Abstract
BACKGROUND
Coronavirus disease 2019 (COVID-19) is an emerging, rapidly evolving disease that spreads through the respiratory system and is highly contagious. In March 2020, the World Health Organization declared the COVID-19 outbreak a pandemic. In China, the pandemic was controlled after 2 mo through effective policies and containment measures. Describing the detailed policies and containment measures used to control the epidemic in Chongqing will provide a reference for the prevention and control of COVID-19 in other areas of the world.
AIM
To explore the effects of different policies and containment measures on the control of the COVID-19 epidemic in Chongqing.
METHODS
Epidemiological data on COVID-19 in Chongqing were prospectively collected from January 21 to March 15, 2020. The policies and prevention measures implemented by the government during the epidemic period were also collected. Trend analysis was performed to explore the impact of the main policy measures on the effectiveness of the control of COVID-19 in Chongqing.
RESULTS
As of March 15, the cumulative incidence of COVID-19 in Chongqing was 1.84/100000 (576 cases) and the infection fatality rate was 1.04% (6/576). The spread of COVID-19 was controlled by effective policies that involved establishing a group for directing the COVID-19 epidemic control effort; strengthening guidance and supervision; ensuring the supply of daily necessities and medical supplies and equipment to residents; setting up designated hospitals; implementing legal measures; and enhancing health education. Medical techniques were implemented to improve the recovery rate and control the epidemic. Policies such as “the lockdown of Wuhan”, “initiating a first-level response to major public health emergencies”, and “implementing the closed management of residential communities” significantly curbed the spread of COVID-19. Optimizing the diagnosis process, shortening the diagnosis time, and constructing teams of clinical experts facilitated the provision of “one team of medical experts for each patient” treatment for severe patients, which significantly improved the recovery rate and reduced the infection fatality rate.
CONCLUSION
The prevention policies and containment measures implemented by the government and medical institutions are highly effective in controlling the spread of the epidemic and increasing the recovery rate of COVID-19 patients.
Keywords: Prevention policies, Containment measures, COVID-19, Epidemic trend, Control effectiveness, Public health
Core tip: The coronavirus disease 2019 (COVID-19) pandemic is an emerging, rapidly evolving situation, and effective treatment measures are difficult to formulate in a short time. Public health policies and containment measures play a vital role in the prevention and control of COVID-19. Policies such as “the lockdown of Wuhan”, “initiating a first-level response to major public health emergencies”, and “implementing the closed management of residential communities” significantly controlled the spread of COVID-19. Optimizing the diagnosis process, shortening the diagnosis time, and constructing teams of clinical experts facilitated the provision of “one team of medical experts for each patient” treatment for severe cases, significantly improved the recovery rate, and reduced the incidence rate (1.84/100000) and the infection fatality rate [1.04% (6/576)] of COVID-19.
INTRODUCTION
Since December 2019, a deadly emerging infectious disease called coronavirus disease 2019 (COVID-19) has rapidly spread from Wuhan (China), the outbreak epicenter, to more than 200 countries, territories, and areas. On March 11, 2020, the World Health Organization declared COVID-19 a pandemic[1]. Global travel has been severely restricted. The borders of some countries with severe epidemics have been closed, and large-scale quarantine and containment measures have been implemented in almost every country[2]. By May 11, 2020, a total of 4013728 cases had been confirmed worldwide, and 278993 deaths had been reported; the infection fatality rate of COVID-19 (7.00%) is gradually approaching that of severe acute respiratory syndrome (SARS) (9.6%)[3,4].
At present, the numbers of total confirmed cases and deaths in ten countries have exceeded those in China[5]. The United States has the largest number of confirmed cases in the world (> 30%), and tens of thousands of infected people have been identified every day from March to the present because of the delay in the implementation of containment measures, such as large-scale nucleic acid testing (NAT)[6]. Italy is the second typical COVID-19 epicenter after China. The number of patients infected in Italy has followed an exponential trend since February 21, 2020[7]. Some restrictive measures implemented in Italy beginning on March 8, 2020 (such as the lockdown of some regions, school closures, and the suspension of group activities), temporarily controlled the development of the COVID-19 epidemic[7]. However, due to the country’s aging population and the imbalance in the supply of and demand for medical resources, Italy has a high case fatality rate (reaching 14%) and the epidemic there is severe. Iran is a developing country. Although intervention policies have been implemented since the beginning of the outbreak, Iran has experienced a serious surge of cases and deaths due to the shortage of medical resources[8]. As of May 11, the upward trend in the number of daily confirmed cases in the Russian Federation and Brazil has not shown a clear turning point. The international COVID-19 epidemic situation remains serious.
China experienced the earliest outbreak of COVID-19. The first report of identified COVID-19 cases occurred on December 31, 2019, and in the following month, the number of new confirmed cases exploded. During this period, the Chinese government implemented a series of policies and containment measures to respond to the COVID-19 epidemic, such as locking down Wuhan on January 23, screening travelers with a fever at important transportation hubs, testing high-risk groups, and tracking close contacts in a timely manner. With the gradual implementation of these measures, the number of new confirmed cases started to decline in early February 2020 and stopped rising in early March 2020. Obviously, the quick control of the COVID-19 epidemic in China depended on the rapid formulation and decisive implementation of a series of prevention and containment policies and measures, which together cut off the transmission pathways (main routes: respiratory droplets and close contact) of COVID-19. The effectiveness of these measures has been proven in many studies and in practice in other countries[9]. Therefore, an effective global response is urgently needed to meet this unprecedented challenge, and the experience of China will provide some reference.
The current research worldwide has focused primarily on etiology[10,11], clinical characteristics[12,13], modes of transmission[14,15], and clinical diagnosis and treatment methods[16,17]. There is limited research on public health issues, such as epidemiological survey methods and quarantine methods[18]. This study is the first to describe the effect of detailed public health policies on the control of COVID-19 in Chongqing. Various prevention and control measures adopted by governments at all levels in response to the COVID-19 pandemic in China have indeed had a considerable impact on the control of the spread of COVID-19. For example, on January 23, 2020, the lockdown of Wuhan prevented the migration of exposed people to other areas of China and curbed the nationwide spread of the disease. At the end of January, the Chinese government announced an extension of the Spring Festival holiday and postponed the start of the new semester nationwide. In addition, the closed management of residential communities and travel restrictions for community residents were implemented beginning in early February, which further prevented the intergenerational transmission of COVID-19.
Several studies have used the dynamic model of infectious diseases to explore trends in the epidemiology of COVID-19[19,20], focusing mainly on predicting the number of confirmed cases by time period while ignoring the impact of control policies and measures. Several of these studies have considered the impact of the lockdown of Wuhan on the epidemic trend of COVID-19 but have not considered the effects of other prevention and control policies and measures[21,22].
Therefore, this study summarized the policies and control measures adopted by the government and medical institutions in Chongqing for the prevention and control of COVID-19 and explored the impact of the lockdown of Wuhan, the closed management of residential communities, and other relevant policy measures on the epidemic trend in Chongqing. It will provide policy suggestions for other countries to curb the spread of COVID-19, and will also provide a theoretical basis for the prevention and control of emerging infectious diseases in the future.
MATERIALS AND METHODS
Epidemiological data collection
Epidemiological data were collected from the official website of the Chongqing Municipal Health Commission from January 21, 2020 (the first date that a COVID-19 case was reported in Chongqing) to March 15, 2020 (when the epidemic was controlled). The data included the daily number of new confirmed cases, total confirmed cases, suspected cases, close contacts, people under medical observation, inpatient cases, severe cases, death cases, and discharged cases.
Collecting materials on prevention and control policies for COVID-19
Some of the management policy materials and their implementation dates for COVID-19 were collected from the official websites of the government and the Municipal Health Commission of Chongqing. Other policy materials on implementation and containment measures were obtained by querying the leaders and frontline workers at the CDC and local medical institutions.
Statistical analysis
Data were double-entered into Microsoft Access 2007 by two researchers using a blinded method, and a consistency check was performed before analysis. The descriptive analysis for this study was performed by Excel 2016 and included (1) The epidemic trend of the daily number of new confirmed cases, total confirmed cases, new discharged cases, total discharged cases, new close contacts, total close contacts, and cases under medical obeservation of COVID-19 in Chongqing; and (2) The trend (after logarithmic transformation) of the incidence rate, cumulative incidence rate, and composition ratio of severe cases, deaths, and discharged cases after diagnosis of COVID-19 in Chongqing. The χ2 test was used to test the differences in the incidence rate and infection fatality rate.
The data was analyzed using SAS 9.4 software (Copyright© 2020 SAS Institute Inc. Cary, NC, United States). A significant difference was defined at an α level of 0.05.
RESULTS
Policies and measures for prevention and control of COVID-19 in Chongqing
Organization and management policies: Establish a group responsible for leading the COVID-19 epidemic control effort. The governor of Chongqing served as the leader of the group responsible for leading the COVID-19 epidemic control effort. The group comprehensively approached the task of pandemic prevention and control, implemented policies, and responded quickly to deal with the emergency work related to COVID-19. All departments insisted that the top leader took full responsibility, and the leader in charge of the prevention and control work was responsible for arranging the implementation details. All leaders and heads of department were required to stay at work and to carry out field work to ensure the completion of the prevention and control tasks. Leaders who failed to do so were punished and fired. Community institutions were organized to participate in COVID-19 prevention and control. For example, workers in sub-district offices and neighborhood committees were organized to participate in the closed management of neighborhoods and epidemiology surveys.
Strengthen guidance and supervision to ensure the implementation of various prevention and containment measures. Leaders at all institutions were instructed to intensify the guidance and supervision of the prevention and control work related to the COVID-19 pandemic. They were to focus their investigative efforts on severely affected districts and organize expert meetings to determine the causes and implement more rigorous measures to ensure the effect of prevention and control tasks.
Ensure the supply of daily necessities to residents. Large supermarkets were responsible for the supply of daily necessities to residents, and the municipal leaders supervised the amount and price of basic supplies at all supermarkets. A “green channel” was established for the supply of important materials, with priority given to the transportation of materials needed by residents for daily life to ensure an adequate supply and meet residents’ daily needs. In some communities, automatic vegetable, fruit, and meat vending machines were installed, and residents could access these goods conveniently. These machines were expected to reduce residents’ opportunity for contact and their movement. The government encouraged people to donate daily necessities (such as rice, vegetables, and meat) to seriously affected areas. Moreover, policy levers were used by agencies to postpone mortgage payments and the delivery time of utility bills for electricity, heat, and water for citizens.
Ensure the supply of medical supplies and equipment. The municipal government ensured the provision of the funds, supplies, and manpower required for the prevention, control, and treatment of COVID-19 and allocated and coordinated these resources among hospitals and the CDC. The government not only organized and encouraged local pharmaceutical and medical device manufacturers to produce personal protective equipment such as masks and protective clothing but also increased the import of protection medical supplies from abroad. The government also encouraged the social anticipation of the procurement of medical materials. In the short term, the government ensured the provision of medical supplies for designated COVID-19 hospitals and fever clinics.
Providing medical cost compensation for patients and salary subsidies for medical staff. The government and medical insurance covered all medical costs and provided nutrition support for suspected and confirmed COVID-19 patients. Moreover, the government provided free novel coronavirus (SARS-CoV-2) NAT for high-risk and susceptible populations from the beginning of the COVID-19 outbreak. The government issued a policy to provide an additional salary subsidy of 200-300 yuan per day for medical staff participating in the prevention and treatment of COVID-19 according to the intensity of their work in local hospitals and an additional salary subsidy of 600-700 yuan per day for medical staff who were sent to Hubei to support COVID-19 prevention and treatment.
Set up designated hospitals to diagnose and cure patients. According to the principle of “centralizing patients, experts, medical resources, and hospitals”, the municipal government of Chongqing set up 4 designated medical institutions with sophisticated medical technology to improve the diagnosis and treatment procedure, focus on curing severe cases, and receive and cure all confirmed cases of COVID-19. Forty-six hospitals distributed in 38 counties were designated as diagnostic hospitals, and all secondary general hospitals were equipped with negative-pressure wards and negative pressure operating rooms and intensive care units. Critical care beds were established, accounting for more than 2% of the total number of beds. Fever cases and suspected COVID-19 cases were quarantined and treated in designated diagnostic hospitals with the capacity to set up isolation wards and prevent nosocomial infections. When suspected cases were confirmed, patients were sent to the designated COVID-19 medical institutions for treatment. Hospitals of all grades complied with the graded diagnosis and treatment procedure, which saved a considerable amount of medical resources. A medical team was established at every centralized isolated point. After the CDC investigated the close contacts of confirmed cases, the close contacts were sent to the centralized isolated points and isolated for 14 d under the monitoring of medical teams. If they had symptoms, they were transferred to the designated hospitals. Except for community health centers, every hospital set up 24-h working special fever clinics to diagnose COVID-19 during the pandemic.
Adopt legal measures for COVID-19 prevention and control. The judicial authorities of Chongqing issued a Notice on Severely Punishing Illegal and Criminal Activities against the Prevention and Control of Novel Coronavirus Infection According to Law to ensure the prevention and control of the COVID-19 epidemic. The law on the prevention and cure of infectious diseases was widely publicized to improve people’s understanding of and cooperation with the COVID-19 prevention and control efforts. Those who deliberately spread the pathogen of the novel coronavirus or who concealed their contact history with an epidemic area or a confirmed case or refused to quarantine were convicted and punished for crimes against public safety. The market supervisory authorities were responsible for the price enforcement of the supply of goods. They punished illegal acts such as spreading price increase information and price fraud, and intensified law enforcement on the on-site slaughter and illegal sales of livestock and wild animals. The Chongqing Municipal Public Security Bureau mobilized 41000 policemen and 28000 auxiliary policemen to participate in the prevention and control of the COVID-19 epidemic until March 11. They were tasked with identifying the activity path of confirmed cases and ensuring the safety and stability of the overall social situation. The above measures were intended to ensure social stability and order.
Report the status of the epidemic through the media to help people understand and support the COVID-19 control policies. First, the media released information about the pandemic accurately, publicly, and clearly. Second, through in-depth reporting, examples of disease control or the cure of special cases were provided to allay people’s concerns. This helped citizens to treat the epidemic objectively, calmly, and rationally and encourage them to support and cooperate with the government to control the pandemic. Third, health knowledge training about the prevention and containment measures was published every day through the media. Finally, the health management institutes sent information about how to prevent COVID-19 every day through short messages to every citizen.
Medical technical measures: Organize temporary medical teams to carry out centralized treatment. The government designated 4 hospitals to treat confirmed cases by region (with the whole municipality divided into four regions) based on the principle of proximity. The expert groups on COVID-19 treatment were established in each of the four centralized treatment hospitals and improved the diagnosis and treatment procedures, and guidelines were established according to the symptoms and adjusted when more effective treatment methods were found. Moreover, Chinese medicine and a combination of Western and Chinese medicine were applied in COVID-19 treatment to improve symptoms. Treatments were carried out carefully. The hospitals organized enough medical staff and prepared medical equipment to carry out a “one expert group for each patient” treatment plan for critically ill patients to improve the effectiveness of treatment and reduce the death rate. Experts major in infectious disease treatment throughout the city were registered and deployed to support areas with severe epidemic conditions. On January 29, China Mobile Chongqing Company opened 5G networks in 4 designated hospitals and connected 5G remote consultation systems for the treatment of COVID-19.
Quarantine the whole municipality. Quarantine focused on four types of high-risk populations: Confirmed cases, suspected cases, fever patients, and migrants. The government organized the CDC, hospitals, and community clinics to enforce comprehensive and in-depth quarantine measures at transport entry points (such as traffic toll stations, airports, train stations, bus stations for long distance travel, and ports) by guarding the entrances and taking the temperature of all individuals entering and leaving, one by one. Special inspections were carried out in public places, hospitals, shopping malls, and other important hubs. The CDC and communities carried out household surveys of people arriving from Hubei and abroad to achieve effective prevention and control in communities. Household quarantine in rural areas was enforced by temporary teams composed of staff from towns, villages, and communities. In addition, the authorities paid attention to the management of people in nursing homes, jails, and detoxification centers and implemented a 14-d continuous work period in those locations.
Optimize the NAT process. The CDC improved the test plan, optimized the test process, and achieved the goal of “completing testing of accumulated samples and immediately testing the new samples”, shortening the diagnosis time of suspected cases. To expand NAT capacity, the CDC trained staff from hospitals and community health centers on how to collect pharyngeal samples, nasopharyngeal samples, and anal samples. For highly suspected cases, we usually need to repeatedly collect and test pharyngeal specimen, and use nasopharyngeal specimens and anal specimens for verification, or perform virus-specific antibody IgM and IgG tests, CT test, or biochemical test to make a comprehensive diagnosis. Sample collection was carried out in all hospitals and community health centers. The medical institutions sent samples 2-3 times per day to the CDC or other NAT agencies. Initially, the NAT was carried out mainly at the CDC, which could not process so many samples in a timely manner; then, the government recruited NAT companies to participate. As of 25 May, there were approximately 62 NAT institutions in Chongqing, with a total of 733 thousand samples tested, and every county had at least two NAT institutes. Every hospital with two-stage levels or above will implement NAT until September. Therefore, results can be reported 4-5 h after sample collection, as there are more NAT institutes. In addition, the government expanded the population for NAT to include patients in fever clinics, all inpatients, close contacts, suspected cases, those in special institutions (jails, nursing homes, and centralized production factories), and people from Hubei and abroad.
Adjust the risk level dynamically according to the recommendations of experts. To realize scientific, systematic, precise, and effective prevention and control of COVID-19, expert teams analyzed and interpreted the development of the epidemic dynamically. Risk stages were defined according to the dynamic development of the epidemic in every district and country and were adjusted accordingly. Differentiated prevention and control strategies were implemented in different areas.
Strengthen the infection management of hospitals to prevent nosocomial infections. The hospitals strictly implemented nosocomial infection preventive measures, such as training medical staff to enhance their personal protection awareness; establishing standardized fever clinics and isolation wards in all medical institutions to cure COVID-19 cases; optimizing diagnosis, treatment, and isolation procedures; and learning from the experience of other regions. Moreover, hospitalization patients and their chaperones must receive NAT before they enter wards, and medical staff should receive NAT regularly.
Control the source of infection and strictly prevent imported cases. The government blocked the source of infection by preventing the import of external cases and the spread of local cases. The main measures for preventing imported cases included setting up temporary quarantine stations at traffic stations and entry-exit ports to identify individuals with fever symptoms and transferring them to designated places for medical observation; implementing traffic control at provincial borders during the serious outbreak period to ban people from high-risk areas from entering Chongqing starting on February 1 and implementing a highway reservation system for cars from other provinces starting on February 3 to control the number of people entering Chongqing; suspending interprovincial passenger transport starting on January 27; cracking down on illegal vehicles to eliminate imported infection risks; and strengthening the inspection of towns and villages bordering Hubei. The main measures taken to prevent the spread of local cases included extending the Spring Festival holiday and increasing control of public traffic in the city; carrying out inspections on every vehicle entering and leaving residential areas; conducting centralized isolation or home isolation or home medical observation for high-risk populations(people from Hubei, fever patients, close contacts of confirmed cases or suspected cases, and recovery cases after discharge); increasing the inspection of public places and canceling group dining and entertainment activities; strengthening the clinical identification of asymptomatic infected persons and the follow-up monitoring of febrile patients to control the “moving source of infection”; and carrying out epidemiological follow-up investigations on confirmed cases and suspected cases. As of February 8, 95 centralized isolation points with 5754 rooms were arranged, and centralized isolation was implemented for all close contacts in Chongqing. Hotels far from residential areas were used as the centralized isolation points. Moreover, community managers visited every family in person or contacted them over the telephone to investigate the movement status and health situation of family members and to find high-risk populations. Finally, a “health WeChat QR code” was used to record the travel and health information of all citizens starting on February 19, and people traveling to other places and entering public places were required to show their health WeChat QR code.
Control the transmission route and protect vulnerable populations. First, the measures taken by the Chongqing municipality to reduce the movement of people included the closed management of residential communities beginning on February 7, 2020 (earlier than in Beijing, Shanghai, and Wuhan) to minimize travel and the suspension of free bus cards for the elderly in urban areas from February 8, 2020, until the end of the epidemic. The government also issued mandates to close all crowded places, to postpone the start of the new semester, and to cancel major meetings. Moreover, institutions implemented staggered working and eating hours during the pandemic period. Second, disinfection and ventilation measures were strictly implemented and included disinfecting public transportation and public spaces once a day, maintaining indoor air circulation, disinfecting air conditioning filters, disinfecting elevators frequently, and providing disposable paper towels or disinfectants. Additionally, the CDC carried out disinfection in the home and activity areas of every confirmed case and suspected case. Third, the government emphasized the importance of wearing a mask, and it was strictly forbidden to go in or out without wearing a mask. When the pandemic began, masks were first sent to hospitals to guarantee that the needs of medical staff were met. In addition, the supervision of enterprises that resumed work and production was intensified.
Focus on psychological intervention and humanistic care. The Chongqing Municipal Health Commission dispatched psychologists to provide psychological counseling and aid for citizens through a 24-h hotline to alleviate their panic and prevent adverse events caused by COVID-19. A handbook on psychological intervention for COVID-19 medical staff was created in Chongqing to help relieve staff’s psychological pressure. Moreover, a psychological crisis intervention volunteer vanguard was established to manage psychological pressure in a hierarchical manner, identifying high-risk groups and low-risk group, carrying out psychological crisis interventions for high-risk groups, carrying out mental health education for low-risk group, and actively carrying out emergency psychological crisis intervention and psychological counseling to ensure professional and efficient mental health education and classification guidance.
Carry out health education. To promote health knowledge on COVID-19, the Chongqing Municipal Health Commission provided citizens with authoritative, detailed, and feasible family prevention and control guidelines to enhance self-protection awareness and ability and issued a manual about COVID-19 prevention and control knowledge to every household. An operation manual for the prevention and control of the epidemic in Chongqing listing 50 measures was formulated and distributed to all institutions of learning after the Spring Festival.
Conduct online work and online teaching. Many institutions and departments adopted “Chongqing Quick Handling”, an online work platform, to complete the entire process of handling approval matters online during the COVID-19 pandemic. Government agencies were encouraged to carry out work on the Internet, and schools were recommended to conduct online teaching to achieve the aim of “suspending classes but not stopping learning”.
Analysis of epidemic trend of COVID-19 in Chongqing
Characteristics of Chongqing: Chongqing is located in southwest China, bordering Hubei Province. It has 26 districts, 8 counties and 4 autonomous counties, with a total area of 82400 square kilometers. In 2019, the permanent population was 31243200, the urban population was 20869900 and the migrant population was 10280000.
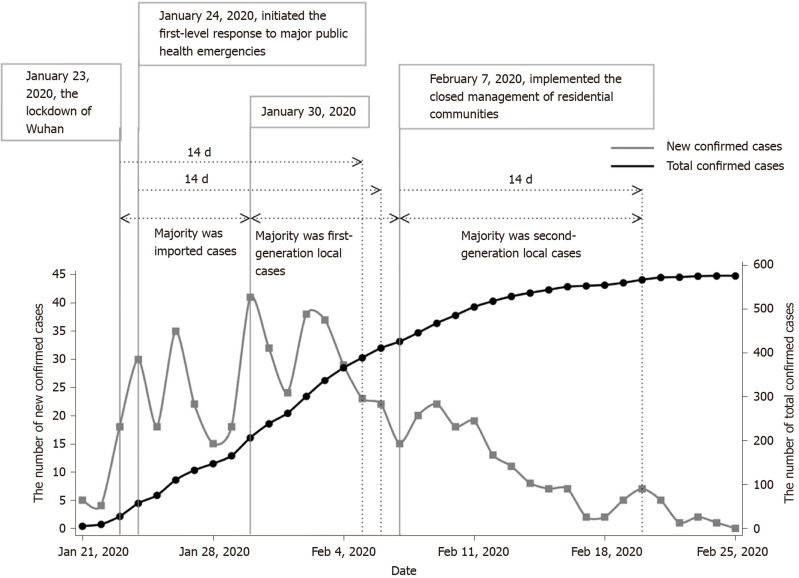
The numbers of new and total confirmed cases of COVID-19 in Chongqing were significantly related to prevention and control policies: The lockdown of Wuhan significantly affected the COVID-19 epidemic trend in Chongqing. From January 21 (5 new confirmed cases) to February 3 (37 new confirmed cases), the number of new confirmed cases of COVID-19 in Chongqing showed a daily rising trend. However, the number of new confirmed cases began to decline after February 5 (23 new confirmed cases), the 14th day after the lockdown of Wuhan and the end of the incubation period for cases imported from Hubei Province to Chongqing (Figure 1 and Table 1).
Figure 1.
Trends in the numbers of new confirmed cases and total confirmed cases of coronavirus disease 2019 in Chongqing. From February 25, 2020 to March 15, 2020, there were no new confirmed cases.
Table 1.
Number of confirmed cases from January 1 to March 15
| Date | New confirmed cases | Total confirmed cases |
| January 21-22 | 9 | 9 |
| January 23-291,2 | 156 | 165 |
| January 30-February 5 | 224 | 389 |
| February 6-123 | 129 | 518 |
| February 13-19 | 42 | 560 |
| February 20-26 | 16 | 576 |
| February 27-March 4 | 0 | 576 |
| March 5-11 | 0 | 576 |
| March 12-15 | 0 | 576 |
January 23, 2020: The lockdown of Wuhan.
January 24, 2020: Initiated the first-level response to major public health emergencies.
February 7, 2020: Implemented the closed management of residential communities.
Second, the implementation of the closed management of residential communities in Chongqing further effectively controlled the occurrence of new confirmed cases. After February 5 (23 new confirmed cases), new confirmed cases were mainly second-generation local cases. On February 7 (15 new confirmed cases), the Chongqing municipal government announced that it would impose closed management of residential communities throughout the city. After an average incubation period (7 d), the number of new confirmed cases dropped to 8 on February 14, and on February 18, the number dropped to 2 (Figure 1).
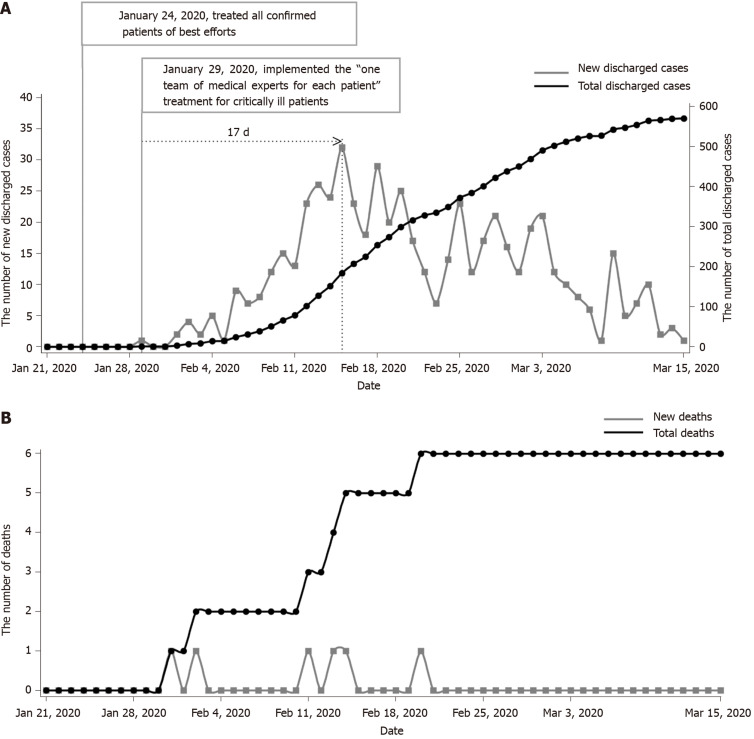
Designated medical institutions and organized teams of medical experts were appointed, and a “one team of medical experts for each patient” treatment plan for critically ill cases was implemented to improve the treatment effect: From January 29 (the first recovered case) to February 23 (335 discharged cases), the discharge rate of COVID-19 patients in Chongqing increased significantly to 58.26% (from 0.61%, P < 0.001) (Figure 2A and Table 2). From January 31 to February 22, there were 6 deaths (infection fatality rate: 0.42% to 1.05%, P = 0.380), and the number of deaths has not continued to increase (Figure 2B and Table 2). The infection fatality rate of COVID-19 in Chongqing was lower than that in Wuhan and several other provinces and cities, an outcome significantly related to the prevention and control measures implemented by designated medical institutions and the integration and distribution of medical resources by the government.
Figure 2.
Trends in the numbers of new discharged cases, total discharged cases, new deaths, and total deaths of coronavirus disease 2019 in Chongqing. A: Number of new discharged cases and total discharged cases of coronavirus disease 2019 (COVID-19); B: Number of new deaths and total deaths of COVID-19.
Table 2.
Numbers of deaths and discharged cases from January 1 to March 15
| Date | New deaths | Total deaths | New discharged cases | Total discharged cases |
| January 21-22 | 0 | 0 | 0 | 0 |
| January 23-291,2 | 0 | 0 | 1 | 1 |
| January 30- February 5 | 2 | 2 | 14 | 15 |
| February 6-12 | 1 | 3 | 87 | 102 |
| February 13-19 | 2 | 5 | 172 | 274 |
| February 20-26 | 1 | 6 | 110 | 384 |
| February 27- March 4 | 0 | 6 | 118 | 502 |
| March 5-11 | 0 | 6 | 52 | 554 |
| March 12-15 | 0 | 6 | 16 | 570 |
January 24, 2020: Treated all confirmed patients of best efforts.
January 29, 2020: Implemented the “one team of medical experts for each patient” treatment for critical patients.
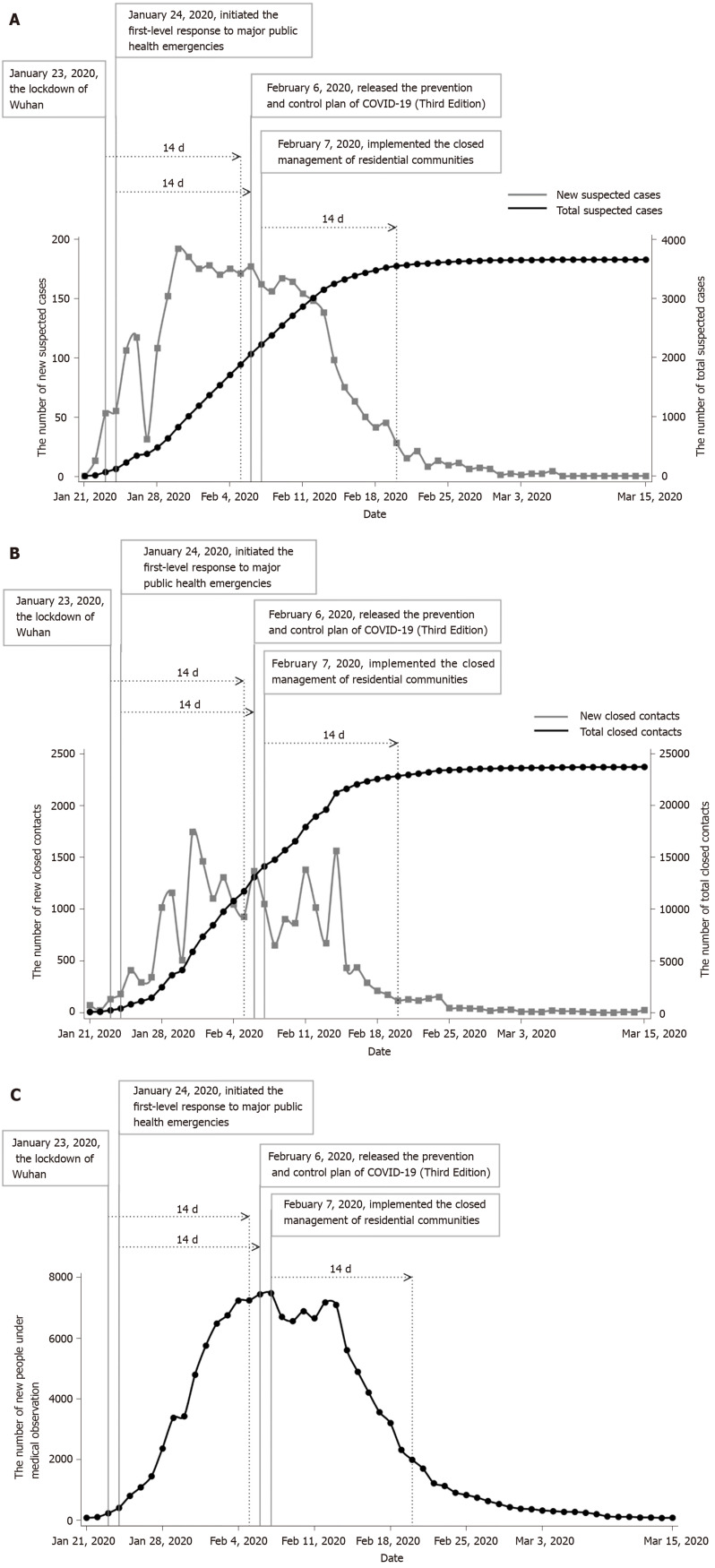
Prevention and control measures impacted the number of people under medical observation: From January 21 (72 new close contacts, 0 new suspected cases) to February 1 (1459 new close contacts, 175 new suspected cases), with the confirmation of the cases imported from Hubei Province and the development of epidemiological investigations, the number of new close contacts and suspected cases increased gradually and showed a certain downward trend by February 5 (924 new close contacts, 171 new suspected cases) (Figure 3A and 3B and Table 3). Eight days (February 15) after the implementation of the closed management of residential communities (starting on February 7), the number of new close contacts (431) decreased significantly and has remained at a low level since then [1743 (5.58/100000) vs 431 (1.38/100000), P < 0.001].
Figure 3.
Trends in the numbers of new suspected cases, total suspected cases, new close contacts, total close contacts, and people under medical observation for coronavirus disease 2019 in Chongqing. A: Numbers of new suspected cases and total suspected cases of coronavirus disease 2019 (COVID-19); B: Numbers of new close contacts and total close contacts of COVID-19; C: Number of people under medical observation for COVID-19. COVID-19: Coronavirus disease 2019.
Table 3.
Numbers of suspected cases, close contacts, and people under medical observation from January 1 to March 15
| Date | New suspected cases | Total suspected cases | New close contacts | Total close contacts | People under medical obeservation5 |
| January 21-22 | 13 | 13 | 94 | 94 | 83 |
| January 23-291,2 | 622 | 635 | 3525 | 3619 | 1381 |
| January 30-February 5 | 1246 | 1881 | 8081 | 11700 | 5949 |
| February 6-123,4 | 1128 | 3009 | 7225 | 18925 | 6980 |
| February 13-19 | 510 | 3519 | 3775 | 22700 | 4403 |
| February 20-26 | 105 | 3624 | 741 | 23441 | 1211 |
| February 27- March 4 | 25 | 3649 | 171 | 23612 | 416 |
| March 5-11 | 6 | 3655 | 69 | 23681 | 185 |
| March 12-15 | 0 | 3655 | 35 | 23716 | 77 |
January 23, 2020: The lockdown of Wuhan.
January 24, 2020: Initiated the first-level response to major public health emergencies.
February 6, 2020: Released the prevention and control plan of COVID-19 (Third Edition).
February 7, 2020: Implemented the closed management of residential communities.
Mean (weekly).
From the beginning of the lockdown of Wuhan to February 5, the number of people under medical observation increased significantly each day, and the number was 7239 on February 5. Seven days after the implementation of the closed management of residential communities [starting on February 7 (7474 people under medical observation)], the number of people under medical observation began to decline and reached 1120 on February 23 [7474 (23.92/100000) vs 1120 (3.59/100000), P < 0.001] (Figure 3C and Table 3).
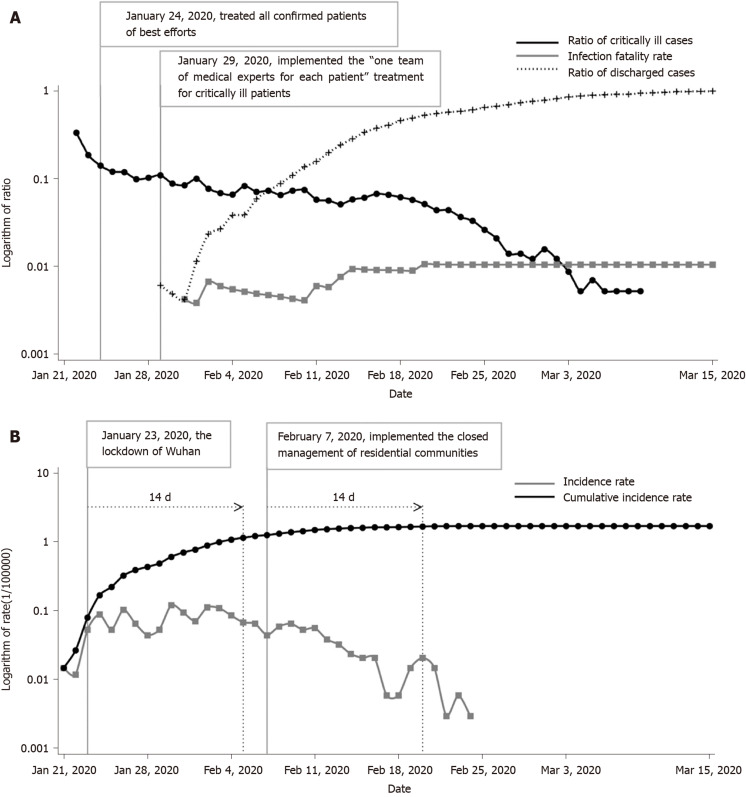
Trends in the COVID-19 incidence rate, cumulative incidence rate, and case ratio (deaths, discharged cases, and critically ill cases) in Chongqing: There were 2 critically ill patients for every 6 confirmed cases on January 22 in Chongqing, revealing a high ratio of critically ill cases. After the adoption of the “one team of medical experts for each patient” treatment plan for critically ill cases and the optimization of the allocation of medical resources and the diagnosis and treatment plan, the ratio of critically ill patients was well controlled and slowly decreased, the discharge rate increased rapidly each day, and the death rate was well controlled (Figure 4 and Table 4).
Figure 4.
Trends in the incidence rate, cumulative incidence rate, and ratio of deaths, discharged cases, and critically ill cases of coronavirus disease 2019 in Chongqing. A: Infection fatality rate and ratio of discharged cases and critically ill cases of coronavirus disease 2019 (COVID-19); B: Incidence rate and cumulative incidence rate of COVID-19.
Table 4.
Incidence rate, cumulative incidence rate, and ratio of deaths, discharged cases, and critically ill cases from January 1 to March 15
| Date | Infection fatality rate | Ratio of discharged cases | Ratio of critically ill cases3 | Incidence rate (1/100000) | Cumulative incidence (1/100000) |
| January 21-22 | 0.000 | 0.000 | 0.170 | 0.029 | 0.029 |
| January 23-291,2 | 0.000 | 0.006 | 0.120 | 0.499 | 0.528 |
| January 30- February 5 | 0.005 | 0.039 | 0.080 | 0.717 | 1.245 |
| February 6-12 | 0.006 | 0.197 | 0.070 | 0.413 | 1.658 |
| February 13-19 | 0.009 | 0.489 | 0.060 | 0.134 | 1.792 |
| February 20-26 | 0.010 | 0.667 | 0.040 | 0.051 | 1.844 |
| February 27-March 4 | 0.010 | 0.872 | 0.010 | 0.000 | 1.844 |
| March 5-11 | 0.010 | 0.962 | 0.000 | 0.000 | 1.844 |
| March 12-15 | 0.010 | 0.990 | 0.000 | 0.000 | 1.844 |
January 24, 2020: Treated all confirmed patients of best efforts.
January 29, 2020: implemented the “one team of medical experts for each patient” treatment plan for critical patients.
Mean (weekly).
As of February 23, the cumulative incidence of COVID-19 in Chongqing was 1.84/100000 (575 cases), and the infection fatality rate was 1.04% (6/575). The incidence rate continued to increase from January 21 to January 31 (5 (0.02/100000) vs 32 (0.10/100000), P < 0.001) and gradually declined after February 7 (32 (0.10/100000) vs 15 (0.07/100000), P = 0.013). The upward trend of cumulative incidence flattened out. After the closed management of residential communities was implemented (starting on February 15 (0.054/100000)), the incidence rate showed a more significant downward trend and fell to 0.006/100000 (P = 0.002) by February 18.
DISCUSSION
Our study first summarized the policies and measures implemented by the government in Chongqing for the prevention and control of COVID-19 in two domains. The first domain includes organization and management measures, and the second includes technical measures. Second, the policy impact on the epidemic trend of COVID-19 in Chongqing was analyzed. The results showed that the Chongqing municipal government adopted suitable policies and measures to prevent and control COVID-19, achieving remarkable effects.
Current studies on COVID-19 mainly focus on trend predictions[23], clinical diagnosis and treatment plans[24], prevention and containment measures[25], and social-psychological problems[26,27]. We found no related study on the effect of the prevention and containment measures taken by Chongqing to stop the local spread of COVID-19. Some studies[23,28] did note that the lockdown of Wuhan city could effectively reduce the potential peak number of COVID-19 infections and delay the time of peak infection. To prevent and control COVID-19, governments have not only learned from the experience of SARS prevention and control[23] but also adopted more powerful management and technical measures. In accordance with other studies[28,29], this study showed that through the strict lockdown of Wuhan and the quarantine measures adopted by Chongqing (such as the closed management of residential communities and “recurrent” and “one by one” inspections), the goal of “preventing the input of external cases and curbing the spread of local cases” was realized. The source of infection was controlled, and the transmission pathways were cut off quickly. Moreover, the number of close contacts and people under medical observation was reduced after 14 d of the closed management of residential communities, which saved a considerable amount of medical and social resources. Clearly, the number of new confirmed cases in Chongqing decreased significantly after the incubation period following the lockdown of Wuhan; this suggests that travel restrictions effectively controlled the spread of local cases in Chongqing, consistent with the results from Marino Gatto et al[30]. Other countries have also employed quarantine measures[30], but the pandemic was not controlled quickly in some countries[7,31], which may be due to differences in social distancing measures and China’s capacity to quickly build dedicated facilities.
The configuration of medical resources and measures is crucial for the prevention and control of COVID-19. A previous study[32] proposed that public health management measures and clinical diagnostic criteria for SARS should be formulated separately according to the different risk levels of pandemic and non-pandemic areas[33], which can contribute significantly to saving medical manpower and resources and financial resources. Similar to the prevention and treatment strategies used for SARS, the measures implemented in Chongqing (such as naming designated medical institutions and organizing medical expert teams, implementing a “one team of experts for each patient” treatment plan for critically ill cases, receiving and treating confirmed patients quickly, and optimizing the diagnosis and treatment plan continuously) significantly improved the cure rate and reduced the infection fatality rate of COVID-19. A study including 144 geopolitical areas worldwide found that public health interventions (restrictions on mass gatherings, school closures, and the implementation of social distancing measures) were strongly associated with reduced growth of the COVID-19 epidemic[18]. Similar to governments in other areas[34], the Chongqing government strengthened the infection management of hospitals to prevent nosocomial infections and ensure hospital staff members' safety. Moreover, health resources have inevitable impacts on the control and treatment of COVID-19. The Chinese government provided adequate health resources for fighting the COVID-19 pandemic and covered all medical costs associated with NAT, centralized isolation, and the care of suspected and confirmed cases. It also provided additional salary subsidies for medical staff participating in the prevention, control, and treatment of COVID-19, which ensured that every high-risk person and confirmed case could be effectively managed and treated and reduced the spread of infection. In contrast, there was not adequate health financing to prevent and constrain the COVID-19 epidemic in Iran[8], which caused the number of cases and deaths to progressively increase. In addition, the measures taken by the Chongqing government not only included the correct guidance of media publicity to instill a common understanding in the populace but also involved strengthening awareness of the law regarding the prevention and transmission containment to curb malicious manmade disease spread.
Based on the experience with SARS, the risk levels were adjusted accurately and dynamically according to the epidemic control scenarios in each district and county by the health management authority, which was remarkably effective in saving resources. The COVID-19 epidemic was dynamic and impacted by containment measures[35,36]; therefore, it was necessary that the strength of the containment measures be adjusted accordingly. For example, in low-risk areas, the main task was to prevent imported cases and gradually resume production under the condition of ensuring the health and safety of the people. This study showed that the various prevention and control policies and measures implemented by the authorities in Chongqing were significantly related to the local epidemic trend, which indicates that containment measures have had a significant effect on controlling the spread of the pandemic, improving the cure and recovery rate, and reducing the infection fatality rate. The prevention and control policies and measures implemented in Chongqing were under the guidance of the National Health Commission, and every province and municipality had its own method to implement the measures according to its conditions. Therefore, parts of the policy and measures have similarities among different provinces. In addition to describing the impact of the “lockdown of Wuhan” on the pandemic of COVID-19 in Chongqing, our study reviewed the policies and measures implemented in Chongqing, which represents a moderate epidemic area that is adjacent to the outbreak epicenter of COVID-19.
This study explored the impacts of some policies on controlling the COVID-19 epidemic. However, there are some limitations to this study. First, this study did not explore emergency networks combined with different institutes to respond to the control of emergent infectious diseases. Second, it did not examine medical insurance in the context of emergent infectious diseases.
Other areas and countries can learn much from the policies and containment measures decisively imposed by China and by the Chongqing municipal government to curb the spread of COVID-19. Our research can guide the development of emergency plans for infectious disease outbreaks, which should consider prevention and control policies and government measures. More scientific emergency plans for infectious diseases will be developed to predict the epidemic spread more precisely and guide medical institutions to make more effective preparations. The media can also guide the public through scientific predictions that account for the impact of policies and measures to prevent panic. These policies and measures provide a reference for the formulation of emergency prevention and control strategies for sudden outbreaks of infectious diseases of unknown origin and the development of related research.
ARTICLE HIGHLIGHTS
Research background
Since December 2019, a deadly emerging infectious disease called coronavirus disease 2019 (COVID-19) has rapidly spread from Wuhan (China), the outbreak epicenter, to more than 200 countries, territories, and areas. Several studies have considered the impact of the lockdown of Wuhan on the epidemic trend of COVID-19 but have not considered the effects of other prevention and control policies and measures. The prevention and control policies and measures implemented by the Chinese government controlled the pandemic as quickly as possible. These policies and measures can provide policy suggestions for other countries to curb the serious spread of COVID-19 and provide a theoretical basis for the prevention and control of emerging infectious diseases in the future.
Research motivation
This study analyzed the policies and control measures adopted by the government and medical institutions in Chongqing for the prevention and control of COVID-19 and explored the impact of the lockdown of Wuhan, the closed management of residential communities, and other relevant policy measures on the epidemic trend in Chongqing. Our results revealed that interdepartmental collaboration and medical insurance need to be further explored in future studies in the face of emergent infectious diseases of unknown etiologies.
Research objectives
This study aimed to analyze the policies and containment measures implemented by the Chongqing government and medical institutes in terms of the management and technical aspects and to explore the effects of different policies and containment measures on the control of the COVID-19 epidemic in Chongqing. This study will provide guidance for future research on emergent infectious diseases.
Research methods
Epidemiological data and survey of key people were used to conduct this study. Epidemiological data were collected from the official website of the Chongqing Municipal Health Commission from January 21, 2020 (the first date that a COVID-19 case was reported in Chongqing) to March 15, 2020 (when the epidemic was controlled). The management policy materials and their implementation dates for COVID-19 were collected from the official websites of the government and the Municipal Health Commission of Chongqing. In addition, some policy materials on implementation and containment measures were obtained by querying leaders and frontline workers at the CDC and local medical institutions. The epidemic trend of COVID-19 in Chongqing was analyzed by an experienced statistical analyst using SAS 9.4.
Research results
As of March 15, the cumulative incidence of COVID-19 in Chongqing was 1.84/100000 (576 cases), and the infection fatality rate was 1.04% (6/576). The spread of COVID-19 was controlled by effective policies that involved establishing a group for directing the COVID-19 epidemic control effort; strengthening guidance and supervision; ensuring the supply of daily necessities and medical supplies and equipment to residents; setting up designated hospitals; implementing legal measures; and enhancing health education. Medical techniques were implemented to improve the recovery rate and control the epidemic. Policies such as “the lockdown of Wuhan”, “initiating a first-level response to major public health emergencies”, and “implementing the closed management of residential communities” significantly curbed the spread of COVID-19. Optimizing the diagnosis process, shortening the diagnosis time, and constructing teams of clinical experts facilitated the provision of “one team of medical experts for each patient” treatment for severe cases, which significantly improved the recovery rate and reduced the infection fatality rate. This study did not explore interdepartmental collaboration between medical institutes and government authorities.
Research conclusions
The prevention policies and containment measures implemented by the government and medical institutions were highly effective in controlling the spread of the epidemic and increasing the recovery rate of COVID-19 patients. This study analyzed the policies and measures used to control the COVID-19 epidemic and found that it showed apparent effects in epidemic prevention and control. In conclusion, primary prevention policies and measures are effective in curbing emergent infectious diseases.
Research perspectives
This study explored the impact of some policies and measures on controlling the COVID-19 epidemic. Emergency networks combined with different institutes to control emergent infectious diseases should be explored in future studies. Medical insurance in the context of emergent infectious diseases also needs to be studied in the future.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the laboratory support of the Ministry of Education Key Laboratory of Child Development and Disorders.
Footnotes
Institutional review board statement: This study was approved by the Institutional Review Board of Chongqing Medical University.
Informed consent statement: Participants were informed about the plan about our study details. And if they agreed to participate in, written informed consent was obtained from each participant prior to their inclusion in the study.
Conflict-of-interest statement: The authors report no conflicts of interest.
Data sharing statement: Data are available from Xiao-Hua Liang (contact via xiaohualiang@hospital.cqmu.edu.cn or liangxiaohua666@sina.com).
STROBE statement: The authors have read the STROBE Statement checklist of items and prepared and revised the manuscript accordingly.
Manuscript source: Invited manuscript
Peer-review started: May 19, 2020
First decision: June 4, 2020
Article in press: June 29, 2020
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang L S-Editor: Ma YJ L-Editor: Wang TQ E-Editor: Liu JH
Contributor Information
Xiao-Hua Liang, Clinical Epidemiology and Biostatistics Department, Children’s Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, Key Laboratory of Pediatrics in Chongqing, China International Science and Technology Cooperation Center of Child Development and Critical Disorders, Chongqing 400014, China. xiaohualiang@hospital.cqmu.edu.cn.
Xian Tang, Clinical Epidemiology and Biostatistics Department, Children’s Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, Key Laboratory of Pediatrics in Chongqing, China International Science and Technology Cooperation Center of Child Development and Critical Disorders, Chongqing 400014, China.
Ye-Tao Luo, Clinical Epidemiology and Biostatistics Department, Children’s Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, Key Laboratory of Pediatrics in Chongqing, China International Science and Technology Cooperation Center of Child Development and Critical Disorders, Chongqing 400014, China.
Min Zhang, Clinical Epidemiology and Biostatistics Department, Children’s Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, Key Laboratory of Pediatrics in Chongqing, China International Science and Technology Cooperation Center of Child Development and Critical Disorders, Chongqing 400014, China.
Ze-Pei Feng, Clinical Epidemiology and Biostatistics Department, Children’s Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, Key Laboratory of Pediatrics in Chongqing, China International Science and Technology Cooperation Center of Child Development and Critical Disorders, Chongqing 400014, China.
References
- 1.Who Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus disease (COVID-19) pandemic. Available from: https://www.paho.org/en/topics/coronavirus-infections/coronavirus-disease-covid-19-pandemic.
- 4.Chan-Yeung M, Xu RH. SARS: epidemiology. Respirology. 2003;8 Suppl:S9–14. doi: 10.1046/j.1440-1843.2003.00518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVID-19 situation update worldwide, as of 27 June 2020. Available from: https://www.Ecdc.Europa.Eu/en/geographical-distribution-2019-ncov-cases.
- 6.Cohen J, Kupferschmidt K. Countries test tactics in 'war' against COVID-19. Science. 2020;367:1287–1288. doi: 10.1126/science.367.6484.1287. [DOI] [PubMed] [Google Scholar]
- 7.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Behzadifar M, Ghanbari MK, Bakhtiari A, Behzadifar M, Bragazzi NL. Ensuring adequate health financing to prevent and control the COVID-19 in Iran. Int J Equity Health. 2020;19:61. doi: 10.1186/s12939-020-01181-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kraemer MUG, Yang CH, Gutierrez B, Wu CH, Klein B, Pigott DM Open COVID-19 Data Working Group, du Plessis L, Faria NR, Li R, Hanage WP, Brownstein JS, Layan M, Vespignani A, Tian H, Dye C, Pybus OG, Scarpino SV. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fang Z, Yi F, Wu K, Lai X, Zhong N, Liu Z. Clinical characteristics of coronavirus pneumonia 2019 (covid-19): An updated systematic review. medRxiv 2020. [Google Scholar]
- 13.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, Zhang LJ. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020:200490. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Dupont HT, Honoré S, Colson P, Chabrière E, La Scola B, Rolain JM, Brouqui P, Raoult D. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020:Online ahead of print. doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jüni P, Rothenbühler M, Bobos P, Thorpe KE, da Costa BR, Fisman DN, Slutsky AS, Gesink D. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ. 2020;192:E566–E573. doi: 10.1503/cmaj.200920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roosa K, Lee Y, Luo R, Kirpich A, Rothenberg R, Hyman JM, Yan P, Chowell G. Real-time forecasts of the COVID-19 epidemic in China from February 5th to February 24th, 2020. Infect Dis Model. 2020;5:256–263. doi: 10.1016/j.idm.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang S, Cao P, Du P, Wu Z, Zhuang Z, Yang L, Yu X, Zhou Q, Feng X, Wang X, Li W, Liu E, Chen J, Chen Y, He D. Early estimation of the case fatality rate of COVID-19 in mainland China: a data-driven analysis. Ann Transl Med. 2020;8:128. doi: 10.21037/atm.2020.02.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang B, Bragazzi NL, Li Q, Tang S, Xiao Y, Wu J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov) Infect Dis Model. 2020;5:248–255. doi: 10.1016/j.idm.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang B, Wang X, Li Q, Bragazzi NL, Tang S, Xiao Y, Wu J. Estimation of the Transmission Risk of the 2019-nCoV and Its Implication for Public Health Interventions. J Clin Med. 2020;9 doi: 10.3390/jcm9020462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hou C, Chen J, Zhou Y, Hua L, Yuan J, He S, Guo Y, Zhang S, Jia Q, Zhao C, Zhang J, Xu G, Jia E. The effectiveness of quarantine of Wuhan city against the Corona Virus Disease 2019 (COVID-19): A well-mixed SEIR model analysis. J Med Virol. 2020;92:841–848. doi: 10.1002/jmv.25827. [DOI] [PubMed] [Google Scholar]
- 24.Chan JF, Yip CC, To KK, Tang TH, Wong SC, Leung KH, Fung AY, Ng AC, Zou Z, Tsoi HW, Choi GK, Tam AR, Cheng VC, Chan KH, Tsang OT, Yuen KY. Improved Molecular Diagnosis of COVID-19 by the Novel, Highly Sensitive and Specific COVID-19-RdRp/Hel Real-Time Reverse Transcription-PCR Assay Validated In Vitro and with Clinical Specimens. J Clin Microbiol. 2020;58 doi: 10.1128/JCM.00310-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92:568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, Du H, Li R, Kang L, Su M, Zhang J, Liu Z, Zhang B. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Front Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, Mei S. The Effect of COVID-19 on Youth Mental Health. Psychiatr Q. 2020 doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang Z, Zeng Z, Wang K, Wong SS, Liang W, Zanin M, Liu P, Cao X, Gao Z, Mai Z, Liang J, Liu X, Li S, Li Y, Ye F, Guan W, Yang Y, Li F, Luo S, Xie Y, Liu B, Wang Z, Zhang S, Wang Y, Zhong N, He J. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J Thorac Dis. 2020;12:165–174. doi: 10.21037/jtd.2020.02.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, Pastore Y Piontti A, Mu K, Rossi L, Sun K, Viboud C, Xiong X, Yu H, Halloran ME, Longini IM, Jr, Vespignani A. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Basu A. Estimating The Infection Fatality Rate Among Symptomatic COVID-19 Cases In The United States. Health Aff (Millwood) 2020:101377hlthaff202000455. doi: 10.1377/hlthaff.2020.00455. [DOI] [PubMed] [Google Scholar]
- 32.Lipsitch M, Cohen T, Cooper B, Robins JM, Ma S, James L, Gopalakrishna G, Chew SK, Tan CC, Samore MH, Fisman D, Murray M. Transmission dynamics and control of severe acute respiratory syndrome. Science. 2003;300:1966–1970. doi: 10.1126/science.1086616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zeng G. Some problems about sars prevention and control. Zhonghua Jibing Kongzhi Zazhi. 2003;3:164–167. [Google Scholar]
- 34.Chang YT, Lin CY, Tsai MJ, Hung CT, Hsu CW, Lu PL, Hou MF. Infection control measures of a Taiwanese hospital to confront the COVID-19 pandemic. Kaohsiung J Med Sci. 2020;36:296–304. doi: 10.1002/kjm2.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shi P, Dong Y, Yan H, Zhao C, Li X, Liu W, He M, Tang S, Xi S. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci Total Environ. 2020;728:138890. doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gatto M, Bertuzzo E, Mari L, Miccoli S, Carraro L, Casagrandi R, Rinaldo A. Spread and dynamics of the COVID-19 epidemic in Italy: Effects of emergency containment measures. Proc Natl Acad Sci USA. 2020;117:10484–10491. doi: 10.1073/pnas.2004978117. [DOI] [PMC free article] [PubMed] [Google Scholar]