Abstract
Introduction: Community-based direct observed treatment (DOT) providers are an important bridge for the national tuberculosis programme in India to reach the unreached. The present study has explored the knowledge, attitude, practice and barriers perceived by the community-based DOT providers.
Methods: Mixed–methods study design was used among 41 community-based DOT providers (Accredited Social Health Activist (ASHAs)) working in 67 villages from a primary health center in Raisen district of Madhya Pradesh, India. The cross-sectional quantitative component assessed the knowledge and practices and three focus-group discussions explored the attitude and perceived barriers related to DOT provision.
Result: ‘Adequate knowledge’ and ‘satisfactory practice’ related to DOT provision was seen in 14 (34%) and 13 (32%) ASHAs respectively. Only two (5%) received any amount of honorarium for completion of DOT in last 3 years. The focus-group discussions revealed unfavourable attitude; inadequate training and supervision, non-payment of honorarium, issues related to assured services after referral and patient related factors as the barriers to satisfactory practice of DOT.
Conclusion: Study revealed inadequate knowledge and unsatisfactory practice related to DOT provision among ASHAs. Innovations addressing the perceived barriers to improve practice of DOT provision by ASHAs are urgently required.
Keywords: Directly observed therapy, Community-health workers, Perceived barriers, Operational research, Mixed-method study
1. Introduction
Despite many serious and organized efforts worldwide, TB remains one of the major public health concerns more so in South-East Asia and African countries [1,2]. Of the estimated global annual incidence of 10.4 million TB cases, 2.8 million (27%) were estimated to have occurred in India [1]. In 2013, 53% got registered for treatment, 45% completed treatment and 39% achieved the optimal outcome of one year recurrence free survival [3]. This attrition in TB cascade of care in India is unacceptably high because, with timely diagnosis and correct treatment, almost all people with TB can be cured [4]. India has attained the Millennium Development Goals (MDGs) targets for TB; but a lot has to be done if we are to meet the year 2030 targets of Sustainable Development Goals (SDGs) and year 2035 targets of the End TB strategy [5,6].
The Revised National Tuberculosis Control Programme (RNTCP) in India, based on the direct observed treatment short course (DOTS) strategy, recommends the decentralization of DOTS beyond the primary health care facility [7]. The DOT providers are the community-health workers whose involvement and active participation is crucial along with Designated Microscopic Centres (DMCs) and DOT centres for the success of programme [8–10]. One of the main challenges of RNTCP has been that it has not been able to ‘reach the last mile’ i.e. its inaccessibility to underprivileged, rural and tribal communities [11].
The Government of India launched the National Rural Health Mission in 2005 to reduce in equity in health care and improve availability and accessibility to health services in public health facilities. Around half million community-health workers were appointed on voluntary basis, one per thousand populations (≈one village) and were called as Accredited Social Health Activist (ASHA). Though appointed as a volunteer, they get outcome-based remuneration [12]. In various parts of India, the responsibility of DOT provision was delegated to ASHAs.
Worldwide, qualitative studies have been done to study the patient perspective while on DOTS [13–19]. Qualitative studies involving DOT providers have been few and far between and identified that cash incentives are required and there is a need to address the barriers at the level of DOT provider [8,20–23]. There is lack of qualitative studies from Central India involving DOT providers, especially ASHAs in rural setting. We have also found treatment interruptions and default during DOT provision by ASHA in the region [24]. Therefore, we planned a mixed-method study to explore the knowledge, attitude, practice and perceived barriers related to DOT provision among the village-level DOT providers (role performed by ASHAs) in rural and tribal central India.
2. Material and methods
2.1. Study design
It was a mixed-method study (explanatory design) [25] where the quantitative data collection (phase I – cross sectional study for the assessment of adequate knowledge and satisfactory practices related to DOT provision) was followed by qualitative data collection (phase II – Focus Group Discussion to explore the attitude and perceived barriers related to DOT provision). Findings from former fed into latter [25].
2.2. Study setting
2.2.1. General setting
Madhya Pradesh is the second largest state and is situated in central India. Raisen district is situated approximately 100 km to the east of Bhopal, the capital of Madhya Pradesh. It has a population of 1.4 million is predominantly rural [26]. RNTCP infrastructure includes one District TB Centre (DTC), 4 sub-district level programme management units (Tuberculosis Units – TU) and 15 designated microscopic centres (DMCs) for sputum acid fast bacilli examination. In programme, one TB Health visitor (TB HV) is recommended for every DMC for initial home visits of patients, facilitation of diagnosis and treatment; record keeping, and supervision of DOT providers. However for DTC Raisen, only 2TB HVs are currently working. Senior Treatment Supervisors (STS) at TU level are responsible for registration and tracking the patient till treatment completion.
2.2.2. Specific setting
This study was conducted at a non-DMC Primary Health Center (PHC Chiklod), in Raisen district of Madhya Pradesh, India. It is predominantly a rural habitat, caters a population of approximately 38,000 in 67 villages. The villages are scattered and population is mostly hilly and tribal. The PHC has four health sub centres. The distance of nearest DMC is approximately 30 km from the PHC. This DMC is one of the 5 operational DMCs of Raisen TU. The number of registered TB patients under RNTCP year 2012, 2013 and 2014 were 17, 24 and 25 respectively in Chiklod PHC.
2.3. Study population and period
All ASHAs working as DOT providers in villages of PHC Chiklod between 1st January 2015 and 30th September 2015 were the study population. There are a total of 47 ASHAs in 67 villages of PHC; some ASHAs have more than one village under them and all are working as DOT providers in the PHC.
2.4. Data collection method and tool
2.4.1. Quantitative data collection (Phase I)
Data collection was done during October to November 2015. A sampling frame was generated by identifying all 46 ASHAs working as a DOT provider as per records of PHC Chiklod. All were invited to participate after explaining them the purpose of the study. Place of interview was decided as per their convenience, after telephonic conversation; it was either their village or at the PHC. At least, 2 attempts were made to interview every ASHA before excluding them from the study. Those who were willing to participate were interviewed through a rater-administered mobile-based pretested questionnaire (Annexure 1&2).
2.4.2. Qualitative data collection (Phase II)
Focus group discussions (FGDs) with ASHAs were conducted at the PHC in December 2015. We were flexible in deciding the number of FGDs (n = 3); till the saturation and as per the feasibility. The principal investigator (ARS) who is a trained in qualitative research methods conducted the FGDs. ASHAs who were willing, vocal and available to participate were purposively selected for the study. FGDs were done at the date and time convenient to participants. Participants were informed of the purpose of the study. An FGD guide with broad open ended questions was prepared, pilot-tested and used to conduct the FGDs. Results of phase I fed into the development of FGD guide (Annexure 3). Video recording (after consent) and verbatim notes were taken. Verbatim notes were taken by one medical social service officer and another drew the sociogram [27]. The duration of the FGDs ranged from 35 to 45 min. Transcription was done on the same day by the PI (ARS). Field notes from observations during were also made.
2.5. Analysis and statistics
2.5.1. Quantitative data analysis (Phase I)
Data collection and entry were combined into a single step using mobile-based technology [28]. Data was extracted in excel file and analysed using EpiData software (EpiData version 2.2.2.183 for analysis, EpiData Association, Odense, Denmark) and STATA (version 12.1 STATA Corp., College Station, TX, USA).
Key analytic output was number (proportion) of ASHAs with adequate knowledge and practice. The study variables related to knowledge level of ASHAs were assessed through the pretested and predesigned questionnaire containing set of 12 questions related to their role and responsibility in RNTCP setting. The responses were submitted as correct and incorrect only, missing values were categorised as incorrect responses. “Adequate knowledge” was defined as those who answered at-least 6 out of 12 questions correctly. Practice was considered satisfactory if the ASHA completed DOT for at-least one patient in last 3 years.
2.5.2. Qualitative data analysis (Phase II)
The transcripts obtained were compiled and the PI (ARS) read the transcripts to become familiar with the data. Manual descriptive content analysis was used by the PI to analyse the transcripts [29]. It was reviewed by a second investigator (AP) to reduce bias and interpretive credibility. The decision on coding rules and theme generation was done by using standard procedures and in consensus. Any difference between the two was resolved by discussion. Both inductive and deductive codes were generated. Similar codes were combined into themes. To ensure that the results are a reflection of the data, the codes/themes were related back to the original data. The themes were described and complete, de-identified representative statements were included in the results to illustrate the themes. The final results arising after qualitative data analysis was shared with the stakeholders for their feedback and approval.
2.6. Ethics approval
ASHAs were interviewed after explaining the objectives of the study and obtaining written informed consent in local language (Hindi). For qualitative part, verbal consent was taken from all the study participants for FGD and video recording. The study including the consent process was approved by the Institutional Ethics Committee of the All India Institute of Medical Sciences, Bhopal, India. Programmatic approval was also obtained before starting the study.
3. Results
3.1. Quantitative component (Phase I)
Among 47 ASHAs working in PHC Chiklod, we could interview 41. Six ASHAs couldn’t be interviewed because of their non-availability, despite of our two attempts to contact them. Mean (SD) age of ASHAs was 31 years (4.4), thirty (73%) were educated up to 10th grade or less and 34 (83%) worked for more than 3 years in their respective villages. Twenty-three (56%) ASHAs attended any training related to RNTCP in past 3 years. The nearest DMC from most of the villages (80%) was more than 20 km away.
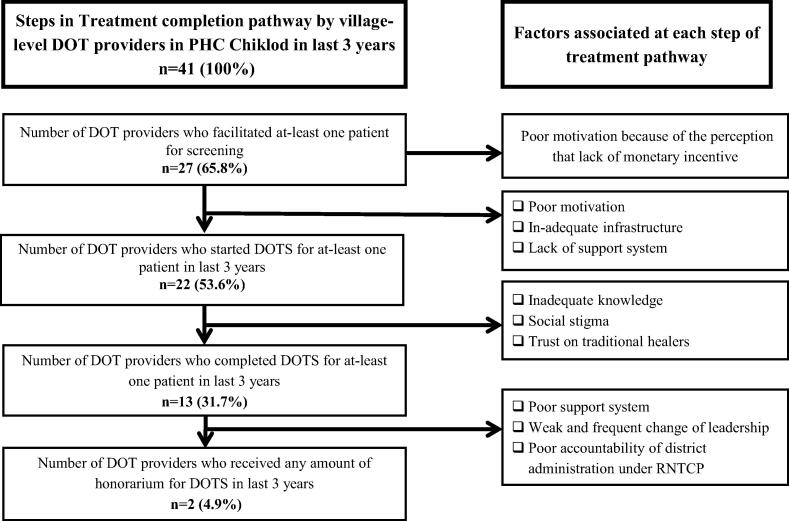
‘Adequate knowledge’ related to DOT provision was found in 14 (34%) ASHAs. The Chronbach’s alpha coefficient was 0.784 for these twelve items under knowledge. Maximum correct response was obtained for the item “duration of category-1 treatment” (75.6%) and minimum correct response was obtained for the item “awareness about MDR TB” (12%). Satisfactory practice (successful completion of DOT in last previous three years) was reported by 13 (32%) ASHAs: among them two (5%) received honorarium for completion of DOT (Table 1) (Fig. 1).
Table 1.
Knowledge and practice related to DOT provision among village-level DOT providers in PHC Chiklod, Madhya Pradesh, India (2015).
| Variables | Adequate/Satisfactory (%) |
|---|---|
| Total | 41 (100) |
| Knowledge related to DOT provision | |
| Categories of DOTS | 27 (66) |
| Duration of Cat 1 treatment | 31 (76) |
| Follow up sputum examination in cat 1 treatment | 19 (46) |
| Duration of Cat 2 treatment | 12 (29) |
| Follow up sputum examination in cat 2 treatment | 8 (20) |
| Duration till sputum should be done after the completion of treatment | 16 (39) |
| Aware about ‘Nikshay’ entry of registered patients | 11 (27) |
| Aware about side effect of DOTS | 10 (24) |
| Aware about INH chemoprophylaxis to HH contacts | 9 (22) |
| Aware about MDR TB | 5 (12) |
| Aware about honorarium of Cat 1 treatment | 12 (29) |
| Aware about honorarium of Cat 2 treatment | 9 (22) |
| ASHAs who answered ‘at least’ 6 out 12 questions correctly | 14 (34) |
| Practices related to DOTS provision (At-least one in last 3 years) | |
| ‘At least’ one patients facilitated for screening in last 3 years | 27 (66) |
| ‘At least’ one patient initiated on DOT in last 3 years | 22 (54) |
| ‘At least’ one patient completed DOT in last 3 years | 13 (32) |
| ‘At least’ one patient in your village currently taking non-DOT | 7 (17) |
| Perceive problem in filling RNTCP# form while DOT | 22 (53) |
| Received honorarium for DOT completion for ‘at least’ one patient | 2 (5) |
Cat – Category; DOT – Directly observed treatment;
RNTCP – Revised National Tuberculosis Control Programme; PHC – Primary Health Center.
Fig. 1.
Flow diagram for treatment pathways for patients with TB facilitated by ASHA Workers of PHC Chiklod, Madhya Pradesh, India (2015). DOTS: Directly observed treatment short course chemotherapy, PHC: Primary Health Center, RNTCP: Revised National Tuberculosis Control Programme.
Distance of village from nearest DMC (>20 km) was associated with ‘unsatisfactory practice’, however after adjusting for other potential confounder the association was not significant (data not shown).
3.2. Qualitative component (Phase II)
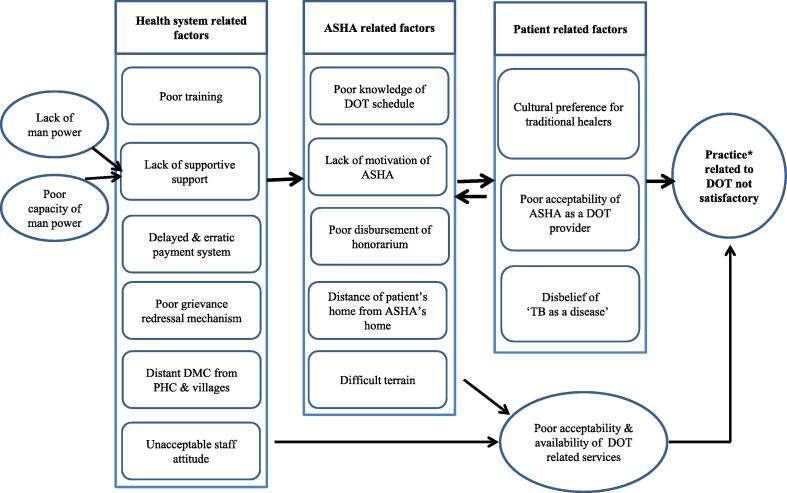
The themes that emerged following the analysis of transcripts and field notes are summarised in Fig. 2.
Fig. 2.
Perceived challenges by the ASHA workers of PHC Chiklod, Madhya Pradesh, India (2015), ASHA: Accredited Social Health Activist performing the role of village-level DOT provider, DOTS: Directly observed treatment short course chemotherapy, PHC: Primary Health Center, RNTCP: Revised National Tuberculosis Control Programme, DMC: Designated Microscopy Center, *Unsatisfactory practice: If the ASHA did not completed DOT for at-least one patient in last 3 years.
Overall the attitude of DOT providers towards DOT provision was unfavourable. Five themes emerged out clearly for perceived barriers of DOT providers for non-satisfactory implementation of DOTS i.e. poor payment system, poor capacity for DOT provision, generic RNTCP issues, difficult terrain and patient related factors (Fig. 1).
3.2.1. Poor payment system
It was perceived as the main barrier. In some instances there was a delay in disbursement of honorarium. A 26 year old DOTS provider working for 5 years told
“During the meeting, they talk about targets of patients for sputum examination but nobody talks about due payment. Since January we didn’t get any payment [That includes TB related honorarium also] now they don’t ask for meeting even [sic]”
.
In other instances there was irregular payment without accountability of health system, as reflected by the another quote
“Our payment should be regular and prompt like in JSY (Janani Suraksha Yojana: A Incentive-based maternal and child health programme) [sic]”
There was also a lack of knowledge among ASHAs of the criteria to be fulfilled so that they can get honorarium. This led to failure in getting incentives even though they completed the DOT. A 22 year old ASHA told
“We are not sure how many times patient have to go for sputum examination during the whole treatment and at the end of treatment [sic]”
3.2.2. Poor capacity for DOT provision
Similar to quantitative findings, poor knowledge related to TB was observed. One of the ASHA mentioned
“Mainly it [TB disease] spread through coughing but when the disease is severe at the start (of disease), it can spread through sharing of food, talking very closely and even with the sexual contact with the patients [sic].”
The ASHAs did not feel comfortable enough to discharge their responsibilities related to DOT provision. Infrequent and inadequate training was stated as one of the reasons. As suggested by an ASHA of 32 years age and work experience of 7 years.
“We didn’t received any sort of training related to TB in last four or five years [sic]”
Language barrier in filling TB treatment card was one of the reasons. The RNTCP treatment card was written in English, and the first language of DOT providers was not English so they found filling up forms very difficult as stated by a DOT provider
“Card is written in English, so we feel difficulty while filling it and nobody in training has taught us properly. However we tick the boxes after giving the treatment to patient but not sure about the other parts of cards. There has to be somebody who can support us, teach us in Hindi (local language understood by DOT providers) [sic]”
The ASHAs perceived apathy from the health system and felt health care providers (doctors and other paramedical staff related to RNTCP) didn’t support them enough, as reflected by the following quote:
“Doctor (Medical Officers) should supervise and help us during the DOT [sic].”
.
“The DMC (Designated Microscopic Center) staff should behave politely and co-operate with patients as well as with us [sic].”
.
3.2.3. Generic RNTCP issues
These were lack of coordinated assured service delivery on referral of the patients (including closure of DMC at 1300 h), poor supervision by RNTCP staff, no home visit by TB HVs and STS, very few patient provider and community participation meetings and frequent change of leadership in district related to TB programme. One of the ASHAs mentioned this:
“DMC is located at Obedullaganj (30 km away from PHC). Many times staff of DMC don’t behave well with the patient we send, either they don’t collect the sample after 1.00PM–2.00PM or ask the patient to come on next day with two samples which patient feel very uncomfortable. Most of the time patients were not communicated properly for what they are being suspected of? And how will they be investigated for it? So they remain reluctant to visit DMC again [sic]”
.
3.2.4. Difficult terrain
As the PHC had hilly & sparse terrain; people lived in small hamlets so a single ASHA had to cover more than one village/hamlet that made her job even more difficult. In addition, there was poor public transport system that also discouraged both the paramedical workers to reach to the patients and patient to access TB related services from programme.
3.2.5. Patient related factors
Due to poor accessibility of health system for TB related services, lack of awareness, poor education had compelled the patients to seek services from traditional healers. Due to stigma or confidentiality related issues, patient was also reluctant to reveal their TB status in community, so they preferred not to seek care from health system but from traditional healers as reflected by the following quote form a ASHA:
“Patients do not want to reveal their disease status publicly so they prefer the traditional healers for treatment so many times disease get worst. Patient also feels DOT is less effective because it is available for free [sic]”
4. Discussion
This mixed-method research found that less than one-third of ASHAs had adequate knowledge and satisfactory practices related to DOT provision. Qualitative findings suggested unfavourable attitude of ASHAs; inadequate training and supervision of ASHAs, non-payment of honorarium, issues related to assured services once referred to DMC; and patient related factors as the main barriers to satisfactory practice of DOT provision.
Most of the ASHAs were young, still majority of them had experience of more than 3 years for working in the community and could prove as an asset for the programme. ASHAs as community-health workers in RNTCP have a huge potential, as they have done in improving maternal and child health services after launch of NRHM in the country [30]. The onus is on health system to utilize them as a dividend to fulfil the goal of reaching the unreached [11]. ASHAs are village-level DOT providers staying in the same village/hamlet nearby village/hamlet. Despite this, their practice of DOT provision was not satisfactory; around half of the ASHAs had started DOTS for at-least one patient, only one-third of them managed to complete the treatment. The reasons for this unsatisfactory practice for DOT provision among ASHAs are complex and intermingled with health system related factors, ASHA related factors & patient related factors (Fig. 2). However, if we delineate these factors further, there seems to be following reasons for this.
First, there was a serious knowledge-gap that existed. The main reasons of this were the lack of training and poor support system by programme staff. Due to this inadequate knowledge, ASHAs might be unequipped to answer questions raised by the patient related to the erroneous belief about their disease and treatment [31,32]. This knowledge gap was consistent with the various studies in various other developing countries [20,33–35].
Second, there were serious issues related to payment of output linked honorarium. Only two ASHAs received any amount of honorarium for successful completion of DOT in last 3 years. Many ASHAs were neither aware about these preconditions nor were properly told by the support staff of the programme. ASHAs were not convinced with the payment system for DOT. Only few ASHAs were correctly aware about Category I and Category II honorarium for successful completion of DOT. DOT allowance had some incentive effect on DOT providers, but its extent may be circumscribed by the small amount and operational problems [21].
Third, issues related to accessibility of TB services, lack of assured service on visiting the DMC, compounded with faith of patients in traditional healers made matter worse. Like a study from Africa, this study also suggests that distance of villages or hamlets from the public health institution is a barrier for accessibility of health services related to treatment of TB [36]. Some patients were not willing to take treatment from ASHAs due to issues related to acceptability of her as a DOT provider.
4.1. Implications for policy and practice
Based on the findings of our study, we suggest some policy and practice related recommendations. First, regular and hands-on training of community-health workers will eventually empower them for efficient counselling and education of patients with TB.
Second, fixing the issues related to payment of honorariums need to be sorted out. The pre-conditions for disbursement of the honorarium must be reinforced among ASHAs. The accountability of existing man power has to be fixed; and grievance redressal mechanism related to payment system is an essential component in an order to motivate the DOT providers.
Third, raising DOT allowance and removing existing barriers to DOTS provision might result in a greater motivational impact, particularly in resource constraint setting, where community-health workers like ASHAs are more likely to encounter financial and other obstacles in delivering DOT services in rural areas. Innovative measures like sputum collection and transport for follow up sputum examination through the support of non-governmental organization working in the area could address issues related to accessibility and lack of assured service delivery post referral.
Fourth, for villages where there are issues related to acceptability of ASHAs as DOT providers or in hilly, hard to reach terrain, the programme needs to be flexible in its approach. Mobile DOT provider through the support of non-governmental organizations, where the mobile DOT provider were asked to take daily videos of the patient swallowing their medications or take real time thumb impression of patients on hand held devices may prove to be a feasible solution [37]. The community participation has to be ensured through involving non-governmental organizations, community meeting at-least once in a month and by involving traditional healers/private practitioners in the RNTCP.
4.2. Strengths and limitations
The study had several strengths. First, community-based mixed-method study design was used which not only quantified the magnitude of the problem, but also provided insights into the reasons for the problem, thus providing holistic overview. Second, we conducted the study in programmatic settings of central India, thus reflecting the realities on the ground. Third, we used internationally accepted guidelines for reporting the quantitative and qualitative parts of the study [38,39].
There were also few limitations in the study. For the quantitative part, the sample size was small. Given that only DOT providers of a given PHC were chosen as a study subjects, this study might not be the true representative of the whole area/district but we have reasons to believe that the situation in this region may not be very different from the present study [24]. We did not explore the perception of DOT providers about the traditional healers in detail. The possibility of observer bias cannot be completely ruled out. The perception of district health authorities related to RNTCP was also not included.
5. Conclusion
A mixed method study among village-level DOT providers in central India identified inadequate knowledge and unsatisfactory practice related to DOT provision. Innovations addressing the barriers to improve practice of DOT provision by ASHAs are urgently required in an order to make it accessible for unreached area i.e. underprivileged and tribal communities.
Acknowledgements
The authors wish to thank Dr Bhavna Benjamin, Dr Ragini Jain and other staff of PHC Chiklod, district Raisen, Madhya Pradesh for their support during the study. Authors are also thankful for Mrs Manuradha Dahiya and Mr Ajeet Singh Chandel both working as Medical Social Service Officer, Department of Community and Family Medicine, All India Institute of Medical Sciences, Bhopal for their support during data collection. We thank the Department for International Development (DFID), UK, for funding the Global Operational Research Fellowship Programme in which HDS works as a Senior Operational Research Fellow.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jegh.2017.07.002.
Footnotes
Peer review under responsibility of Ministry of Health, Saudi Arabia.
Funding
The study was conducted as an operational research under the programme conditions using programme staff. Therefore, no separate budget was required.
Availability of data and materials
The dataset(s) supporting the conclusions of this article are available on request from the corresponding author.
Conflict of interest
The authors declare no competing interest.
References
- [1].World Health Organization . Global Actions And Investments Fall Far Short Of Those Needed To End The Global Tb Epidemic. Geneva: World Health Organization; 2016. Global Tuberculosis Report [Internet] Available from: http://www.who.int/tb/publications/global_report/gtbr2016_executive_summary.pdf?ua=1. [Google Scholar]
- [2].World Health Organization . Tuberculosis Control in South-East Asia Region: Annual TB report 2015 [Internet] Geneva: Regional Office for South-East Asia, World Health Organization; 2015. p. 6. Available from: http://www.searo.who.int/tb/annual-tb-report-2015.pdf. [Google Scholar]
- [3].Subbaraman R, Nathavitharana RR, Satyanarayana S, Pai M, Thomas BE, Chadha VK, et al. The tuberculosis cascade of care in india’s public sector: a systematic review and meta-analysis. PLoS Med. 2016 doi: 10.1371/journal.pmed.1002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].World Health Organization . Global Tuberculosis Report 2015 [Internet] Geneva: 2015. [cited 2017 May 1]. Available from: http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf. [Google Scholar]
- [5].World Health Organization . The End TB Strategy [Internet] Geneva: World Health Organization; 2015. [cited 2017 May 2]. Available from: http://www.who.int/tb/strategy/End_TB_Strategy.pdf?ua=1. [Google Scholar]
- [6].World Health Organization . Health in 2015 from Millennium Development Goals (MDG) to Sustainable Development Goals (SDG) [Internet] Geneva: World Health Organization; 2015. [cited 2017 May 2]. Available from: http://apps.who.int/iris/bitstream/10665/200009/1/9789241565110_eng.pdf. [Google Scholar]
- [7].Central TB Division TB India 2013: Ministry of Health and Family Welfare [Internet] 2014 Revised National Tuberculosis Programme; [cited 2017 May 2]. Available from: http://www.tbcindia.nic.in/showfile.php?lid=3163.
- [8].Fiseha D, Demissie M. Assessment of directly observed therapy (DOTS) following tuberculosis regimen change in Addis Ababa, Ethiopia: a qualitative study. BMC Infect Dis. 2015;15:405. doi: 10.1186/s12879-015-1142-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kironde S, Bajunirwe F. Lay workers in directly observed treatment (DOT) programmes for tuberculosis in high burden settings: should they be paid? A review of behavioural perspectives. Afr Health Sci. 2002;2(2):73–8. [PMC free article] [PubMed] [Google Scholar]
- [10].Arcêncio RA, Oliveira MF, Cardozo-Gonzales RI, Ruffino-Netto A, Pinto IC, Villa TCS. City tuberculosis control coordinators’ perspectives of patient adherence to DOT in São Paulo State, Brazil, 2005. Int J Tuberc Lung Dis. 2008;12(5):527–31. [PubMed] [Google Scholar]
- [11].Kamineni VV, Wilson N, Das A, Satyanarayana S, Chadha S, Sachdeva KS, Chauhan LS. Addressing poverty through disease control programmes: examples from Tuberculosis control in India. Int J Equity Health. 2012 Mar 26;11(1):17. doi: 10.1186/1475-9276-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ministry of Health & Family Welfare . National Rural Health Mission Mission Document [Internet] New Delhi: National Rural Health Mission; 2005. [cited 2017 May 2]. Available from: http://www.pbnrhm.org/docs/mission_doc.pdf. [Google Scholar]
- [13].Behzadifar M, Mirzaei M, Behzadifar M, Keshavarzi A, Behzadifar M, Saran M. Patients’ experience of tuberculosis treatment using directly observed treatment, short-course (DOTS): a qualitative study. Iran Red Crescent Med J. 2015;17(4):e20277. doi: 10.5812/ircmj.17(4)2015.20277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kawatsu L, Sato N, Ngamvithayapong-Yanai J, Ishikawa N. Leaving the street and reconstructing lives: impact of DOTS in empowering homeless people in Tokyo, Japan. Int J Tuberc Lung Dis. 2013;17(7):940–6. doi: 10.5588/ijtld.12.0503. [DOI] [PubMed] [Google Scholar]
- [15].Tadesse T, Demissie M, Berhane Y, Kebede Y, Abebe M. Long distance travelling and financial burdens discourage tuberculosis DOTs treatment initiation and compliance in Ethiopia: a qualitative study. BMC Public Health. 2013;13:424. doi: 10.1186/1471-2458-13-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hasker E, Khodjikhanov M, Sayfiddinova S, Rasulova G, Yuldashova U, Uzakova G, et al. Why do tuberculosis patients default in Tashkent City, Uzbekistan? A qualitative study. Int J Tuberc Lung Dis. 2010;14(9):1132–9. [PubMed] [Google Scholar]
- [17].Jaggarajamma K, Ramachandran R, Charles N, Chandrasekaran V, Muniyandi M, Ganapathy S. Psycho-social dysfunction: perceived and enacted stigma among tuberculosis patients registered under revised national tuberculosis control programme. Indian J Tuberc. 2008;55(4):179–87. [PubMed] [Google Scholar]
- [18].Okeibunor JC, Onyeneho NG, Chukwu JN, Post E. Barriers to care seeking in directly observed therapy short-course (DOTS) clinics and tuberculosis control in southern Nigeria: a qualitative analysis. Int Q Community Health Educ. 2006;27(1):23–37. doi: 10.2190/iq.27.1.c. [DOI] [PubMed] [Google Scholar]
- [19].Sagbakken M, Bjune GA, Frich JC. Humiliation or care? A qualitative study of patients’ and health professionals’ experiences with tuberculosis treatment in Norway. Scand J Caring Sci. 2012;26(2):313–23. doi: 10.1111/j.1471-6712.2011.00935.x. [DOI] [PubMed] [Google Scholar]
- [20].Ibrahim LM, Hadjia IS, Nguku P, Waziri NE, Akhimien MO, Patrobas P, et al. Health care workers’ knowledge and attitude towards TB patients under direct observation of treatment in Plateau state Nigeria, 2011. Pan Afr Med J. 2014;18(Suppl. 1):8. doi: 10.11604/pamjs.supp.2014.18.1.3408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Tao T, Zhao Q, Jiang S, Ma L, Wan L, Ma Y, et al. Motivating health workers for the provision of directly observed treatment to TB patients in rural China: does cash incentive work? A qualitative study. Int J Health Plann Manage. 2013;28(4) doi: 10.1002/hpm.2175. [DOI] [PubMed] [Google Scholar]
- [22].Khan MA, Walley JD, Witter SN, Shah SK, Javeed S. Tuberculosis patient adherence to direct observation: results of a social study in Pakistan. Health Policy Plann. 2005:354–65. doi: 10.1093/heapol/czi047. [DOI] [PubMed] [Google Scholar]
- [23].Banerjee A, Sharma BV, Ray A, Kannuri NK, Venkateswarlu TV. Acceptability of traditional healers as directly observed treatment providers in tuberculosis control in a tribal area of Andhra Pradesh, India. Int J Tuberc Lung Dis. 2004;8(10):1260–5. [PubMed] [Google Scholar]
- [24].Singh AR, Pakhare A, Chauhan A, Singh A. Some interesting observations regarding TB patient management from a rural area of Madhya Pradesh: TB case series. J Fam Med Primary care. 2015;4(4):591–3. doi: 10.4103/2249-4863.174300. Medknow Publications. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Creswell J, Plano Clark V. Designing and Conducting Mixed Methods Research. London (United Kingdom): Sage Publications Ltd; 2007. [Google Scholar]
- [26].Census of India 2011: provisional population totals-India data sheet [Internet] New Delhi: Registrar General of India; 2011. Office of the Registrar General Census Commissioner, India. Indian Census Bureau. Available from: http://www.census2011.co.in/census/state/madhya+pradesh.html. [Google Scholar]
- [27].Baiardi JM, Gultekin L, Brush BL. Using sociograms to enhance power and voice in focus groups. Public Health Nurs. 2015 Sep-Oct;32(5):584–91. doi: 10.1111/phn.12199. . Epub 2015 May 4. [DOI] [PubMed] [Google Scholar]
- [28].Kobo Toolbox . Data Collection Just Became Easier 2016. 2016. Data Collection Just Became Easier [Internet] Available from: http://www.kobotoolbox.org. [Google Scholar]
- [29].Saldana J. The Coding Manual for Qualitative Research. Los Angeles: Sage Publication; 2010. [Google Scholar]
- [30].National Health Mission . Executive summary: All India Health Status [Internet] Ministry of Health & Family Welfare, Government of India; 2015. [cited 2015 Mar 18]. Available from: http://nrhm.gov.in/images/pdf/mis-report/Sept-2015/1-NRHM.pdf. [Google Scholar]
- [31].Gopu GS, Rao VB, Vadivet J. Impact of health education on the knowledge of tuberculosis among sputum-positive pulmonary TB patients and their care-givers. Nurs J India. 2012;103(4):160. [PubMed] [Google Scholar]
- [32].Mesfin MM, Newell JN, Walley JD, Gessessew A, Tesfaye T, Lemma F, et al. Quality of tuberculosis care and its association with patient adherence to treatment in eight Ethiopian districts. Health Policy Plann. 2009;24(6):457–66. doi: 10.1093/heapol/czp030. Oxford University Press. [DOI] [PubMed] [Google Scholar]
- [33].Loveday M, Thomson L, Chopra M, Ndlela Z. A health systems assessment of the KwaZulu-Natal tuberculosis programme in the context of increasing drug resistance. Int J Tuberc Lung Dis. 2008;12(9):1042–7. [PubMed] [Google Scholar]
- [34].Odero W, Ayaya SO, Sitienei J, Rotich J. Knowledge, attitudes, and practices of private medical practitioners on tuberculosis among Hiv/Aids patients in Eldoret, Kenya. East Afr Med J. 2003;80(2) doi: 10.4314/eamj.v80i2.8651. [DOI] [PubMed] [Google Scholar]
- [35].Minnery M, Contreras C, Pérez R, Solórzano N, Tintaya K, Jimenez J, et al. A cross sectional study of knowledge and attitudes towards tuberculosis amongst front-line tuberculosis personnel in high burden areas of Lima, Peru. PLoS One. 2013;8(9) doi: 10.1371/journal.pone.0075698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Massey PD, Wakageni J, Kekeubata K, Maena’adi J, Laete’esafi J, Waneagea J, et al. TB questions, East Kwaio answers: community-based participatory research in a remote area of Solomon Islands. Rural Remote Health. 2012;12(4) [PubMed] [Google Scholar]
- [37].Hoffman JA, Cunningham JR, Suleh AJ, Sundsmo A, Dekker D, Vago F, et al. Mobile direct observation treatment for tuberculosis patients: a technical feasibility pilot using mobile phones in Nairobi, Kenya. Am J Prev Med [Internet] 2010;39(1):91–2. doi: 10.1016/j.amepre.2010.02.018. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20537846. [DOI] [PubMed] [Google Scholar]
- [38].von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- [39].Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Tuberc Lung Dis. 2007;19:349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jegh.2017.07.002.
Data Availability Statement
The dataset(s) supporting the conclusions of this article are available on request from the corresponding author.