Abstract
Purpose
Because of the unprecedented disruption of health care services caused by the COVID-19 pandemic, the American Society of Radiation Oncology (ASTRO) and the European Society for Radiotherapy and Oncology (ESTRO) identified an urgent need to issue practice recommendations for radiation oncologists treating head and neck cancer (HNC) in a time of limited resources and heightened risk for patients and staff.
Methods and Materials
A panel of international experts from ASTRO, ESTRO, and select Asia-Pacific countries completed a modified rapid Delphi process. Topics and questions were presented to the group, and subsequent questions were developed from iterative feedback. Each survey was open online for 24 hours, and successive rounds started within 24 hours of the previous round. The chosen cutoffs for strong agreement (≥80%) and agreement (≥66%) were extrapolated from the RAND methodology. Two pandemic scenarios, early (risk mitigation) and late (severely reduced radiation therapy resources), were evaluated. The panel developed treatment recommendations for 5 HNC cases.
Results
In total, 29 of 31 of those invited (94%) accepted, and after a replacement 30 of 30 completed all 3 surveys (100% response rate). There was agreement or strong agreement across a number of practice areas, including treatment prioritization, whether to delay initiation or interrupt radiation therapy for intercurrent SARS-CoV-2 infection, approaches to treatment (radiation dose-fractionation schedules and use of chemotherapy in each pandemic scenario), management of surgical cases in event of operating room closures, and recommended adjustments to outpatient clinic appointments and supportive care.
Conclusions
This urgent practice recommendation was issued in the knowledge of the very difficult circumstances in which our patients find themselves at present, navigating strained health care systems functioning with limited resources and at heightened risk to their health during the COVID-19 pandemic. The aim of this consensus statement is to ensure high-quality HNC treatments continue, to save lives and for symptomatic benefit.
Introduction
The coronavirus (SARS-CoV-2) outbreak is considered a global pandemic by the World Health Organization.1 Most infected people develop a mild respiratory illness, but based on an early census from the U.S. Centers for Disease Control, 20% to 30% of persons aged ≥45 years require hospital admission, and fatality rates range from 10% to 17% in persons aged ≥85 years, 3% to 11% among persons aged 65 to 84 years, and 1% to 3% among persons aged 55 to 64 years.2 Those with cancer or receiving treatment for cancer are at enhanced risk of serious morbidity, including the need for ventilator support or death (hazard ratio, 3.56 [95% confidence interval, 1.65-7.69]).3 The pandemic has strained cancer services, with routine outpatient appointments cancelled, elective surgeries postponed, and resources diverted to the front line.
For the oncology clinician wishing to offer palliative therapies, there is a Hobson’s choice: a high symptom burden from cancer without treatment or an increased risk of more imminent death from SARS-CoV-2 infection resulting from the exposure and stress of therapy. For curative-intent treatments, there are parallel and specific challenges facing the head and neck (HN) oncologist: (1) operating room closures, with increased requirement for nonsurgical treatments; (2) an altered risk-benefit ratio of chemotherapy and radiation therapy as a result of increased susceptibility for SARS-CoV-2 infection; (3) a need to suppress coronavirus spread by minimizing travel of patients for daily treatments and the exposure of hospital and radiation therapy staff; and (4) a shortage of radiation therapy resources because of staff sickness or leave for family care, entailing allocation of resources and triage of patients. The use of hypofractionated radiation therapy (radiation schedules that are shorter overall but give a larger dose per treatment) could help address the latter 2 concerns, but these regimens may be unfamiliar to many radiation oncologists, and there is a risk of inappropriate application if these fall outside current international guidelines.
Because of this unprecedented disruption of health care services resulting from the COVID-19 pandemic, the American Society of Radiation Oncology (ASTRO) and the European Society for Radiotherapy and Oncology (ESTRO) identified an urgent need to issue practice recommendations for radiation oncologists treating head and neck cancer (HNC), in a time of limited resources and heightened risk for patients and staff.
Methods and Materials
With endorsement of the ASTRO and ESTRO executive committees, a panel of international experts was identified to provide practice recommendations for HNC during the COVID-19 pandemic. Panelists were nominated in equal numbers from the 2 societies, along with select representation from a few affected Asia-Pacific countries. A modified rapid Delphi process was used to develop consensus recommendations. A systematic literature review was not performed because of the urgency and lack of information on the conduct of cancer treatment related to the COVID-19 pandemic. The organizers (D.T., S.Y., D.P., M.G.) presented the initial topics and questions to the group by electronic survey, and subsequent questions were developed based on iterative feedback from the panelists. Questions were not asked again after agreement was reached. Each survey was open online for 24 hours, and successive rounds started within 24 hours of the previous round. The chosen cutoffs for strong agreement (≥80%) and agreement (≥66%) were extrapolated from RAND methodology.4 5
Two scenarios, both of current and global relevance to the COVID-19 pandemic, were evaluated:
-
•
Early COVID-19 pandemic scenario 1—risk mitigation, given the potential for (1) patient and/or staff infection as a result of repeat hospital visits, (2) risk of more serious infection in those receiving radiation therapy and/or chemotherapy, and (3) negative impact on strained health care resources from the management of the expected severe toxicities associated with intensive chemoradiation therapy.
-
•
Later COVID-19 pandemic scenario 2—severely reduced radiation therapy resources: the additional consideration of a lack of resources, whereby some patients are unable to receive radiation therapy.
The panel was asked to develop treatment recommendations for 5 common clinical cases of head and neck squamous cell carcinoma (HNSCC):
-
1.Oropharyngeal squamous cell carcinoma (SCC), T2 with multiple ipsilateral nodes <3 cm, M0; this was subdivided into
-
1a:p16 negative (OP–) and
-
1b:p16 positive (OP+)
-
1a:
-
2.
Laryngeal glottic SCC, T1bN0M0 (GLOT)
-
3.
Laryngeal SCC, T3N1M0 with impaired vocal cord mobility (LX)
-
4.
Metastatic hypopharyngeal SCC, T4aN1M1—obstructed, bleeding, with several lung metastases (HXpal)
-
5.Resected oral cavity SCC, pT2N2aM0; this was subdivided into
-
5a:with positive margins (OC+) and
-
5b:with close but clear 3 mm margins (OC–)
-
5a:
Supplementary questions concerned the conditions for delaying or interrupting radiation or chemotherapy for intercurrent SARS-CoV-2 infection, treatment prioritization in the case of severely limited resources, management in the case of surgical operating room closures, and how HN oncologists are adjusting clinics to account for the attendant risks. For all cases, we assumed a representative HNC patient fit for chemotherapy and/or radiation therapy.
This consensus statement was developed through an agreement between ASTRO and ESTRO, although given the urgency and differences in the societies’ usual development processes, adjustments to the societies’ usual procedures were allowed. The process was further endorsed by the Head and Neck Cancer International Group. Waiver of consent and exempt status was conferred by the University of California, San Francisco, Institutional Review Board (no. 20-30633).
Results
In total, 29 of 31 of those invited (94%) accepted, and after a replacement nomination by ESTRO, 30 of 30 completed all 3 surveys (100% response rate). In the respective rounds there were 80, 35, and 5 questions, taking on average a total of 73, 25, and 5 minutes to complete. The list of questions and panelists’ responses are included in Appendix E1.
Treatment prioritization
Panelists were asked whether certain cases should be postponed in either the early or late pandemic scenario. There was strong agreement (for cases of OP–, OP+, LX, HXpal, OC+) or agreement (GLOT) not to postpone the initiation of HNSCC radiation therapy by more than 4 to 6 weeks in both the early and late scenarios. For OC– in the late scenario, there was no consensus.
Panelists were then asked to prioritize the cases. Compared with all other types of cancer within one’s department requiring radiation therapy, there was strong agreement that OP–, OP+, and LX were very high (top 20%) or high (top 20%-40%) priority. On average, GLOT and OC+ were also deemed high priority, whereas HXpal was of average (40%-60%) priority. OC– was lower priority, and some (23%) would omit radiation therapy in the case of severely limited radiation therapy capacity.
In a situation of severely reduced resources, we further asked for these cases to be ranked in order of treatment priority against each other. These were ranked by the panel from high to low as OP+, OP–, LX, OC+, GLOT, HXpal, OC–. To further understand the trade-offs between treatment urgency and clinical priority, we asked respondents to set a policy by which a group of 20 patients would be treated before the other group could start. In this situation of policy determination, panelists prioritized LX over OP– (62%), OC+ over HXpal (63%), and HXpal over GLOT (73%).
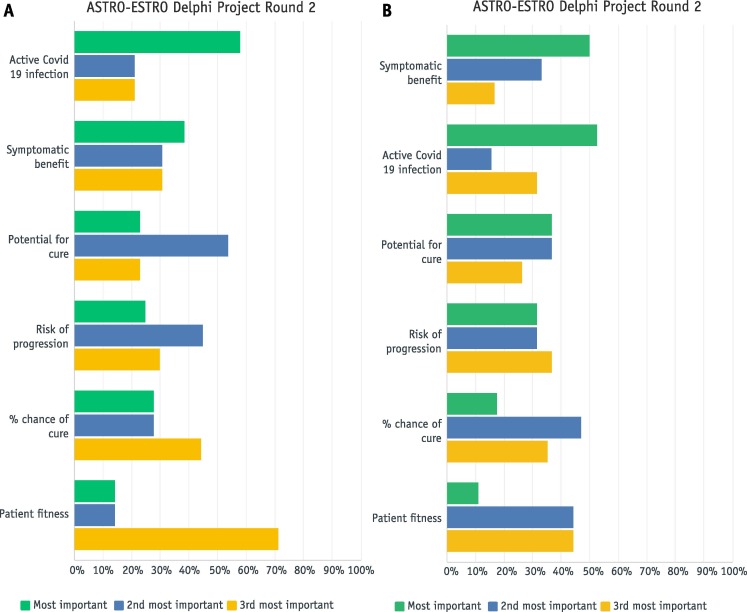
Panelists were finally asked to prioritize factors that would matter most in starting radiation therapy either within the next week or next 2 to 3 weeks. These rankings are shown by the highest to lowest weighted average from top to bottom (Fig. 1A and 1 B). In a scenario of late pandemic entailing severely reduced resources, the 3 factors of active SARS-CoV-2 infection, symptomatic benefit, and potential for cure (as opposed to the specific percentage likelihood of cure) were the most important in triage for radiation therapy over the next week (Fig. 1A). With an additional week or two of time before starting, active SARS-CoV-2 infection fell to the second highest weighted position behind symptomatic benefit (Fig. 1B).
Fig. 1.
(A) In scenario 2 (severely reduced radiation therapy resources), which are your top 3 factors to inform the triage (prioritization) of patients with head and neck cancer to start this week? Factors are ordered from highest to lowest weighted. (B) In scenario 2 (severely reduced radiation therapy resources), which are your top 3 factors to inform the triage (prioritization) of patients with head and neck cancer to start within 2 to 3 weeks? Factors are ordered from highest to lowest weighted.
COVID-19 Practice Recommendations: Treatment Prioritization
| Do not postpone the initiation of HNSCC radiation therapy by 4-6 weeks. | Strong agreement |
| HNSCC radical radiation therapy is high or very high priority. | Strong agreement |
| HNSCC postoperative radiation therapy for involved margins is high priority. | Agreement |
| HNSCC postoperative radiation therapy for minor risk factors is lower priority. | Agreement |
Intercurrent SARS-CoV-2 infection
In the case of a patient testing positive for SARS-CoV-2 infection, there was strong agreement (OP, GLOT, OC) or agreement (LX, HXpal) to delay the initiation of radiation therapy until the patient had recovered. However, for all cases there was initially agreement not to interrupt radiation therapy (except for HXpal, where a single fraction could be used). We therefore sought to better understand the recommendation not to interrupt radiation therapy and the interaction of this decision with SARS-CoV-2 symptom severity and timing during radiation therapy.
Panelists were instructed to assume that appropriate personal protective equipment would be available and best practices would be implemented, such as treating the patient at the end of the day in a designated vault, limiting exposure by using minimal staff, and properly sanitizing the vault. Under assurance of these conditions, for patients testing positive with mild symptoms (cough but normal activity level), 63% of the panel voted to continue radiation therapy, 17% would only interrupt in the first or second week of radiation therapy, and 20% would interrupt in any week of radiation therapy until the patient recovered. In other words, there was strong agreement to continue radiation therapy in those with SARS-CoV-2–related mild symptoms who had completed more than 2 weeks of treatment. On the other hand, there was also strong agreement among panelists to interrupt radiation therapy in any SARS-CoV-2+ patient demonstrating more severe symptoms (cough, chest pain, and trouble breathing at rest requiring oxygen support) until the patient had fully recovered. Different centers reported varying policies on deciding when a SARS-CoV-2+ patient would be able to return, including repeat negative testing as well as 10- to 14-day waiting periods.
For the minority who would interrupt radiation therapy even for mild symptoms, the top stated reasons included (1) concern for worsening the patient’s respiratory and general condition, (2) increased likelihood of emergency admission and/or need for feeding tube insertion, and (3) risk of infecting other patients and staff. A few panelists expressed that protection of staff and other patients should be prioritized over treatment of a single patient if unavailability of resources would endanger the many for the one.
COVID-19 Practice Recommendations: Intercurrent SARS-CoV-2 Infection
For patients testing positive for SARS-CoV-2 infection:
| Delay initiation of radiation therapy until recovery ± SARS-CoV-2 test is negative. | Strong agreement |
| Do not interrupt radiation therapy for mild SARS-CoV-2–related symptoms. | Agreement |
| Do not interrupt after week 2 of radiation therapy for mild SARS-CoV-2–related symptoms. | Strong agreement |
| Do interrupt radiation therapy for severe SARS-CoV-2–related symptoms. | Strong agreement |
Case-specific radiation therapy and chemotherapy practice
For each case, we asked participants to provide their center’s standard radiation therapy dose fractionation and how (if at all) this would be varied for scenarios of risk mitigation or severely restricted radiation therapy capacity (Table 1 ). In scenario 1 of early pandemic, there was strong agreement (OP and OC) or agreement (GLOT and LX) to stay with the same radiation therapy dose fractionation. There was no consensus for HXpal. In scenario 2 of late pandemic, there was strong agreement to use a more hypofractionated schedule for all of the cases compared with the average standard approach.
Fractionation schedules for 5 clinical cases: standard, early pandemic, and late pandemic recommendations
| Clinical case | Standard approach: percent agreement and favored schedules∗ | Scenario 1 Early pandemic: risk mitigation Change from standard: percent agreement and favored schedules∗ |
Scenario 2 Late pandemic: severe shortage of radiation therapy capacity Change from standard: percent agreement and favored schedules∗ |
|---|---|---|---|
| 1. Oropharynx SCC T2N2bM0, p16 negative (OP–) |
2.0-2.2 Gy/f (100%) (strong agreement) 70 Gy/35 f (63%) 70 Gy/33 f (17%) 65-66 Gy/30 f (13%) |
No change (strong agreement) |
Hypofractionated 2.41-3.0 Gy/f (70%) (strong agreement) 55 Gy/20 f (30%) 54 Gy/18 f (7%) 62.5-64 Gy/25 f (7%) |
| 2. Larynx SCC T1bN0M0 (GLOT) |
2.0-2.4 Gy/f (80%) (strong agreement) 63 Gy/28 f (52%) 70 Gy/35 f (14%) 66 Gy/33 f (10%) 50 Gy/16 f (7%) 55 Gy/20 f (7%) |
No change (agreement) |
Hypofractionated 2.41-3.2 Gy/f (70%) (strong agreement) 50 Gy/16 f (30%) |
| 3. Larynx SCC T3N1M0 (LX) |
2.0-2.2 Gy/f (97%) (strong agreement) 70 Gy/35 f (63%) |
No change (agreement) |
Hypofractionated 2.21-2.8 Gy/f (80%) (strong agreement) 55 Gy/20 f (30%) 54 Gy/18 f (7%) |
| 4. Hypopharynx SCC T4aN1M1, palliative (HXpal) |
Various (no agreement) 30 Gy/10 f (17%) 44.4 Gy/12 f (17%)† 20 Gy/5 f (13%) 32 Gy/4 f (7%) 8 Gy/1 f (4%)‡ |
Various(no agreement) 8 Gy/1 f (17%)‡ 44.4 Gy/12 f (13%)† 20 Gy/5 f (7%) |
Hypofractionated Various (strong agreement) 8 Gy/1 f (30%)‡ 20 Gy/5 f (20%) |
| 5. Oral cavity SCC Postoperative pT2N2aM0, involved margins (OC+) |
2.0 Gy/f (87%) (strong agreement) 66 Gy/33 f (53%) 60 Gy/30 f (30%) |
No change (strong agreement) |
Hypofractionated Various (strong agreement) 50 Gy/20 f (30%) 62.5 Gy/25 f (10%) |
Abbreviations: f = fraction; SCC = squamous cell carcinoma.
Percentage of panelists in agreement with dose/fraction range, followed by listing of the most commonly cited schedules arranged by percentage of panelists giving that response (latter does not add up to 100%).
Panelists called this schedule “quad shot,” but the exact schedule can vary; the schedule is based on 3.5-4.0 Gy given twice daily for 2 days, repeated for 3 cycles.
Some panelists mentioned that 8 Gy could be repeated, resembling the schedule called “0-7-21” where 8 Gy is given on those days according to patient tolerance.
Panelists stated that their usual standard concomitant chemotherapy schedules were cisplatin at 80 to 100 mg/m2 every 3 weeks (60%) and cisplatin at 30 to 40 mg/m2 once a week (40%). In early pandemic, there was strong agreement to continue the use of chemotherapy for all relevant cases where it would be applied (OP–, OP+, LX, OC+; Table 2 ) and agreement not to alter the schedules they used in standard practice. However, numerous panelists stated they would consider switching from high-dose to weekly cisplatin. In the late pandemic setting there was agreement to omit chemotherapy for OP+, and the majority (63%, near-agreement) would omit chemotherapy for HNC in general in this situation.
Table 2.
Chemotherapy recommendations: standard, early pandemic, and late pandemic approaches
| Standard approach | Scenario 1 Early pandemic: risk mitigation Standard therapy: percentage endorsement |
Scenario 2 Late pandemic: severe shortage of radiation therapy capacity Standard therapy: percentage endorsement |
|
|---|---|---|---|
| 1. Oropharynx SCC T2N2bM0, p16 negative (OP–) |
Concomitant chemotherapy | Yes: 93% No: 7% (strong agreement) |
Yes: 50% No: 50% |
| 1b. Oropharynx SCC T2N1M0, p16 positive (OP+) |
Concomitant chemotherapy | Yes: 87% No: 13% (strong agreement) |
Yes: 23% No: 77% (agreement) |
| 3. Larynx SCC T3N1M0 (LX) |
Concomitant chemotherapy | Yes: 83% No: 7% (strong agreement) |
Yes: 40% No: 60% |
| 5. Oral cavity SCC pT2pN2aM0, involved margins (OC+) |
Concomitant chemotherapy | Yes: 94% No: 6% (strong agreement) |
Yes: 50% No: 50% |
Abbreviation: SCC = squamous cell carcinoma.
Given the recommendations to use more hypofractionated radiation therapy schedules, we sought to understand the maximum dose per fraction that panel members considered safe and acceptable to use with concomitant chemotherapy. There was agreement favoring use of concomitant chemotherapy only with conventional or mildly hypofractionated radiation therapy of ≤2.4 Gy/fraction (f) (52%: 2.0-2.2 Gy/f; 21%: 2.2-2.4 Gy/f; 24%: 2.4-2.6 Gy/f; 3%: 2.6-2.8 Gy/f).
Of note, most panelists (63%, near-agreement) stated they did not consider induction chemotherapy to be a standard treatment for LX. A few (10%) supported induction as a standard treatment, and a minority (27%) supported its consideration as a temporizing measure in times of pandemic. In the end a majority (63%) recommended against use of induction chemotherapy in either of the pandemic scenarios, although it should be noted that this did not meet the predetermined cutoff for agreement. Several panelists expressed concern about the SARS-CoV-2–specific risk that could be incurred from an extended period of myelosuppression.
COVID-19 Practice Recommendations: Radiation Therapy and Chemotherapy Practice
In scenario 1, risk mitigation:
| Do not alter standard HNSCC radical radiation dose fractionation. | Agreement |
| Continue to use concomitant chemotherapy. | Strong agreement |
| Continue to use the standard concomitant chemotherapy schedule. | Agreement |
| Do not use induction chemotherapy for locoregionally advanced larynx SCC. | Majority, near-agreement |
In scenario 2, risk mitigation with severely reduced radiation therapy capacity:
| Use a hypofractionated radiation schedule. | Strong agreement |
| Reserve concomitant chemotherapy for use with conventional or mildly hypofractionated radiation therapy (≤2.4 Gy/f). | Agreement |
| Do not use induction chemotherapy to delay initiation of treatment. | Majority, near-agreement |
Operating room closures and the management of surgical cases
In many afflicted regions around the world, operating room capacity has been curtailed or, in severe pandemic scenarios, discontinued. However, many patients with HNC are traditionally treated with primary surgery. In the case of absolute operating room closure, we asked about the panelists’ recommended nonsurgical treatment strategy for 5 cases typically managed by primary surgery. In most cases, radical (chemo-)radiation was recommended (as opposed to clinical surveillance, systemic therapy, or palliative RT).
|
Radical radiation therapy | Agreement |
|
Radical chemoradiation therapy | Strong agreement |
|
Radical chemoradiation therapy | Agreement |
|
50% radical radiation therapy, 47% surveillance | No agreement |
|
Radical chemoradiation therapy | Strong agreement |
In response to this question, a few panelists commented that they would not wait more than 2 to 3 months for surgery. Therefore, for oral cavity cancers, where primary radiation therapy is less effective and more toxic, we specifically asked what amount of time would be acceptable for a patient to wait for operating room availability rather than starting radical (chemo-)radiation therapy.
|
Wait up to 8 weeks | Agreement |
|
Wait up to 4 weeks | Strong agreement |
A few practitioners commented that in these conditions they might wait longer, such as 12 or 6 weeks, respectively, to obtain surgery for these 2 cases.
COVID-19 Practice Recommendations: Operating Room Closures and Surgical Cases
Where faced with operating room closures and no capacity for HNC surgery:
| (Chemo-)radiation therapy should be used for locoregionally advanced HNSCC. | Agreement |
| Nontreatment is acceptable in certain cases of slow-growing cancers. | No agreement |
| For early oral cavity cancers, consider waiting for surgical capacity if this is predicted to be available within 8 weeks, and in this situation check on the patient every few weeks for progression. | Agreement |
| For locoregionally advanced oral cavity cancers, consider waiting for surgical capacity if this is predicted to be available within 4 weeks. | Strong agreement |
Adjustments to outpatient clinic appointments and supportive care
During the pandemic, there was strong agreement to modify the routine weekly in-person (face-to-face, in the same room) on-treatment reviews for patients receiving radiation therapy. There was also agreement to change the usual practice of conducting all new patient consultations in person. For both situations, there was no consensus approach; some (23%) had stopped in-person reviews altogether and others had reduced the frequency of in-person visits, replacing them with telephone (50%) or video (26%) consultations. A few panelists commented on concomitant reduction of dental, nutrition, or speech pathology services.
Panel members were in strong agreement not to increase the use of prophylactic placement of percutaneous endoscopic gastrostomy feeding tubes; some commented that interventional radiology services were unavailable because of the pandemic, and percutaneous endoscopic gastrostomy use was actually decreased. More than half of the panelists (53%) were no longer performing aerosol-generating procedures within the radiation therapy department (tracheostomy care, airway suctioning, flexible fiberoptic nasopharyngoscopy, nasogastric tube insertion).
COVID-19 Practice Recommendations: Appointments and Supportive Care
Where possible, reduce in-person (face-to-face, in the same room) consultations and replace with telephone or video for:
| Routine weekly on-treatment reviews | Strong agreement |
| New patient consultations | Agreement |
Discussion
The aim of this ASTRO-ESTRO practice recommendation was to provide urgent support for clinicians faced with managing HNC during the COVID-19 pandemic. There are a number of practice recommendations, structured around typical cases in distinct pandemic scenarios, but treatment decisions in the real world must take into account all the clinical factors relevant at the time. These decisions are informed by local and national policies and must be made within political, financial, and regulatory frameworks. On a practical level, the ability to implement hypofractionated radiation therapy schedules will depend on the circumstances of the particular radiation therapy department and the capability and capacity to do so (eg, knowledge of altered fractionation, critical structure dose constraints, and dosimetrist and physicist resources).
In the early pandemic risk-mitigation scenario, neither the potential benefits of using hypofractionated radiation therapy to reduce frequency of patient attendance nor the omission of concomitant chemotherapy to reduce risk of immunosuppression or treatment complications were deemed sufficient justification to alter standard practices for locoregionally advanced HNC. However, our scenarios described a patient fit for a combined-therapy regimen. Patient-specific factors (eg, age, fitness, comorbidities) were not addressed in this study. It has been recognized that the benefit of concomitant chemotherapy decreases with increasing age (especially for those older than 60 years).6 Therefore, for older patients or those with comorbidities who are at higher risk of more serious SARS-CoV-2 infection,7 and for whom concomitant chemotherapy will have less benefit, the use of chemotherapy should be restricted.
In the later scenario of severely reduced capacity (wherein some patients would need to go without radiation therapy), there was strong support for hypofractionated radiation therapy. For early larynx cancer (T1N0), 50 Gy/16 f was most commonly recommended,8 , 9 and there are data for 55 Gy/20 f in T2N0 disease.10 , 11 There is limited evidence to support the use of hypofractionated radical radiation therapy over 4 to 5 weeks for locoregionally advanced disease, but panelists suggested schedules, including 55 Gy/20 f,12, 13, 14, 15 62.5-64 Gy/25 f,16 , 17 and 54 Gy/18 f.18 , 19 Most would not use concomitant chemotherapy in this setting, and there was agreement to restrict concomitant chemotherapy to schedules of ≤2.4 Gy/f. Although there are data to support the use of concomitant platinum chemotherapy with higher doses per fraction,13 , 14 , 16 panelists expressed reservations about the potential lack of benefit (eg, no apparent local control or overall survival advantage from the combination of chemotherapy with accelerated radiation therapy)20 , 21 and the risk of increased acute and late toxicities.
It is important to recognize the continuum between the early and late scenarios described in this statement. The prevalence of SARS-CoV-2 infection in a given community may reach a point at which risk-mitigation strategies such as shorter fractionation schemes and the omission of concurrent chemotherapy must be considered before the actual onset of severely reduced capacity. Unfortunately, because predictors of how long a pandemic condition will last in a given geographic area are not exact, individual clinicians and policymakers are forced to make complex decisions with considerable uncertainty; this is, in fact, a limitation of many recommendations in this consensus statement because of marked variability in the extent, duration, and characterization of pandemic conditions across nations and regions. Decision making within the context of continually evolving pandemic conditions is further challenged by the prolonged nature of a course of chemoradiation in the HNC population.
Panelists also wished to address the conditions under which a SARS-CoV-2+ patient might be treated. As resources permit, clinicians should adhere to formal, prespecified screening and viral testing algorithms for HNC patients, because mucosal symptoms related to HN radiation may mimic mild infectious symptoms. For patients developing mild symptoms during radiation therapy and testing positive for SARS-CoV-2 infection, there was agreement not to interrupt treatment, especially if the patient had already completed the first 2 weeks of radiation therapy, because of more limited ability to reirradiate to a curative-intent dose and concerns about accelerated tumor repopulation later in the treatment course. The minority who wished to interrupt radiation therapy even for mild SARS-CoV-2–related symptoms cited concerns about the tolerability of treatment and the increase in exposure of staff and resource burden on the department and hospital. On the other hand, there was near-unanimous agreement that treatment of a patient highly symptomatic with SARS-CoV-2 infection should be interrupted.
In the later pandemic situation of severely reduced radiation therapy resources, decisions about treatment prioritization are required. When asked to determine the priority for each case compared with all other cancers and then among only the HNC cases, the average rankings were consistent, from highest to lowest priority: OP+, OP–, LX, OC+, GLOT, HXpal, OC–. However, when further tested as direct trade-offs choosing whether to start groups of 20 patients over the others, there were 2 areas of divergence. First, in these larger-scale policy terms, it was agreed that HXpal should be prioritized over GLOT with the rationale that (1) the treatment course could be delivered expediently by a single radiation fraction (note the increase from 4% to 30% of panelists who would use a single fraction in these late pandemic circumstances), which would result in important symptomatic benefit, and (2) GLOT could wait to start radiation therapy for a period of time without risk of significant progression or change in the chance of cure. This approach is in keeping with the earlier finding where postponement of GLOT by 4 to 6 weeks was acceptable to more than 20% of panelists. Second, the majority (62%) now agreed LX should be treated before OP–. This was important to prevent potential airway obstruction (ie, for symptomatic benefit), where both cases had a similar chance of cure. This preference was consistent with our finding that symptomatic benefit and chance of cure were 2 of the top 3 factors for panelists in determining which group of patients should start treatment within a week or 2 to 3 weeks in the face of severely reduced radiation therapy capacity. In terms of factors conditioning whether to initiate radiation therapy, the third most important factor was SARS-CoV-2 status, which reflects the strong agreement to delay the start of treatment in patients testing positive for SARS-CoV-2 infection.
An unfortunate consequence of the COVID-19 pandemic is the closure of operating rooms because of a lack of protective equipment to counteract increased exposure risk and redeployment of anesthesiologists and ventilators to critical care. There was consensus that HNC cases normally managed by primary surgery should generally be treated with radical (chemo-)radiation therapy rather than have no treatment. However, for a test case of oral cavity cancer, where radiation therapy is less effective and more toxic than surgery, there was agreement that waiting for up to 8 and 4 weeks for surgery was acceptable for T1-2 cancers and T3-4 cancers, respectively, with close clinical surveillance every few weeks to monitor for clinical progression.
A major effect of the COVID-19 pandemic is a shift in the risk-benefit ratio that typically governs HNC management. In the face of severely reduced resources, unaccustomed trade-offs may become necessary with the consequence of being forced to consider treatments that could carry a higher risk of late effects (hypofractionation) or could be suboptimal (without chemotherapy, nonsurgical) to ensure safety and therapeutic benefit for the greatest number of persons. These newly developed practice recommendations provide a global consensus and basic harmonization of approach in the face of limited clinical data to direct these difficult, unfamiliar decisions. One tangible benefit already achieved has been the rapid sharing and comparison of hypofractionation schedules considered “acceptable” by global HNC experts in times of extreme crisis such as COVID-19.
This urgent practice recommendation was issued in the knowledge of the difficult circumstances in which our patients find themselves at present, navigating strained health care systems functioning with limited resources and at heightened risk to their health from SARS-CoV-2 infection. The aim of this consensus statement is to ensure that high-quality HNC treatments continue, to save lives and for symptomatic benefit. The process was unusual in that several members of this panel participated even as they continued to deliver treatments while facing serious personal risks to themselves. This statement attempts to address the immediate impacts of the COVID-19 pandemic on HNC clinical practice. An understanding of future consequences (impacts on clinical research and scientific advancement, health care systems’ financial standing, health and psychological consequences for practitioners and patients) will require continued attention.
Acknowledgments
The authors thank Anne W.M. Lee, MD, of the University of Hong Kong; Jean Bourhis, MD, PhD, of the University of Lausanne; Joseph T.S. Wee, MD, PhD, of the National Cancer Centre Singapore; Cai Grau, MD, DMSc, of Aarhus University; Louis Harrison, MD, of the Moffitt Cancer Center; Hisham Mehanna, PhD, FRCS, of the Head and Neck International Group; Thomas Eichler, MD, and Laura Dawson, MD, of ASTRO; and Ben Slotman, MD, PhD, and Umberto Ricardi, MD, of ESTRO, for their support and advice on dissemination of this research.
Footnotes
Reprinted from International Journal of Radiation Oncology, Biology, Physics, published by Elsevier Inc. D.J. Thomson, C. Palma, M. Guckenberger et al., Practice Recommendations for Risk-Adapted Head and Neck Cancer Radiation Therapy During the COVID-19 Pandemic: An ASTRO-ESTRO Consensus Statement. International Journal of Radiation Oncology, Biology, Physics 107 (2020) 618-627, https://doi.org/10.1016/j.ijrobp.2020.04.016.
Research data are stored in an institutional repository and will be shared on request to the corresponding author.
Disclosures: D.B. reports other from ASTRO, UpToDate, and Sanofi-Celgene outside the submitted work; J.C. reports grants and personal fees from Varian Medical Systems outside the submitted work; KH. reports grants and personal fees from AstraZeneca, personal fees from BMS, grants and personal fees from Boehringer-Ingelheim, personal fees from Merck Serono, grants and personal fees from MSD, personal fees from Pfizer, and grants and personal fees from Replimune outside the submitted work; S.K. reports grants from Merck, grants from BMS, and personal fees from UpToDate outside the submitted work; J.A.L. reports grants, personal fees, and nonfinancial support from IBA, grants and nonfinancial support from RaySearch, nonfinancial support from Siemens, and grants and nonfinancial support from Mirada Medical outside the submitted work; Q.T.L. reports being a Merck scientific advisory committee member and Pfizer DSMB member outside the submitted work; N.L. reports grants and personal fees from Pfizer, grants and personal fees from Merck, grants from Astra Zeneca, grants and personal fees from Merck Serono, personal fees from Sanofi Aventis, personal fees from Lilly, personal fees from UpToDate, and a patent SK2016-129-01 issued outside the submitted work; W.B. reports personal fees from MSD, personal fees from BMS, personal fees from Pfizer, and personal fees from Merck outside the submitted work; S.S.Y. reports grants from Genentech, Bristol-Myers Squibb, Merck, and BioMimetix and personal fees from Springer and UpToDate outside the submitted work.
Supplementary material for this article can be found at https://doi.org/10.1016/j.ijrobp.2020.04.016.
Supplementary Data
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report-51 https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn = 1ba62e57_10pdficon Available at:
- 2.Centers for Disease Control and Prevention Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liang W., Guan W., Chen R., et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fitch K., Bernstein S.J., Aguilar M., et al. RAND Distribution Services; Santa Monica, CA: 2003. The RAND/UCLA Appropriateness Method User's Manual. [Google Scholar]
- 5.Guckenberger M, Belka C, Bezjak A, et al. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus statement [e-pub ahead of print]. Radiother Oncol. 10.1016/j.radonc.2020.04.001. Accessed May 3, 2020. [DOI] [PMC free article] [PubMed]
- 6.Pignon J.-P., le Maître A., Maillard E., et al. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): An update on 93 randomised trials and 17,346 patients. Radiother Oncol. 2009;92:4–14. doi: 10.1016/j.radonc.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Chen N., Zhou M., Dong X., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gowda R.V., Henk J.M., Mais K.L., et al. Three weeks radiotherapy for T1 glottic cancer: The Christie and Royal Marsden Hospital experience. Radiother Oncol. 2003;68:105–111. doi: 10.1016/s0167-8140(03)00059-8. [DOI] [PubMed] [Google Scholar]
- 9.Cheah N.L.C., Lupton S., Marshall A., et al. Outcome of T1N0M0 squamous cell carcinoma of the larynx treated with short-course radiotherapy to a total dose of 50 Gy in 16 fractions: The Birmingham experience. Clin Oncol (R Coll Radiol) 2009;21:494–501. doi: 10.1016/j.clon.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Ermis E., Teo M., Dyker K.E., et al. Definitive hypofractionated radiotherapy for early glottic carcinoma: Experience of 55Gy in 20 fractions. Radiat Oncol. 2015;10:203. doi: 10.1186/s13014-015-0505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chera B.S., Amdur R.J., Morris C.G., et al. T1N0 to T2N0 squamous cell carcinoma of the glottic larynx treated with definitive radiotherapy. Int J Radiat Oncol Biol Phys. 2010;78:461–466. doi: 10.1016/j.ijrobp.2009.08.066. [DOI] [PubMed] [Google Scholar]
- 12.Tobias J.S., Monson K., Gupta N., et al. Chemoradiotherapy for locally advanced head and neck cancer: 10-year follow-up of the UK Head and Neck (UKHAN1) Trial. Lancet Oncol. 2010;11:66–74. doi: 10.1016/S1470-2045(09)70306-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benghiat H., Sanghera P., Cashmore J., et al. Four week hypofractionated accelerated intensity modulated radiotherapy and synchronous carboplatin or cetuximab in biologically staged oropharyngeal carcinoma. Cancer Clin Oncol. 2014;3 [Google Scholar]
- 14.Jacinto A.A., Filho E.S.B., de Souza Viana L., et al. Feasibility of concomitant cisplatin with hypofractionated radiotherapy for locally advanced head and neck squamous cell carcinoma. BMC Cancer. 2018;18:1026. doi: 10.1186/s12885-018-4893-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehanna H., Wong W.-L., McConkey C., et al. PET-CT surveillance versus neck dissection in advanced head and neck cancer. N Engl J Med. 2016;374:1444–1454. doi: 10.1056/NEJMoa1514493. [DOI] [PubMed] [Google Scholar]
- 16.Meade S., Gaunt P., Hartley A., et al. Feasibility of dose-escalated hypofractionated chemoradiation in human papilloma virus-negative or smoking-associated oropharyngeal cancer. Clin Oncol (R Coll Radiol) 2017;30:366–374. doi: 10.1016/j.clon.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Thomson D.J., Ho K.F., Ashcroft L., et al. Dose intensified hypofractionated intensity-modulated radiotherapy with synchronous cetuximab for intermediate stage head and neck squamous cell carcinoma. Acta Oncol. 2015;54:88–98. doi: 10.3109/0284186X.2014.958528. [DOI] [PubMed] [Google Scholar]
- 18.Agger A., von Buchwald C., Rørbæk Madsen A., et al. Squamous cell carcinoma of the nasal vestibule 1993–2002: A nationwide retrospective study from DAHANCA. Head Neck. 2009;31:1593–1599. doi: 10.1002/hed.21132. [DOI] [PubMed] [Google Scholar]
- 19.Stavas M.J., Shinohara E.T., Attia A., et al. Short course high dose radiotherapy in the treatment of anaplastic thyroid carcinoma. J Thyroid Res. 2014 doi: 10.1155/2014/764281. 2014:764281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ang K.K., Harris J., Wheeler R., et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bourhis J., Sire C., Graff P., et al. Concomitant chemoradiotherapy versus acceleration of radiotherapy with or without concomitant chemotherapy in locally advanced head and neck carcinoma (GORTEC 99-02): An open-label phase 3 randomised trial. Lancet Oncol. 2012;13:145–153. doi: 10.1016/S1470-2045(11)70346-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.