicitly considered differences according to the context in which support or control is received. This study attempted to disentangle these effects by taking a nuanced approach to defining different forms of social control and examining the effects across a range of weight loss contexts, examining the effects of three types of support on weight change over time: indirect social control (e.g., a sense of guilt or social responsibility motivating behavior change), persuasion (e.g., trying to convince or persuade in an attempt to effect behavior change), and pressure (e.g., criticism or restrictions to effect behavior change). It was expected that pressure would be the most detrimental to weight loss, indirect social control would be beneficial, and persuasion would fall somewhere in the middle. Differences across intervention condition (i.e., structured treatment vs. a self-guided control group) and role (i.e., structured weight loss participant vs. untreated spouse) were also examined. The inclusion of untreated spouses allows for a unique opportunity to examine four distinct types of weight loss contexts: 1) people who want to lose weight and are receiving treatment, 2) people who want to lose weight and are attempting to do so through self-guidance only (control participants), and spouses who may not want to lose weight—but who often do as a result of an intervention “ripple” effect (Gorin et al., 2008; 2013) —who live with someone either 3) attempting to lose weight alone or 4) enrolled in a structured treatment program. Given the lack of clarity regarding the effects of support in different contexts, this was largely exploratory. However, speculation that pressures to lose weight might be less welcome when an individual is not interested or engaged in weight loss efforts led us to tentatively predict that more controlling forms of supports, such as pressure, would be most harmful for untreated spouses.
Methods
Participants
This is a secondary analysis of data from a randomized controlled trial examining weight loss in untreated spouses of intervention participants (Gorin et al., in press). The goal of the primary outcome study was to track weight change in untreated spouses of intervention participants who were participating in either a structured weight loss program or who were randomized to a self-guided control condition. In brief, results from the primary outcome analysis indicated that untreated spouses lost significant weight, independent of condition (treatment vs. control). Treated participants in both conditions also experienced significant weight loss, and couples tended to have similar weight-loss trajectories over time. In contrast, the present analysis was concerned with how prescriptive supports affected weight change in both treated participants and untreated spouses in both conditions.
A total of 384 couples were screened for eligibility via phone, and 130 enrolled in the study (33.85%; 260 individuals). Couples were recruited through direct mailings and community and online postings. One member of the couple (i.e., the treated participant) had to be willing to participate in a weight loss program, and the other member of the couple (i.e., the untreated spouse) had to be willing to attend assessments only. Inclusion criteria were: 1) 25–70 years old, and 2) a body mass index (BMI) between 27.0–40.0 kg/m2 in treated participants and ≥ 25 kg/m2 in untreated spouses, and 3) couples were cohabitating (may or may not be married; for clarity the untreated partner is referred to as a “spouse” given that “partner” has a double meaning and is often used to describe statistical effects in dyadic models; Kenny, Kashy, & Cook, 2006). Exclusion criteria were: 1) current enrollment in a weight loss program, dieting, or taking medications that might affect weight, 2) participation in a weight loss program in the past year, 3) lost ≥ 5% of their body weight in the past 6 months, 4) planning to or had undergone weight loss surgery, 5) had any orthopedic limitations or contraindications to physical activity, 6) were pregnant, lactating, or less than 6 months postpartum, or were planning to become pregnant in the next year, 7) reported uncontrolled hypertension, history of coronary heart disease, stroke, or peripheral arterial disease, 8) reported chronic gastrointestinal disease, 9) endorsed having hepatitis B or C, cirrhosis, or HIV, 10) had a history of cancer within the past 5 years, or 11) reported a significant psychiatric illness that might interfere with completion of the study. Individuals who had diabetes or other significant medical conditions not listed above were required to obtain written consent from a physician to participate in the study.
Procedure
Couples were randomized to either participate in Weight Watchers (WW, n = 65), a nationally available weight loss program or to a self-guided condition (SG, n = 65). Treated participants assigned to WW received free access to WW, comprised of online tools and in-person meetings, for six months (untreated spouses did not). In the SG condition, treated participants received a four-page handout with basic information regarding healthy eating, exercise, and weight control strategies. SG participants were offered six months of free access to WW at the conclusion of the study.
Treated participants and untreated spouses were weighed at baseline, three, and six months, and reported on receipt of indirect social control, persuasion, and pressure at each visit. Treated participants and untreated spouses were paid $25 for the baseline and three month visits and $50 for the visit at six months. All study procedures were approved by the Institutional Review Board at the University of Connecticut, and couples completed informed consent before participating.
Measures
BMI
Weight and height were used to calculate Body Mass Index (BMI). Weight at each visit was measured using a calibrated standard digital scale (Tanita BWB 800) to the nearest 0.1 kg, and height was measured at each visit using a stadiometer to the nearest cm. Shoes were removed. Height and weight were taken twice, and the means of these readings were used to compute BMI.
Indirect social control
Indirect social control was measured using four items assessing a general obligation to one’s partner to be healthy, such as, “I feel a sense of responsibility to my spouse to try to stay in good health” (Tucker, 2002). Response options ranged from 0, never, to 4, often. At baseline, α = .82; three months, α = .81; six months, α = .84.
Persuasion
Persuasion was measured using three items encompassing weight-related behaviors, including both diet and exercise, such as, “Over the past month, how often did your spouse… try to persuade you to do more to follow your diet or exercise regimen?” (Sorkin et al., 2014). Response options ranged from 0, not at all, to 5, extremely. At baseline, α = .90; three months, α = .87; six months, α = .87.
Pressure
Pressure was measured using four items encompassing weight-related behaviors, including both diet and exercise, such as, “Over the past month, how often did your spouse… criticize your poor food choices or physical inactivity?” (Sorkin et al., 2014). Response options ranged from 0, not at all, to 5, extremely. At baseline, α = .93; three months, α = .92; six months, α = .93.
Data Analysis Strategy
Couple members are more likely to be similar to each other than to other study participants, and individuals are more likely to be similar to themselves over time (Kenny et al., 2006). To account for this interdependence, multilevel models were specified using the MIXED command in SPSS version 20. Multilevel models also allow for flexibility with missing data (i.e., if a participant has missing values at one timepoint, he or she can still be included in the model). BMI was specified as the outcome rather than percent weight loss, given that all participants would start at a value of zero percent weight loss, thereby eliminating all intercept variance (see Cornelius et al., 2016). In this model, absolute BMI is the outcome, and the coefficient for time indicates the predicted change between each assessment. Indirect social control, persuasion, and pressure were included as time-varying covariates. All prescriptive support variables were grand mean centered prior to analysis. High and low values were set at +1SD and −1SD (this was set at 0 for low levels of pressure due to skew in the variable, such that −1SD would have represented a negative and impossible value). Centered, high, and low values were calculated using the pooled means and standard deviations across all three timepoints.
Nested deviance comparison tests were conducted to test the significance of interactions across role, condition, and time. Maximum likelihood (ML) estimation was used for model building, given that these models differed in fixed effects. Final model results are reported using restricted maximum likelihood (REML).
Results
Treated participants had a mean BMI of 33.93 at baseline (SD = 3.68), and untreated spouses had a mean BMI of 32.99 (SD = 5.54). Age was similar for treated participants and untreated spouses (M = 53.40, SD = 10.51, and M = 53.91, SD = 10.49, respectively). Participants and spouses were 96.2% white and reported a median income of $75,000 or greater. Treated participants reported a median education of a bachelor’s degree, and untreated spouses reported a median education of an associate’s degree or technical degree. Most treated participants were female (68.5%) whereas most untreated spouses were male (68.5%). Only two couples dropped out during the study, and all participants provided full data for at least one assessment. Due to the flexibility of multilevel modeling in handling missing data, all participants were represented in the analysis.
A series of nested deviance comparison tests indicated that the effects of time and condition differed across role (treated participant or untreated spouse), Δχ2(3) = 17.77, p < .01, and that the effects of indirect social control, persuasion, and pressure differed across time, condition, and role, Δχ2(21) = 41.28, p < .01. In the final model, there was a significant four-way interaction between time, condition, role, and indirect social control, B = .11, 95% CI [.00, .22], p < .05. The interaction between time, condition, role, and pressure approached significance, B = −.03, 95% CI [−.06, .00], p = .06.
The final model was highly complex. Because of this, simple slopes analyses are reported only for the focal relationships: interactions between indirect social control, persuasion, and pressure and time predicting BMI (see Table 1 for means and standard deviations; correlations are reported in Table 2).
Table 1.
BMI and directive supports at baseline, three, and six months for treated participants and untreated spouses in both conditions (WW and SG). Couples’ scores are compared using paired t-tests at each timepoint
| WW | SG | ||||
|---|---|---|---|---|---|
| Treated Participants | Untreated Spouses | Treated Participants | Untreated Spouses | ||
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Age | 52.31 (10.24) | 52.56 (9.74) | 54.52 (10.81) | 55.32 (11.13) | |
| BMI | Baseline | 34.09 (3.87) | 33.82 (6.17) | 33.72 (3.51) | 32.26 (4.76)* |
| 3 Months | 33.06 (4.09) | 33.05 (6.28) | 32.97 (3.55) | 31.92 (4.91)+ | |
| 6 Months | 32.64 (4.33) | 32.84 (6.53) | 32.68 (3.72) | 31.61 (4.90)+ | |
| Indirect Social Control | Baseline | 2.81 (.81) | 2.86 (.82) | 3.10 (.85) | 3.08 (.71) |
| 3 Months | 2.04 (.77) | 2.26 (.65)+ | 2.23 (.73) | 2.38 (.61) | |
| 6 Months | 2.04 (.86) | 2.24 (.74) | 2.17 (.82) | 2.36 (.70) | |
| Persuasion | Baseline | 4.58 (4.11) | 4.09 (4.22) | 4.97 (4.23) | 4.32 (4.26) |
| 3 Months | 4.92 (2.96) | 5.05 (4.33) | 4.77 (4.17) | 4.89 (4.15) | |
| 6 Months | 3.41 (3.73) | 4.02 (3.63) | 3.86 (3.71) | 4.80 (4.51) | |
| Pressure | Baseline | 3.64 (4.53) | 3.64 (5.01) | 4.34 (5.40) | 3.63 (4.57) |
| 3 Months | 3.45 (4.21) | 3.73 (4.76) | 3.00 (4.06) | 3.49 (4.59) | |
| 6 Months | 2.23 (3.11) | 2.71 (4.05) | 2.23 (3.27) | 3.22 (5.15) | |
p < .10
p < .05
p < .01.
Table 2.
Correlations between indirect social control, persuasion, and pressure for treated participants (above the diagonal) and untreated spouses (below the diagonal) at baseline, three, and six months
| Baseline | 3 Months | 6 Months | |||||||
| ISC | PE | PR | ISC | PE | PR | ISC | PE | PR | |
| Indirect Social Control (ISC) | - | .37** | 39** | - | 44** | 33** | - | 44** | 77** |
| Persuasion (PE) | 29** | - | .72** | - | 78** | 78** | - | 74** | |
| Pressure (PR) | 28** | .76** | - | .26** | .77** | - | .16+ | .78** | - |
p < .10
p < .05
p < .01.
Treated Participants
Indirect social control and pressure were related to BMI change, indicating that weight-loss success varied depending on the level of these supports. This relationship varied by treatment condition: indirect social control, B = −.18, 95% CI [−.34, −.01], p = .04; pressure, B = .06, 95% CI [.01, .10], p = .02. Because the interaction with time and condition was not significant for persuasion (p = .15), we examined the effect of persuasion on BMI change for treated participants pooled across conditions—this effect was nonsignificant, B = −.03 [−.08, .02], p = .29.
Interactions with condition revealed that indirect social control and pressure were related to BMI change in the for treated WW participants only: indirect social control, B = −.29, 95% CI [−.53, −.06], p = .01; pressure, B = .09, 95% CI [.02, .16], p < .01 (indirect social control and pressure were unrelated to BMI change for treated SG participants, B = .06 [−.17, .29], p = .62, and, B = −.02 [−.08, .05], p = .56, respectively).
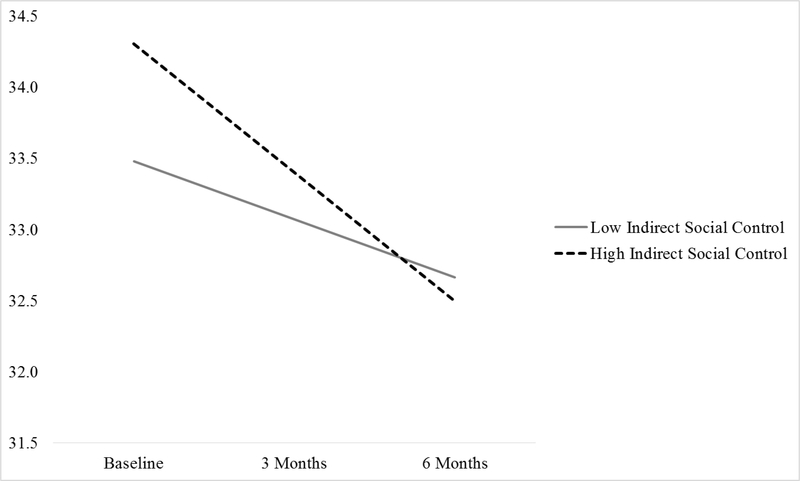
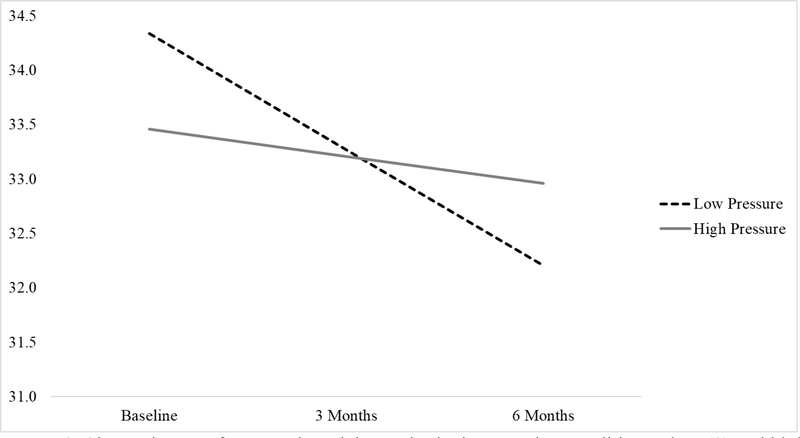
Treated participants in the WW condition had a steeper decrease in BMI over time when indirect social control was high (+1SD), B = −.91, 95% CI [−1.23, −.58], p < .001, than when it was low (−1SD), B = −.41, 95% CI [−.70, −.11], p < .01. Stated otherwise, higher levels of indirect social control benefitted weight loss. Pressure worked in the opposite direction: treated participants in the WW group did not have a significant change in BMI over time when pressure was high (+1SD), B = −.25, 95% CI [−.65, .15], p = .22, but did when pressure was low (set at 0 as −1SD would have been a negative value), B = −.96, 95% CI [−1.28, −.63], p < .001. Stated otherwise, higher levels of pressure were detrimental to weight loss. The interaction for indirect social control is displayed in figure 1, and the interaction for pressure is displayed in figure 2.
Figure 1.
Change in BMI for treated participants in the intervention condition at low (−1SD) and high (+1SD) indirect social control.
Figure 2.
Change in BMI for treated participants in the intervention condition at low (0) and high (+1SD) pressure.
Untreated Spouses
The effects of indirect social control, pressure, and persuasion did not vary by condition in untreated spouses, and were unrelated to BMI change for untreated spouses across both the WW and SG conditions (B = .04 [−.12, .19], p = .65; B = −.03 [−.07, .01], p = .10; and B = .04 [−.00, .09], p = .08, respectively).
Discussion
Social support affects weight management; however, previous studies examining the ways in which more prescriptive supports (i.e., social control and directive support) impact weight loss have demonstrated inconsistent findings (e.g., Gorin et al., 2014; Koestner et al., 2012; Novak & Webster, 2011). This highlights the need for a more deliberate, nuanced approach, and for comparisons between different ways of operationalizing prescriptive supports. In this study, the association of support with weight change over time differed across context and based on the way in which these supports were conceptualized. Specifically, greater indirect social control was associated with greater weight loss, whereas greater pressure was associated with no significant weight loss during the course of the intervention. This pattern was restricted to treated participants in the WW condition, indicating that, for health-behavior change, both the type of control or directive support and the context in which support is provided must be considered.
Indirect social control, or reporting an obligation to one’s spouse to stay healthy, was related to more weight loss over the course of the study among treated participants in the WW condition. It is possible that feelings of obligation reflect care and concern on the part of the spouse, higher quality relationships, and increased positive social support. For example, if an individual senses more indirect social control, this might indicate that one’s spouse is invested in the health of the individual, and is more supportive of the individual’s weight loss efforts. Future studies should explore these possibilities by gathering couples’ reports of types of support that are provided rather than just perceptions of supports that are received, and comparing these measures. That is, if one member of the couple reports experiencing indirect social control, does the other report greater investment in his or her partner’s health?
In contrast to indirect social control, treated participants in the WW condition, reporting greater pressure to lose weight through criticism and direct control, did not achieve significant weight loss. This finding is in line with earlier research demonstrating a detrimental effect of directive support and social control on weight loss and weight-related behaviors (Gorin et al., 2014; Novak & Webster, 2011). Models of influence and social control (e.g., Hughes & Gove, 1981; Lewis & Rook, 1999) have posited that there is a trade-off, or “dual effect,” whereby both positive behavior change and emotional distress are simultaneously elicited by partner attempts at behavioral control and directive support. This could, in part, explain the differential effects of indirect social control and pressure: if indirect social control elicits less emotional distress than pressure, it could be more effective. The idea that pressure to lose weight via criticism or coercion can be stigmatizing and hinder positive behavior change (Brewis, 2014; Hunger et al., 2015; Wang et al., 2014) also supports this possibility. Finally, it is unclear why indirect social control and pressure predicted weight loss, but persuasion did not. Perhaps persuasion is effective only if it leads to a sense of obligation to change, and this was captured by some conceptual overlap with indirect social control.
It was predicted that social control and directive supports would have the greatest effect on individuals in the self-guided condition, due to the fact that less active involvement (e.g., not attending weekly meetings, using an app, etc.) and lack of structure (e.g., prescribed behaviors) from an intervention may lead those in the self-guided condition to interpret such supports as unwarranted or unwelcome. Yet, the effects of indirect social control and pressure on weight loss were restricted to treated participants in the WW treatment condition. Indeed, there were no effects of supports measured in this study on untreated spouses in the self-guided or WW conditions, or on treated participants who were attempting weight loss through a self-guided approach only. This is not a result of a lack of weight change (i.e., it was not that there was no weight loss to predict). Spouses often have similar BMI status (Christakis & Fowler, 2007; Cornelius, Gettens, & Gorin, 2016; Meyler, Stimpson, & Peek, 2007), and, as indicated in the primary outcomes paper, treated participants and untreated spouses in both conditions tended to experience significant weight loss over time (Gorin et al., in press). It may be that WW participants were more reactive to spousal pressures and may have felt that their efforts were not being appreciated, leading to disengagement. WW participants may also have felt better equipped to respond to feelings of obligation or partner concerns given their access to treatment resources, prompting increased weight loss efforts, or may have been more responsive to partner concerns or pressures due to the social components (i.e., group-based aspects) of WW treatment. These possibilities are speculative, and should be explored in future research.
Although study results begin to shed light on the ways in which different types of social control and directive support might shape weight change across contexts, there are a number of limitations. The sample was largely white, middle aged, heterosexual, and upper income. Thus, study results may not generalize to more diverse populations. The majority of treated participants were also female. Due to the complexity of the model and loss of power, 5-way interactions with gender were not included. Including these 5-way interactions (and associated 4-, 3-, and 2-way interactions) could compromise the interpretability and power of the model to detect significant effects, so results may not be trustworthy. It is possible, however, that these relationships may differ across gender. This is a significant limitation, and should be explored in future studies. Similarly, relationship satisfaction may affect the way people interpret or react to prescriptive supports. As this body of work progresses, it will be necessary to explore potential nuances due to differences in relationship quality.
Power may have been limited to detect significant 4-way interactions, given the sample consisted of 130 couples (260 individuals). The original study was powered to detect weight loss within untreated spouses using individual-level analysis, rather than to detect weight change and interactions using data nested both within couples and over time. Therefore, lack of significant effects of prescriptive supports in untreated spouses or SG participants may be due to a lack of power rather than to a true null effect. The assessments of indirect social control, persuasion, and pressure were also limited in that these scales consist of few items and have not undergone rigorous validation procedures. This may have also have masked significant effects of these prescriptive supports on weight loss in other conditions (i.e., untreated spouses, or SG participants); however, these scales were internally consistent and behaved in theoretically plausible ways. Future research is needed to rigorously examine the psychometric properties of these measures. Because provision of support was not assessed in this study, it is also not clear if individual reports of support received match spouse reports of support that is provided. That is, this study cannot determine whether these results are driven by perceived, rather than actual, support. The measures also asked about general health-related social control and diet/exercise simultaneously, so it is not possible to determine which behaviors or mechanisms might be driving these effects. Future studies should gather reports of behavior change over time, and should also consider emotional reactions and experienced stigma resulting from partner directive supports, and ways in which different context might foster collaborative weight loss efforts.
A final consideration is causality. Although we conceptualized support as facilitating (or impeding) weight loss, due to the time-varying nature of the support variables, it is possible that results also reflect the reverse (i.e., BMI change precipitated different types of support). For example, a flat BMI-change trajectory, representing a lack of weight loss, could precipitate greater spousal pressure and coercive forms of support. Future studies might consider alternatives types of analyses, such as lagged analyses, to provide more rigorous evidence for causal inference.
This study suggests that it is critical to differentiate between types of social control and directive support, given the different implications these supports have for weight loss. Feeling obligated to a spouse to maintain health can improve weight loss outcomes, whereas pressures to lose weight can impede weight loss. Further, the context of support matters: individuals actively attempting to lose weight, who are enrolled in a structured weight loss program, may be particularly affected by prescriptive supports in ways that may both help or hinder weight loss. Future research should explore the mechanisms that underlie these effects. If the “when” and “how” is better understood, couple-targeted interventions could incorporate training to increase helpful types of support, while building in buffers against more negative types (e.g., reframing on the part of the person receiving support, or reducing pressures within the relationship).
Acknowledgments
Funding: Weight Watchers International, Inc. (PI: Gorin)
Talea Cornelius was supported by T32MH074387 (PI: Kalichman)
Footnotes
Clinical trial registration: NCT03042208
Disclosure: ACW and GDF are employees of Weight Watchers International, Inc.
References
- Brewis AA (2014). Stigma and the perpetuation of obesity. Social Science & Medicine, 118, 152–158. [DOI] [PubMed] [Google Scholar]
- Brunson JA, Overup CS, Nguyen ML, Novak SA, & Smith V (2014). Good intentions gone awry? Effects of weight-related social control on health and well-being. Body Image, 11(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2007). The spread of obesity in a large social network over 32 years. New England Journal of Medicine, 357(4), 370–379. [DOI] [PubMed] [Google Scholar]
- Cornelius T, Gettens K, & Gorin AA (2016). Dyadic dynamics in a randomized weight loss intervention. Annals of Behavioral Medicine, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL, & Ryan RM (2008). Self-determination theory: A macrotheory of human motivation, development, and health. Canadian Psychology, 49(3), 182–185. [Google Scholar]
- Elfhag K, & Rössner S (2005). Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews, 6(1), 67–85. [DOI] [PubMed] [Google Scholar]
- Gabriele JM, Walker MS, & Gill DL (2005). Differentiated roles of social encouragement and social constraint on physical activity behavior. Annals of Behavioral Medicine, 29, 210–215. [DOI] [PubMed] [Google Scholar]
- Gabriele JM, Walker MS, & Heins JM (2006). Neighborhood climate, nondirective and directive support, health behavior and emotional status. Annals of Behavioral Medicine, 30, S063. [Google Scholar]
- Gabriele JM, Carpenter BD, Tate DF, & Fisher EB (2011). Directive and nondirective e-coach support for weight loss in overweight adults. Annals of Behavioral Medicine. 41(2). 252–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Lenz EM, Cornelius T, Huedo-Medina T, Wojtanowski AC, & Foster GD (in press). Randomized controlled trial examining the ripple effect of a nationally available weight management program on untreated spouses. Obesity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Powers TA, Koestner R, Wing RR, & Raynor HA (2014). Autonomy support, self-regulation, and weight loss. Health Psychology, 33(4), 332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Raynor HA, Fava J, Maguire K, Robichaud E, Trautvetter J, … & Wing RR (2013). Randomized controlled trial of a comprehensive home environment-focused weight-loss program for adults. Health Psychology, 32(2), 128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Wing RR, Fava JL, Jakicic JM, Jeffery R, West DS, Brelje K, & DiLillo VG (2008). Weight loss treatment influences untreated spouses and the home environment: Evidence of a ripple effect. International Journal of Obesity, 32(11), 1678–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes M, & Gove WR (1981). Living alone, social integration, and mental health. American Journal of Sociology, 87, 48–74. [DOI] [PubMed] [Google Scholar]
- Hunger JM, Major B, Blodorn A, & Miller CT (2015). Weighed down by stigma: How weight-based social identity threat contributes to weight gain and poor health. Social and Personality Psychology Compass, 9(6), 255–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, & Cook WL (2006). Dyadic data analysis. New York, NY: The Guilford Press. [Google Scholar]
- Kiernan M, Moore SD, Schoffman DE, Lee K, King AC, Taylor CB, Kiernan NE, & Perri MG (2012). Social support for healthy behaviors: scale psychometrics and prediction of weight loss among women in a behavioral program. Obesity, 20(4), 756–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koestner R, Powers TA, Carbonneau N, Milyavskaya M, & Chua SN (2012). Distinguishing autonomous and directive forms of goal support: Their effects of goal progress relationship quality and personal well being. Personality and Social Psychology Bulletin, 38(12), 1609–1620. [DOI] [PubMed] [Google Scholar]
- Lewis MA, & Rook KS (1999). Social control in personal relationships: impact on health behaviors and psychological distress. Health Psychology, 18(1), 63. [DOI] [PubMed] [Google Scholar]
- Lewis MA, & Butterfield RM (2005). Antecedents and reactions to health-related social control. Personality and Social Psychology Bulletin, 31(3), 416–427. [DOI] [PubMed] [Google Scholar]
- Markey CN, Gomel JN, & Markey PM (2008). Romantic relationships and eating regulation an investigation of partners’ attempts to control each others’ eating behaviors. Journal of Health Psychology, 13(3), 422–432. [DOI] [PubMed] [Google Scholar]
- McLean N, Griffin S, Toney K, & Hardeman W (2003). Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. International Journal of Obesity, 27(9), 987–1005. [DOI] [PubMed] [Google Scholar]
- McSpadden KE, Patrick H, Oh AY, Yaroch AL, Dwyer LA, & Nebeling LC (2016). The association between motivation and fruit and vegetable intake: The moderating role of social support. Appetite, 96, 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyler D, Stimpson JP, & Peek MK (2007). Health concordance within couples: a systematic review. Social Science & Medicine, 64(11), 2297–2310. [DOI] [PubMed] [Google Scholar]
- Novak SA, & Webster GD (2011). Spousal social control during a weight loss attempt: a daily diary study. Personal Relationships, 18(2), 224–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okun MA, Huff BP, August KJ, & Rook KS (2007). Testing hypotheses distilled from four models of the effects of health-related social control. Basic and Applied Social Psychology, 29(2), 185–93. [Google Scholar]
- Ryan RM, Patrick H, Deci EL, & Williams GC (2008). Facilitating health behaviour change and its maintenance: Interventions based on self-determination theory. The European Health Psychologist, 10(1), 2–5. [Google Scholar]
- Sorkin DH, Mavandadi S, Rook KS, Biegler KA, Kilgore D, Dow E, & Ngo-Metzger Q (2014). Dyadic collaboration in shared health behavior change: The effects of a randomized trial to test a lifestyle intervention for high-risk Latinas. Health Psychology, 33(6), 566–575. [DOI] [PubMed] [Google Scholar]
- Stephens MAP, Rook KS, Khan C, & Iida M (2010). Spouses use of social control and dietary adherence. Families, Systems, & Health. 28(3), 199–208. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Carraca EV, Markland D, Silva MN, & Ryan RM (2012). Exercise, physical activity, and self-determination theory: a systematic review. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira PJ, Silva MN, Mata J, Palmeira AL, & Markland D (2012). Motivation, self-determination, and long-term weight control. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe CT, Lewis MA, & Sterba KR (2008). Reactions to health-related social control in young adults with type I diabetes. Journal of Behavioral Medicine, 31, 93–103. [DOI] [PubMed] [Google Scholar]
- Tucker JS (2002). Health-related social control within older adults’ relationships. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 57(5), P387–P395. [DOI] [PubMed] [Google Scholar]
- Tucker JS, & Anders SL (2001). Social control of health behaviors in marriage. Journal of Applied Social Psychology, 31(3), 467–485. [Google Scholar]
- Wang ML, Pbert L, & Lemon SC (2014). Influence of family, friend and coworker social support and social undermining on weight gain prevention among adults. Obesity, 22(9), 1973–1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild TC, Cunningham JA, & Ryan RM (2006). Social pressure, coercion, and client engagement at treatment entry: a self-determination theory perspective. Addiction Behavior, 31(10), 1858–1872 [DOI] [PubMed] [Google Scholar]
- Wing RR & Jeffery RW (1999). Benefits of recruitment participants with friends and increasing social support for weight loss and maintenance. Journal of Consulting and Clinical Psychology, 67(1), 132–138. [DOI] [PubMed] [Google Scholar]