Abstract
In recent months, the COVID-19 pandemic has threatened the financial viability of pediatric ophthalmology practices. To measure the economic impact, the American Association of Pediatric Ophthalmology and Strabismus (AAPOS) Socio-economic Committee surveyed current US members at the peak of the COVID shutdown, in April 2020. With a robust response rate, the survey portrays that some pediatric ophthalmology practices are ominously strained, if not irreparably harmed.
The COVID-19 2020 pandemic has created unprecedented challenges for many, and most medical specialists, including pediatric ophthalmologists, have found themselves uniquely isolated. Both the American Academy of Pediatrics (AAP and the American Academy of Ophthalmology (AAO) offered pandemic-related recommendations and guidelines, but neither national society has fully addressed the challenges unique to pediatric ophthalmology.
With fewer than 1,100 pediatric ophthalmologists (POs) available to meet the eyecare needs of 75 million American children,1 the American Association for Pediatric Ophthalmology and Strabismus (AAPOS) anticipated potentially severe access-of-care consequences from the COVID-19 quarantine. AAPOS conducted a membership survey in April 2020 to assess the effects on pediatric ophthalmology practices, including the interim effects on finances and staffing, as well as the expected effect of government aid and future practice changes. The results are sobering and portend access-of-care issues for children with blinding, if not life-threatening, diseases. As pediatric specialists struggle to keep their practices viable, children in America may suffer medical outcomes not anticipated in first-world countries.
Methods
The University of California San Diego Institutional Review Board / Ethics Committee ruled that approval was not required for this study. A 19-question online survey was created by the AAPOS Socio-economic Committee, led by the authors. On April 22, 2020, AAPOS distributed the survey via direct email to all US-based full members and candidates-in-training (all whom were physicians in practice and not in training programs), allowing 5 days to collect anonymous responses. The survey is provided as eSupplement 1 (available at jaapos.org).
Results
Distribution Characteristics
There was a 40% response rate, with 416 respondents of 1,047 physicians polled. Complete data sets to all relevant questions were submitted by 92% of respondents. Almost all states were represented (46 states and Puerto Rico), with practice locations characterized as suburban (53%), urban (45%), and rural (3%).
The individual ophthalmologists self-identified as belonging to one of five groups: employed hospital (EH), employed university / academic center (EA), private practice solo (PPS), private practice multispecialty ophthalmology group (PPMOG), and private practice pediatric ophthalmology / strabismus–only group (PPPOG). Employed physicians made up 32% of the respondents (131 of 413), with 10% hospital employed (n = 40) and 22% university employed (n = 91). Private practice physicians made up 68% (282 of 413), with 17% solo (n = 70), 28% multispecialty (n = 119) and 23% group peds (n = 93). See Figure 1 . This is a similar but slightly less private practice percentage than is representative of the AAPOS membership, which is approximately 80% private practice according to Christie Morse, MD, Executive Vice-President of the American Association for Pediatric Ophthalmology and Strabismus (personal communication, June 26, 2020).
Fig 1.
Distribution of practice types.
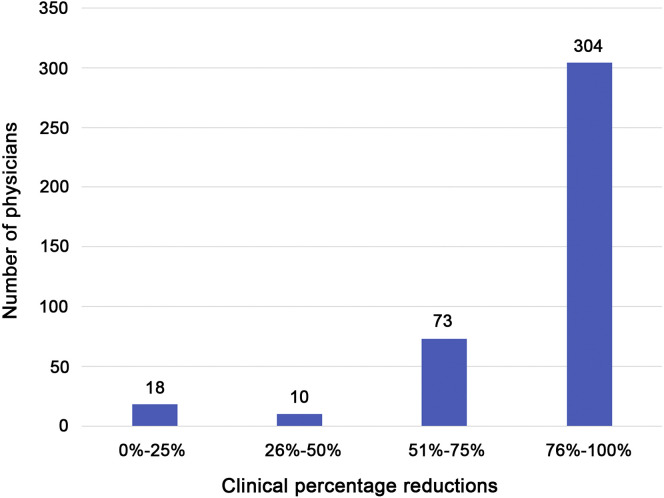
Clinical Revenue
All five groups reported a significant decrease in clinical (nonsurgical) revenue during the first month of the shutdown. For most states, mid-March was the beginning of the shutdown, coinciding with the March 16, 2020, presidential issuance of guidelines for limiting number of people at social gatherings and social distancing. The loss of clinic revenue was 76%-100% in 75% of all responding practices (304/405); 18% of all practices (73/405) noted a 51%-75% loss of clinical revenue. Overall, 93% of practices (377/405) suffered at least a 51% loss of clinical revenue during this period (Figure 2 ).
Fig 2.
Clinical revenue percentage reductions.
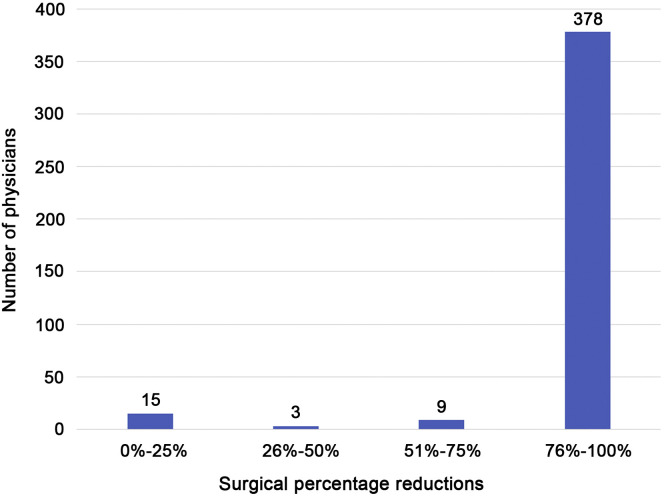
Surgical Revenue
Irrespective of practice type, virtually all pediatric ophthalmology groups experienced a severe loss of surgical revenue. For 93% of respondents (378/405), surgery revenue decreased by at least 76%. Of all respondents, 96% (387/405) had a surgical revenue decrease of >51% (Figure 3 ).
Fig 3.
Surgical revenue percentage reductions.
Salary Guarantees
For EH and EA physicians, 53% had at least 70% of their income guaranteed; however, 21% had no guaranteed income.
Revenue Generation
With regard to generating revenue, 78% generated 0%-25% of normal revenue during the pandemic shutdown, whereas only 11% were able to generate at least 51% of their normal revenue. The average reported practice revenue generated was 13% of usual amounts.
Economic Injury Disaster Loans (EIDL) and Other Non-Paycheck Protection Program (PPP) Loans
Both the EIDL and PPP loans were federal mechanisms for financial assistance early in in the shutdown. Because of the program's structure, only a handful of employed physicians (hospitals and academic centers) applied for either loan: EIDL (EH, 1; EA, 6). Of employed physician applicants 0 of 1 EH (0%) and 4 of 6 EA (67%) received EIDL loans. For private practices (solo, multispecialty, and pediatric only), 43% of physicians (122/282) applied for the EIDL, and 40% received the loan. Taking all practices combined, 39% (51/129) received a non-PPP loan.
Application/ Received Paycheck Protection Program (PPP) Loans
Of private practices, 74% (232/315) applied for PPP loans, and 50% of applicants (116) received the loan in the first tranche. The survey predated the second tranche. Only 3 applicants were EH (n = 1 applied, 0% received) or EA (n = 2 applied, 50% received). Of solo practices, there was a 42% success rate (25/60); of multispecialty practices, a 62% success rate (55/89). Of the pediatric ophthalmology–only group practices, there was a 44% success rate (33/75).
PPP loans successfully obtained varied widely by state and geographic area, with 35 of 46 states represented by loan recipients. Some states had much higher representation of loans than their population. East of the Mississippi, 76% (86/113) loans were given, although only 58% of the US population lives in that region. The respondents' states that received the most PPP loans were Virginia (n = 11), New York (n = 10), Florida (n = 9), Georgia (n = 8), Pennsylvania (n = 7), Illinois (n = 6), and North Carolina (n = 5). All other states had fewer than 5 recipients.
Staff Furlough, Lay-off, Dismissal
In many cases, loss of revenue was in part offset by payroll modification, including furloughing, laying off, dismissal, and reduction of staff hours or salaries. Private practice groups resorted to staff furloughs and dismissal much more readily than other groups.
Just over 30% of employed physicians responded to this query, with the majority reporting preservation of staffing. Of those employed practices that did reduce staff, the vast majority furloughed or dismissed 25% or less. The presence of union employed staff may have played a part in these numbers. In contrast, for private practices, with 90% responding to the question, 50% (157/315) reported a reduction of >51% in staff through furlough or dismissal; 36% (112/315) reduced staff by >76 %.
Understandably, EH and EA physicians employed different strategies than private practice doctors in managing staff. With only 11 EH physicians responding, 7 reported a reduction in staff of <25%. Of the 42 EA physicians who replied, 36 reduced staff by <25%, and 25 of those 36 reported a 0% reduction. Very few employed physicians (EH, 3; EA, 5) reported staff reductions of more than 51%.
Regarding private practice groups' greater utilization of staff dismissals and furloughs, 55% of multispecialty practices (62/112) reported staff reduction of >76%, with 13% (15/112) reporting a reduction of 51%-75%. Thus, 69% (77/112) had more than a 51% reduction. For pediatric-only groups, 38% of respondents (35/93) reported a reduction of >76%; 9% (8/93), a reduction of 51%-75% reduction; and 46% (43/93), a reduction of >51% reduction. For solo practices, 30% (19/68) reported a staff reduction of >76%; 4% (3/68), a reduction of 51%-75%. Thus, 32% (22/68), had a staff reduction >51%.
In summary, 52% of private practices (142/273) reported a staff reduction of >51%. For EH and EA, most did not reduce staff. One could surmise that many EH and EA physicians bypassed this question, because there was no significant reduction in staff or they did not participate in this decision. Additionally, the physicians that did respond were likely affected by a significant presence of union staff in the employed environments.
Staff Not Furloughed
All practice types also controlled staff expense by means other than furlough and dismissal, with >65% reducing staff hours or salary. Among all respondents, the full-time working staff rate was 20% (63/309), the reduced hours rate was 60% (186/309), and the reduced salary rate was 5% (16/309). Family First Act (FFA) mechanisms such as the government-funded Paid Time Off and Family Medical Leave Act were used by 2% of practices; a combination of reduced hours, salary rate adjustment, and/or FFA mechanisms was used by 13% of practices (39/309).
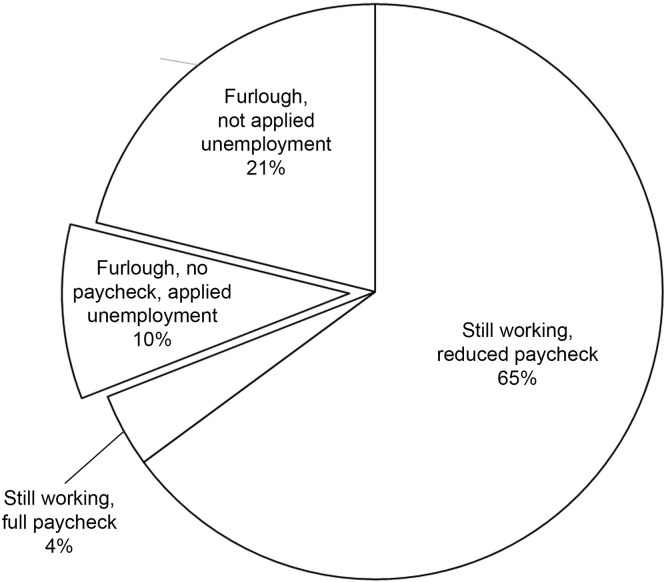
Physician Furlough or Unemployment
Of the 317 respondents, 87% (277/317) reported having been furloughed or having their salary reduced. There was a significant disparity between hospital and academic physicians compared with private practice physicians: 35% of the 53 EH or EA respondents reported having had their salary reduced or being furloughed, whereas 90% of the 264 private practice respondents reported having a reduction in salary or furlough. Nearly 10% of private practice physicians applied for unemployment benefits. See Figure 4 .
Fig 4.
Private practice physician employment and paycheck reduction.
Rehiring
A total of 215 physicians responded to the question regarding how they would manage staff layoffs, furloughing, and eventual rehiring of staff. In the private practice group, 34% (74/183) were undecided, 33% (71/183) planned to increase staff gradually, and 5% (10/183) said they would reduce staff permanently. Of the total, 60% indicated that they would rehire all staff on receipt of the PPP loan.
Pace of Return
Physicians from each practice type had similar views on the future of their practice when limitations are lifted. Nearly half (46% [n = 176]) anticipate a slow return to their normal practice productivity; 33% (n = 126) expect a slow return, which could jeopardize their practice viability; 13% (n = 48) expressed pessimism that their practice productivity will return to pre-COVID levels. Only 8.0% of respondents (n = 30) expect a rapid return of their practice.
Bankruptcy
Bankruptcy was considered an option by 10% of respondents (38/362). Most of those who indicated they would consider bankruptcy (36/38) were in private practice. This number rose when only private practice respondents were analyzed to 13% (36/260).
Medicaid Limitations
More private practice physicians than employed hospital and academic physicians expressed plans to limit Medicaid patients. Of EH and EA physicians, 7% planned to limit Medicaid, whereas 27% of private practices (72/262) planned to do the same. Within the private practice subgroups, each reported similar rates of respondents who will limit Medicaid patients.
Retirement Plans
Asked whether or not practice limitations related to COVID-19 would change their retirement plans, just over half (57%) of 375 respondents reported that they would not change their plans. About a third (35%) reported that they would need to delay retirement and 9% would retire earlier.
Discussion
The COVID national emergency sent shock waves through pediatric ophthalmology, creating a near-paralyzing tension between patients' medical needs, COVID-related safety issues, and the financial viability of practices. As one patient lightheartedly stated, “Normal is now just a setting on the clothes dryer.” While almost all sectors of global industry were negatively affected by the pandemic, the consequences to medical subspecialties may lead to loss of practices and therefore loss of healthcare to patients.
This survey shines light on the struggle for financial viability experienced by many American pediatric ophthalmologists. Despite the robust response rate of 40%, all such surveys lend themselves to self-reporting and judgment bias. The effect of private equity ownership was not explored in this study. Despite these limitations, it is probable that the survey results reflect accurate trends, given the relatively large number of responses.
Although the United States instituted sweeping, stay-at-home orders beginning around March 19, 2020, pandemic-related socioeconomic effects began earlier. Despite the narrow timeline of this preliminary study, severe economic ramifications for pediatric ophthalmologists were already evident approximately 1 month after stay-at-home orders went into effect.
The AAP has recommended that its members continue to provide routine pediatric medical examinations in order to prevent future diseases and worsening of other medical conditions,2 whereas the AAO has recommended ceasing all nonemergent eye care.3 These conflicting recommendations contributed to unique challenges for pediatric ophthalmologists, making patient triage during the COVID-19 shutdown difficult. Pediatric patients often do not self-report symptoms, creating the potential for undetected visual damage with lifelong and potentially life-threatening ramifications. Symptoms and signs reported by a parent or pediatrician may under- or over-represent the severity of the child's condition; for example, “headaches” may stem from mild seasonal allergies or malignancy-related papilledema. Choosing, through triage, to not see a patient may contribute to a parental decision to visit an emergency room or urgent care, potentially creating an unnecessary exposure to COVID-19. In addition, the triage process may prevent patients from receiving necessary care and have subsequent repercussions. All of these individual health concerns needed to be weighed and balanced with the community health concerns during the shutdown.
As physicians struggle to balance health concerns, safety issues, and financial viability, the triage process during the COVID-19 shutdown and subsequent reopening have been further complicated by the frequency of presymptomatic carriers actively shedding viral particles.4 The newly discovered coronavirus 2019 is known to shed in tears5 and is aerosolized in crying,6 singing, or screaming. The extremely close contact required for ophthalmologic examinations (often only several inches), and the limitations of equipment use with protective gear make this area of medicine more high-risk for patient-physician transmission than most subspecialties. A recent study found that ophthalmologists in general were among the highest risk specialties for contracting COVID-19.7 It may be that pediatric ophthalmology would be an even higher risk, given the higher chance of aerosols from patients, the inability of young children to wear masks during examinations, and with the potential for pediatric patients with presymptomatic infections.
The risk of pediatric ophthalmologists and their staff being infected with COVID-19 on reopening is of great concern. The following data were provided by MRG O'Gorman, MBA, M.Sc, PhD, D(AMBLI), Chief of Laboratory Medicine at Children's Hospital Los Angeles and Professor of Pathology and Pediatrics, Keck School of Medicine, University of Southern California (personal communication, May 22, 2020 by). Testing of healthy asymptomatic preoperative patients in the Southern California/Los Angeles area found that 1.9% of asymptomatic children are COVID-19 positive This rate of positivity increased in tested children from local pediatric clinics, with degree of positivity noted with symptoms of 5.8%-21.6%. Similar tests confirmed that nearly 10% of children in Los Angeles area are COVID-19 antibody positive. Extrapolating from O'Gorman's data, a daily pediatric ophthalmology clinic of 50 patients in Southern California could be expected to have at least 1 presymptomatic child carrying COVID-19. Regional variation, limited testing, false negative and positive tests, and prolonged turnaround time on tests further impede management protocols for all localities. Family members in the examination room multiply this risk.
Disproportionate consequences for financially disadvantaged children may accelerate, as financial concerns lead both private and academic providers to reduce access of care for Medicaid patients, as suggested by survey results. Practice closures will exacerbate this funneling phenomenon of Medicaid patients, potentially leading to longer travel time, decreased appointment availability, delayed care, and increased cost of care. However, the number of private practices that are planning to limit Medicaid patient access may be mildly overestimated, because some private practices never accepted Medicaid patients before COVID-19. Our study found that 27% of private practices were planning to limit Medicaid patients, compared with <20% of practices before COVID-19. These numbers are magnified, because the Medicaid population accounts for approximately 50% of pediatric ophthalmology patient volume. Pre-COVID-19 Medicaid statistics were provided by ophthalmic practice management consultant John Pinto (personal communication, on June 23, 2020). This will place additional financial stress on the centers that continue to provide care for Medicaid patients as they see their payor-mix affected.
Revenue for both employed and private practice was markedly decreased for both clinic-based (93% of practices had >51% loss) and surgery-based patient care (96% of practices had >51% loss). Whereas most employed physicians were able to rely on financial support from their institutions, private practice physicians did not have that option. However, the employed sector suffered as well, with almost half of employed physicians (EH and EA) having salary guarantees of <70% of their norm. Across all practices, the average revenue generation was only 13% of usual. This last number cannot be overemphasized as a threat to the viability of practices across the United States.
The effectiveness of economic aid in preserving practices' viability and ability to serve patients has yet to be determined. An EIDL of $10,000 would not help most practices greatly; nevertheless, approximately one-quarter of all survey respondents applied, of whom only 34% received the loan. Programs such as the Coronavirus Aid, Relief, and Economic Security (CARES) Act Provider Relief Fund are limited, because the offer help for practices that are Medicare based, excluding most pediatric ophthalmology practices at the time of this study. Practice finance loans and refinances as well as any conventional SBA loans were basically unavailable. The Paycheck Protection Program (PPP) offered some financial assistance, but its structure made it largely inaccessible to hospital and academic practices. PPP loans did benefit private practices, with 79% applying for and 50% receiving it the first tranche. The PPP loan has some limitations. First, it covers salary only up to $100K. Though many staff salaries were protected, physicians and highly compensated employees were only partially covered. Second, the PPP benefit was limited mainly to salary protection, with roughly 25% allocated for other overhead. Yet for most ophthalmic practices only 50%-70% of expenses are staff and physician salaries.8 In the context of significant fixed expenses and, on average, production of only 13% normal revenue, many expenses were left uncovered. Third, payments were based on 2 months of payroll, although the economic sequelae will persist for many more months or years. Finally, only 50% of respondents received PPP loans in the first tranche, leaving the 50% who were unsuccessful in obtaining the loan and the 21% who did not apply financially vulnerable.
Because it is difficult to reduce fixed costs (eg, rent, insurance, utilities), cost containment is largely focused on elimination and reduction of staffing expenses. Although reduction of staff was noted in all practice settings, it was most drastic in private practices that did not have the safety net of major institutional backing. For hospital and academic employed respondents, most did not reduce staff and, if so, by <25%. Because of the low response for employed respondents (30%), it is not clear whether the hospitals did not furlough staff or whether the physicians did not know and could not answer the question. In contrast, for private practices, over 90% responded to the question, with over 50% having reduction in staff of >51%. The reduction in staff was most apparent in the multispecialty group. Disproportionate staff reduction by multispecialty groups may result from the AAO recommendation to cease all nonemergent care in contrast to pediatric ophthalmology practices, which may have been more influenced by the AAP's directive to remain available for patients.
Physician unemployment in the United States was almost inconceivable in the recent past, measuring at 0.4% in 2019 by the US Bureau of Labor Statistics.9 This survey revealed that a large number (nearly 90%) of pediatric ophthalmologists were either furloughed or had their salary reduced, and approximately 10% of those in private practice filed for unemployment. As noted in a Washington Post article published in May of 2020, “Health-care spending [has] decline[d] at an annualized rate of 18 percent in the first three months of the year, according to Commerce Department data, the largest reduction since the government started keeping records in 1959. And that proved the biggest factor in driving the annualized 4.8 percent decline in first-quarter gross domestic product, which itself was the worst overall contraction in GDP since the Great Recession. An even worse decline is projected for the current quarter, which ends in June. Morgan Stanley forecasts a record 37.9 percent drop in second-quarter GDP.”10
Finally, with this survey reflecting a snapshot 1 month into the shutdown, results do not represent mid- or long-term effects on pediatric ophthalmology practices. However, the short-term effects of the pandemic suggest that practices will struggle to regain baseline levels of function. Ongoing sequelae will ultimately decrease pediatric ophthalmologists' ability to serve patients, especially those who are most financially disadvantaged. The pace of return and rehiring of staff will be influenced by additional stimulus monies that were distributed after the data collection in late April 2020. For the 10% of pediatric ophthalmologists who were considering bankruptcy, one can hope that additional stimulus monies will prevent the need. A follow-up survey is planned to measure pace of economic recovery and long-term effect of COVID-19 on US pediatric ophthalmology.
In conclusion, this early survey reveals that the financial toll of canceling care, even after only 1 month of US COVID-19 stay-at-home orders, was devastating to pediatric ophthalmology practices. Although all sectors of pediatric ophthalmology were affected by the reduction in patient volume, at the 1-month juncture, the effect on private practices was greatest. As the pandemic and associated shutdown continues, further financial, medical care delivery and provider availability issues will ensue. Further longitudinal studies (eg, recovery models, telemedicine effectiveness) will be paramount in addressing the needs and concerns of the pediatric ophthalmology sector as the COVID-19 pandemic continues. We hope that quantification of the severe economic effects on pediatric ophthalmology in the United States can be useful in the legislative process to advocate for this healthcare sector in order to promote the highest quality medical and surgical eye care for children and for adults with strabismus.
Acknowledgments
The Socioeconomic Committee would like to thank the officers of AAPOS for their guidance and tireless efforts, specifically Jane Edmond, Christie Morse, Bob Gold, Eric Lichtenstein, and Kathy Lee. The authors are also indebted to David Kuo, UC San Diego Ophthalmology resident extraordinaire, for his assistance with graphic interpretation of this study, and Craig Kishaba, UC San Diego Department of Ophthalmology Business Officer, for providing reference statistics.
AAPOS Socioeconomic Committee: Robert Arnold, Michael Bartiss, Angela N. Buffenn, Brian Campolattaro, Christopher Gappy, Corina Gerontis, Jonathan Go, Kartik Kumar, Carolyn Lederman, Danielle Ledoux, Eric Lichtenstein, Eric Packwood, Joseph Paviglianiti, Andrew Reynolds, Shira L. Robbins, Lance Siegel, Julia Stevens, Ron Teed, Ben Ticho, and Lisa Vredevoogd.
Contributor Information
AAPOS Socioeconomic Committee:
Robert Arnold, Michael Bartiss, Angela N. Buffenn, Brian Campolattaro, Christopher Gappy, Corina Gerontis, Jonathan Go, Kartik Kumar, Carolyn Lederman, Danielle Ledoux, Eric Lichtenstein, Eric Packwood, Joseph Paviglianiti, Andrew Reynolds, Shira L. Robbins, Lance Siegel, Julia Stevens, Ron Teed, Ben Ticho, and Lisa Vredevoogd
Supplementary Data
References
- 1.Children's Defense Fund The State of America's Children 2020. https://www.childrensdefense.org/wp-content/uploads/2020/02/The-State-Of-Americas-Children-2020.pdf Available at:
- 2.American Academy of Pediatrics Guidance on Providing Pediatric Well-Care During COVID-19. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/guidance-on-providing-pediatric-ambulatory-services-via-telehealth-during-covid-19 Available at:
- 3.American Academy of Ophthalmology Recommendations for Urgent and Non-Urgent Patient Care. https://www.aao.org/headline/new-recommendations-urgent-nonurgent-patient-care Available at:
- 4.He X., Lau E.H.Y., Wu P., et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 5.Seah I.Y.J., Anderson D.E., Kang A.E.Z., et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) Ophthalmology. 2020;127:977–979. doi: 10.1016/j.ophtha.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sivabalan S., Srinath M.V. Does a crying child enhance the risk for COVID-19 transmission? Indian Pediatr. 2020;57:586–587. doi: 10.1007/s13312-020-1870-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breazzano M.P., Shen J., Abdelhakim A.H., et al. Resident physician exposure to novel coronavirus (2019-nCoV, SARS-CoV-2) within New York City during exponential phase of COVID-19 pandemic: Report of the New York City Residency Program Directors COVID-19 Research Group. MedRxIV platform. https://www.medrxiv.org/content/10.1101/2020.04.23.20074310v1 Available at:
- 8.Masercola E. 5 key benchmarks that make or break your practice. Eye Care Leaders, December 2, 2016, 18-20. https://eyecareleaders.com/5-key-benchmarks-that-make-or-break-your-ophthalmology-practice/ Available at:
- 9.Stebbins S. Jobs with the best and worst security based on unemployment rates. USA Today. March 6, 2019. https://www.usatoday.com/story/money/careers/2019/03/06/unemployment-rate-2019-occupations-best-worst-job-security/39124227/ Available at:
- 10.Frankel T., Roman T. Historic financial decline hits doctors, dentists and hospitals—despite covid-19—threatening overall economy. Washington Post, May 4, 2020. https://www.washingtonpost.com/business/2020/05/04/financial-distress-among-doctors-hospitals-despite-covid-19-weighs-heavily-economy/ Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.