Abstract
Self-injurious behavior (SIB) is inherently problematic because it can lead to injuries, including those that are quite severe and may result in loss of function or permanent disfigurement. The current study replicated and extended Rooker et al. (2018) by classifying the physical characteristics of injuries across groups of individuals with automatically maintained SIB (ASIB Subtypes 2 and 3) and socially maintained SIB. Individuals with Subtype 2 ASIB had the most frequent and severe injuries. Further, an inverse relation was found between the level of differentiation in the functional analysis and the number of injuries across groups. Studying the response products of SIB (the injuries) documents the risks associated with SIB, justifies the need for research and the intensive intervention, and advances knowledge of SIB. Additional research is needed to replicate these findings, and determine the variables that produce different characteristics of injury secondary to SIB.
Keywords: automatically maintained, functional analysis, injury, self-injury
Some individuals diagnosed with intellectual and developmental disabilities (IDD) engage in self-injurious behavior (e.g., Cooper et al., 2009; Soke et al., 2016). Self-injurious behavior (SIB) is problematic because it inherently leads to injuries (SIB-related injuries). SIB-related injuries are the response products of SIB, but relatively few studies have systematically examined the injuries produced by SIB. Rather, the extensive literature on SIB has largely focused on the occurrence of SIB (rate or percentage of time), typically as a dependent variable in the context of behavioral assessment and treatment.
The study of SIB-related injuries is important for several reasons. First, by measuring injuries prior to and after treatment (in addition to the reduction of SIB), an additional dimension of treatment outcome can be measured, which is consistent with the need to measure both treatment efficacy and effectiveness (Flay et al., 2005; Hunsley & Lee, 2007; Narzisi, Costanza, Umberto, & Filippo, 2014). That is, demonstration that a treatment reduces both the occurrence of SIB and SIB-related injury provides further support that the outcomes were socially and practically meaningful (e.g., McDonough, Hillery, & Kennedy, 2000; Twohig & Woods, 2001; Wilson, Iwata, & Bloom, 2012). Second, measuring injuries produced by SIB helps provide more information about the importance of this problem to the health and well-being of those who engage in SIB. Thus, documenting SIB-related injury provides support for funding of services and research as well as establishes the need for the use of protective procedures, including the use of restraint in clinical practice (Vollmer et al., 2011). Finally, research aimed at studying SIB-related injuries has potential heuristic value, particularly in the case of automatically maintained SIB (ASIB) where the controlling variables are neither observable nor practically controllable (Vollmer, 1994). For ASIB, there is the potential that examining the response products of this behavior could provide information about its functional properties, particularly if differences in injuries are found across functional classes of SIB.
In an extensive review of the literature on SIB, Kahng, Iwata, and Lewin (2002) found a range of topographies of SIB, with head banging, self-biting, eye-poking, self-scratching, hair pulling, and head-hitting as the most common topographies. Less common topographies of SIB including ear pulling, removing fingernails, inserting objects in ears or nose were also noted (see also Hyman, Fisher, Mercugliano, & Cataldo, 1990 for additional information on common forms of SIB). Further, many individuals exhibit multiple topographies of SIB, and injuries produced by SIB can be quite severe, with a single bout of behavior producing bleeding, fractures, concussion, or other serious injury. Documented SIB-related injuries include scars, skin discoloration, calluses, calcification, fractures, and hematomas as well as secondary complications such as infections, sensory or nerve damage, and eye injuries, including retinal detachment (Patton, 2004). In a retrospective review of 97 inpatients with SIB admitted to a specialized hospital unit for the assessment and treatment of SIB, physical injury resulting from SIB was reported in 76.3% of cases reviewed (Hyman et al., 1990).
The development of the Self-Injury Trauma (SIT) Scale (Iwata, Pace, Kissel, Nau, & Farber, 1990) represents a major technological advancement for the quantification of SIB-related injuries. The SIT Scale is designed to evaluate various characteristics of SIB-related injuries (i.e., location, number, type, severity) and to predict estimated risk for further injury. The SIT Scale has been used in two studies that also examined the function of SIB (Hall, Hustyi, Chui, & Hammond, 2014; Hustyi, Hammond, Rezvami, & Hall, 2013). Both studies examined several dimensions of SIB, including SIB-related injury characteristics for individuals diagnosed with Prader-Willi syndrome (PWS). The researchers reported on the topography of SIB, the function of SIB, and the characteristics of injuries sustained using the SIT Scale. Hustyi et al. (2013) determined function using an indirect assessment and did not report injury characteristics based on function. In Hall et al. (2014), a functional analysis (FA) of SIB was conducted for each case. They found that SIB was automatically maintained for 8 of 13 individuals with PWS, six of whom had a high estimated risk based on the SIT Scale. For the remaining five individuals, the FAs were inconclusive, and three were classified as high risk. However, because an automatic function of SIB was the only function identified across individuals, it is not possible to determine the extent to which the findings on injuries were specific to the functional class of SIB (automatic) or the syndrome (PWS).
More recently, Rooker et al. (2018) used the SIT Scale to examine injury characteristics for individuals with different functional classes of SIB (socially versus automatically maintained). This exploratory research was initiated as part of a broader program of research aimed at understanding ASIB, which included, among other things, measurement of its response products (injuries). Rooker et al. examined medical records (physical examinations conducted by nursing staff), clinical care descriptions (FA descriptions), and clinical data (FA outcomes) for 64 individuals who engaged in SIB and were admitted to an inpatient unit specializing in the assessment and treatment of severe behavior disorders. In that study, the SIT Scale was completed based on a retrospective review of medical records. For the 35 individuals with at least one injury present at admission, differences were observed across individuals with socially maintained SIB versus ASIB. Function was broadly predictive of the location and type of the most severe injuries across groups in that the most severe contusions to the head were observed in individuals with ASIB, whereas the most severe abrasions and lacerations on the body and extremities were observed in individuals with socially maintained SIB.
Rooker et al. (2018) was the first study to show differences in injuries across functional classes of SIB, but the study had several limitations. First, the study involved a retrospective review of the medical record, wherein the SIT scale was completed based on a written report of medical staff describing injuries rather than the direct observation of the injury. Second, and interrelated, the exact number of injuries at each body site was often not reported in the medical record. Third, the method of classifying the function of individuals’ SIB may have been overly broad. Specifically, individuals were classified as having either ASIB or socially maintained SIB, with no additional analysis based on subtypes of ASIB (i.e., Subtype 1, 2, or 3; Hagopian, Rooker, & Zarcone, 2015). This final limitation is significant because research has demonstrated meaningful differences in the clinical presentation of functional classes and subtypes of SIB (e.g., Iwata et al., 1994; Hagopian et al., 2015). Research indicates that (a) Subtype 1 ASIB is generally responsive to reinforcement-only treatment at a level nearly comparable to socially maintained SIB, and (b) Subtypes 2 and 3 ASIB are resistant to reinforcement-only treatment, frequently necessitating more intensive procedures (Hagopian et al., 2015; Hagopian, Rooker, Zarcone, Bonner, & Arevalo, 2017). Thus, the purpose of the current study was to replicate and extend Rooker et al. by prospectively examining the relation between functional class of SIB and SIB-related injuries across individuals with different functional classes and subtypes of ASIB.
METHOD
Participants
Individuals were enrolled as research participants in an Institutional Review Board-approved research study designed to examine subtypes of ASIB. Caregiver consent was obtained prior to participation. Participants were recruited from patients admitted to an inpatient unit for the assessment and treatment of severe problem behavior, including SIB. Inclusion criteria were the presence of SIB with an identified function (functional analysis procedures described in next section), age between 4 and 25 years old (the age range typical to individuals admitted to the inpatient unit), and a diagnosis of IDD. The presence of an injury was not an inclusion criterion; however, all individuals recruited did have at least one injury. Participants were not excluded if SIB was maintained by multiple sources of reinforcement. All persons who met these criteria were recruited. We recruited 17 males and 6 females (Table 1). This ratio of males and females is generally reflective of the population admitted to our inpatient unit.
Table 1.
Participant Demographics
| Subtype 2 ASIB n = 6 |
Subtype 3 ASIB n = 8 |
Social SIB n = 9 |
|
|---|---|---|---|
| Age | |||
| Children (5-12) | 2 | 2 | 4 |
| Adolescent (13-17) | 1 | 4 | 3 |
| Adults (> 18) | 3 | 2 | 2 |
| Sex | |||
| Female | 2 | 2 | 2 |
| Male | 4 | 6 | 7 |
| Level of Intellectual | |||
| Disability | |||
| Mild–Moderate | 2 | 1 | 1 |
| Severe-Profound | 1 | 3 | 1 |
| Unspecified | 3 | 4 | 6 |
| Unknown | 0 | 0 | 1 |
| Diagnosis | |||
| Autism Spectrum | 6 | 7 | 7 |
| Disorder | |||
| Cornelia de Lange | 0 | 1 | 0 |
| Syndrome | |||
Functional analysis (FA).
An FA (Iwata, Dorsey, Slifer, Bauman, & Richman, 1982) was conducted with each participant to determine the variables that maintained their SIB. In almost every case (22 participants), FAs were conducted by participants’ clinical team as part of routine clinical care during their hospitalization. The clinical team was composed of a faculty-level behavior analyst who oversaw the FA, as well as extensively trained clinicians who conducted the FA and collected data on SIB. For one participant, the FA was conducted by extensively trained research assistants and directed by the second author. In this case, an FA had previously been conducted by the clinical team, but an additional analysis was conducted to clarify the outcome.
All FAs were conducted in a similar manner to that described by Iwata et al. (1982) and involved test conditions in which specific antecedents were presented and, contingent on SIB, specific consequences were provided. Antecedent and consequent events in test conditions (attention, escape, and tangible), and a control condition (play) were identical to those described in Hagopian, Rooker, Jessel, and DeLeon (2013). For four cases, an alone condition was conducted (Participants 1, 4, 5, and 8). For the remaining 18 cases, an ignore condition was conducted.1 FA designs included multielement (n = 11), pairwise (n = 11), or reversal (n = 1) designs. Table 2 shows the topographies of SIB assessed in these FAs and the rates of SIB in the relevant conditions for each participant. Across all FAs, procedures to ensure patient safety (e.g., session pausing, termination, brief suspension and medical oversight) were present and continuously employed.
Table 2.
Self-injury Topographies, Levels of Behavior in Control and Test Condition, Levels of Self-Restraint, Group and Function
| Part. | Topographies | Play Rate |
Test Rate |
Mean Percent Self-Restraint |
Group | Other Functions* |
|---|---|---|---|---|---|---|
| 1 | 1) Head hitting 2) Body hitting 3) Head banging |
33.5 | 32.2 | n/a | ASIB-2 | None |
| 2 | 1) Head banging 2) Skin biting 3) Head hitting |
3.9 | 4.5 | n/a | ASIB-2 | None |
| 3 | 1) Head/Neck hitting 2) Banging body on surfaces 3) Stomping on the surfaces 4) Skin biting 5) Body hitting 6) Skin scratching 7) Skin pinching |
4.2 | 1.6 | n/a | ASIB-2 | None |
| 4 | 1) Skin picking 2) Skin scratching 3) Skin pinching 4) Rubbing injured areas |
1.3 | 1.2 | n/a | ASIB-2 | None |
| 5 | 1) Skin picking 2) Skin scratching |
2.8 | 2.5 | n/a | ASIB-2 | None |
| 6 | 1) Head hitting 2) Head kneeing |
7.0 | 9.5 | n/a | ASIB-2 | A |
| 7 | 1) Body hitting 2) Body kicking |
0.0 | 1.9 | 63.3 | ASIB-3 | None |
| 8 | 1) Head hitting 2) Hitting chin with shoulder 3) Body hitting 4) Banging body on surfaces |
4.1 | 2.3 | 82.5 | ASIB-3 | None |
| 9 | 1) Head hitting 2) Knee/Shoulder heading |
3.4 | 5.1 | 96.7 | ASIB-3 | None |
| 10 | 1) Body hitting 2) Head hitting 3) Head banging 4) Pulling hair 5) Skin picking 6) Skin scratching 7) Skin pinching 8) Skin biting |
12.3 | 16.7 | 89.1 | ASIB-3 | E |
| 11 | 1) Head hitting | 32.3 | 36.8 | 59.3** | ASIB-3 | A; T |
| 12 | 1) Head hitting 2) Body hitting 3) Body kicking 4) Skin biting 5) Skin scratching 6) Skin pinching |
0.4 | 2.8 | 100 | ASIB-3 | None |
| 13 | 1) Body hitting 2) Lip/Tongue biting 3) Body kicking 4) Skin pinching 5) Skin scratching 6) Skin biting 7) Banging body on surfaces |
0.3 | 1. 2 | 98.6 | ASIB-3 | None |
| 14 | 1) Head hitting 2) Kneeing head 3) Pressing chin against surfaces 4) Body hitting 5) Body kicking 6) Skin scratching 7) Skin pinching 8) Lip/Tongue biting |
3.9 | 6.7 | 99.7 | ASIB-3 | E |
| 15 | 1) Head hitting 2) Skin biting |
0.0 | 1.4 | n/a | Social-A | E; T |
| 16 | 1) Head hitting 2) Head banging 3) Skin biting |
0.0 | 3.8 | n/a | Social-A | T |
| 17 | 1) Head hitting 2) Body hitting 3) Eye poking 4) Pressing chin against objects or surfaces 5) Skin biting 6) Skin scratching 7) Skin picking 8) Hair pulling |
0.0 | 0.3 | n/a | Social-A | None |
| 18 | 1) Head hitting 2) Kneeing head 3) Body hitting |
0.0 | 0.4 | n/a | Social-T | None |
| 19 | 1) Head hitting 2) Body hitting 3) Pressing chin against objects or surfaces 4) Skin biting 5) Skin scratching 6) Skin picking |
0.0 | 0.7 | n/a | Social-T | None |
| 20 | 1) Head hitting 2) Kneeing head 3) Body hitting 4) Pulling hair 5) Skin pinching 6) Skin biting 7) Skin scratching |
0.0 | 2.4 | n/a | Social-T | None |
| 21 | 1) Head hitting 2) Body hitting 3) Skin biting 4) Skin scratching 5) Skin pinching |
0.0 | 0.4 | n/a | Social-T | None |
| 22 | 1) Head hitting 2) Body hitting 3) Skin picking 4) Eye rubbing 5) Skin biting |
0.0 | 0.4 | n/a | Social-A | None |
| 23 | 1) Head hitting 2) Kicking surfaces 3) Knee/Leg banging 4) Skin picking 5) Skin pinching |
0.2 | 3.7 | n/a | Social-A | E |
Note. Part. = Participant number; Group = Subcategory or subclassification of function used to group participant; n/a = not applicable; ASIB = automatically maintained SIB; Social = socially maintained SIB; A = attention; E = escape; T = tangible.
= Additional functions for SIB found either in the same or some other functional analysis.
= Participant’s self-restraint data were gathered from an analogous no interaction condition.
Structured criteria (an objective and replicable standard) were used to determine the function of SIB as discussed in Rooker et al. (2018). In addition, for each individual with ASIB, the subtype was identified using the criteria described by Hagopian et al. (2017). If an individual’s FA indicated any form of SIB was automatically maintained, the individual was grouped as automatic and into the appropriate subtype. If an individual’s FA indicated SIB was socially maintained and no form of SIB was automatically maintained, the individual was grouped as social. In all cases, multiple phases of the FA were conducted with design or procedural modifications (cf. Hagopian et al., 2013) to clarify the function of SIB. To classify individuals in the current study based on function, we chose the analysis or phase with the strongest design that had clear, conclusive results regarding the function and that had most recently been conducted. Based on the outcome of these analyses, individuals were assigned to one of three groups: Subtype 2 group (n = 6), Subtype 3 group (n = 8), or the Social group (n = 9). No individual’s SIB met criteria for classification as Subtype 1 ASIB. Although no individuals in the social group had any form of SIB maintained by automatic reinforcement, social reinforcement could not be ruled out as one of the variables maintaining SIB for one individual in the Subtype 2 group and three individuals in the Study 3 group (see Table 2). In the social group, six individuals were found to have SIB maintained by a single social function, and three individuals were found to have SIB maintained by multiple social functions (see Table 2).
SIT Scale.
Injuries were scored using procedures similar to those described by Iwata et al. (1990), including data on the location, number, type, and severity of injury. Data across all injury characteristics were collected by trained coders (see below for training procedures) who completed the SIT Scale by directly observing the participant. The SIT Scale data sheet and scoring guidelines are available as Supporting Information.
Location of injury.
Data were collected on injuries across all 21 segments of the body. The injury sites were then grouped based on the superordinate categories described by Iwata et al. (1990; i.e., head, torso, and extremities). We also present data using the following subordinate categories: (a) the upper head (including the scalp and forehead), (b) the ears (including left and right ear), (c) the eyes (including left and right eye, as well as left and right eye area), (d) the lower head (including the face, nose, and lips/tongue), (e)the upper torso (including the neck/throat, left and right shoulders, and left and right chest), (f) the lower torso (including the stomach and back), (g) the arms (including the left and right upper arms, the left and right lower arms, the left and right hands/fingers), (h) the legs (including the left and right upper legs and low legs/ankles), and (i) the feet (including the left and right foot/ toe). These categories were used only for ease of data presentation (i.e., Figure 1) and data analysis was not conducted on these subordinate categories.
Figure 1.
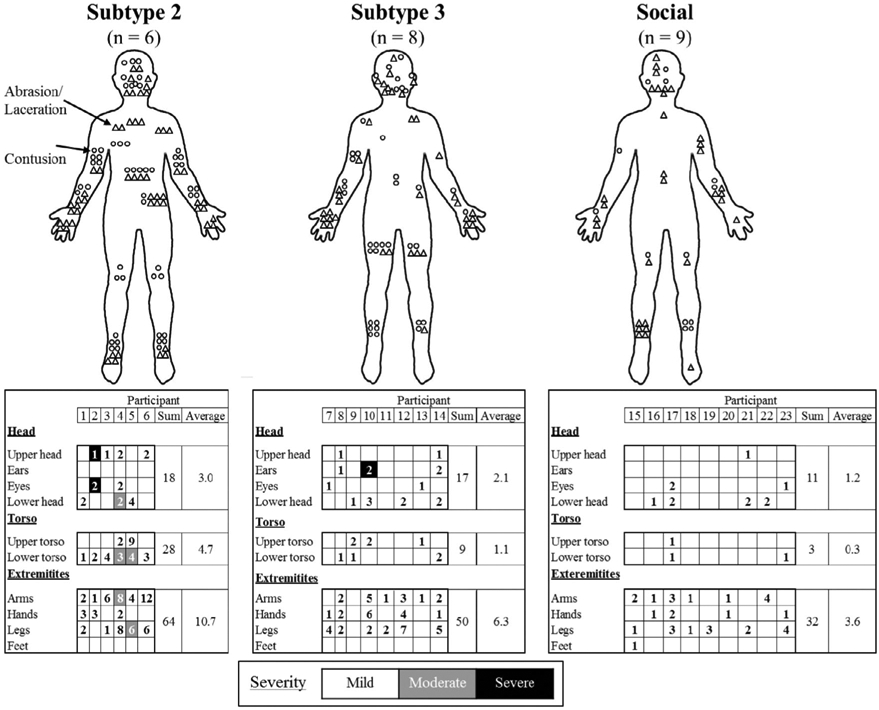
Injury characteristics for all individuals across groups. Top panel (body images) shows the type: abrasion/laceration (triangle) or contusion (circle), and approximate location of each injury in each group. Bottom panel shows the the number (denoted by the number) and severity of injuries for each participant (denoted by the shading of the box): mild (white box with number), moderate (grey box with number), and severe (black box with number). For two individuals at two locations, two different severities of injuries were noted (Participant 4, six mild and two moderate on the arms; participant 5, one mild and three moderate on the lower torso); in these cases the box is shaded to indicate the more severe injury.
Number of injuries.
For each participant, the number of injuries in a particular location was coded on the number scale from 0 to 3 (where 0 = no injuries, 1 = one injury, 2 = two to four injuries, and 3 = five or more injuries). We then coded numbers for each person both over-all and at particular superordinate sites (e.g., the head).
Type of injury.
Each injury was noted as an abrasion/laceration (a break in the skin) or a contusion (a distinct area marked by abnormal colorization or swelling).
Severity of injury.
A severity score of 1 (i.e., mild tissue damage), 2 (i.e., moderate tissue damage), or 3 (i.e., severe tissue damage) was determined based on the type of injury. The severity scoring criteria for abrasion/laceration and contusion was identical to that described by Iwata et al. (1990).
Estimate of current risk.
An estimate of current risk was calculated by incorporating the location, number, type, and severity of injury. This was done by examining the injuries scored with reference to the definitions of low, moderate, and high risk (see Iwata et al., 1990, and Supporting Information for details).
Administration and scoring.
The SIT Scale was completed as soon as possible after admission to the inpatient unit (i.e., at admission and retrieved after consent was obtained, as soon as consent had been obtained2). The single-time immediate assessment was used because efforts to heal existing injuries and prevent injuries are initiated immediately upon admission. Measuring injuries that were present before intensive clinical interventions could be applied was done to better reflect the individual’s capacity for causing injuries and allow us to examine differences across functional classes of SIB. Measuring injuries later, after intensive treatment and monitoring, would inform us about the effectiveness of treatment and the clinical teams’ ability to keep an individual safe (reflecting the behavior of others rather than that of the 23 participants), which was not the purpose of the current study.
SIT Scale training.
Registered nurses and research assistants, who worked on the inpatient unit to which the participants were admitted, were trained to code injuries using the SIT Scale using the following steps. First, 10 images that contained a variety of injury characteristics were identified and obtained from a Google images search (Google Images™ search services) of “abrasion”, “laceration”, and “contusion”. Next, the number, type, and severity of the depicted injury were scored by the sixth author, a senior nurse who oversaw the inpatient nursing staff and had a long history of care for SIB-related injury. To train a new coder, the senior nurse (or a previously trained coder) reviewed the scoring definitions and rules with the new coder, as well as answered any questions from the new coder. Next, the new coder independently scored the 10 images of injuries. For each image, the new coder scored the number, type, and severity of the depicted injury. Finally, agreement was calculated between the scoring completed by the new coder and the senior nurse for each image. If agreement was 90% or greater for each image (across injury characteristics), training was complete. If agreement was less than 90%, the trainer reviewed the disagreements and answered any relevant questions. The training steps were then repeated with 10 novel images (identified in the same manner) until agreement was at least 90% agreement with 10 novel images.
Interobserver Agreement
Functional analysis.
For 22 individuals, two clinicians or two research assistants simultaneously, but independently, collected data on average for 47.7% (range: 21.4 %-100.0%) of FA sessions across participants. For these 22 individuals, interobserver agreement (IOA) was calculated for each form of SIB, which was individually defined, using the partial-agreement-within-intervals method (Mudford, Martin, Hui, & Taylor, 2009). Each session was divided into consecutive 10-s bins, and the smaller number of recorded responses in each bin was divided by the larger number of recorded responses for each bin and multiplied by 100. Agreement was averaged across all 10-s bins for each form of SIB. Mean IOA across participants was 95.5% (range: 82.1%-100.0%). For one individual, no IOA was collected during the FA that was interpreted to determine group assignment. However, IOA was collected in a methodologically identical FA where data were collected on SIB (same response definitions and data collectors) in 34.6% of sessions with a high degree of agreement (M = 91.3%; range: 66.7%-100.0%).
SIT Scale.
Two coders independently completed the SIT Scale on 43.5% of participants. Exact agreement for the number score, the type of injury, and severity for each injury was calculated. The location of injury was implicit in each of these calculations. For each item, an agreement was counted if both observers scored the same number (e.g., number score of 1 on the left ear), same type of injury (e.g., abrasion on left ear), and the same severity of injury (e.g., severity 2 on the left ear) at each location. The number of agreements for each of these three characteristics (number, type, and severity) was then divided by the total number of locations and multiplied by 100 to obtain an agreement score for each administered scale. Agreement was then averaged across all scales in which a second observer collected data. Mean IOA across SIT Scales was 91.0% (range: 70.0%-100.0%) for number of injuries, 91.7% (range: 63.3%-100.0%) for type of injury, and 90.7 % (range: 63.3%-100.0%) for severity of injury. Because the range of IOA indicated some SIT Scales had only moderate agreement, we conducted additional analyses. Of the 10 scales that had IOA, agreement was highly consistent for seven scales (Ms = 100% agreement for number, 99.5% agreement for type, and 100% agreement for severity). For the remaining three scales, there were more disagreements (SIT Scales for Participants 8, 10, and 17). For Participant 10 (79.4% agreement for number, 93.3% agreement for type, and 82.8% agreement for severity), the secondary observer appeared to have consistently and incorrectly recorded data by switching values recorded for the number and severity of injuries (i.e., recording the number in the severity column and the severity in the number column), potentially reflecting a data collection error rather than an observation error. For Participant 17 (68.3% agreement for number, 70.0% agreement for type, and 70.0% agreement for severity), the secondary observer recorded injuries at five sites with near perfect agreement with the primary observer, but did not score any injuries at the other nine sites where the primary observer recorded injuries. The source of disagreements for Participant 8 (71.7% agreement for number, 63.3% agreement for type, and 66.8% agreement for severity) is unclear. Neither the primary nor secondary data collectors for these three participants collected data on any other SIT Scale.
Data analysis.
In the current study, we examined differences in injury characteristics related to (a) categorical function/subtype group (Subtypes 2 and 3 ASIB, and socially maintained SIB) and (b) rate of responding and level of differentiation in relevant test and control conditions of the FA used to determine group assignment. Rate of SIB was selected for analysis, as the number of times an individual engages in SIB could be directly related to injuries. Percentage differentiation in the FA was selected for analysis, as this dimension of responding has been shown to predict response to treatment (Hagopian, Rooker, & Yenokyan, 2018), and thus, may be an important variable related to injuries.
Descriptive statistics were generated to examine differences in injury characteristics between groups and, when appropriate, statistical tests of significance were performed to examine difference across groups of individuals. Group differences related to injury characteristics were assessed using nonparametric statistical tests due to the small sample sizes included in this study. Secondarily, the mean rate of SIB from the relevant FA test and control conditions, as well as the differentiation between these conditions were correlated with the number of injuries across groups. For this analysis, a nonparametric test was selected to examine correlations (Spearman rho) because it was possible for individuals both within and across groups to have the same number of injuries but different mean rates of SIB or levels of differentiation in the FA, and because the sample size was inadequate for more advanced statistical modeling (e.g., regression analysis). Statistical analyses were completed using SPSS v. 22 or GraphPad Prism v. 7.04.
RESULTS
Functional Analysis Results
Of the 23 participants included in the study, six met the criteria for Subtype 2 ASIB, eight met the criteria for Subtype 3 ASIB, and nine met criteria for socially maintained SIB. Table 2 shows the rate of SIB in relevant FA conditions and outcomes of subtype classification for each individual. Although detailed rules for subtype classification can be found in Hagopian et al. (2017), we describe the general features of these FAs. Classification of Subtype 2 ASIB was determined through quotient scores for five individuals (i.e., < .5). For the remaining individual, the percentage of over-lapping data points indicated Subtype 2 ASIB. For these individuals, the rate of SIB in the alone or ignore conditions ranged from 1.2 RPM to 32.2 RPM and the rate of SIB ranged from 1.3 RPM to 33.5 RPM in the play condition. Differentiation in the FA was negative (indicating response rate was higher in the plan condition than the alone or ignore condition) for four of the six individuals with Subtype 2 ASIB (range: -162.5%-26.3%). Classification of Subtype 3 ASIB was determined by the percentage of sessions with self-restraint occurring in the FA ignore or alone conditions (in at least 30% of the alone or ignore sessions, self-restraint occurred in at least 25% of the session). For individuals with Subtype 3 ASIB, the percentage of the session with self-restraint (when it was permitted) across FA or analogous conditions ranged from 63.3% to 100%. For these individuals, the rate of SIB (when self-restraint was blocked) in the alone or ignore conditions ranged from 1.9 RPM to 36.8 RPM and the rate of SIB in play condition ranged from 0 RPM to 32.3 RPM. Differentiation in the FA was negative for one of eight individuals with Subtype 3 ASIB (range: -78.3%-100%). For the nine individuals with socially maintained SIB, the rate of SIB in the relevant social test ranged between 0.3 and 3.8 RPM and the rate of SIB in the play condition ranged between 0 RPM and 0.2 RPM. Differentiation in the FA was always positive for these individuals (range: 94.6%-100%).
The Relation between Functional Class and Injury Characteristics
Figure 1 (top panel) shows the number of injuries by location (approximate) and type of injury for every participant in each group; the bottom panel shows the number and severity of injuries using the superordinate and subordinate categories. The number of injuries refers to the number score and the severity of injury refers to the severity score. The key differences are discussed below; however, across functional classes, differences in terms of the absolute numbers and types of injuries are actually greater than they appear as there are fewer participants with Subtypes 2 and 3 ASIB than with socially maintained SIB.
Injury location.
Every participant with Subtype 2 ASIB (6 of 6 cases) had at least one injury to each of the superordinate sites (head, torso, and extremities). In comparison, individuals with other functional classes of SIB were less likely to have injuries at all locations. Only four of eight (50%) individuals with Subtype 3 ASIB and two of nine (22.2%) with socially maintained SIB had at least one injury at all locations. A Kruskal-Wallis test indicated that there was a significant effect of group on the number of injury locations (H = 8.43, p = .015). Pairwise comparisons with a Bonferroni correction indicated that the Subtype 2 group was significantly different than the Social group (p = .011).
Injury number.
Individuals with Subtype 2 ASIB generally had the most injuries, ranging from 9 to 29 (Mdn. = 17.5); followed by Subtype 3 ASIB who had 3 to 20 injuries (Mdn. = 7.5); and those with socially maintained SIB had the least injuries, ranging from 2 to 14 (Mdn. = 4). A Kruskal-Wallis test with a Bonferroni correction indicated a significant difference in groups (H = 8.31, p = .016); specifically, there were significantly more injuries in the Subtype 2 group than the Social group (p = .012). No other significant differences were found across groups on this injury characteristic.
Injury type.
As seen in Figure 1 (top panel), although the number of individuals included are small, there appeared to be some difference in the proportion of abrasions/lacerations and contusions across individuals. Individuals with Subtype 3 ASIB were most likely to have both abrasions/lacerations and contusions (75% of individuals had both types of injuries). A similar but slightly lower proportion of individuals with Subtype 2 ASIB had injuries of both kinds (66.7% of individuals). In comparison, only 44% of individuals with socially maintained SIB had both kinds of injuries. When only one type of injury was observed for a given participant, the injury was more likely to be a contusion for those with Subtype 2 ASIB (2 of 2 individuals), an abrasion/ laceration for those with socially maintained SIB (4 of 5 individuals), or equally likely to be an abrasion/laceration or contusion for those with Subtype 3 ASIB group (two individuals in the that group each with a different type of injury). This finding should be considered preliminary given the small number of individuals.
Injury severity.
Figure 1 (bottom panel) shows the number and severity of injuries at the superordinate and subordinate levels of the body. Across all participants, a total of five injuries classified as “severe” were observed. Three were observed in one individual with Subtype 2 ASIB (participant 2). Two were observed in one individual with Subtype 3 ASIB (participant 10). No participants with socially maintained SIB had severe injuries. Three of six of the individuals with Subtype 2 ASIB (50%) were found to have either a moderate or severe injury. In contrast, only one individual with Subtype 3 ASIB (12.5%), and no individuals with socially maintained had a moderate or severe injury. Thus, injuries of greater severity (moderate and severe) were most often observed in individuals with Subtype 2 ASIB, and did not occur for any individual with socially maintained SIB. The importance of this finding is unknown given the numbers of individuals across groups.
Current estimated risk.
Based on the interaction of these injury characteristics (number, location, type, and severity), a “current estimated risk” was calculated based on procedures described by Iwata et al. (1990). For example, high risk would be indicated by two contusions to the head with a severity of 2 or any injury with severity 3 (e.g., Figure 1, participant 10). One individual with Subtype-2 (Participant 2) and one with Subtype-3 ASIB (Participant 10) were found to be at the highest level of risk. However, for all other individuals across groups, the estimated risk was low.
Severity by location.
Rooker et al. (2018) found differences in the severity of injury by the location of that injury as related to functional class (e.g., individuals in the Automatic group had significantly more severe head injuries than individuals in the Social group). Thus, we also investigated injury severity ratings by injury location. Notably, for the individuals who had the most severe injuries (Participants 2 and 10, who had Subtype 2 and 3 ASIB, respectively), these injuries were to the head. In addition, two participants with Subtype 2 ASIB also had moderate injuries (severity score of 2) to the torso and extremities (Participants 4 and 5); in both of these cases, these injuries were abrasions/lacerations.
The Relation between Functional Analysis Results and Injury Number
Figure 2 depicts the relations between the level of differentiation of SIB in the FA (x-axis) and the number of injuries (y-axis) for each participant. We determined the mean rate of SIB in the relevant test and control conditions of the FA (see Table 2), and calculated the level of differentiation using the formula described in the data analysis section. An outcome near + 100 indicated a lower level of SIB in the control relative to the test condition. An outcome near 0 indicated relatively equal rates of SIB in the control and test. A negative outcome (e.g., near -100) indicated a lower level of SIB in the test condition in comparison to the control condition. Generally, the higher the level of positive differentiation, the fewer the number of injuries observed and vice versa. When these data were subjected to a correlational analysis (Spearman’s rho), a moderate negative correlation was obtained (r = -.57; p = .004). Interestingly, there was no apparent relation between number of injuries and the absolute rate of SIB in the test condition (r = .23, p > .05); however, the rate of SIB in the play condition had a moderate positive correlation with the number of injuries (r = .50, p = .015). Collectively, these data suggest that the level of differentiation of SIB in the FA (and to a lesser extent, the rate of SIB in the play condition) is related to the number of injuries.
Figure 2.
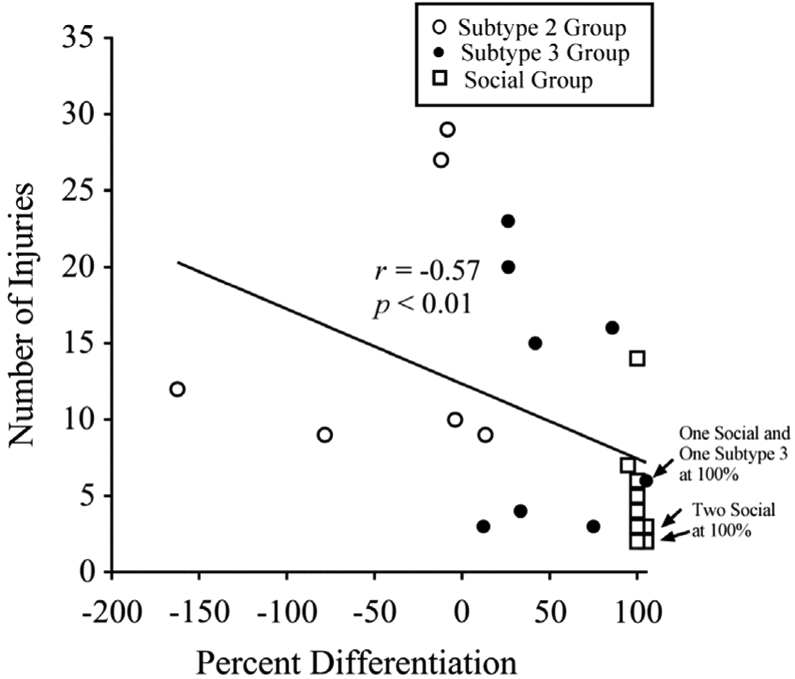
The percentage differentiation plotted against the number of injuries from the Self-Injury Trauma Scale for each participant. Icon shape indicates the participant’s group. When the same level of differentiation and number of injuries were present for two individuals, the data point for one of these individuals was nudged to the right. In all cases, this occurred with 100% differentiation.
DISCUSSION
The current study replicated and expanded upon the differences in injury characteristics across functional classes of SIB reported by Rooker et al. (2018). In the current study, we found that a greater proportion of individuals with Subtype 2 ASIB had more injuries and had injuries to all body sites (head, torso, and extremity). This difference was most dramatic in comparison to individuals with socially maintained SIB, where only one individual had injuries in a similar range (Participant 17), and fewer individuals had injuries to all body sites. Further, the more severe injuries were found in a greater proportion of individuals with Subtype 2 ASIB in comparison individuals with Subtype 3 ASIB or socially maintained SIB. Individuals with Subtype 3 ASIB tended to have less severe injury characteristics than individuals with Subtype 2 ASIB. This may be because these individuals may have mitigated injury production by engaging in self-restraint, which is the defining feature of Subtype 3 ASIB.
Further replication is needed, ideally by other research groups using larger samples, including participants with Subtype 1 ASIB. However, these findings suggest that, in addition to Subtype 2 ASIB being highly resistant to treatment (Hagopian et al., 2018), this class of behavior is also more dangerous (i.e., produces more injuries and more severe injuries). These results also suggest that the rate of SIB in the FA test condition is less important to injury production than the relative rate of SIB across FA test and control conditions. Put another way, the number of contexts in which an individual engages in SIB would seem to be the most relevant variable to injuries. These results provide another level of evidence that once Subtype 2 ASIB is identified for a client, a practitioner may want to seek additional resources (e.g., set caregiver expectations, consult additional experts, request more hours of treatment, refer to an intensive treatment provider) as treatment is likely to be difficult (Hagopian et al., 2017) and injury is more likely.
In addition, the finding that functional classes of SIB are associated with different injury characteristics appears robust and warrants additional research. At this point we can only speculate on why socially and automatically maintained SIB may differ with respect to injuries. It seems possible that function of SIB may affect its form (rate, location, topography, etc.), which in turn could influence the injuries that are a product of this response. With socially maintained SIB, SIB occurs to produce a consequence such as attention or escape mediated by another person, thus injuries may be a collateral by-product of the behavior. One possible reason why individuals with socially maintained SIB may have fewer and less severe injuries (and specifically avoid the head) is because they may be able to maximize access to social reinforcement without incurring painful contingencies associated with injury resultant from repeated blows to the same area of the body. If the only purpose of engaging in SIB is to produce social reinforcement, then the topography of SIB may be distributed over more areas of the body (e.g., shifting to avoid previously targeted and traumatized areas, avoiding the head area) to avoid aversive consequences.3
With ASIB, however, the source of reinforcement could be the endogenous consequences of the behavior, including the observable injury (which requires repeated trauma to be produced). That is, with ASIB, the injury may be either a collateral by-product of endogenous reinforcement (e.g., sensory stimulation associated with hits or bites) or the injury may directly provide reinforcement itself (e.g., sensory stimulation of the injury). Thus, rather than distributing SIB across the body to avoid aversive contingencies, the traumatized area may be repeatedly targeted and ultimately suffer an observable injury. From this perspective, the finding from the current study (as well as Rooker et al., 2018) that individuals with ASIB are more likely to produce severe injuries to the head is particularly noteworthy. It seems that blows to the head area would likely produce a different quality of endogenous contingency than blows to the torso or extremities. These studies were not designed to answer these questions, but they have demonstrated that injuries differ across functional classes of SIB, and that Subtype 2 ASIB appears to be associated with injuries that are greater in number and severity and disproportionally on the head. This observation requires further replication and provides an empirical basis for further study on this topic.
The current study has a number of limitations. It would have been ideal for all SIT Scales to be collected immediately upon admission to control for events that may have altered injury over the course of the inpatient admission. However, no differences in injury characteristics were detected when comparing individuals who received the SIT Scale at admission or consent. Further, there is no guarantee that the injuries observed were the direct result of SIB, as they likely occurred prior to admission. Similarly, we only administered the SIT Scale at a single time point. We believe that injury at that initial time point would provide a more representative sample of injuries compared to obtaining repeated measures of injury while highly intensive interventions were in place 24 hr per day to minimize injury and heal existing injuries. In addition, direct analysis of specific aspects of the form of SIB that led to injury was not possible as some injuries can appear long after the response that produced it was emitted. The operational definitions for SIB in the current FAs often include multiple topographies of SIB. For example, head-directed SIB might be defined to include instances of head banging, head hitting (including slapping), and hair-pulling. Thus, even reviewing each instance of SIB observed in the FA did not allow for demarcating responses that may be more likely to produce abrasions/lacerations (i.e., sharp trauma from the nails and teeth) and contusions (i.e., blunt trauma from the fist or a flat surface in the environment) in all cases. Future research should endeavor to better understand what forms and patterns of SIB lead directly to injury and what forms of self-restraint may limit injuries. This research could be conducted in a similar manner as Wilson et al. (2012), who were able to quantify instances of SIB and the production of injuries at a local level.
There were also limitations related to sample characteristics. The sample in the current study is arguably in the upper end of the distribution for severity of SIB; thus, it is unclear if our findings would generalize to a population with less severe SIB. However, we were specifically interested in ASIB, which can be resistant to treatment. It seems plausible that Subtypes 2 and 3 ASIB cases will tend to engage in frequent and severe forms of SIB, which make them appropriate groups to study with regard to injury characteristics. There were no cases with Subtype 1 ASIB in the current study. This was not because we excluded Subtype 1, but because no Subtype 1 cases were admitted to our unit during the time of the study. Future research may attempt to compare all three ASIB subtypes. Finally, the relatively small sample size limits our ability to fully examine the relations between the various injury characteristics and the many dimensions of SIB. Therefore, our findings should be considered preliminary and used as a springboard for further research. Replicating the current study with a larger sample certainly should be a goal for future research on this topic. That said, the fact that some differences were found between functional classes and subtypes of SIB replicates Rooker et al. (2018), which may suggest the generality of these findings.
Supplementary Material
Acknowledgments
Manuscript preparation was supported by Grant R01 HD076653 and from the Eunice K. Shriver National Institute of Child Health and Human Development (NICHD). The contents are solely the responsibility of the authors and do not necessarily represent the official views of NICHD.
Special thanks to the members of the Nursing Department of the Neurobehavioral Inpatient Unit, without whom this research could not have been conducted. Additionally, we would like to thank Michelle Frank-Crawford for her assistance in conducting this research.
Footnotes
For one individual (Participant 11), data on self-restraint was gathered from an additional assessment. In the initial FA, although self-restraint occurred, it did not meet the requirement for formal characterization as Subtype 3 ASIB. However, in subsequent assessments and treatments, self-restraint consistently occurred for long durations in sessions. Thus, self-restraint data from an extended ignore period were used to determine Subtype 3 ASIB.
Twelve participants had a SIT Scale administered upon admission to the inpatient hospital. The remaining 11 participants had the SIT Scale administered upon enrolling in this study. There were no significant differences on SIT Scale scoring of any injury characteristic between these two groups.
Further, these individuals may be more likely to engage in alternative behavior (e.g., aggression, disruption) to obtain these social consequences. It is beyond the scope of this analysis, and beyond our ability given the purpose of the study, to specifically address how response class hierarchies of problem behavior may reduce the instances of SIB-related injury. However, review of data from all assessments of SIB and other major target behaviors conducted with these individuals indicates that individuals in the Social group were more likely to have engaged in aggression (77.8% of individuals) or disruption (77.8% of individuals), than individuals in the Subtype 2 group (50% of individuals engaged aggression and 50% of individuals engaged in disruption) or the Subtype 3 group (62.5% of individuals engaged aggression and 62.5% of individuals engaged in disruption).
Contributor Information
Griffin W. Rooker, THE KENNEDY KRIEGER INSTITUTE AND JOHNS HOPKINS UNIVERSITY SCHOOL OF MEDICINE
Louis P. Hagopian, THE KENNEDY KRIEGER INSTITUTE AND JOHNS HOPKINS UNIVERSITY SCHOOL OF MEDICINE AND UNIVERSITY OF MARYLAND, BALTIMORE COUNTY
Jessica L. Becraft, THE KENNEDY KRIEGER INSTITUTE AND JOHNS HOPKINS UNIVERSITY SCHOOL OF MEDICINE
Noor Javed, THE KENNEDY KRIEGER INSTITUTE AND UNIVERSITY OF MARYLAND, BALTIMORE COUNTY.
Alyssa B. Fisher, THE KENNEDY KRIEGER INSTITUTE
Katharine S. Finney, THE KENNEDY KRIEGER INSTITUTE
REFERENCES
- Cooper S, Smiley E, Allan LM, Jackson A, Finlayson J, Mantry D, & Morrison J (2009). Adults with intellectual disabilities: Prevalence, incidence and remission of self-injurious behaviour, and related factors. Journal of Intellectual Disability Research, 53, 200–216. 10.1111/j.1365-2788.2008.01060.x. [DOI] [PubMed] [Google Scholar]
- Flay BR, Biglan A, Boruch RF, Castro FG, Gottfredson D, Kellam S, ... Ji P (2005). Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prevention Science, 6, 151–175. 10.1007/s11121-005-5553-y. [DOI] [PubMed] [Google Scholar]
- Hagopian LP, Rooker GW, Jessel J, & DeLeon IG (2013). Initial functional analysis outcomes and modifications in pursuit of differentiation: A summary of 176 inpatient cases. Journal of Applied Behavior Analysis, 46, 88–100. 10.1002/jaba.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagopian LP, Rooker GW, & Yenokyan G (2018). Identifying predictive behavioral markers: A demonstration using automatically reinforced self-injurious behavior. Journal of Applied Behavior Analysis, 51, 443–465. 10.1002/jaba.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagopian LP, Rooker GW, & Zarcone JR (2015). Delineating subtypes of self-injurious behavior maintained by automatic reinforcement. Journal of Applied Behavior Analysis, 48, 523–543. 10.1002/jaba.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagopian LP, Rooker GW, Zarcone JR, Bonner AC, & Arevalo AR (2017). Further analysis of subtypes of automatically reinforced SIB: A replication and quantitative analysis of published datasets. Journal of Applied Behavior Analysis, 50, 48–66. 10.1002/jaba.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall SS, Hustyi KM, Chui C, & Hammond JL (2014). Experimental functional analysis of severe skin-picking behavior in Prader-Willi syndrome. Research in Developmental Disabilities, 35, 2284–2292. 10.1016/j.ridd.2014.05.025. [DOI] [PubMed] [Google Scholar]
- Hunsley J, & Lee CM (2007). Informed benchmarks for psychological treatments: Efficacy studies, effectiveness studies, and beyond. Professional Psychology: Research and Practice, 38, 21 10.1037/0735-7028.38.1.21. [DOI] [Google Scholar]
- Hustyi K, Hammond JL, Rezvami AB, & Hall SS (2013). An analysis of the topography, severity, potential sources of reinforcement, and treatments utilized for skin picking in Prader-Willi syndrome. Research in Developmental Disabilities, 34, 2890–2899. 10.1016/j.ridd.2013.06.014. [DOI] [PubMed] [Google Scholar]
- Hyman SL, Fisher W, Mercugliano M, & Cataldo MF (1990). Children with self-injurious behavior. Pediatrics, 85, 437–441. Accessed at:. https://pediatrics.aappublications.org/content/85/3/437.abstract. [PubMed] [Google Scholar]
- Iwata BA, Dorsey MF, Slifer KJ, Bauman KE, & Richman GS (1982/1994). Toward a functional analysis of self-injury. Journal of Applied Behavior Analysis, 27, 197–209. (Reprinted from Analysis and Intervention in Developmental Disabilities, 2, 3-20, 1982). 10.1901/jaba.1994.27-197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata BA, Pace GM, Dorsey MF, Zarcone JR, Vollmer TR, Smith RG, ... Willis KD (1994). The functions of self-injurious behavior: An experimental-epidemiological analysis. Journal of Applied Behavior Analysis, 27, 215–240. 10.1901/jaba.1994.27-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata BA, Pace GM, Kissel RC, Nau PA, & Farber JM (1990). The Self-Injury Trauma (SIT) Scale: A method for quantifying surface tissue damage caused by self-injurious behavior. Journal of Applied Behavior Analysis, 23, 99–110. 10.1901/jaba.1990.23-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahng S, Iwata BA, & Lewin AB (2002). Behavioral treatment of self-injury, 1964 to 2000. American Journal on Mental Retardation, 107, 212–221. . [DOI] [PubMed] [Google Scholar]
- McDonough M, Hillery J, & Kennedy N (2000). Olanzapine for chronic, stereotypic self-injurious behaviour: A pilot study in seven adults with intellectual disability. Journal of Intellectual Disability, 44, 677–684. 10.1111/j.1365-2788.2000.00306.x. [DOI] [PubMed] [Google Scholar]
- Mudford OC, Martin NT, Hui JK, & Taylor SA (2009). Assessing observer accuracy in continuous recording of rate and duration: Three algorithms compared. Journal of Applied Behavior Analysis, 42, 527–539. 10.1901/jaba.2009.42-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi A, Costanza C, Umberto B, & Filippo M (2014). Non-pharmacological treatments in autism spectrum disorders: An overview on early interventions for preschoolers. Current Clinical Pharmacology, 9, 17–26. 10.2174/15748847113086660071. [DOI] [PubMed] [Google Scholar]
- Patton N (2004). Self-inflicted eye injuries: A review. Eye, 18, 867–872. 10.2174/15748847113086660071. [DOI] [PubMed] [Google Scholar]
- Rooker GW, Hausman NL, Fisher AB, Gregory MK, Lawell JL, & Hagopian LP (2018). Classification of injuries observed in functional classes of self-injurious behavior. Journal of Intellectual Disabilities Research, 62, 1086–1096. 10.1111/jir.12535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soke GN, Rosenberg SA, Hamman RF, Fingerlin T, Robinson C, Carpenter L, ... DiGuiseppi C (2016). Brief report: Prevalence of self-injurious behaviors among children with autism spectrum disorder: A population-based study. Journal of Autism and Developmental Disorders, 46, 3607–3614. 10.1007/s10803-016-2879-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twohig MP, & Woods DW (2001). Habit reversal as a treatment for chronic skin picking in typically developing adult male siblings. Journal of Applied Behavior Analysis, 34, 217–220. 10.1901/jaba.2001.34-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer TR (1994). The concept of automatic reinforcement: Implications for behavioral research in developmental disabilities. Research in Developmental Disabilities, 15, 187–207. 10.1016/0891-4222(94)90011-6. [DOI] [PubMed] [Google Scholar]
- Vollmer TR, Hagopian LP, Bailey JS, Dorsey MF, Hanley GP, Lennox D, . Spreat S (2011). The Association for Behavior Analysis International position statement on restraint and seclusion. The Behavior Analyst, 34, 103–110. 10.1007/BF03392238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DM, Iwata BA, & Bloom SE (2012). Computer-assisted measurement of wound size associated with self-injurious behavior. Journal of Applied Behavior Analysis, 45, 797–808. 10.1901/jaba.2012.45-797. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


