Abstract
Background
Cardiac injury is now a common complication of coronavirus disease (COVID-19), but it remains unclear whether cardiac injury-related biomarkers can be independent predictors of mortality and severe disease development or intensive care unit (ICU) admission.
Methods
Two investigators searched the PubMed, EMBASE, Cochrane Library, MEDLINE, Chinese National Knowledge Infrastructure (CNKI), Wanfang, MedRxiv, and ChinaXiv databases for articles published through March 30, 2020. Retrospective studies assessing the relationship between the prognosis of COVID-19 patients and levels of troponin I (TnI) and other cardiac injury biomarkers (creatine kinase [CK], CK myocardial band [CK-MB], lactate dehydrogenase [LDH], and interleukin-6 [IL-6]) were included. The data were extracted independently by two investigators.
Results
The analysis included 23 studies with 4631 total individuals. The proportions of severe disease, ICU admission, or death among patients with non-elevated TnI (or troponin T [TnT]), and those with elevated TnI (or TnT) were 12.0% and 64.5%, 11.8% and 56.0%, and 8.2% and. 59.3%, respectively. Patients with elevated TnI levels had significantly higher risks of severe disease, ICU admission, and death (RR 5.57, 95% CI 3.04 to 10.22, P < 0.001; RR 6.20, 95% CI 2.52 to 15.29, P < 0.001; RR 5.64, 95% CI 2.69 to 11.83, P < 0.001). Patients with an elevated CK level were at significantly increased risk of severe disease or ICU admission (RR 1.98, 95% CI 1.50 to 2.61, P < 0.001). Patients with elevated CK-MB levels were at a higher risk of developing severe disease or requiring ICU admission (RR 3.24, 95% CI 1.66 to 6.34, P = 0.001). Patients with newly occurring arrhythmias were at higher risk of developing severe disease or requiring ICU admission (RR 13.09, 95% CI 7.00 to 24.47, P < 0.001). An elevated IL-6 level was associated with a higher risk of developing severe disease, requiring ICU admission, or death.
Conclusions
COVID-19 patients with elevated TnI levels are at significantly higher risk of severe disease, ICU admission, and death. Elevated CK, CK-MB, LDH, and IL-6 levels and emerging arrhythmia are associated with the development of severe disease and need for ICU admission, and the mortality is significantly higher in patients with elevated LDH and IL-6 levels.
Graphical abstract
Keywords: Cardiac injury, Biomarkers, COVID-19, Meta-analysis, Mortality
Background
Coronavirus disease (COVID-19) has spread worldwide, becoming a public health and medical care challenge in many countries. As of April 25, 2020, COVID-19 had spread to 213 countries, areas or territories, with 2,719,897 confirmed cases and 187,705 confirmed deaths worldwide [1]. COVID-19, the clinical manifestation of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection, is characterized by respiratory tract symptoms. Severe cases can involve acute respiratory distress syndrome (ARDS) and shock [2]. COVID-19 is considered mainly a respiratory tract disease, but cardiovascular complications can also occur, eventually leading to sudden deterioration [3, 4]. A large-scale study including 44,672 patients reported that cardiovascular disease was the risk factors for fatality of COVID-19 patients [5]. Intensive care unit (ICU) occupancy is very fluid, and COVID-19 patients still require better evidence-based cardiovascular treatment [6]. Inciardi et al. reported the case of a patient who recovered from the influenza-like syndrome but then developed symptoms of heart failure [3]. A recent study recommended that cardiac biomarkers should be evaluated in all hospitalized patients with confirmed COVID-19 [7]. However, there has been less concern about cardiac complications in other published studies. Data such as those from transthoracic echocardiography, cardiac magnetic resonance imaging (MRI), coronary angiography, and other examinations of cardiovascular diseases, as well as the biomarkers of cardiac injury have been less often described or are even missing.
Recent case reports have suggested that acute cardiac injury can cause cardiac dysfunction, leading to cardiogenic shock and the proclivity for malignant arrhythmia [8]. Another study reported that COVID-19 was associated with myocarditis and arrhythmia [9]. Studies have shown that cardiac injury is related to higher in-hospital mortality rate [4] and is commonly observed in severe COVID-19 cases [9]. Therefore, paying attention to the occurrence of cardiac complications in patients with COVID-19 and performing risk stratification may greatly reduce patient mortality rates, especially of those with severe disease or requiring ICU admission. To our knowledge, this is the first study to comprehensively evaluate the impact of cardiac injury and its related biomarkers on mortality and other prognosis in patients infected with SARS-CoV-2.
Methods
Data sources and study selection
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement [10]. Two investigators (X.L. and Y.X.) independently conducted a comprehensive search of the relevant literature published until March 30, 2020, in the PubMed, EMBASE, Cochrane Library, MEDLINE, Chinese National Knowledge Infrastructure (CNKI), Wanfang, MedRxiv, and ChinaXiv databases. Combinations of the relevant medical subject heading (MeSH) terms, key words, and word variants of “novel coronavirus,” “coronavirus disease 2019,” “COVID-19,” “2019-nCoV,” “SARS-2-CoV,” “clinical or characteristic,” and “relative risk or RR” were utilized to identify all potentially relevant studies. After the elimination of duplicates, the titles and abstracts of all retrieved studies were assessed by two independent reviewers (Y.L. and N.A.) to eliminate irrelevant articles. Any disagreements were settled by consensus or by a third reviewer. Language restrictions were not applied during filtering, to maximize search sensitivity.
The inclusion criteria were as follows: (1) diagnosis of COVID-19 according to the World Health Organization interim guidance [11] and (2) reported prognosis (severe disease, ICU admission, or death) with or without cardiac injury, reported cardiac injury biomarkers (for example, troponin I [TnI], troponin T [TnT], creatine kinase [CK], CK myocardial band [CK-MB], and lactate dehydrogenase [LDH]), or arrhythmia. The exclusion criteria were as follows: (1) repeated articles, letters, editorials, and expert opinions and (2) studies with overlapping or unusable data. The primary outcome was the incidence of death, severe disease, or ICU admission in COVID-19 patients with elevated TnI levels versus non-elevated TnI levels. The secondary outcomes were as follows: (1) incidences of elevated TnI, CK, CK-MB, LDH, or interleukin-6 (IL-6) of the non-severe disease/non-ICU versus severe disease/ICU groups; (2) incidences of elevated TnI, CK, CK-MB, LDH, or IL-6 of the survivors versus non-survivors groups; (3) TnI, CK, CK-MB, LDH, or IL-6 levels of the non-severe disease/non-ICU versus severe disease/ICU groups; (4) TnI, CK, CK-MB, LDH, or IL-6 levels of the survivors versus non-survivors groups; (5) incidence of arrhythmia (defined as newly occurring of any type) of the non-severe disease/non-ICU versus severe disease/ICU groups.
Data extraction
Two investigators (X.L. and X.P.) independently extracted the relevant data from the eligible studies using predesigned forms. Disagreements were resolved by consensus. If the mean and standard deviation (SD) of the laboratory findings were not directly given, we used the estimation formula based on the median, range, and sample size [12]. Definitions used for severity assessment, ICU admission, and cardiac injury were also extracted.
Quality assessment and publication bias
Two researchers (X.P. and N.A.) independently assessed the quality of the included studies, using the Newcastle-Ottawa Quality Assessment Scale [13]. Studies were defined as high quality if a score of 7 or higher was attained [13]. Potential publication bias was evaluated using the visual inspection of funnel plots and formal testing with the Egger’s testing [14].
Statistical analysis
Effect estimates are presented as relative risk (RR) or standard mean differences (SMD) with 95% confidence interval (CI). The I2 statistic was used to quantify the heterogeneity across studies. I2 > 50% suggested significant statistical heterogeneity [15]. In this case, a random-effects model was used considering the intra- and interstudy variation. Otherwise, the pooled effect was calculated using a fixed-effects model. All analyses were performed using Stata 16.0 (StataCorp, College Station, TX, USA). Values of P < 0.05 were considered statistically significant.
Results
Study selection
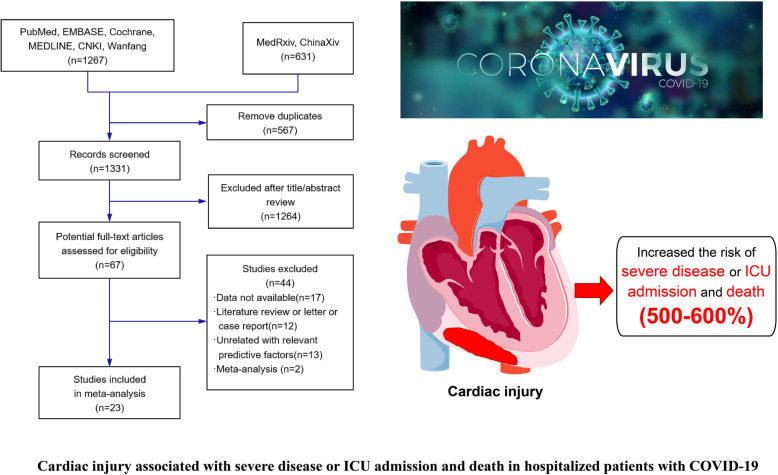
We identified 1898 studies using the predefined search terms. After the removal of duplicates and filtering of titles and abstracts to exclude irrelevant articles, 67 records remained. The full text of the 67 records was reviewed; of them, 44 records were excluded for the following reasons: data not available (n = 17), literature review or letter or case report (n = 12), unrelated to relevant predictive factors (n = 13), and meta-analysis (n = 2). Finally, 23 studies were included in this meta-analysis, of which one was not written in English. The flow diagram of this study selection is shown in Fig. 1.
Fig. 1.
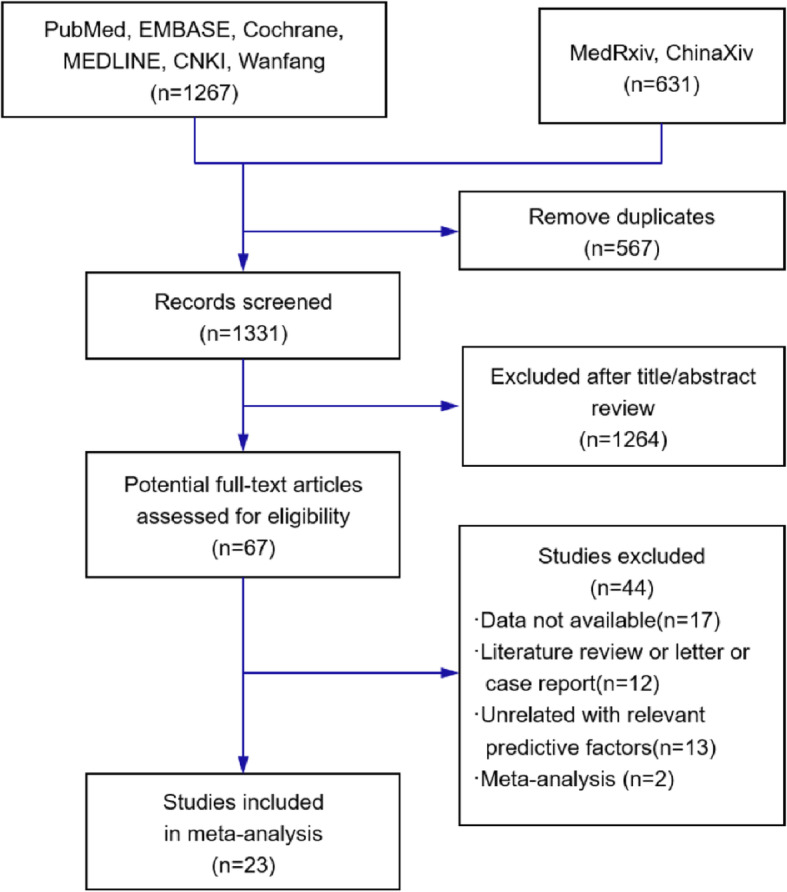
Flow diagram showing study search and selection. CNKI=Chinese National Knowledge Infrastructure
Study characteristics
The primary characteristics of the 23 included studies are listed in Table 1, with 4631 individuals incorporated. The sample size of 16 studies was greater than 100. The definition of cardiac injury was extracted (Table 2). The clinical characteristics of all included patients with COVID-19 are shown in Additional file 1: Table S1. Overall, 16 studies reported cardiac injury biomarkers, and 4 reported arrhythmias. All the results calculated using Stata are shown in Table 3.
Table 1.
Characteristics of the studies included in the meta-analysis and systematic review
| Study | Study period and location | Study design | Population, N | Male, N (%) | Median/mean age, year | Non-severe disease/severe disease, N | Non-ICU/ICU, N | Survivors/Non-survivors, N | Definition of severe disease | Study population | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang DW et al. [16] | Jan 1 to Jan 28, 2020, Wuhan, China | SC, retrospective case series | 138 | 75 (54.3) | 56 (IQR: 42–68) | NA | 102/36 | NA | Developed ARDS | Consecutive hospitalized patients with confirmed NCIP | 9 |
| Wu CM et al. (a) [17] | Dec 25, 2019, to Jan 26, 2020, Wuhan, China | SC, retrospective cohort study | 201* | 128 (63.7) | 51 (IQR: 43–60) | 117/84 | NA | 40/44 | Developed ARDS | Patients with confirmed COVID-19 pneumonia | 9 |
| Yang XB et al. [18] | Dec 24, 2019, to Jan 26, 2020, Wuhan, China | SC, retrospective, observational study | 52 | 35 (67.3) | 59.7 (SD: 13.3) | NA | NA | 20/32 | NA | Critically ill patients with SARS-CoV-2 pneumonia | 8 |
| Huang CL et al. [2] | Dec 16, 2019, to Jan 2, 2020, Wuhan, China | NA, retrospective | 41 | 30 (73.2) | 49 (IQR: 41–58) | NA | 28/13 | 35/6 | Required high-flow nasal cannula or higher-level oxygen support measures to correct hypoxemia | Patients identified as having laboratory-confirmed 2019-nCoV infection and admitted hospital | 8 |
| Chen D et al. [19] | Jan 11 to Feb 15, 2020, Wenzhou, China, | MC, retrospective study | 175 | 83 (47.4) | 46 (IQR: 34–54) | 40/135 | NA | NA | Showed pneumonia and any of acute respiratory distress syndrome | Patients with COVID-19 | 8 |
| Fu L et al. [20] | Jan 1 to Jan 30,2020, Wuhan, China | SC, retrospective cohort study | 200 | 99 (49.5) | NA | NA | NA | 166/34 | NA | Patients with confirmed COVID-19 | 8 |
| Guan WJ et al. [21] | Jan 1 to Jan 29,2020, China | MC, retrospective study | 1099 | 640 (58.2) | 47 (IQR: 35–58) | 926/173 | NA | 1084/15 | NA | Patients with laboratory-confirmed 2019-nCoV ARD | 8 |
| Hui H et al. [22] | Jan 21 to Feb 03, 2020, Beijing, China | SC, retrospective study | 41 | 19 (46.3) | 47 (IQR: 35.5–64) | 34/7 | NA | NA | NA | Patients with confirmed COVID-19 | 7 |
| Liu YL et al. [23] | Jan 2 to Feb 12, 2020, Wuhan, China | SC, retrospective study | 109 | 59 (54.1) | 55 (IQR: 43–66) | 56/53 | NA | 78/31 | Developed ARDS | Patients with confirmed COVID-19 | 8 |
| Liu L et al. [24] | Jan 20 to Feb 3, 2020, Chongqing, China | SC, retrospective case series | 51 | 32 (62.7) | 45 (IQR: 34–51) | 44/7 | NA | NA | NA | Patients with confirmed COVID-19 | 8 |
| Qi D et al. [25] | Jan 19 to Feb 16, 2020, Chongqing, China | MC, retrospective, descriptive study | 267 | 149 (55.8) | 48 (IQR: 35–65) | 217/50 | 214/53 | 263/4 | According to the American Thoracic Society guideline | Patients with COVID-19 confirmed by real-time RT-PCR | 7 |
| Wang YF et al. [26] | Jan 1 to Feb 10, 2020, Wuhan, China | SC, retrospective | 110 | 48 (43.6) | NA | 72/38 | NA | NA | Fever or suspected respiratory infection, plus one of a respiratory rate > 30 breaths/min, severe respiratory distress, or SpO2 < 90% on room air | Patients with confirmed COVID-19 pneumonia | 8 |
| Wu CM et al. (b) [27] | Dec 25, 2019 to Jan 27, 2020, Wuhan, China | SC, retrospective cohort study | 188 | 119 (63.3) | 51.9 (SD: 14.26) | NA | 138/50 | 145/4 | NA | Patients with confirmed COVID-19 pneumonia | 8 |
| Xu HY et al. [28] | Jan 02 to Feb 14, 2020, NA | NA, retrospective | 53 | 28 (52.8) | NA | 34/19 | 45/8 | 53/3 | More likely to have underlying comorbidities, and AMI | Consecutive laboratory-confirmed and hospitalized patients with confirmed NCIP | 7 |
| Xu YH et al. [29] | Jan 14 to Feb 28, 2020, Guangdong, China | MC, retrospective, observational study | 45 | 29 (64.4) | 56.7 (SD: 15.4) | 25/20 | 0/45 | 44/1 | Defined as those required oxygen therapy, symptoms of respiratory distress or required mechanical ventilation |
critically ill patients with SARS-CoV-2 pneumonia RT-PCR confirmed positive patients |
8 |
| Liu YB et al. [30] | Jan 10 to Feb 24, 2020, Guangzhou, China | SC, retrospective | 291 | 133 (45.7) | 48.1 (IQR: 34–62) | 262/29 | 265/26 | 290/1 | NA | Laboratory-confirmed patients with NCIP | 8 |
| Peng YD et al. [31] | Jan 20 to Feb, 15, 2020, Wuhan, China | SC, retrospective, cohort study | 112 | 53 (47.0) | 62 (IQR: 55–67) | 96/16 | NA | 84/28 | Required mechanical ventilation; shock; combined with other organ failure | COVID-19 patients with CVD | 7 |
| Zhang GQ et al. [32] | Jan 2 to Feb, 10, 2020, Wuhan, China | SC, retrospective case series study | 221 | 108 (48.9) | 55 (IQR: 39–66.5) | 166/55 | NA | 209/12 | Fever plus one of these conditions, including respiratory rate ≥ 30 breaths/min, severe respiratory distress, SpO2 ≤ 93% on room air, occurrence of respiratory failure requiring mechanical ventilation, shock and other organ failure | Patients who were confirmed diagnosed as COVID-19 according to WHO interim guidance | 8 |
| Liu T et al. [33] | Jan 21, to Feb 16, 2020, Wuhan, China | NA, retrospective | 80 | 34 (42.5) | 53 (range: 26–86) | 11/69 | NA | 80/0 | Defined when any of the following criteria was met: dyspnea, respiration rate ≥ 30 times/min; oxygen saturation by pulse oximeter ≤93% in resting state; partial pressure of arterial oxygen to fraction of inspired oxygen ratio ≤ 300 mmHg | SARS-CoV-2 nucleic acid or RT-PCR confirmed positive patients | 8 |
| Shi SB et al. [4] | Jan 20, to Feb 10, 2020, Wuhan, China | SC, retrospective cohort study | 416 | 205 (49.3) | 64 (range: 21–95) | 319/97 | NA | 359/57 | NA | Consecutive inpatients with laboratory-confirmed COVID-19 | 9 |
| Wu J et al. [34] | Jan 20 to Feb 20,2020, Jiangsu and Anhui Province, China | MC, retrospective case series | 280 | 151 (53.9) | 43.1 (SD:19.02) | 197/83 | NA | NA | NA | Patients infected with SARS-CoV-2 | 8 |
| Chen T et al. [35] | Jan 13, to Feb 28, 2020, Wuhan, China | SC, retrospective | 274 | 171 (62) | 62 (IQR: 44–70) | NA | NA | 161/113 | NA | Patients with confirmed COVID-19 pneumonia | 8 |
| Guo T et al. [36] | Jan 23, to Feb 23, 2020, Wuhan, China | SC, retrospective | 187 | 91 (48.7) | 58.5 (SD:14.66) | NA | NA | 144/43 | NA | Patients with confirmed COVID-19 pneumonia | 9 |
AMI acute myocardial injury, ARDS acute respiratory distress syndrome, COVID-19 coronavirus disease 2019, CVD cardiovascular disease, 2019-nCoV novel coronavirus, IQR interquartile range, MC multicenter study, N number, NA not available, NCIP novel coronavirus-infected pneumonia, RT-PCR reverse transcriptase polymerase chain reaction, SARS-CoV-2 severe acute respiratory syndrome coronavirus-2, SC single-center study, SD standard deviation
Table 2.
Clinical characteristics of COVID-19 patients with or without elevated TnI (TnT)
| Source | Severe disease/ARDS | ICU | Death | NT-proBNP, Median (IQR), pg/mL | Definition of cardiac injury | ||||
|---|---|---|---|---|---|---|---|---|---|
| Elevated TnI/TnT, N/total | Non-elevated TnI/TnT, N/total | Elevated TnI/TnT, N/total | Non-elevated TnI/TnT, N/total | Elevated TnI/TnT, N/total | Non-elevated TnI/TnT, N/total | Elevated TnI/TnT | Non-elevated TnI/TnT | ||
| Liu et al. [30] | 11/15 | 18/276 | 11/15 | 15/276 | 1/15 | 0/276 | NA | NA | TnI > 0.03 μg/L |
| Xu et al. [28] | 6/6 | 13/47 | 6/6 | 2/47 | 3/6 | 0/47 | NA | NA | TnT-HSST > 28 pg/ml |
| Wu et al. (b) [27] | NA | NA | 27/62 | 23/126 | 31/62 | 12/126 | NA | NA | Hs-TnI ≥ 6.126 pg/mL |
| Hui et al. [22] | 4/4 | 1/16 | NA | NA | NA | NA | NA | NA | NA |
| Wang et al. [16] | NA | NA | 8/10 | 28/128 | NA | NA | NA | NA | NA |
| Yang et al. [18] | NA | NA | NA | NA | 9/12 | 23/40 | NA | NA | Hs-TNI > 28 pg/mL |
| Shi et al. [4] | 48/82 | 49/334 | NA | NA | 42/82 | 15/334 | 1689 (698–3327) | 139 (51–335) | Hs-TnI > 0.04 ng/mL |
| Chen et al. [35] | NA | NA | NA | NA | 68/83 | 26/120 | NA | NA | Hs-TnI > 15.6 pg/mL |
| Guo et al. [36] | NA | NA | NA | NA | 31/52 | 12/135 | 817.4 (336.0–1944.0) | 141.4 (39.3–303.6) | Elevated TnT levels |
ARDS acute respiratory distress syndrome, Hs-TnI high-sensitivity troponin I, ICU intensive care unit, IQR interquartile range, N number, NA not available, NT-proBNP N-terminal pro-B-type natriuretic peptide, TnI troponin I, TnT troponin T, TnT-HSST troponin T-hypersensitivity
Table 3.
All the results calculated using Stata
| Characteristic | Non-elevated TnI/TnT vs. elevated TnI/TnT | Non-severe disease/non-ICU vs. severe disease/ICU | Survivors vs. non-survivors | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I2(%) | RR | 95%CI | Z | P | I2(%) | RR/SMD | 95%CI | Z | P | I2(%) | RR/SMD | 95%CI | Z | P | |
| Severe, n | 78.6 | 5.57 | (3.04, 10.22) | 5.55 | 0.00 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| ICU, n | 89.3 | 6.20 | (2.52, 15.29) | 3.96 | 0.00 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Death, n | 89.1 | 5.64 | (2.69, 11.83) | 4.57 | 0.00 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| NT-proBNP (pg/ml) | 86.6 | 1.63 | (1.02, 2.23) | 5.27 | 0.00 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Elevated TnI/TnT, n | NA | NA | NA | NA | NA | 83.7 | 15.10 | (4.10, 55.61) | 4.08 | 0.00 | 22.5 | 4.69 | (3.39, 6.48) | 9.37 | 0.00 |
| TnI (pg/ml) | NA | NA | NA | NA | NA | 84.6 | 0.74 | (0.19, 1.30) | 2.62 | 0.009 | NA | NA | NA | NA | NA |
| Elevated CK, n | NA | NA | NA | NA | NA | 0.0 | 1.98 | (1.50, 2.61) | 4.78 | 0.00 | NA | NA | NA | NA | NA |
| CK (U/L) | NA | NA | NA | NA | NA | 69.0 | 0.39 | (0.11, 0.67) | 2.76 | 0.006 | NA | NA | NA | NA | NA |
| Elevated CK-MB, n | NA | NA | NA | NA | NA | 79.8 | 3.24 | (1.66, 6.34) | 3.44 | 0.001 | NA | NA | NA | NA | NA |
| CK-MB (U/L) | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Elevated LDH, n | NA | NA | NA | NA | NA | 79.7 | 2.20 | (1.55, 3.12) | 4.40 | 0.00 | NA | NA | NA | NA | NA |
| LDH (U/L) | NA | NA | NA | NA | NA | 92.7 | 1.15 | (0.61, 1.70) | 4.16 | 0.00 | 98.6 | 2.86 | (0.67, 5.06) | 2.56 | 0.01 |
| BNP (pg/ml) | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Arrhythmia, n | NA | NA | NA | NA | NA | 42.0 | 13.09 | (7.00, 24.47) | 8.06 | 0.00 | NA | NA | NA | NA | NA |
| IL-6 (pg/ml) | NA | NA | NA | NA | NA | 0.0 | 0.54 | (0.27, 0.81) | 3.94 | 0.00 | 13.7 | 1.28 | (1.00, 1.57) | 8.85 | 0.00 |
BNP B-type natriuretic peptide, CK creatinine kinase, CK-MB creatinine kinase–myocardial band, ICU intensive care unit, LDH lactate dehydrogenase, IL-6 interleukin-6, n number, NA not available, NT-proBNP N-terminal pro-B-type natriuretic peptide, RR risk ratios, SMD standard mean
Non-elevated TnI vs. elevated TnI groups
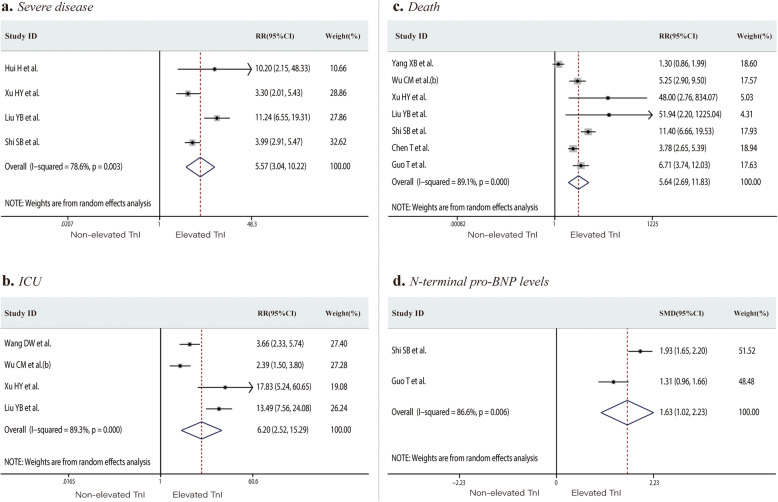
First, we restricted our analysis to studies that assessed the prognosis of COVID-19 patients with or without elevated TnI (or TnT). Nine studies reported the outcome events (including severe disease, ICU admission, and death) of patients with non-elevated or elevated TnI (TnT). TnI, which defines cardiac injury, was measured in a total of 1548 COVID-19 patients. The proportions of severe cases, ICU admissions, or death in the non-elevated TnI versus elevated TnI groups were 12.0% versus 64.5%, 11.8% versus 56.0%, and 8.2% versus 59.3%, respectively. Patients with elevated TnI levels had a significantly higher risk of severe disease, ICU admission, and death than those in the non-elevated TnI group (RR 5.57, 95% CI 3.04 to 10.22, P < 0.001; I2 = 78.6%, Fig. 2a; RR 6.20, 95% CI 2.52 to 15.29, P < 0.001; I2 = 89.3%, Fig. 2b; RR 5.64, 95% CI 2.69 to 11.83, P < 0.001; I2 = 89.1%, Fig. 2c, respectively). The mean N-terminal pro-BNP (NT-proBNP) level was significantly higher in the elevated TnI group than in the non-elevated TnI group (SMD 1.63, 95% CI 1.02 to 2.23, P < 0.001; I2 = 86.6%, Fig. 2d).
Fig. 2.
Forest plots comparing of risk of severe disease (a), ICU admission (b), and death (c), and the N-terminal pro-BNP levels (d) in patients with or without elevated troponin I (or troponin T). ICU, intensive care unit; BNP, B-type natriuretic peptide; RR, risk ratios; SMD, standard mean
Non-severe disease/non-ICU vs. severe disease/ICU groups and survivors vs. non-survivors groups
Cardiac injury biomarkers
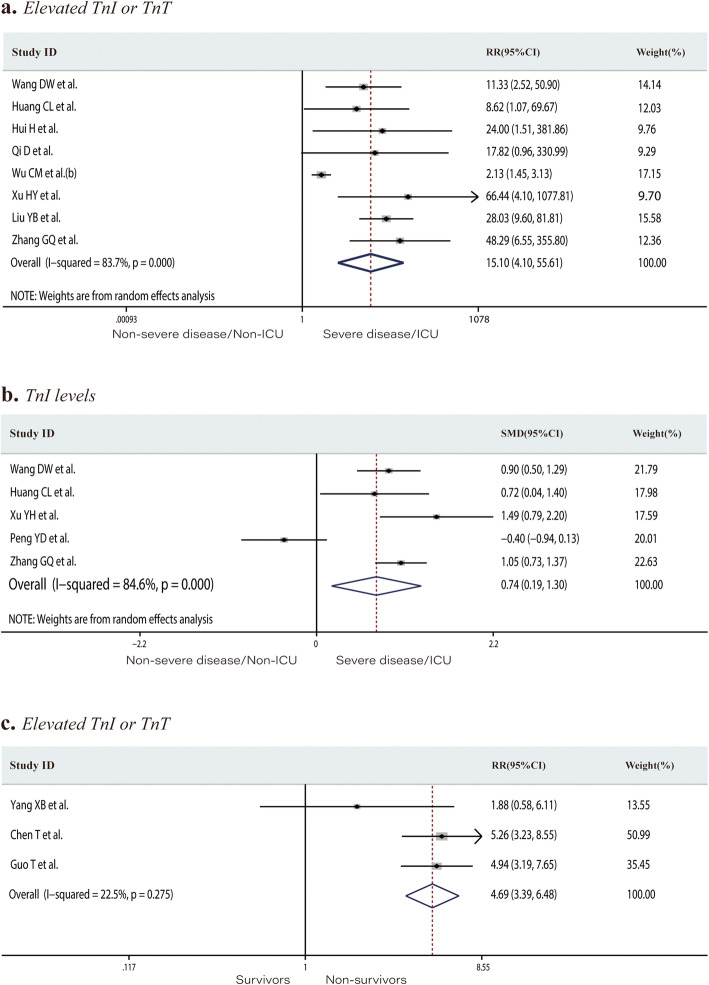
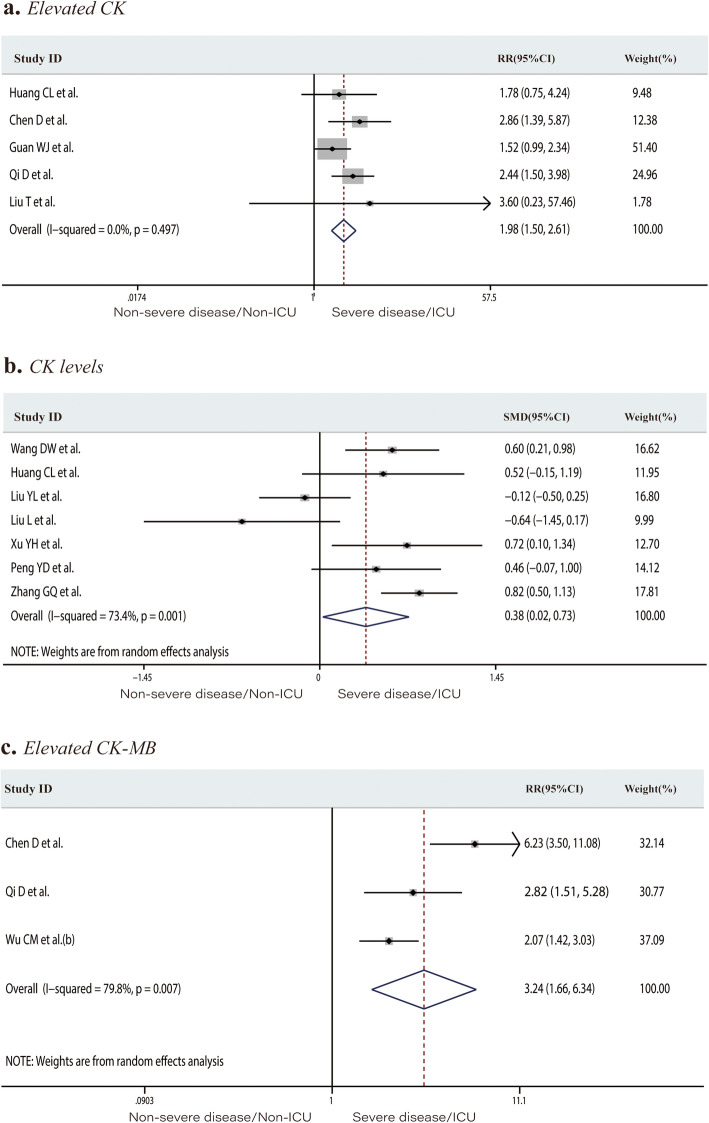
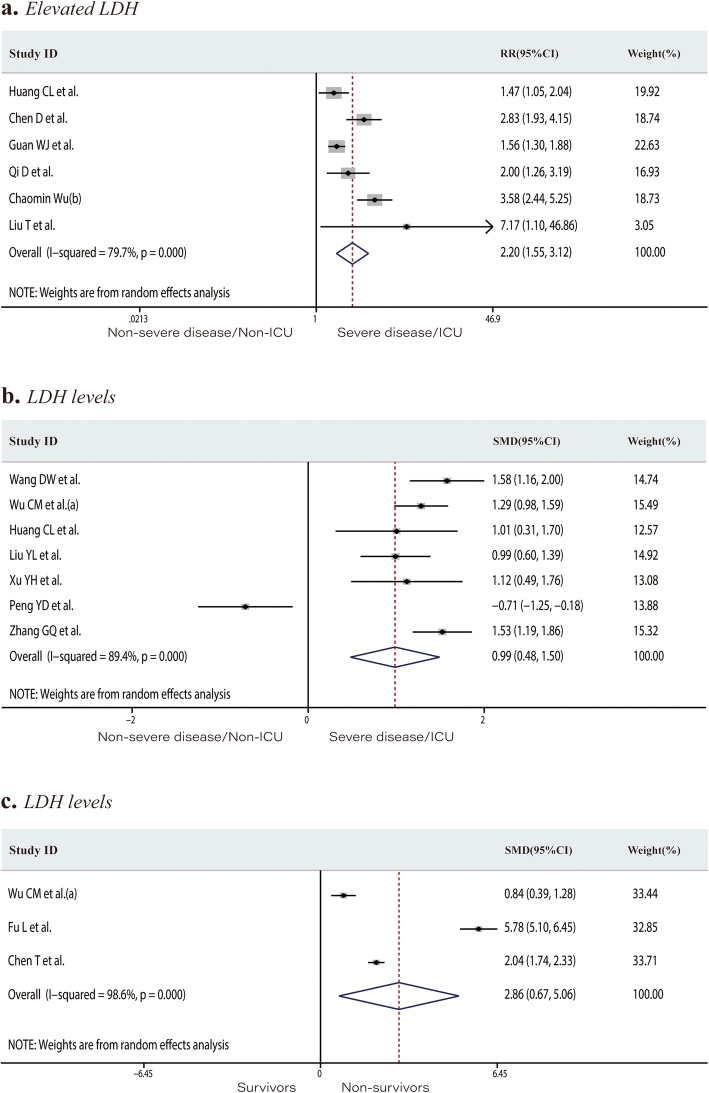
Eight studies including 1028 patients in the non-severe disease/non-ICU group or severe disease/ICU group reported the number of patients with elevated TnI or TnT levels (total rate, 11.9%). Elevated TnI or TnT levels occurred at a rate of 2.3% in the non-severe disease/non-ICU group and 36.9% in the severe disease/ICU group. Patients in the severe/ICU group had an increased risk of developing elevated TnI or TnT levels (RR 15.10, 95% CI 4.10 to 55.61, P < 0.001; I2 = 83.7%, Fig. 3a). The mean TnI level was significantly higher in the severe disease/ICU admission group (SMD 0.74, 95% CI 0.19 to 1.30, P = 0.009; I2 = 84.6%, Fig. 3b). The proportion of patients with elevated TnI or TnT levels in the survivors and non-survivor groups was 14.3% and 63.9%, respectively. Significantly more non-survivors than survivors had elevated TnI or TnT levels (RR 4.69, 95% CI 3.39 to 6.48, P < 0.001; I2 = 22.5%, Fig. 3c). Twelve studies including 2174 individuals reported the CK levels or the number of patients with above-normal CK levels. The incidence of elevated CK in the severe disease/ICU group was significantly higher than that in the non-severe disease/non-ICU group (12.9% and 23.2%, respectively; RR 1.98, 95% CI 1.50 to 2.61, P < 0.001; I2 = 0.0%, Fig. 4a). The mean CK level was significantly higher in severe disease/ICU group than in the non-severe disease/non-ICU group (SMD 0.39, 95% CI 0.11 to 0.67, P = 0.006; I2 = 69.0%, Fig. 4b). The proportion of patients with an elevated CK-MB level in the non-severe disease/non-ICU and severe disease/ICU groups was 14.1% and 45.7%, respectively. Patients in the severe disease/ICU admission group were at higher risk of developing an elevated CK-MB level than those in the non-severe disease/non-ICU group (RR 3.24, 95% CI 1.66 to 6.34, P = 0.001; I2 = 79.8%, Fig. 4c). Of the 2532 patients from 15 studies, 29.7% of those in the non-severe disease/non-ICU group versus 60.1% of the severe disease/ICU group had elevated LDH levels. COVID-19 patients with elevated LDH levels were at significantly increased risk of developing severe disease or requiring ICU admission (RR 2.20, 95% CI 1.55 to 3.12, P < 0.001; I2 = 79.7%, Fig. 5a). LDH levels were significantly higher in the severe disease/ICU admission group than in the non-severe disease/non-ICU group (SMD 1.15, 95% CI 0.61 to 1.70, P < 0.001; I2 = 92.7%, Fig. 5b) and in non-survivors than in survivors (SMD 2.86, 95% CI 0.67 to 5.06, P = 0.01; I2 = 98.6%, Fig. 5c).
Fig. 3.
Forest plots comparing of the proportion of patients with elevated troponin I or troponin T levels in the severe disease/ICU group and in the non-severe disease/non-ICU group (a), the troponin I levels in the severe disease/ICU group and in the non-severe disease/non-ICU group (b), and the proportion of patients with elevated troponin I or troponin T levels in the survivors and non-survivors groups (c). ICU, intensive care unit; RR, risk ratios; SMD, standard mean
Fig. 4.
Forest plots comparing of the proportion of patients with elevated creatinine kinase levels in the severe disease/ICU group and in the non-severe disease/non-ICU group (a), the creatinine kinase levels in the severe disease/ICU group and in the non-severe disease/non-ICU group (b), and the proportion of patients with elevated creatinine kinase–myocardial band levels in the severe disease/ICU group and in the non-severe disease/non-ICU group (c). ICU, intensive care unit; RR, risk ratios; SMD, standard mean
Fig. 5.
Forest plots comparing of the proportion of patients with elevated lactate dehydrogenase levels in the severe disease/ICU group and in the non-severe disease/non-ICU group (a), the lactate dehydrogenase levels in the severe disease/ICU group and in the non-severe disease/non-ICU group (b), and the lactate dehydrogenase levels in the survivors and non-survivor groups (c). ICU, intensive care unit; RR, risk ratios; SMD, standard mean
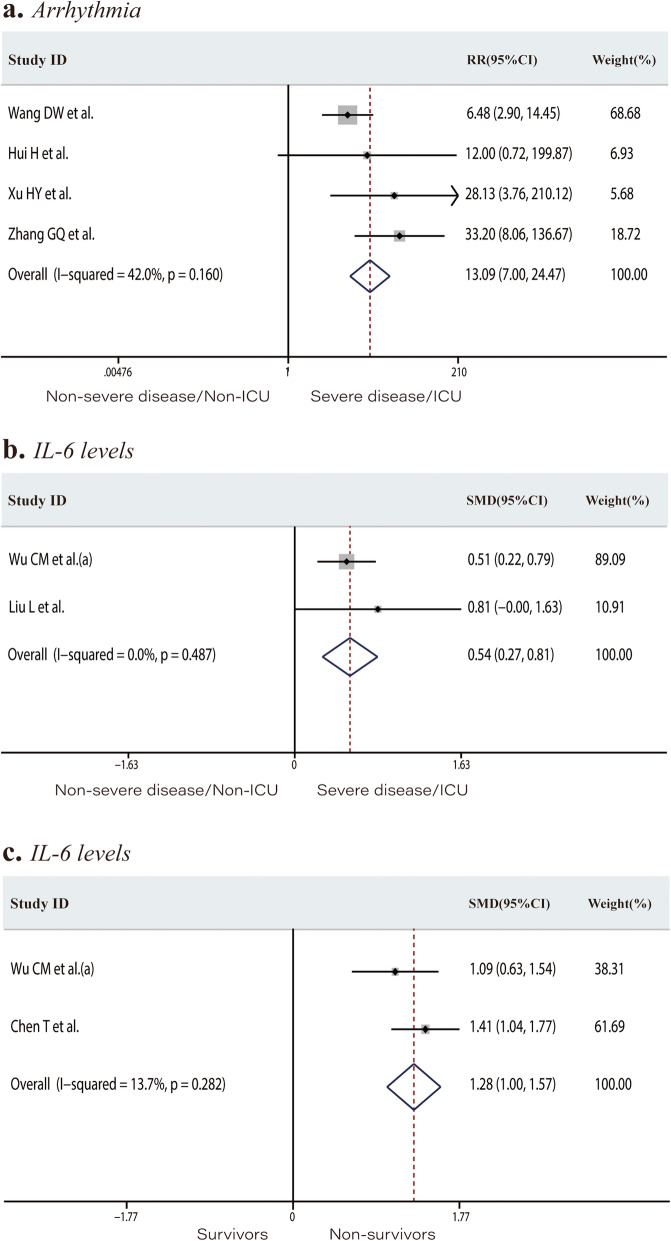
Arrhythmia and IL-6
The incidence of arrhythmia was 3.1% in the non-severe disease/non-ICU group versus 43.8% in the severe disease/ICU group. Patients with newly occurring arrhythmias were at a higher risk of developing severe disease or requiring ICU admission (RR 13.09, 95% CI 7.00 to 24.47, P < 0.001; I2 = 42.0%, Fig. 6a). IL-6 levels were significantly higher in the severe disease/ICU group than in the non-severe disease/non-ICU group, as well as in non-survivors than in survivors (SMD 0.54, 95% CI 0.27 to 0.81, P < 0.001; I2 = 0.0%, Fig. 6b; SMD 1.28, 95% CI 1.00 to 1.57, P < 0.001; I2 = 13.7%, Fig. 6c, respectively).
Fig. 6.
Forest plots comparing of the risk of developing to severe disease or requiring ICU admission among patients with or without newly occurring arrhythmias (a), the interleukin-6 levels in the severe disease/ICU group (b), and in the non-severe disease/non-ICU group and the interleukin-6 levels in the survivors and non-survivors groups (c). ICU, intensive care unit; RR, risk ratios; SMD, standard mean
Discussion
This systematic review and meta-analysis of 23 high-quality retrospective studies systematically evaluated the risk of severe disease, ICU admission, or death associated with COVID-19-related cardiac injury performance. Our findings are as follows: (1) COVID-19 patients with elevated TnI levels are at significantly higher risk of developing severe disease, requiring ICU admission, or death; (2) elevated CK, CK-MB, LDH, and IL-6 levels and emerging arrhythmia are associated with the development of severe disease or requirement for ICU admission; and (3) mortality rates are significantly higher among patients with elevated LDH and IL-6 levels.
Cardiac injury
Cardiac injury was defined as a serum cardiac biomarker level (e.g., troponin I) above the 99th percentile upper reference limit or new abnormalities seen on electrocardiography (ECG) and echocardiography [2]. CK, CK-MB, and LDH are also indicators associated with cardiac injury [37, 38]. An elevated cardiac TnI level has high specificity for cardiac injury and is a preferred biomarker of cardiac injury. Overall, in 8 studies including 1028 patients, the rates of elevated TnI or TnT in the non-severe disease/non-ICU admission group and severe disease/ICU admission group were 2.3% and 36.9%, respectively; in the total population, elevated TnI or TnT occurred at a rate of 11.9%. Our analysis suggests that COVID-19 patients with elevated TnI levels are at higher risk of developing severe disease, requiring ICU admission, and death. Two studies from Wuhan (one with 416 cases, another with 187 cases) reported higher mortality among patients with cardiac injury than among those without (51.2% vs. 4.5%; P < 0.001; 59.6% vs. 8.9%, P < 0.001, respectively) [4, 36]. Patients with cardiac injury had higher serum concentrations of NT-proBNP than those without cardiac injury [36, 39]. Patients with cardiac injury more commonly developed ARDS, were more likely to have ventricular tachycardia (VT) or ventricular fibrillation (VF), and had higher mortality rates than those without VT or VF [36, 39].
TnI has great prognostic significance for patients with COVID-19 as well as those with other influenza virus infections. In a study of 75 inpatients with SARS, acute myocardial infarction was the cause of 2 of 5 deaths [40]. Elevated TnI levels are also common in infections caused by other influenza virus subtypes [41–45]. TnI may play an important role in predicting the acute or long-term risk of influenza virus infection. Other biomarkers closely related to cardiac injury, such as CK, CK-MB, and LDH, were also selected in the meta-analysis. Our analysis showed that those with elevated CK, CK-MB, and LDH were at a higher risk of developing severe disease or requiring ICU admission. The LDH level had a predictive value for death. Previous studies suggested that CK at ICU admission serves can be used as a biomarker of the severity of 2009 pandemic influenza A (pH1N1) infection [46].
Elevated TnI and CK-MB levels indicate cardiac injury such as viral myocarditis or myocardial infarction as well as multiple organ injury [47]. Initial reports showed that the possible pattern of myocardial injury is the early presentation of primary cardiovascular symptoms, as well as changes on echocardiography and ECG [3, 6, 48–50]. Stress cardiomyopathy, supply demand mismatch (type II myocardial infarction), and myocarditis, sometimes similar to ST-segment elevation myocardial infarction, are all possible mechanisms [3, 6, 49]. In a study describing a single case without a history of cardiovascular disease, the patient had myocardial injury, and diffuse edema was seen on cardiac MRI [3]. Twelve lead ECG showed minimal diffuse ST-segment elevation and an ST-segment depression with T-wave inversion of lead V1 and aVR. Even in the absence of respiratory tract or infection symptoms, SARS-CoV-2 infection may cause cardiac involvement. However, it is a pity that an endomyocardial biopsy was not performed; thus, there was no histological evidence [3]. Cardiac injury is an important prognostic factor for COVID-19. It is rational to presume that the virus affects the myocardium, and once patients develop severe pneumonia, cardiac injury or dysfunction is more likely to occur, leading to deterioration. In a study of critically ill patients, including 21 who had SARS-CoV-2 infection in the USA, the incidence of cardiomyopathy was high (n = 7 [33%]) [51]. In a patient without fever and respiratory symptoms, the initial ECG showed diffuse ST elevations and an admission TnI level of 7.9 ng/mL, but angiography demonstrated non-obstructive coronary artery disease. After treatment, this patient improved in the short term, but the long-term effects of myocardial injury remain to be determined [8].
The etiology of cardiac dysfunction may be multifactorial and related to infective myocarditis and/or ischemia. Pathological findings suggested a few interstitial mononuclear inflammatory infiltrates in the myocardial interstitial [52]. Viral invasion may cause direct cardiac injury, and COVID-19-induced cytokine storm may also have toxic effects on the myocardium [53]. Cytokine storm may play a role in the development of ARDS and fulminant myocarditis. In our analysis, 3 studies reported the laboratory findings of IL-6 levels in 526 patients. IL-6 levels were significantly higher in the severe disease/ICU groups than non-severe disease/non-ICU groups, as well as in non-survivors than in survivors. Cardiac involvement reportedly occurred a few days after the influenza syndrome, suggesting the mechanisms of a potential myocyte dissemination of the virus activating the immune system, eventually leading to the onset of heart failure [3]. A study reported that, compared to survivors, non-survivors had increased concentrations of C-reactive protein, decreased lymphocyte counts, and significantly reduced numbers of CD3 + CD8 + T cells, resulting in an immune response [54]. Anti-IL-6, as a drug targeting cytokine pathway and based on its mechanism of action, has potential benefits in COVID-19-related ARDS and pneumonia [55].
Arrhythmia
Our analysis also found that the patients with emerging arrhythmia are at a higher risk of developing severe disease or requiring ICU admission. In a study of 41 patients with COVID-19, atrial fibrillation occurred in 2 of 3 severe and critical patients with tachycardia, with a peak heart rate of 160 bpm [22]. Newly occurring arrhythmias are often closely related to cardiac injury. The incidence of ventricular arrhythmias (VT/VF) among 187 patients with COVID-19 was 5.9%, primarily affecting those with elevated cardiac troponin levels [36]. One study reported that 5 of 6 acute myocardial injury patients had more than two kinds of ECG abnormalities, including ST-T/Q curve abnormality, atrioventricular block, and arrhythmia [28]. Severe pneumonia increases the resistance of the pulmonary circulation, increasing the pressure of the right atrium, and leading to atrial tachyarrhythmia. Antiviral drugs such as hydroxychloroquine may also prolong the QT interval. Alternatively, the virus directly damages the myocardium and the cardiac conduction system, causing multiple ventricular premature and atrioventricular block. More attention is needed on arrhythmia among severe disease/ICU admission COVID-19 patients. However, in the studies reviewed here, ECG or echocardiography was rarely performed and the occurrence of arrhythmia was rarely reported.
Conclusion
This meta-analysis included the largest sample size and is the first to analyze the correlation of cardiac injury biomarkers and arrhythmia with mortality and other prognosis. Our systematic review and meta-analysis indicate that patients with elevated TnI (TnT) levels are at significantly higher risk of developing severe disease, requiring ICU admission, or death. Our analysis also reveals that patients with elevated CK, CK-MB, and LDH levels and emerging arrhythmia were at a higher risk of developing severe disease, requiring ICU admission. LDH levels also have predictive value for death. Therefore, we strongly recommend the close monitoring of cardiac injury-related biomarkers in COVID-19 patients, especially during the acute disease phase.
Limitations and prospects
The current clinical attention given to cardiac injury may be insufficient, and the strong infection of the virus makes cardiovascular examinations such as MRI, echocardiography, and coronary angiography difficult to perform [56]. The evaluation of cardiac injury biomarkers combined with cardiac examinations may help better assessments of the condition. There are few reports on cardiac injury in COVID-19 patients, and a large amount of evidence is still needed to make the necessary risk predictions and stratifications. The present results provide some evidence for COVID-19 treatment guidelines. In the future, it well be necessary to strengthen the monitoring of cardiac injury biomarkers, combined with echocardiography [57], ECG, MRI, and other cardiac examinations, in patients with severe SARS-CoV-2 infection. When circulation support is needed in severe COVID-19 cases, the use of an intra-aortic balloon pump or extracorporeal membrane oxygenation may be considered [8].
Supplementary information
Additional file 1: Table S1. Clinical characteristics of patients with COVID-19.
Acknowledgements
None.
Abbreviations
- 2019-nCoV
Novel coronavirus
- ARDS
Acute respiratory distress syndrome
- CI
Confidence interval
- CK
Creatinine kinase
- CK-MB
Creatinine kinase–myocardial band
- COVID-19
Coronavirus disease
- Hs-TnI
High-sensitivity troponin I
- ICU
Intensive care unit
- IL-6
Interleukin-6
- IQR
Interquartile range
- LDH
Lactate dehydrogenase
- MC
Multicenter study
- n
Number
- NA
Not available
- NCIP
Novel coronavirus-infected pneumonia
- NT-proBNP
N-terminal pro-B-type natriuretic peptide
- RT-PCR
Reverse transcriptase polymerase chain reaction
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus-2
- SC
Single-center study
- SD
Standard deviation
- TnI
Troponin I
- TnT
Troponin T
- TnT-HSST
Troponin T-hypersensitivity
Authors’ contributions
XL, HS, and YWX had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. XL, XP, YL, NA, HS, and YWX designed the study, searched the scientific literature, collected the data, and performed statistical analyses. XL, YL, NA, and YWX drafted the manuscript. XL, XP, YL, and HS participated in the design and resolved differences. HS and YWX contributed to the conception and quality assessment of the study. YFX, FY, LT, JS, YG, and HS helped to revise the manuscript and provided technical or material support. The authors have read and approved the final manuscript.
Funding
This work was supported by the National Key R&D Program of China (grants 2018YFC1704900 & 2018YFC1704901).
Availability of data and materials
All the data supporting the conclusions of this article are included within the article.
Ethics approval and consent to participate
This article is meta-analysis and does not require ethics committee approval or a consent statement.
Consent for publication
All authors have agreed to the publication of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xinye Li, Xiandu Pan, Yanda Li and Na An contributed equally to this work.
Contributor Information
Hongcai Shang, Email: shanghongcai@126.com.
Yanwei Xing, Email: xingyanwei12345@163.com.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13054-020-03183-z.
References
- 1.Coronavirus disease (COVID-19) Pandemic. Accessed 25 Apr 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 2.Huang CL, Wang YM, Li XW, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020. [DOI] [PMC free article] [PubMed]
- 4.Shi SB, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China JAMA Cardiol Published online March 25, 2020. [DOI] [PMC free article] [PubMed]
- 5.Deng G, Yin M, Chen X, Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Critical care (London, England) 2020;24(1):179. doi: 10.1186/s13054-020-02902-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cortese B. COVID-19 pandemic-some cardiovascular considerations from the trench. Am Heart J. 2020;225:1–2. doi: 10.1016/j.ahj.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loungani RS, Rehorn MR, Newby LK, Katz JN, Klem I, Mentz RJ, Jones WS, Vemulapalli S, Kelsey AM, Blazing MA, et al. A care pathway for the cardiovascular complications of COVID-19: insights from an institutional response. Am Heart J. 2020;225:3–9. doi: 10.1016/j.ahj.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fried JA, Ramasubbu K, Bhatt R, Topkara VK, Clerkin KJ, Horn E, et al. The variety of cardiovascular presentations of COVID-19. Circulation. 2020;141(23):1930-6. [DOI] [PMC free article] [PubMed]
- 9.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020. [DOI] [PubMed]
- 10.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected: interim guidance. Published January 28, 2020. Accessed April 5, 2020. https://www.who.int/publications-detail/clinical-managementof-severe-acute-respiratory-infection-when-novelcoronavirus-(ncov)-infection-is-suspected.
- 12.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 14.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–1129. doi: 10.1016/S0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- 15.Leung WK, Ho HJ, Lin JT, Wu MS, Wu CY. Prior gastroscopy and mortality in patients with gastric cancer: a matched retrospective cohort study. Gastrointest Endosc. 2018;87(1):119–127. doi: 10.1016/j.gie.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Wang DW, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China JAMA Published online February 7, 2020. [DOI] [PMC free article] [PubMed]
- 17.Wu CM, Chen XY, Cai YP, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China JAMA Intern Med Published online March 13, 2020. [DOI] [PMC free article] [PubMed]
- 18.Yang XB, Yu Y, Xu JQ, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-81. [DOI] [PMC free article] [PubMed]
- 19.Chen D, Li XK, Song QF, Hu CC, Su FF, Dai JY. Hypokalemia and clinical implications in patients with coronavirus disease 2019 (COVID-19). Published 2020. Accessed 19 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.02.27.20028530v1.
- 20.Fu L, Fei J, Xiang HX, et al. Influence factors of death risk among COVID-19 patients in Wuhan, China: a hospital-based case-cohort study. Published 2020. Accessed 18 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.13.20035329v1.
- 21.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020:382(18):1708-20. [DOI] [PMC free article] [PubMed]
- 22.Hui H, Zhang YQ, Yang X, et al. Clinical and radiographic features of cardiac injury in patients with 2019 novel coronavirus pneumonia. Published 2020. Accessed 19 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.02.24.20027052v1.
- 23.Liu YL, Sun WW, Li J, et al. Clinical features and progression of acute respiratory distress syndrome in coronavirus disease 2019. Published 2020. Accessed 19 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.02.17.20024166v3.
- 24.Liu L, Gao JY. Clinical characteristics of 51 patients discharged from hospital with COVID-19 in Chongqing, China. Published 2020. Accessed 18 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.02.20.20025536v1.
- 25.Qi D, Yan XF, Tang XM, et al. Epidemiological and clinical features of 2019-nCoV acute respiratory disease cases in Chongqing municipality, China: a retrospective, descriptive, multiple-center study. Published 2020. Accessed 21 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.01.20029397v1.
- 26.Wang YF, Zhou Y, Yang Z, Xia DP, Geng S. Clinical characteristics of patients with severe pneumonia caused by the 2019 novel coronavirus in Wuhan, China. Published 2020. Accessed 21 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.02.20029306v1.
- 27.Wu CM, Hu XL, Song JX, et al. Heart injury signs are associated with higher and earlier mortality in coronavirus disease 2019 (COVID-19). Published 2020. Accessed 23 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.02.26.20028589v1.
- 28.Xu HY, Hou KK, Xu H, et al. Acute myocardial injury of patients with coronavirus disease 2019. Published 2020. Accessed 23 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.05.20031591v1.
- 29.Xu YH, Xu ZH, Liu XS, et al. Clinical findings in critical ill patients infected with SARS-Cov-2 in Guangdong Province, China: a multi-center, retrospective, observational study. Published 2020. Accessed 20 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.03.20030668v1.
- 30.Liu YB, Li JL, Liu DH, et al. Clinical features and outcomes of 2019 novel coronavirus-infected patients with cardiac injury. Published 2020. Accessed 21 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.11.20030957v1.
- 31.Peng YD, Meng K, Guan HQ, et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(0):E004. doi: 10.3760/cma.j.cn112148-20200220-00105. [DOI] [PubMed] [Google Scholar]
- 32.Zhang GQ, Hu C, Luo LJ, et al. Clinical features and outcomes of 221 patients with COVID-19 in Wuhan, China. Published 2020. Accessed 16 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.02.20030452v1. [DOI] [PMC free article] [PubMed]
- 33.Liu T, Zhang JY, Yang YH, et al. The potential role of IL-6 in monitoring severe case of coronavirus disease 2019. Published 2020. Accessed 22 Mar 2020. https://www.medrxiv.org/content/10.1101/2020.03.01.20029769v2.
- 34.Wu J, Li W, Shi XW, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med. 2020:288(1):128-38. [DOI] [PubMed]
- 35.Chen T, Wu D, Chen HL, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo T, Fan YZ, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed]
- 37.Ndrepepa G, Kastrati A. Creatine kinase myocardial band - a biomarker to assess prognostically relevant periprocedural myocardial infarction. Int J Cardiol. 2018;270:118–119. doi: 10.1016/j.ijcard.2018.07.077. [DOI] [PubMed] [Google Scholar]
- 38.Vasudevan G, Mercer DW, Varat MA. Lactic dehydrogenase isoenzyme determination in the diagnosis of acute myocardial infarction. Circulation. 1978;57(6):1055–1057. doi: 10.1161/01.CIR.57.6.1055. [DOI] [PubMed] [Google Scholar]
- 39.Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020. [DOI] [PMC free article] [PubMed]
- 40.Peiris JS, Chu CM, Cheng VC, Chan KS, Hung IF, Poon LL, Law KI, Tang BS, Hon TY, Chan CS, et al. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet (London, England) 2003;361(9371):1767–1772. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Erden I, Erden EC, Ozhan H, Basar C, Yildirim M, Yalçin S, Aydin LY, Dumlu T. Echocardiographic manifestations of pandemic 2009 (H1N1) influenza a virus infection. J Infection. 2010;61(1):60–65. doi: 10.1016/j.jinf.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 42.Haessler S, Paez A, Rothberg M, Higgins T. 2009 pandemic H1N1-associated myocarditis in a previously healthy adult. Clin Microbiol Infection. 2011;17(4):572–574. doi: 10.1111/j.1469-0691.2010.03315.x. [DOI] [PubMed] [Google Scholar]
- 43.Chacko B, Peter JV, Pichamuthu K, Ramakrishna K, Moorthy M, Karthik R, John G. Cardiac manifestations in patients with pandemic (H1N1) 2009 virus infection needing intensive care. J Critical Care. 2012;27(1):106. doi: 10.1016/j.jcrc.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 44.Kumar K, Guirgis M, Zieroth S, Lo E, Menkis AH, Arora RC, Freed DH. Influenza myocarditis and myositis: case presentation and review of the literature. Can J Cardiol. 2011;27(4):514–522. doi: 10.1016/j.cjca.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Ito T, Akamatsu K, Ukimura A, Fujisaka T, Ozeki M, Kanzaki Y, Ishizaka N: The Prevalence and findings of subclinical influenza-associated cardiac abnormalities among Japanese Patients. Internal Med (Tokyo, Japan) 2018, 57(13):1819–1826. [DOI] [PMC free article] [PubMed]
- 46.Borgatta B, Pérez M, Rello J, Vidaur L, Lorente L, Socías L, Pozo JC, Pozo J, Garnacho-Montero J, Rello J. Elevation of creatine kinase is associated with worse outcomes in 2009 pH1N1 influenza A infection. Intensive Care Med. 2012;38(7):1152–1161. doi: 10.1007/s00134-012-2565-5. [DOI] [PubMed] [Google Scholar]
- 47.O'Brien PJ. Cardiac troponin is the most effective translational safety biomarker for myocardial injury in cardiotoxicity. Toxicology. 2008;245(3):206–218. doi: 10.1016/j.tox.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 48.Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020. [DOI] [PMC free article] [PubMed]
- 49.Sala S, Peretto G, Gramegna M, Palmisano A, Villatore A, Vignale D, De Cobelli F, Tresoldi M, Cappelletti AM, Basso C, et al. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J. 2020;41(19):1861–1862. doi: 10.1093/eurheartj/ehaa286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zeng JH, Liu YX, Yuan J, Wang FX, Wu WB, Li JX, Wang LF, Gao H, Wang Y, Dong CF, et al. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection. 2020:1–5. [DOI] [PMC free article] [PubMed]
- 51.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. Jama. 2020. [DOI] [PMC free article] [PubMed]
- 52.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–2. [DOI] [PMC free article] [PubMed]
- 53.Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141(20):1648-55. [DOI] [PubMed]
- 54.Du RH, Liang LR, Yang CQ, Wang W, Cao TZ, Li M, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524. [DOI] [PMC free article] [PubMed]
- 55.Convertino I, Tuccori M, Ferraro S, Valdiserra G, Cappello E, Focosi D, Blandizzi C. Exploring pharmacological approaches for managing cytokine storm associated with pneumonia and acute respiratory distress syndrome in COVID-19 patients. Critical Care (London, England) 2020;24(1):331. doi: 10.1186/s13054-020-03020-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Welt FGP, Shah PB, Aronow HD, Bortnick AE, Henry TD, Sherwood MW, et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC’s interventional council and SCAI. J Am Coll Cardiol. 2020. [DOI] [PMC free article] [PubMed]
- 57.Peng QY, Wang XT, Zhang LN. Using echocardiography to guide the treatment of novel coronavirus pneumonia. Critical Care (London, England) 2020;24(1):143. doi: 10.1186/s13054-020-02856-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Clinical characteristics of patients with COVID-19.
Data Availability Statement
All the data supporting the conclusions of this article are included within the article.