Abstract
BACKGROUND
Some patients with hepatolithiasis cannot tolerate surgery due to severe cardiac or pulmonary comorbidities, or cannot be endoscopically treated because of altered gastrointestinal anatomies.
AIM
To propose a modified percutaneous transhepatic papillary balloon dilation procedure, and evaluate the clinical efficacy and safety of this modality.
METHODS
Data from 21 consecutive patients who underwent modified percutaneous transhepatic papillary balloon dilation with hepatolithiasis were retrospectively analyzed. Using auxiliary devices, intrahepatic bile duct stones were pushed into the common bile duct and expelled into the duodenum with an inflated balloon catheter. The outcomes recorded included success rate, procedure time, hospital stay, causes of failure, and procedure-related complications. Patients with possible long-term complications were followed up for 2 years.
RESULTS
Intrahepatic bile duct stones were successfully removed in 20 (95.23%) patients. Mean procedure time was 65.8 ± 5.3 min. Mean hospital stay was 10.7 ± 1.5 d. No pancreatitis, gastrointestinal, or biliary duct perforation was observed. All patients were followed up for 2 years, and there was no evidence of reflux cholangitis or calculi recurrence.
CONCLUSION
Modified percutaneous transhepatic papillary balloon dilation was feasible and safe with a small number of patients with hepatolithiasis, and may be a treatment option in patients with severe comorbidities or in patients in whom endoscopic procedure was not successful.
Keywords: Intrahepatic cholestasis, Sphincter of Oddi, Dilation, Common bile duct, Percutaneous, Balloon
Core tip: Some patients with hepatolithiasis cannot tolerate surgery due to severe cardiac or pulmonary comorbidities, or cannot be endoscopically treated because of altered gastrointestinal anatomies. For these patients, modified percutaneous transhepatic papillary balloon dilation, providing a path with compliance and only requiring intravenous anesthesia, should be considered as a treatment option, especially when the endoscopic procedure is not successful.
INTRODUCTION
Hepatolithiasis is defined as the presence of gall stones in the bile duct peripheral to the confluence of the right and left hepatic duct. It is a benign disease, but with a poor prognosis due to possible complications including recurrent intrahepatic stones, secondary common bile duct (CBD) stones, biliary strictures, recurrent cholangitis, biliary cirrhosis, liver atrophy, and intrahepatic cholangiocarcinoma[1,2].
Hepatolithiasis is present with the coexistence of choledocholithiasis or cholecystolithiasis in 70% of patients. This disease is prevalent in Eastern Asia[3-7], but rare in Western countries[8]. However, population migration has resulted in the increased prevalence in the West[9]. Several factors are related to hepatolithiasis including parasitic infestation[10], bacterial infection[11], bile stasis, diet and anatomy[12].
As one of the most complex cholelithiasis, the treatment is complicated and difficult requiring a team including interventional radiologist, gastroenterologist and surgeons, and has improved due to advanced technologies. The combined approach is percutaneous, endoscopic, and surgical[13].
Based on our previous experience, for certain groups of elderly patients suffering from CBD stones with previous gastrointestinal surgery, gastrointestinal anatomical abnormalities, esophageal and gastric varices, severe cardiac or pulmonary comorbidities, endoscopic procedures or surgery may be difficult to perform, and percutaneous transhepatic papillary balloon dilation (PTPBD) could be an alternative[14,15]. We evaluated the clinical efficacy and safety of a modified PTPBD for the removal of intrahepatic bile duct stones in patients with severe comorbidities, especially when endoscopic retrograde cholangio-pancreatography (ERCP) was not successful.
MATERIALS AND METHODS
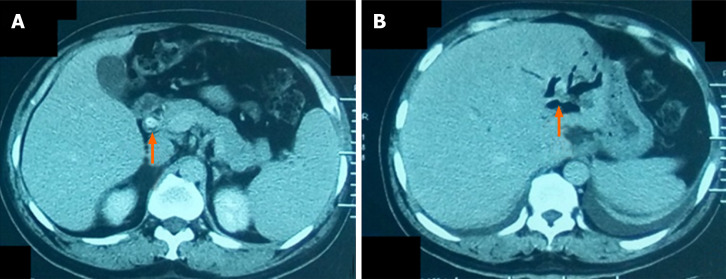
From February 2014 to June 2015, 21 patients admitted with hepatolithiasis (16 cases with concomitant CBD stones) diagnosed by ultrasonography, computed tomography (CT) or magnetic resonance cholangiopancreatography (MRCP) (Figure 1) were enrolled and underwent modified PTPBD. This retrospective study was approved by the ethics committee and all patients provided written informed consent.
Figure 1.
A 58-yr-old man with common bile duct stone and intrahepatic bile duct stone. A: Computed tomography after contrast administration of the common bile duct stone (arrow); B: Computed tomography without contrast of the intrahepatic bile duct stone (arrow).
Laboratory values, including white blood cell (WBC) count, total bilirubin (TBIL), direct bilirubin (DBIL), aspartate aminotransferase (AST), albumin (ALB), and amylase were obtained using routine laboratory tests.
Inclusion criteria included: (1) Intrahepatic stones in the right or left hepatic duct with symptoms of obstructive jaundice, pain, or fever; (2) Intolerance of endotracheal anesthesia; (3) Inability to tolerate or refuse to undergo open surgical, laparoscopic, or cholangioscopic procedures; (4) Predicted life span ≥ 1 year; and (5) Karnofsky score > 70.
Exclusion criteria included: (1) Concomitant CBD stone with a diameter > 20 mm; (2) Four or more intrahepatic stones; (3) Severe cardiac insufficiency (New York Heart Association class III-IV) or advanced lung disease (determined by consultation with respiratory disease specialists), liver disease (Child-Pugh class C), or advanced renal dysfunction (stage G3 to G5 of chronic kidney disease); and (4) Severe coagulopathy (prothrombin time > 17 s and/or platelet count ≤ 60 × 109/L).
Procedure: Modified PTPBD
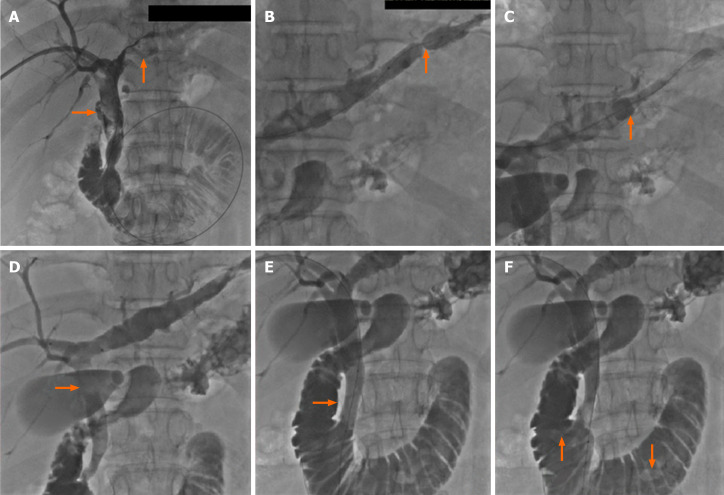
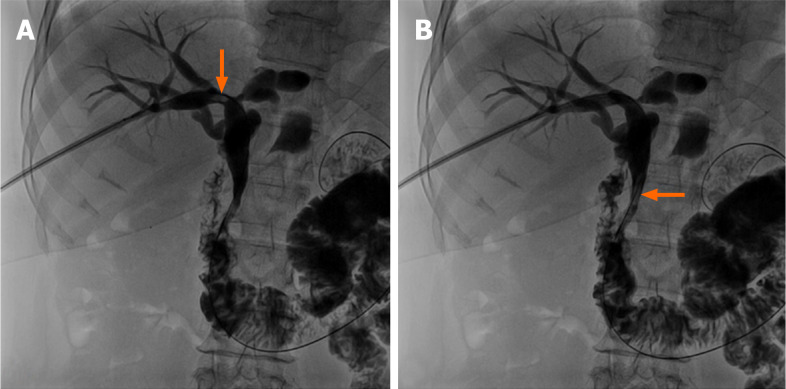
All procedures were performed with intravenous anesthesia. The intrahepatic bile duct (usually right) was punctured under ultrasonic sound and fluoroscopic guidance. Cholangiography with diluted contrast media delineated biliary duct anatomy and revealed the location, number and size of the bile duct stones (Figure 2A). An 8- to 14-French introducer sheath was inserted into the punctured branch, and then a 150-cm-long guidewire was advanced into the intrahepatic bile duct branch peripheral to the stones, with the help of a 5-French tapered-angle angiographic catheter. A stiff 260-cm-long guidewire was exchanged into the bile duct. Affected bile duct was dilated with a balloon (Advance 35LP; Cook Medical, Bloomington, IN, United States) if stenosis was present (Figure 2B). A Fogarty catheter (Edwards Lifesciences, Irvine, CA, United States) was introduced along the guidewire, crossing the stones into the peripheral bile duct branch. The balloon was inflated and stones were pushed into CBD (Figure 2C and D). For large stones, basket mechanical lithotripsy was used to reduce the stone size. For stones located in the punctured bile duct with no or moderate stenosis, injection of saline through the sheath or a moderately inflated balloon dilation catheter was used to push the stones into the CBD (Figure 3A and B).
Figure 2.
Cholangiography. A: Cholangiography revealed the location, size, and number of the intrahepatic and common bile duct stones; B: The left bile duct with stones was dilated with a balloon catheter in presence of stenosis; C: The intrahepatic bile duct stone was pushed with a dilated Fogarty catheter; D: Stone was pushed into common bile duct; E: The papilla was dilated; F: Stones in the common bile duct were pushed into the duodenum.
Figure 3.
For stones located in the punctured bile duct with no or moderate stenosis, injection of saline through the sheath or a moderately inflated balloon dilation catheter was used to push the stones into common bile duct. A: A stone (arrow) located in the right hepatic bile duct; B: Saline was injected through the sheath and the stone was pushed into the common bile duct (arrow).
Stones in CBD should be managed according to the procedure, which has been described in our previous publications[14,15]. The papilla was gradually and intermittently dilated until the balloon’s “waist” disappeared (Figure 2E). The inflation process took 30 to 60 s and the dilation was repeated 3 to 4 times for each patient[10,11]. The balloon size depended on the diameter of the dilated CBD and largest stone, and ranged from 10 to 20 mm. After sphincter dilatation, stones were pushed into the duodenum through the dilated papilla (Figure 2F). After the procedure, the stools of each patient were checked for 1 wk to collect the stones. Stone number and sizes were estimated according to imaging modalities and stools. After 1 wk, cholangiography was performed to exclude residual stone. PTPBD was performed again if there were residual stones. If not, the drainage catheter was withdrawn.
Follow-up
Recorded outcomes included success rate, procedure time, hospital stay, causes of failure, and procedure-related complications. The levels of WBC count, TBIL, DBIL, AST and serum amylase were recorded before the procedure, at 1 wk, and at 1, 3, 6, 12, 18, and 24 mo after the procedure. Imaging modalities such as ultrasound (preferred examination), CT, or MRCP were repeated during follow-up every 3 mo. Biliary duct infection, hemorrhage, pancreatitis, and gastrointestinal and biliary duct perforation, considered as short-term complications, were assessed before discharge. Long-term complications such as reflux cholangitis and calculi recurrence were recorded for 2 years.
Statistical analysis
Continuous variables with normal distribution are expressed as mean ± standard deviation (SD), and analyzed with the Student’s t-test. Continuous variables with unnormal distribution were expressed as the median and interquartile range, and analyzed with the rank sum test. Categorical variables were presented as number and percentage, and analyzed using the χ2 test. All data were analyzed with SPSS version 24.0 (SPSS Inc., Chicago, IL, United States). P < 0.05 was considered statistically significant.
RESULTS
There were 11 men and 10 women aged 51 to 82 (mean, 68.3 ± 4.2) years. Eleven patients (52.4%) with concomitant intrahepatic and CBD stones were admitted with obstructive jaundice. Six patients (28.6%) suffered from intermittent fever and four patients (19%) from abdominal pain. All cases were diagnosed with cardiac or pulmonary diseases including pulmonary emphysema, respiratory insufficiency, coronary heart disease, and cardiac insufficiency.
The mean age of the 21 patients was 68.3 ± 4.2 years old. A total of 36 intrahepatic stones were successfully expelled into the duodenum by modified PTPBD in 20 (95.23%) patients. The diameters of intrahepatic stones ranged from 5 to 15 mm. The diameter of 17 (47.22%) stones was < 10 mm and 19 (52.78%) ranged from 10 to 15 mm. Concomitant CBD stones were present in 16 patients, with stone size between 5 to 20 mm. Characteristics of patients and treatments are summarized in Table 1. Mean procedure time was 65.8 ± 5.3 min. PTPBD was repeated in one patient due to residual stones. Mean hospitalization was 10.7 ± 1.5 d.
Table 1.
Patient and treatment characteristics
| Characteristic | n (%) |
| No. of patients | 21 |
| Gender | |
| Female | 10 (47.6) |
| Male | 11 (58.8) |
| Comorbidity | |
| Emphysema | 5 (23.8) |
| Pulmonary insufficiency | 6 (28.6) |
| Coronary artery disease | 4 (19) |
| Cardiac insufficiency | 5 (23.8) |
| Hypoproteinemia | 1 (4.8) |
| Concomitant CBD stones | 16 (76.2) |
| Symptoms | |
| Obstructive jaundice | 11 (52.4) |
| Fever | 6 (28.6) |
| Abdominal pain | 4 (19) |
| Success rate | 20 (95.2) |
| No. of IHS | 36 |
| Diameter of largest IHS | |
| 5-10 mm | 17 (47.2) |
| 10-15 mm | 19 (52.8) |
| No. of CBD stones | 22 |
| Diameter of Largest CBD stones | |
| 5-10 mm | 4 (18.2) |
| 10-15 mm | 5 (22.7) |
| 15-20 mm | 8 (36.4) |
| 20-25 mm | 4 (18.2) |
| 25-28 mm | 1 (4.5) |
| Total No. of stones | 58 |
| Types of stones | |
| Cholesterol stone | 27 (45.7) |
| Mixed stone | 25 (43.1) |
| Bilirubin stone | 6 (10.3) |
IHS: Intrahepatic bile duct stones; CBD: Common bile duct.
The procedure failed in one patient because of stone impaction in the intrahepatic bile duct. The inflated Fogarty catheter could not push the stone into the CBD. The patient was transferred to the Department of General Surgery and underwent percutaneous transhepatic cholangioscopy.
Abdominal pain was common during papillary dilation but was relieved immediately after the procedure. The symptoms of jaundice disappeared after the procedure in all patients. WBC count, TBIL, DBIL, and AST declined markedly after the procedure. The differences in these indexes before and 1 wk after the procedure were significant. In contrast, ALB concentration significantly increased after the procedure (Table 2).
Table 2.
Relevant variables before and 1 wk after the procedure
| Laboratory variables | Before the procedure | 1 wk after the procedure | P value1 |
| AST, U/L | 128.6 ± 14.3 | 42.8 ± 7.9 | 0.0069 |
| TBIL, µmol/L | 169.5 ± 16.7 | 68.7 ± 8.4 | 0.0093 |
| DBIL, µmol/L | 110.7 ± 19.4 | 35.2 ± 6.3 | 0.0054 |
| WBC, 109/L | 23.9 ± 3.3 | 11.4 ± 2.8 | 0.037 |
| ALB, g/L | 20.8 ± 2.6 | 33.5 ± 1.7 | 0.041 |
Rank sum test for paired samples. Data are presented as mean ± standard deviation. AST: Aspartate aminotransferase; TBIL: Total bilirubin; DBIL: Direct bilirubin; WBC: White blood cell; ALB: Albumin.
Fever and chills suggesting biliary duct infection, occurred in 2 patients (9.52%), and subsided after antibiotic therapy for 2 to 3 d. Mild elevated serum amylase was seen in one patient (4.76%), without sign of peritoneal irritation or fever and decreased to normal levels in 2 d after procedure. We considered it a minimal subclinical reaction and not true pancreatitis. No sign of gastrointestinal or biliary duct perforation were present. All patients were followed up for 2 years, and there was no evidence of reflux cholangitis and calculi recurrence.
DISCUSSION
Vachell et al[16] first reported intrahepatic calculi in 1906. The incidence was reported to be 20%-30% of all patients undergoing surgery for gallstone disease. Most patients are affected in the 3rd to 7th decades on life with equal gender distribution. Concomitant intrahepatic and extrahepatic stones are found in approximately 70% of all hepatolithiasis cases[7,17].
Hepatolithiasis is characterized by recurrent pyogenic cholangitis with inflammatory bile duct wall leading to progressive biliary stricture, causing bile stasis, liver atrophy, and cholangiocarcinoma[18]. In China, 80% of patients with peripheral intrahepatic cholangiocarcinoma have associated intrahepatic stones[19,20].
The aims of treatment are prevention of liver damage by elimination of stones and recovery of bile fluidity and includes stone clearance, recovery of bile duct stricture, and providing good drainage of bile[21-23]. Surgical options are considered by many authors the preferred treatment. However, the surgical procedure has significant morbidity and mortality. ERCP is used for papillotomy, sphincterotomy and retrieval basket for stone extraction, which should be considered the first attempt to treat hepatolithiasis. The application is limited because large or impacted stones could not be easily managed by conventional endoscopy. Brewer Gutierrez et al[24] reported peroral cholangioscopy with the development of flexible, high-resolution endoscopes have enabled successful endoscopic therapy in laser and electrohydraulic treatment in > 85% of patients. However, such a procedure cannot be performed in most hospitals in China due to the lack of access to cholangioscopy. In addition, for patients with altered gastrointestinal anatomies, the endoscopic procedure could be very difficult. Endoluminal approach with intraductal lithotripsy combined with extracorporeal shock wave lithotripsy may remove stones in approximately 66% of patients.
Percutaneous options provide biliary drainage, with transhepatic placement of catheters, stents, basket/balloon catheters and cholangiography to detect or confirm clearance of biliary stones. Percutaneous approach is advantageous for high-surgical-risk patients with altered gastrointestinal anatomies, multiple stones in several segments or patients rejected to undergo surgery.
Furthermore, patients with cardiac or pulmonary comorbidities may not tolerate endotracheal anesthesia and surgery. Therefore, modified PTPBD under intravenous anesthesia has advantages and such patients may benefit from this procedure.
In 2000, Shirai et al[25] reported that PTPBD could relieve obstructive jaundice caused by CBD stones. To the best of our knowledge, our team performed the first PTPBD procedure to treat CBD in China in 2008[26]. Compared with ERCP, the inflated balloon dilates the entire papilla but keeps the whole structure intact[27], with low incidences of biliary duct infection and hemorrhage and no pancreatitis or perforation of the gastrointestinal or biliary duct[26].
The first step for hepatolithiasis is to move the stones into CBD. A Fogarty balloon catheter is useful for small stones, while a mechanical basket crashes and reduces the size of large stones. The presence of bile duct stenosis has been considered a cause of lithogenesis and stone recurrence. Bile stenosis is also a major factor in hepatic atrophy and cholangiocarcinoma developing[28]. Therefore, balloon dilation is necessary when bile duct stenosis is present.
Simultaneous CBD stones are not contraindications. However, the size of CBD stones should be limited. Endoscopic treatments, including endoscopic sphincterotomy and endoscopic papillary balloon dilation, usually consider stones with a diameter exceeding 10 mm to 12 mm as large stones[28,29]. For these difficult cases, percutaneous approach with a large balloon (≥ 10mm) and long-term dilation could be safer, and the short procedure time remarkably decreased the incidence of pancreatitis. This is a significant advantage and was verified in our clinical practice and in previous studies of PTPBD[14,15,25,26]. The maximum balloon diameter we used in this study was 20 mm and no pancreatitis occurred after the procedure (unpublished data). Hence, the maximum diameter of CBD stones was determined to be no larger than 20 mm in this study.
As in endoscopic procedures, multiple stones are challenging in PTPBD. Repeated procedure may damage mucosa, causing bleeding and local edema, while an extended procedure time may increase the cardiopulmonary morbidities and anesthetic risk. Based on the current experience of our team, PTPBD should not be attempted if there are four or more stones.
Nevertheless, this study had two limitations. First, as a pilot study, the number of patients was small, and this method is devised for a specific subset of patients in one center. Second, the retrospective character of the study may have caused a selection bias of cases.
In conclusion, our results indicate that modified PTPBD is a safe, feasible, and effective treatment option for intrahepatic bile duct stones. It is a new alternative procedure for a small number of patients with hepatolithiasis and may be a treatment option in patients with severe comorbidities or in patients in which ERCP was not successful. A prospective study in multiple centers and the generalizability of our findings to the broader population will be investigated in the future.
ARTICLE HIGHLIGHTS
Research background
The treatment of hepatolithiasis is complicated and difficult. Some patients cannot tolerate surgery due to severe cardiac or pulmonary comorbidities, or cannot be treated with endoscopy because of altered gastrointestinal anatomies.
Research motivation
Our previous experience indicated percutaneous transhepatic papillary balloon dilation (PTPBD) could be an alternative for common bile duct stones.
Research objectives
In this retrospective study, the clinical efficacy and safety of modified PTPBD were assessed for the removal of intrahepatic bile duct stones in patients with cardiopulmonary comorbidities or altered gastrointestinal anatomies.
Research methods
Twenty-one patients with intrahepatic bile duct stones who underwent modified PTPBD were enrolled in this study. Outcomes, including success rate, cause of failure, complications, procedure time and hospital stay, were analyzed. Reflux cholangitis and calculi recurrence were recorded for 2 years.
Research results
The success rate was 95.23%. No pancreatitis or perforation occurred. No evidence of reflux cholangitis and calculi recurrence were observed for 2 years.
Research conclusions
Modified PTPBD could be considered as a safe, feasible, and effective treatment option for intrahepatic bile duct stones in patients with cardiopulmonary comorbidities or altered gastrointestinal anatomies.
Research perspectives
Multi-center prospective study should be conducted to compare modified PTPBD to surgery or endoscopic procedures to gain more evidence.
Footnotes
Institutional review board statement: This study was approved by the ethics committee of the Second Hospital of Shandong University, No. KYLL-2014(LW)02.
Informed consent statement: All participants provided written informed consent.
Conflict-of-interest statement: All authors declare no conflicts-of-interest related to this article.
Manuscript source: Unsolicited manuscript
Peer-review started: May 6, 2020
First decision: May 21, 2020
Article in press: July 4, 2020
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dik VK, Malieckal A, Treepongkaruna S, Wang MH S-Editor: Wang JL L-Editor: Filipodia E-Editor: Ma YJ
Contributor Information
Bin Liu, Department of Interventional Medicine, The Second Hospital of Shandong University, Jinan 250033, Shandong Province, China; Interventional Oncology Institute of Shandong University, Jinan 250033, Shandong Province, China.
Pi-Kun Cao, Department of Cancer Center, The First Affiliated Hospital of Shandong First Medical University, Jinan 250014, Shandong Province, China.
Yong-Zheng Wang, Department of Interventional Medicine, The Second Hospital of Shandong University, Jinan 250033, Shandong Province, China; Interventional Oncology Institute of Shandong University, Jinan 250033, Shandong Province, China.
Wu-Jie Wang, Department of Interventional Medicine, The Second Hospital of Shandong University, Jinan 250033, Shandong Province, China; Interventional Oncology Institute of Shandong University, Jinan 250033, Shandong Province, China.
Shi-Lin Tian, School of Medicine, Shandong University, Jinan 250014, Shandong Province, China.
Yancu Hertzanu, Department of Interventional Medicine, The Second Hospital of Shandong University, Jinan 250033, Shandong Province, China; Interventional Oncology Institute of Shandong University, Jinan 250033, Shandong Province, China.
Yu-Liang Li, Department of Interventional Medicine, The Second Hospital of Shandong University, Jinan 250033, Shandong Province, China; Interventional Oncology Institute of Shandong University, Jinan 250033, Shandong Province, China. lyl.pro@sdu.edu.cn.
Data sharing statement
No additional data are available.
References
- 1.Blechacz B, Komuta M, Roskams T, Gores GJ. Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 2011;8:512–522. doi: 10.1038/nrgastro.2011.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011;54:173–184. doi: 10.1002/hep.24351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Catena M, Aldrighetti L, Finazzi R, Arzu G, Arru M, Pulitanò C, Ferla G. Treatment of non-endemic hepatolithiasis in a Western country. The role of hepatic resection. Ann R Coll Surg Engl. 2006;88:383–389. doi: 10.1308/003588406X98711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park Y, Kim D, Lee JS, Kim YN, Jeong YK, Lee KG, Choi D. Association between diet and gallstones of cholesterol and pigment among patients with cholecystectomy: a case-control study in Korea. J Health Popul Nutr. 2017;36:39. doi: 10.1186/s41043-017-0116-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang CM, Chiu THT, Chang CC, Lin MN, Lin CL. Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study. Nutrients. 2019;11:335. doi: 10.3390/nu11020335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park YH, Park SJ, Jang JY, Ahn YJ, Park YC, Yoon YB, Kim SW. Changing patterns of gallstone disease in Korea. World J Surg. 2004;28:206–210. doi: 10.1007/s00268-003-6879-x. [DOI] [PubMed] [Google Scholar]
- 7.Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic) Best Pract Res Clin Gastroenterol. 2006;20:1075–1083. doi: 10.1016/j.bpg.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 8.Kayhan B, Akdoğan M, Parlak E, Ozarslan E, Sahin B. Hepatolithiasis: a Turkey experience. Turk J Gastroenterol. 2007;18:28–32. [PubMed] [Google Scholar]
- 9.Park HS, Lee JM, Kim SH, Jeong JY, Kim YJ, Lee KH, Choi SH, Han JK, Choi BI. CT Differentiation of cholangiocarcinoma from periductal fibrosis in patients with hepatolithiasis. AJR Am J Roentgenol. 2006;187:445–453. doi: 10.2214/AJR.05.0247. [DOI] [PubMed] [Google Scholar]
- 10.Khuroo MS, Rather AA, Khuroo NS, Khuroo MS. Hepatobiliary and pancreatic ascariasis. World J Gastroenterol. 2016;22:7507–7517. doi: 10.3748/wjg.v22.i33.7507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheen-Chen S, Chen W, Eng H, Sheen C, Chou F, Cheng Y, Lee T. Bacteriology and antimicrobial choice in hepatolithiasis. Am J Infect Control. 2000;28:298–301. doi: 10.1067/mic.2000.107071. [DOI] [PubMed] [Google Scholar]
- 12.Nitin Rao AR, Chui AK. Intrahepatic stones - an etiological quagmire. Indian J Gastroenterol. 2004;23:201–202. [PubMed] [Google Scholar]
- 13.Cha SW. [Management of Intrahepatic Duct Stone] Korean J Gastroenterol. 2018;71:247–252. doi: 10.4166/kjg.2018.71.5.247. [DOI] [PubMed] [Google Scholar]
- 14.Wang W, Wang C, Qi H, Wang Y, Li Y. Percutaneous transcystic balloon dilation for common bile duct stone removal in high-surgical-risk patients with acute cholecystitis and co-existing choledocholithiasis. HPB (Oxford) 2018;20:327–331. doi: 10.1016/j.hpb.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Li D, Li YL, Wang WJ, Liu B, Chang HY, Wang W, Wang YZ, Li Z. Percutaneous transhepatic papilla balloon dilatation combined with a percutaneous transcystic approach for removing concurrent gallbladder stone and common bile duct stone in a patient with billroth II gastrectomy and acute cholecystitis: A case report. Medicine (Baltimore) 2017;96:e7964. doi: 10.1097/MD.0000000000007964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vachell HR, Stevens WM. Case of Intrahepatic Calculi. Br Med J. 1906;1:434–436. doi: 10.1136/bmj.1.2356.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blumgart LH, Fong Y. Surgery of the Liver and Biliary Tract. 3rd ed. Philadelphia: W. B. Saunders Company, 2000. [Google Scholar]
- 18.Kusano T, Isa T, Ohtsubo M, Yasaka T, Furukawa M. Natural progression of untreated hepatolithiasis that shows no clinical signs at its initial presentation. J Clin Gastroenterol. 2001;33:114–117. doi: 10.1097/00004836-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Meng ZW, Han SH, Zhu JH, Zhou LY, Chen YL. Risk Factors for Cholangiocarcinoma After Initial Hepatectomy for Intrahepatic Stones. World J Surg. 2017;41:835–843. doi: 10.1007/s00268-016-3752-2. [DOI] [PubMed] [Google Scholar]
- 20.Kim HJ, Kim JS, Suh SJ, Lee BJ, Park JJ, Lee HS, Kim CD, Bak YT. Cholangiocarcinoma Risk as Long-term Outcome After Hepatic Resection in the Hepatolithiasis Patients. World J Surg. 2015;39:1537–1542. doi: 10.1007/s00268-015-2965-0. [DOI] [PubMed] [Google Scholar]
- 21.Cai X, Wang Y, Yu H, Liang X, Peng S. Laparoscopic hepatectomy for hepatolithiasis: a feasibility and safety study in 29 patients. Surg Endosc. 2007;21:1074–1078. doi: 10.1007/s00464-007-9306-9. [DOI] [PubMed] [Google Scholar]
- 22.Gao JB, Shi WJ, Hu ZJ, Bai LS, Chai XQ. Hepatectomy for hepatolithiasis among patients with a history of biliary surgery. Int J Clin Exp Med. 2016;9:13184–13189. [Google Scholar]
- 23.Pan GD, Yan LN, Li B, Lu SC, Zeng Y, Wen TF, Zhao JC, Cheng NS, Ma YK, Wang WT, Yang JY, Li ZH. Liver transplantation for patients with hepatolithiasis. Hepatobiliary Pancreat Dis Int. 2005;4:345–349. [PubMed] [Google Scholar]
- 24.Brewer Gutierrez OI, Bekkali NLH, Raijman I, Sturgess R, Sejpal DV, Aridi HD, Sherman S, Shah RJ, Kwon RS, Buxbaum JL, Zulli C, Wassef W, Adler DG, Kushnir V, Wang AY, Krishnan K, Kaul V, Tzimas D, DiMaio CJ, Ho S, Petersen B, Moon JH, Elmunzer BJ, Webster GJM, Chen YI, Dwyer LK, Inamdar S, Patrick VB, Attwell A, Hosmer A, Ko C, Maurano A, Sarkar A, Taylor LJ, Gregory MH, Strand DS, Raza A, Kothari S, Harris JP, Kumta NA, Manvar A, Topazian MD, Lee YN, Spiceland CM, Trindade AJ, Bukhari MA, Sanaei O, Ngamruengphong S, Khashab MA. Efficacy and Safety of Digital Single-Operator Cholangioscopy for Difficult Biliary Stones. Clin Gastroenterol Hepatol. 2018;16:918–926.e1. doi: 10.1016/j.cgh.2017.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Shirai N, Hanai H, Kajimura M, Kataoka H, Yoshida K, Nakagawara M, Nemoto M, Nagasawa M, Kaneko E. Successful treatment of percutaneous transhepatic papillary dilation in patients with obstructive jaundice due to common bile duct stones after Billroth II gastrectomy: report of two emergent cases. J Clin Gastroenterol. 2000;30:91–93. doi: 10.1097/00004836-200001000-00020. [DOI] [PubMed] [Google Scholar]
- 26.Li YL, Geng JL, Jia YM, Lu HL, Wang W, Liu B, Wang WJ, Chang HY, Wang YZ, Li Z. [Clinical study of percutaneous transhepatic balloon dilation:a novel procedure for common bile duct stone] Zhonghua Yi Xue Za Zhi. 2013;93:3586–3589. [PubMed] [Google Scholar]
- 27.Ding J, Li F, Zhu HY, Zhang XW. Endoscopic treatment of difficult extrahepatic bile duct stones, EPBD or EST: An anatomic view. World J Gastrointest Endosc. 2015;7:274–277. doi: 10.4253/wjge.v7.i3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cai H, Kong WT, Chen CB, Shi GM, Huang C, Shen YH, Sun HC. Cholelithiasis and the risk of intrahepatic cholangiocarcinoma: a meta-analysis of observational studies. BMC Cancer. 2015;15:831. doi: 10.1186/s12885-015-1870-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jin PP, Cheng JF, Liu D, Mei M, Xu ZQ, Sun LM. Endoscopic papillary large balloon dilation vs endoscopic sphincterotomy for retrieval of common bile duct stones: a meta-analysis. World J Gastroenterol. 2014;20:5548–5556. doi: 10.3748/wjg.v20.i18.5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.