Abstract
Falls affect more than 29 million American adults ages ≥65 years annually. Many older adults experience recurrent falls requiring medical attention. These recurrent falls may be prevented through screening and intervention. In 2014 to 2015, records for 199 older adult patients admitted from a major urban teaching hospital’s emergency department were queried. Open-ended variables from clinicians’ notes were coded to supplement existing closed-ended variables. Of the 199 patients, 52 (26.1%) experienced one or more recurrent falls within 365 days after their initial fall. Half (50.0%) of all recurrent falls occurred within the first 90 days following discharge. A large proportion of recurrent falls among older adults appear to occur within a few months and are statistically related to identifiable risk factors. Prevention and intervention strategies, delivered either during treatment for an initial fall or upon discharge from an inpatient admission, may reduce the incidence of recurrent falls among this population.
Keywords: falls, elderly, recurrent, balance, prevention
Introduction
Geriatric fall injuries present a pressing public health concern in the United States. More than 1 in 4 Americans aged ≥65 years (older adults) reports falling each year, totaling approximately 29 million falls annually.1 An estimated 7 million of these falls result in injuries, leading 2.8 million older adults to receive treatment in the emergency department (ED), with roughly 800 000 admitted to the hospital for more intensive care.1 Older adult falls have serious cost consequences, accounting for an estimated US$30 to US$50 billion in direct medical costs in 20152,3—roughly 1% of annual health expenditures.4 Care for those patients who are admitted to the hospital is more expensive per capita than is care for those who are only treated in the ED.5,6 Geriatric falls also result in significant indirect costs, such as loss of functioning,7 declining quality of life,8 and burden to social services.9
Those individuals who experience 2 or more falls within a year constitute a sizable and particularly high-risk subset of older adults who experience falls: They are more likely to sustain serious injuries10 and have a distinct set of risk factors as compared to older adults who experience only a single fall event.11,12 Reported recurrent fall rates vary significantly due to heterogeneity in study methods and populations, with estimates suggesting that between one- and two-thirds of older adults who fall experience a recurrent fall within the next year.11,13-15 In a systematic review of studies of population-based or community-dwelling samples, Carpenter (2014) reports that 10% of all older adults sustain 2 or more falls in a given year.16
While there are multiple contexts—including primary care, supportive housing facilities, and long-term care institutions—in which it is possible to identify and intervene with older adults at high risk of recurrent falls, hospital venues constitute an important setting for assessment and intervention because they are where older adults frequently present after sustaining an initial fall-related injury.1 Older adults presenting to the ED with fall-related complaints represent an intrinsically high-risk population for future falls, and past work has shown that ED-based risk assessment and intervention models can be effective in preventing future falls.17,18 Many geriatric and emergency medicine societies have released guidelines promoting the integration of fall risk assessment practices into clinical care and ED workflows.19,20 However, fall risk assessments have yet to become standard practice, and many older adult fallers seen in the ED do not receive recommended evaluations, referrals, and other postdischarge supports.21,22 Given concerns about time and resource constraints,23 hospital-based practitioners need an accurate and limited set of predictor variables to efficiently prioritize older adults for multifactorial risk assessment and intervention.
The purpose of this study is to assist efforts in preventing recurrent falls by informing medical practitioners of the major risk factors for recurrent falls based on quantitative and qualitative data collected among older adults admitted to the trauma surgery department from the ED of a major urban teaching hospital. Not only do older adults who experience recurrent falls tend to experience more serious injuries10 they also have different characteristics11,12 as compared to older adults who experience nonrecurrent falls. Through a chart review-based analysis, we quantify risk factors for recurrent falls that are already captured as data points or field notes during routine hospital care. We also integrate data from the US Census Bureau’s American Community Survey to explore how demographic characteristics not collected in patients’ charts may be related to their risks of recurrent falls. The identification of risk factors from this free, secondary source, in conjunction with variables collected during routine clinical care, may allow hospitals to more efficiently identify and refer or intervene with patients at high risk of recurrent fall while reducing screening and assessment burdens on clinical staff.
Methods
This study was reviewed and approved by the institutional review board (IRB) of the hospital from which patient data were collected, as well as by the IRB of the collaborating investigators’ home institution.
Data Collection
The study population comprised older adults ages ≥65 years who were treated in the ED of a major, urban teaching hospital for a fall-related concern and were subsequently admitted to the trauma surgery department. Cases were eligible for inclusion in the study if they met the following criteria: (1) age ≥ 65 years; (2) no prior history of falls; and (3) admitted to the trauma surgery department between January 1, 2014, and December 31, 2015, with a primary diagnosis of a fall-related injury. However, to allow for a 3-month follow-up window to capture recurrent fall data for all cases, we removed initial falls occurring after September 30, 2015.(note 1) We employed a simple random sampling approach until we reached a sample size (N = 199) sufficient to power analyses of important predictor variables. Because a limited number of individuals (13.1%, n = 26) experienced a recurrent fall requiring readmittance within 3 months, we expanded our definition of recurrent fall to capture a year-long window after the initial fall.
Data were queried from the hospital’s electronic health record systems (EHRs): WellSoft Trauma Registry and a proprietary database. Many variables of interest were available only in open-ended text fields, such as clinicians’ notes. A team of trained medical students, supervised by a research coordinator, manually reviewed and coded open-ended fields in preparation for statistical analysis. Coded records were joined and then imported into IBM SPSS (version 26)24,25 in which all analyses were run.
Since no socio-economic measures were available from patients’ records, we decided to include Census tract-level measures from the 5-year 2015 American Community Survey. The Census tract is a small geography created by the US Census Bureau for the purpose of analyzing population-level data; there are 375 census tracts in Philadelphia with population of at least 100 and each tract has less than 9000 residents. An average of nearly 20% of residents residing in each tract are age 65 or older. Due to these small population sizes, individual socio-economic measures, such as income and education, tend to closely reflect the aggregate norm. Therefore, we are assuming that individuals from tracts with lower or higher income and education scores are themselves more likely to be lower or higher in their socio-economic standing. We extracted 3 measures26: (1) median household income; (2) percent of adults aged ≥65 years with at least a high school education; and (3) percent of adults aged ≥65 years with at least a 4-year college education. To assign patients to tracts, we geocoded their home addresses and intersected these point data with a shapefile of 2010 Census tract polygons using the Geographic Information Systems (GIS) software ArcGIS Desktop 10.4.27 Due to the diversity in socio-economic statuses across nearby urban neighborhoods close to Jefferson Hospital, there was a substantial range in these socio-economic scores among fall victims.
The extant the literature and practitioners’ judgments of clinical relevance informed our choices when categorizing continuous variables. We created a dichotomous variable for recurrent falls as our primary outcome measure given that few cases experienced multiple recurrent falls. Health conditions, which comprised many discrete bivariate variables, were categorized into neurological, psychiatric, orthopedic, and other conditions. We tested the validity of this categorization strategy by omitting high-frequency conditions from each category—for example, dropping dementia from the psychiatric conditions category—during preliminary analyses to ensure that individual conditions were not accounting for the entire influence of a category. We created a composite variable reflecting the “mechanism of injury” that contained 2 categories: (1) falling while standing; and (2) falling from a height, falling while on the stairs, tripping, slipping, being intoxicated, or being pushed. We also created a dichotomous variable, “Location of Fall,” which captured whether the fall took place inside the home or outside of the home.
Data Analysis
Pearson χ2 tests were conducted to evaluate bivariate relationships between potential predictor variables and our dichotomous recurrent fall variable. Odds ratios were included to assess predictive strength and compare to adjusted odds ratios produced by binary logistic regression analysis. Binary logistic regression analysis was done in 4 blocks: demographic, medical, situational, and situation by age interaction terms. Block one included potential confounding socio-demographic variables: sex, age, race, education, income, and insurance. Block 2 contained health-related variables: number of medications, prescribed medications, over-the-counter medications, dietary supplements, health conditions, comorbidities, overnight stay, and cancer diagnosis. We conducted 3 separate 3-block binary logistic regression analyses to examine the relative importance of each of the situational variables: fall while standing, fall indoors, and fall while living alone. Block 4 examined interaction effects between age and our situational variables to assess any joint impacts beyond the additive effects of each variable.
Results
Of our sample of 199 patients, 52 (26.1%) patients experienced one or more recurrent falls during the year after their initial fall, with half (n = 26, 50.0%) experiencing a recurrent fall within 90 days after their initial fall. Nine (17.3% of those who experienced a recurrent fall) patients experienced more than 1 recurrent fall within the year following their initial fall; these patients accounted for nearly a third (30.6%) of all recurrent falls among the sample.
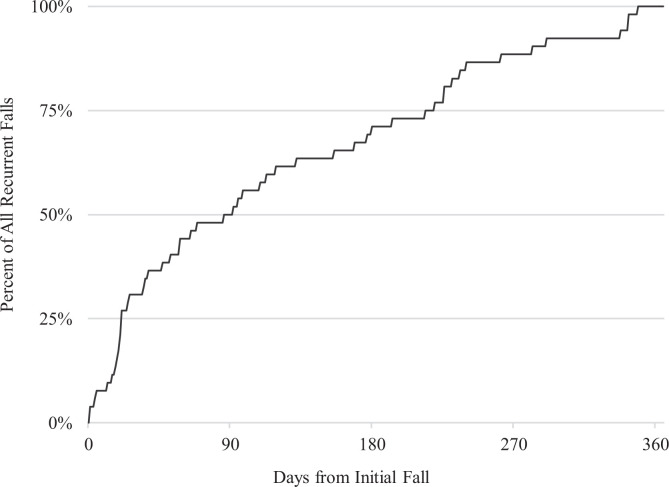
Figure 1 details the cumulative percentage of all recurrent falls that occurred over time, plotted relative to how long they occurred after the initial fall. Exactly half of all recurrent falls experienced by individuals in our sample occurred within 90 days of their initial fall.
Figure 1.
Cumulative percent of recurrent falls occurring over time.
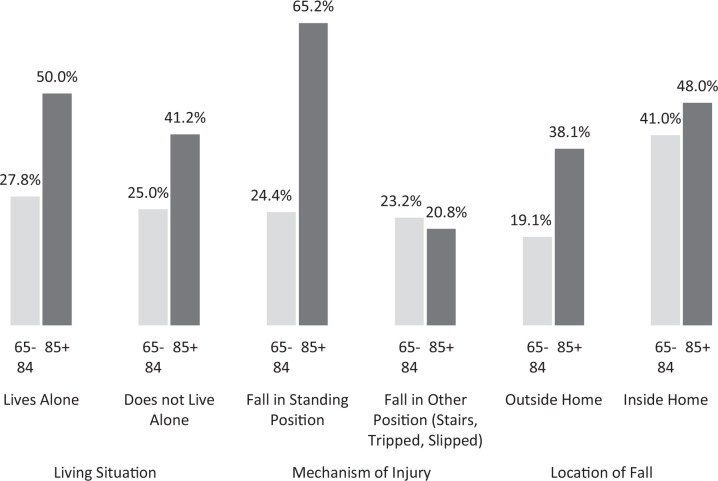
While older adults aged ≥85 years were more likely than older adults aged 65 to 84 years to experience a recurrent fall within 1 year (see Table 1), this younger subset of older adults experienced recurrent falls more quickly than did their older counterparts. The hazard estimate (based on the Kaplan-Meier estimator) for recurrent falls in these 2 age groups is visualized in Figure 2; the hazard estimate demonstrates that older adults aged 65 to 84 years were more likely to experience a recurrent fall within the first 7 months following an initial fall, whereas older adults aged ≥85 years accumulated a higher proportion of recurrent falls after the 7-month mark.
Table 1.
Crosstab of Sociodemographic, Medical, and Situational Predictors.
| Variable | Total N = 199 | % with recurrent fall | P value (χ2) | Unadjusted odds ratio |
|---|---|---|---|---|
| Socio-demographic variables | ||||
| Gender | 199 | .61 | ||
| Female | 117 | 24.8% | Reference | |
| Male | 82 | 28.0% | 1.18 | |
| Age | 199 | .02 | ||
| 65-84 | 147 | 21.8% | Reference | |
| 85+ | 52 | 38.5% | 2.25 | |
| Race | 199 | .29 | ||
| White | 135 | 25.2% | Reference | |
| Black | 56 | 25.0% | .99 | |
| Other | 8 | 50.0% | 2.97 | |
| % Adults 65+ in Census Tract who Graduated from High School | 188 | .03 | ||
| <70% | 62 | 35.5% | 2.26 | |
| 70%+ | 137 | 20.6% | Reference | |
| Insurance type | 198 | .89 | ||
| Private | 62 | 25.8% | Reference | |
| Medicaid/Medicare | 113 | 25.7% | .99 | |
| Self-pay | 23 | 30.4% | 1.26 | |
| Medical variables | ||||
| Number of medications | 187 | <.01 | ||
| 0-4 | 108 | 15.7% | Reference | |
| 5-8 | 46 | 32.6% | 2.59 | |
| 9+ | 33 | 42.4% | 3.94 | |
| Prescribed medications | 187 | .02 | ||
| No | 63 | 14.3% | Reference | |
| Yes | 124 | 29.8% | 2.55 | |
| Over the counter (OTC) medications | 187 | <.01 | ||
| No | 93 | 12.9% | Reference | |
| Yes | 94 | 36.2% | 3.83 | |
| Dietary supplements | 187 | <.01 | ||
| No | 149 | 18.8% | Reference | |
| Yes | 38 | 47.4% | 3.89 | |
| Neurological condition | 199 | <.01 | ||
| No | 142 | 19.0% | Reference | |
| Yes | 57 | 43.9% | 3.33 | |
| Psychiatric condition | 199 | .80 | ||
| No | 174 | 26.4% | Reference | |
| Yes | 25 | 24.4% | .88 | |
| Orthopedic condition | 199 | .61 | ||
| No | 158 | 25.3% | Reference | |
| Yes | 41 | 29.3% | 1.22 | |
| Two or more comorbidities | 199 | .31 | ||
| No | 84 | 23.8% | Reference | |
| Yes | 115 | 27.8% | 1.58 | |
| Cancer diagnosis | 197 | .24 | ||
| No | 164 | 28.0% | Reference | |
| Yes | 33 | 18.2% | .57 | |
| Overnight stay | .60 | |||
| No | 169 | 25.4% | Reference | |
| Yes | 30 | 30.0% | 1.26 | |
| Situational variables | ||||
| Living situation | 154 | .68 | ||
| Does not live alone | 130 | 29.2% | Reference | |
| Lives alone | 24 | 33.3% | 1.21 | |
| Mechanism of injury | 183 | .02 | ||
| Other (stairs, tripped, slipped) | 64 | 22.7% | Reference | |
| Fall in standing position | 119 | 39.1% | 2.18 | |
| Location of fall | 153 | <.01 | ||
| Outside home | 89 | 23.6% | Reference | |
| Inside home | 64 | 43.8% | 2.52 | |
Figure 2.
Cumulative hazard estimates for recurrent fall by age-group.
Figure 2 plots the cumulative hazard estimates—modified conditional probabilities—for recurrent falls among our 2 age groups: older adults aged 65 to 84 years (in blue) and older adults aged ≥ 85 (in green).
Table 1 presents results of crosstabs conducted on our dichotomous recurrent fall variable against each of our predictor variables. For each predictor variable, we present the total number of valid cases and a χ2 P value. For each level of each predictor, we present an n value, the percentage of cases that experienced a recurrent fall, and an unadjusted odds ratio.
Given that 2 of our 3 situational variables were statistically significant predictors of recurrent fall in bivariate analyses, we conducted a series of logistic regression analyses to control for potential confounding variables. We first conducted a logistic regression of all our socio-demographic variables, then we conducted another logistic regression to determine the additional impact of our medical predictors. Lastly, we conducted independent logistic regressions for each of our situational variables, controlling for our socio-demographic and medical variables.
On the left side of Table 2 are our demographic predictors, which accounted for approximately 11% of the variance in recurrent falls (based on Nagelkerke R2 approximation). On the right side of Table 2 are the combined demographic and medical predictors. The addition of medical variables to the analysis resulted in an R2 value of .333. However, due to high multicollinearity between our number of medications variable and our variables for each medication type (r = .47 or higher), we removed our number of medications variable from the multivariate analysis; this had only a marginal impact on the Nagelkerke R2 value, which decreased from .333 to .332.
Table 2.
Logistic Regression—Socio-Demographic and Medical Predictors of Recurrent Fall.
| Variable | Block 1: demographic predictors | Block 2: demographic and medical predictors | ||
|---|---|---|---|---|
| Adjusted OR | P value (Wald) | Adjusted OR | P value (Wald) | |
| Socio-demographic variables | ||||
| Gender | ||||
| Female | 1.25 | .56 | 1.39 | .46 |
| Male | Reference | |||
| Age | ||||
| 65-84 | Reference | |||
| 85+ | 2.64 | .01 | 2.27 | .06 |
| Race | ||||
| White | Reference | |||
| Black | 1.60 | .29 | .68 | .45 |
| Other | 2.17 | .34 | 3.30 | .25 |
| % Adults 65+ in census tract who graduated from high school | ||||
| <70% | 2.28 | .04 | 3.55 | <.01 |
| 70%+ | Reference | |||
| Insurance type | ||||
| Private | Reference | |||
| Medicaid/Medicare | 1.00 | .98 | .71 | .47 |
| Self-pay | 1.35 | .74 | 1.21 | .79 |
| Medical variables | ||||
| Prescribed medication(s) | - | - | 1.84 | .27 |
| Over the counter medication(s) | - | - | 2.65 | .04 |
| Dietary supplement(s) | - | - | 2.62 | .06 |
| Neurological condition(s) | - | - | 3.52 | <.01 |
| Psychiatric condition(s) | - | - | .69 | .56 |
| Orthopedic condition(s) | - | - | .79 | .66 |
| Comorbidity(ies) | - | - | .78 | .70 |
| Cancer diagnosis | - | - | .47 | .25 |
| Overnight hospital stay | - | - | 1.12 | .86 |
Table 2 presents the results of a 2-block logistic regression analysis. In the first block, we included only our socio-demographic variables and did not control for the effects of medical variables. In the second block, we included both our demographic and medical variables.
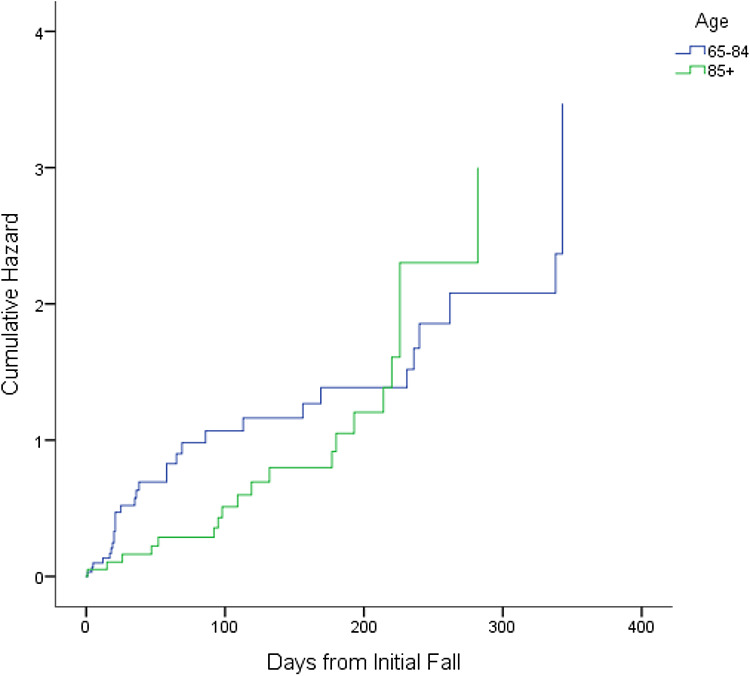
Table 3 presents the results of logistic regression analyses of our situational variables and interaction terms between our situational variables and age, controlling for the effects of our socio-demographic and medical variables. Falling inside the home proved to be a significant predictor of recurrent fall even after controlling for socio-demographic and medical factors, and 2 interaction terms—falling in a standing position by age and falling inside the home by age—also were significant after controlling for other variables in the model.
Table 3.
Logistic Regression—Situational Predictors and Interaction Terms.
| Variable/interaction term | Unadjusted OR | P value (χ2) | Adjusted OR | P value (Wald) |
|---|---|---|---|---|
| Block 3: situational predictors of a recurrent fall | ||||
| Fall while standing | 2.18 | .02 | 2.14 | .09 |
| Fall inside home | 2.52 | <.01 | 2.75 | .03 |
| Fall living alone | 1.21 | .69 | 1.27 | .72 |
| Block 4: interactions between situational predictors and age | ||||
| Lives alone by age | - | - | 1.1 | .93 |
| Fall in standing position by age | - | - | 10.0 | .02 |
| Fall inside home by age | - | - | 8.6 | .04 |
Table 3 presents the results of block 3 and block 4 logistic regression analyses; each variable or interaction term was analyzed separately to preserve sample size. Variables analyzed in block 3 control for the effects of socio-demographic and medical variables included in the preceding 2 blocks, while interaction terms analyzed in Block 4 control for the effects of socio-demographic, medical, and situational variables included in the preceding 3 blocks.
Results presented in Table 3 provide further context to the interactions between our situational variables and age. Although sample size constraints limited our ability to identify statistical significance, older adults ages 85+ were more likely than their younger counterparts to experience recurrent falls based on an initial fall while not living alone (P = .07), from a standing position (P < .01), or from a fall occurring outside of the home (P = .07).
Figure 3 presents the percentages of individuals per situational predictor by age-group interaction who experienced a recurrent fall. The lighter gray bars represent older adults 65 to 84 years of age, while the darker gray bars represent older adults 85+.
Figure 3.
Interactions between situational predictors and age.
Discussion
This study contributes important findings relating to patient and fall characteristics specific to those older adults admitted to the hospital from the ED, which may help hospitals to more effectively assess recurrent fall risk and target appropriate prevention strategies to reduce that risk. Our findings corroborate prior older adult falls findings relating to risk factors such as neurological conditions28 while also identifying unexplored or underexplored variables that may be promising indicators of recurrent fall risk, including use of over-the-counter medications and Census tract-level high school graduation rates among adults ages ≥65 years.
The incidence of recurrent falls among our sample—26.1% of our sample experienced at least 1 recurrent fall—is lower than some recurrent fall rates reported in other studies.11,13-15 Our low recurrent fall rate may reflect differences in our sample characteristics or recruitment venue as compared to other studies; methodological limitations (see the corresponding section below) may also have contributed to our relatively low recurrent fall rate. However, an incidence of 26.1% still speaks to the significance of recurrent falls as a clinical and population health concern.
Our approach to supplementing data from patients’ charts with imputed values from secondary data sets—in our case, Census tract-level data—proved promising and may be relevant as other hospitals consider how best to evaluate recurrent fall risk. While we included both median tract income and the Census tract-level high school graduation rate among adults aged ≥65 years as potential proxy measures for patients’ socioeconomic statuses, median tract income was not a statistically significant bivariate predictor; this may be due to the fact that median income, unlike the high school graduation rate among adults aged ≥65 years, was only available for the entire Census tract population, as opposed to being broken down by age-group. However, the Census tract-level high school graduation rate was a significant predictor of recurrent falls in both bivariate and multivariate analyses. Hospitals may consider similar approaches to imputing socioeconomic or other variables derived from secondary data sets given that these data are freely available and that the process is easily replicated and can significantly add to the explanatory power of the risk prediction model. Alternately, given the value of these data, hospitals may consider incorporating such demographic fields into their data collection protocols rather than relying on secondary, population-level data sources.
Our preliminary findings that older adults aged 65 to 84 years were more likely than their older counterparts to experience a recurrent fall within the first 7 months following their initial fall are also of note. That older adults aged 85+ years appear to be disproportionately at risk of recurrent fall later in the 1-year window following an initial fall suggests that the underlying drivers for their recurrent falls may differ from those of older adults 65 to 84 years. This finding may have implications for design and delivery of prevention and intervention strategies to reduce recurrent fall risk.
The inclusion of situational variables in our set of potential predictors for recurrent falls differed from the approaches taken in many similar studies. This is relevant in that falling inside the home was a significant predictor in both bivariate and multivariate analyses and that falling while standing was significant in bivariate analyses and approached significance (P = .09) in multivariate analyses. The significance of interactions between situational variables and age was also notable and suggests that older adults aged 85+ who experience initial falls in particular contexts, for example, from a standing position, may be particularly likely to experience a recurrent fall. These variables and other situational variables bear further investigation and may be worthwhile to capture systematically (eg, in closed-ended fields in patients’ charts) as opposed to in open-ended formats such as in clinicians’ notes.
In keeping with prior research, presence of a neurological condition was a strong and significant predictor of a recurrent fall.28 Of the 57 patients with a neurological condition who experienced an initial fall, 49.1% (n = 28) experienced a recurrent fall. The exceedingly high recurrent fall rate for this subpopulation suggests there are significant opportunities to improve discharge planning and posttreatment services and follow-up.
Of the predictor variables we considered, it is notable that very few appeared to exert a strong or significant influence on the likelihood of a recurrent fall. All of our demographic variables, with the exception of tract-level high school graduation rates among older adults, were nonsignificant. It is also notable that other predictor variables identified in the literature, such as prescribed medications,29 were not significant. While our sample size may have limited our ability to identify significant effects, this suggests the need to continue to refine identified predictor variables to ensure that those incorporated into risk screening protocols are accurate.
The identification of risk factors for recurrent falls among older adults is an important first step to support hospitals’ efforts to improve long-term outcomes for older adults presenting with fall-related conditions. Hospitals should consider how the risk factors identified here and in the broader literature may inform their risk assessment and risk stratification processes, as well as how they may better tailor discharge planning and posttreatment services to mitigate the likelihood of recurrent falls.
Limitations
Our study had several significant limitations. Due to resource and time constraints, our sample size was relatively small, thus limiting our ability to detect the significance of potential predictor variables. While we were able to collect data for all patients during the 90 days following their initial fall, we were unable to collect data for all patients for the full year following their initial fall. As we were only able to analyze data from a single hospital, some patients included in our sample may have experienced recurrent falls that were treated at other hospitals in the area.
Conclusion
A rapidly aging population and recent upward trends in older adult falls suggest issues of prevention and treatment of recurrent falls will become increasingly salient. For those high-risk, high-cost older adults who sustain falls sufficiently serious to be admitted following an ED visit, hospitals need appropriate risk factors to screen for risk of recurrent fall and to appropriately target fall prevention interventions. This study identifies a limited number of risk factors that are closely tied to the likelihood of a recurrent fall, including risk factors identified in prior recurrent fall research as well as novel risk factors (eg, over-the-counter medications). Further, the approach taken here of imputing socio-demographic variables not typically available in an EHR is one that hospitals may replicate to better evaluate their patients’ risks for recurrent fall without increasing the patient-level data collection burden. Additional research is needed to further refine a set of core risk factors that trauma and ED practitioners can employ to support their decision-making and to effectively connect patients to needed supports after an initial fall.
Note
The gap in our sample for these three months should not represent a significant threat to the sample’s validity given that seasonality has not been identified as a risk factor for falls among older adults.24
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: William Curran-Groome  https://orcid.org/0000-0001-6432-7561
https://orcid.org/0000-0001-6432-7561
Stanton B. Miller, MD, MPH, FACS  https://orcid.org/0000-0001-5028-6949
https://orcid.org/0000-0001-5028-6949
Azor Hui, PhD, MSPH  https://orcid.org/0000-0002-9668-3912
https://orcid.org/0000-0002-9668-3912
Venkata Masarapu, BS, MD(c)  https://orcid.org/0000-0001-6351-2730
https://orcid.org/0000-0001-6351-2730
Andre Alabd, BS, MD(c)  https://orcid.org/0000-0002-3307-5602
https://orcid.org/0000-0002-3307-5602
References
- 1. Bergen G. Falls and fall injuries among adults aged ≥ 65 years—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993–998. [DOI] [PubMed] [Google Scholar]
- 2. Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. J Safety Res. 2016;58:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018;66(4):693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Medicare and Medicaid Services. National Health Expenditures Summary: CY 1960-2016. National Health Expenditure Data; 2016. Accessed June 3, 2018 https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/NHEGDP16.zip [Google Scholar]
- 5. HCCI Annual Report.pdf. Google docs. 2018. Accessed July 5, 2018. https://drive.google.com/file/d/1vi3S2pjThLFVwB7OtYwFmOiLVPTFl_wk/view?usp=drive_web&usp=embed_facebook
- 6. Hospital Adjusted Expenses per Inpatient Day. In: Henry J, ed. Kaiser Family Foundation. 2017. Accessed July 5, 2018 https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day/
- 7. Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 1998;53(2):M112–M119. [DOI] [PubMed] [Google Scholar]
- 8. Hartholt KA, van Beeck EF, Polinder S, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma Acute Care Surg. 2011;71(3):748–753. [DOI] [PubMed] [Google Scholar]
- 9. Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57(9):740–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pluijm SM, Smit JH, Tromp EAM, et al. A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: results of a 3-year prospective study. Osteoporos Int. 2006;17(3):417–425. [DOI] [PubMed] [Google Scholar]
- 11. Nevitt MC, Cummings MD. Recurrent non syncopal falls. Jama. 1989;261:2663–2668. [PubMed] [Google Scholar]
- 12. Graafmans WC, Ooms ME, Hofstee HMA, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143(11):1129–1136. [DOI] [PubMed] [Google Scholar]
- 13. O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–354. [DOI] [PubMed] [Google Scholar]
- 14. Stalenhoef PA, Diederiks JPM, Knottnerus JA, Kester ADM, Crebolder H. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55(11):1088–1094. [DOI] [PubMed] [Google Scholar]
- 15. Tinetti ME. Factors associated with serious injury during falls by ambulatory nursing home residents. J Am Geriatr Soc. 1987;35(7):644–648. [DOI] [PubMed] [Google Scholar]
- 16. Carpenter CR, Avidan MS, Wildes T, Stark S, Fowler SA, Lo AX. Predicting geriatric falls following an episode of emergency department care: a systematic review. Acad Emerg Med. 2014;21(10):1069–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–97. [DOI] [PubMed] [Google Scholar]
- 18. Davison J, Bond J, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending accident & emergency benefit from multifactorial intervention—a randomised controlled trial. Age Ageing. 2005;34(2):162–168. [DOI] [PubMed] [Google Scholar]
- 19. American Geriatrics Society BGS. AGS/BGS Clinical Practice Guideline: Prevention of Falls in Older Persons. American Geriatrics Society; 2010. [Google Scholar]
- 20. Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American college of emergency physicians, American geriatrics society, emergency nurses association, and society for academic emergency medicine. Ann Emerg Med. 2014;63(5):e1–e3. [DOI] [PubMed] [Google Scholar]
- 21. Naughton C, McGrath E, Drennan J, et al. The profile and follow-up of patients who attend the emergency department following a fall. Int Emerg Nurs. 2012;20(4):243–250. [DOI] [PubMed] [Google Scholar]
- 22. Tirrell G, Srion J, Lipsitz LA, Camargo Jr CA, Kabrhel C, Liu SW. Evaluation of older adult patients with falls in the emergency department: discordance with national guidelines. Acad Emerg Med. 2015;22(4):461–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Institute of Medicine C on the F of EC in the UHS. Hospital-Based Emergency Care: At the Breaking Point. National Academies Press; 2006. [Google Scholar]
- 24. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people:” a systematic review and meta-analysis”. Epidemiology. 2010;21(5):658–668. [DOI] [PubMed] [Google Scholar]
- 25. IBM Corp. IBM SPSS Statistics for Windows. IBM Corp; 2016. [Google Scholar]
- 26. United States Census Bureau. 2011-2015 American Community Survey (ACS) 5-year Estimates. American Community Survey; 2015. Accessed February 1, 2018 https://www2.census.gov/programs-surveys/acs/summary_file/2015/data/ [Google Scholar]
- 27. Environmental Systems Research Institute. ArcGIS Desktop. 2019. Environmental Systems Research Institute. [Google Scholar]
- 28. Stolze H, Klebe S, Zechlin C, Baecker C, Friege L, Deuschl G. Falls in frequent neurological diseases. J Neurol. 2004;251(1):79–84. [DOI] [PubMed] [Google Scholar]
- 29. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. [DOI] [PubMed] [Google Scholar]