Introduction
The COVID-19 pandemic has put the world in a state of emergency. In addition to the impact of the virus itself, the World Health Organization (WHO) has raised concern over the impact of the societal changes associated with the pandemic – for example, social distancing, quarantine, lockdown and economic recession – on the mental health of the affected populations (WHO, 2020). We recently reported results from wave 1 of the COVID-19 Consequences Denmark Panel Survey 2020 (CCDPS 2020 – fielded from March 31 to April 6, 2020), which showed that (1) the level of psychological well-being as reported on the WHO five-item well-being scale [WHO-5 (Topp et al., 2015)] was reduced compared to comparable data from the Danish Mental Health and Well-Being Survey 2016 (DMHWBS 2016) (Nielsen et al., 2017), and (2) that the level of psychological well-being correlated negatively with levels of self-reported symptoms of anxiety and depression (Sønderskov et al., 2020). These findings are consistent with those from studies of mental health from other countries and settings affected by the COVID-19 pandemic (Wang et al., 2020, Vindegaard & Eriksen Benros, 2020, Rohde et al., 2020).
A pandemic is a dynamic phenomenon, and mental health of the affected populations is plausibly equally dynamic. To study this, we conducted a follow-up survey to gauge the mental health of the Danish population approximately 3 weeks after wave 1 of the CCDPS 2020. Here, we report the results from wave 2 of the CCDPS 2020 and compare them to those from wave 1.
Methods
We commissioned the survey agency Epinion, which undertook wave 1 of the CCDPS 2020, to conduct a follow-up survey (wave 2) targeting the same sample of people and containing the same questions pertaining to psychological well-being/distress [the WHO-5 and the six questions regarding the experienced level of anxiety/depression over the past 2 weeks reported on a scale from 0 (not present) to 10 (present to an extreme degree)]. Wave 2 was fielded from April 22 to April 30, 2020 and was completed by 2149 respondents who also had responded to wave 1 of the survey, resulting in a retention rate of 87.4% (2458 individuals responded to wave 1). After weighting (applied in all analyses), the sample is representative of the population on key demographic and political variables (gender, age, education, region and party choice in the last election).
We compared the following indicators of psychological well-being/distress in the two waves of the CCDPS 2020 survey: the WHO-5 scores (paired sample t-test) and reported symptom levels of anxiety/depression (paired sample t-test). Lastly, we also compared the scores on the WHO-5 in the second wave of the CCDPS 2020 with those from the DMHWBS 2016 (see Nielsen et al. (2017) and the Supplementary Material in Sønderskov et al. (2020) for a description).
Results
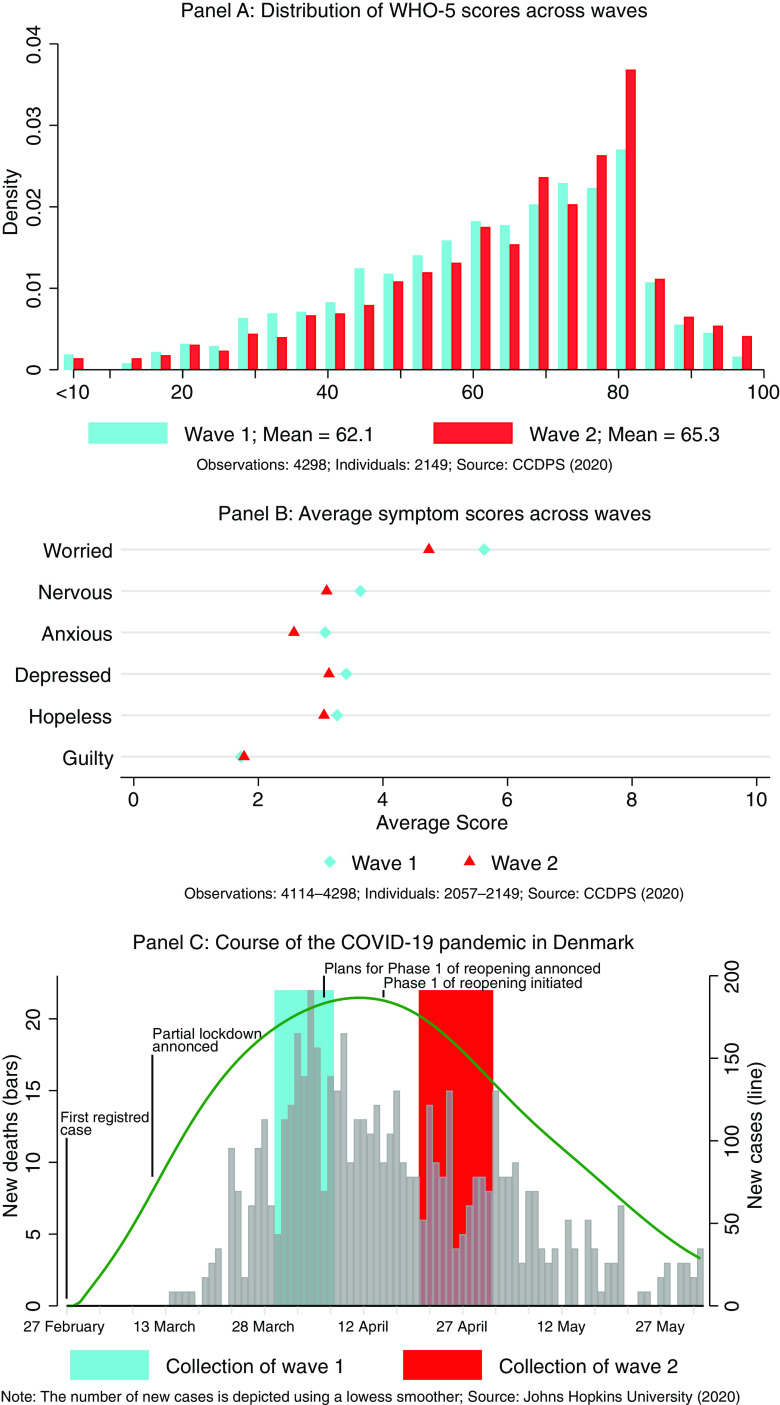
The mean age of the 2149 respondents who participated in both wave 1 and wave 2 in the CCDPS 2020 was 49.2 years and 51% were females. The mean WHO-5 score for these participants (see panel A in Fig. 1) was 62.1 for the total sample (64.8 for males and 59.5 for females) at wave 1 and 65.3 for the total sample (67.2 for males and 63.3 for females) at wave 2. This increase in self-reported well-being was statistically significant for the total sample (p < 0.001), for males (p < 0.001) and for females (p < 0.001). The mean scores on the self-reported anxiety/depression symptom items are shown in panel B in Fig. 1. There were statistically significant decreases from wave 1 to wave 2 on all symptoms except for feelings of guilt. The changes were most pronounced for worrying and feeling anxious. The WHO-5 scores at wave 2 were slightly higher than those from the DMHWBS 2016 (mean score: 64.3, 2-sided p-value for difference = 0.084).
Fig. 1.
Psychological well-being (panel A), symptoms of anxiety/depression (panel B) and pandemic development in the Danish population (panel C). Sources: The COVID-19 Consequences Denmark Panel Survey 2020 (CCDPS 2020) (Sønderskov et al., 2020) and (Johns Hopkins University, 2020).
Discussion
The main result of this study is that the psychological well-being of the Danish population seems to have increased from the first wave (March 31 to April 6, 2020) to the second wave (April 22 to April 30, 2020), possibly as a consequence of decreased symptoms of anxiety and depression. In support of this explanation, we found (post hoc) statistically significant negative correlations between changes in the level of each of the six anxiety/depression symptoms from wave 1 to wave 2 and changes in the WHO-5 scores from wave 1 to wave 2 (see the Supplementary Material). A main reason for this development may be the reduction in the spread of the coronavirus between the two waves of the survey and the associated societal response (see panel C in Fig. 1). Specifically, both the number of new COVID-19 cases (green curve in panel C) and the number of COVID-19 patients dying (grey bars in panel C) were markedly reduced from wave 1 to wave 2. The mean number of new COVID-19 cases/related deaths per day was 303/16 during wave 1 and 163/9 during wave 2. This progression was covered extensively in the news media and is therefore likely to be commonly known in the general population. In response to this development, the lockdown of the Danish society was gradually lifted between the two waves of the survey. Most notably perhaps, schools, kindergartens and other institutions, which had been closed from March 13, 2020, were gradually reopened on April 15, 2020. Many small businesses were allowed to reopen between the two survey waves as well. In other words, in the period separating the two surveys, the Danish society was slowly but safely approaching the pre-pandemic state, which is likely to have had a substantial positive impact on the mental health of the population.
In another two-wave survey of mental health/distress during the COVID-19 pandemic, Wang et al. (2020) found no differences in the levels of stress, anxiety and depression in the Chinese population from wave 1 (31st January to 2nd February – shortly after the initial outbreak in China) to wave 2 (28th February to 1st March – approximately at the apex of the pandemic in China). However, this survey used snowball sampling (population representation unclear) and the two waves consisted of (partly) different respondents, making it hard to draw any valid inferences regarding the development in well-being.
In conclusion, while we can by no means claim causality, the results of our study are intuitively compatible with psychological well-being, co-varying with the intensity of the COVID-19 pandemic and the associated societal restrictions. Valid longitudinal data on the mental health of populations that have been more severely affected by the COVID-19 pandemic than has been the case in Denmark are urgently needed.
Acknowledgements
The authors are grateful to the group behind the DMHWBS 2016 for making the results of this survey available for our analyses.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/neu.2020.26.
click here to view supplementary material
Author contributions
The study was designed by KMS, PTD and SDØ. The analyses were conducted by KMS. The results were interpreted by all authors. SDØ wrote the first draft of the manuscript, which was subsequently revised for important intellectual content by the remaining authors. All authors approved the final version of the manuscript prior to submission.
Financial support
This study was supported by an unconditional grant from the Novo Nordisk Foundation (Grant number: NNF20SA0062874), a grant from Independent Research Fund Denmark (Case number: 9038-00123B), and funding from the Department of Political Science, Aarhus University.
Conflicts of interest
None.
References
- Johns Hopkins University (2020). Novel Coronavirus (COVID-19) Cases - The Center for Systems Science and Engineering (CSSE). Available at https://github.com/CSSEGISandData/COVID-19/blob/master/csse_covid_19_data/csse_covid_19_time_series/time_series_covid19_confirmed_global.csv (accessed 9 June 2020).
- Nielsen L, Hinrichsen C, Santini ZI and Koushede V (2017). The Danish Mental Health and Well-Being Survey 2016. Copenhagen, Denmark: Statens Institut for Folkesundhed; Available at http://www.abcmentalsundhed.dk/media/1368/maaling_af_mental_sundhed.pdf (accessed 9 June 2020). [Google Scholar]
- Rohde C, Hougaard Jefsen O, Nørremark B, Aalkjær Danielsen A and Østergaard SD (2020). Psychiatric symptoms related to the COVID-19 pandemic. Acta Neuropsychiatrica, 1–3. doi: 10.1017/neu.2020.24 [DOI] [PubMed] [Google Scholar]
- Sønderskov KM, Dinesen PT, Santini ZI and Østergaard SD (2020) The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatrica 32(4), 226–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp CW, Ostergaard SD, Sondergaard S and Bech P (2015) The WHO-5 well-being index: a Systematic Review of the Literature. Psychotherapy and Psychosomatics 84, 167–176. [DOI] [PubMed] [Google Scholar]
- Vindegaard N and Eriksen Benros M (2020). COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain, Behavior, and Immunity. [DOI] [PMC free article] [PubMed]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Mcintyre RS, Choo FN, Tran B, Ho R, Sharma VK and Ho C (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. [DOI] [PMC free article] [PubMed]
- WHO (2020). World Health Organization: Substantial investment needed to avert mental health crisis. Available at https://www.who.int/news-room/detail/14-05-2020-substantial-investment-needed-to-avert-mental-health-crisis (accessed 9 June 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/neu.2020.26.
click here to view supplementary material