Abstract
Benign prostatic hyperplasia (BPH) is a benign enlargement of the prostate in which incidence increases linearly with age, beginning at about 50 years old. BPH is a significant source of morbidity in aging men by causing lower urinary tract symptoms and acute urinary retention. Unfortunately, the etiology of BPH incidence and progression is not clear. This review highlights the role of the androgen receptor (AR) in prostate development and the evidence for its involvement in BPH. The AR is essential for normal prostate development, and individuals with defective AR signaling, such as after castration, do not experience prostate enlargement with age. Furthermore, decreasing dihydrotestosterone availability through therapeutic targeting with 5α-reductase inhibitors diminishes AR activity and results in reduced prostate size and symptoms in some BPH patients. While there is some evidence that AR expression is elevated in certain cellular compartments, how exactly AR is involved in BPH progression has yet to be elucidated. It is possible that AR signaling within stromal cells alters intercellular signaling and a “reawakening” of the embryonic mesenchyme, loss of epithelial AR leads to changes in paracrine signaling interactions, and/or chronic inflammation aids in stromal or epithelial proliferation evident in BPH. Unfortunately, a subset of patients fails to respond to current medical approaches, forcing surgical treatment even though age or associated co-morbidities make surgery less attractive. Fundamentally, new therapeutic approaches to treat BPH are not currently forthcoming, so a more complete molecular understanding of BPH etiology is necessary to identify new treatment options.
Keywords: Prostate development, Benign prostatic hyperplasia, Androgen receptor, Prostate stroma, Inflammation
1. Introduction
1.1. Prostate anatomy and function
The prostate is a male urogenital organ located at the base of the bladder surrounding the urethra. Lowsley's classical studies [1] of the fetal human prostate described the organ as beginning to develop in the fetal male around the end of the first trimester, when “tubules” extend from the prostatic urethra defining lobes, or distinct anatomical regions, of the early prostate. However, the lobes he described in the developing prostate were not easily isolated or identified in the adult organ. The biological mechanisms underlying prostate development have continued to be studied largely because of their relevance to diseases such as benign prostatic hyperplasia (BPH) and prostate cancer (PCa). A comprehensive review of human prostate development describing the changes in thinking over the last century and summarizing current knowledge was recently published [2]. As with the fetal development, descriptions of the adult anatomy of this organ underwent a series of revisions during the 20th century. The field has now generally accepted the idea of prostatic zones, originally proposed by McNeal [3,4]. In this view, the prostate is comprised of three glandular zones, designated the central, peripheral, and transition zones with one non-glandular region of the anterior prostate composed of fibromuscular stroma which provides structural support [3].
The function of the prostate relies on its composition of both glandular and fibromuscular tissue. The fibromuscular tissue aids in the compartmentalization of fluids during urination and ejaculation. During urination, the central zone muscles contract, preventing urine from entering prostatic ducts. During ejaculation, the muscles near the top of the prostate, surrounding the base of the bladder, contract to prevent back-flow of semen into the bladder. The glandular tissue contributes a reproductive function through its significant secretory contribution to seminal fluid, including both ions (notably zinc and citrate) and proteins such as prostatic acid phosphatase (PAcP), β-microseminoprotein, and prostate-specific antigen (PSA) [5,6].
1.2. Overview of BPH
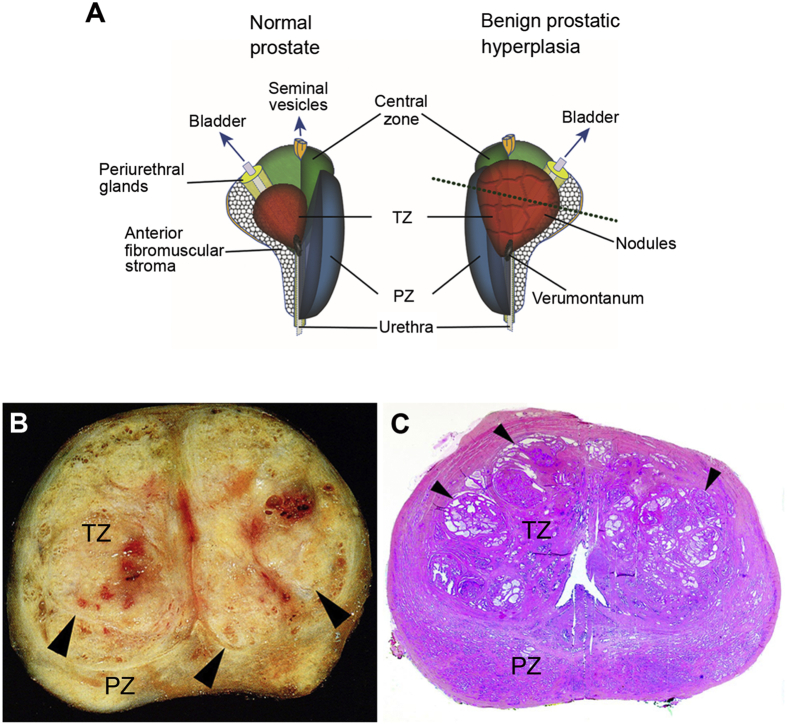
Benign enlargement of the prostate is a common, perhaps universal, condition in aging men (Fig. 1). While the terms BPH and benign prostatic hypertrophy have been used interchangeably in some clinical literature, this disease is a benign enlargement of the human prostate due to hyperplastic (increased cell number) rather than hypertrophic (increased cell size) expansion of glandular and/or stromal tissue. The major site of origin of BPH pathogenesis is the preprostatic region of the prostate [3], immediately distal to the urinary bladder, surrounding the preprostatic sphincter, and extending along the prostatic urethra prior to the verumontanum (Fig. 1A). While its histology is similar to the peripheral zone, within which it was originally included by McNeal, there is an abrupt reduction in the size and degree of development of the duct system from the peripheral zone to the preprostatic region. The preprostatic region is further subdivided into the periurethral glands and transition zone. The periurethral zone surrounds the urethra within the sleeve of the preprostatic sphincter while the transition zone in turn surrounds the sphincter. McNeal [4] made clear that the site of BPH origin includes both periurethral and transition zones even though this is a restricted region comprising perhaps 5% of the total volume of a normal young prostate.
Figure 1.
Benign prostatic hyperplasia (BPH) in human prostate tissue. (A) Diagrams representing anatomical features of normal human prostate and BPH. BPH originates within the preprostatic region, containing the transition zone (TZ) and periurethral glands. A dashed line through the BPH diagram represents an approximate cross-sectional location of a whole-mount pathological view of BPH, as in (B) and (C). Human prostate cut along the transverse plan to observe a gross view (B) or whole mount H&E section (C). TZ and peripheral zone (PZ) are labeled and BPH nodules are indicated by black arrows. Modified from Aaron et al. [8].
BPH involves two primary phases of progression, pathological and clinical. The pathological phase of BPH is subdivided into microscopic and macroscopic BPH. Microscopic BPH includes enhanced proliferation/hyperplasia of either epithelial or stromal cells that may lead to abnormal enlargement of the prostate gland (i.e. macroscopic BPH). Normal prostatic glands contain a luminal epithelial layer surrounded by a monolayer of basal cells, while pseudostratification leading to two or more layers of basal nuclei causing a papillary-like configuration is evident in microscopic BPH. If macroscopic BPH develops, a subset of men with enlarged prostates will present with symptomatic dysuria, resulting in the clinical phase of BPH [7]. Although BPH itself, at least in the face of medical care, is not fatal, it is a significant cause of morbidity due to the development of lower urinary tract symptoms (LUTS). LUTS includes both voiding symptoms, such as weakness of urinary stream, hesitancy, intermittency, sense of incomplete emptying of bladder, and straining to void, as well as storage symptoms, including frequency, nocturia, and urgency [8,9]. Some of these symptoms of clinical BPH are the result of increased transition zone volume pushing on or occluding the urethra as well as extending the periphery of the prostate outward (macroscopic BPH) [10,11]. However, alternative processes including fibrosis or smooth muscle contractility changes may also contribute to LUTS [12,13].
BPH nodules are of two distinct types. Periurethral nodules are usually stromal in character or show only a few small glands penetrating from the periphery. The stromata in these nodules have been described as reminiscent of the embryonic mesenchyme; this observation gave rise to McNeal's hypothesis that BPH involves a “reawakening” of embryonic stromal cells [3]. Transition zone nodules are almost always composed of glandular tissue derived from newly formed small duct branches. These branches bud off from pre-existing ducts, grow into the adjacent stroma and repeatedly branch creating a new architectural system within the nodule. Individual patients usually have several nodes which appear to grow in a coordinated manner, but they may have all glandular, all stromal, or mixed BPH nodules within their prostate. Different nodules within BPH patients have been indicated as a source of phenotypic heterogeneity, with one or more nodules that respond to targeted therapies while other nodules may be resistant [14]. Thus, it is evident that heterogeneity in BPH exists to some degree, but whether cellular heterogeneity exists in BPH as defined in PCa and other cancers has not been studied.
BPH is extremely common and disease risk increases linearly with age, beginning at about age 40; almost all men who live to 90 years of age will develop microscopic BPH [15]. However, not all of these men will develop macroscopic disease and only about half of men with macroscopic BPH will progress to the clinical stage with associated LUTS [7]. Due to the requirement of androgens for progression of this disease, therapies aimed at reducing androgen receptor (AR) activity have been used as a treatment to alleviate symptoms of clinical BPH through the reduction of prostate size [11]. This review will highlight the role of AR in BPH pathogenesis, beginning with the contributions of AR in prostate development.
2. The importance of androgens and the AR in prostate development
2.1. Androgen action in early prostatic development
The prostate is completely dependent on testicular androgens for both its development and the maintenance of its structural and functional integrity. In humans this is reflected in the natural history of the organ. The prostate is small in boys during childhood, weighing around 2 g. At puberty it undergoes a phase of exponential growth, increasing in size to about 20 g. This corresponds to the rise in serum testosterone to adult levels. The human prostate reaches its normal adult size by 18–20 years of age and subsequently halts growth despite sustained circulating levels of androgen. This transition from prostatic growth to a steady-state phase is maintained by a balance of cell proliferation/death and is controlled by AR signaling in both the stroma and epithelium. After puberty, mean prostatic weight stabilizes and remains fairly constant until the end of the fifth decade of life. At this point, mean prostatic weight in the population begins to rise slowly, predominantly reflecting the incidence of BPH as men age [15].
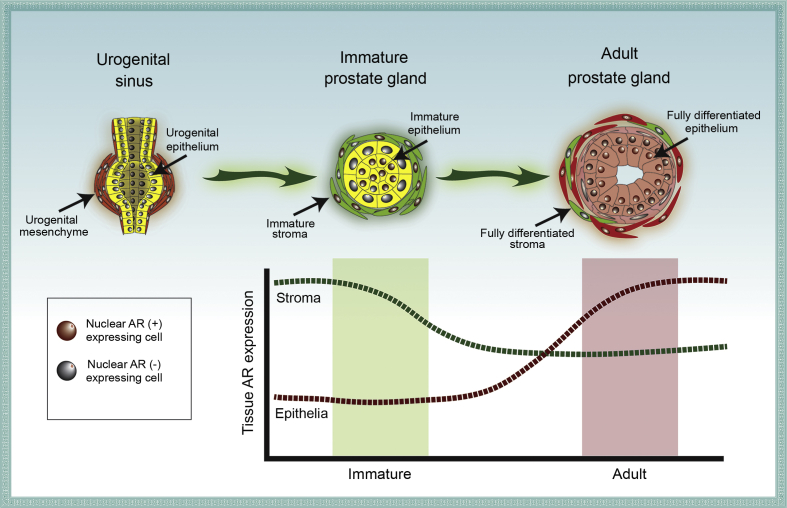
The AR is a transcription factor that mediates the effects of androgens in concert with a number of, often tissue specific, co-factors [16,17]. AR is expressed early in prostatic development and androgens are essential for development of the prostate gland and other reproductive organs in males in utero [18]. AR is expressed in the mesenchyme of the fetal urogenital sinus and androgen action on these stromal receptors is necessary to induce the initiation of prostatic buds in the epithelium of the sinus. AR expression in the epithelium lags that of the mesenchyme but can be detected in mice as epithelial prostatic buds start to form around embryonic Day 18 [19]. Throughout development, epithelial AR signaling increases during epithelial bud protrusion and extension [20,21]. Deletion and mutations of the AR leading to a non-functional receptor result in the lack of a prostate, showing the AR is critical for prostatic cell growth and development [22]. Work by Cunha and others [23,24] demonstrated that stromal AR is required for epithelial cell proliferation and differentiation during normal development, while epithelial AR expression is essential for the differentiated functions of the gland (Fig. 2).
Figure 2.
Androgen receptor (AR) expression in prostatic cell types during development. Prostatic development is initiated with development of a urogenital sinus (UGS), followed by extension of prostatic buds forming an immature prostate gland. The adult prostate gland contains fully differentiated stromal and epithelial compartments which form a mature and functional organ. AR is initially expressed in just a proportion of the urogenital sinus mesenchyme (UGM). Epithelial cells gain AR expression throughout development. While only a subset of stromal cells (e.g. fibroblasts and smooth muscle cells) maintain AR expression in the adult prostate, virtually all luminal epithelial cells express AR.
The primary source of androgens, namely testosterone, is from testicular secretion. Once androgens reach prostatic tissue, three 5α-reductase isozymes (produced by the SRD5A1, SRD5A2, and SRD5A3 genes) convert testosterone to dihydrotestosterone (DHT), which binds the receptor with two- to five-fold higher affinity in prostate cells and elevates AR signaling 10-fold compared to testosterone [25,26]. In the prostate the dominant 5α-reductase is isozyme 2. Individuals without functional 5α-reductase 2 (SRD5A2) have small or undetectable prostates in addition to ambiguous genitalia throughout childhood, but at the time of puberty increased testosterone production induces masculinization of the external genitalia. These individuals maintain small prostates throughout adulthood but treatment with DHT can increase prostate size. Together, these data indicate that DHT is required for complete development of the adult prostate [27]. Androgen availability, AR expression, and 5α-reductase activity all serve critical roles in prostate development.
2.2. AR structure and function in prostate cells
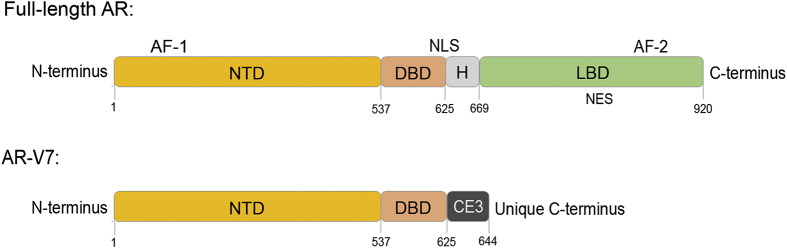
The AR is a member of the steroid and nuclear receptor family of transcription factors which contains an N-terminal domain (NTD), DNA-binding domain (DBD), hinge region, and a C-terminal ligand-binding domain (LBD) (Fig. 3). The NTD contains an activation function (AF)-1 region and can promote transcriptional activity of the AR in the presence or absence of the LBD. The DBD contains two zinc-finger domains which recognize androgen-response elements for DNA-binding and transcriptional activation but also for dimerization [28]. The hinge region allows for flexibility between domains of the protein but also contains a nuclear localization signal that is exposed upon ligand binding to AR [29]. Finally, the LBD contains the androgen binding site and an AF-2 region which is necessary for binding of AR coactivators [30,31].
Figure 3.
General protein structures of androgen receptor (AR) and AR-V7. Full-length AR contains functional domains: NTD, N terminal domain; DBD, DNA-binding domain; H, hinge region; LBD, ligand-binding domain. General locations of the nuclear localization signal (NLS) and nuclear export signal (NES) are indicated, along with regions of transcriptional activation function (AF)-1 and AF-2 binding sites. AR-V7 contains the NTD and DBD, but alternative splicing of the gene truncates the protein leaving only cryptic exon 3 (CE3) at the C-terminus. Numbers flanking domains indicate the approximate amino acid at that location.
Throughout the last decade, the discovery of AR variants, which are produced from alternative splicing of the full-length AR mRNA transcript has complicated our perception of androgenic signaling. Numerous splice variants have been discovered to-date, most of which maintain the NTD and DBD, but contain truncated, missing, or variable C-termini (Fig. 3) [32,33]. AR variants have been discovered in normal tissues, and one example has been shown to have a regulatory role of full-length AR in PCa cells [33,34]. Without the LBD, AR variants can dimerize without ligand (either homodimerize with one another or heterodimerize with full-length AR) and promote activation of AR target genes [35].
When unbound to ligand, the inactive AR resides in the cytoplasm in complex with other proteins. In this inactive state, AR is bound to the chaperone proteins heat shock protein (HSP) 70 and HSP40 along with co-chaperones [36] to form a mature aporeceptor complex maintaining AR in a conformation suitable for binding of DHT [37,38]. In the absence of ligand, the AR degrades quickly to end the chaperone cycle and the chaperones become available to form new complexes in an ATP-dependent process [25]. Binding of ligand, such as DHT, induces a conformational change in the ligand-binding domain of AR causing release of the chaperone complex and stabilization, phosphorylation, and dimerization of AR [37]. HSP27 binding to the AR homodimer prompts translocation to the nucleus and facilitates transcriptional activity of the AR [39].
In the nucleus, AR acts as a transcription factor by recognizing sequence-specific regions of DNA, AREs, where it can bind and promote transcription of specific genes. Other transcription factors have been demonstrated to associate with AR, such as direct interaction with forkhead box A1 (FOXA1) or FOXO1, with further complex formation with nuclear factor IB (NFIB) [16,40,41]. AR transcriptional activity has a very pronounced impact on gene regulation within some prostate cells. For example, AR has been defined to regulate transcription of 1.5%–4.3% of all gene transcripts within LNCaP cells, a cell line representing androgen-responsive PCa [42]. The targets of AR-driven transcription are dependent upon the profile of transcription factors expressed in a cell. This profile varies between organs and tissues resulting in different target genes being activated on a cell type-specific basis [43].
2.3. AR function in the adult prostate
In the adult prostate, the AR continues to be critical for maintenance of the organ. Unlike in the developing prostate, AR in the adult organ is primarily expressed in the prostatic luminal epithelial cells rather than stromal cells (Fig. 2). At any age, depletion of testosterone through surgical or chemical castration causes the prostate to involute and/or decrease in size due to loss of secretory luminal epithelial cells. The prostate has incredible self-renewal potential, since many cycles of involution followed by restoration with androgen supplementation demonstrated that the organ can continuously regenerate to its original size [44]. This ability reflects cyclic changes in androgen levels and prostate size that occur in many seasonally-breeding mammals [45,46]. In vivo modeling suggests that involution of the prostate, consistent with development, is a function of loss of androgen action on stromal rather than on epithelial cells [47,48]. Initial cellular changes following castration in rodent models are first seen in the endothelial cells sub-adjacent to the epithelium, with epithelial apoptosis apparently occurring as a secondary consequence [49].
Circulating androgens are primarily bound by proteins in the serum, but only androgens which are “free” of association with proteins are presumed to be capable of diffusing into the cells of target tissues, allowing for a cellular response to circulating hormones [50]. However, androgens, primarily testosterone or DHT, bound to sex hormone binding globulin (SHBG) secure increased half-life and allow serum androgen levels to rise while simultaneously preventing hypertrophy of reproductive organs [51]. Circulating testosterone levels have been demonstrated to decrease with age while SHBG levels increase with age, meaning that free testosterone becomes less available [52,53]. On the other hand, prostatic diseases become more prevalent with age and both BPH and PCa utilize androgens for their development and progression, indicating that prostatic cells in these diseased states are still able to function in the environment of lower circulating testosterone in aged men [7]. Nonetheless, both androgens and the AR are required for proper development and function of the adult prostate and there is an ongoing research effort to understand the mechanisms involved in androgen availability, transport, and AR activity in the prostate.
2.4. Generalized function of AR in prostate diseases
AR plays a role in multiple cellular processes such as differentiation, secretory function, metabolism, morphology, proliferation, and survival. As described above, AR activity is heavily involved in maintaining prostate function; in one analysis, researchers found that almost one-half of androgen-regulated genes are involved in synthesis and modification of secretory proteins [54]. Ligand occupancy of AR in luminal epithelial cells was determined to promote cellular quiescence and induce the completion of differentiation into secretory cells detectable by expression of PSA, PAcP, and other prostate luminal-secretory differentiation markers [55]. Cunha et al. [23,56] and Kurita et al. [47] demonstrated that when wild-type urogenital mesenchyme (UGM) was recombined with AR-null urogenital epithelium (UGE), the resulting prostatic tissues lacked fully differentiated luminal cells expressing secretory proteins. Similarly, selective deletion of luminal AR using targeted Cre recombinase expression resulted in poorly differentiated and hyper-proliferative epithelial structures [57]. Proteins involved in apoptosis were also determined to be regulated by AR activity, namely p53 regulator MDM2, caspase-2, and c-FLIP [[58], [59], [60]]. Mechanistically, luminal cell AR signaling induces G0 arrest by inhibiting c-MYC and RB function, while promoting p21 and p27 expression [61]. AR is recognized as a growth suppressor for a variety of other normal human epithelial cell types, such as thyroid and adrenocortical epithelial cells, where ligand-dependent endogenous AR signaling suppresses growth [62,63]. Further, Xin et al. [64] demonstrated that expression of AR suppressed the growth of murine prostate epithelial cells using an in vivo prostate regeneration system. These observations demonstrate an important growth suppressive and pro-differentiation role for AR in the normal prostate, particularly as it reaches adult steady-state size and function.
In contrast, studies of AR in PCa have clearly demonstrated that AR signaling acquires an oncogenic gain-of-function that drives cancer proliferation and tumor progression. The vast majority of prostate tumors express AR, and androgen-deprivation therapy is the predominant therapeutic strategy to reduce tumor burden and block cancer progression. Furthermore, AR remains a critical oncogenic driver in castration-resistant PCa [65,66]. Castration-resistant PCa cells do not undergo apoptosis when androgens are depleted or androgen antagonists are used; however, mechanistic studies in cell lines demonstrated that such cells stop proliferating and activate cell death if the AR protein level is reduced below a critical level both in vitro and in vivo [[67], [68], [69], [70]]. Thus, both clinical and mechanistic studies have documented an oncogenic dependency of cancer cells to AR signaling and have justified continued development of novel anti-androgens targeting AR.
In BPH, AR function within luminal cells mimics that of a tumor suppressor, and there is little evidence of AR converting to a driver of cell proliferation such as in PCa. Thus, luminal epithelial cells in BPH remain differentiated and proliferatively quiescent. This supports a model whereby AR signaling within the prostate epithelium retains its normal adult function in BPH but instead inflammation and fetal reprogramming disrupt normal stromal/epithelial paracrine signaling. Such changes to the prostate microenvironment enable prostate epithelial cells to exit a steady-state of proliferation/death and enter into an abnormal growth phase leading to cellular overexpansion [44].
3. AR expression and function in BPH
3.1. Evidence for a role of the AR in BPH
An association between BPH and testicular hormone production has long been suspected, based on observations that men castrated before 40 years old do not develop BPH. For example, Russian Skoptzys, who underwent ritual castration at 35 years old did not develop prostatic enlargement [71]. In the late 1800's, elimination of testicular function by castration was found to induce atrophy in the prostates of 87% of men with BPH symptoms [72]. Finally, study of individuals who became Chinese Imperial eunuchs between the ages of 10–26 also indicated that testosterone is essential for prostatic development and preservation, since the prostates of these men remained rectally impalpable in 21/26 men or small (1–2 cm) in 5/26 men 5 decades later [73].
Some research has been conducted to determine the levels of testosterone and DHT in men with or without BPH. Prostatic levels of testosterone seem to be similar in patients with BPH compared to younger, normal individuals. In contrast, circulating levels of androgens tend to decrease as men age and are inversely correlated with a diseased prostate [52,74,75]. Interestingly, a small study investigating the effects of testosterone replacement therapy in aging men described elevated serum testosterone levels but no change in prostatic testosterone/DHT, indicating that prostatic androgen titers may not be inherently linked to serum levels [76]. In addition, some evidence suggests circulating DHT is not significantly altered throughout aging, supporting the role of SRD5A in peripheral tissues [74,77]. Serum PSA levels have been determined to correlate with prostate size, specifically of the transition zone [78,79]. This suggests that AR activity is involved in the cell proliferation observed in BPH.
Clinically, 5α-reductase inhibitors (5-ARIs) have been used for decades to alleviate LUTS symptoms associated with BPH. Two widely-used 5-ARIs have been developed to inhibit conversion of testosterone to DHT: finasteride is a SRD5A2 specific inhibitor and dutasteride is a dual SRD5A1/2 inhibitor. In general, patients with larger prostates respond more favorably to finasteride treatment versus an alternative therapy (α-blocker, discussed below), suggesting that BPH/LUTS symptoms due to increased prostate volume can be resolved by inhibition of AR activity. Furthermore, finasteride treatment decreases surgical intervention and the risk of urinary retention on account of its ability to reduce prostate volume [80,81].
The clinical use of 5-ARIs clearly demonstrates a potential role for AR in promoting macroscopic BPH, but studies in human patients have obvious limitations. For further analysis of mechanistic contributions of AR toward the etiology of BPH, most researchers utilize one or more models of BPH in vitro or in vivo. Of course, in vivo models are preferred over in vitro models as more accurate representations of disease state containing diverse cell types in a complex microenvironment. Unfortunately, the murine prostate is composed of four distinct pairs of lobes which are not closely associated with the urethra, a stark anatomical difference to the human organ [20]. Nonetheless, rodent models remain one of the limited options for in vivo study of BPH. One notable model that recapitulates some aspects of the human disease is a testosterone+estrogen steroid hormone implantation protocol, mimicking the decreased trend in serum testosterone levels along with stagnant or increasing serum estrogen levels in aging men [52,82,83]. This model induces expansion of prostatic ductal tissue within the rhabdosphincter, causing urinary retention in mice and rats [84,85]. Numerous alternative BPH models have been studied and have been reviewed previously [[88], [87], [86]].
3.2. Inflammation in BPH
Increased inflammation is closely associated with the severity of BPH/LUTS. Data from the Medical Therapy of Prostatic Symptoms (MTOPS) study show that the risk of BPH progression and acute urinary retention is greater in men with prostatic inflammation [81,89]. Inflammation has also been linked to the development of hyperplasia. In BPH patients, stromal nodules were found to contain increased numbers of T and B lymphocytes [90]. Elevated levels of inflammatory cells were also detected in the interstitium and surrounding epithelial glands of human BPH tissues [91]. Chemokines and cytokines acting within and between the immune/inflammatory infiltrate and the prostatic epithelium and stroma provide mitogenic signals that can contribute to prostate growth [92,93]. Type-1 cytokines are produced by T-helper 1 (Th1) cells while Type-2 cytokines are those produced by Th2 cells. Type-1 cytokines include IL-2, IFN-γ, IL-12 and TNF-β, while Type-2 cytokines include IL-4, -5, -6, -10, and -13. Monocytes/macrophages produce some of the cytokines associated with Type-2 Th cells, such as IL-6 and IL-10. In response to IFNs, they release proinflammatory cytokines such as TNF-α and IL-1, which interact with Type-1 and -2 cytokines as part of the complex interregulatory cytokine networks [94]. A number of different immune and inflammatory cell types are commonly seen in the prostate [95]. B and T cells (notably CD4+) as well as macrophages and mast cells are seen throughout the stromal and glandular tissue. As men age, the number of T cells increases and can be pronounced in BPH. Inflammatory cell infiltrates in BPH are mixed, but include chronically activated T cells (approximately 70%), B lymphocytes (approximately 15%), and macrophages (approximately 15%) [96].
Progression of BPH towards increased LUTS or surgical intervention is also associated with increases in inflammatory infiltrate. In late stage human BPH samples, leukocytes typically make up around 20% of the total cells and CD11b+ cells on the monocyte/macrophage lineage are around 50% of the total leukocytes [97,98]. These cells are candidate players in the development and progression of BPH/LUTS. Macrophages are functionally diverse, modulating the adaptive immune response. They are involved in the induction and resolution of inflammation and are an important part of the immune/inflammatory environment seen in BPH [95,99,100]. This diversity requires changes in cellular phenotype notably towards the classically described M1 (broadly proinflammatory) and M2 (broadly inflammation resolving) phenotypes. As a crude measure of the M1/M2 ratio in BPH, the ratio of CD68+ cells (a surrogate for M1 macrophages) and CD163+ cells (a surrogate for M2 macrophages) changes with time, more than doubling the proportion of CD68+ cells relative to the CD163+ cells as BPH progresses to surgery (Aaron-Brooks and Hayward, unpublished data). This result is consistent with the plasticity of macrophages, which modulate phenotype in response to environmental signals [101].
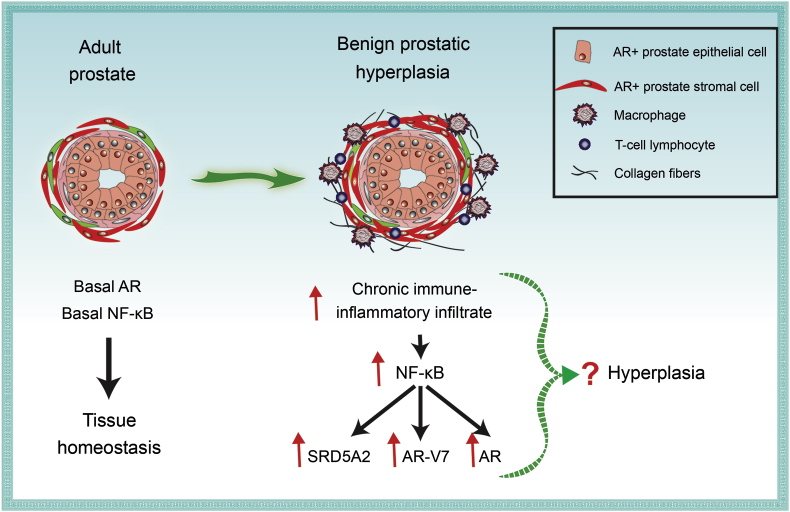
On a molecular level, inflammatory mediators seem to be involved in BPH progression toward surgery. Surgical BPH specimens have significantly elevated AP-1 transcription factor expression (specifically JUN and c-FOS) in the basal epithelium and stromal compartments compared to incidental BPH samples [102]. Furthermore, canonical NF-κB signaling is enhanced in both epithelial and stromal compartments of advanced versus early stage/low symptom BPH samples, providing evidence for enhanced inflammatory signaling within the prostate as BPH progresses [103]. Indeed, chronic inflammation in the MTOPS cohort increased the risk of BPH progression, but 5-ARI treatment reduced the risk of progression in patients with chronic inflammation [89]. These data suggest a link between inflammatory signaling and AR activity. Elevated NF-κB activity is seen in BPH samples, particularly as disease progresses, and is associated with expression of the constitutively active splice variant AR-V7 as well as with elevation of SRD5A2 expression. Experimentally, NF-κB activation has been shown to elevate the proliferation rates of benign epithelial and stromal cell lines in vitro, as well as upregulate SRD5A2 and stimulate AR and AR-V7 expression [103,104] (Fig. 4). It is also note-worthy that expression of NF-κB and AR-V7 in BPH may provide a mechanism for 5-ARI resistance via stimulation of SRD5A isoform expression [104].
Figure 4.
Summary of alterations in BPH. The normal adult prostate has low immune cell infiltration, basal AR expression, and basal levels of NF-κB activity, allowing for steady-state cell death/proliferation rates and maintenance of tissue homeostasis. In a prostate with BPH, there is increased collagen deposition and infiltration of inflammatory mediators, such as T cells and macrophages, resulting in a chronic inflammatory status within the prostate. Elevated inflammation results in NF-κB activation, which has been demonstrated to stimulate expression of SRD5A2, AR, and AR-V7. Inflammation, NF-κB activity, or AR could each be involved in the development of hyperplasia in epithelial or stromal cells observed in BPH nodules. AR, androgen receptor; BPH, benign prostatic hyperplasia; SRD5A2, 5α-reductase 2.
3.3. The role of AR in BPH etiology: A summary of mechanisms
Several transcription factors have been determined to influence AR target gene expression or play a role in the hyperplastic phenotype in the prostate. Deletion of FOXA1 in the luminal epithelium of adult mice causes basal cell expansion and progressive hyperplasia within the anterior prostate [105]. Additionally, NFIB-binding sites have been shown to have significant overlap with AR- and FOXA1-binding sites, and loss of NFIB induces hyperplasia in a mouse model. Grabowska et al. [40] also demonstrated that loss of NFIB is associated with BPH severity in patients. SRY-related HMG box 2 (SOX2) is another transcription factor that has been implicated in prostatic diseases, since 26/30 BPH specimens display SOX2+ staining in basal cells while only 2/24 PCa specimens maintain SOX2 expression [106]. While the exact mechanism of how these transcription factors contribute to BPH pathogenesis is unknown, it seems that alterations in expression of these factors influences AR transcriptional activity and/or hyperplastic response in the prostate.
While epithelial AR continues to be extensively studied, it is becoming increasingly clear that stromal AR expression may have alternate and/or cooperative effects. Clinically, loss of stromal AR correlates with poor clinical outcome in PCa patients, perhaps due to diminished extracellular matrix protein expression causing increased metastatic potential [5]. Conversely, stromal AR may also contribute to carcinogenesis, since its activity is capable of promoting PCa in early stages [107,108]. Androgen treatment has been determined to inhibit AR activity in stromal cells, while it is known to enhance AR activity in epithelial cells [109]. In fact, investigation of the overlap of AR target genes in stromal versus epithelial cells using primary embryonic prostate fibroblasts and PCa cell lines determined very little overlap in AR binding sites by ChIPseq [43]. These studies indicate that the target gene profile of AR is strikingly different in epithelial versus stromal cells, and stromal AR targets are only just beginning to be studied. The differences in androgen-regulated genes between prostate epithelial and stromal cells may be due to the distinct profile of transcription factors in these cell types in relation to their specific function. For example, even though FOXA1 is the dominant pioneer factor in prostate epithelial cells, the JUN/AP-1 complex or zinc finger protein, X-linked (ZFX) primarily associates with AR in prostate fibroblasts [17,43]. Following suit, the profile of androgen regulated genes in prostate epithelial cells differs from those of seminal vesicle epithelial cells [105,110]. Stromal AR has also been implicated in BPH, since AR has been shown to enhance stromal cell proliferation both in response to macrophage infiltration and via insulin-like growth factor (IGF)-1 [100,107]. More studies are necessary to fully understand the role of stromal AR in prostatic diseases.
Surprisingly, it is not completely clear whether or not AR expression changes throughout BPH progression. In general, it seems that both epithelial and stromal AR may be involved in this disease, and perhaps an increase in the ratio of stromal: Epithelial AR in BPH compared to normal adult prostate influences disease outcome. In one study, AR mRNA expression was increased in stromal cells but decreased in epithelial cells of BPH compared to normal prostate [111]. Further, transcript levels of AR and ERβ indicated higher ratios of AR:ERβ in BPH compared to normal in primary stromal cells, suggesting elevated AR activity [111]. In another study, analysis of 26 advanced and 37 early BPH cases identified no significant changes in AR expression, but did verify decreased PSA expression in patients taking 5-ARIs compared to those without [102]. Thus, a subset of patients taking 5-ARIs progressed toward surgery due to continued enlargement of their prostate, even though the drugs were apparently functionally successful. This has been supported by development of prostatic hyperplasia in the non-obese diabetic (NOD) mouse model, where focal growth persists in diabetic animals even though these animals demonstrate testicular atrophy [112].
The implications of altered AR expression throughout the progression of BPH are still being investigated, but several studies suggest a role for AR in localized inflammation. In the NOD mouse model, both diabetic and non-diabetic NOD mice had an association between local inflammation and increased severity of prostatic hyperplasia [112]. In other studies using a mouse model with a conditional AR knockout in luminal epithelial cells (K8-CreERT2; Arfl/Y), Zhang et al. [113] demonstrated that loss of AR signaling in luminal cells increases epithelial proliferation by enhancing local inflammation in an IL-1-dependent manner. Stromal AR has also been shown to be involved in the inflammatory process. Stromal AR expression induces proliferation and macrophage recruitment in a CCL3-dependent mechanism [100]. In this case, preferential BPH pathogenesis in the transition zone of the prostate may be explained by increased AR expression in transition zone fibroblasts compared to peripheral zone fibroblasts [114].
In summary, it is evident that alterations in AR expression/signaling seem to be involved in the etiology of BPH, although many questions remain. Is BPH truly caused by a “reawakening” of the prostate stroma with elevated AR expression, can BPH be initiated by the perturbation of AR signaling in luminal cells, or is BPH the consequence of altered paracrine signaling interactions within the prostate? Even though much evidence suggests a positive association between AR activity and BPH progression, mechanistic studies demonstrate an alternative hypothesis: Inhibition of AR activity, increased inflammation, and NF-κB activation within the prostate aid in the enhanced cell proliferation observed in BPH (Fig. 4). While this seems counter-intuitive when considering the clinical data, it is likely that prostatic inflammation contributes to BPH progression in ways that are not yet understood.
4. Alternate treatment strategies for BPH
As discussed above, 5-ARIs are one of the primary treatment strategies for patients with BPH. By inhibiting SRD5A activity, finasteride and dutasteride aim to reduce prostate size causing alleviation of BPH symptoms within about 3 months of initiation of therapy [80]. An alternate medical approach is also used as a primary treatment option for BPH. Alpha-adrenergic receptor antagonists (α-blockers) bind to the α1-adrenergic receptors causing smooth muscle relaxation in the prostate and bladder neck [81]. Doxazosin or terazosin, α-blockers used clinically, have been used both individually and in combination with 5-ARIs for treatment of BPH. The MTOPS study determined that combination therapy could reduce the incidence of progression but not decrease the risk of invasive therapy or acute urinary retention over finasteride alone in men with BPH [81]. Unfortunately, many patients either fail to respond or become resistant to current medical approaches over time, resulting in progression to surgical intervention [81]. As a result, both understanding treatment failure and developing new medical therapies appropriately targeted to specific patient groups are necessary to move toward precision medicine for BPH.
5. Conclusion
AR activity is necessary for prostate development and linked to development and progression of prostatic diseases, including BPH. Treatment of BPH patients with 5-ARIs to reduce AR activity remains one of the primary approaches to attempt to alleviate clinical symptoms and LUTS, but not all patients respond to 5-ARIs. The data discussed in this review support a role for AR activation in the development of BPH, but the mechanism(s) involved are unclear. There is some evidence using BPH models which indicate elevated AR or AR-V7 expression in BPH compared to normal tissue, but other studies suggest BPH tissues harbor a loss of AR activity in luminal epithelial cells or a decreased epithelial: Stromal ratio of AR expression/activity. In any case, it is likely that inflammation is involved in progression of BPH toward surgery. While the role or consequence of elevated inflammation in BPH initiation and progression is not entirely understood, the induction of inflammation in BPH could be related to luminal AR expression/activity. Also, inflammatory signaling (NF-κB) is linked to both AR expression and proliferation of epithelial and stromal cells. Both AR and inflammation are involved in BPH progression but the complex mechanistic interactions have yet to be elucidated.
Author contributions
Study design: Renee E. Vickman, Donald J. Vander Griend, Praveen Thumbikat, Simon W. Hayward.
Data acquisition: Renee E. Vickman, Omar E. Franco, Daniel C. Moline, Donald J. Vander Griend, Praveen Thumbikat, Simon W. Hayward.
Data analysis: Renee E. Vickman, Omar E. Franco, Simon W. Hayward.
Drafting of manuscript: Renee E. Vickman, Omar E. Franco, Daniel C. Moline, Donald J. Vander Griend, Praveen Thumbikat, Simon W. Hayward.
Critical revision of the manuscript: Renee E. Vickman, Simon W. Hayward.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
This work was supported by grants 1R01DK117906 and 1P20DK116185 from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and by the NorthShore Foundation.
Footnotes
Peer review under responsibility of Second Military Medical University.
References
- 1.Lowsley O.S. The development of the human prostate gland with reference to the development of other structures at the neck of the urinary bladder. Am J Anat. 1912;13:299–349. [Google Scholar]
- 2.Cunha G.R., Vezina C.M., Isaacson D., Ricke W.A., Timms B.G., Cao M. Development of the human prostate. Differentiation. 2018;103:24–45. doi: 10.1016/j.diff.2018.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McNeal J.E. Anatomy of the prostate and morphogenesis of BPH. Prog Clin Biol Res. 1984;145:27–53. [PubMed] [Google Scholar]
- 4.McNeal J.E. The zonal anatomy of the prostate. Prostate. 1981;2:35–49. doi: 10.1002/pros.2990020105. [DOI] [PubMed] [Google Scholar]
- 5.Leach D.A., Need E.F., Toivanen R., Trotta A.P., Palethorpe H.M., Tamblyn D.J. Stromal androgen receptor regulates the composition of the microenvironment to influence prostate cancer outcome. Oncotarget. 2015;6:16135–16150. doi: 10.18632/oncotarget.3873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lilja H., Abrahamsson P.A. Three predominant proteins secreted by the human prostate gland. Prostate. 1988;12:29–38. doi: 10.1002/pros.2990120105. [DOI] [PubMed] [Google Scholar]
- 7.Isaacs J.T., Coffey D.S. Etiology and disease process of benign prostatic hyperplasia. Prostate Suppl. 1989;2:33–50. doi: 10.1002/pros.2990150506. [DOI] [PubMed] [Google Scholar]
- 8.Aaron L., Franco O.E., Hayward S.W. Review of prostate anatomy and embryology and the etiology of benign prostatic hyperplasia. Urol Clin N Am. 2016;43:279–288. doi: 10.1016/j.ucl.2016.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mobley D., Feibus A., Baum N. Benign prostatic hyperplasia and urinary symptoms: evaluation and treatment. Postgrad Med. 2015;127:301–307. doi: 10.1080/00325481.2015.1018799. [DOI] [PubMed] [Google Scholar]
- 10.Le Duc I.E. The anatomy of the prostate and the pathology of early benign hypertrophy. J Urol. 1939;42:1217–1241. [Google Scholar]
- 11.Izumi K., Mizokami A., Lin W.J., Lai K.P., Chang C. Androgen receptor roles in the development of benign prostate hyperplasia. Am J Pathol. 2013;182:1942–1949. doi: 10.1016/j.ajpath.2013.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fusco F., Palmieri A., Ficarra V., Giannarini G., Novara G., Longo N. Alpha1-blockers improve benign prostatic obstruction in men with lower urinary tract symptoms: a systematic review and meta-analysis of urodynamic studies. Eur Urol. 2016;69:1091–1101. doi: 10.1016/j.eururo.2015.12.034. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Nieves J.A., Macoska J.A. Prostatic fibrosis, lower urinary tract symptoms, and BPH. Nat Rev Urol. 2013;10:546–550. doi: 10.1038/nrurol.2013.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strand D.W., Costa D.N., Francis F., Ricke W.A., Roehrborn C.G. Targeting phenotypic heterogeneity in benign prostatic hyperplasia. Differentiation. 2017;96:49–61. doi: 10.1016/j.diff.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berry S.J., Coffey D.S., Walsh P.C., Ewing L.L. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132:474–479. doi: 10.1016/s0022-5347(17)49698-4. [DOI] [PubMed] [Google Scholar]
- 16.Gao N., Zhang J., Rao M.A., Case T.C., Mirosevich J., Wang Y. The role of hepatocyte nuclear factor-3 alpha (Forkhead Box A1) and androgen receptor in transcriptional regulation of prostatic genes. Mol Endocrinol. 2003;17:1484–1507. doi: 10.1210/me.2003-0020. [DOI] [PubMed] [Google Scholar]
- 17.Leach D.A., Panagopoulos V., Nash C., Bevan C., Thomson A.A., Selth L.A. Cell-lineage specificity and role of AP-1 in the prostate fibroblast androgen receptor cistrome. Mol Cell Endocrinol. 2017;439:261–272. doi: 10.1016/j.mce.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 18.Cooke P.S., Young P., Cunha G.R. Androgen receptor expression in developing male reproductive organs. Endocrinology. 1991;128:2867–2873. doi: 10.1210/endo-128-6-2867. [DOI] [PubMed] [Google Scholar]
- 19.Mirosevich J., Gao N., Matusik R.J. Expression of Foxa transcription factors in the developing and adult murine prostate. Prostate. 2005;62:339–352. doi: 10.1002/pros.20131. [DOI] [PubMed] [Google Scholar]
- 20.Cunha G.R., Donjacour A.A., Cooke P.S., Mee S., Bigsby R.M., Higgins S.J. The endocrinology and developmental biology of the prostate. Endocr Rev. 1987;8:338–362. doi: 10.1210/edrv-8-3-338. [DOI] [PubMed] [Google Scholar]
- 21.Cunha G.R., Fujii H., Neubauer B.L., Shannon J.M., Sawyer L., Reese B.A. Epithelial-mesenchymal interactions in prostatic development. I. morphological observations of prostatic induction by urogenital sinus mesenchyme in epithelium of the adult rodent urinary bladder. J Cell Biol. 1983;96:1662–1670. doi: 10.1083/jcb.96.6.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunha G.R. The dual origin of vaginal epithelium. Am J Anat. 1975;143:387–392. doi: 10.1002/aja.1001430309. [DOI] [PubMed] [Google Scholar]
- 23.Cunha G.R., Chung L.W. Stromal-epithelial interactions-I. Induction of prostatic phenotype in urothelium of testicular feminized (Tfm/y) mice. J Steroid Biochem. 1981;14:1317–1324. doi: 10.1016/0022-4731(81)90338-1. [DOI] [PubMed] [Google Scholar]
- 24.Donjacour A.A., Cunha G.R. Assessment of prostatic protein secretion in tissue recombinants made of urogenital sinus mesenchyme and urothelium from normal or androgen-insensitive mice. Endocrinology. 1993;132:2342–2420. doi: 10.1210/endo.132.6.7684975. [DOI] [PubMed] [Google Scholar]
- 25.Kemppainen J.A., Lane M.V., Sar M., Wilson E.M. Androgen receptor phosphorylation, turnover, nuclear transport, and transcriptional activation. Specificity for steroids and antihormones. J Biol Chem. 1992;267:968–974. [PubMed] [Google Scholar]
- 26.Gao W., Bohl C.E., Dalton J.T. Chemistry and structural biology of androgen receptor. Chem Rev. 2005;105:3352–3370. doi: 10.1021/cr020456u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Imperato-McGinley J.G.L., Gautier T., Peterson RE. Steroid 5alpha-reductase deficiency in man: an inherited form of male pseudohermaphroditism. Science. 1974;186:1213–1215. doi: 10.1126/science.186.4170.1213. [DOI] [PubMed] [Google Scholar]
- 28.Umesono K., Evans R.M. Determinants of target gene specificity for steroid/thyroid hormone receptors. Cell. 1989;57:1139–1146. doi: 10.1016/0092-8674(89)90051-2. [DOI] [PubMed] [Google Scholar]
- 29.Cutress M.L., Whitaker H.C., Mills I.G., Stewart M., Neal D.E. Structural basis for the nuclear import of the human androgen receptor. J Cell Sci. 2008;121:957–958. doi: 10.1242/jcs.022103. [DOI] [PubMed] [Google Scholar]
- 30.Lonergan P.E., Tindall D.J. Androgen receptor signaling in prostate cancer development and progression. J Carcinog. 2011;10:20. doi: 10.4103/1477-3163.83937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lallous N., Dalal K., Cherkasov A., Rennie P.S. Targeting alternative sites on the androgen receptor to treat castration-resistant prostate cancer. Int J Mol Sci. 2013;14:12496–12519. doi: 10.3390/ijms140612496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu J., Van der Steen T., Tindall D.J. Are androgen receptor variants a substitute for the full-length receptor? Nat Rev Urol. 2015;12:137–144. doi: 10.1038/nrurol.2015.13. [DOI] [PubMed] [Google Scholar]
- 33.Dehm S.M., Tindall D.J. Alternatively spliced androgen receptor variants. Endocr Relat Cancer. 2011;18:R183–R196. doi: 10.1530/ERC-11-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahrens-Fath I., Politz O., Geserick C., Haendler B. Androgen receptor function is modulated by the tissue-specific AR45 variant. FEBS J. 2005;272:74–84. doi: 10.1111/j.1742-4658.2004.04395.x. [DOI] [PubMed] [Google Scholar]
- 35.Hu R., Dunn T.A., Wei S., Isharwal S., Veltri R.W., Humphreys E. Ligand-independent androgen receptor variants derived from splicing of cryptic exons signify hormone-refractory prostate cancer. Cancer Res. 2009;69:16–22. doi: 10.1158/0008-5472.CAN-08-2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cano L.Q., Lavery D.N., Bevan C.L. Mini-review: foldosome regulation of androgen receptor action in prostate cancer. Mol Cell Endocrinol. 2013;369:52–62. doi: 10.1016/j.mce.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 37.Picard D. The role of heat-shock proteins in the regulation of steroid receptor function. In: Freedman L.P., editor. Molecular Biology of Steroid and Nuclear Hormone Receptors. Progress in Gene Expression. Birkhäuser; Boston, MA: 1998. pp. 1–18. [Google Scholar]
- 38.Fang Y., Fliss A.E., Robins D.M., Caplan A.J. Hsp90 regulates androgen receptor hormone binding affinity in vivo. J Biol Chem. 1996;271:28697–28702. doi: 10.1074/jbc.271.45.28697. [DOI] [PubMed] [Google Scholar]
- 39.Zoubeidi A., Zardan A., Beraldi E., Fazli L., Sowery R., Rennie P. Cooperative interactions between androgen receptor (AR) and heat-shock protein 27 facilitate AR transcriptional activity. Cancer Res. 2007;67:10455–10465. doi: 10.1158/0008-5472.CAN-07-2057. [DOI] [PubMed] [Google Scholar]
- 40.Grabowska M.M., Kelly S.M., Reese A.L., Cates J.M., Case T.C., Zhang J. Nfib regulates transcriptional networks that control the development of prostatic hyperplasia. Endocrinology. 2016;157:1094–1109. doi: 10.1210/en.2015-1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao Y., Tindall D.J., Huang H. Modulation of androgen receptor by FOXA1 and FOXO1 factors in prostate cancer. Int J Biol Sci. 2014;10:614–619. doi: 10.7150/ijbs.8389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dehm S.M., Tindall D.J. Molecular regulation of androgen action in prostate cancer. J Cell Biochem. 2006;99:333–344. doi: 10.1002/jcb.20794. [DOI] [PubMed] [Google Scholar]
- 43.Nash C., Boufaied N., Mills I.G., Franco O.E., Hayward S.W., Thomson A.A. Genome-wide analysis of AR binding and comparison with transcript expression in primary human fetal prostate fibroblasts and cancer associated fibroblasts. Mol Cell Endocrinol. 2018;471:1–14. doi: 10.1016/j.mce.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 44.Isaacs J.T. Prostate stem cells and benign prostatic hyperplasia. Prostate. 2008;68:1025–1034. doi: 10.1002/pros.20763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paris D.B., Taggart D.A., Shaw G., Temple-Smith P.D., Renfree M.B. Changes in semen quality and morphology of the reproductive tract of the male tammar wallaby parallel seasonal breeding activity in the female. Reproduction. 2005;130:367–378. doi: 10.1530/rep.1.00538. [DOI] [PubMed] [Google Scholar]
- 46.Siwela A.A., Tam W.H. Ultrastructural changes in the prostate gland of a seasonally breeding mammal, the grey squirrel (Sciurus carolinensis Gmelin) J Anat. 1984;138:153–162. [PMC free article] [PubMed] [Google Scholar]
- 47.Kurita T., Wang Y.Z., Donjacour A.A., Zhao C., Lydon J.P., O'Malley B.W. Paracrine regulation of apoptosis by steroid hormones in the male and female reproductive system. Cell Death Differ. 2001;8:192–200. doi: 10.1038/sj.cdd.4400797. [DOI] [PubMed] [Google Scholar]
- 48.Wang Y., Sudilovsky D., Zhang B., Haughney P.C., Rosen M.A., Wu D.S. A human prostatic epithelial model of hormonal carcinogenesis. Cancer Res. 2001;61:6064–6072. [PubMed] [Google Scholar]
- 49.Shabsigh A., Chang D.T., Heitjan D.F., Kiss A., Olsson C.A., Puchner P.J. Rapid reduction in blood flow to the rat ventral prostate gland after castration: preliminary evidence that androgens influence prostate size by regulating blood flow to the prostate gland and prostatic endothelial cell survival. Prostate. 1998;36:201–206. doi: 10.1002/(sici)1097-0045(19980801)36:3<201::aid-pros9>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 50.Mendel C.M. The free hormone hypothesis: a physiologically based mathematical model. Endocr Rev. 1989;10:232–274. doi: 10.1210/edrv-10-3-232. [DOI] [PubMed] [Google Scholar]
- 51.Laurent M.R., Hammond G.L., Blokland M., Jardí F., Antonio L., Dubois V. Sex hormone-binding globulin regulation of androgen bioactivity in vivo: validation of the free hormone hypothesis. Sci Rep. 2016;6 doi: 10.1038/srep35539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harman S.M., Metter E.J., Tobin J.D., Pearson J., Blackman M.R. Baltimore longitudinal study of aging. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore longitudinal study of aging. J Clin Endocrinol Metab. 2001;86:724–731. doi: 10.1210/jcem.86.2.7219. [DOI] [PubMed] [Google Scholar]
- 53.Gray A., Feldman H.A., McKinlay J.B., Longcope C. Age, disease, and changing sex hormone levels in middle-aged men: results of the massachusetts male aging study. J Clin Endocrinol Metab. 1991;73:1016–1025. doi: 10.1210/jcem-73-5-1016. [DOI] [PubMed] [Google Scholar]
- 54.DePrimo S.E., Diehn M., Nelson J.B., Reiter R.E., Matese J., Fero M. Transcriptional programs activated by exposure of human prostate cancer cells to androgen. Genome Biol. 2002;3 doi: 10.1186/gb-2002-3-7-research0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang Q., Carroll J.S., Brown M. Spatial and temporal recruitment of androgen receptor and its coactivators involves chromosomal looping and polymerase tracking. Mol Cell. 2005;19:631–642. doi: 10.1016/j.molcel.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 56.Cunha G.R., Chung L.W., Shannon J.M., Taguchi O., Fujii H. Hormone-induced morphogenesis and growth: role of mesenchymal-epithelial interactions. Recent Prog Horm Res. 1983;39:559–598. doi: 10.1016/b978-0-12-571139-5.50018-5. [DOI] [PubMed] [Google Scholar]
- 57.Wu C.T., Altuwaijri S., Ricke W.A., Huang S.P., Yeh S., Zhang C. Increased prostate cell proliferation and loss of cell differentiation in mice lacking prostate epithelial androgen receptor. Proc Natl Acad Sci U S A. 2007;104:12679–12684. doi: 10.1073/pnas.0704940104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nantermet P.V., Xu J., Yu Y., Hodor P., Holder D., Adamski S. Identification of genetic pathways activated by the androgen receptor during the induction of proliferation in the ventral prostate gland. J Biol Chem. 2004;279:1310–1322. doi: 10.1074/jbc.M310206200. [DOI] [PubMed] [Google Scholar]
- 59.Rokhlin O.W., Taghiyev A.F., Guseva N.V., Glover R.A., Chumakov P.M., Kravchenko J.E. Androgen regulates apoptosis induced by TNFR family ligands via multiple signaling pathways in LNCaP. Oncogene. 2005;24:6773–6774. doi: 10.1038/sj.onc.1208833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gao S., Lee P., Wang H., Gerald W., Adler M., Zhang L. The androgen receptor directly targets the cellular Fas/FasL-associated death domain protein-like inhibitory protein gene to promote the androgen-independent growth of prostate cancer cells. Mol Endocrinol. 2005;19:1792–1802. doi: 10.1210/me.2004-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vander Griend D.J., Litvinov I.V., Isaacs J.T. Conversion of androgen receptor signaling from a growth suppressor in normal prostate epithelial cells to an oncogene in prostate cancer cells involves a gain of function in c-Myc regulation. Int J Biol Sci. 2014;10:627–642. doi: 10.7150/ijbs.8756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rossi R., Zatelli M.C., Valentini A., Cavazzini P., Fallo F., del Senno L. Evidence for androgen receptor gene expression and growth inhibitory effect of dihydrotestosterone on human adrenocortical cells. J Endocrinol. 1998;159:373–380. doi: 10.1677/joe.0.1590373. [DOI] [PubMed] [Google Scholar]
- 63.Rossi R., Zatelli M.C., Franceschetti P., Maestri I., Magri E., Aguiari G. Inhibitory effect of dihydrotestosterone on human thyroid cell growth. J Endocrinol. 1996;151:185–194. doi: 10.1677/joe.0.1510185. [DOI] [PubMed] [Google Scholar]
- 64.Xin L., Teitell M.A., Lawson D.A., Kwon A., Mellinghoff I.K., Witte O.N. Progression of prostate cancer by synergy of AKT with genotropic and nongenotropic actions of the androgen receptor. Proc Natl Acad Sci U S A. 2006;103:7789–7794. doi: 10.1073/pnas.0602567103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shah R.B., Mehra R., Chinnaiyan A.M., Shen R., Ghosh D., Zhou M. Androgen-independent prostate cancer is a heterogeneous group of diseases: lessons from a rapid autopsy program. Cancer Res. 2004;64:9209–9216. doi: 10.1158/0008-5472.CAN-04-2442. [DOI] [PubMed] [Google Scholar]
- 66.van Bokhoven A., Varella-Garcia M., Korch C., Johannes W.U., Smith E.E., Miller H.L. Molecular characterization of human prostate carcinoma cell lines. Prostate. 2003;57:205–225. doi: 10.1002/pros.10290. [DOI] [PubMed] [Google Scholar]
- 67.Zegarra-Moro O.L., Schmidt L.J., Huang H., Tindall D.J. Disruption of androgen receptor function inhibits proliferation of androgen-refractory prostate cancer cells. Cancer Res. 2002;62:1008–1013. [PubMed] [Google Scholar]
- 68.Yang Q., Fung K.M., Day W.V., Kropp B.P., Lin H.K. Androgen receptor signaling is required for androgen-sensitive human prostate cancer cell proliferation and survival. Cancer Cell Int. 2005;5:8. doi: 10.1186/1475-2867-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dehm S.M., Tindall D.J. Androgen receptor structural and functional elements: role and regulation in prostate cancer. Mol Endocrinol. 2007;21:2855–2863. doi: 10.1210/me.2007-0223. [DOI] [PubMed] [Google Scholar]
- 70.Snoek R., Cheng H., Margiotti K., Wafa L.A., Wong C.A., Wong E.C. In vivo knockdown of the androgen receptor results in growth inhibition and regression of well-established, castration-resistant prostate tumors. Clin Cancer Res. 2009;15:39–47. doi: 10.1158/1078-0432.CCR-08-1726. [DOI] [PubMed] [Google Scholar]
- 71.Zuckerman S. The endocrine control of the prostate: (section of urology) Proc R Soc Med. 1936;29:1557–1568. [PMC free article] [PubMed] [Google Scholar]
- 72.White J.W. The results of double castration in hypertrophy of the prostate. Ann Surg. 1895;22:1–80. doi: 10.1097/00000658-189507000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wu C.P., Gu F.L. The prostate in eunuchs. Prog Clin Biol Res. 1991;370:249–255. [PubMed] [Google Scholar]
- 74.Pirke K.M., Doerr P. Age related changes in free plasma testosterone, dihydrotestosterone and oestradiol. Acta Endocrinol. 1975;80:171–178. doi: 10.1530/acta.0.0800171. [DOI] [PubMed] [Google Scholar]
- 75.Trifiro M.D., Parsons J.K., Palazzi-Churas K., Bergstrom J., Lakin C., Barrett-Connor E. Serum sex hormones and the 20-year risk of lower urinary tract symptoms in community-dwelling older men. BJU Int. 2010;105:1554–1559. doi: 10.1111/j.1464-410X.2009.09090.x. [DOI] [PubMed] [Google Scholar]
- 76.Marks L.S., Mazer N.A., Mostaghel E., Hess D.L., Dorey F.J., Epstein J.I. Effect of testosterone replacement therapy on prostate tissue in men with late-onset hypogonadism: a randomized controlled trial. J Am Med Assoc. 2006;296:2351–2361. doi: 10.1001/jama.296.19.2351. [DOI] [PubMed] [Google Scholar]
- 77.Belanger A., Candas B., Dupont A., Cusan L., Diamond P., Gomez J.L. Changes in serum concentrations of conjugated and unconjugated steroids in 40- to 80-year-old men. J Clin Endocrinol Metab. 1994;79:1086–1090. doi: 10.1210/jcem.79.4.7962278. [DOI] [PubMed] [Google Scholar]
- 78.Hammerer P.G., McNeal J.E., Stamey T.A. Correlation between serum prostate specific antigen levels and the volume of the individual glandular zones of the human prostate. J Urol. 1995;153:111–114. doi: 10.1097/00005392-199501000-00038. [DOI] [PubMed] [Google Scholar]
- 79.Weber J.P., Oesterling J.E., Peters C.A., Partin A.W., Chan D.W., Walsh P.C. The influence of reversible androgen deprivation on serum prostate-specific antigen levels in men with benign prostatic hyperplasia. J Urol. 1989;141:987–992. doi: 10.1016/s0022-5347(17)41083-4. [DOI] [PubMed] [Google Scholar]
- 80.McConnell J.D., Bruskewitz R., Walsh P., Andriole G., Lieber M., Holtgrewe H.L. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. Finasteride long-term efficacy and safety study group. N Engl J Med. 1998;338:557–563. doi: 10.1056/NEJM199802263380901. [DOI] [PubMed] [Google Scholar]
- 81.McConnell J.D., Roehrborn C.G., Bautista O.M., Andriole G.L., Jr., Dixon C.M., Kusek J.W. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–2398. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- 82.Bjornerem A., Straume B., Midtby M., Fønnebø V., Sundsfjord J., Svartberg J. Endogenous sex hormones in relation to age, sex, lifestyle factors, and chronic diseases in a general population: the Tromso study. J Clin Endocrinol Metab. 2004;89:6039–6047. doi: 10.1210/jc.2004-0735. [DOI] [PubMed] [Google Scholar]
- 83.Ricke W.A., shii K., Ricke E.A., Simko J., Wang Y., Hayward S.W. Steroid hormones stimulate human prostate cancer progression and metastasis. Int J Cancer. 2006;118:2123–2131. doi: 10.1002/ijc.21614. [DOI] [PubMed] [Google Scholar]
- 84.Bernoulli J., Yatkin E., Konkol Y., Talvitie E.M., Santti R., Streng T. Prostatic inflammation and obstructive voiding in the adult Noble rat: impact of the testosterone to estradiol ratio in serum. Prostate. 2008;68:1296–1306. doi: 10.1002/pros.20791. [DOI] [PubMed] [Google Scholar]
- 85.Nicholson T.M., Ricke E.A., Marker P.C., Miano J.M., Mayer R.D., Timms B.G. Testosterone and 17β-estradiol induce glandular prostatic growth, bladder outlet obstruction, and voiding dysfunction in male mice. Endocrinology. 2012;153:5556–5565. doi: 10.1210/en.2012-1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mahapokai W., Van Sluijs F.J., Schalken J.A. Models for studying benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 2000;3:28–33. doi: 10.1038/sj.pcan.4500391. [DOI] [PubMed] [Google Scholar]
- 87.Hieble J.P. Animal models for benign prostatic hyperplasia. Handb Exp Pharmacol. 2011:69–79. doi: 10.1007/978-3-642-16499-6_4. [DOI] [PubMed] [Google Scholar]
- 88.Nicholson T.M., Ricke W.A. Androgens and estrogens in benign prostatic hyperplasia: past, present and future. Differentiation. 2011;82:184–199. doi: 10.1016/j.diff.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McVary K.T. A review of combination therapy in patients with benign prostatic hyperplasia. Clin Ther. 2007;29:387–398. doi: 10.1016/s0149-2918(07)80077-4. [DOI] [PubMed] [Google Scholar]
- 90.Bierhoff E., Vogel J., Benz M., Giefer T., Wernert N., Pfeifer U. Stromal nodules in benign prostatic hyperplasia. Eur Urol. 1996;29:345–354. doi: 10.1159/000473774. [DOI] [PubMed] [Google Scholar]
- 91.Theyer G., Kramer G., Assmann I., Sherwood E., Preinfalk W., Marberger M. Phenotypic characterization of infiltrating leukocytes in benign prostatic hyperplasia. Lab Investig. 1992;66:96–107. [PubMed] [Google Scholar]
- 92.Bushman W.A., Jerde T.J. The role of prostate inflammation and fibrosis in lower urinary tract symptoms. Am J Physiol Renal Physiol. 2016;311:F817–F821. doi: 10.1152/ajprenal.00602.2015. [DOI] [PubMed] [Google Scholar]
- 93.Jerde T.J., Bushman W. IL-1 induces IGF-dependent epithelial proliferation in prostate development and reactive hyperplasia. Sci Signal. 2009;2:ra49. doi: 10.1126/scisignal.2000338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dinarello C.A. Historical insights into cytokines. Eur J Immunol. 2007;37(Suppl1):S34–S45. doi: 10.1002/eji.200737772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kramer G., Marberger M. Could inflammation be a key component in the progression of benign prostatic hyperplasia? Curr Opin Urol. 2006;16:25–29. [PubMed] [Google Scholar]
- 96.Ribal M.J. The link between benign prostatic hyperplasia and inflammation. Eur Urol Suppl. 2013;12:103–109. [Google Scholar]
- 97.Torkko K.C., Wilson R.S., Smith E.E., Kusek J.W., van Bokhoven A., Lucia M.S. Prostate biopsy markers of inflammation are associated with risk of clinical progression of benign prostatic hyperplasia: findings from the MTOPS study. J Urol. 2015;194:454–461. doi: 10.1016/j.juro.2015.03.103. [DOI] [PubMed] [Google Scholar]
- 98.Strand D.W., Aaron L., Henry G., Franco O.E., Hayward S.W. Isolation and analysis of discreet human prostate cellular populations. Differentiation. 2016;91:139–151. doi: 10.1016/j.diff.2015.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Taoka R., Tsukuda F., Ishikawa M., Haba R., Kakehi Y. Association of prostatic inflammation with down-regulation of macrophage inhibitory cytokine-1 gene in symptomatic benign prostatic hyperplasia. J Urol. 2004;171:2330–2335. doi: 10.1097/01.ju.0000127760.87421.e9. [DOI] [PubMed] [Google Scholar]
- 100.Wang X., Lin W.J., Izumi K., Jiang Q., Lai K.P., Xu D. Increased infiltrated macrophages in benign prostatic hyperplasia (BPH): role of stromal androgen receptor in macrophage-induced prostate stromal cell proliferation. J Biol Chem. 2012;287:18376–18385. doi: 10.1074/jbc.M112.355164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Galdiero M.R., Bonavita E., Barajon I., Garlanda C., Mantovani A., Jaillon S. Tumor associated macrophages and neutrophils in cancer. Immunobiology. 2013;218:1402–1410. doi: 10.1016/j.imbio.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 102.Lin-Tsai O., Clark P.E., Miller N.L., Fowke J.H., Hameed O., Hayward S.W. Surgical intervention for symptomatic benign prostatic hyperplasia is correlated with expression of the AP-1 transcription factor network. Prostate. 2014;74:669–679. doi: 10.1002/pros.22785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Austin D.C., Strand D.W., Love H.L., Franco O.E., Grabowska M.M., Miller N.L. NF-kappaB and androgen receptor variant expression correlate with human BPH progression. Prostate. 2016;76:491–511. doi: 10.1002/pros.23140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Austin D.C., Strand D.W., Love H.L., Franco O.E., Grabowska M.M., Miller N.L. NF-kappaB and androgen receptor variant 7 induce expression of SRD5A isoforms and confer 5ARI resistance. Prostate. 2016;76:1004–1018. doi: 10.1002/pros.23195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.DeGraff D.J., Grabowska M.M., Case T.C., Yu X., Herrick M.K., Hayward W.J. FOXA1 deletion in luminal epithelium causes prostatic hyperplasia and alteration of differentiated phenotype. Lab Investig. 2014;94:726–739. doi: 10.1038/labinvest.2014.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yu X., Cates J.M., Morrissey C., You C., Grabowska M.M., Zhang J. SOX2 expression in the developing, adult, as well as, diseased prostate. Prostate Cancer Prostatic Dis. 2014;17:301–309. doi: 10.1038/pcan.2014.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lai K.P., Yamashita S., Vitkus S., Shyr C.R., Yeh S., Chang C. Suppressed prostate epithelial development with impaired branching morphogenesis in mice lacking stromal fibromuscular androgen receptor. Mol Endocrinol. 2012;26:52–66. doi: 10.1210/me.2011-1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Niu Y., Altuwaijri S., Yeh S., Lai K.P., Yu S., Chuang K.H. Targeting the stromal androgen receptor in primary prostate tumors at earlier stages. Proc Natl Acad Sci U S A. 2008;105:12188–12193. doi: 10.1073/pnas.0804701105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Singh M., Jha R., Melamed J., Shapiro E., Hayward S.W., Lee P. Stromal androgen receptor in prostate development and cancer. Am J Pathol. 2014;184:2598–2607. doi: 10.1016/j.ajpath.2014.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wang Z., Tufts R., Haleem R., Cai X. Genes regulated by androgen in the rat ventral prostate. Proc Natl Acad Sci USA. 1997;94:12999–13004. doi: 10.1073/pnas.94.24.12999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bauman D.R., Steckelbroeck S., Peehl D.M., Penning T.M. Transcript profiling of the androgen signal in normal prostate, benign prostatic hyperplasia, and prostate cancer. Endocrinology. 2006;147:5806–5816. doi: 10.1210/en.2006-0627. [DOI] [PubMed] [Google Scholar]
- 112.Aaron-Brooks L.M., Sasaki T., Vickman R.E., Wei L., Franco O.E., Ji Y. Hyperglycemia and T cell infiltration are associated with stromal and epithelial prostatic hyperplasia in the nonobese diabetic mouse. Prostate. 2019;79:980–993. doi: 10.1002/pros.23809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhang B., Kwon O.J., Henry G., Malewska A., Wei X., Zhang L. Non-cell-autonomous regulation of prostate epithelial homeostasis by androgen receptor. Mol Cell. 2016;63:976–989. doi: 10.1016/j.molcel.2016.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Xu D., Wang X., Jiang C., Ruan Y., Xia S., Wang X. The androgen receptor plays different roles in macrophage-induced proliferation in prostate stromal cells between transitional and peripheral zones of benign prostatic hypertrophy. EXCLI J. 2017;16:939–948. doi: 10.17179/excli2017-335. [DOI] [PMC free article] [PubMed] [Google Scholar]