Abstract
Purpose
Resistance exercise (RE) can improve many cardiovascular disease (CVD) risk factors, but specific data on the effects on CVD events and mortality are lacking. We investigated the associations of RE with CVD and all-cause mortality, and further examined the mediation effect of body mass index between RE and CVD outcomes.
Methods
We included 12,591 participants (mean age 47 years) who received at least two clinical examinations 1987–2006. RE was assessed by a self-reported medical history questionnaire.
Results
During a mean follow-up of 5.4 and 10.5 years, 205 total CVD events (morbidity and mortality combined) and 276 all-cause deaths occurred, respectively. Compared with no RE, weekly RE frequencies of one, two, three times or total amount of 1–59 minutes were associated with approximately 40–70% decreased risk of total CVD events, independent of aerobic exercise (AE) (all p-values <0.05). However, there was no significant risk reduction for higher weekly RE of more than four times or ≥60 minutes. Similar results were observed for CVD morbidity and all-cause mortality. In the stratified analyses by AE, weekly RE of one time or 1–59 minutes was associated with lower risks of total CVD events and CVD morbidity regardless of meeting the AE guidelines. Our mediation analysis showed that RE was associated with the risk of total CVD events in two ways: RE had a direct U-shape association with CVD risk (p-value for quadratic trend <0.001) and RE indirectly lowered CVD risk by decreasing BMI.
Conclusion
Even one time or less than one hour/week of RE, independent of AE, is associated with reduced risks of CVD and all-cause mortality. BMI mediates the association of RE with total CVD events.
Keywords: resistance exercise, cardiovascular disease, mortality, body mass index, mediation analysis, aerobic exercise
Introduction
Cardiovascular disease (CVD) such as heart attack or stroke is the leading cause of death, particularly in most developed countries (1). Therefore, continuous efforts are needed to reduce CVD risk. The health benefits of physical activity (PA), primarily aerobic exercise (AE), have been well-documented from the perspective of CVD and premature mortality (2–4). However, most studies on resistance exercise (RE) have focused on bone health, physical function, and quality of life in older adults, or metabolic health outcomes such as type 2 diabetes (5–8). There is still limited research directly examining the association of RE with the risk of CVD and mortality, and studies have reported inconsistent results (9–11). Several studies have suggested favorable effects of muscular strength, as a proxy indicator of RE, on cardiovascular health and mortality (12–15, 16). However, these results can not directly inform recommendations on practical exercise. Thus, further evidence is warranted to reveal the association of RE and cardiovascular health and mortality independent of AE, as well as to inform recommendations on RE.
Obesity commonly classified using body mass index (BMI) is among the mediators in the mechanisms linking PA, focusing on AE, to cardiovascular health (17). Some individuals even including medical professionals believe that the cardiovascular benefits of exercise may be mostly from weight loss. Furthermore, to our knowledge, there is very limited study investigating the mechanism underlying the association of RE, independent of AE, with cardiovascular health. Investigating the potential mediation effect of BMI on the association between RE and CVD adjusting for other CVD risk factors provides us with important data on RE related CVD preventive strategies.
Our study aimed to investigate the associations of RE, independent of AE, with the risk of total CVD events (morbidity and mortality combined), CVD morbidity, and all-cause mortality in a large prospective cohort of adult men and women. Based on the hypothesis of the pairwise causal relationship of RE and BMI with CVD risk, we further examined the mediation effect of BMI on the associations of RE with total CVD events, CVD morbidity, and all-cause mortality through a joint modeling approach.
Methods
Study Population.
The Aerobics Center Longitudinal Study (ACLS) is a cohort study of individuals who received periodic preventive medical examinations at the Cooper Clinic in Dallas, Texas. The participants were volunteers sent by their employers, physicians, or were self-referred. They came to the Cooper Clinic periodically for preventive health examinations and for counseling on lifestyle habits including exercise, nutrition, stress management, etc. The participants are primarily non-Hispanic white (> 95%), well-educated (80% college graduates), and from middle to upper socioeconomic strata (18). In the present study, we included participants who received at least two clinical examinations between 1987 and 2006. Among 13,722 individuals, 1,131 participants were excluded due to reported myocardial infarction, stroke, or cancer at baseline. Our final sample included 12,591 participants (21% women) aged 18 to 89 years (mean age 47) at baseline. The study was annually reviewed and approved by the Cooper Institute institutional review board. Written informed consents were obtained from all participants for baseline and follow-up examinations.
Clinical Examination.
All participants received comprehensive medical examinations at baseline and follow-up visits after an overnight fast of at least 12 hours. Body mass index was calculated as weight in kilograms divided by height in meters squared. Resting blood pressure was measured according to standard procedures with a mercury sphygmomanometer. Serum samples were analyzed for glucose and total cholesterol using standardized bioassays. The assessment of hypertension, diabetes, and hypercholesterolemia were based on a history of physician diagnosis or measured phenotypes that met clinical thresholds for each condition. Age, sex, smoking status, alcohol consumption, parental history of CVD, and PA were assessed by a self-reported medical history questionnaire. Participants were classified as non-smokers or current smokers. Heavy alcohol drinker was defined as >14 alcohol drinks per week for men and more than seven for women (19). In the medical questionnaire, leisure-time aerobic and resistance exercises during the past three months were assessed as part of the medical examination. Aerobic exercise was categorized as meeting the recommended guidelines (≥500 metabolic equivalent [MET]-minutes per week, which was equivalent to 150 minutes of moderate or 75 minutes of vigorous weekly AE) or not, according to the United States (U.S) Department of Health and Human Services (DHHS) PA Guidelines (2).
Assessment of Resistance Exercise History.
Resistance exercise using either free weights or weight training machines was evaluated by weekly frequency (times/week) and average exercise time (minutes) for each session. The total weekly amount of RE was calculated by multiplying weekly frequency with the average minutes per session. Participants were classified into five categories by RE frequency of zero, one, two, three, and four or greater≥ times/week and four categories by total RE amount of 0, 1–59, 60–119, and ≥120 minutes/week for the main analyses. PA questionnaire including both resistance and aerobic exercise is available in an earlier study (20).
Assessment of End Points.
In this study, CVD morbidity was defined as an incidence of myocardial infarction or stroke, and was assessed at baseline and each follow-up examination. Mortality through December 31, 2003 was ascertained by the National Death Index. Death from CVD was identified by the International Classification of Diseases, Ninth Revision codes 390–449.9 and Tenth Revision codes I00-I78. The primary outcomes were total CVD events (development of CVD morbidity or death from CVD), development of CVD morbidity, and all-cause mortality. In the corresponding longitudinal analysis, we included all the records from baseline to the end points for the participants with event, or from baseline to the last examination through 2006 for the participants who survived (did not develop the event). In Cox regression models, the follow-up years (survival time) of participants with event were calculated from baseline to the end points. For the ones who survived, follow-up years were counted from baseline to the last examination for CVD morbidity, and for CVD and all-cause mortality, from baseline to the end year of 2003 (since mortality data is available until 2003) or the last examination through 2006, which came later.
Statistical Analysis.
We described baseline characteristics of participants by their weekly frequency and amount of RE.
A series of Cox proportional hazard models were fitted to assess the effect of weekly RE frequency (times/week) and total amount (minutes/week) on total CVD events, CVD morbidity, and all-cause mortality. Like all human activities, weekly RE and AE levels (represented by frequency or total amount) naturally vary over time. Such variations, broadly termed as measurement errors in the statistics literature (21), are known to cause estimation biases and reduced statistical power. Since the baseline RE and AE levels were subject to such measurement error, we instead used the long term RE and AE levels, measured by average frequency or average minutes/week during the follow-ups (e.g., average 3.7 times of RE measurement during 5.3 years of follow-up in total CVD events), as covariates in the Cox models. Using the average of repeated measurements as the covariate is a simple practice of regression calibration (21) and was used in a similar study (22). We classified participants according to average RE frequency and total amount in Cox models, therefore the number of participants in corresponding categories for CVD outcomes and all-cause mortality were slightly different. We fitted the following two sets Cox models to examine the associations of RE frequency and total amount with CVD events and all-cause mortality adjusting for different confounders: in model 1, the results were adjusted for baseline examination year, age, and sex; in model 2, we further adjusted for baseline smoking status, heavy alcohol drinking, BMI, parental history of CVD, meeting the AE guidelines, hypertension, diabetes, and hypercholesterolemia. To assess the effect of RE independent of AE, we further conducted stratified analysis by meeting AE guideline or not. Interactions between AE and RE categories were also tested by comparing the Cox models containing both main effects and interaction terms with models containing main effects only using likelihood ratio test.
To investigate the association between RE and BMI, we applied a linear mixed effect model, which was a standard model in longitudinal data analysis taking into account the follow-up observations. We then examined the mediation relationship among RE, BMI, and the outcomes following the standard procedures of mediation analysis proposed by Baron and Kenny (23). With total CVD events as an example, we presented causal relationships between RE and BMI, BMI and the risk of total CVD events, and RE and the risk of total CVD events (Figure 1). In the first step of mediation analysis, we ran a series of Cox models to examine the association of RE with total CVD events, with adjustment for all potential confounders excluding BMI. In the second step, we assessed the longitudinal association between RE and BMI with a linear mixed effect model. To model the variation in baseline BMI levels and temporal trend, we included subject-specific intercepts and slopes as random effects, while controlling the fixed effects of examination year, baseline age, sex, current smoking, heavy alcohol drinking, and meeting the AE guidelines. In the final step, we applied a joint model of longitudinal and survival data (24, 25) in which the longitudinal observation of BMI was modeled through a linear mixed effect model, the risk of total CVD events was fitted by a Cox proportional hazard model, and the association of these two models lied in that BMI was simultaneously a covariate for the Cox model. Since joint modeling is a relatively new approach in epidemiological research, we provide here more detailed explanations and methods to help readers, including future investigators, understand it clearly. The hazard function of total CVD events was modeled as:
| [1] |
where Mi(t) denoted the true value of BMI of the i-th subject at time t, Xi represented confounding variables including baseline examination year, age, sex, current smoking, heavy alcohol drinking, parental history of CVD, meeting the AE guidelines, hypertension, diabetes and hypercholesterolemia, and h0(t) was a baseline risk function. Parameter α indicated the effect of the underlying true BMI on the risk of total CVD events, while γ1 and γ2 quantified the direct effect of RE on total CVD events. The longitudinal model for observations of BMI was as follows:
| [2] |
where the error item , and the random intercept b0i and random slope b1i were assumed to follow a joint normal distribution with mean 0, Zi represented covariates including examination year, baseline age, sex, current smoking, heavy alcohol drinking and meeting the AE guidelines. Since β2 represented the effect of RE on BMI, αβ2 represented an indirect effect of RE on the risk of total CVD events through the Cox model. We fitted this model with a Bayesian approach. The baseline hazard function in Cox model was estimated by penalized spline, and independent univariate diffuse normal priors were assumed for fixed effect parameters in the longitudinal model, and parameters in the Cox model (26). Mediation analyses were also conducted for CVD morbidity and all-cause mortality in the same way.
FIGURE 1— Path Diagram for Mediation Association among Resistance Exercise, Body Mass Index, and Total CVD Events.
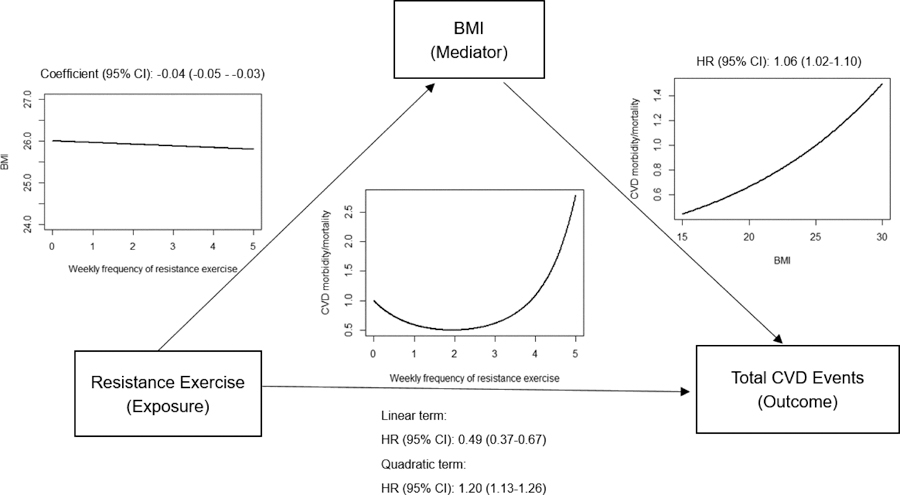
This figure depicts result of a joint model with total CVD events as outcome. The solid arrows represent significant effect. The relationship curves and hazard ratios (coefficients) and 95% confidence intervals were positioned above or under the arrows.
Based on no significant interactions by sex on the associations between RE and the outcomes using interaction terms in the regression and by comparing risk estimates in the sex-stratified analyses, pooled analyses including both men and women were performed. Also, the proportional hazard assumptions were confirmed by Schoenfeld tests (27). All statistical analyses were conducted using R version 3.3.2. R package “JMbayes” was applied for joint modeling analysis and 2-sided p-values <0.05 were deemed significant.
Results
Among 12,591 participants, 205 total CVD events, 127 CVD morbidity (nonfatal CVD events), and 276 all-cause deaths occurred during an average follow-up of 5.4, 5.3 and 10.5 years. Table 1 shows baseline characteristics of participants according to their frequency of RE (supplemental Table S1 shows baseline characteristics by amount of RE). At baseline, 3,438 individuals (27%) engaged in some RE in this population. Compared with non-participants of RE, the participants of RE tend to be male, younger, non-smokers, more aerobically active, and with lower BMI. They also had a lower rate of hypertension, diabetes, hypercholesterolemia, and history of parental CVD.
TABLE 1.
Baseline Characteristics by Weekly Frequency of Resistance Exercise
| Weekly Frequency of Resistance Exercise (times/week) |
|||||
|---|---|---|---|---|---|
| Baseline Characteristics | 0 (n=9,153) |
1 (n=258) |
2 (n=902) |
3 (n=1,534) |
≥4 (n=744) |
| Female | 1,891 (20.7) | 42 (16.3) | 235 (26.1) | 304 (19.8) | 138 (18.5) |
| Age (year) | 47.0 ± 9.7 | 44.0 ± 8.1 | 44.8 ± 8.5 | 45.7 ± 8.9 | 45.5 ± 10.3 |
| Heavy alcohol drinkera | 1,082 (11.8) | 32 (12.4) | 117 (13.0) | 176 (11.5) | 91 (12.2) |
| Current smoker | 1,101 (12) | 28 (10.9) | 91 (10.1) | 139 (9.1) | 83 (11.2) |
| Parental CVD | 2,451 (26.8) | 58 (22.5) | 207 (22.9) | 393 (25.6) | 178 (23.9) |
| Meeting aerobic exercise guidelinesb | 4,589 (50.1) | 185 (71.7) | 727 (80.6) | 1,245 (81.2) | 630 (84.7) |
| Body mass index (kg/m2)c | 26.3 ± 4.2 | 25.7 ± 3.4 | 25.2 ± 3.7 | 25.5 ± 3.6 | 25.2 ± 3.6 |
| Hypertensiond | 2,723 (29.7) | 55 (21.3) | 212 (23.5) | 394 (25.7) | 182 (24.5) |
| Diabetese | 398 (4.3) | 11 (4.2) | 30 (3.3) | 49 (3.2) | 20 (2.7) |
| Hypercholesterolemiaf | 2,986 (32.6) | 65 (25.2) | 245 (27.2) | 399 (26.0) | 156 (21.0) |
Values are number (%) or mean ± SD.
Defined as alcohol drinks >14 and >7 per week for men and women, respectively.
Defined as aerobic exercise ≥500 MET-minutes per week.
Calculated as the weight in kilograms divided by the square of the height in meters.
Defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or previous diagnosis by a physician.
Defined as fasting glucose ≥126 mg/dl, previous diagnosis by a physician, or insulin use.
Defined as total cholesterol ≥240 mg/dl, or previous diagnosis by a physician.
CVD, cardiovascular disease; SD, standard deviation.
Compared with no RE, hazard ratios (HRs) (95% confidence intervals [CIs]) of total CVD events across weekly RE frequencies of one, two, three, and four or greater times were 0.26 (0.16 to 0.42), 0.41 (0.27 to 0.63), 0.52 (0.31 to 0.86), and 1.17 (0.67 to 2.04), respectively, after adjusting for examination year, age, and sex in Model 1 (Table 2). The HRs (95% CIs) of total CVD events across weekly total RE amount of 1–59, 60–119, and ≥120 minutes were 0.33 (0.23–0.47), 0.57 (0.36–0.91), and 0.81 (0.46–1.44), respectively, in the same Model 1. These associations were slightly attenuated, but mostly remained significant after additional adjustment for potential confounders including meeting the AE guidelines and health conditions in the full Model 2. When assessed as a continuous variable, weekly RE frequency had a U-shape association with total CVD events (p-value for quadratic trend <0.001), which reached the lowest HR (95% CI) of 0.51 (0.35 to 0.68) at about two times/week (Figure 2(a)). We observed similar trend for the total amount of weekly RE, with the lowest HR at 1.5 hours/week (Figure 2 (b)) although not significant. For CVD morbidity, we observed reduced risk of adverse events for RE frequency of one, two times/week and total amount of 1–59 minutes/week compared with no RE, after adjusting for all potential confounders. For all-cause mortality, decreased risk was observed for RE frequency of one times/week and total amount of 1–59 minutes/week. In the dose-response analysis, the association of RE frequency with both CVD morbidity and all-cause mortality showed a U-shape curve, with the lowest risk achieved at RE frequency of two times/week (Figure 2 (c) and (e)). However, quadratic trends for the associations of total RE amount with CVD morbidity and all-cause mortality were not significant (p-values were 0.21 and 0.75 respectively). When we used the baseline values of RE frequency and amount in further sensitivity analyses, we did not observe significant results after adjusting for all potential confounders (data not shown). Therefore, it is possible that the risks of CVD and all-cause mortality were associated with long-term RE, rather than one time baseline value of RE, which has significant measurement errors because people in general over-report their physical activity. When we excluded those early cases of CVD events and all-cause mortality within the first two years of follow-up to reduce potential subclinical conditions on the associations of RE with outcomes and minimize possible reverse causation, we found similar results (data not shown).
TABLE 2.
Hazard Ratio (95% CI) of Total CVD Events, CVD Morbidity, and All-Cause Mortality by Resistance Exercise
| Total CVD Events | CVD Morbidity | All-Cause Mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of Events / No. of Participants | HR (95% CI) |
No. of Events / No. of Participants | HR (95% CI) |
No. of Events / No. of Participants | HR (95% CI) |
||||
| Model 1a | Model 2b | Model 1a | Model 2b | Model 1a | Model 2b | ||||
| Weekly Frequency of Resistance Exercise (times/week) | |||||||||
| 0 | 127/5,955 | 1.00 (Reference) |
1.00 (Reference) |
74/5,955 | 1.00 (Reference) |
1.00 (Reference) |
184/5,925 | 1.00 (Reference) |
1.00 (Reference) |
| 1 | 20/2,216 | 0.26 (0.16–0.42) |
0.28 (0.17–0.46) |
13/2,216 | 0.32 (0.18–0.58) |
0.35 (0.19–0.63) |
30/2,236 | 0.62 (0.42–0.91) |
0.65 (0.44–0.97) |
| 2 | 27/2,385 | 0.41 (0.27–0.63) |
0.46 (0.29–0.70) |
19/2,385 | 0.52 (0.31–0.86) |
0.58 (0.34–0.98) |
30/2,398 | 0.65 (0.44–0.95) |
0.68 (0.46–1.01) |
| 3 | 17/1,407 | 0.52 (0.31–0.86) |
0.57 (0.33–0.96) |
12/1,407 | 0.64 (0.34–1.17) |
0.72 (0.38–1.36) |
17/1,407 | 0.62 (0.38–1.02) |
0.67 (0.40–1.11) |
| ≥4 | 14/628 | 1.17 (0.67–2.04) |
1.33 (0.75–2.36) |
9/628 | 1.27 (0.63–2.53) |
1.52 (0.74–3.11) |
15/625 | 1.09 (0.64–1.84) |
1.29 (0.75–2.20) |
| p-value for Linear Trend: | |||||||||
| 0.15 | 0.73 | 0.50 | 0.84 | 0.46 | 0.96 | ||||
| p-value for Quadratic Trend: | |||||||||
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| Weekly Minutes of Resistance Exercise (minutes/week) | |||||||||
| 0 | 127/5,955 | 1.00 (Reference) |
1.00 (Reference) |
74/5,955 | 1.00 (Reference) |
1.00 (Reference) |
184/5,925 | 1.00 (Reference) |
1.00 (Reference) |
| 1–59 | 44/3,764 | 0.33 (0.23–0.47) |
0.35 (0.24–0.51) |
31/3,764 | 0.44 (0.29–0.68) |
0.57 (0.30–0.74) |
57/3,786 | 0.61 (0.45–0.82) |
0.64 (0.47–0.88) |
| 60–119 | 21/1,910 | 0.57 (0.36–0.91) |
0.63 (0.39–1.03) |
14/1,910 | 0.61 (0.34–1.09) |
0.69 (0.38–1.25) |
21/1,916 | 0.78 (0.49–1.23) |
0.84 (0.53–1.34) |
| ≥120 | 13/962 | 0.81 (0.46–1.44) |
0.93 (0.51–1.68) |
8/962 | 0.81 (0.39–1.69) |
0.96 (0.45–2.05) |
14/964 | 0.92 (0.53–1.58) |
1.03 (0.59–1.80) |
| p-value for Linear Trend: | |||||||||
| 0.62 | 0.56 | 0.83 | 0.28 | 0.28 | 0.65 | ||||
| p-value for Quadratic Trend: | |||||||||
| 0.002 | 0.02 | 0.049 | 0.21 | 0.48 | 0.75 | ||||
Model 1 was adjusted for baseline examination year, age (years) and sex.
Model 2 was adjusted for Model 1 plus baseline smoking status (current smoker or not), alcohol consumption (heavy drinker or not),parental history of cardiovascular disease (yes or no), body mass index (kg/m2), aerobic exercise (average physical activity ≥500 MET- minutes/week or not), hypertension (yes or no), diabetes (yes or no), and hypercholesterolemia (yes or no).
CI, confidence interval; CVD, cardiovascular diseases; HR, hazard ratio.
FIGURE 2— The Dose-response Relationship between Resistance Exercise and Risk of Total CVD Events, CVD Morbidity, and All-Cause Mortality.
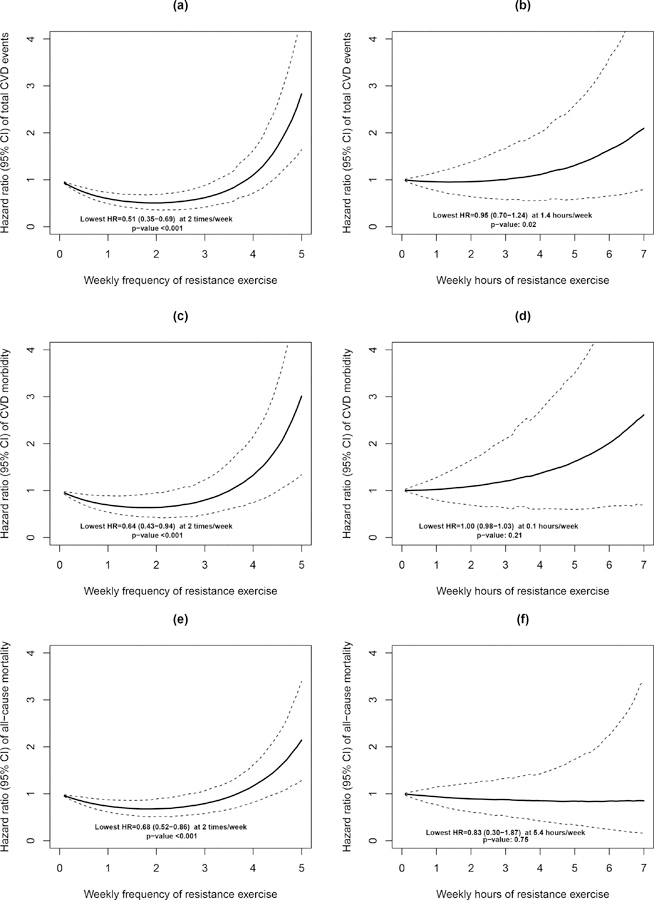
Dotted lines represent 95% confidence intervals for the hazard ratios. Quadratic trend p value is presented in each figure. Models were adjusted for baseline examination year, age (years), sex, baseline smoking status (current smoker or not), alcohol consumption (heavy drinker or not), parental history of cardiovascular disease (yes or no), body mass index (kg/m2), aerobic exercise (average physical activity ≥500 MET-minutes/week or not), hypertension (yes or no), diabetes (yes or no), and hypercholesterolemia (yes or no). Figure (a), (c) and (e) shows significant U-shape associations between weekly frequency of resistance exercise with three outcomes. The lowest risk of CVD and all-cause mortality is attained at resistance exercise of two times/week. Figure (b) shows significant quadratic association between weekly hours of resistance exercise with risk of total CVD events. Figure (d) and (e) shows weekly hours of resistance exercise has no significant quadratic association with risk of CVD morbidity and all-cause mortality.
To assess the effects of RE on the risks of CVD and all-cause mortality independent of AE, stratified analyses were conducted by meeting the recommended AE guidelines or not (supplemental Table S2). Compared with no RE, RE frequency of one time/week and the total amount of 1–59 minutes/week were associated with 75% (HR: 0.25, 95% CI: 0.14 to 0.46) and 60% (HR: 0.40, 95% CI: 0.21 to 0.52) lower risk of total CVD events, respectively, among the ones meeting AE guidelines, and 65% (HR: 0.35, 95% CI: 0.16 to 0.77) and 59% (HR: 0.41, 95% CI: 0.23 to 0.74) lower risk of total CVD events, respectively, among those not meeting AE guidelines. We also observed similar results for CVD morbidity with significantly reduced risks in one time/week of RE frequency and the total amount of 1–59 minutes/week of RE regardless of meeting AE guidelines.. Compared with no RE, engaging in RE of one, two, or three times/week and 1–59 minutes/week was associated with decreased risk of all-cause mortality among participants meeting recommended AE. However, we did not observe significant all-cause mortality risk reduction with doing RE in the group of not meeting AE guidelines. These stratified analyses suggest that one could get CVD benefits from RE whether they meet the AE guidelines or not. However, all-cause mortality benefits from RE is only obtained when they meet the recommended AE (p-values for the interaction between RE and AE for all-cause mortality were 0.06 and 0.04 for RE frequency and amount, respectively).
Before testing the mediation effect of BMI between RE and CVD, we investigated the longitudinal association of RE with BMI in additional analyses. When taken as continuous variable, weekly frequency and total amount of RE were significantly associated with BMI after adjusting for all potential confounders including AE (p-value <0.001). Participants who did any RE would have a 0.13 (SE: 0.017) kg/m2 lower level of BMI compared with the ones with no RE. We then examined the mediation associations among RE, BMI, and total CVD events, CVD morbidity, and all-cause mortality by a joint modeling approach (Table 3). For the risk of total CVD events, in the longitudinal model, weekly frequency of RE was inversely associated with BMI (coefficient: −0.04; 95% CI: −0.05 to −0.03 in each RE frequency); in the Cox model, higher BMI was associated with a higher risk of total CVD events (HR: 1.06; 95% CI: 1.02 to 1.10 in each BMI unit), and RE frequency had a U-shape association with the risk of total CVD events (p-value for quadratic trend <0.001 between each RE frequency and total CVD events). Based on this joint modeling result, we found that RE frequency was associated with the reduced risk of total CVD events in two ways: RE had a U-shape association with the risk of total CVD events. On the other hand, RE also lowered the risk of total CVD events through decreasing BMI, which is depicted in Figure 1. However, the mediation effects of BMI were relatively weaker on the associations of RE frequency with CVD morbidity (HR: 1.04; 95% CI: 0.99–1.09) and all-cause mortality (HR: 1.03; 95% CI: 0.996–1.07). For the total amount of RE (weekly hours), we did not observe significant associations between weekly hours of RE and three outcomes in Cox model part. The inverse association between RE hours and BMI in the longitudinal model, combining with the significant effect of BMI on risk of total CVD event and all-cause mortality in Cox model, implies that RE hours lowers the risk of total CVD event and all-cause mortality indirectly through BMI.
TABLE 3.
Regression Coefficients (95% CI) and Hazard Ratios (95% CI) of Total CVD Events, CVD Morbidity, and All-Cause Mortality by Resistance Exercise with BMI in Joint Model
| Total CVD Events | CVD Morbidity | All-Cause Mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (95% CI) | HR (95% CI) | p-value | Coefficient (95% CI) | HR (95% CI) | p-value | Coefficient (95% CI) | HR (95% CI) | p-value | |
| Linear Mixed Effect Model (BMI as Outcome)a | |||||||||
| Weekly Frequency of Resistance exercise | −0.04 (−0.05 – −0.03) |
<0.001 | −0.04 (−0.05 – −0.03) |
<0.001 | −0.04 (−0.05 – −0.03) |
<0.001 | |||
| Cox Model (Total CVD Events, CVD Morbidity, and All-Cause Mortality as Outcome)b | |||||||||
| Weekly Frequency of Resistance Exercise | |||||||||
| Linear Term | 0.49 (0.37–0.67) |
<0.001 | 0.64 (0.48–0.89) |
0.01 | 0.66 (0.52–0.86) |
<0.001 | |||
| Quadratic Term | 1.20 (1.13–1.26) |
<0.001 | 1.15 (1.07–1.22) |
<0.001 | 1.12 (1.05–1.18) |
<0.001 | |||
| BMI | 1.06 (1.02–1.10) |
0.002 | 1.04 (0.99–1.09) |
0.09 | 1.03 (0.996–1.07) |
0.08 | |||
| Linear Mixed Effect Model (BMI as Outcome)a | |||||||||
| Weekly Hours of Resistance exercise | −0.05 (−0.06 – −0.03) |
<0.001 | −0.04 (−0.06 – −0.03) |
<0.001 | −0.05 (−0.06 – −0.03) |
<0.001 | |||
| Cox Model (Total CVD Events, CVD Morbidity, and All-Cause Mortality as Outcome)b | |||||||||
| Weekly Hours of Resistance Exercise | |||||||||
| Linear Term | 0.92 (0.73–1.18) |
0.54 | 1.04 (0.68–1.51) |
0.78 | 1.03 (0.76–1.40) |
0.88 | |||
| Quadratic Term | 1.02 (0.99–1.04) |
0.14 | 1.01 (0.97–1.04) |
0.60 | 0.97 (0.90–1.03) |
0.52 | |||
| BMI | 1.07 (1.03–1.11) |
0.002 | 1.04 (0.99–1.09) |
0.09 | 1.05 (1.02–1.09) |
0.005 | |||
The first part of this table shows the result of joint model for weekly frequency of resistance exercise, and the second part shows result for weekly hours of resistance exercise.
The linear mixed effect model part was adjusted for follow-up years, examination year, baseline age (years), sex, current smoking (yes or no), heavy alcohol drinking (yes or no), and meeting the aerobic exercise guidelines (yes or no).
The Cox model part was adjusted for baseline examine year, age (years), sex, current smoking (yes or no), heavy alcohol drinking (yes or no), parental history of cardiovascular disease (yes or no), meeting the aerobic exercise guidelines (yes or no), hypertension (yes or no), diabetes (yes or no), and hypercholesterolemia (yes or no).
BMI, body mass index; CI, confidence interval; CVD, cardiovascular diseases; HR, hazard ratio.
Discussion
In this study, we found that RE, especially low-to-moderate frequency (one-three times/week) or even <one hour/week, was associated with lower risks of total CVD events, independent of AE, compared with no RE, in a large cohort of men and women (mean age: 46.5 years, range: 18–96). In addition, higher RE frequency of ≥four times/week and amount of ≥120 minutes/week did not show significant cardiovascular benefits. These results are consistent with the findings of the U-shaped associations between RE and CVD events from the dose-response analyses using the continuous variables of weekly RE frequency and amount (Figure 2 (a) and (b)). For the associations of RE with CVD morbidity and all-cause mortality, the results of the dose-response analyses were similar although less strong. Previous studies have shown mixed results regarding the association between RE and CVD risk. In the Women’s Health Study, Kamada et al. (22) also found that strength training for 1–59 minutes/week was associated with lower risk of CVD mortality (including death from myocardial infarction, stroke, angioplasty, and coronary artery bypass grafting), compared with no strength training, for a cohort of middle aged and older women. They also observed significant quadratic associations between amount of weekly RE with CVD mortality and all-cause mortality. For the same study, another research showed that strength training for 60–120 minutes/week was associated with significant risk reduction of CVD events, and no further significant benefits was observed for strength training of >120 minutes/week (9). Although not tested statistically, the results implied the quadratic association as similar with the current findings. In this study, they also observed a 17% risk reduction for CVD events among women engaging in strength training, compared with the ones who reported no strength training. In our study, the corresponding reduction of risk was 55% (HR: 0.45; 95% CI: 0.33 to 0.61). The possible explanations of the higher total CVD risk reduction in our study would be related to the facts that our study includes both men and women who are also younger (mean age: 46.5 years, range: 18–96) than the participants in the Women’s Health Study (mean age: 62.6 years, range: 47–98). It is noteworthy that results in the last research were not adjusted for CVD risk factors including hypertension, diabetes and hypercholesterolemia. In a cohort of middle aged and older men from the Health Professionals’ Follow-Up Study, Tanasescu et al.(10) found that weight training for at least 30 minutes per week was associated with a 23% risk reduction of coronary heart disease compared with no weight training after adjusting for potential confounders excluding baseline diabetes, high cholesterol levels, and hypertension. However, in another report from the same study with higher amounts of weight training categories, they found an U-shaped association between weight training and total CVD events (fatal and nonfatal myocardial infarction and stroke) with significant benefits below 120 minutes/week, but no further benefits in ≥120 minutes/week of weight training (11).
There has been compelling evidence that RE prevents decline in skeletal muscle mass (28), and long-term participation in RE increases energy expenditure (29, 30), and relieves anxiety, depression, and insomnia in clinical depression (31). It was also shown that RE had beneficial effects on cardiovascular risk factors including obesity, diabetes, hypertension, hypercholesterolemia, and decreased physical function (5–8, 32–36). We observed a significant U-shaped association between RE and CVD risk after adjusting for BMI, diabetes mellitus, hypertension and hypercholesterolemia. Possible explanations for the CVD benefits from low-to-moderate RE might include improved physical function, increased energy expenditure, and emotional factors as mentioned above. Although there is no clear understanding why there is no further cardiovascular benefits in the higher amounts of RE, a meta-analysis suggested that high intensity RE may increase arterial stiffness leading to subsequent CVD events (37). A significant pressure load is imposed on the heart during RE, and heavy RE may lead to a mild form of cardiac hypertrophy (38). In addition, a marked rise in blood pressure is secondary to RE, thus high level of RE may have adverse effect on those with uncontrolled hypertension (6, 39). Another possible explanation of no further cardiovascular benefits in the higher amounts of RE would be that the room for benefits could be much smaller for those participants in the higher amounts of RE (≥four times/week) in which 85% of them met the AE guidelines compared with those doing one time/week of RE in which 72% of them met the AE guidelines. However, further investigations are clearly needed on this controversial issue of the dose-response relationship between RE and CVD risk.
We also confirmed that BMI was a mediator in the relationship of RE with total CVD events. Several studies in the literature took BMI into account as a potential mediator in the relationship of PA and CVD risk. Erez et al. (40) indicated that BMI was among the CVD risk factors affecting the association of cardiorespiratory fitness and CVD morbidity. The Women’s Health Study reported that BMI contributed 10% of the observed inverse association between PA and risk of CVD events (17). The previous research mostly focused on associations between baseline cardiorespiratory fitness (baseline PA), baseline observations of CVD risk factors, and subsequent CVD outcomes (17, 40, 41). Mora et al. showed no significant association existed between baseline PA and risk of CVD after adjusting for baseline levels of known risk factors. However, Kamada et al. (22) revealed a quadratic association between cumulative-averaged amount of strength training and mortality of CVD after adjusting for baseline CVD risk factors. In the current study, we considered the associations between long-term RE, longitudinal observation of BMI, and risk of CVD events in mediation analysis, and the result showed that weekly RE frequency had a U-shape relationship with risk of CVD events (lowest risk attained at two times/week, not shown) after adjusting for AE, longitudinal observation of BMI, and other potential confounders. The result implies that one would get CVD benefits from RE regardless of the long-term levels of BMI. On the other hand, the result seems more convincible including the baseline as well as the dynamic information of variables into mediation analysis.
Strengths of this study include the large sample size across a wide age-range, extensive CVD morbidity and mortality follow-up, and repeated measures of exposures. In addition, we proposed the application of a joint modeling approach in mediation analysis to more rigorously investigate the effect of BMI on the association between RE and the risks of CVD as well as all-cause mortality.
Study Limitations.
There are several limitations in this study. We used self-reported AE and RE in the current study, and people tend to over-report their leisure-time exercise, especially RE possibly more in men (e.g., a competitive, bragging culture in weight lifting). Therefore, this overestimation of self-reported RE may have induced possible underestimation of the true health effects of RE on BMI, CVD, and mortality outcomes. For example, the possible explanation of the weaker associations between the total amount of RE (total weekly hours) and all three outcomes may be related to the additive over-reporting of RE because total weekly hours of RE were calculated by multiplying self-reported weekly frequency of RE with self-reported average exercise time (minutes) per session. However, to our knowledge, this is the first comprehensive study investigating the independent associations among RE, BMI, and CVD morbidity and mortality in both men and women in a large cohort study. Furthermore, intensity of AE and RE were not evaluated in this study. Therefore, more studies on the effects of different intensity of RE on cardiovascular health is clearly warranted. In addition, we assumed causal associations for this observational study. However, it is possible that healthier individuals were more likely to participate in RE who are less likely to develop CVD and die prematurely, which refers to a possible reverse causality. Therefore, further studies with objective measurement of RE and a large randomized clinical trials of RE training are clearly warranted to examine the causal effects of RE on the risk of developing CVD and mortality as well as to confirm the U-shaped dose-response association between RE and CVD risk.
Conclusion
This study suggests that low-to-moderate frequency and amount of RE is associated with reduced risk of nonfatal CVD events, total CVD events, and all-cause mortality independent of AE, and high frequency and amount of RE did not show significant cardiovascular benefits. A mediation association exists among RE, BMI, and the risks of total CVD events, showing that RE has a direct U-shape association with the risk of total CVD events, and RE also decreases the risk of CVD events indirectly by lowering BMI. These results have potential public health applications, especially for the prevention of CVD, as RE is needed in addition to AE to maximize CVD prevention.
Supplementary Material
Acknowledgements
We thank the Cooper Clinic physicians and technicians for collecting the data and staff at the Cooper Institute for data entry and data management.
This study was supported by the National Institutes of Health grants (AG06945, HL62508, DK088195, and HL133069). Steven N. Blair has received unrestricted research grants from The Coca-Cola Company, but the grants were not used to support this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest
The authors report no conflicts of interest. The results of the study are presented clearly, honestly, without fabrication, falsification, or inappropriate data manipulation, and do not constitute endorsement by the American College of Sports Medicine.
References
- 1.Mendis S, Puska P, Norrving B. Global atlas on cardiovascular disease prevention and control. World Health Organization; 2011. [Google Scholar]
- 2.US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008. Available at: http://health.gov/PAGuidelines. Accessed December 1, 2017.
- 3.Lee DC, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol. 2014;64(5):472–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lavie CJ, Arena R, Swift DL, et al. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circulation research. 2015;117(2):207–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams MA, Haskell WL, Ades PA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update. Circulation. 2007;116(5): 572–584. [DOI] [PubMed] [Google Scholar]
- 6.Braith RW, Stewart KJ. Resistance exercise training. Circulation. 2006;113(22):2642–2650. [DOI] [PubMed] [Google Scholar]
- 7.Grøntved A, Pan A, Mekary RA, et al. Muscle-strengthening and conditioning activities and risk of type 2 diabetes: a prospective study in two cohorts of US women. PLoS medicine. 2014;11(1):e1001587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Church TS, Blair SN, Cocreham S, et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2010;304(20):2253–2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shiroma EJ, Cook NR, Manson JE, et al. Strength Training and the Risk of Type 2 Diabetes and Cardiovascular Disease. Medicine and science in sports and exercise. 2017;49(1):40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tanasescu M, Leitzmann MF, Rimm EB, et al. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288(16):1994–2000. [DOI] [PubMed] [Google Scholar]
- 11.Chomistek AK, Cook NR, Flint AJ, et al. Vigorous-intensity leisure-time physical activity and risk of major chronic disease in men. Medicine and science in sports and exercise. 2012;44(10):1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawman HG, Troiano RP, Perna FM, et al. Associations of relative handgrip strength and cardiovascular disease biomarkers in US adults, 2011–2012. American journal of preventive medicine. 2016;50(6):677–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruiz JR, Sui X, Lobelo F, et al. Association between muscular strength and mortality in men: prospective cohort study. Bmj. 2008;337:a439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leong DP, Teo KK, Rangarajan S, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. The Lancet. 2015;386(9990):266–273. [DOI] [PubMed] [Google Scholar]
- 15.Gale CR, Martyn CN, Cooper C, et al. Grip strength, body composition, and mortality. International journal of epidemiology. 2007;36(1):228. [DOI] [PubMed] [Google Scholar]
- 16.Artero EG, Lee D, Lavie CJ, et al. Effects of muscular strength on cardiovascular risk factors and prognosis. Journal of cardiopulmonary rehabilitation and prevention. 2012;32(6):351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mora S, Cook N, Buring JE, Ridker PM, Lee IM. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation. 2007;116(19):2110–2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blair SN, Kannel WB, Kohl HW, et al. Surrogate measures of physical activity and physical fitness: evidence for sedentary traits of resting tachycardia, obesity, and low vital capacity. American journal of epidemiology. 1989;129(6):1145–1156. [DOI] [PubMed] [Google Scholar]
- 19.National Institute on Alcohol Abuse and Alcoholism. Alcohol use and alcohol use disorders in the United States: Main findings from the 2001–2002 National Epidemiologic survey on alcohol and related conditions (NESARC). NIH Publication No. 05–5737 2006.
- 20.Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, Utter AC, Zmuda JM. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 Suppl):S1–205. [PubMed] [Google Scholar]
- 21.Carroll RJ, Ruppert D, Stefanski LA, et al. Measurement error in nonlinear models: a modern perspective. CRC press; 2006. 71 p. [Google Scholar]
- 22.Kamada M, Shiroma EJ, Buring JE, et al. Strength Training and All‐Cause, Cardiovascular Disease, and Cancer Mortality in Older Women: A Cohort Study. Journal of the American Heart Association. 2017;6(11):e007677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173. [DOI] [PubMed] [Google Scholar]
- 24.Rizopoulos D Joint models for longitudinal and time-to-event data: With applications in R. CRC Press; 2012. p. 51–56. [Google Scholar]
- 25.Rizopoulos D Dynamic predictions and prospective accuracy in joint models for longitudinal and time‐to‐event data. Biometrics. 2011;67(3): 819–829. [DOI] [PubMed] [Google Scholar]
- 26.Rizopoulos D The R package JMbayes for fitting joint models for longitudinal and time-to-event data using MCMC. Journal of Statistical Software. 2016;72(7):1–45. [Google Scholar]
- 27.Schoenfeld D Partial residuals for the proportional hazards regression model. Biometrika. 1982;69(1):239–241. [Google Scholar]
- 28.American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. [DOI] [PubMed] [Google Scholar]
- 29.Nelson ME, Fiatarone MA, Morganti CM, Trice I, Greenberg RA, Evans WJ. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures: a randomized controlled trial. JAMA. 1994;272:1909–1914. [DOI] [PubMed] [Google Scholar]
- 30.Vincent KR, Braith RW, Feldman RA, Kallas HE, Lowenthal DT. Improved cardiorespiratory endurance following 6 months of resistance exercise in elderly men and women. Arch Intern Med. 2002;162: 673–678. [DOI] [PubMed] [Google Scholar]
- 31.Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of progressive resistance training in depressed elders. J Gerontol A Biol Sci Med Sci. 1997;52: M27–M35. [DOI] [PubMed] [Google Scholar]
- 32.Cornelissen VA, Fagard RH, Coeckelberghs E, et al. Impact of resistance training on blood pressure and other cardiovascular risk factors. Hypertension. 2011; HYPERTENSIONAHA: 111.177071. [DOI] [PubMed]
- 33.Strasser B, Siebert U, Schobersberger W. Resistance training in the treatment of the metabolic syndrome. Sports medicine. 2010;40(5):397–415. [DOI] [PubMed] [Google Scholar]
- 34.Bakker EA, Lee D, Sui X, et al. Association of resistance exercise, independent of and combined with aerobic exercise, with the incidence of metabolic syndrome. Mayo Clinic Proceedings. 2017;92(8):1214–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bakker EA, Lee D, Sui X, et al. Association of resistance exercise with the incidence of hypercholesterolemia in men. Mayo Clinic Proceedings. 2018;93(4);419–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mann S, Beedie C, Jimenez A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports Medicine. 2014;44(2):211–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miyachi M Effects of resistance training on arterial stiffness: a meta-analysis. Br J Sports Med. 2013;47(6):393–396. [DOI] [PubMed] [Google Scholar]
- 38.Longhurst JC, Stebbins CL. The power athlete. Cardiol Clin. 1997;15: 413–429. [DOI] [PubMed] [Google Scholar]
- 39.McKelvie RS, McCartney N, Tomlinson C, Bauer R, MacDougall JD. Comparison of hemodynamic responses to cycling and resistance exercise in congestive heart failure secondary to ischemic cardiomyopathy. Am J Cardiol. 1995;76: 977–979 [DOI] [PubMed] [Google Scholar]
- 40.Erez A, Kivity S, Berkovitch A, et al. The association between cardiorespiratory fitness and cardiovascular risk may be modulated by known cardiovascular risk factors. American Heart Journal. 2015;169(6):916–923.e1. [DOI] [PubMed] [Google Scholar]
- 41.Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, Utter AC, Zmuda JM. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 Suppl):S1–205. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


