Abstract
Rosacea is a chronic skin disease characterized by a waxing and waning course. It can encompass different symptoms including erythema, papules/pustules, telangiectasia, and phymata and sometimes secondary manifestations, such as itching, burning, or stinging. This article reviews recent changes in rosacea management. Discussion of relevant medical literature augmented with clinical expertise is also provided. Notably, while patients report that rosacea negatively impacts their emotional and overall well-being, they also tend to have low satisfaction with treatment and are prone to discontinuing therapy and/or using rosacea medications on an intermittent basis, thereby undermining treatment efficacy. Fortunately, the therapeutic armamentarium for rosacea is expanding, and experts now recommend a treatment approach that targets the presenting signs and/or symptoms, with the goal of achieving the greatest possible clearance. More so than in the past, several treatments can be used concurrently to best address the overall presentation of rosacea in an individual patient.
Keywords: Rosacea, targeted treatment, combination therapy, erythema, papulopustular lesions
Rosacea is a chronic inflammatory skin disease, typically involving centrofacial skin, that manifests as a constellation of signs and symptoms, which can change over time and can occur singly or together.1–3 Symptoms include erythema—persistent redness with periodic worsening is considered a defining feature of rosacea—papules and pustular lesions, telangiectasias, phymatous changes, and painful stinging or burning sensations.4 In addition to the skin manifestations, ocular signs and symptoms are also present in a subset of individuals with rosacea.5 It is estimated that approximately 16 million people in the United States have rosacea, with millions more who may have a dormant form of the disease.6,7
Rosacea is estimated to affect 2 to 10 percent of the population, and is more common in women than men. Centrofacial redness due to lesional color and background erythema is a common feature (Figure 1). Telangiectasias is also a common feature of rosacea, particularly on the nose. Though there is a spectrum of signs and symptoms associated with rosacea, Del Rosso et al8 reported that blushing and/or flushing and facial bumps (pimples) were the most bothersome clinical manifestations, followed by skin sensitivity (e.g., stinging/burning sensations, pain).8 While rosacea is more commonly diagnosed in individuals with fair skin, experts have reported that people with darker skin types can also suffer from the disease (Figure 2).9
FIGURE 1.

Rosacea presentation with centrofacial redness due to both lesions and background erythema
Photo courtesy of DermQuest.com
FIGURE 2.

Example of rosacea in dark skin
Photo courtesy of DermQuest.com
Because symptoms of rosacea can be highly visible (i.e., occurs on the face), the disease has been associated with a significant emotional burden, which has been underestimated by clinicians.10 According to data from the National Rosacea Society (NRS), as many as 90 percent of patients with rosacea reported experiencing diminished self-esteem and confidence and up to 41 percent reported avoiding social activities due to the effect of rosacea on their appearance.11 Additionally, as many as 30 percent of patients with rosacea reported feeling stigmatized due to their disease.10 Survey results reported by Del Rosso et al8 indicated that a majority of patients who had both erythema and lesional rosacea symptoms employed techniques to reduce stress and anxiety and regularly concealed rosacea with makeup.8 In 2018, survey data reported by Zeichner12 indicated that, despite experiencing an overall negative impact on emotional and social well-being and quality of life, treatment utilization was low among patients with rosacea. Survey respondents also indicated a low level of satisfaction with rosacea treatments, marked by intermittent use of specific treatments.12 These recent findings all underscore the need for clinicians to optimize management strategies for patients with rosacea.
CURRENT TREATMENT APPROACHES
In recent years, there has been a theoretical change in how rosacea is viewed, with experts moving away from subtype classification to a phenotype-based approach.4, 13, 14 This shift is largely based on the understanding that patients with rosacea usually do not exhibit one isolated symptom, but rather experience a combination of symptoms, such as persistent erythema with papules and pustules.4, 13 In addition, data collected by Steinhoff et al13,14 suggest that erythema and rosacea lesions have common characteristics of inflammation, including the influx of inflammatory cells (e.g., macrophages, T cells, mast cells).13,14 Research suggests that persistent erythema could be the initial sign of underlying inflammation and, as such, is deserving of treatment.13 With expanded treatment options, clinicians can now tailor therapy to better match individual symptoms and achieve optimal results.
New evidence suggests that it is important to reconsider the goals of rosacea therapy in terms of efficacy. Webster et al15 analyzed data from patients in controlled clinical trials who achieved a clinician’s rating of “clear” and compared it to that from patients who were rated “almost clear.” In these trials, a total of 1,366 subjects were treated with ivermectin, metronidazole, or vehicle. The comparison showed that significantly more subjects who were rated as “clear”(vs. those who were rated “almost clear”) had clinically meaningful improvements in Dermatology Life Quality Index (DLQI) scores or had scores of 0 to 1, which indicated no impact on quality of life (Table 1). Not surprisingly, there was also a significant difference (P<.001) in the mean percentage reduction of inflammatory lesions by end of treatment for “clear” subjects compared to those who were rated “almost clear.”16 It is also very important to note that achieving “clear” was associated with a marked delay in relapse (i.e., those who were “clear” maintained remission for at least 5 months longer than those rated “almost clear”). The investigators noted that “continuing a maintenance treatment after reaching ‘clear’ may be expected to further extend the time to relapse.”16
TABLE 1.
Rosacea presentation with centrofacial redness due to both lesions and background erythema
| IGA SCORE (PATIENT #) | Before Treatment | End of Treatment | |
|---|---|---|---|
| DLQI Score 0–1, % | DLQI Score 0–1, % | MCID≥4, % | |
| 0 (341) | 16.1 | 84.2 | 58.7 |
| 1 (1,003) | 16.9 | 66.0 | 44.3 |
DLQI: Dermatology Life Quality Index; MCID: minimal clinically important difference; IGA: Investigators Global Assessment
Table adapted from Webster et al15
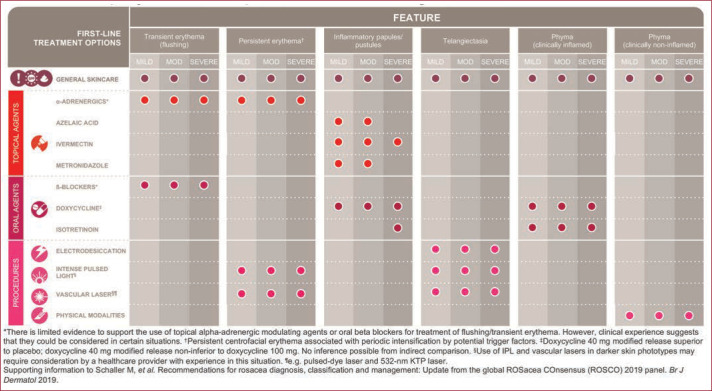
Expert consensus indicates that multiple rosacea symptoms are best treated using a combinations of treatments, which can include medical therapy, skin care, and physical modalities.13 Figure 3 provides a treatment algorithm, outlining when topical and systemic options are most appropriate.
FIGURE 3.
ROSCO Project 2019 updated treatment algorithm
TOPICAL THERAPIES
Topical treatments for rosacea approved by the United States Food and Drug Administration (FDA) include ivermectin 1% cream, metronidazole 0.75% cream (twice daily), metronidazole gel 1% (daily), and azelaic acid 15% gel or foam (twice daily) for inflammatory lesions, and brimonidine gel 0.33% and oxymetazoline cream 1% for erythema.13, 17 Topical therapy is indicated in most cases of rosacea.
Papules and pustules. Ivermectin. Randomized controlled studies of topical ivermectin (IVM) 1% cream versus placebo in moderate to severe papulopustular rosacea showed a statistically significant difference in favor of IVM for both successbased on Investigator Global Assessment (IGA) scores and lesion reductions.18 Siddiqui et al19 performed a meta-analysis of 19 studies, reporting greater efficacy using IVM in reducing rosacea papulopustular lesions, compared to other currently available options, with a safety/tolerability profile that was at least comparable.19 The long-term extensions of the IVM pivotal trials included azelaic acid (AzA) gel 15% as an active comparator for 40 weeks.20 Long-term data indicated lower rates of treatment-related side effects and higher IGA scores (“clear” or “almost clear”) in the IVM group, compared to the AzA gel group.20 Comparison of IVM to metronidazole cream 0.75% twice daily indicated IVM was more effective and markedly delayed time to relapse.21 Of note, Schaller et al22 recently reported that topical ivermectin improved symptoms of ocular rosacea, including foreign body sensation, burning, and sensitivity to light.22
Metronidazole. Metronidazole was one of the first approved therapies for rosacea and is available in 0.75% and 1% concentrations in gel, lotion, and cream formulations. Metronidazole is thought to have anti-inflammatory and antioxidant effects, thought the mechanism of action is not well understood.13 A Cochrane review analyzing multiple controlled studies of metronidazole as treatment for papulopustular rosacea reported superior efficacy, versus placebo.23 Comparative studies of metronidazole versus AzA demonstrated similar efficacy in reducing rosacea lesions between the two therapies.23,24 Metronidazole is generally well tolerated, with adverse events that generally are mild and involve skin sensations such as pruritus, irritation, and dryness.23
AzA. AzA has been shown to reduce papules and pustules in both controlled clinical trials and in a small (N=20) single-center, postmarketing, open-label study.25-27 In Phase III studies, AzA 15% gel reduced inflammatory lesions by 17.5 to 17.8 percent, while the AzA 15% foam reduced inflammatory lesions by 21.2 to 21.7.26, 28-30 Cutaneous irritation (e.g., pain, pruritus, dryness, erythema) are the most common adverse events associated with AzA therapy.31 AzA gel is in a water-based vehicle, and the foam is a hydrophilic oil-in-water emulsion.28 While there has not been a head-to-head study comparing the foam to the gel, similarities in registration study results suggest their efficacy in rosacea are comparable.28 This suggests that vehicle selection may be based primarily on patient preference.28
Erythema. Redness, a hallmark of rosacea, can take many forms, and treatment approaches for rosacea-related erythema can vary, depending on the cause (e.g., vasodilation; abnormalities of superficial skin vasculature, including, but not restricted to telangiectasias; lesional redness at the site of papules or pustules; and/or inflammatory redness secondary to barrier dysfunction.32-34 Enlarged abnormal superficial blood vessels occur through vasoactive smooth muscle; as a result, stimulation of α-adrenergic receptors leads to vasoconstriction and reduced visible facial erythema.35, 36 In contrast, telangiectasias are not directly affected by the sympathetic nervous system, and do not respond to α-adrenergic receptor stimulation.34 Perilesional redness may respond best to treatments for papules/pustules, and inflammatory redness can be targeted both by topical therapies and by optimized skin care regimens to improve barrier function.34
Alpha-adrenergic receptor agonists. Recently, two α-adrenergic receptor agonists were introduced for treatment of persistent facial erythema related to rosacea. Brimonidine gel 0.33% was the first of these approved by FDA (August 2013) for once-daily therapy for persistent facial erythema of rosacea followed in January 2017 by approval of oxymetazoline 1% cream.32 Brimonidine affects α2 receptors with a less prominent effect on α1 receptors, while oxymetazoline targets α1 receptors; it is not known whether differences in receptor activity are associated with different clinical activity, but differences have been proposed (Table 2).32 In rosacea-related erythema, brimonidine acts by cutaneous vasoconstriction and may also have anti-inflammatory effects.37,38 According to a 2016 Cochrane review, the efficacy of brimonidine in improving moderate to severe erythema in rosacea is well proven with adverse events that were generally mild and most frequently included worsening of erythema, flushing, and pruritus.17, 23 Brimonidine has a fast onset of action, and its effect lasts approximately 12 hours. Application of oxymetazoline to facial redness also reduces erythema for several hours, with an impact that fades by 12 hours and a slower onset compared to brimonidine.32 Because oxymetazoline was introduced to the rosacea market very recently, there are few data showing clinical differences between the two agents.32
TABLE 2.
Anatomic differences within the vasculature among a-adrenergic receptors and possible pharmacologic/pharmacodynamic effects. Reprinted with permission from Del Rosso32
Maintenance of vascular tone occurs at the junctional synapse between the sympathetic nerve terminal and the blood vessel wall. The α1-receptors are located postsynaptically in the vascular smooth muscle within the region of the synapse; α2-receptors are located presynaptically at the nerve terminal, postsynaptically in the vascular smooth muscle outside the direct region of the synapse and within the endothelial wall.
|
The presence of presynaptic α2-receptors appears to inhibit norepinephrine release, which might contribute to vasodilation via a negative feedback loop mechanism.
|
The presence of α2 receptors on endothelial cells has been shown to mediate release of nitric oxide (NO), which induces vasodilation. Hence, stimulation of endothelial cell α2 receptors might invoke a vasodilatory response.
|
ORAL THERAPY
Oral medications may be indicated in moderate-severe rosacea and are often used in ocularosacea.23
Antibiotics. While tetracyclines and azithromycin have been used off-label in the treatment of rosacea, only subantimicrobial dose doxycycline (40mg) has been approved by the FDA for this disease. It is thought that, in rosacea, antibiotics act through anti-inflammatory mechanisms rather than antimicrobial effects, as seen with subantimicrobial dose doxycycline, which has anti-inflammatory effects at concentrations below the minimum inhibitory concentrations of susceptible bacteria.39 Due to changing patterns of antimicrobial resistance, clinicians are moving away from using conventional doses of antibiotics to treat rosacea.40,41 If conventional doses of antibiotics are used, they should be limited in duration, with patients being transitioned to topical therapy as the primary treatment once improvement has become apparent.23,
PHYSICAL MODALITIES
Physical modalities may be indicated for treatment of rosacea-associated telangiectasia and phymatous changes. A recent Cochrane review found that lasers and intense pulsed light therapy were both effective treatment modalities for rosacea-associated telangiectasia and phymatous changes, but the data were limited due to small sample sizes.23 The authors of the Cochrane review also reported that data from randomized, controlled trials was limited, with regard to light therapies, and recommended that further study of this modality be a research priority.23 One of the authors of this article (SMJ) has utilized pulsed dye laser regularly with favorable results in clinical practice for the treatment of telangiectasia and erythema associated with rosacea.
PATIENT EDUCATION
Rosacea is a chronic inflammatory disease, and education is key in helping patients to cope with their condition. Clinicians should explain that rosacea is benign, while acknowledging that it can cause significant distress. Patients should also be reassured that current treatments can effectively control the signs and symptoms.13, 38 Finally, clinicians should educate patients with rosacea on changes in lifestyle they can make to improve symptoms of rosacea. Table 3 presents common triggers for rosacea, which were identified by large scale surveys conducted by the National Rosacea Society.42
TABLE 3.
Top 10 most frequent rosacea triggers from National Rosacea Society survey of 1,066 rosacea patients42
| FACTORS | PATIENTS AFFECTED, % |
|---|---|
| Sun exposure | 81.0 |
| Emotional stress | 79.0 |
| Hot weather | 75.0 |
| Wind | 57.0 |
| Heavy exercise | 56.0 |
| Alcohol consumption | 52.0 |
| Hot baths | 51.0 |
| Cold weather | 46.0 |
| Spicy foods | 45.0 |
| Humidity | 44.0 |
SKIN CARE
It is important to educate patients with rosacea on proper skin care practices, such as the need for barrier repair and protection from UV exposure. Rosacea is associated with impaired epidermal barrier integrity, which makes barrier repair an important component of the skin care routine. Using topical medications on skin that has compromised barrier function increases the risk for treatment tolerability issues. Williamson et al43 reported that patients with rosacea who experienced treatment-related adverse events had significantly higher rosacea-related health costs compared to those with no adverse events.43
Patients with rosacea should be instructed to regularly use sunscreen with a sun protection factor (SPF) of 30 or higher and broad spectrum protection against UVA, UVB, infrared, and blue light. The use of bland moisturizers and gentle over-the-counter cleansers is recommended.13 In a recent consensus statement, Schaller et al reported that proper skin care is currently a primary treatment approach to managing dry skin appearance and sensation, as well as stinging sensation, for patients with rosacea.13
CONCLUSION
The expanding treatment armamentarium now allows clinicians to individualize rosacea therapy to the needs of each patient, with excellent clinical results. Topical treatments form the foundation of rosacea therapy and can be highly efficacious in reducing lesions and decreasing the intensity of erythema. Topical agents may also help manage secondary rosacea symptoms, such as itching, stinging, and burning sensations. In addition, general measures, such as avoiding triggers and patient education on proper skin care, work together with rosacea medications to enhance outcomes. The importance of treating rosacea to clearance has been shown by Webster et al,16 and this information should guide clinicians in both type of therapy and duration of therapy.
ACKNOWLEDGMENT
The authors wish to acknowledge Valerie Sanders, Sanders Medical Writing, for editorial assistance with preparation of this article.
REFERENCES
- Blount BW, Pelletier AL. Rosacea: a common, yet commonly overlooked, condition. Am Fam Physician. 2002;66:435–40. [PubMed] [Google Scholar]
- Del Rosso JQ, Thiboutot D, Gallo R et al. Consensus recommendations from the American Acne & Rosacea Society on the management of rosacea, part 1: a status report on the disease state, general measures, and adjunctive skin care. Cutis. 2013;92:234–40. [PubMed] [Google Scholar]
- Napierkowski DB. Rosacea: diagnosis and management. Nurse Pract. 2016;41:8–13. doi: 10.1097/01.NPR.0000470359.23708.33. [DOI] [PubMed] [Google Scholar]
- Tan J, Almeida LM, Bewley A et al. Updating the diagnosis, classification and assessment of rosacea: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol. 2017;176:431–438. doi: 10.1111/bjd.15122. [DOI] [PubMed] [Google Scholar]
- Alvarenga LS, Mannis MJ. Ocular rosacea. the ocular surface. Ocul Surf. 2005;3(1):41–58. doi: 10.1016/s1542-0124(12)70121-0. Jan. [DOI] [PubMed] [Google Scholar]
- Drake L. Rosacea now estimated to affect at least 16 million American. Rosacea Review site. Winter. 2010. https://www.rosacea.org/rosacea-review/2010/winter/rosacea-now-estimated-to-affect-at-least-16-million-americans Accessed 30 Mar 2020.
- Del Rosso JQ, Tanghetti EA, Baldwin HE et al. The burden of illness of erythematotelangiectatic rosacea and papulopustular posacea: Findings from a web-based survey. J Clin Aesthet Dermatol. 2017;10:17–31. [PMC free article] [PubMed] [Google Scholar]
- Alexis AF. Rosacea in patients with skin of color: uncommon but not rare. Cutis. 2010;86:60–62. [PubMed] [Google Scholar]
- Heisig M, Reich A. Psychosocial aspects of rosacea with a focus on anxiety and depression. Clin Cosmet Investig Dermatol. 2018;11:103–107. doi: 10.2147/CCID.S126850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Rosacea Society site. All about rosacea. https://www.rosacea.org/patients/all-about-rosacea Accessed 30 Mar 2020.
- Zeichner JA, Eichenfield LF, Feldman SR et al. Quality of life in individuals with erythematotelangiectatic and papulopustular rosacea: Findings from a web-based survey. J Clin Aesthet Dermatol. 2018;11:47–52. [PMC free article] [PubMed] [Google Scholar]
- Schaller M, Schofer H, Homey B et al. Rosacea management: update on general measures and topical treatment options. J German Soc Dermat. 2016;14:17–27. doi: 10.1111/ddg.13143. Suppl 6. [DOI] [PubMed] [Google Scholar]
- Tan J, Steinhoff M, Berg M et al. Shortcomings in rosacea diagnosis and classification. Br J Dermatol. 2017;176:197–199. doi: 10.1111/bjd.14819. [DOI] [PubMed] [Google Scholar]
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69:S15–S26. doi: 10.1016/j.jaad.2013.04.045. [DOI] [PubMed] [Google Scholar]
- Webster G, Schaller M, Tan J et al. Defining treatment success in rosacea as 'clear' may provide multiple patient benefits: results of a pooled analysis. J Dermatol Treat. 2017;28:469–474. doi: 10.1080/09546634.2017.1343435. [DOI] [PubMed] [Google Scholar]
- van Zuuren EJ, Fedorowicz Z. Interventions for rosacea. J Am Med Assoc. 2015;314:2403–404. doi: 10.1001/jama.2015.15287. [DOI] [PubMed] [Google Scholar]
- Stein L, Kircik L, Fowler J et al. Efficacy and safety of ivermectin 1% cream in treatment of papulopustular rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studies. J Drugs Dermatol. 2014;13:316–323. [PubMed] [Google Scholar]
- Siddiqui K, Stein Gold L, Gill J. The efficacy, safety, and tolerability of ivermectin compared with current topical treatments for the inflammatory lesions of rosacea: a network meta-analysis. SpringerPlus. 2016;5:1151. doi: 10.1186/s40064-016-2819-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein Gold L, Kircik L, Fowler J et al. Long-term safety of ivermectin 1% cream vs azelaic acid 15% gel in treating inflammatory lesions of rosacea: results of two 40-week controlled, investigator-blinded trials. J Drugs Dermatol. 2014;13:1380–1386. [PubMed] [Google Scholar]
- Taieb A, Khemis A, Ruzicka T et al. Maintenance of remission following successful treatment of papulopustular rosacea with ivermectin 1% cream vs. metronidazole 0.75% cream: 36-week extension of the ATTRACT randomized study. J Eur Acad Dermatol Venereol. 2016;30:829–836. doi: 10.1111/jdv.13537. [DOI] [PubMed] [Google Scholar]
- Schaller M, Pietschke K. Successful therapy of ocular rosacea with topical ivermectin. Br J Dermatol. 2018;179(2):520–521. doi: 10.1111/bjd.16534. [DOI] [PubMed] [Google Scholar]
- van Zuuren EJ, Fedorowicz Z. Interventions for rosacea: abridged updated Cochrane systematic review including GRADE assessments. Br J Dermatol. 2015;173:651–662. doi: 10.1111/bjd.13956. [DOI] [PubMed] [Google Scholar]
- Wolf JE, Jr., Kerrouche N, Arsonnaud S. Efficacy and safety of once-daily metronidazole 1% gel compared with twice-daily azelaic acid 15% gel in the treatment of rosacea. Cutis. 2006;77:3–11. [PubMed] [Google Scholar]
- Wirth PJ, Henderson Berg MH, Sadick N. Real-world efficacy of azelaic acid 15% gel for the reduction of inflammatory lesions of rosacea. Skin Therapy Lett. 2017;22:5–7. [PubMed] [Google Scholar]
- Draelos ZD, Elewski BE, Harper JC et al. A phase 3 randomized, double-blind, vehicle-controlled trial of azelaic acid foam 15% in the treatment of papulopustular rosacea. Cutis. 2015;96:54–61. [PubMed] [Google Scholar]
- Draelos ZD, Elewski B, Staedtler G, Havlickova B. Azelaic acid foam 15% in the treatment of papulopustular rosacea: a randomized, double-blind, vehicle-controlled study. Cutis. 2013;92:306–317. [PubMed] [Google Scholar]
- Del Rosso JQ. Azelaic acid topical formulations: differentiation of 15% gel and 15% foam. J Clin Aesthet Dermatol. 2017;10:37–40. [PMC free article] [PubMed] [Google Scholar]
- Thiboutot DM, Fleischer AB, Jr., Del Rosso JQ, Graupe K. Azelaic acid 15% gel once daily versus twice daily in papulopustular rosacea. J Drugs Dermatol. 2008;7:541–6. [PubMed] [Google Scholar]
- Thiboutot D, Thieroff-Ekerdt R, Graupe K. Efficacy and safety of azelaic acid (15%) gel as a new treatment for papulopustular rosacea: results from two vehicle-controlled, randomized phase III studies. J Am Acad Dermatol. 2003;48:836–845. doi: 10.1067/mjd.2003.308. [DOI] [PubMed] [Google Scholar]
- Finacea (azelaic acid) Foam PI. Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc; 2015. [Google Scholar]
- Del Rosso JQ. Topical a-agonist therapy for persistent facial erythema of rosacea and the addition of oxmetazoline to the treatment Aamamentarium: Where are we now? J Clin Aesthet Dermatol. 2017;10:28–32. [PMC free article] [PubMed] [Google Scholar]
- Del Rosso JQ. Advances in understanding and managing rosacea: part 1: connecting the dots between pathophysiological mechanisms and common clinical features of rosacea with emphasis on vascular changes and facial erythema. J Clin Aesthet Dermatol. 2012;5:16–25. [PMC free article] [PubMed] [Google Scholar]
- Del Rosso JQ. Advances in understanding and managing rosacea: part 2: the central role, evaluation, and medical management of diffuse and persistent facial erythema of rosacea. J Clin Aesthet Dermatol. 2012;5:26–36. [PMC free article] [PubMed] [Google Scholar]
- Fowler J, Jarratt M, Moore A et al. Once-daily topical brimonidine tartrate gel 0.5% is a novel treatment for moderate to severe facial erythema of rosacea: results of two multicentre, randomized and vehicle-controlled studies. Br J Dermatol. 2012;166:633–641. doi: 10.1111/j.1365-2133.2011.10716.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanler SD, Ondo AL. Successful treatment of the erythema and flushing of rosacea using a topically applied selective alpha1-adrenergic receptor agonist, oxymetazoline. Arch Dermatol. 2007;143:1369–1371. doi: 10.1001/archderm.143.11.1369. [DOI] [PubMed] [Google Scholar]
- Piwnica D, Rosignoli C, de Menonville ST et al. Vasoconstriction and anti-inflammatory properties of the selective alpha-adrenergic receptor agonist brimonidine. J Dermatol Sci. 2014;75:49–54. doi: 10.1016/j.jdermsci.2014.04.002. [DOI] [PubMed] [Google Scholar]
- Schaller M, Almeida LM, Bewley A et al. Rosacea treatment update: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol. 2017;176:465–471. doi: 10.1111/bjd.15173. [DOI] [PubMed] [Google Scholar]
- Korting HC, Schollmann C. Current topical and systemic approaches to treatment of rosacea. J Eur Acad Dermatol Venereol. 2009;23:876–882. doi: 10.1111/j.1468-3083.2009.03167.x. [DOI] [PubMed] [Google Scholar]
- Yentzer BA, Fleischer AB., Jr Changes in rosacea comorbidities and treatment utilization over time. J Drugs Dermatol. 2010;9:1402–1406. [PubMed] [Google Scholar]
- Del Rosso JQ, Leyden JJ, Thiboutot D, Webster GF. Antibiotic use in acne vulgaris and rosacea: clinical considerations and resistance issues of significance to dermatologists. Cutis. 2008;82:5–12. [PubMed] [Google Scholar]
- National Rosacea Society. Rosacea triggers survey. https://www.rosacea.org/patients/rosacea-triggers/rosacea-triggers-survey Accessed 31 Mar 2020.
- Williamson T, Kamalakar R, Ogbonnaya A et al. Rate of adverse events and healthcare costs associated with the topical treatment of rosacea. Am Health Drug Benefits. 2017;10:113–119. [PMC free article] [PubMed] [Google Scholar]