To the editor,
The article by Ren et al. reported that there was an extremely high incidence (85.4%) of lower extremity deep venous thrombosis (DVT) among 48 patients with severe coronavirus disease 2019 (COVID-19) in Wuhan, China [1]. As the global pandemic of COVID-19, there have been several studies on the incidence, risk factors, and preventive strategies of DVT [1–4]. However, the incidence of DVT has been reported diversely among different clinical centers. Thus, we performed a meta-analysis to estimate the pooled prevalence of DVT in confirmed COVID-19 patients.
We searched PubMed, EMBASE, Web of Science, and medRxiv databases until June 22, 2020, for relevant studies, using the keywords (“coronavirus” or “COVID-19” or “SARS-CoV-2” or “2019-nCoV”) and (“thrombosis” or “thrombi” or “thrombus”). In addition, we screened out the relevant potential articles in the references of selected studies. Articles reporting the prevalence of DVT in confirmed COVID-19 patients were included.
The pooled prevalence and its 95% confidence interval (CI) were used to estimate the combined effects. We calculated the prevalence estimates with the variance stabilizing double arcsine transformation [5, 6]. The heterogeneity among studies was assessed with the I2 statistic and Cochran’s Q test. The meta-regression and subgroup analysis were used to investigate the potential heterogeneity sources (such as sample size, prevalence of prophylaxis in COVID-19 patients, location, design of studies, screening methods of DVT, and COVID-19 patients in intensive care unit (ICU)). We chose Egger’s test and Begg’s test to assess publication bias. All analyses were performed using the Stata 11.2 (StataCorp, College Station, TX), and a two-tailed P value < 0.05 was considered to be statistically significant.
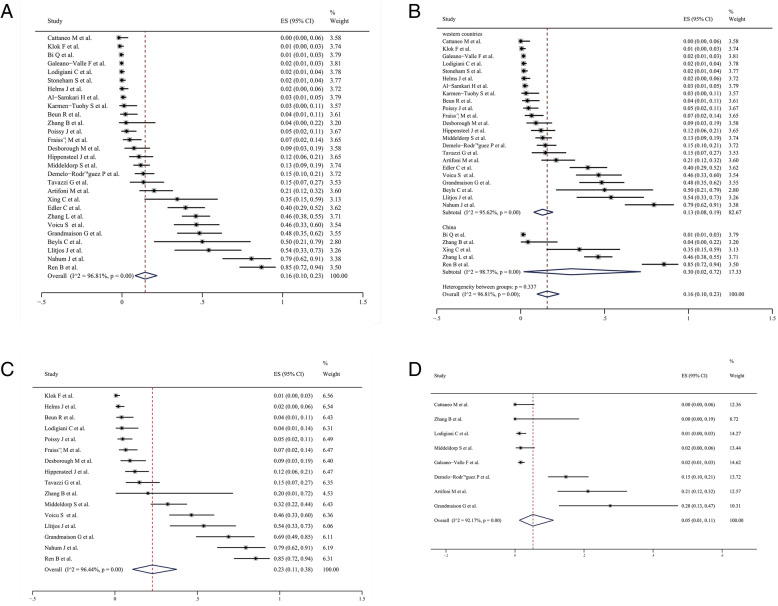
A total of 1202 records were initially identified by our searches. We finally included 28 articles in our meta-analysis. The basic characteristics of included studies are shown in Table 1. There were 397 DVT cases in a total of 4138 COVID-19 patients. The pooled estimate of the prevalence for DVT was 16% by using a random-effects model (95% CI 10–23%, P < 0.01, I2 = 96.81, Q = 846.41, P < 0.01) (Fig. 1a). According to patients’ geographic location, the much higher pooled prevalence of DVT was found in COVID-19 patients from China (30%, 95% CI 2–72%, P = 0.02, I2 = 98.73%, Q = 313.90, P < 0.01) compared with those from western countries (13%, 95% CI 8–19%, P < 0.01, I2 = 95.62%, Q = 502.07, P < 0.01) (Fig. 1b). Twenty articles clearly reported the prevalence of DVT in COVID-19 patients treated in ICU or non-ICU. The pooled prevalence of DVT in COVID-19 patients treated in ICU was 23% (95% CI 11–38%, P < 0.01, I2 = 96.44%, Q = 421.29, P < 0.01), which was significantly higher than in COVID-19 patients treated in non-ICU (5%, 95% CI 1–11%, P < 0.01, I2 = 92.17%, Q = 89.42, P < 0.01) (Fig. 1c, d). We found significant publication bias by Egger’s test (P < 0.001) and Begg’s test (P < 0.001). The subgroup analysis showed that none of these factors could explain the significant heterogeneity. However, the meta-regression analysis of multiple covariates indicated that the geographic location of patients could partially explain heterogeneity (P = 0.036).
Table 1.
Characteristics of the included studies
| Authors | Sample | Age | Male (%) | Location | Design of studies | Screening of DVT | ICU/non-ICU* | Prophylaxis (%) | DVT (%) |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al. (PMID: 32421381) | 143 | 63 (mean) | 74 (51.7) | China | Cross-sectional study | Ultrasound | N/R | 53 (37.1) | 66 (46.2) |
| Ren et al. (PMID: 32412320) | 48 | 70 (median) | 26 (54.2) | China | Cross-sectional study | Ultrasound | ICU | 47 (97.9) | 41 (85.4) |
| Demelo-Rodríguez et al. (PMID: 32405101) | 156 | 68.1 (mean) | 102 (65.4) | Spain | Prospective study | Ultrasound | Non-ICU | 153 (98.1) | 23 (14.7) |
| Middeldorp et al. (PMID: 32369666) | 198 | 61 (mean) | 130 (65.7) | Netherlands | Retrospective study | Ultrasound | ICU/non-ICU | 198 (100) | 26 (13.1) |
| Bi et al.† | 420 | 45 (mean) | 200 (47.6) | China | Prospective study | N/R | N/R | N/R | 6 (1.4) |
| Klok et al. (PMID: 32291094) | 184 | 64 (mean) | 139 (75.5) | Netherlands | Prospective study | Ultrasound | ICU | 184 (100) | 1 (0.5) |
| Karmen-Tuohy et al.‡ | 63 | 61 (mean) | 57 (90.5) | USA | Prospective study | N/R | N/R | N/R | 2 (3.2) |
| Llitjos et al. (PMID: 32320517) | 26 | 68 (median) | 20 (76.9) | France | Retrospective study | Ultrasound | ICU | 8 (30.8) | 14 (53.8) |
| Lodigiani et al. (PMID: 32353746) | 388 | 66 (median) | 264 (68.0) | Italy | Retrospective study | Ultrasound | ICU/non-ICU | 307 (79.1) | 6 (1.7)§ |
| Helms et al. (PMID: 32367170) | 150 | 63 (median) | 122 (81.3) | France | Prospective study | Imaging | ICU | 150 (100) | 3 (2.0) |
| Stoneham et al. (PMID: 32423903) | 274 | N/R | N/R | UK | Prospective study | Imaging | N/R | N/R | 5 (1.8) |
| Galeano-Valle et al. (PMID: 32425261) | 785 | N/R | N/R | Spain | Prospective study | Ultrasound | Non-ICU | 780 (99.4) | 13 (1.7) |
| Xing et al. (PMID: 32345353) | 20 | N/R | 12 (60.0) | China | Retrospective study | Ultrasound | N/R | N/R | 7 (35.0) |
| Beyls et al. (PMID: 32414510) | 12 | 62 (median) | 10 (83.3) | France | Retrospective study | Ultrasound | N/R | N/R | 6 (50.0) |
| Poissy et al. (PMID: 32330083) | 107 | N/R | N/R | France | Retrospective study | Ultrasound | ICU | 107 (100) | 5 (4.7) |
| Beun et al. (PMID: 32311843) | 75 | N/R | N/R | Netherlands | Retrospective study | N/R | ICU | N/R | 3 (4.0) |
| Cattaneo et al. (PMID: 32349132) | 64 | 70 (median) | 35 (54.7) | Italy | Retrospective study | Ultrasound | Non-ICU | 64 (100) | 0 (0.0) |
| Tavazzi et al. (PMID: 32322918) | 54 | N/R | N/R | Italy | Retrospective study | Ultrasound | ICU | 54 (100) | 8 (14.8) |
| Voicu et al. (PMID: 32479784) | 56 | N/R | 42 (75.0) | France | Prospective study | Ultrasound | ICU | 49 (87.5) | 26 (46.4) |
| Hippensteel et al. (PMID: 32484907) | 91 | 56.5 (mean) | 53 (58.2) | USA | Retrospective study | Ultrasound | ICU | N/R | 11 (12.1) |
| Fraissé et al. (PMID: 32487122) | 92 | 61 (median) | 73 (79.3) | France | Retrospective study | N/R | ICU | 92 (100) | 6 (6.5) |
| Desborough et al. (PMID: 32485437) | 66 | 59 (median) | 48 (72.7) | UK | Retrospective study | Imaging | ICU | 66 (100) | 6 (9.1) |
| Al-Samkari et al. (PMID: 32492712) | 400 | 61.8 (mean) | 228 (57.0) | USA | Retrospective study | Imaging | N/R | 400 (100) | 10 (2.5) |
| Edler et al. (PMID: 32500199) | 80 | 79.2 (mean) | 46 (57.5) | Germany | Prospective study | N/R | N/R | N/R | 32 (40.0) |
| Grandmaison et al. (PMID: 32529170) | 58 | N/R | N/R | Switzerland | Cross-sectional study | Ultrasound | ICU/non-ICU | N/R | 28 (48.3) |
| Artifoni et al. (PMID: 32451823) | 71 | 64 (median) | 43 (60.6) | France | Retrospective study | Ultrasound | Non-ICU | 70 (98.6) | 15 (21.1) |
| Nahum et al. (PMID: 32469410) | 34 | 62.2 (mean) | 25 (73.5) | France | Prospective study | Ultrasound | ICU | 34 (100) | 27 (79.4) |
| Zhang et al. (PMID: 32553905) | 23 | 44.7 (mean) | 15 (65.2) | China | Prospective study | N/R | ICU/non-ICU | N/R | 1 (4.3) |
DVT deep vein thrombosis, ICU intensive care unit, N/R not (clearly) reported
*Articles clearly reported the prevalence of DVT in COVID-19 patients treated in ICU or non-ICU
†doi: 10.1101/2020.04.22.20076190
‡doi: 10.1101/2020.05.07.20094797
§Data missing for patients
Fig. 1.
Forest plots of pooled prevalence and its 95% confidence interval (CI) for deep vein thrombosis (DVT) in confirmed coronavirus disease 2019 (COVID-19) patients (a) and subgroup analysis by patients’ geographic location (b) and the severity of disease (c, d)
In conclusion, more attention should be paid to the prevention and clinical management of DVT, especially for COVID-19 patients in ICU, and timely assessment of DVT is essential. However, there was considerable heterogeneity in our meta-analysis. In addition, there was significant publication bias in our meta-analysis, although we searched four databases as many and as carefully as possible. Finally, we included non-survival patients who were seriously ill and may exaggerate the prevalence of DVT in COVID-19 patients.
Acknowledgements
Not applicable.
Authors’ contributions
Ying Wang, Li Shi, and Yadong Wang designed the study, performed the analyses, and wrote the manuscript; Ying Wang, Li Shi, Haiyan Yang, and Guangcai Duan performed the statistics; and all authors critically reviewed and approved the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (no. 81973105). The funder has no role in the preparation of manuscript and decision to submission.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ying Wang and Li Shi contributed equally to this work.
Contributor Information
Haiyan Yang, Email: yhy@zzu.edu.cn.
Yadong Wang, Email: wangyd76@163.com.
References
- 1.Ren B, Yan F, Deng Z, Zhang S, Xiao L, Wu M, Cai L. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan. Circulation. 2020. 10.1161/circulationaha.120.047407. [DOI] [PubMed]
- 2.Zhang L, Feng X, Zhang D, Jiang C, Mei H, Wang J, Zhang C, Li H, Xia X, Kong S, et al. Deep vein thrombosis in hospitalized patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: prevalence, risk factors, and outcome. Circulation. 2020. 10.1161/circulationaha.120.046702. [DOI] [PubMed]
- 3.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020. 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed]
- 4.Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller MCA, Bouman CCS, Beenen LFM, Kootte RS, Heijmans J, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thrombosis Haemostasis. 2020. 10.1111/jth.14888. [DOI] [PMC free article] [PubMed]
- 5.Hargreaves S, Rustage K, Nellums LB, McAlpine A, Pocock N, Devakumar D, Aldridge RW, Abubakar I, Kristensen KL, Himmels JW, et al. Occupational health outcomes among international migrant workers: a systematic review and meta-analysis. Lancet Glob Health. 2019;7:e872–e882. doi: 10.1016/S2214-109X(19)30204-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–872. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article.