Abstract
Bright light exposure is as one of the non-pharmacological measures to sleep management in shift-worker. This study was conducted to determine the effectiveness of bright light exposure in shift-worker nurses. We performed a systematic review and meta-analysis according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and using existing literature in the following databases: Cochrane Library, Embase, PubMed, Scopus, Web of Science, to examine any eligible and relevant interventional (randomized controlled trial, experimental and quasi-experimental studies) which were published by December 31, 2018. The obtained documents were analyzed using Stata 14.1 and Cochrane Collaboration's RevMan 5.3. Five studies met eligibility criteria. Results from fixed-effect meta-analysis of the included studies revealed that the exposure could decrease the sleepiness levels, complaints related to shift-work, insomnia and increased the psychomotor error (95% confidence interval (CI): -0.87,-0.43, p=0.000, I2=98.6%), alertness and daytime sleep duration following night shifts (95% CI: 0.08,0.99, p=0.000, I2=92.7%). However, in the random effects model, none of them were statistically significant. Although the results of fixed-effect are in favor of beneficial effects of bright light exposure in shift-worker nurses, the random effects could not approve these findings. Maybe because of either large heterogeneity or insufficiency of the number of studies. Besides, because of the low number of studies, it was impossible to deal with high amount of heterogeneity using subgroup analysis or meta-regression. So the controversy on this topic continues to persist, which highlights the need for more well-designed randomized control trials with larger sample sizes in the future.
Keywords: Sleep Initiation and Maintenance Disorders, Sleep Stages, Systematic Review, Nurse, Shift Work Schedule
INTRODUCTION
On average, one-third of the human lifetime is spent in sleep. Sleep and sufficient rest are one of the basic needs for human and the basis for physical and mental health, as the sleep deprivation can reduce people's productive behavior1. Shift-work is considered as a condition in which people work in times other than the usual time of work in an organization such as evening, night or a combination of these two that changes periodically. The night shift is considered as the hardest part of the shift-work that can interfere with the circadian and homeostatic regulation of sleep2-4. Almost 20-25% of the general population's work around the world is as the shift-worker. Shift-work as an occupational and safety hazard is common in jobs (protection services such as police, healthcare, and transport) that directly affect the health and safety of others. However, the health, quality of life and safety of shift-worker is affected by their job5-7.
The health of shift-worker who works non-standard hours is threatened by problems such as cardiovascular diseases, digestive problems, fatigue, cancer, especially breast cancer, peptic ulcer disease, type 2 diabetes, rheumatoid arthritis, anxiety, depression and sleep problems8-10. In fact, the sleep disorders is the most challenging issue among people with variable and circulating shift-work such as nurses. Nurses experience sleepiness and napping during shift-work and they are forced to devote many hours to sleep at home, in order to compensate for the sleep shortage and improve the quality of their sleep11-13.
Also, sleep disturbance and deprivation caused by shift-work can affect the cognitive performance, skills such as memory, learning, logical reasoning, mathematics calculation, recognition patterns, complex verbal processing and decision making of nurses that lead to increased risk of work injuries, decreased job performance and affects the outcome, health and safety of patients11,12,14,15. Although the experience of shift-work is inevitable in the nursing profession such as police and firemen; but having a high-quality sleep is considered as the primary rights of nurses and part of high-quality care chain of patients16.
For adaptation to shift-work as the significant need of nurses, there are pharmacological and non-pharmacological measures and solutions which shift-worker nurses can use to have better sleep management. However, studies have shown pharmaceutical solutions have the relative impact with numerous adverse effects5,17-20.
Bright light exposure was considered as one of the preventive and non-pharmacological measures that affects the melatonin secretion and helps the circadian rhythm adaptation and sleep management process in shift-workers. It can influence the biological clock, cognitive performance, and alertness21. The results of some studies suggest a beneficial effect of brief exposure to bright light for shift-worker nurse22-25. However, there is limited and scarce systematic review and meta-analysis studies that provide clear information about the effect of bright light exposure for shift-worker, especially nurses. This study is the first systematic review and meta-analysis which was conducted to determine the effectiveness of bright light exposure in shift-worker nurses until December 31, 2018.
MATERIAL AND METHODS
Selection criteria
Eligible studies: Included randomized controlled trial (RCT), experimental and quasi-experimental study designs and,
Eligible participants: Shift-worker nurses that work in the form of night shift or rotating shift and,
Eligible interventions: Effectiveness of bright light exposure that can be used with or without dark goggles and,
Eligible outcome measures: Studies that used bright light indicator included the sleep time, sleepiness level and performance and measured these items using valid scales and device (Shift-Work Complaints, Karolinska Sleepiness Scale, Insomnia Severity Index, Stanford Sleepiness Scale, Psychomotor Vigilance Test and nightcap device) were considered.
Search strategy and selection criteria
A systematic search of literature was conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement26 and using existing literature in the following databases: Embase, Cochrane Library, PubMed, Scopus, Web of Science, to examine any eligible and relevant interventional (randomized controlled trial (RCT), experimental and quasi-experimental studies) which were published until December 31, 2018. In this study, all the steps including search, identification, quality assessment, and data extraction were independently done by two reviewers and disagreements were solved through discussion and mutual agreement between authors. We searched the English language studies according to the following Medical Subject Heading (MeSH) terms and keywords ("nurses"[MeSH Terms] OR "nurses" OR "nurse") AND (shift-work OR ("shift work schedule"[MeSH Terms] OR ("shift" AND "work" AND "schedule") OR "shift work schedule" OR ("night" AND "shift" AND "work") OR "night shift work") OR ("shift work schedule"[MeSH Terms] OR ("shift" AND "work" AND "schedule") OR "shift work schedule" OR ("rotating" AND "shift" AND "work") OR "rotating shift work")) AND (bright AND ("light"[MeSH Terms] OR "light")) that investigated the effectiveness of bright light exposure in shift-worker nurses. All book chapters, systematic and literature reviews, anonymous studies, letters to the editor, historical articles were excluded (Figure 1).
Figure 1.
A flow diagram of included and excluded studies.
Evaluation of methodological quality
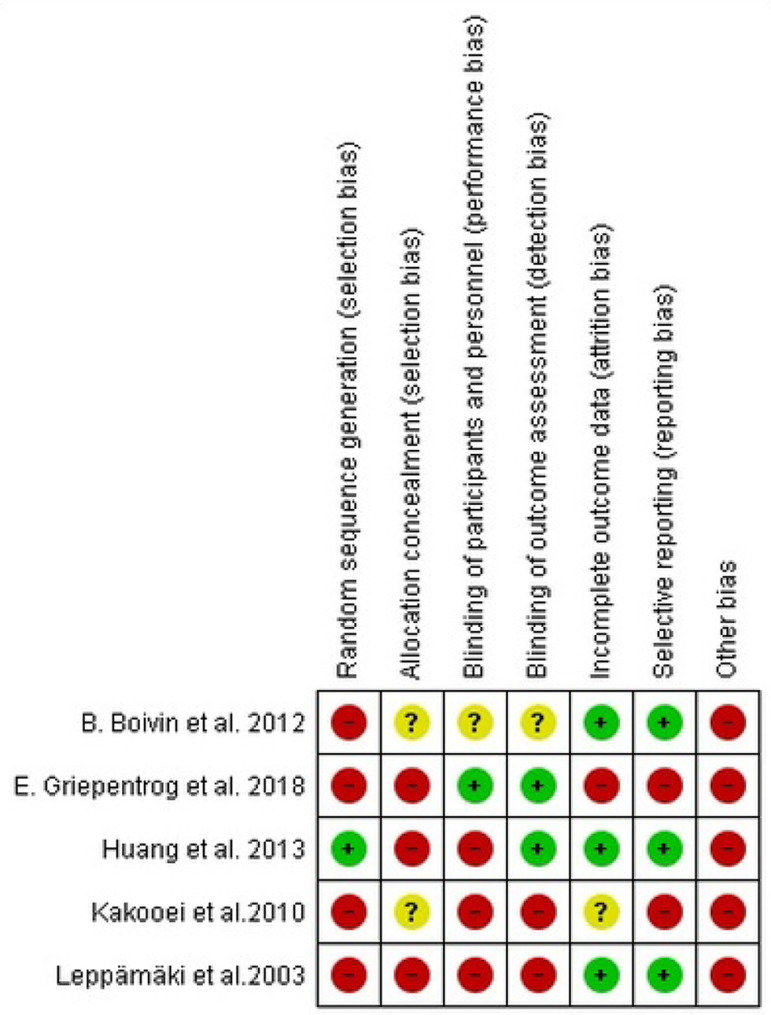
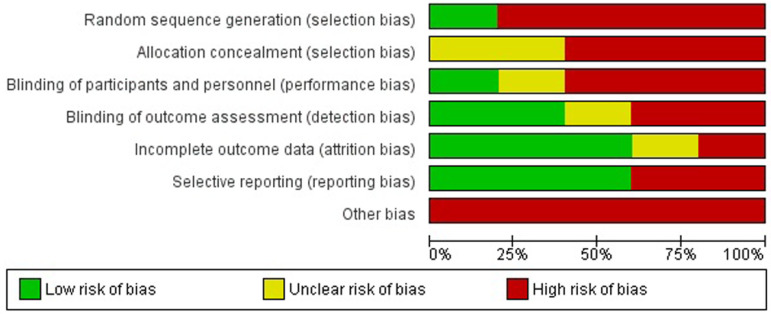
Two authors independently assessed the publication bias of the included studies by using the criteria of the Cochrane Handbook for Systematic Reviews of Interventions27 that evaluated: random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective reporting; and other bias. In this assessment, each item was graded as 'low', 'high' or 'unclear' risk of bias.
Data synthesis and statistical analysis
In this review, outcomes were presented as continuous variables. Because we have the outcome on different scales, the standard mean difference (SMD) was used for continuous variables and the degree of the treatment effects was determined by the magnitude of SMD28. We used the calculation of 95% confidence interval (CI) for each effect size estimate and the I-statistic (I2) to examine the heterogeneity among studies. Since I2 was greater than 50% and it indicated a notable heterogeneity29, we reported a fixed-effect model in addition to random effect model. A p-value <0.05 was considered to determine statistical significance. All statistical analyses were performed using Stata 14.1 and Review Manager, version 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark).
FINDING
Based on the exclusion and inclusion criteria, of 212 papers which were identified from the databases, five papers were included in this review. Search strategy outlines in Figure 1.
Characteristics of included articles
Of the five included papers, two papers had an RCT design22,24 and three papers were experimental design23,30,31. All the included studies presented in English language from 2003 to 2018 and were done in different geographical areas, including Asian, European countries and USA. Sample sizes of the reported studies ranged from 14 to 86. Different lux, time, duration and distance of bright light were used in the experimental groups. Two studies used the dark goggles during the morning commute home after bright light intervention24,31 (Table 1).
Table 1.
Characteristics of included studies into a meta-analysis.
| Author (year) country | Study design | Sample size | Questionnaire | Outcome | Intervention |
|---|---|---|---|---|---|
| Leppämäki et al. (2003)30 Finland | Experimental (before-after) | 86 | Shift-Work Complaints | Complaints related to shift work | Brief periods (4 × 20 minutes) of bright light (5000 lux) at scheduled times during every night shift over a 2-week period |
| Kakooei et al. (2010)23 Iran | Experimental (before-after) | 34 | Karolinska Sleepiness Scale | Alertness | Bright light (4500 lux) during 2 breaks (21:15-22:00 and 3:15-4:00) in night shift for 4 weeks |
| Boivin et al. (2012)31 USA | Experimental | 14 | Nightcap device | Daytime sleep following night shifts | Bright light (3243±2274 lux) during the first 6 h of each night shift and wore dark goggles during the morning commute home |
| Huang et al. (2013)24 Taiwan | RCT | 46 (in each group) | Insomnia Severity Index | Insomnia | Bright light (7,000-10,000 lux) for ≥ 30 minutes in night shift that continued for at least 10 days. Subjects avoided daytime outdoor sun exposure after work by wearing dark sunglasses |
| Griepentrog et al. (2018)22 USA | RCT (crossover clinical trial) | 43 (in each group) | 1. Stanford Sleepiness Scale 2. Psychomotor Vigilance Test |
1. Sleepiness 2. Number of lapses and errors |
Bright light (1500-2000 lx) for 10 h in night shift |
Quality appraisal
Based on the Cochrane Handbook for Systematic Reviews of Interventions, only one study reported sufficient methods in random sequence generation24 and none of these studies had reported an sufficient method of allocation concealment. Also, sufficient blinding of participants and personnel was reported in one study22, while the blinding of outcome assessment was reported in two studies22,24. So, there was a high number of missing data in one study that did not provide the reason22 and one study has insufficient reporting about incomplete outcome data23. Also, a high risk of selective reporting were presented in two included studies22,23 and all included studies have a reason for other risks. The details are shown in Figures 2 and 3.
Figure 2.
Risk of bias summary.
Figure 3.
Risk of bias graph.
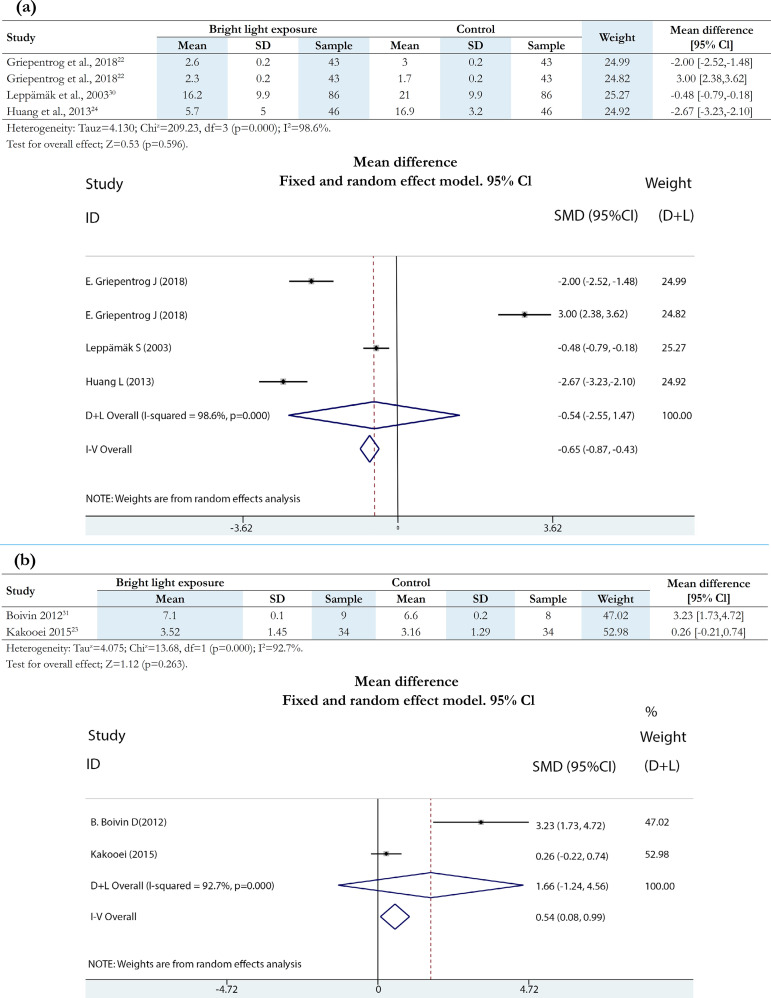
Effects of bright light exposure on the shift-worker nurses
Results from fixed-effect meta-analysis of the included studies showed that bright light exposure could decrease sleepiness levels22, complaints related to shift-work30 and insomnia24 in shift-worker nurses. Also, the results show that the psychomotor error increased in the intervention group than control group22 (SMD: -0.65, 95% CI: -0.87, -0.43, p=0.000, I2=98.6%) (Figure 4a).
Figure 4.
Forest plot for comparison of experimental versus control outcomes: (a) sleepiness levels, psychomotor error, complaints related to shift work and insomnia; (b) daytime sleep duration following night shifts and alertness. CI, confidence interval; SD, standard deviation.
Two studies reported that the bright light exposure could increase the alertness23 and daytime sleep duration following night shifts in shift-worker nurses31 (SMD: 0.54, 95% CI: 0.08, 0.99, p=0.000, I2=92.7%) (Figure 4b). However, in the random effects model, none of them were statistically significant.
DISCUSSION
Pooled data of this meta-analysis result provided the evidence that bright light exposure decreased the sleepiness levels, complaints related to shift-work and insomnia in shift-worker nurses. Also, these exposures increased the alertness, daytime sleep duration following night shifts and psychomotor error. We expected as the bright light exposure can decrease the sleepless level, the psychomotor error would also decrease in shift-worker nurses. But, author of the study claimed alertness and overall performance are degraded as the early morning approaches in diurnal creatures such as human which can increase the susceptibility to committing errors and reduce the work efficiency22.
Nursing is a difficult job and the shift-work is considered to be an integral part of this profession and as a stressor. The stress and pressure effects of shift-work condition on personal and social relationships, health habits and outcomes of nurses can reduce the available resources and capacity of them for coping with the other stressors and problems encountered in their job and family roles. Nurses need to learn and be educated in the shift-work coping strategies as a topic in their students' clinical education, in order to adapt and manage their sleep process in clinical settings and protect their mental and physical health7,32-34.
On the other hand, due to different shift-work systems in organizations, there is no single optimum solution for sleep management process of shift-worker nurses. Some preventive and compensatory non-pharmacological measures that are suggested in studies are: exposure to the bright light, napping, shift-worker participation in shift system design, correction of work conditions, education of managers and shift-workers, preventive health examination and medical check-up of shift-worker, non driving to and from work, familial and social support, possibility to rest and sleep before, during (nap) and after shifts at home, use of appropriate nutrition and improved physical fitness, lifestyle training, cognitive and behavioral interventions (exercise, optimal timing to rest breaks at work, social activities during breaks, sensory stimulation) and consideration of chronotype pattern of person. Nurses can use these strategies according to their conditions and discretion7,35,36.
According to our knowledge, this is the first systematic review evaluating the effects of bright light exposure in shift-worker nurses. Because shift-work in addition to sleep, can affect many aspects of the nurse's performance; many scales and tools have been used to test the treatment effect of bright light exposure in review studies. In this review, direct comparisons across interventions or amongst outcomes is difficult, because there is a different pattern of bright light exposure with regards to timing, duration, frequency, and intensity.
Also, our study has other limitations. First, due to the small number and low quality of the available RCTs, our meta-analysis results were limited. Second, our review was limited to English language studies. Third, the data identified via five main databases and maybe some of the related articles were not indexed on these five databases. Besides, some databases were not available to us such as CINAHL Nursing Journal Databases.
Although the results of fixed-effect are in favor of beneficial effects of bright light exposure in shift-worker nurses, the random effects could not approve these findings. Perhaps because of either large heterogeneity or insufficiency of the number of studies. Moreover, because of the low number of studies, it was impossible to deal with high amount of heterogeneity using subgroup analysis or meta-regression. On the other hand, the existence of clinical heterogeneity in studies such as the different baseline of selected shift-worker nurses, the different pattern of bright light with regards to timing, frequency, duration and intensity, might be affected the result.
CONCLUSION
The results of our systematic review and meta-analysis suggested that bright light exposure may help shift-worker nurses learn better sleep management by decrease in the sleepiness levels, complaints related to shift-work, insomnia and increase in the alertness and daytime sleep duration following night shift. So the controversy on this topic continues to persist, which highlights the need for more well-designed randomized control trials with larger sample sizes to assess the non-pharmacological intervention such as bright light exposure in shift-worker nurses in the future.
Also, assess the safety of bright light exposure in shift-worker nurses is considered an important issue. It may be side-effects such as a headache, concomitant nausea, and irritation of the eye30 for nurses that should be taken into account in future studies.
ACKNOWLEDGMENT
This review is a part of the PhD thesis of Seyedeh Zahra Aemmi and authors would like to thank the Nursing Care Research Center in Chronic Diseases, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran for financial support (Grant No. NCRCCD-9601).
REFERENCES
- 1.Razmpa E, Ghaffarpour M, Sadeghniiat Haghighi K, Ghelichnia H, Ghobaei M, Rezaei N, et al. Sleep disorders and its risk factors in nurses. Occup Med J. 2009;1(1):20–23. [Google Scholar]
- 2.Pati AK, Chandrawanshi A, Reinberg A. Shift work: consequences and management. Curr Sci. 2001;81(1):32–52. [Google Scholar]
- 3.Akerstedt T, Wright Jr KP. Sleep Loss and Fatigue in Shift Work and Shift Work Disorder. Sleep Med Clin. 2009;4(2):257–271. doi: 10.1016/j.jsmc.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fadeyi BA, Ayoka AO, Fawale MB, Alabi QK, Oluwadaisi AM, Omole JG. Prevalence, predictors and effects of shift work sleep disorder among nurses in a Nigerian teaching hospital. Sleep Sci Pract. 2018;2:6–6. [Google Scholar]
- 5.Flo E, Pallesen S, Magerøy N, Moen BE, Grønli J, Hilde Nordhus I, et al. Shift work disorder in nurses--assessment, prevalence and related health problems. PLoS One. 2012;7(4):e33981. doi: 10.1371/journal.pone.0033981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kilpatrick K, Lavoie-Tremblay M. Shiftwork: what health care managers need to know. Health Care Manag (Frederick) 2006;25(2):160–166. doi: 10.1097/00126450-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Richter K, Acker J, Adam S, Niklewski G. Prevention of fatigue and insomnia in shift workers-a review of non-pharmacological measures. EPMA J. 2016;7:16–16. doi: 10.1186/s13167-016-0064-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eldevik MF, Flo E, Moen BE, Pallesen S, Bjorvatn B. Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLoS One. 2013;8(8):e70882. doi: 10.1371/journal.pone.0070882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson JL. The impact of shift patterns on healthcare professionals. J Nurs Manag. 2002;10(4):211–219. doi: 10.1046/j.1365-2834.2002.00308.x. [DOI] [PubMed] [Google Scholar]
- 10.Hughes V. Leadership strategies to reduce risks for nurse night shift workers. J Nurs Health Care. 2015;3(1):128–137. [Google Scholar]
- 11.Salehi K, Alhani F, Sadegh-Niat K, Mahmoudifar Y, Rouhi N. Quality of Sleep and Related Factors among Imam Khomeini Hospital Staff Nurses. Iran J Nurs. 2010;23(63):18–25. [Google Scholar]
- 12.Øyane NM, Pallesen S, Moen BE, Akerstedt T, Bjorvatn B. Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One. 2013;8(8):e70228. doi: 10.1371/journal.pone.0070228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saleh AM, Awadalla NJ, El-masri YM, Sleem WF. Impacts of nurses' circadian rhythm sleep disorders, fatigue, and depression on medication administration errors. Egypt J Chest Dis Tuberc. 2014;63(1):145–153. [Google Scholar]
- 14.Bagheri H, Shahabi Z, Ebrahimi H, Alaeenejad F. The association between quality of sleep and health-related quality of life in nurses. Hayat. 2007;12(4):13–20. [Google Scholar]
- 15.Rhéaume A, Mullen J. The impact of long work hours and shift work on cognitive errors in nurses. J Nurs Manag. 2018;26(1):26–32. doi: 10.1111/jonm.12513. [DOI] [PubMed] [Google Scholar]
- 16.Chan MF. Factors associated with perceived sleep quality of nurses working on rotating shifts. J Clin Nurs. 2009;18(2):285–293. doi: 10.1111/j.1365-2702.2008.02583.x. [DOI] [PubMed] [Google Scholar]
- 17.Asadzandi M, Sayari R, Sanayinasab H, Ebadi A, Rahmati NF, Chavoshi F. Sleep disorders in military nurses. J Pol Med. 2014;3(3):149–158. [Google Scholar]
- 18.Rajaratnam SM, Howard ME, Grunstein RR. Sleep loss and circadian disruption in shift work: health burden and management. Med J Aust. 2013;199(8):S11–S15. doi: 10.5694/mja13.10561. [DOI] [PubMed] [Google Scholar]
- 19.Czeisler CA, Walsh JK, Roth T, Hughes RJ, Wright KP, Kingsbury L, et al. U.S. Modafinil in Shift Work Sleep Disorder Study Group Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med. 2005;353(5):476–486. doi: 10.1056/NEJMoa041292. [DOI] [PubMed] [Google Scholar]
- 20.West SH, Ahern M, Byrnes M, Kwanten L. New graduate nurses adaptation to shift work: can we help? Collegian. 2007;14(1):23–30. doi: 10.1016/s1322-7696(08)60544-2. [DOI] [PubMed] [Google Scholar]
- 21.Simons KS, Boeijen ERK, Mertens MC, Rood P, de Jager CPC, van den Boogaard M. Effect of Dynamic Light Application on Cognitive Performance and Well-being of Intensive Care Nurses. Am J Crit Care. 2018;27(3):245–248. doi: 10.4037/ajcc2018908. [DOI] [PubMed] [Google Scholar]
- 22.Griepentrog JE, Labiner HE, Gunn SR, Rosengart MR. Bright environmental light improves the sleepiness of nightshift ICU nurses. Crit Care. 2018;22(1):295–295. doi: 10.1186/s13054-018-2233-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kakooei H, Zamanian Ardakani Z, Ayattollahi MT, Karimian M, Nasl Saraji G, Owji AA. The effect of bright light on physiological circadian rhythms and subjective alertness of shift work nurses in Iran. Int J Occup Saf Ergon. 2010;16(4):477–485. doi: 10.1080/10803548.2010.11076860. [DOI] [PubMed] [Google Scholar]
- 24.Huang LB, Tsai MC, Chen CY, Hsu SC. The effectiveness of light/dark exposure to treat insomnia in female nurses undertaking shift work during the evening/night shift. J Clin Sleep Med. 2013;9(7):641–646. doi: 10.5664/jcsm.2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tanaka K, Takahashi M, Tanaka M, Takanao T, Nishinoue N, Kaku A, et al. Brief morning exposure to bright light improves subjective symptoms and performance in nurses with rapidly rotating shifts. J Occup Health. 2011;53(4):258–266. doi: 10.1539/joh.l10118. [DOI] [PubMed] [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 27.Tarsilla M. Cochrane Handbook for Systematic Reviews of Interventions. J Multidiscip Eval. 2008;6(14):142–148. [Google Scholar]
- 28.Faraone SV. Interpreting estimates of treatment effects: implications for managed care. P T. 2008;33(12):700–711. [PMC free article] [PubMed] [Google Scholar]
- 29.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Hoboken: John Wiley & Sons; 2011. [Google Scholar]
- 30.Leppämäki S, Partonen T, Piiroinen P, Haukka J, Lönnqvist J. Timed bright-light exposure and complaints related to shift work among women. Scand J Work Environ Health. 2003;29(1):22–26. doi: 10.5271/sjweh.700. [DOI] [PubMed] [Google Scholar]
- 31.Boivin DB, Boudreau P, James FO, Kin NM. Photic resetting in night-shift work: impact on nurses' sleep. Chronobiol Int. 2012;29(5):619–628. doi: 10.3109/07420528.2012.675257. [DOI] [PubMed] [Google Scholar]
- 32.Nasrabadi A, Seif H, Latifi M, Rasoolzadeh N, Emami A. Night shift work experiences among Iranian nurses: a qualitative study. Int Nurs Rev. 2009;56(4):498–503. doi: 10.1111/j.1466-7657.2009.00747.x. [DOI] [PubMed] [Google Scholar]
- 33.Clissold G, Smith P. A study of female nurses combining partner and parent roles with working a continuous threeshift roster: The impact on sleep, fatigue and stress. Contemp Nurse. 2002;12(3):294–302. doi: 10.5172/conu.12.3.294. [DOI] [PubMed] [Google Scholar]
- 34.Novak RD, Auvil-Novak SE. Focus group evaluation of night nurse shiftwork difficulties and coping strategies. Chronobiol Int. 1996;13(6):457–463. doi: 10.3109/07420529609020916. [DOI] [PubMed] [Google Scholar]
- 35.Knauth P, Hornberger S. Preventive and compensatory measures for shift workers. Occup Med (Lond) 2003;53(2):109–116. doi: 10.1093/occmed/kqg049. [DOI] [PubMed] [Google Scholar]
- 36.Neil-Sztramko SE, Pahwa M, Demers PA, Gotay CC. Health-related interventions among night shift workers: a critical review of the literature. Scand J Work Environ Health. 2014;40(6):543–556. doi: 10.5271/sjweh.3445. [DOI] [PubMed] [Google Scholar]