Abstract
Coronavirus disease 2019 (COVID-19) has become a global pandemic. Its relationship with environmental factors is an issue that has attracted the attention of scientists and governments. This article aims to deal with a possible association between COVID-19 and environmental factors and provide some recommendations for adequately controlling future epidemic threats. Environmental management through ecosystem services has a relevant role in exposing and spreading infectious diseases, reduction of pollutants, and control of climatic factors. Pollutants and viruses (such as COVID-19) produce negative immunological responses and share similar mechanisms of action. Therefore, they can have an additive and enhancing role in viral diseases. Significant associations between air pollution and COVID-19 have been reported. Particulate matter (PM2.5, PM10) can obstruct the airway, exacerbating cases of COVID-19. Some climatic factors have been shown to affect SARS-CoV-2 transmission. Yet, it is not well established if climatic factors might have a cause-effect relationship to the spreading of SARS-CoV-2. So far, positive as well as negative indirect environmental impacts have been reported, with negative impacts greater and more persistent. Too little is known about the current pandemic to evaluate whether there is an association between environment and positive COVID-19 cases. We recommend smart technology to collect data remotely, the implementation of “one health” approach between public health physicians and veterinarians, and the use of biodegradable medical supplies in future epidemic threats.
Keywords: COVID-19, SARS-CoV-2, Environment, Pollutants, Environmental impacts, One health
Graphical abstract
Highlights
-
•
Unsustainable environmental management contributes to an increase of zoonotic diseases.
-
•
Pollutants produce immune alterations and can affect the respiratory system similar to viral diseases.
-
•
Indirect environmental impacts have been described. Negative impacts are projected to be greater over time.
-
•
Climatic factors are not well established as factors influencing COVID-19 pandemic dissemination.
-
•
One Health approach and biodegradable medical devices for future epidemiological threats should be considered.
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by SARS-CoV-2, started in November 2019 in Wuhan (China), and from there it was transmitted and rapidly dispersed all over the world (Jin et al., 2020). In March 2020, the WHO declared COVID-19 to be a pandemic. The global emergency committee indicated the need for early detection, quarantine, and rapid treatment (Sohrabi et al., 2020). This pandemic has caused more uncertainty and debate globally than previous ones such as SARS (2002–2003), avian influenza (2003–2009), swine flu (2009–2010), and Ebola (2014–2016), and most of its impacts are still uncertain (Sarkodie and Owusu, 2020a). However, all the evidence so far indicates that these pandemics are not random diseases, but a consequence of inappropriate interaction between humans and wild fauna.
Environmental sciences must play an important role in understanding and mitigating the current changes and challenges at the global level (Bernhardt et al., 2017; Eagles-Smith et al., 2018). A global sustainable development approach is highly needed to address these global variations, which must consider all sectors simultaneously in order to understand the interactions between environment, diseases, and human activities (Liu et al., 2018).
The relationships between the environment and COVID-19, the factors that caused the virulence of the respiratory disease, the measures to control the pandemic and the future impacts associated with the disease, are issues that need to be well understood scientifically. This article aims to synthesize key topics about the environment and COVID-19, thus providing recommendations for future epidemic threats. These may be useful for government decision-makers and researchers.
Although this article focuses on the environment and COVID-19, we recognize that this pandemic is primarily a human tragedy, which has already taken half million people's lives. At present, human health must be the priority, along with avoiding the spread of the virus. Nevertheless, the need for critical analysis of this pandemic can be useful to anticipate what may happen when global activities return to normality and also what actions should be taken into consideration with future epidemiological threats.
2. Environmental management and its influence on the global pandemic
The management of natural resources has an impact on the quality of human life. The current economic system with a strong focus on unsustainable exploitation of natural resources, in addition to the modern lifestyle that encourages mega-cities, has heavily modified natural environments (Boger and Hart, 2008; Molina and Molina, 2004). This contributes to the generation of artificial environments ideal for the development and spread of new diseases, due to the agglomeration of people in small spaces and the lack of natural barriers that work as buffer zones between high density populated zones (Hunter, 2017). Natural ecosystems not only provide economically valuable resources but also provide services to human well-being, through its natural ecological functions. The ecosystem services allow the regulation of climatic conditions, the control of water and air quality, the purification of pollutants, and the control of pest/disease, and they provide habitat for wild species (Fisher et al., 2009). Inadequate environmental management reduces the benefits of ecosystem services, and threatens the sustainability of biodiversity, including human diversity.
In terrestrial ecosystems, the rising conflict between humans and wildlife has increased habitat competition to the detriment of flora and fauna, which has meant changes in land cover, especially in areas with increasing agricultural/forestry activities. Natural habitat loss favors the interaction between wildlife, domestic animals, and humans. Scientific evidence supports the idea that a greater interaction between humans and animals enhances the transmission of pathogens (Jones et al., 2013). Pathogenic viruses and bacteria have co-evolved with their original animal hosts in such a way that they do not produce severe effects on them, but can have catastrophic health effects if they cross over to infect new human hosts (Zohdy et al., 2019), as evidenced by the current global scenario. A substantial number of the emerging infectious diseases that affect humans are zoonotic, mostly originated in wildlife (Chomel et al., 2007). The zoonotic capacity of viruses of the family Coronaviridae is not recent, as zoonotic outbreaks have been reported since 1960. The first coronavirus causing lethal severe acute respiratory syndrome (SARS) was reported in 2002. The SARS-CoV-1outbreak originated in Guangdong (China) and spread to 29 countries. In 2012, a zoonotic outbreak of a β-coronavirus was reported in Saudi Arabia. This virus, called MERS-CoV, spread to 27 countries. In contrast, SAS-CoV-2 resulting from zoonosis has spread to over 166 countries (Docea et al., 2020). For these reasons, it is important to manage natural environments correctly, preventing pathogens from leaving their natural environment and the species with which they have co-evolved. At present, many of these infectious agents found in wildlife are unknown.
Ecosystems can degrade or retain anthropogenic pollutants (Philp et al., 2005). Net primary production through chemical weathering of mineral silicates, occlusion of carbon to soil phytoliths, and the oceanic biological silicon pump, can be powerful allies in atmospheric carbon reduction programs (Carey and Fulweiler, 2012). The scarcity of green spaces and the high atmospheric emissions of human activities in mega-cities, result in high concentrations of air pollution in nearby inhabited areas (Chen et al., 2019). Correct environmental management also allows regulating the climate, for example. But, if there are too few green areas in a city, the average temperature increases, and the humidity decreases (Fisher et al., 2009), generating a man-made microclimate within a city with its own rainfall, snowfall, air pressure, and wind patterns. The spread of emerging infectious diseases such as COVID-19 has a link to unsustainable use of the environment.
3. Pollutants and their relationship to COVID-19
Pollutants such as persistent organic pollutants (polychlorinated biphenyls (PCBs), polycyclic aromatic hydrocarbons (PAHs), organochlorines, organophosphates, carbamates, dioxins), heavy metals, methylmercury, and endocrine disrupters have increased their concentrations and widened their presence in the environment due to anthropogenic activities (intensive industrial activities and population increase). These chemicals pollutants are widely disseminated worldwide, and can be found in water, air, soil, vegetation, and animals (Hill, 2020). Their main route of exposure in animals and humans is through diet (Thompson and Darwish, 2019). They produce many biological effects on wildlife and humans, including immunological, mutagenic, and reproductive alterations (Yu et al., 2011). A continuous increase in chronic and infectious diseases associated with contaminant exposure has been observed in recent decades (DeSantis et al., 2019; Dimakakou et al., 2018; Liu et al., 2019). A relationship between pollutants and viral diseases (such as COVID-19) was recently reported (Tsatsakis et al., 2020). They found that these chemical stressors share some action mechanisms capable to alter Toll-like receptors, growth factors, cytokine receptors, and B cell receptors. Similarly, both can affect the metabolism of Ca2+, K+, Cl−, and vitamin D, and both affect inflammatory processes and disrupt redox biology (increasing reactive oxygen species and oxidative stress). This is an important finding, because pollutants can depress the immune system of animals and thus might increase the impacts of pathogens, such as the current global coronary disease (COVID-19).
The main effects of COVID-19 on human health are related to respiratory problems (Xu et al., 2020b). The respiratory system can also be affected by air pollution, mainly by fine particulate matter (PM2.5, PM10) produced by diesel engine combustion, coal and wood burning, and industrial emissions (Garcia-Chevesich et al., 2014). This fine particulate matter can obstruct the airways, exacerbating the effects of COVID-19. In addition, fine particulate matter contains organic pollutants, heavy metals, dust, and pollen that can disrupt immune responses (Tsatsakis et al., 2020). Particulate matter can interfere with LL37 (a peptide involved in innate immune response) and may reduce effective immunity of the organism (Crane-Godreau et al., 2020). Some research has correlated fine particulate matter (PM2.5, PM10) with confirmed cases of deaths due to COVID-19 (Table 1 ).
Table 1.
Air pollution variation due to COVID-19 lockdown measures in different countries.
| Author | Country | Area covered | Environmental pollution | Conclusions |
|---|---|---|---|---|
| Wu et al., 2020a | USA | 3000 cities | PM2.5 | An increase of 1 μg/m3 of PM2.5 explained an 8% increase of COVID-19 mortality rate |
| Bashir et al., 2020a | USA | California | PM2.5, PM10, SO2, NO2, Pb, VOC and CO | PM2.5, PM10, SO2, NO2, and CO have a significant correlation with COVID-19 |
| Yongjian et al., 2020 | China | 120 cities | PM2.5, PM10, NO2 and O3 | Confirmed cases increase by 2.24%, 1.76%, 6.94% and 4.76%, respectively |
| Yao et al., 2020 | China | 49 cities | PM2.5 and PM10 | PM2.5 and PM10 increased 0.24% and 0.26% the case fatality of COVID-19, respectively |
| Zhang et al., 2020 | China | 219 cities | Air quality index | Air pollution has exerted a positive impact on the transmission and infection by COVID-19 |
| Xu et al., 2020a | China | 33 locations | Air quality index (AQI) | There is a direct correlation between AQI and confirmed COVID-19 cases |
| Fattorini and Regoli, 2020 | Italy | 71 provinces | NO2, O3, PM2.5 and PM10 | Significant correlation between poor air quality and COVID-19 cases |
| Zoran et al., 2020 | Italy | Milan | PM2.5 and PM10 | New COVID-19 cases have positively correlated with PM2.5 and PM10 |
| Filippini et al., 2020 | Italy | 28 provinces of Northern Italy | NO2 | High NO2 levels were associated with COVID-19 spread |
| Saha et al., 2020 | India | 25 cities | PM2.5, PM10, NO2, SO2, CO, and O3 | Significant correlation between poor air quality and COVID-19 deaths |
| Pansini and Fornacca, 2020 | China, Italy and USA | Countrywide | PM2.5, PM10, O3, NO2, SO2 and CO | Significant correlation between air quality and COVID-19 spread and mortality |
| Travaglio et al., 2020 | England | Countrywide | O3, NO and NO2 | Ozone, nitrogen oxide and nitrogen dioxide are significantly associated with COVID-19 deaths |
| Andree, 2020 | Netherlands | 355 municipalities | PM2.5 and PM10 | PM2.5 can be a significant predictor of the number of confirmed COVID-19 cases |
| Magazzino and Schneider, 2020 | French | Paris, Lyon, and Marseille | PM2.5 and PM10 | Suggests that there are certain conditions that increase the likelihood of the spread and aggravation of the disease |
| Suhaimi et al., 2020 | Malaysia | Kuala Lumpur | PM2.5, PM10, SO2, NO2, CO and O3 | Air pollutant influenced the incidence of COVID-19 cases |
| Ogen, 2020 | Italy, Spain, France and Germany | 66 administrative regions | NO2 | The long-term exposure to nitrogen dioxide may contribute to fatality caused by COVID-19 |
In a study covering 98% of the United States population, Wu et al. (2020a, Table 1) considered more than 20 different factors that may influence deaths, among which were individual conditions (obesity, smoking, age), epidemiological (time of onset of outbreak and time in which confinement was decreed), population (size, density), socioeconomic (hospital beds), and climate. They found a strong relationship between PM2.5 and death risk from COVID-19. Similar findings were reported regarding China (Pansini and Fornacca, 2020; Xu et al., 2020a; Yao et al., 2020; Yongjian et al., 2020; Zhang et al., 2020), Italy (Fattorini and Regoli, 2020; Filippini et al., 2020; Zoran et al., 2020), England (Travaglio et al., 2020), Netherlands (Andree, 2020), France (Magazzino and Schneider, 2020), Malaysia (Suhaimi et al., 2020), Germany (Ogen, 2020), and India (Saha et al., 2020). The study conducted by Saha et al. (2020) also reported that areas with better air quality showed a larger number of COVID-19 recoveries. Concerns have been raised regarding an association of indoor air pollution with susceptibility to COVID-19, mainly in geographical areas where wood or coal is still used for cooking and heating (Mbandi, 2020; Sharma and Hossain, 2020).
All available research so far show a positive correlation between air pollution (PM2.5) and COVID-19. Moreover, a recent study showed that fine particulate matter (PM2.5) is a carrier of SARS-CoV-2, indicated by the presence of viral RNA (Setti et al., 2020), although more research is needed on this matter. The evidence indicates that particulate matter appears to play a key role in the incidence and severity of cases of COVID-19, because it acts as a carrier of viruses, influences lung obstruction, and produces immunological effects by chemicals associated with it. The underlying question here is whether multiple pollutants carried simultaneously on particulate matter act in an additive, synergistic way to increase the severity of COVID-19-like diseases.
4. Environmental factors and the spread of SARS-CoV-2
The main form of SARS-CoV-2 transmission that has been identified is person-to-person, which occurs by touching infected surfaces and then touching the mouth, nose, or eyes (Peng et al., 2020). However, virus transmission probably also occurs through inhaling respiratory droplets exhaled by animals and humans (Qu et al., 2020). The influence of environmental factors on SARS-CoV-2 transmission has been examined. Chin et al. (2020) reported that SARS-CoV-2 viruses can survive for a long time at temperatures between −2 and 4 °C, while they can survive only 5 min at 70 °C. They are also stable at ambient temperature at a pH range of 3–10 (Chin et al., 2020).
The relationships between confirmed cases or deaths by COVID-19 and environmental factors has been studied in Europe, Middle East, and Asia (mainly China, Table 2 ). Temperature appears to be the environmental factor most related to COVID-19 spreading. However, those recent results should be weighed with caution. A study performed in several locations of China found that environmental factors by themselves could not explain variations in those cases of confirmed COVID-19 (Poirier et al., 2020). Interestingly, environmental variables have been found to be crucial just in the initial phase of the COVID-19 infection, during which time the dynamics of transmission are more affected by airborne viral infectivity rather than human-to-human transmission (Coccia, 2020). Other studies from Indonesia (Tosepu et al., 2020), USA (Bashir et al., 2020b), Spain (Briz-Redón and Serrano-Aroca, 2020), Iraq (Amin and Amin, 2020), Singapore (Pani et al., 2020), Chile (Correa-Araneda et al., 2020), Mexico (Méndez-Arriaga, 2020), Brazil (Prata et al., 2020), Germany (Biktasheva, 2020), Turkey (Şahin, 2020), Norway (Menebo, 2020), Ghana (Iddrisu et al., 2020), Iran (Ahmadi et al., 2020) and Japan (Hirata et al., 2020) support this finding.
Table 2.
Environmental factors linked to COVID-19 cases, and associated deaths.
| Climate parameters | Country | Conclusions | Authors |
|---|---|---|---|
| Temperature | Worldwide | COVID-19 fast-spreading has an association with average high and low temperatures | Iqbal et al., 2020a |
| 166 countries | Temperature was negatively correlated with daily new cases and deaths by COVID-19 | Wu et al., 2020b | |
| China | At low temperatures, a raise of 1 °C increased the number of COVID-19 confirmed cases by a rate of 0.83, while at higher temperatures each 1 °C increase reduced the number of confirmed cases by a rate of 0.86 | Wang et al., 2020a | |
| China | Low temperature and mild daytime temperature range promote SARS-CoV-2 transmission | Liu et al., 2020b | |
| China | An increase of 1 °C decreases between 36% and 57% COVID-19 infested cases | Qi et al., 2020 | |
| China | An increase of 1 °C increased COVID −19 deaths by 2.92% | Ma et al., 2020 | |
| China | Temperature played no role on COVID-19 at Wuhan (China) | Iqbal et al., 2020b | |
| China | Positive relationship (Hubei, Hunan and Anhui provinces) and negative relationship (Zhejiang and Shandong provinces) between temperature and COVID-19 | Shahzad et al., 2020 | |
| China | The incidence of COVID-19 decreased with an increase of temperature | Shi et al., 2020 | |
| China | Ambient temperature has a significantly negative effect on COVID-19 transmission | Zhang et al., 2020 | |
| China and Italy | Moderate relationship with COVID-19 confirmed cases | Bhattacharjee, 2020 | |
| USA | Average and minimum temperatures have significant correlation with COVID-19 at New York City. | Bashir et al., 2020 | |
| Indonesia | Temperature average was significantly correlated with COVID-19 | Tosepu et al., 2020 | |
| Spain | No correlation between COVID-19 cases and temperature was found | Briz-Redón and Serrano-Aroca, 2020 | |
| Iraq | Low temperatures might enhance COVID-19 infection risk | Amin and Amin, 2020 | |
| Singapore | Temperature showed positive significant associations with SARS-CoV-2 transmission | Pani et al., 2020 | |
| Chile | Lower temperature can favor COVID-19 transmission speed | Correa-Araneda et al., 2020 | |
| Mexico | Temperature associates negatively with the local confirmed COVID-19 cases | Méndez-Arriaga, 2020 | |
| Brazil | 1 °C rise was associated with a 4.9% decrease in the number of daily cumulative COVID-19 confirmed cases | Prata et al., 2020 | |
| Turkey | Temperature have high impacts on COVID-19 cases | Şahin, 2020 | |
| Italy | Warm season promotes COVID-19 spreading | Zoran et al., 2020 | |
| Norway | Maximum and normal temperature are positively associated with COVID-19 | Menebo, 2020 | |
| Ghana | Maximum temperature significantly predict COVID-19 new cases | Iddrisu et al., 2020 | |
| Humidity | 166 countries | Relative humidity was negatively related to daily new cases and deaths by COVID-19 | Wu et al., 2020b |
| China and Italy | No relationship between humidity and COVID-19 confirmed cases | Bhattacharjee, 2020 | |
| China | 1% increase in relative humidity decreased 11–22% COVID-19 infected cases | Qi et al., 2020 | |
| China | Relative humidity is negatively associated with COVID-19 daily deaths | Ma et al., 2020 | |
| China | Low humidity promotes the transmission of SARS-CoV-2 | Liu et al., 2020b | |
| Iraq | Increased relative humidity might enhance virus infection risk | Amin and Amin, 2020 | |
| Singapore | Humidity showed positive significant associations with SARS-CoV-2 transmission | Pani et al., 2020 | |
| Japan | The absolute humidity affected SARS-CoV-2 spread duration | Hirata et al., 2020 | |
| Chile | Lower humidity can favor coronavirus transmission speed | Correa-Araneda et al., 2020 | |
| Germany | Lower humidity increased Covid-19 mortality | Biktasheva, 2020 | |
| Italy | Dry air supports COVID-19 transmission | Zoran et al., 2020 | |
| Norway | Precipitation are negatively associated with COVID-19 | Menebo, 2020 | |
| Ghana | Relative humidity was significantly associated with daily new cases and new deaths of COVID-19 | Iddrisu et al., 2020 | |
| Iran | Low humidity associated with high SARS-CoV-2 infection rate | Ahmadi et al., 2020 | |
| Wind | China and Italy | No relationship between wind and COVID-19 confirmed cases | Bhattacharjee, 2020 |
| Chile | Higher wind speed can favor a higher disease transmission speed | Correa-Araneda et al., 2020 | |
| Turkey | Wind speed have high impacts on COVID-19 cases | Şahin, 2020 | |
| Iran | Low wind speed associated with high rate of infection of SARS-CoV-2 | Ahmadi et al., 2020 |
Although SARS-CoV-2 RNA has been detected in the air (Liu et al., 2020c), the way environmental factors may affect COVID-19 transmission is not well established. It is necessary to assess whether environmental factors really have a cause-and-effect relationship for infection cases or deaths by COVID-19. The spread of SARS-CoV-2 is very complex, because the factors involved, including climatic factors, are very heterogeneous and dynamic, even confining observations to a single city during daylight hours. This heterogeneity of climatic factors generates dynamic scenarios that influences the number of confirmed cases (Sarkodie and Owusu, 2020b). This dynamic in the factors involved and the political decisions taken to address them (e.g. as effective containment, Asamoah et al., 2020) influence on environmental health and economic systems in the different countries (Sarkodie and Owusu, 2020a).
5. Indirect impact of COVID-19 on the environment
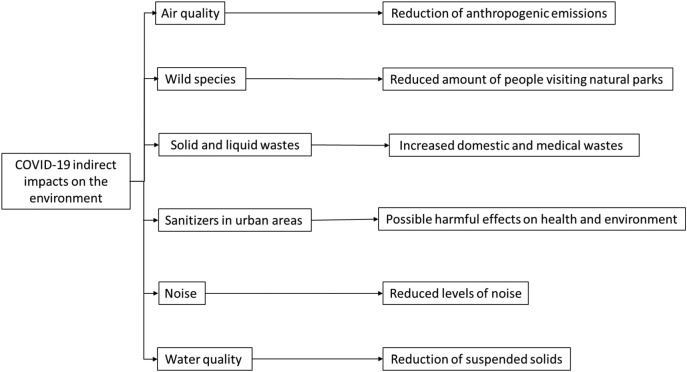
There is evidence for an indirect effect (negative/positive) of COVID-19 on environmental outcomes, mainly related to preventive confinement measures on the population imposed worldwide by various authorities (Fig. 1 , Braga et al., 2020, Corlett et al., 2020, Saadat et al., 2020, Zambrano-Monserrate et al., 2020).
Fig. 1.
Schematic representation of COVID-19 indirect impacts on the environment.
5.1. Indirect impact on air quality
The worldwide COVID-19 pandemic has caused various positive impacts on the environment and the climate (Sarkodie and Owusu, 2020a). A global daily CO2 emission decrease about 17% has been estimated, reaching CO2 emission levels similar to those in 2006 (Le Quéré et al., 2020). In China, the reduction in the use of coal (50%) and oil (20–30%) caused a 25% CO2 decrease, equivalent to 6% of global emissions (Myllyvirta, 2020). Ten cities in China exhibited a 20% decrease of PM2.5 (Wang et al., 2020b). In Kazakhstan, a reduction of CO (49%) and NO2 (35%) was found (Kerimray et al., 2020), whereas a 50% and 62% reduction of NO2 concentrations was reported from Barcelona and Madrid, respectively (Baldasano, 2020). Also, a significant reduction of NO2 was noted in Turkey (Kaplan and Avdan, 2020). In USA, NO2 declined around 25% during the COVID-19 pandemic as compared to 2017–2019 levels (Berman and Ebisu, 2020). In Brazil, a decrease of CO (64.8%), NO (77.3%), NO2 (54.3%) was found in São Paulo (Nakada and Urban, 2020), and significant reductions of CO and NO2 in Rio de Janeiro (Dantas et al., 2020). In Morocco, a 5% decrease of PM10, 49% of SO2, and 96% of NO2 were reported (Otmani et al., 2020). Other studies have indicated a PM2.5 decrease in Asian (India, China) and European (Spain, France, and Italy) countries (Gautam, 2020). Prior to the COVID-19 pandemic, greenhouse gases raised average global temperatures, causing melting of glaciers and rising sea levels. The reduction of economic activities during this pandemic has temporary stopped global warming as well as air and marine pollution, allowing the environment slowly flourish (Sarkodie and Owusu, 2020a). Another positive impact is the environmental protection through the European Union's seven-year recovery plan called “Next Generation EU”, which seeks to reserve 25% of EU spending for climate-friendly expenditures (Jones et al., 2020). However, these partial improvements are unlikely to mitigate pollution in the long term. Adverse weather conditions (low wind, high humidity, and a greater number of foggy days) may stop the reduction of air pollution and thus have a significant impact (Wang et al., 2020b). Some locations in the Southern Hemisphere use mostly wood for heating during the cold season or for daily cooking (Sanhueza et al., 2009). The use of wood for heating, along with other commonly used fossil fuel, probably increases outdoor and/or indoor air pollution, which is worrisome considering that air pollution is associated with COVID-19 (Setti et al., 2020; Wu et al., 2020b).
5.2. Indirect impact on wildlife species
Restriction measures during this pandemic have notably reduced the number of people visiting natural parks, thus diminishing stress on wild fauna (Corlett et al., 2020). Wild animals have been returning towards suburban areas from which they previously fled because of the human presence (Corlett et al., 2020). On the other hand, some countries are allowing tourists to visit protected areas as a measure for reducing the stress generated by the pandemic (Corlett et al., 2020). Hence, it will be crucial to have regulations for protecting wildlife, as more visitors may increase stress and pollution within protected areas. In light of these observations, it is expected that most countries will develop strict protocols concerning X before confinement orders are lifted.
5.3. Indirect impact on solid and liquid waste
During the recent periods of confinement, people have stopped attending entertainment and recreation areas (parks, beaches, ski centers, music concerts, among others). Consequently, waste in public places and natural and urban areas has been reduced (Zambrano-Monserrate et al., 2020). People are expected to return to social recreation activities after confinement, probably causing a dramatic increase of waste in public places.
Now, domestic and hospital waste has increased due to the difficulty of satisfactory solid and liquid waste management (Platon et al., 2020). In the case of domestic waste, food delivery containers have notoriously increased in number. Some countries have suspended their recycling to reduce possible virus infection and protect workers (Zambrano-Monserrate et al., 2020). Only a part of the plastic waste is being recycled, while the rest goes to landfills or is thrown into the environment (Klemeš et al., 2020). In Wuhan (China), clinical waste increased four times, reaching 200 tons per day (Saadat et al., 2020). To prevent the possible spread of the virus, hospitals have stopped recycling glass-made medical materials, although they may be biologically harmless to workers.
Hospital wastewater usually contains high levels of drugs, and one would expect that their concentrations and diversity has increased during the COVID-19 pandemic due to a higher demand by patients (Escher et al., 2011; Jelic et al., 2011; Ort et al., 2010). Hydroxychloroquine and chloroquine are some of the drugs that have been used to treat COVID-19 (Liu et al., 2020a). These drugs have been described as persistent, bioaccumulative, and dangerous to aquatic organisms (Ramesh et al., 2018), and they are considered emerging pollutants (Daughton, 2014; Zurita et al., 2005). This is highly relevant since it is known that wastewater treatment systems do not have adequate processes for treatment these drugs, which will enter into freshwater ecosystems (Ashfaq et al., 2017).
As of July 2020, there are more than 15 million confirmed COVID-19 cases around the world, and an unknown number of negative cases (Dong et al., 2020). Confirmation has generally taken place in diagnostic laboratories. Those laboratories usually use disposable supplies, generating large amounts of plastics and chemicals that pollute soil and water (Corman et al., 2020). Most personal prevention equipment, such as reusable masks and disinfectant containers, contain plastic (Das et al., 2020; Fadare and Okoffo, 2020; Saadat et al., 2020). Devices that are used as physical barriers to control people near restricted areas are made of methacrylate (a transparent, flexible and resistant plastic material), which comes from propylene (an oil derivative). When ending their useful life, those products reach landfills or the environment. In Asian countries, an increase of disposable masks and gloves has been reported on beaches (Saadat et al., 2020) and the sea floor (CNN, 2020). Along with plastic waste, disposable masks can reach land and aquatic systems, where animals may become entangled or eat them by mistake (Sigler, 2014; Vegter et al., 2014). Recent evidence has shown that microplastics can reach remote regions of the planet, and also end up in our bodies through food intake and breathing (Allen et al., 2020).
The incineration of contaminated medical wastes is a source of pollution as well, which can have a significant impact on Public health (Tait et al., 2020; Walker and Cooper, 1992). The use of this technique to eliminate coronavirus may have indirect health consequences over time.
5.4. Other indirect impact
The use of sanitizers in public environments has been a practice employed by some countries during the pandemic (Atolani et al., 2020). For example, triclosan is a universal antimicrobial used in drugs and personal care products, as well as growth promoting antibiotics in food animal production (Daughton and Ternes, 1999). Therefore, triclosan is classified as an emerging contaminant (Wang et al., 2018). Excessive use of this and other sanitizers can have harmful effects on health and environment.
Confinement has also led to a reduction of noise, mainly due to the reduction of traffic congestion, airflights, and commercial activities (Zambrano-Monserrate et al., 2020). Noise reduction might help birds, as noise has been shown to have negative effects on physiology, nesting, and reproduction of birds in urban areas (Zollinger et al., 2019).
In addition, water quality improvement has been reported in Venice (Italy), where clear waters were observed due to the reduction of suspended solids, because of lesser use of motorboats (Braga et al., 2020).
Considering all of the above, it is expected that when the confinement around the planet is finally over, all anthropogenic activities will return to their pre-pandemic state, and the present reduction of human impacts will no longer prevail on Earth (McCloskey and Heymann, 2020). On the contrary, plastics and drugs in wastewater produced during this pandemic by COVID-19 will persist longer, particularly those are not biodegradable.
6. Recommendations for future epidemic threats
Certainly, people's confinement has limited the possibilities for data collection concerning the relationship between indoor air quality parameters and human health status. Based on technological advances, we believe that “smart care”, “smart home”, and “health monitoring gadget” can be powerful allies to collect data remotely. Data standardization and the accessibility of data from any platforms should help smart technology to be valuable in the event of a pandemic (Allam and Jones, 2020).
There are key lessons that can be learned from COVID-19, which relate to the need to be prepared and environmentally responsible. Following them will help control future pandemics. The “one health” approach, which integrates environmental science, veterinary science, and health science research, should be pivotal (Bonilla-Aldana et al., 2020). Having good interaction between these areas might guarantee quick and timely feedback in case of future epidemic episodes. In addition, researchers, medical personnel and social leaders need to work together to design strategies based on environmental and socio-economic terms, and not only on health sciences. This pandemic provides an opportunity to remember that human beings are linked to a healthy environment, especially in countries that are highly dependent on their natural resources.
In order to prevent any future pandemics, proper environmental management to avoid the transmission of viruses from wild species to humans will be required (Zohdy et al., 2019). More studies on wildlife virology and wildlife immunology should be carried out to identify potential pathogens and how wild animals cope with them.
Urban management is vital and must be taken into consideration when designing cities. Urban land-use planning must give more emphasis to the positive benefits that ecosystem services provide so that they can help to reduce infection and disease. The megacities model must be reformulated. Fortunately, technological advances allow us to carry out activities remotely, which helps us to interact despite distance. Small village models should be considered, thus decreasing population density and helping to avoid saturating an ecosystem, giving it the possibility to cope with low atmospheric emissions. Governments should enforce environmental and sustainable policies based on the use of green energies in order to reduce air pollution. In the end, public health will benefit from a natural environment, with all that this entails.
Chemical management should be integrated, not only motivated by the direct adverse effects that a pollutant individually may have on wildlife and human health but also the synergistic effects as a whole associated with infectious agents. The environmental impacts that this pandemic will bring are of global scope (Saadat et al., 2020), and the attention the pandemic has commanded should be redirected towards controlling anthropogenic pollution, towards improvements in waste management during periods of extreme confinement, and towards confronting increases in medical waste. The potential rebound of pollutant emissions may be generated after confinement as an attempt to revive the global economy is worrisome (Sarkodie and Owusu, 2020a). On the other hand, massive amounts of domestic and hospital waste have been generated during this pandemic, mostly plastics; this increase might hinder actions currently ongoing to reduce plastic usage and it is dumping into the environment. Initiatives to seek alternatives to plastic for routine domestic and medical tasks should be encouraged. It is necessary to establish preventive epidemiological models (e.g., monitoring of domestic wastewater) to detect the occurrence of COVID-19 in advance. Wastewater plants should include effective treatments for dealing with a high concentration of drugs. All these actions could help to design protocols according to environmentally sustainable practices for facing a pandemic in the future.
CRediT authorship contribution statement
Winfred Espejo: Conceptualization, Investigation, Resources, Writing - original draft. José E. Celis: Writing - original draft. Gustavo Chiang: Writing - review & editing. Paulina Bahamonde: Investigation, Resources, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
W. Espejo thanks the Society of Toxicology of Chile (SoTox), as this article originated from a requested talk. W. Espejo is supported by the postdoc 219.153.026-P of the VRID (Universidad de Concepción), Chile. P. Bahamonde is supported by Nucleo Milenio INVASAL funded by Chile's Government Program, P. Bahamonde also thanks the projects FONDECYT Initiation 11180914. G. Chiang is supported by CAPES, Center for Applied Ecology and Sustainability. Thanks to Jeff Elhai for reviewing the English of the manuscript.
Editor: Jay Gan
References
- Ahmadi M., Sharifi A., Dorosti S., Ghoushchi S.J., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allam Z., Jones D.S. Healthcare. vol 8. Multidisciplinary Digital Publishing Institute; 2020. On the coronavirus (COVID-19) outbreak and the smart city network: universal data sharing standards coupled with artificial intelligence (AI) to benefit urban health monitoring and management; p. 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen S., Allen D., Moss K., Le Roux G., Phoenix V.R., Sonke J.E. Examination of the ocean as a source for atmospheric microplastics. PLoS One. 2020;15(5) doi: 10.1371/journal.pone.0232746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amin H.N.M., Amin H.N.M. Climate analysis to predict potential spread and seasonality for global (COVID-19) in Iraqi Kurdistan region. Kurdistan Journal of Applied Research. 2020:72–83. [Google Scholar]
- Andree B.P.J. The World Bank; 2020. Incidence of COVID-19 and Connections with Air Pollution Exposure: Evidence from the Netherlands. [Google Scholar]
- Asamoah E.F., Kwaku E., Sarkodie S.A., Maina J. 2020. Effective Containment Explains the Velocity of COVID-19 Spread. (Available at SSRN 3625341) [Google Scholar]
- Ashfaq M., Khan K.N., Rehman M.S.U. Ecological risk assessment of pharmaceuticals in the receiving environment of pharmaceutical wastewater in Pakistan. Ecotoxicol. Environ. Saf. 2017;136:31–39. doi: 10.1016/j.ecoenv.2016.10.029. [DOI] [PubMed] [Google Scholar]
- Atolani O., Baker M.T., Adeyemi O.S. Letter to the editor: COVID-19: critical discussion on the applications and implica-tions of chemicals in sanitizers and disinfectants. EXCLI J. 2020;19:785–799. doi: 10.17179/excli2020-1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldasano J.M. COVID-19 lockdown effects on air quality by NO2 in the cities of Barcelona and Madrid (Spain) Sci. Total Environ. 2020;741 doi: 10.1016/j.scitotenv.2020.140353. [DOI] [PubMed] [Google Scholar]
- Bashir M.F., Bilal B.M., Komal B. Correlation between environmental pollution indicators and COVID-19 pandemic: a brief study in Californian context. Environ. Res. 2020;187 doi: 10.1016/j.envres.2020.109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman J.D., Ebisu K. Changes in US air pollution during the COVID-19 pandemic. Sci. Total Environ. 2020;739 doi: 10.1016/j.scitotenv.2020.139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernhardt E.S., Rosi E.J., Gessner M.O. Synthetic chemicals as agents of global change. Front. Ecol. Environ. 2017;15(2):84–90. [Google Scholar]
- Bhattacharjee S. arXiv preprint arXiv:200311277. 2020. Statistical investigation of relationship between spread of coronavirus disease (COVID-19) and environmental factors based on study of four mostly affected places of China and five mostly affected places of Italy. [Google Scholar]
- Biktasheva I.V. Role of a habitat’s air humidity in Covid-19 mortality. Sci. Total Environ. 2020;736 doi: 10.1016/j.scitotenv.2020.138763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boger D., Hart B. 2008 International Seminar on Paste and Thickened Tailings, Gaborone, Botswana. 2008. Making an unsustainable industry more sustainable; pp. 3–5. [Google Scholar]
- Bonilla-Aldana D.K., Dhama K., Rodriguez-Morales A.J. Revisiting the one health approach in the context of COVID-19: a look into the ecology of this emerging disease. Adv Anim Vet Sci. 2020;8(3):234–237. [Google Scholar]
- Braga F., Scarpa G.M., Brando V.E., Manfè G., Zaggia L. COVID-19 lockdown measures reveal human impact on water transparency in the Venice lagoon. Sci. Total Environ. 2020;736 doi: 10.1016/j.scitotenv.2020.139612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briz-Redón Á., Serrano-Aroca Á. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey J.C., Fulweiler R.W. The terrestrial silica pump. PLoS One. 2012;7(12) doi: 10.1371/journal.pone.0052932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M., Dai F., Yang B., Zhu S. Effects of neighborhood green space on PM2. 5 mitigation: evidence from five megacities in China. Build. Environ. 2019;156:33–45. [Google Scholar]
- Chin A., Chu J., Perera M. Stability of SARS-CoV-2 in different environmental conditions. medRxiv. 2020 doi: 10.1101/2020.03.15.20036673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomel B.B., Belotto A., Meslin F.-X. Wildlife, exotic pets, and emerging zoonoses. Emerg. Infect. Dis. 2007;13(1):6. doi: 10.3201/eid1301.060480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CNN Conservationists warn Covid waste may result in more masks than jellyfish' in the sea. 2020. https://edition.cnn.com/2020/06/24/us/plastic-pollution-ocean-covid-waste-trnd/index.html
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corlett R.T., Primack R.B., Devictor V. Impacts of the coronavirus pandemic on biodiversity conservation. Biol. Conserv. 2020;246 doi: 10.1016/j.biocon.2020.108571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman V.M., Landt O., Kaiser M. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correa-Araneda F., Ulloa-Yañez A., Núñez D. 2020. Environmental Determinants of COVID-19 Transmission across a Wide Climatic Gradient in Chile. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane-Godreau M.A., Clem K.J., Payne P., Fiering S. Vitamin D deficiency and air pollution exacerbate COVID-19 through suppression of antiviral peptide LL37. Front. Public Health. 2020;8:232. doi: 10.3389/fpubh.2020.00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantas G., Siciliano B., França B.B., da Silva C.M., Arbilla G. The impact of COVID-19 partial lockdown on the air quality of the city of Rio de Janeiro, Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das O., Neisiany R.E., Capezza A.J. The need for fully bio-based facemasks to counter coronavirus outbreaks: a perspective. Sci. Total Environ. 2020;736 doi: 10.1016/j.scitotenv.2020.139611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughton C.G. The Matthew effect and widely prescribed pharmaceuticals lacking environmental monitoring: case study of an exposure-assessment vulnerability. Sci. Total Environ. 2014;466:315–325. doi: 10.1016/j.scitotenv.2013.06.111. [DOI] [PubMed] [Google Scholar]
- Daughton C.G., Ternes T.A. Pharmaceuticals and personal care products in the environment: agents of subtle change? Environ. Health Perspect. 1999;107(Suppl. 6):907–938. doi: 10.1289/ehp.99107s6907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis C.E., Ma J., Gaudet M.M. Breast cancer statistics, 2019. CA Cancer J. Clin. 2019;69(6):438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- Dimakakou E., Johnston H.J., Streftaris G., Cherrie J.W. Exposure to environmental and occupational particulate air pollution as a potential contributor to neurodegeneration and diabetes: a systematic review of epidemiological research. Int. J. Environ. Res. Public Health. 2018;15(8):1704. doi: 10.3390/ijerph15081704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Docea A.O., Tsatsakis A., Albulescu D. A new threat from an old enemy: re-emergence of coronavirus. Int. J. Mol. Med. 2020;45(6):1631–1643. doi: 10.3892/ijmm.2020.4555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eagles-Smith C.A., Silbergeld E.K., Basu N. Modulators of mercury risk to wildlife and humans in the context of rapid global change. Ambio. 2018;47(2):170–197. doi: 10.1007/s13280-017-1011-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escher B.I., Baumgartner R., Koller M., Treyer K., Lienert J., McArdell C.S. Environmental toxicology and risk assessment of pharmaceuticals from hospital wastewater. Water Res. 2011;45(1):75–92. doi: 10.1016/j.watres.2010.08.019. [DOI] [PubMed] [Google Scholar]
- Fadare O.O., Okoffo E.D. Covid-19 face masks: a potential source of microplastic fibers in the environment. Sci. Total Environ. 2020;737:140279. doi: 10.1016/j.scitotenv.2020.140279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filippini T., Rothman K.J., Goffi A. Satellite-detected tropospheric nitrogen dioxide and spread of SARS-CoV-2 infection in northern Italy. Sci. Total Environ. 2020;739 doi: 10.1016/j.scitotenv.2020.140278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher B., Turner R.K., Morling P. Defining and classifying ecosystem services for decision making. Ecol. Econ. 2009;68(3):643–653. [Google Scholar]
- Garcia-Chevesich P.A., Alvarado S., Neary D.G. Respiratory disease and particulate air pollution in Santiago Chile: contribution of erosion particles from fine sediments. Environ. Pollut. 2014;187:202–205. doi: 10.1016/j.envpol.2013.12.028. [DOI] [PubMed] [Google Scholar]
- Gautam S. COVID-19: air pollution remains low as people stay at home. Air Quality, Atmosphere, & Health. 2020:1. doi: 10.1007/s11869-020-00842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill M.K. Cambridge University Press; 2020. Understanding Environmental Pollution. [Google Scholar]
- Hirata A., Kodera S., Gomez-Tames J., Rashed E.A. 2020. Influence of Absolute Humidity and Population Density on COVID-19 Spread and Decay Durations: Multi-Prefecture Study in Japan. arXiv preprint arXiv:200602197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter P. More science in urban development: scientific evidence is crucial for managing health and infrastructures of megacities. EMBO Rep. 2017;18(2):201–204. doi: 10.15252/embr.201643843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iddrisu W.A., Appiahene P., Kessie J.A. 2020. Effects of Weather and Policy Intervention on COVID-19 Infection in Ghana. arXiv preprint arXiv:200500106. [Google Scholar]
- Iqbal M.M., Abid I., Hussain S., Shahzad N., Waqas M.S., Iqbal M.J. The effects of regional climatic condition on the spread of COVID-19 at global scale. Sci. Total Environ. 2020;739 doi: 10.1016/j.scitotenv.2020.140101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal N., Fareed Z., Shahzad F., He X., Shahzad U., Lina M. Nexus between COVID-19, temperature and exchange rate in Wuhan City: new findings from partial and multiple wavelet coherence. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelic A., Gros M., Ginebreda A. Occurrence, partition and removal of pharmaceuticals in sewage water and sludge during wastewater treatment. Water Res. 2011;45(3):1165–1176. doi: 10.1016/j.watres.2010.11.010. [DOI] [PubMed] [Google Scholar]
- Jin Y., Yang H., Ji W. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12(4):372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones B.A., Grace D., Kock R. Zoonosis emergence linked to agricultural intensification and environmental change. Proc. Natl. Acad. Sci. 2013;110(21):8399–8404. doi: 10.1073/pnas.1208059110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones L., Palumbo D., Brown D. BBC News. 2020. Coronavirus: a visual guide to the economic impact.https://www.bbc.com/news/business-51706225 [Google Scholar]
- Kaplan G., Avdan Z.Y. COVID-19: Spaceborne nitrogen dioxide over Turkey. Eskişehir Technical University Journal of Science and Technology A-Applied Sciences and Engineering. 2020;21(2):251–255. [Google Scholar]
- Kerimray A., Baimatova N., Ibragimova O.P. Assessing air quality changes in large cities during COVID-19 lockdowns: the impacts of traffic-free urban conditions in Almaty, Kazakhstan. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.139179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemeš J.J., Van Fan Y., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sust. Energ. Rev. 2020;127 doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Quéré C., Jackson R.B., Jones M.W. Temporary reduction in daily global CO 2 emissions during the COVID-19 forced confinement. Nat. Clim. Chang. 2020:1–7. [Google Scholar]
- Liu J., Hull V., Godfray H.C.J. Nexus approaches to global sustainable development. Nature Sustainability. 2018;1(9):466–476. [Google Scholar]
- Liu Y., Chen S., Zühlke L. Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int. J. Epidemiol. 2019;48(2):455–463. doi: 10.1093/ije/dyz009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Cao R., Xu M. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell discovery. 2020;6(1):1–4. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ning Z., Chen Y. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020:1–4. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magazzino C., Schneider N. 2020. The Relationship between Air Pollution and COVID-19-Related Deaths: An Application to Three French Cities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbandi A.M. Air pollution in Africa in the time of COVID-19: the air we breathe indoors and outdoors. Clean Air Journal. 2020;30(1):1–3. [Google Scholar]
- McCloskey B., Heymann D.L. SARS to novel coronavirus–old lessons and new lessons. Epidemiology & Infection. 2020;148 doi: 10.1017/S0950268820000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Méndez-Arriaga F. The temperature and regional climate effects on communitarian COVID-19 contagion in Mexico throughout phase 1. Sci. Total Environ. 2020;735 doi: 10.1016/j.scitotenv.2020.139560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M.M. Temperature and precipitation associate with Covid-19 new daily cases: a correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737 doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina M.J., Molina L.T. Megacities and atmospheric pollution. J. Air Waste Manage. Assoc. 2004;54(6):644–680. doi: 10.1080/10473289.2004.10470936. [DOI] [PubMed] [Google Scholar]
- Myllyvirta L. Carbon Brief. 2020. Coronavirus temporarily reduced China’s CO2 emissions by a quarter.https://www.carbonbrief.org/analysis-coronavirus-has-temporarily-reduced-chinas-co2-emissions-by-a-quarter [Google Scholar]
- Nakada L.Y.K., Urban R.C. COVID-19 pandemic: impacts on the air quality during the partial lockdown in São Paulo state, Brazil. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.139087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to the coronavirus (COVID-19) fatality rate. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ort C., Lawrence M.G., Reungoat J., Eaglesham G., Carter S., Keller J. Determining the fraction of pharmaceutical residues in wastewater originating from a hospital. Water Res. 2010;44(2):605–615. doi: 10.1016/j.watres.2009.08.002. [DOI] [PubMed] [Google Scholar]
- Otmani A., Benchrif A., Tahri M., Bounakhla M., El Bouch M., Krombi Mh. Impact of Covid-19 lockdown on PM10, SO2 and NO2 concentrations in Salé City (Morocco) Sci. Total Environ. 2020;735 doi: 10.1016/j.scitotenv.2020.139541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani S.K., Lin N.-H., RavindraBabu S. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci. Total Environ. 2020;740 doi: 10.1016/j.scitotenv.2020.140112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pansini R., Fornacca D. 2020. COVID-19 Higher Induced Mortality in Chinese Regions with Lower Air Quality. (DOI 10(2020.04):04.20053595) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. International Journal of Oral Science. 2020;12(1):1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philp J.C., Bamforth S., Singleton I., Atlas R.M. Bioremediation. American Society of Microbiology; 2005. Environmental pollution and restoration: a role for bioremediation; pp. 1–48. [Google Scholar]
- Platon V., Frone S., Constantinescu A., Jurist S. România, prin gestionarea corespunzătoare a deșeurilor medicale periculoase. 2020. Atenuarea impactului COVID-19. [Google Scholar]
- Poirier C., Luo W., Majumder M.S. 2020. The Role of Environmental Factors on Transmission Rates of the COVID-19 Outbreak: An Initial Assessment in Two Spatial Scales. (Available at SSRN 3552677) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R. COVID-19 transmission in mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu G., Li X., Hu L., Jiang G. ACS Publications; 2020. An Imperative Need for Research on the Role of Environmental Factors in Transmission of Novel Coronavirus (COVID-19) [DOI] [PubMed] [Google Scholar]
- Ramesh M., Anitha S., Poopal R.K., Shobana C. Evaluation of acute and sublethal effects of chloroquine (C18H26CIN3) on certain enzymological and histopathological biomarker responses of a freshwater fish Cyprinus carpio. Toxicol. Rep. 2018;5:18–27. doi: 10.1016/j.toxrep.2017.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saadat S., Rawtani D., Hussain C.M. Environmental perspective of COVID-19. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha B., Debnath A., Saha B. 2020. Analysis and Finding the Correlation of Air Quality Parameters on the Spread and Deceased Case of COVID-19 Patients in India. [Google Scholar]
- Şahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanhueza P.A., Torreblanca M.A., Diaz-Robles L.A., Schiappacasse L.N., Silva M.P., Astete T.D. Particulate air pollution and health effects for cardiovascular and respiratory causes in Temuco, Chile: a wood-smoke-polluted urban area. J. Air Waste Manage. Assoc. 2009;59(12):1481–1488. doi: 10.3155/1047-3289.59.12.1481. [DOI] [PubMed] [Google Scholar]
- Sarkodie S.A., Owusu P.A. Global assessment of environment, health and economic impact of the novel coronavirus (COVID-19) Environ. Dev. Sustain. 2020:1–11. doi: 10.1007/s10668-020-00801-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkodie S.A., Owusu P.A. Investigating the cases of novel coronavirus disease (COVID-19) in China using dynamic statistical techniques. Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e03747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G. SARS-Cov-2RNA found on particulate matter of Bergamo in northern Italy: first evidence. Environ. Res. 2020;188 doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahzad F., Shahzad U., Fareed Z., Iqbal N., Hashmi S.H., Ahmad F. Asymmetric nexus between temperature and COVID-19 in the top ten affected provinces of China: a current application of quantile-on-quantile approach. Sci. Total Environ. 2020;736 doi: 10.1016/j.scitotenv.2020.139115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma R., Hossain M.M. 2020. Household Air Pollution and COVID-19 Risk in India: A Potential Concern. [Google Scholar]
- Shi P., Dong Y., Yan H. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigler M. The effects of plastic pollution on aquatic wildlife: current situations and future solutions. Water Air Soil Pollut. 2014;225(11):2184. [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suhaimi N.F., Jalaludin J., Latif M.T. Demystifying a possible relationship between COVID-19, air quality and meteorological factors: evidence from Kuala Lumpur, Malaysia. Aerosol Air Qual. Res. 2020;20 [Google Scholar]
- Tait P.W., Brew J., Che A. The health impacts of waste incineration: a systematic review. Aust. N. Z. J. Public Health. 2020;44(1):40–48. doi: 10.1111/1753-6405.12939. [DOI] [PubMed] [Google Scholar]
- Thompson L.A., Darwish W.S. Environmental chemical contaminants in food: review of a global problem. Journal of toxicology. 2019;2019 doi: 10.1155/2019/2345283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Lestari H., Bahar H., Asfian P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M., Yu Y., Popovic R., Leal N.S., Martins L.M. Links between air pollution and COVID-19 in England. medRxiv. 2020 doi: 10.1101/2020.04.16.20067405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsatsakis A., Petrakis D., Nikolouzakis T.K. COVID-19, an opportunity to reevaluate the correlation between long-term effects of anthropogenic pollutants on viral epidemic/pandemic events and prevalence. Food Chem. Toxicol. 2020;141 doi: 10.1016/j.fct.2020.111418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vegter A.C., Barletta M., Beck C. Global research priorities to mitigate plastic pollution impacts on marine wildlife. Endanger. Species Res. 2014;25(3):225–247. [Google Scholar]
- Walker B.L., Cooper C.D. Air pollution emission factors for medical waste incinerators. J. Air Waste Manage. Assoc. 1992;42(6):784–791. [Google Scholar]
- Wang P., Chen K., Zhu S., Wang P., Zhang H. Severe air pollution events not avoided by reduced anthropogenic activities during COVID-19 outbreak. Resour. Conserv. Recycl. 2020;158 doi: 10.1016/j.resconrec.2020.104814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Jiang A., Gong L. Temperature significant change COVID-19 transmission in 429 cities. MedRxiv. 2020 doi: 10.1101/2020.02.22.20025791. [DOI] [Google Scholar]
- Wang F., Xu R., Zheng F., Liu H. Effects of triclosan on acute toxicity, genetic toxicity and oxidative stress in goldfish (Carassius auratus) Exp. Anim. 2018;67:219–227. doi: 10.1538/expanim.17-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. Exposure to air pollution and COVID-19 mortality in the United States. medRxiv. 2020 doi: 10.1101/2020.04.05.20054502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Jing W., Liu J. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z., Shi L., Wang Y. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Yan C., Fu Q. Possible environmental effects on the spread of COVID-19 in China. Sci. Total Environ. 2020;731 doi: 10.1016/j.scitotenv.2020.139211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Wang W. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci. Total Environ. 2020;741 doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yongjian Z., Jingu X., Fengming H., Liqing C. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M.-H., Tsunoda H., Tsunoda M. crc press; 2011. Environmental Toxicology: Biological and Health Effects of Pollutants. [Google Scholar]
- Zambrano-Monserrate M.A., Ruano M.A., Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Xue T., Jin X. Effects of meteorological conditions and air pollution on COVID-19 transmission: evidence from 219 Chinese cities. Sci. Total Environ. 2020;741 doi: 10.1016/j.scitotenv.2020.140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zohdy S., Schwartz T.S., Oaks J.R. The coevolution effect as a driver of spillover. Trends Parasitol. 2019;35(6):399–408. doi: 10.1016/j.pt.2019.03.010. [DOI] [PubMed] [Google Scholar]
- Zollinger S.A., Dorado-Correa A., Goymann W. Traffic noise exposure depresses plasma corticosterone and delays offspring growth in breeding zebra finches. Conservation physiology. 2019;7(1) doi: 10.1093/conphys/coz056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between surface levels of PM2. 5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020;738 doi: 10.1016/j.scitotenv.2020.139825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurita J.L., Jos Á., del Peso A., Salguero M., López-Artíguez M., Repetto G. Ecotoxicological evaluation of the antimalarial drug chloroquine. Aquat. Toxicol. 2005;75(2):97–107. doi: 10.1016/j.aquatox.2005.07.009. [DOI] [PubMed] [Google Scholar]