Abstract
Remote consultations likely will grow in importance if the COVID-19 pandemic continues. This review analyzes which methods of teledermatology patients prefer by categorizing how recent studies have defined satisfaction, conducted surveys and concluded patients respond to the different modalities of teledermatology. Using PubMed and Cochrane databases, we reviewed studies from April 5th, 2010 to April 5th, 2020 that included the search terms patient satisfaction and teledermatology. All studies that included patient satisfaction as an outcome were included, but studies not published in English were excluded. We examined domains of satisfaction, survey method, study characteristics (including patient population, country, age, study design and evidence score), findings and statistical comparisons. We thoroughly reviewed 23 studies. Definitions of satisfaction varied, but all concluded patients were satisfied with the live-interactive and store-and-forward modalities. The studies reveal that store-and-forward is appropriate for clinicians with established patients who require regular follow-up. Verified areas of care include treatment of chronic conditions, topical skin cancer therapy, wound monitoring, and post-procedural follow-up. Only four studies conducted statistical analyses. One of those studies compared patient preference for each modality of teledermatology with face-to-face dermatology. While this study reported high satisfaction with each mode of teledermatology, patients still preferred face-to-face. Favorable responses to remote diagnostic capabilities suggest that these offerings improve preference for teledermatology. With only one study evaluating preference between each modality and face-to-face dermatology, more studies should address the discrepancy. Surveys that cover all domains of satisfaction may improve assessments and identify where gaps in preference exist.
Keywords: Teledermatology, Patient satisfaction, Survey methods, Store and forward, Live interactive
Introduction
Medical practices have transformed in the wake of the COVID-19 pandemic. Telemedicine has emerged as a critical tool for practitioners to provide care without increasing transmission risks among patients and clinicians. Many dermatology offices have transitioned to remote care to maintain operations amid physical distancing requirements [1].
Teledermatology is the form of telemedicine directed to dermatology [2–5]. Teledermatology developed in two primary formats: a real-time, live-interactive technology and a store-and-forward technology. In live-interactive teledermatology, a dermatologist speaks with patients over a live video conference in a manner similar to an in-person consultation [6]. In store-and-forward teledermatology, a nurse, medical assistant or general practitioner acquires clinical and dermascopic images at an office or hospital and sends the images to a remote dermatologist for evaluation [6]. Technologies such as high-resolution cameras capable of acquiring high-quality dermascopic images have allowed practitioners to preserve evidence of suspicious lesions until a dermatologist has time to review and make recommendations to the primary care provider or patient [7].
The increased need for remote access to medical care has prompted practitioners to ask how their patient populations will respond to these prevailing forms of telemedicine, especially when selecting methods suitable to their practice. In this review, we evaluate recent studies that have analyzed patient satisfaction with teledermatology. We explore in depth how these studies have defined and measured patient satisfaction, where conclusions have been made, and how satisfaction differs between live-interactive, store-and-forward, and face-to-face dermatology.
Methods
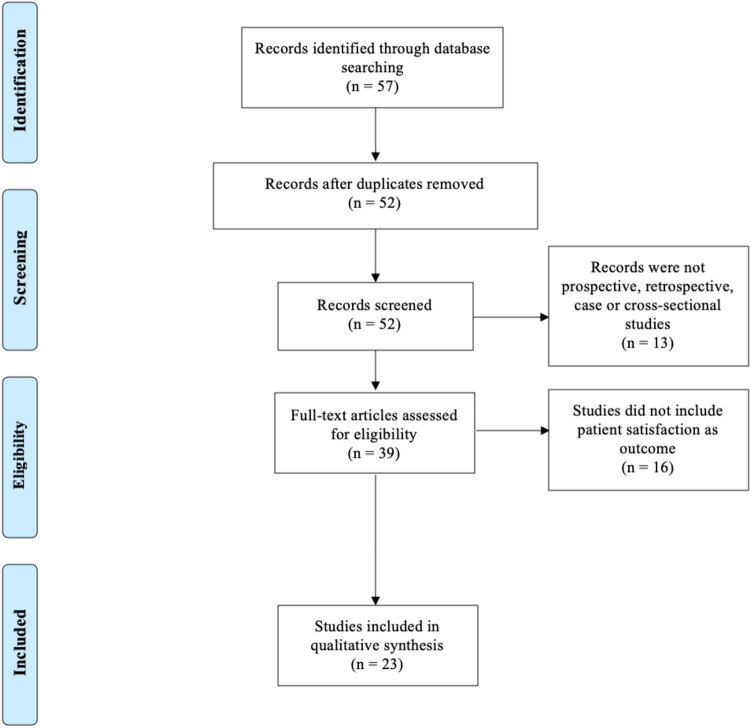
This systematic review was conducted according to the PRISMA guidelines [8]. We ran search strings on PubMed and Cochrane Library databases designed to identify articles that discussed patient satisfaction in teledermatology. Our search was broad, keying all fields for combinations of the term teledermatology with iterations of the term patient satisfaction. The search spanned articles published during the 10 years beginning April 5th, 2010 and ending April 5th, 2020.
The initial search identified a total of 57 articles. Five duplicate studies were excluded. Non-English studies were also excluded. Acceptable studies included cross-sectional, case–control, prospective, retrospective studies and clinical trials that focused on patient satisfaction as a primary or secondary outcome. If a study did not explore patient satisfaction as an outcome, it was excluded. Twenty-three studies met these criteria for thorough review. The search logic is summarized in Fig. 1.
Fig. 1.
Literature review
We reviewed how each study defined patient satisfaction and the characteristics of each survey method. We noted the characteristics of every study population. We summarized detailed findings across studies. The quality of evidence in each study was scored using the Oxford Center for Evidence-Based Medicine algorithm [9].
Literature review
Operational defintion for patient satisfaction
Definitions of patient satisfaction were not consistent across surveys [10–32]. To create a framework to organize studies, we selected a review by Kraai et al. [33], which presents one of the broadest definitions of patient satisfaction. Kraai et al. applies a theoretical definition of patient satisfaction presented by Ware et al. for use in a general telemedicine population [34]. This resulted in a definition covering eight domains: interpersonal manner, technical quality, accessibility, financial burden, efficacy, continuity, physical environment, and availability [34].
Each study defined patient satisfaction, but inconsistently [10–32]. For example, three studies in our analysis used surveys that had been previously developed. One such study [28] used a survey provided by Locatis et al. [35] that prompted patients to rate their response to 12 statements using a five-point Likert scale. Statements included, ‘I felt at ease talking with the medical professional … at ease talking with the interpreter … that the medical professional heard and understood me … I understood what the medical professional was telling me … my privacy was respected … the interpreter noticed when I had problems understanding … I had opportunities to ask questions … the medical professional understands my problem … I feel overall that the meeting today was satisfactory’ [35]. The other two, by Frühauf et al. [13, 32], were adapted from Eminovic et al. [36] to ask 15 questions, each soliciting a five-point response scale ranging from (1) (very negative) to (5) (very positive). Frühauf et al. addressed areas such as the patient’s perception of teledermatology, the patient’s confidence in the dermatologist’s responses, and whether the patient needed to be seen again in person [36]. Based on our framework, those two studies covered the most domains of patient satisfaction [13, 32].
Overall, accessibility, efficacy, technical quality, and physical environment were the most studied domains of patient satisfaction in the studies we reviewed. Interpersonal manner and finances were addressed less frequently. Availability and continuity were covered the least. A summary of the total domains addressed by each study is set out in Table 1.
Table 1.
Teledermatology satisfaction studies and domains of satisfaction
| Study | Accessibility | Efficacy | Technical quality | Physical Environment | Interpersonal manner | Finances | Availability | Continuity | Total domains in study |
|---|---|---|---|---|---|---|---|---|---|
| Frühauf et al. (2015) [32] | + | + | + | − | + | + | + | + | 7 |
| Frühauf et al. (2012) [13] | + | + | + | − | + | + | + | + | 7 |
| Nicholson et al. (2020) [10] | + | + | + | + | + | − | + | − | 6 |
| Wang et al. (2018) [22] | + | + | + | − | + | + | + | − | 6 |
| Rajda et al. (2018) [27] | + | + | + | + | − | − | − | − | 4 |
| Bianciardi et al. (2016) [20] | + | + | + | − | − | + | − | − | 4 |
| Azfar et al. (2011) [15] | + | + | + | + | − | − | − | − | 4 |
| Baranowski et al. (2019) [18] | + | + | − | − | + | − | − | − | 3 |
| Marchell et al. (2017) [28] | − | − | + | + | + | − | − | − | 3 |
| Quran et al. (2015) [17] | + | − | − | − | − | + | + | − | 3 |
| Hsueh et al. (2012) [12] | + | + | − | − | − | − | − | + | 3 |
| Bosanac et al. (2018) [26] | − | + | + | − | − | − | − | − | 2 |
| Lim et al. (2018) [16] | + | − | − | − | − | + | − | − | 2 |
| Fiks et al. (2018) [19] | + | − | − | + | − | − | − | − | 2 |
| Pathipati et al. (2016) [24] | − | − | − | + | − | + | − | − | 2 |
| Livingstone et al. (2015) [30] | − | − | − | + | + | − | − | − | 2 |
| Ford et al. (2015) [31] | − | + | − | + | − | − | − | − | 2 |
| Kaliyadan et al. (2013) [23] | − | + | − | + | − | − | − | − | 2 |
| Chee et al. (2016) [29] | − | − | + | + | − | − | − | − | 1 |
| Thind et al. (2011) [21] | + | − | − | − | − | − | − | − | 1 |
| Mehrtens et al. (2019) [11] | − | − | − | − | − | − | − | − | 0 |
| Lester et al. (2014) [25] | − | − | − | − | − | − | − | − | 0 |
| Koller et al. (2011) [14] | − | − | − | − | − | − | − | − | 0 |
| Total studies per domain | 13 | 12 | 10 | 10 | 7 | 7 | 5 | 3 |
Study survey method
Many studies assessed satisfaction using self-developed questionnaires; however, one study conducted in-person interviews of patients [24], and another reviewed satisfaction anecdotally [25]. Thirteen studies employed a Likert five-point scale [10–14, 22, 26–32], ranging from strongly disagree (1) to strongly agree (5). For those 13 studies, scores of agree (4) and strongly agree (5) generally were deemed satisfactory [10–14, 22, 26–32]. Three studies scored statements of satisfaction on an agree/disagree basis [18–20]. The survey characteristics (whether a five-point grading scale was used, the method of administration, and acceptable scores) are set out in Table 2.
Table 2.
Characteristics of survey method
| Study | Employed five-point response scale | Interview, questionnaire or other | Acceptable score |
|---|---|---|---|
| Nicholson et al. (2020) [10] | + | Questionnaire | 4/5 + |
| Mehrtens et al. (2019) [11] | + | Questionnaire | 4/5 + |
| Wang et al. (2018) [22] | + | Questionnaire | 4/5 + |
| Bosanac et al. (2018) [26] | + | Questionnaire | 4/5 + |
| Rajda et al. (2018) [27] | + | Questionnaire | 4/5 + |
| Marchell et al. (2017) [28] | + | Questionnaire | 4/5 + |
| Chee et al. (2016) [29] | + | Questionnaire | 4/5 + |
| Livingstone et al. (2015) [30] | + | Questionnaire | 4/5 + |
| Ford et al. (2015) [31] | + | Questionnaire | 4/5 + |
| Frühauf et al. (2015) [13] | + | Questionnaire | 4/5 + |
| Hsueh et al. (2012) [12] | + | Questionnaire | 4/5 + |
| Frühauf et al. (2012) [13] | + | Questionnaire | 4/5 + |
| Koller et al. (2011) [14] | + | Questionnaire | 4/5 + |
| Azfar et al. (2011) [15] | − | Questionnaire | Variable |
| Lim et al. (2018) [16] | − | Questionnaire | Preferred/did not prefer fewer visits |
| Quran et al. (2015) [17] | − | Questionnaire | More/Same/ Less |
| Baranowski et al. (2019) [18] | − | Questionnaire | Agree/disagree |
| Fiks et al. (2018) [19] | − | Questionnaire | Agree/Disagree |
| Bianciardi et al. (2016) [20] | − | Questionnaire | Agree/Disagree |
| Thind et al. (2011) [21] | − | Questionnaire | 5/6 + |
| Kaliyadan et al. (2013) [23] | − | Questionnaire | 3/4 + |
| Pathipati et al. (2016) [24] | − | Interview | N/A |
| Lester et al. (2014) [25] | − | Anecdotally assessed | N/A |
Characteristics of studies and findings
The 23 articles directed towards patient satisfaction and teledermatology described a total of 1,996 patient responses. Twenty-one studies focused specifically on the store-and-forward model [10–16, 18–27, 29–32], one focused on live-interactive [17], and one was a quasi-randomized control trial that compared store-and-forward, live-interactive, and face-to-face dermatology [28].
The studies covered a variety of patient conditions. One study followed patients who received topical therapy for actinic keratosis [26]. A second study followed patients with early stage melanoma [16]. Two additional studies followed patients requiring follow-up on cosmetic procedures [22, 29]. Two more studies followed pediatric patients [19, 20]. One study focused on wound care [20]. A further two studies focused primarily on patients with acne [24, 32]. Two studies followed patients with psoriasis [13, 14]. The last study followed patients with cutaneous complications resulting from HIV [15]. Notably, three general dermatology consult practices included patients from the Veterans Affairs [12, 18, 25].
The studies focused on patient populations in different nations. Five studies were conducted in the United Kingdom [10, 11, 30], one in Taiwan [22], three in Austria [13, 14, 32], two in Australia [16, 29], seven in the United States [12, 18, 19, 24–28], one in Italy [20], one in Jordan [17], one in Saudi Arabia [23], and one in Botswana [15].
Which teledermatology models were evaluated, the study location, the patient population, the number of participants, the average age of participants, the study design, the evidence score, and the outcome of each survey are summarized in Table 3. An in-depth summary of the results of each study, including statistical comparisons where performed, is shown in Table 4.
Table 3.
Study characteristics
| Author (year) | Country | Model | Patient population | N = | Average age (years) | Study design and evidence score | Outcomes |
|---|---|---|---|---|---|---|---|
| Nicholson et al. (2020) [10] | United Kingdom | Store-and-forward | Teleconsultative service for general dermatology | 60 | 78% ≤ | Cross-sectional survey, 4 | Primary: patient satisfaction |
| 51% Female | 55 | ||||||
| 65% White | |||||||
| Mehrtens et al. (2019) [11] | United Kingdom | Store-and-forward | Teleconsultative service for general dermatology | 37 | − | Retrospective observational study, 3 | Primary: Number of consultations, number of face-to-face appointments avoided |
| Secondary: Patient satisfaction | |||||||
| Baranowski et al. (2019) [18] | United States | Store-and-forward in comparison to teleconsultative method | Teleconsultative service for Department of Veterans Affairs | 100 | 60.9 | Cross-sectional survey, 4 | Primary: patient satisfaction |
| 60% White | |||||||
| 36% Black or African American | |||||||
| Wang et al. (2018) [22] | Taiwan | Store-and-forward | Follow-up care for cosmetic dermatology patients | 28 | − | Cross-sectional survey, 4 | Primary: patient satisfaction |
| Bosanac et al. (2018) [26] | United States | Store-and-forward | Follow-up care for actinic keratoses patients receiving topical therapy | 13 | 67 | Randomized controlled trial, 1 | Primary: number of treatment doses, times contacted clinic, patient satisfaction |
| 96% Male | |||||||
| Lim et al. (2018) [16] | Australia | Store-and-forward | Patients treated for early stage melanoma who required follow-up via teledermatology | 262 | 64.3 | Retrospective observational study, 3 | Primary: determine proportion of adults who preferred standard scheduled visits or fewer follow-up visits using teledermatology |
| 36% Female | |||||||
| Rajda et al. (2018) [27] | United States | Store-and-forward | General dermatology consultation service | 152 | 37.8 | Case–control study, 2 | Primary: access, satisfaction, utilization, costs |
| Fiks et al. (2018) [19] | United States | Store-and-forward | Pediatric dermatology patients | 197 | 7.3 | Prospective comparative study, 2 | Primary: feasibility study for store-and-forward application; general satisfaction |
| 67% White | |||||||
| Marchell et al. (2017) [28] | United States | Controlled study comparing in-person exam to store-and-forward to live-interactive | Patients cycled through all 3 modalities | 191 | − | Quasi-randomized control trial, 2 | Primary: Patient and provider satisfaction with teledermatology; Absolute preference of in-person, store-and-forward, or live-interactive teledermatology |
| Pathipati et al. (2016) [24] | United States | Store-and-forward | General dermatology service | 38 | 39.3 | Case series study, 4 | Primary: Provider confidence in diagnosis; time to consult |
| 84% Female | |||||||
| Secondary: Patient satisfaction | |||||||
| Chee et al. (2016) [29] | Australia | Store-and-forward | Cosmetic laser resurfacing follow-up | 24 | − | Retrospective observational study, 3 | Primary: Patient satisfaction |
| Bianciardi et al. (2016) [20] | Italy | Store-and-forward | Pediatric dermatology wound care follow-up | 19 | − | Case series study, 4 | Primary: Patient satisfaction |
| Livingstone et al. (2015) [30] | United Kingdom | Store-and-forward | General adult dermatology | 129 | − | Retrospective observational study, 3 | Primary: Cost-effectiveness and patient satisfaction |
| Ford et al. (2015) [31] | United Kingdom | Store-and-forward | 5 general teledermatology practices | 28 | − | Prospective comparative study, 2 | Primary: Reduction of secondary care referrals |
| Secondary: patient satisfaction | |||||||
| Quran et al. (2015) [17] | Jordan | Live-interactive | Teleconsultation services provided to 2 rural hospitals | 88 | − | Cross-sectional survey, 4 | Primary: patient satisfaction |
| Frühauf et al. (2015) [32] | Austria | Store-and-forward | Acne patients followed for isotretinoin therapy | 69 | 18 | Randomized control trial, 1 | Primary: therapeutic outcomes and adverse reactions |
| 25 Females | |||||||
| 44 Males | Secondary: patient satisfaction | ||||||
| Lester et al. (2014) [25] | United States | Store-and-forward | PCP teletriage for dermatologic cases; | 63 | − | Case series study, 4 | Primary: number of secondary referrals |
| Department of Veterans Affairs | |||||||
| Secondary: patient satisfaction | |||||||
| Kaliyadan et al. (2013) [23] | Saudi Arabia | Store-and-forward | General dermatology | 161 | − | Cross-sectional survey, 4 | Primary: diagnostic concordance; patient satisfaction |
| Hsueh et al. (2012) [12] | United States | Store-and-forward | General dermatology, consult service; Department of Veterans Affairs | 196 | 71 | Case–control study, 4 | Primary: patient satisfaction |
| 97% Male | |||||||
| Frühauf et al. (2012) [13] | Austria | Store-and-forward | Patients were followed for response to psoriasis therapy | 10 | 40 | Cross-sectional survey, 4 | Primary: patient satisfaction |
| 60% Male | |||||||
| Koller et al. (2011) [14] | Austria | Store-and-forward | Patients were followed for response to biologic psoriasis therapy | 19 | 46.2 | Case–control study, 4 | Primary: symptom management, safety and adverse events |
| 12 Males | |||||||
| 7 Females | Secondary: patient satisfaction | ||||||
| Azfar et al. (2011) [15] | Botswana | Store-and-forward | Patients with HIV and mucocutaneous complaints | 89 | 71% were 31–50 | Cross-sectional survey, 4 | Primary: patient satisfaction |
| 34 (44%) Males | |||||||
| 44% Unemployed | |||||||
| Thind et al. (2011) [21] | United Kingdom | Store-and-forward | General teledermatology consultation | 23 | 54 | Case–control study, 3 | Primary: patient satisfaction, diagnostic concordance, secondary referrals |
Table 4.
Study findings
| Author (year) | Patient satisfaction results | Determined overall satisfaction | Statistical analysis performed |
|---|---|---|---|
| Nicholson et al. (2020) [10] |
72% felt comfortable having photographs taken 53% agreed TD service saved time 42% patients would rather see dermatologist face-to-face 17% felt something was missing from not having face-to-face consultation 80% would recommend to family and friends |
+ | − |
| Mehrtens et al. (2019) [11] | 82% felt service was very good (47%) or good (36%) | + | − |
| Baranowski et al. (2019) [18] | Teleconsultative model vs telemedicine; no statistical significance between 2 models across 6 areas of satisfaction | + | + |
| Wang et al. (2018) [22] | Total composite satisfaction 4.3/5 | + | − |
| Bosanac et al. (2018) [26] |
70% would use system again (week 4), 92% (week 8) 80% very satisfied or satisfied (week 4), 100% (week 8) 40% would prefer in-person follow-up (week 4), 23% (week 8) |
+ | − |
| Lim et al. (2018) [16] |
Proportion who preferred fewer visits: 30% (CI 25–36%) Fewer patients with stage 0/I (33/127; 26%) than stage II (48/103; 47%) preferred fewer scheduled visits Preferred fewer visits with teledermatology service: Seeing a specialist for another chronic health problem (P = 0.03) Did not have private insurance (P = 0.006) Lived with others (P = 0.001) Had their first primary melanoma on a limb (P = 0.01) No independently significant associations, including participant level of fear of recurrent or new primary melanoma (Fear of cancer recurrence inventory, P = 0.23) |
+ | + |
| Rajda et al. (2018) [27] | Composite satisfaction = 4.38/5 | + | − |
| Fiks et al. (2018) [19] |
97% felt it was time manageable 87% satisfied 93% would use again |
+ | − |
| Marchell et al. (2017) [28] |
Satisfaction for compressed video, uncompressed video, store-and-forward, and in-person was 4.66/5, 4.68/5, 4.74/5, 4.75/5, respectively Preference (out of 3) for in-person, video, and store-and-forward teledermatology was 1.12, 2.41, and 2.40, respectively. Video and store-and-forward (p < 0.001) were significantly lower in preference compared to in-person |
+ | + |
| Pathipati et al. (2016) [24] | Patients reported high satisfaction in one-on-one discussion session post-study | + | − |
| Chee et al. (2016) [29] |
100% felt the service was a positive initiative 95% felt comfortable with image acquisition and transmission 25% concerned about privacy issue 50% had concerns about over accuracy |
+ | − |
| Bianciardi et al. (2016) [20] | Satisfaction 57% (3 months), 71% (6 months), and 84% (12 months) | + | − |
| Livingstone et al. (2015) [30] |
93% found procedure very comfortable/comfortable 100% would recommend to other patients |
+ | − |
| Ford et al. (2015) [31] | 82% very satisfied with service | + | − |
| Quran et al. (2015) [17] |
Satisfaction 90.5 (Scale: 0–100; SD 8.5) Perceived less travel time (96%), reduced waiting time (73%), and lower cost (84%) |
+ | − |
| Frühauf et al. (2015) [32] |
Week 12 composite satisfaction score 77.8 (Scale: 0–100; SD 19.8) Week 24 composite satisfaction score: 74.0 (Scale: 0–100; SD 21.0) |
+ | − |
| Lester et al. (2014) [25] | High satisfaction reported anecdotally | + | − |
| Kaliyadan et al. (2013) [23] |
Comfort with photographed lesion: 89% Satisfied with medical care: 76% 23 patients refused photography of skin lesion (21 females, 2 males) |
+ | − |
| Hsueh et al. (2012) [12] |
78% highly satisfied with face-to-face; 77% highly satisfied with teledermatology Mean patient satisfaction score for teledermatology equivalent to face-to-face: 4.1/5 and 4.3/5, respectively (p = 0.4) |
+ | + |
| Frühauf et al. (2012) [13] |
80% considered service an alternative to in-person 90% felt they were in good hands |
+ | − |
| Koller et al. (2011) [14] |
100% thought teledermatology service was a very good or good idea 94.1% would recommend again |
+ | − |
| Azfar et al. (2011) [15] |
99% comfortable with mobile consultation 8% concerned with not having face-to-face appointment 91% believed service provided same treatment and quality as face-to-face |
+ | − |
| Thind et al. (2011) [21] | 90% completely, or very satisfied | + | − |
All studies, either through surveys or anecdotal evidence, declared overall patient satisfaction with both teledermatology modalities [10–32]. However, only four studies provided statistical analyses [12, 16, 18, 28]. One of those studies further evaluated preference between the different forms of teledermatology and face-to-face dermatology [28], and demonstrated preference for face-to-face dermatology over both teledermatology modalities [28].
Discussion
All studies found patients were satisfied with store-and-forward and live-interactive teledermatology, but variations in how patient satisfaction was defined and evaluated shed light on when patients will prefer certain modalities over others. Such nuances also inform areas in which future research could better capture patient preferences.
Only one study in the last 10 years exclusively addressed patient satisfaction with live-interactive teledermatology [17]. This study showed high levels of satisfaction as patients described increased satisfaction with decreased travel times, waiting times, and cost. However, the study employed a nontraditional response scale and accessibility, finances, and availability were the only domains of satisfaction evaluated in their questionnaire [17].
Instead, most studies conducted in the past ten years have exclusively evaluated the store-and-forward modality. This may be due to the fact that more practices have explored the use of store-and-forward teledermatology, in part due to its cost friendliness, flexibility, and ability to leverage technological advantages in the secure transmission of high-quality images [37].
Store-and-forward teledermatology is well received by patients who require numerous appointments. Patients who require follow-up appointments, such as those receiving cosmetic procedures [22, 29], or topical therapies for actinic keratoses [26], and patients requiring management of chronic skin conditions such as psoriasis [13, 14], were very satisfied with the store-and-forward model. A study by Lim et al. also demonstrated that, in patients with early stage melanoma, those who required follow-up with multiple specialists, did not have private insurance, lived with others at home, or had their first primary melanoma were interested in a patient-directed store-and-forward model of teledermatology that allowed for fewer follow-up visits [16].
Recent research also reveals store-and-forward teledermatology shortcomings. A study by Nicholson et al. reported that 10% of patients felt embarrassed to have photos taken [10]. Similarly, Kaliyaden et al. disclosed in his study that 23% of his patients refused photography of skin lesions (21 females, 2 males) citing social or religious issues [23]. A study by Chee et al. noted that a quarter of patients in their study population had concerns over privacy issues regarding images [29]. So, while store-and-forward teledermatology can provide exceptional satisfaction in terms of decreased wait times and increased access to specialist providers, some patients still do not feel comfortable with the photographing of their skin.
Further research directed at why patients prefer one method to the other could reveal other valuable avenues for the development of teledermatology. Many patients in Nicholson et al. agreed the store-and-forward service saved time and provided flexibility for their lifestyle, but 42% of patients still stated they would rather see a dermatologist face-to-face [10]. An additional 17% felt something was missing from their appointment because they did not have a face-to-face consultation [10].
The 2017 study by Marchell et al. corroborates these results. Marchell et al. performed a unique study where patients had to decide a preference between face-to-face dermatology, live-interactive, and store-and-forward teledermatology [28]. Although patients were satisfied with store-and-forward and live-interactive teledermatology, an overwhelming majority still selected in-person as their main preference [28]. However, this study provided a limited assessment of satisfaction, as only technical quality, physical environment, and interpersonal manner were assessed.
Accuracy of results is an unlikely cause for this discrepancy. Recent reviews have shown exceptional diagnostic concordance with store-and-forward teledermatology [38, 39]. A review published in 2019 by Andrees et al. showed that live-interactive teledermatology was similarly time effective and accurate [40].
Instead, preference for face-to-face dermatology may be due to the immediacy of diagnostic procedures that teledermatological methods lack. Common to both workflows of store-and-forward and live-interactive teledermatology is the need to refer patients to follow up face-to-face appointments for the performance of necessary diagnostic procedures for suspicious lesions [6]. Equalizing preference of teledermatology to face-to-face dermatology may lie in finding new and optimal ways to improve diagnostic measures available to teledermatology, especially when high-risk lesions are evaluated.
Optical coherence tomography or confocal microscopy may allow for immediate diagnosis. Optical coherence tomography (OCT) is a noninvasive diagnostic method that offers view into the superficial layers of the skin in vivo real-time [41]. Similarly, confocal microscopy is a means of providing noninvasive histomorphological analysis of skin lesions [42]. In a recent case in Los Angeles, reflectance confocal microscopy was used during a live-interactive teledermatology session to diagnose a nodular basal cell carcinoma [43]. The diagnosis took around 15 min, and the patient was pleased to understand their condition and discuss options for treatment immediately [43].
With regard to dermatologic surgery, studies have evaluated teledermatology with respect to preoperative consultation, intraoperative consultation via telepathology, and post-procedural monitoring [44]. Still, to our knowledge, no studies have yet explored ways to integrate surgical methods such as laser therapy into teledermatology. Identifying ways to integrate further technologies into teledermatology workflows may improve the diagnostic and procedural measures available to dermatologists that treat patients off site and, in turn, may elevate patients’ preference for teledermatology over face-to-face dermatology.
Conclusion
Although recent studies of teledermatology have reported general patient satisfaction with each modality of teledermatology, each reveals areas in which the practice can improve.
Our understanding of the effect of live-interactive treatment on patient satisfaction is limited. Few studies have addressed patient satisfaction for this modality and those that have covered few domains of satisfaction. More nuanced inquiries could help practitioners better understand which aspects of live-interactive teledermatology are most important to their patients and to plan accordingly.
Store-and-forward teledermatology is a well-received and an appropriate option for clinicians with established patients who have chronic conditions, require topical therapies for skin cancers, wound monitoring, and post-procedural follow-up checks.
However, when faced with the choice between teledermatology modalities and face-to-face dermatology, many prefer face-to-face dermatology. More studies with surveys covering more domains of satisfaction are needed to evaluate this discrepancy. For example, patients have indicated a preference for reduced visits, but continuity is a rarely studied domain. Advanced remote technologies like OCT and reflectance confocal microscopy also provide promising avenues to closing gaps in preference.
Because face-to-face appointments are likely to remain limited, more granular research of patient satisfaction with teledermatology could provide valuable insight to those with reduced access to patients. A single validated survey that encompasses all domains of satisfaction would improve assessments between live-interactive and store-and-forward teledermatology, and better identify where gaps in preference exist.
Acknowledgements
This paper has not been previously published or posted and is not under consideration elsewhere.
Funding
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.COVID-19 and Teledermatology: The Past, Present, and Future|The Dermatologist. [Online]. Available: https://www.the-dermatologist.com/article/covid-19-and-teledermatology-past-present-and-future. Accessed 14-Jun-2020
- 2.Bystryn JC, Feldman SR, Fleischer AB. Dermatology manpower needs. Dermatol Clin. 2000;18(2):303–311. doi: 10.1016/s0733-8635(05)70176-5. [DOI] [PubMed] [Google Scholar]
- 3.Resneck J, Kimball AB. The dermatology workforce shortage. J Am Acad Dermatol. 2004;50(1):50–54. doi: 10.1016/j.jaad.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Suneja T, Smith ED, Chen GJ, Zipperstein KJ, Fleischer AB, Feldman SR. Waiting times to see a dermatologist are perceived as too long by dermatologists: implications for the dermatology workforce. Arch Dermatol. 2001;137(10):1303–1307. doi: 10.1001/archderm.137.10.1303. [DOI] [PubMed] [Google Scholar]
- 5.Tsang MW, Resneck JS. Even patients with changing moles face long dermatology appointment wait-times: a study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55(1):54–58. doi: 10.1016/j.jaad.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Pasquali P, et al. Teledermatology and its current perspective. Indian Dermatol Online J. 2020;11(1):12–20. doi: 10.4103/idoj.IDOJ_241_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bleicher B, Levine A, Markowitz O. Going digital with dermoscopy. Cutis. 2018;102(2):102–105. [PubMed] [Google Scholar]
- 8.Moher D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.“Oxford Centre for Evidence-based Medicine - Levels of Evidence (March 2009) - CEBM.” [Online]. Available: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/. Accessed 13-Apr-2020
- 10.Nicholson P, Macedo C, Fuller C, Thomas L. Patient satisfaction with a new skin cancer teledermatology service. Clin Exp Dermatol. 2020 doi: 10.1111/ced.14191. [DOI] [PubMed] [Google Scholar]
- 11.Mehrtens SH, Shall L, Halpern SM. A 14-year review of a UK teledermatology service: experience of over 40 000 teleconsultations. Clin Exp Dermatol. 2019;44(8):874–881. doi: 10.1111/ced.13928. [DOI] [PubMed] [Google Scholar]
- 12.Hsueh MT, Eastman K, McFarland LV, Raugi GJ, Reiber GE. Teledermatology patient satisfaction in the Pacific Northwest. Telemed e-Health. 2012;18(5):377–381. doi: 10.1089/tmj.2011.0181. [DOI] [PubMed] [Google Scholar]
- 13.Frühauf J, et al. Pilot study on the acceptance of mobile teledermatology for the home monitoring of high-need patients with psoriasis. Australas J Dermatol. 2012;53(1):41–46. doi: 10.1111/j.1440-0960.2011.00852.x. [DOI] [PubMed] [Google Scholar]
- 14.Koller S, et al. Teledermatological monitoring of psoriasis patients on biologic therapy. Acta Derm Venereol. 2011;91(6):680–685. doi: 10.2340/00015555-1148. [DOI] [PubMed] [Google Scholar]
- 15.Azfar RS, et al. HIV-positive patients in Botswana state that mobile teledermatology is an. J Telemed Telecare. 2011;17(6):338–340. doi: 10.1258/jtt.2011.110115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lim W-Y, et al. Patient preferences for follow-up after recent excision of a localized melanoma. JAMA Dermatol. 2018;154(4):420–427. doi: 10.1001/jamadermatol.2018.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al Quran HA, Khader YS, Ellauzi ZM, Shdaifat A. Effect of real-time teledermatology on diagnosis, treatment and clinical improvement. J Telemed Telecare. 2015;21:93–99. doi: 10.1177/1357633X14566572. [DOI] [PubMed] [Google Scholar]
- 18.Baranowski MLH, Balakrishnan V, Chen SC. Patient satisfaction with the veteran’s administration teledermatology service. J Am Acad Dermatol. 2019 doi: 10.1016/j.jaad.2019.01.036. [DOI] [PubMed] [Google Scholar]
- 19.Fiks AG, et al. Usability, acceptability, and impact of a pediatric teledermatology mobile health application. Telemed e-Health. 2018;24(3):236–245. doi: 10.1089/tmj.2017.0075. [DOI] [PubMed] [Google Scholar]
- 20.Bianciardi Valassina MF, Bella S, Murgia F, Carestia A, Prosseda E. Telemedicine in pediatric wound care. Clin Ter. 2016;167(1):e21–e23. doi: 10.7417/T.2016.1915. [DOI] [PubMed] [Google Scholar]
- 21.Thind CK, Brooker I, Ormerod AD. Teledermatology: a tool for remote supervision of a general practitioner with special interest in dermatology. Clin Exp Dermatol. 2011;36(5):489–494. doi: 10.1111/j.1365-2230.2011.04073.x. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y-C, et al. Patient satisfaction with dermatology teleconsultation by using MedX. Comput Methods Programs Biomed. 2018;167:37–42. doi: 10.1016/j.cmpb.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 23.Kaliyadan F, Amin TT, Kuruvilla J, Ali WHAB. Mobile teledermatology - patient satisfaction, diagnostic and management concordance, and factors affecting patient refusal to participate in Saudi Arabia. J Telemed Telecare. 2013;19(6):315–319. doi: 10.1177/1357633X13501778. [DOI] [PubMed] [Google Scholar]
- 24.Pathipati AS, Ko JM. Implementation and evaluation of Stanford Health Care direct-care teledermatology program. SAGE open Med. 2016;4:2050312116659089. doi: 10.1177/2050312116659089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lester J, Weinstock MA. Teletriage for provision of dermatologic care: a pilot program in the department of veterans affairs. J Cutan Med Surg. 2014;18(3):170–173. doi: 10.2310/7750.2013.13086. [DOI] [PubMed] [Google Scholar]
- 26.Bosanac SS, Nguyen V, Bosanac D, Eisen DB, Sivamani RK. Randomized and controlled pilot study of the pragmatic use of mobile phone based follow up of actinic keratoses treated with topical 5-fluorouracil. Dermatol Online J. 2018;24(4):19. [PubMed] [Google Scholar]
- 27.Rajda J, et al. Impact of direct to consumer store-and-forward teledermatology on access to care, satisfaction, utilization, and costs in a commercial health plan population. Telemed e-Health. 2018;24(2):166–169. doi: 10.1089/tmj.2017.0078. [DOI] [PubMed] [Google Scholar]
- 28.Marchell R, Locatis C, Burgess G, Maisiak R, Liu W-L, Ackerman M. Patient and provider satisfaction with teledermatology. Telemed J E Health. 2017;23(8):684–690. doi: 10.1089/tmj.2016.0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chee SN, Lowe P, Lim A. Smartphone patient monitoring post-laser resurfacing. Australas J Dermatol. 2017;58(4):e216–e222. doi: 10.1111/ajd.12507. [DOI] [PubMed] [Google Scholar]
- 30.Livingstone J, Solomon J. An assessment of the cost-effectiveness, safety of referral and patient satisfaction of a general practice teledermatology service. London J Prim Care (Abingdon) 2015;7(2):31–35. doi: 10.1080/17571472.2015.11493433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ford JA, Pereira A. Does teledermatology reduces secondary care referrals and is it acceptable to patients and doctors?: a service evaluation. J Eval Clin Pract. 2015;21(4):710–716. doi: 10.1111/jep.12373. [DOI] [PubMed] [Google Scholar]
- 32.Frühauf J, et al. Mobile teledermatology helping patients control high-need acne: a randomized controlled trial. J Eur Acad Dermatol Venereol. 2015;29(5):919–924. doi: 10.1111/jdv.12723. [DOI] [PubMed] [Google Scholar]
- 33.Kraai IH, Luttik MLA, De Jong RM, Jaarsma T, Hillege HL. Heart failure patients monitored with telemedicine: patient satisfaction, a review of the literature. J Card Fail. 2011;17(8):684–690. doi: 10.1016/j.cardfail.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Ware JE, Snyder MK, Wright WR, Davies AR. Defining and measuring patient satisfaction with medical care. Eval Program Plann. 1983;6(3–4):247–263. doi: 10.1016/0149-7189(83)90005-8. [DOI] [PubMed] [Google Scholar]
- 35.Locatis C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345–350. doi: 10.1007/s11606-009-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eminović N, Witkamp L, De Keizer NF, Wyatt JC. Patient perceptions about a novel form of patient-assisted teledermatology [2] Arch Dermatol. 2006;142(5):648–649. doi: 10.1001/archderm.142.5.648. [DOI] [PubMed] [Google Scholar]
- 37.Wang RH, et al. Clinical effectiveness and cost-effectiveness of teledermatology: Where are we now and what are the barriers to adoption? J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.01.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sola-Ortigosa J, Muñoz-Santos C, Masat-Ticó T, Isidro-Ortega J, Guilabert A. The role of teledermatology and teledermoscopy in the diagnosis of actinic keratosis and field cancerization. J Invest Dermatol. 2020 doi: 10.1016/j.jid.2020.02.013. [DOI] [PubMed] [Google Scholar]
- 39.Vestergaard T, Prasad S, Schuster A, Laurinaviciene R, Andersen M, Bygum A. Diagnostic accuracy and interobserver concordance: teledermoscopy of 600 suspicious skin lesions in Southern Denmark. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16275. [DOI] [PubMed] [Google Scholar]
- 40.Andrees V, Klein TM, Augustin M, Otten M. Live interactive teledermatology compared to in-person care—a systematic review. J Eur Acad Dermatol Venereol. 2019 doi: 10.1111/jdv.16070. [DOI] [PubMed] [Google Scholar]
- 41.Sattler E, Kästle R, Welzel J. Optical coherence tomography in dermatology. J Biomed Opt. 2013;18(6):061224. doi: 10.1117/1.JBO.18.6.061224. [DOI] [PubMed] [Google Scholar]
- 42.Ulrich M, Lange-Asschenfeldt S. In vivo confocal microscopy in dermatology: from research to clinical application. J Biomed Opt. 2013;18(6):061212. doi: 10.1117/1.JBO.18.6.061212. [DOI] [PubMed] [Google Scholar]
- 43.Rubinstein G, Garfinkel J, Jain M. Live, remote control of an in vivo reflectance confocal microscope for diagnosis of basal cell carcinoma at the bedside of a patient 2500 miles away: a novel tele-reflectance confocal microscope approach. J Am Acad Dermatol. 2019;81(2):e41–e42. doi: 10.1016/j.jaad.2019.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sohn GK, Wong DJ, Yu SS. A review of the use of telemedicine in dermatologic surgery. Dermatol Surg. 2020;46(4):501–507. doi: 10.1097/DSS.0000000000002230. [DOI] [PubMed] [Google Scholar]