Abstract
BACKGROUND:
Enteral tubes are prevalent among children with medical complexity (CMC), and complications can lead to costly health care use. Our objective was to design and test the usability of a mobile application (app) to support family-delivered enteral tube care.
METHODS:
Human-centered design methods (affinity diagramming, persona development, and software development) were applied with family caregivers of CMC to develop a prototype. During 3 waves of usability testing with design refinement between waves, screen capture software collected user-app interactions and inductive content analysis of narrative feedback identified areas for design improvement. The National Aeronautics and Space Administration Task Load Index and the System Usability Scale quantified mental workload and ease of use.
RESULTS:
Design participants identified core app functions, including displaying care routines, reminders, tracking inventory and health data, caregiver communication, and troubleshooting. Usability testing participants were 80% non-Hispanic white, 28% lived in rural settings, and 20% had not completed high school. Median years providing enteral care was 2 (range 1–14). Design iterations improved app function, simplification, and user experience. The mean System Usability Scale score was 76, indicating above-average usability. National Aeronautics and Space Administration Task Load Index revealed low mental demand, frustration, and effort. All 14 participants reported that they would recommend the app, and that the app would help with organization, communication, and caregiver transitions.
CONCLUSIONS:
Using a human-centered codesign process, we created a highly usable mobile application to support enteral tube caregiving at home. Future work involves evaluating the feasibility of longitudinal use and effectiveness in improving self-efficacy and reduce device complications.
Children with medical complexity (CMC) often have chronic conditions requiring medical devices to assist or replace impaired body functions.1 One of the most frequently used devices by CMC is an enteral tube (eg, gastrostomy, gastrojejunostomy) to deliver nutrition, hydration, and medications.2 Many family caregivers report they are underprepared and undersupported to deliver enteral care at home.3–5 Beyond the device itself, enteral care requires families to manage supply inventory, nutrition routines, and medication administration; coordinate information transfer among different caregivers and longitudinal clinical appointments; and troubleshoot tube complications.6,7 Although enteral tubes provide life-sustaining treatment, they simultaneously introduce care demands that can influence family outcomes, such as increased care burden, social isolation, stigma, and loss of normalcy.3–5,8–10
The complex nature of enteral tube care also introduces complication risk. Complications include stomal problems (skin and mucosal irritation, infections, bleeding, etc); tube breakage, leakage, obstruction, and dislodgement; and errors related to nutrition, hydration, or medication delivery, any of which can lead to potentially avoidable emergency department (ED) visits and/or hospitalizations.11 As such, enteral tube complications can make up a sizable proportion of overall ED and hospital use experienced by CMC.2,12
Mobile health (mHealth) and mobile applications (apps) have the potential to support CMC enteral tube care, prevent complications, and improve child and family outcomes by serving as a portable resource and organizational tool to improve collaborative symptom tracking, monitoring, and management of chronic conditions and improve caregiver communication.13–15 Although apps to support caregiving exist, most are designed to support patients with less complex conditions (eg, asthma, diabetes), and their impact on health outcomes is poorly understood.16–18 Our objective for this study was to use human-centered design to create and test the usability of a mobile app to support family-delivered enteral tube care for CMC at home.
Methods
Setting and Sample
Our study population included family caregivers of CMC who used enteral tubes and were enrolled in the Pediatric Complex Care Program (PCCP) at a tertiary academic children’s hospital in the Midwest. The PCCP provides outpatient and inpatient medical management and care coordination for CMC who have chronic conditions affecting ≥3 organ systems, who receive ongoing care from ≥3 medical or surgical specialists, and who experienced either ≥5 days of hospitalization or ≥10 specialty clinic visits in the year before referral. The PCCP team includes general pediatricians, advanced practice providers, registered nurses, care coordinators, nutritionists, and a social worker. The team provides inpatient and outpatient care, 24 hour/day availability, and comprehensive care planning to enrolled CMC.
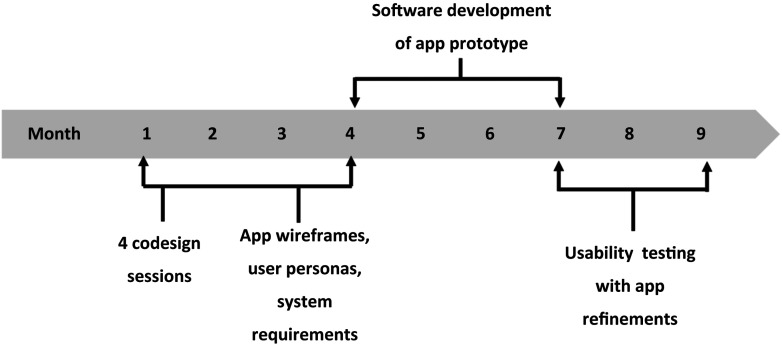
Participants were English-speaking family caregivers of CMC enrolled in the PCCP who were at least 18 years of age, cared for a child with an enteral tube, and lived within 1 hour of the institution. Purposive recruitment was used to enroll participants with varying education levels, urban and rural households, and duration of experience of caring for a child with an enteral tube. Families participating in codesign sessions were different from those participating in usability testing. A schematic of the study activities is provided in Fig 1. This study was approved by the university’s institutional review board.
FIGURE 1.
Sequence of study activities to design and test an enteral tube caregiving app.
Overview
We used a 2-stage process to design the app. In the first stage, we conducted a participatory codesign process19–27 in which we collaborated with family caregivers to design and develop the app prototype. Next, we conducted 3 waves of usability testing to further refine the prototype. We describe each of these stages in detail in the following sections.
Codesign Sessions: Data Collection and Analysis
Four codesign sessions with family caregivers were conducted at 2- to 3-week intervals, with research team meetings after each codesign session. Research team members (N = 8) included 3 human-centered design experts, a PCCP nurse, 2 PCCP pediatricians, a professional family advocate for CMC, and a parent of a CMC. The research team’s role was to facilitate codesign sessions, synthesize ideas proposed by the design session participants, and create digital mock-ups of the app for discussion. At each codesign session, 2 research team members facilitated discussion and activities. The first codesign session involved a discussion of the broad vision of the app,28 the reason for focusing on enteral care; preliminary results from previously conducted in-home interviews with family caregivers of CMC; and an enteral care support needs assessment previously completed with PCCP family caregivers. The sessions began with participants identifying the overall purpose of the app, followed by discussion and affinity diagramming to identify the core app functions. Subsequent codesign sessions were focused on identifying and describing the app user groups and the desired interface features.
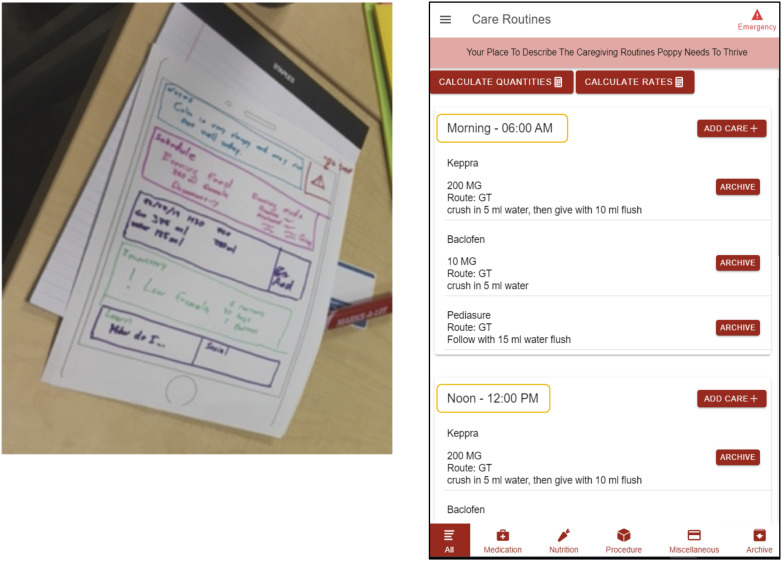
Codesign session data included Post-it Note groupings generated by family caregiver participants during session activities, session audio recordings, research team observation notes, design participant notes, and paper prototypes. The human-centered design experts analyzed data during and between sessions (eg, affinity diagramming) such that each subsequent session built on the findings from the previous session. For example, paper prototypes created by participants in session 2 were transformed into wireframes (ie, digital designs synthesizing the paper prototypes) between sessions. These wireframes were then discussed in codesign session 3. We used personas29,30 to define and iteratively refine user groups from codesign session discussions. Consensus-seeking discussion of the data with the research team helped finalize the overall app purpose, functions, and system requirements (Fig 2, Supplemental Fig 4). On the basis of these results, a fully functioning app prototype was built by a third-party app developer for usability testing and iterative refinement.
FIGURE 2.
Parent design concept and corresponding enteral tube caregiving app screenshot. GT, gastrostomy tube.
Usability Testing
Data Collection
Family caregivers participated in 3 waves of usability testing on iPads, with prototype design refinement occurring between waves. Although we could conduct usability on any device (phone, computer, tablet), we chose a department-owned iPad to keep the technology experience consistent across participants and to enable screen recording.
A subset of the 14 caregivers participated in each wave of testing, with later waves containing a larger number of participants. Testing sessions lasted 2 hours, involved a single caregiver, and were facilitated by 2 research team members. We used task-based protocols to measure the performance of each prototype function, and screen capture software collected on-screen gestures for the performance analysis. Across the 3 waves, we focused on tasks that represented key app functionality, such as account creation and login, adding users to the app, adding and updating care routines and nutrition information, and communicating through the note function.
For each session, the participant was provided minimal overview of the app before beginning testing, advised that the facilitators would be taking notes but not providing any assistance, and then prompted to begin the tasks. To ensure privacy, all participants were provided fictional child information and data to use during testing sessions. The fictional child data were developed by using codesign session information and research team input to ensure that the description and data accurately represented CMC who use enteral tubes. If needed, additional tasks were added during testing waves to reflect feature or functionality refinement. The narrative feedback portion began with participants commenting broadly on their experience using the app. Participants then responded to prompts (including describing areas of confusion or frustration, desired features not in the app, whether they would use the app or recommend it to a friend, and how they see the app assisting caregiving) and provided additional suggestions for refinement.
After testing and feedback sessions, we administered the System Usability Scale (SUS) and National Aeronautics and Space Administration Task Load Index (NASA TLX) to quantify participant experience of ease of use and mental workload of the entire app experience, respectively. The SUS evaluates ease of use (ie, usability) by posing a series of 10 statements suggesting high usability (“I think that I would like to use this app frequently” or “I thought this app was easy to use”) and low usability (“I thought there was too much inconsistency in this app” or “I found this app unnecessarily complex”). Participants rated the degree to which they agreed or disagreed with each statement, which was then represented as a numerical score from 1 to 5. Individual participant SUS scores were then combined and transformed to calculate an overall usability score, which could range from 0 to 100. High scores represent high usability, whereas low scores represent low usability. The NASA TLX evaluates mental workload on the basis of 6 dimensions: mental demand, physical demand, performance, effort, and frustration. Each component was rated by participants on a scale of 0 (low workload) to 100 (high workload) and then averaged to produce an overall score.
Data Analysis
Using screen capture software, we calculated time on task for each task performed and the total number of prolonged pauses (eg, >10 seconds), indicating a participant’s progress had halted. Narrative feedback was inductively analyzed to identify areas of confusion, opportunities for refinement, and potential benefits of the app. Between testing waves, participant performance, narrative feedback, and facilitator notes were qualitatively synthesized by using a team-based consensus approach to identify areas for refinement, such as function layout and ease of use. Refinement data were then incorporated into app development continuously throughout the study. SUS and NASA TLX scores were summarized with descriptive statistics.
Results
Codesign Sessions Results
Codesign session participants (N = 5) were 60% women who provided enteral care for a mean of 5 (range 1–13) years.
Overall Purpose of the App
Design session participants determined that the app’s overall purpose was to centralize and coordinate all aspects of enteral tube care, such as daily routines, medications and dosages, inventory, relevant data logs, individuals involved in enteral tube care, and tube troubleshooting. Participants identified facilitating communication among different caregivers and caregiver handoffs as key to the app’s overall functionality.
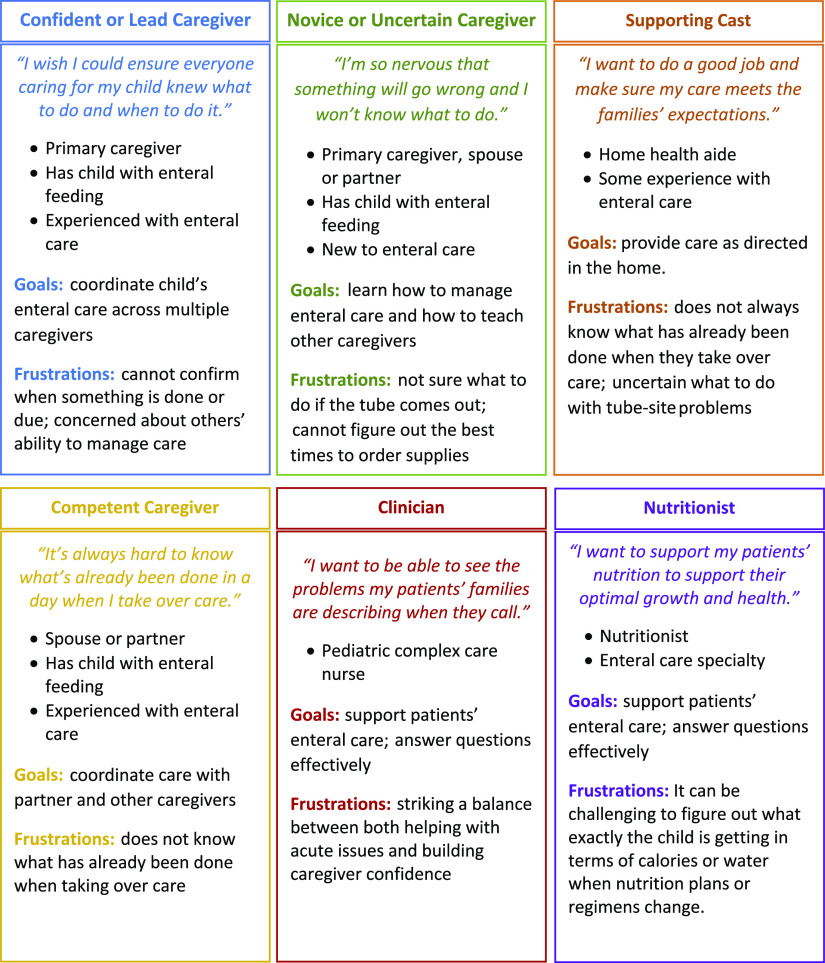
Target User Groups and Personas
Target users of the app included all individuals who provided care to the child in the home and community. Examples included family members, home health aides, and school nurses. Although the clinical team was not considered an app user, per se, family caregivers envisioned sharing exported data with their child’s clinicians. Participants also pointed to the possibility of CMC themselves using a future version of the app. User personas (Fig 3) were created for each user group, highlighting goals of use and current pain points. Personas were used to guide the design of system requirements to account for the spectrum of enteral care experiences and personal user goals, including customizability to appropriately support each caregiver.
FIGURE 3.
User personas emerging through enteral tube caregiving app codesign sessions.
Functions and System Requirements
Design session participants identified 9 key system requirements (Table 1): (1) a homepage where caregivers could view a synthesized summary of upcoming cares, view relevant alerts, and view or create handoff notes; (2) a child profile to indicate key information about the child and their tube; (3) network management to view and manage other app users; (4) a nutrition plan in which the child’s hydration and calorie goals, formula or recipe information, and sick day plans could be housed; (5) a care routines function to organize cares by time of day, to detail specific instructions (eg, food mixing or tube flushing instructions), to mark cares as completed, and to receive reminders about missed cares; (6) an inventory management function to track medical equipment (eg, syringes, tubing, food and formula, medications) and set reminders to reorder supplies or change the tube; (7) a tracking function to monitor clinical indicators over time; (8) crisis planning with directions on handling tube-related emergencies; and (9) general information and troubleshooting about enteral care and addressing common tube problems.
TABLE 1.
Enteral Tube Caregiving App Functions and System Requirements
| Key Function | Description | Purpose | Functional Requirements |
|---|---|---|---|
| Home page (with notes) | The main page of the app where users can view the current care situation | Promote situation awareness around the child and associated care needs | View care routines that need to be done today, receive alerts when a care is completed or overdue, receive inventory alerts (eg, reorder), write and view simple note handoffs |
| Child profile | App page with details about the child | Provide users with essential information to understand and support the child | Record important information about what makes the child who they are (eg, comfort measures, needs, likes), record tube details (eg, size, length, frequency of changes, date of original placement), include image of the child |
| Network management | App function that allows primary user to manage members of the child’s caregiving network | Manage user information and app access | Invite other users to use the app, remove users from the app, view app users and their contact details |
| Nutrition plan | App page focused on all aspects of the child’s nutrition plan | Ensure child receives appropriate and timely nutrition care | Enter meal schedules throughout the day, including formulas, foods, water, and supplements; document child’s daily recipes and regimens; calculate rates and volumes with a simple calculator; indicate child’s sick day nutrition and hydration plans |
| Routines (scheduling) | App page focused on creating schedules for all care | Facilitate continuity and accuracy of care | Create and maintain schedules for what care to do when, labeled and organized by caregiver (user) preference; view when foods, medications, or procedures are due and completed; log when foods, medications, or procedures are completed; set reminders or alarms to distinguish when a care is due or overdue |
| Inventory management | App page that serves as a hub for all inventory-related functions | Streamline inventory management activities | Track medications, supplies, and suppliers; facilitate refill or reorder of supplies |
| Tracking | App page that allows users to create trackers for various clinical indicators | Ability to monitor child health daily and over time | Use standard or create custom trackers for clinical indicators (eg, wt, blood pressure, bowel movements), record clinical indicators and view data over time, automated tracking of nutrition and water intake, connect tracked data to other app functions (eg, prompt water intake) |
| Crisis plans | App page that has specific details for crisis situations | Ensure all caregivers have access to emergency information | Provide direction for common enteral tube–related emergencies (eg, dislodgement, obstruction, infection, etc) |
| Trouble shooting and general information | App page to access tutorials for general information on enteral care and troubleshooting tutorials | Provide all caregivers with basic enteral tube information and support for common challenges | Review basics of enteral tube functions through training tutorials, view videos on troubleshooting common problems or managing equipment |
Usability Testing Results
Usability testing participants (N = 14) were primarily women (86%), 93% white, and 7% non-Hispanic African American. More than one-quarter (28%) lived in rural settings. Participants provided enteral care for a mean of 2 (range 1–14) years (Table 2). These family caregivers were different from those participating in codesign sessions.
TABLE 2.
Usability Testing Participant Characteristics
| N = 14 | |
|---|---|
| Women, % | 86 |
| Age, median (range), y | 38 (28–50) |
| Parent race and ethnicity, % | |
| White, non-Hispanic | 93 |
| African American, non-Hispanic | 7 |
| Child race and ethnicity, % | |
| White, non-Hispanic | 86 |
| African American, non-Hispanic | 7 |
| Hispanic | 7 |
| Urban or rural, % | |
| Urban | 72 |
| Rural | 28 |
| Primary insurance of CMC, % | |
| Public | 100 |
| Private | 0 |
| Highest education, % | |
| High school degree or GED | 21 |
| Some college | 7 |
| Associate degree | 21 |
| Apprenticeship or technical college | 7 |
| College or graduate degree | 44 |
| Enteral tube caregiving duration, median (range), y | 2 (1–14) |
GED, general equivalency diploma.
Task Performance
Time on tasks varied across usability participants, but the average time on tasks decreased across waves (Table 3). For some tasks, such as adding a new food, app refinement between waves resulted in shorter times to complete the task in subsequent waves. For others, such as adding a medication to the inventory or setting up routines, the time on task was relatively stable. The overall number of pauses during tasks decreased across waves, suggesting usability improvements (Table 3).
TABLE 3.
Task Completion, Mental Workload, and Ease of Use During App Usability Testing: Task Completion and Pauses
| Example Tasks | Time on Task, Mean (Range), min | ||
|---|---|---|---|
| Wave 1 (n = 2) | Wave 2 (n = 7) | Wave 3 (n = 5) | |
| Create an account | 7.0 (6.1–7.8) | 3.3 (1.5–4.3) | 2.4 (1.2–3.0) |
| Child profile, complete setup | 3.3 (3.2–3.4) | 2.3 (1.2–3.5) | 0.7 (0.4–1.1) |
| Nutrition plan, add a new food | 6.8 (6.1–7.4) | 3.5 (1.1–7.4) | 3.8 (2.1–5.5) |
| Routines, setup | 1.7 (1.2–2.1) | 2.4 (0.3–4.6) | 1.8 (0.5–4.0) |
| Routines, add a new medicine | 1.6 (1.5–1.6) | 2.0 (0.5–3.0) | 3.1 (1.3–5.5) |
| Inventory, add a new medicine | 3.7 (2.5–4.9) | 3.5 (1.7–6.2) | 4.0 (3.0–5.1) |
| Add a note | 0.8 (0.5–1.1) | 0.7 (0.1–2.5) | 0.4 (0.2–0.5) |
| Pauses >10 s | 10.5 (9–12) | 5.8 (2–17) | 4.5 (0–13) |
Narrative Feedback
Common themes included perceived benefits of the app, such as providing flexibility to manage time and cares, as well as confidence and peace of mind in terms of teaching and providing other caregivers with essential information regarding the child. Participants also felt that the app could facilitate care transitions by supporting intercaregiver communication and accurate documentation of cares. Additional perceived benefits included simplification and consolidation of routines into 1 accessible location and reduction of human errors, such as missed or duplicate medication administrations. Participants also appreciated the incorporation of child-centered language, supporting the child as a person and not a diagnosis. Areas identified for refinement included enhancing data tracking features and building a data export feature, organizing notes, personalizing the child profile to customize the information displayed, and including a list of community resources available to caregivers to support their child and family (Table 4). All usability participants reported that they would recommend the app to a friend, and 78.5% reported that they would use the app in its current state. Of those who reported that they would not use the app in its current state, 1 participant said they would use it only for certain circumstances, such as care handoffs. Others reported that they would have used the app if they had it when their child first got an enteral tube.
TABLE 4.
Themes From Narrative Evaluation During Usability Testing
| Example Quote | |
|---|---|
| Benefits of the app | |
| Gives parents flexibility to manage time and cares | “We’ve never been apart from her for more than 12 hours in 16 years.… The knowledge that—and ability to get feedback on—she was seeing all her tasks met would be really helpful and make us feel a whole lot better.” |
| Provides confidence and peace of mind | “You don’t always teach people the one-off scenarios. So being able to have that already in there for [other caregivers] to feel confident to do it and us having the peace of mind.” |
| Simplifies life and reduces error | “It’s a one-stop…one area where they can have all this information…and that can make life simpler and cut down on human errors—between caregivers and spouses.” |
| Supports the child as a person and not just a diagnosis | “I love the ‘best way to communicate with me, comfort measures’…I like the humanity in ‘I am calmed by, I am upset by.’ This is a person, an individual, not a diagnosis, not a disability.” |
| Areas for app refinement | |
| Customizing the tracking and reporting of relevant health information | “See some longitudinal data, graphing…what was her calorie intake over the last 2 weeks.… Being able to do some quick-view reporting or some sort of reporting function.” |
| Organizing and editing notes | “If you’re starting to write a note, and then you get sidetracked, and then it gets submitted but it actually didn’t happen. That would be nice to be able to go back.” |
| Personalizing information in the child profile | “I would put emergency protocol…or heads up about my [child’s conditions].… So you probably want that in there somewhere.” |
| Including an area highlighting resources for family caregivers | “If my kid’s [device] is wonky, who could they call.… What’s community resources, what’s out there in the world…even if you could put down [that] these people have resources for you.” |
Usability and Mental Workload
The average SUS scores, presented as mean (range), were as follows: wave 1, 72.5 (70.0–75.0); wave 2, 76.1 (62.5–92.5); and wave 3, 76.0 (60.0–100.0). An SUS score of 70 indicates average usability,31 and a score of ∼75 is comparable with that of Microsoft PowerPoint, Microsoft Word, and Nintendo Wii.32 The average NASA TLX scores, presented as mean (range), were as follows: wave 1, 33.8 (29.2–38.3); wave 2, 23.8 (5.0–37.5); and wave 3, 31.7 (20.8–46.7); these scores indicated an overall low mental workload required to use the app (Table 5).
TABLE 5.
Task Completion, Mental Workload, and Ease of Use During App Usability Testing: SUS and NASA TLX Scores
| Usability Measure | Wave 1 (n = 2) | Wave 2 (n = 7) | Wave 3 (n = 5) |
|---|---|---|---|
| SUS, mean (range) | 72.5 (70.0–75.0) | 76.1 (62.5–92.5) | 76 (60.0–100.0) |
| NASA TLX, mean (range) | 33.8 (29.2–38.3) | 23.8 (5.0–37.5) | 31.7 (20.8–46.7) |
In the SUS, participants rate the degree to which they agree or disagree with each of 10 statements. Scores are aggregated and transformed into a total score from 0 (low usability) to 100 (high usability). In the NASA TLX, participants evaluate mental workload in 6 dimensions (mental demand, physical demand, temporal demand, performance, effort, and frustration.) Scores are aggregated and transformed into a total score from 0 (low workload) to 100 (high workload).
Discussion
Using a human-centered, iterative codesign process, family caregivers created a highly usable app to support enteral tube caregiving at home. Although we focused on enteral tube care, it was striking that the system requirements were expansive and extended naturally beyond enteral care. An important implication is that despite rationally attempting to design interventions to support caregivers of CMC by focusing on feasible and discrete processes (eg, enteral tube care), it is unclear whether that can realistically be accomplished. For example, families readily considered enteral care routines and inventory management to account for all caregiving routines, supplies, and medications. From the perspective of family caregivers, focusing on a single aspect of care may be difficult without considering its relation to most, if not all, other aspects of caregiving. This observation is consistent with a recent study in which the authors concluded that existing apps may target management of one condition or disease, yet the reality of multisystem health problems requires technology that can holistically manage and track all conditions.33
The diversity of user personas identified during codesign sessions illustrates the demand placed on family caregivers to coordinate care delivery across diverse caregiver experiences and needs. This further underscores the likely necessity for mHealth solutions for CMC caregivers to maintain a comprehensive approach. Accounting for the interrelated nature of CMC caregiving tasks and diverse users poses unique challenges and opportunities. Ongoing mHealth design work should acknowledge that (1) caregiving needs may be incompletely met if related caregiving tasks are not simultaneously addressed, (2) mHealth adoption is likely to be influenced by the ability to design to meet the needs of all user groups, and (3) sustained use may suffer if the app is too narrow or offers only limited self-management support.34
Family identification of the app’s primary purpose to centralize and coordinate their enteral tube care highlights this as an important unmet need, which we hypothesize directly influences key health outcomes.12 For example, previously described enteral tube caregiving challenges include heightened anxiety, isolation, family strain, and financial distress, among others.3–5,8–10 Because family caregivers described the app’s potential to decrease caregiving workload, reduce care delivery errors, and improve quality of life, future efficacy studies should be conducted to assess the app’s ability to influence these specific outcomes. We also suspect that unmet needs explains how enteral tube complications can drive a sizable proportion of CMC ED and hospital use.12 If this app succeeds in meeting caregivers’ unmet needs, it is plausible to expect these outcomes to improve. In one of few pediatric chronic illness studies examining the influence of app use on health services use, the asthma self-management app by Nkoy et al35 was associated with improvements in quality of life, asthma control, and missed school or work and also reduced ED and hospital use. In addition, a recent meta-analysis highlights the promise of pediatric mHealth interventions to positively influence a wide array of child and family outcomes.36
A small number of studies have highlighted the potential for mobile technology to enhance CMC care. For example, shared care plans can facilitate communication among care providers and family caregivers.37,38 High degrees of usability and personalization are important for sustained engagement with apps that track chronic disease.39,40 Desai et al41 recently described design requirements for cloud-based shared care plans for CMC. Despite differences in scope, our studies have several similarities, including the need for cloud-based accessibility, alerts, collaboration among multiple users, and tailoring to the specific user. Hilliard et al42 explored user preferences and design recommendations for a self-management app for people with cystic fibrosis (CF). Consistent with our results, they underscored the value of involving individuals with CF at all design stages and emphasized the desire for multiple (rather than single) functions, specification to CF, minimal user burden, automation of self-management, and customization to user needs.
Notably, family caregivers prioritized the functions described in this study higher than facilitating communication directly with their clinical team, which differs from some studies.42,43 In another study exploring design requirements for mHealth CMC home monitoring, families identified real-time and direct access to the health care team as essential.44 One reason for this distinction may be that the home monitoring design work was linked more directly toward preventing ED or hospital visits, whereas our app’s primary objective was to support enteral tube care delivery at home (and we hypothesize that this will prevent ED visits and hospitalizations). If we had framed our objective differently, families may have prioritized direct clinical access higher. We also speculate that lower priority for direct ties to the clinical team could reflect their desire for privacy or their perception of limited clinician availability or that alternatives, such as electronic patient portals, already meet this need. Because these children were enrolled in a complex care program, it is possible that their caregivers feel they have unique access to their clinical team. Family caregivers did identify the value of connecting the app data to the electronic health record and exporting information from the app into a shareable format for their clinical teams, perhaps reflecting their interest in transparency while still controlling the manner and tempo at which information is shared. In future research, it would be useful to evaluate how families use the app to transfer information among themselves and their inpatient and outpatient providers.
This work is a first step in a broader effort to design a platform to support caregiving for CMC at home. The next steps include conducting feasibility studies in which families are given the app to use longitudinally in their typical caregiving setting. After further refinement of the app’s features and after introducing a capacity for electronic health record integration, we will adapt the platform to address high-priority challenges identified by CMC families (eg, care for other devices and diagnoses).
Our findings should be interpreted with certain limitations in mind. The study took place within a complex care program at a single institution; thus, family caregiver perceptions may not be generalizable to other settings. Although recruitment was diverse in many respects (education, rurality, duration of care for an enteral tube), participants were predominantly non-Hispanic white mothers. Refining this work with participants from different backgrounds and caregiving roles is a focus of future work and has the potential to increase generalizability. This app was designed as a prototype, and we were unable to develop all levels of possible functionality. Finally, this study’s focus was inherently on design and usability, and we did not evaluate longitudinal use of the app or the influence of its use on outcomes.
Despite these limitations, in our study, we describe the broad unmet care coordination and communication needs of family caregivers delivering enteral tube care to CMC. Through a user-centered design process aimed at addressing those needs, we developed an app prototype that integrates a broad set of functions, is highly usable, and requires a low mental workload. This technology is now poised for longitudinal use and efficacy testing to improve family caregiver self-efficacy and CMC health outcomes, including reductions in enteral tube complications and preventable hospitalizations. If successful, we envision this app to be a scalable and adaptable platform to holistically support CMC caregiving at home.
Footnotes
Ms Cheng assisted with conceptualizing the study, conducted primary data collection and analysis, and drafted the initial manuscript and revisions; Ms Doutcheva and Ms Barton co-led design and usability testing sessions, data collection, and interpretation and reviewed and revised the manuscript; Ms Warner, Ms Wagner, Ms Finesilver, Ms Katz, Ms Nacht, and Drs Kelly and Ehlenbach assisted with data interpretation and reviewed and revised the manuscript; Drs Werner and Coller conceptualized the study, interpreted the data, drafted the initial manuscript, and revised the final manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institutes of Health Clinical and Translational Science Award at University of Wisconsin–Madison (grant 1UL1TR002373) as well as the University of Wisconsin–Madison School of Medicine and Public Health’s Institute for Clinical and Translational Research (ICTR), part of the Wisconsin Partnership Program (WPP) (WPP-ICTR grant 4358). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Wisconsin Partnership Program. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Kuo DZ, Houtrow AJ; Council on Children with Disabilities. Recognition and management of medical complexity. Pediatrics. 2016;138(6):e20163021. [DOI] [PubMed] [Google Scholar]
- 2.Berry JG, Agrawal R, Kuo DZ, et al. Characteristics of hospitalizations for patients who use a structured clinical care program for children with medical complexity. J Pediatr. 2011;159(2):284–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson KE, Lacombe-Duncan A, Cohen E, et al. Family experiences with feeding tubes in neurologic impairment: a systematic review. Pediatrics. 2015;136(1). Available at: www.pediatrics.org/cgi/content/full/136/1/e140 [DOI] [PubMed] [Google Scholar]
- 4.Enrione EB, Thomlison B, Rubin A. Medical and psychosocial experiences of family caregivers with children fed enterally at home. JPEN J Parenter Enteral Nutr. 2005;29(6):413–419 [DOI] [PubMed] [Google Scholar]
- 5.Pedrón-Giner C, Calderón C, Martínez-Costa C, Borraz Gracia S, Gómez-López L. Factors predicting distress among parents/caregivers of children with neurological disease and home enteral nutrition. Child Care Health Dev. 2014;40(3):389–397 [DOI] [PubMed] [Google Scholar]
- 6.Edwards S, Davis AM, Bruce A, et al. Caring for tube-fed children: a review of management, tube weaning, and emotional considerations. JPEN J Parenter Enteral Nutr. 2016;40(5):616–622 [DOI] [PubMed] [Google Scholar]
- 7.Evans S, Preston F, Daly A, Ashmore C, Holden C, MacDonald A. Home enteral tube feeding in children with inherited metabolic disorders: a review of long-term carer knowledge and technique. J Hum Nutr Diet. 2012;25(6):520–525 [DOI] [PubMed] [Google Scholar]
- 8.Wilken M. The impact of child tube feeding on maternal emotional state and identity: a qualitative meta-analysis. J Pediatr Nurs. 2012;27(3):248–255 [DOI] [PubMed] [Google Scholar]
- 9.Lim ML, Yong BYP, Mar MQM, et al. Caring for patients on home enteral nutrition: reported complications by home carers and perspectives of community nurses. J Clin Nurs. 2018;27(13–14):2825–2835 [DOI] [PubMed] [Google Scholar]
- 10.Avitsland TL, Faugli A, Pripp AH, Malt UF, Bjørnland K, Emblem R. Maternal psychological distress and parenting stress after gastrostomy placement in children. J Pediatr Gastroenterol Nutr. 2012;55(5):562–566 [DOI] [PubMed] [Google Scholar]
- 11.Coller RJ, Nelson BB, Sklansky DJ, et al. Preventing hospitalizations in children with medical complexity: a systematic review. Pediatrics. 2014;134(6). Available at: www.pediatrics.org/cgi/content/full/134/6/e1628 [DOI] [PubMed] [Google Scholar]
- 12.Nackers A, Ehlenbach M, Kelly MM, Werner N, Warner G, Coller RJ. Encounters from device complications among children with medical complexity. Hosp Pediatr. 2019;9(1):6–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silva BM, Rodrigues JJ, de la Torre Díez I, López-Coronado M, Saleem K. Mobile-health: a review of current state in 2015. J Biomed Inform. 2015;56:265–272 [DOI] [PubMed] [Google Scholar]
- 14.Shah N, Jonassaint J, De Castro L. Patients welcome the sickle cell disease mobile application to record symptoms via technology (SMART). Hemoglobin. 2014;38(2):99–103 [DOI] [PubMed] [Google Scholar]
- 15.Smith R, Menon J, Rajeev JG, Feinberg L, Kumar RK, Banerjee A. Potential for the use of mHealth in the management of cardiovascular disease in Kerala: a qualitative study. BMJ Open. 2015;5(11):e009367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirwan M, Vandelanotte C, Fenning A, Duncan MJ. Diabetes self-management smartphone application for adults with type 1 diabetes: randomized controlled trial. J Med Internet Res. 2013;15(11):e235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu WT, Huang CD, Wang CH, Lee KY, Lin SM, Kuo HP. A mobile telephone-based interactive self-care system improves asthma control. Eur Respir J. 2011;37(2):310–317 [DOI] [PubMed] [Google Scholar]
- 18.Marcano Belisario JS, Huckvale K, Greenfield G, Car J, Gunn LH. Smartphone and tablet self management apps for asthma. Cochrane Database Syst Rev. 2013;(11):CD010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed R, Toscos T, Rohani Ghahari R, et al. Visualization of cardiac implantable electronic device data for older adults using participatory design. Appl Clin Inform. 2019;10(4):707–718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cavalcanti LHC, Holden RJ, Karanam YLP. Applying participatory design with dementia stakeholders: challenges and lessons learned from two projects. In: Proceedings from the 12th EAI International Conference on Pervasive Computing Technologies for Healthcare; May 21–24, 2018; New York, NY. [Google Scholar]
- 21.Hakobyan L, Lumsden J, O’Sullivan D. Participatory design: how to engage older adults in participatory design activities. International Journal of Mobile Human Computer Interaction. 2015;7(3):78–92 [Google Scholar]
- 22.Halskov K, Hansen NB. The diversity of participatory design research practice at PDC 2002–2012. Int J Hum Comput Stud. 2015;74:81–92 [Google Scholar]
- 23.Hwang AS, Truong KN, Mihailidis A. Using participatory design to determine the needs of informal caregivers for smart home user interfaces. In: Proceedings from the 6th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth) and Workshops; May 21–24, 2012; San Diego, CA. [Google Scholar]
- 24.Reddy A, Lester CA, Stone JA, Holden RJ, Phelan CH, Chui MA. Applying participatory design to a pharmacy system intervention. Res Social Adm Pharm. 2019;15(11):1358–1367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanders EB-N. From user-centered to participatory design approaches. In: Frascara J, ed. Design and the Social Sciences: Making Connections. New York, NY: Taylor & Francis; 2002:1–8 [Google Scholar]
- 26.Schuler D, Namioka A, eds. Participatory Design: Principles and Practices. Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers; 1993 [Google Scholar]
- 27.Spinuzzi C. The methodology of participatory design. Tech Commun. 2005;52(2):163–174 [Google Scholar]
- 28.Coller R, Werner NE. MCHB grand challenge. Available at: https://www.youtube.com/watch?v=OscP5PkjZNY&feature=youtu.be. Accessed January 25, 2020.
- 29.LeRouge C, Ma J, Sneha S, Tolle K. User profiles and personas in the design and development of consumer health technologies. Int J Med Inform. 2013;82(11):e251–e268 [DOI] [PubMed] [Google Scholar]
- 30.Adlin T, Pruitt J. The Essential Persona Lifecycle: Your Guide to Building and Using Personas. Burlington, MA: Morgan Kaufmann; 2010 [Google Scholar]
- 31.Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Int J Hum Comput Interact. 2008;24(6):574–594 [Google Scholar]
- 32.Kortum PT, Bangor A. Usability ratings for everyday products measured with the system usability scale. Int J Hum Comput Interact. 2013;29(2):67–76 [Google Scholar]
- 33.Baysari MT, Westbrook JI. Mobile applications for patient-centered care coordination: a review of human factors methods applied to their design, development, and evaluation. Yearb Med Inform. 2015;10(1):47–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson K, Burford O, Emmerton L. Mobile health apps to facilitate self-care: a qualitative study of user experiences. PLoS One. 2016;11(5):e0156164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nkoy FL, Fassl BA, Wilkins VL, et al. Ambulatory management of childhood asthma using a novel self-management application. Pediatrics. 2019;143(6):e20181711. [DOI] [PubMed] [Google Scholar]
- 36.Fedele DA, Cushing CC, Fritz A, Amaro CM, Ortega A. Mobile health interventions for improving health outcomes in youth: a meta-analysis. JAMA Pediatr. 2017;171(5):461–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ming DY, Jackson GL, Sperling J, et al. Mobile complex care plans to enhance parental engagement for children with medical complexity. Clin Pediatr (Phila). 2019;58(1):34–41 [DOI] [PubMed] [Google Scholar]
- 38.Quigley L, Lacombe-Duncan A, Adams S, Hepburn CM, Cohen E. A qualitative analysis of information sharing for children with medical complexity within and across health care organizations. BMC Health Serv Res. 2014;14:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Birkhoff S, Moriarty H. Interventions using smartphone health apps across various populations: an integrative review of the literature. J Inform Nurs. 2016;1(1):13–24 [Google Scholar]
- 40.Goodwin J, Cummins J, Behan L, O’Brien SM. Development of a mental health smartphone app: perspectives of mental health service users. J Ment Health. 2016;25(5):434–440 [DOI] [PubMed] [Google Scholar]
- 41.Desai AD, Jacob-Files EA, Wignall J, et al. Caregiver and health care provider perspectives on cloud-based shared care plans for children with medical complexity. Hosp Pediatr. 2018;8(7):394–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hilliard ME, Hahn A, Ridge AK, Eakin MN, Riekert KA. User preferences and design recommendations for an mHealth app to promote cystic fibrosis self-management. JMIR Mhealth Uhealth. 2014;2(4):e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ly KH, Janni E, Wrede R, et al. Experiences of a guided smartphone-based behavioral activation therapy for depression: a qualitative study. Internet Interv. 2015;2(1):60–68 [Google Scholar]
- 44.Nkoy FL, Hofmann MG, Stone BL, et al. Information needs for designing a home monitoring system for children with medical complexity. Int J Med Inform. 2019;122:7–12 [DOI] [PubMed] [Google Scholar]