Abstract
目的
寻求影响COVID-19患者临床分型与转归的关键指标以指导临床诊疗,并探索中性粒细胞/淋巴细胞比值(NLR)在COVID-19中的应用。
方法
收集2020年2~4月援鄂期间在湖北省鄂州市中心医院确诊的COVID-19患者共93例,其中ICU危重病例43例,随机选择呼吸科普通型病例50例进行对照研究,收集所有患者入院时和住院期间的基线资料、血常规、生化指标。计算NLR值,按照文献NLR四分类法对患者进行COX生存分析;根据患者转归信息绘制受试者工作曲线(ROC),根据NLR截断值将患者分为2类,与临床分类比较以评价截断值分类的科学性;根据患者转归、NLR截断值分类及临床分型进行多重二元logistics回归,筛选关键变量,并探讨其在COVID-19中的意义。
结果
NLR四分类法不适合COVID-19患者预后判断;NLR预测患者死亡的截断值为11.26,敏感性为0.903,特异性为0.839;NLR < 11.26患者血常规,生化指标与普通型无统计学差异(P > 0.05),NLR≥11.26患者上述指标与危重型患者无统计学差异(P > 0.05);NLR,白血病计数(WBC),中性粒细胞绝对值(NEUT),降钙素原(PCT),D-二聚体(DD),尿素氮(BUN),肌钙蛋白(I TNI),脑钠肽(BNP),乳酸脱氢酶(LDH)对患者临床分型、转归均有明显影响(P < 0.05);此外,血肌酐(Cr)、血清钙(Ca)、PH、乳酸(Lac)对患者转归有较大影响(P < 0.05);血清钠(Na)与动脉血二氧化碳分压(PCO2)对患者临床分型有较大影响(P < 0.05)。
结论
NLR可以作为COVID-19临床分型、预后评估、生化异常的重要预警因子;危重型及预后差的患者多合并细菌感染、炎症反应更强烈、心肺肾功能损伤更重,常伴有DD,LDH明显升高;NLR、NEUT、DD、TNI、BNP、LDH、Ca、PCT、PH、Lac对COVID-19预后影响较大,应动态观察。
Keywords: 新型冠状病毒肺炎, 临床类型, 中性粒细胞/淋巴细胞比值, 生化分析
Abstract
Objective
To identify the key biochemical indicators that affect the clinical type and outcomes of COVID-19 patients and explore the application of neutrophil/lymphocyte ratio (NLR) in COVID-19.
Methods
Ninety-three patients with confirmed diagnosis of COVID-19 admitted in Ezhou Central Hospital from February to April in 2020 were analyzed. Among them, 43 patients were selected from Intensive Care Unit (ICU) with the diagnosis of critical type of COVID-19, and 50 cases of common type were selected from the Department of Respiratory Medicine. The baseline data, blood routine test and biochemical indexes of the patients were collected on the first day of admission. NLRs of the patients were calculated, and COX survival analysis according to the NLR 4-category method was performed. The patients' outcomes were analyzed with receiver operating curves (ROCs). The patients were divided into two groups according to NLR cutoff value for comparison of the biochemical indexes. Based on the patients' outcomes, NLR cutoff value classification and clinical classification, multiple binary logistics regression was performed to screen the key variables and explore their significance in COVID-19.
Results
The NLR four-category method was not applicable for prognostic evaluation of the patients. The cut-off value of NLR for predict the prognosis of COVID-19 was 11.26, with a sensitivity of 0.903 and a specificity of 0.839; the laboratory indicators of the patients with NLR < 11.26 were similar to those in patients of the common type; the indicators were also similar between patients with NLR≥11.26 and those with critical type COVID-19. NLR, WBC, NEUT, PCT, DD, BUN, TNI, BNP, and LDH had significant effects on the clinical classification and outcome of the patients (P < 0.05); Cr, Ca, PH, and Lac had greater impact on the outcome of the patients (P < 0.05), while Na, PCO2 had greater impact on the clinical classification of the patients (P < 0.05).
Conclusion
NLR can be used as an important reference for clinical classification, prognostic assessment, and biochemical abnormalities of COVID-19. Patients of critical type more frequently have bacterial infection with more serious inflammatory reactions, severer heart, lung and kidney damages, and much higher levels of DD and LDH than those of the common type. NLR, NEUT, DD, TNI, BNP, LDH, Ca, PCT, PH, and Lac have obvious influence on the prognosis of COVID-19 and should be observed dynamically.
Keywords: SARS-CoV-2, clinical type, the neutrophil-to-lymphocyte ratio, biochemical analysis
2019新型冠状病毒肺炎(COVID-19)临床表现及预后差异极大。中国疾控中心提供的数据表明:共计72 314例COVID-19患者中,轻型占81.4%,重型占13.9%,危重型占4.7%[1]。目前研究认为[2-3],COVID-19病毒对免疫系统的攻击,导致TH1/TH2免疫失衡与致命性的细胞因子风暴并对组织器官的损伤,是多器官功能衰竭与脓毒症休克的重要病理机制。炎症与免疫紊乱与器官功能的损伤、凝血激活与循环的稳定、患者的临床分型及预后密切相关,是患者病情进展与临床疗效的根本决定因素,也应该成为病情评估与预后判断的依据。
众所周知,不同于其他病毒感染性疾病,许多COVID-19患者表现为外周血淋巴细胞降低[4-5],体现了本病炎症与免疫紊乱的表型的特殊性,这种特征性的炎症状态对于各器官功能影响有何不同,与患者预后和临床分型的紧密相关的指标有哪些,能否筛选出具有代表性的简洁指标作为临床病情判断和预后判断的依据?
既往研究证实:中性粒细胞与淋巴细胞的比值(NLR)可反映全身急慢性炎症的情况[6-9]。对于社区获得性肺炎(CAP)患者,NLR < 11.12时30 d内无死亡发生;NLR为11.12~13.4时死亡率为30%;NLR为13.4~ 28.3时死亡率为50%;NLR > 28.3时死亡率为100%,预测效果优于肺炎严重指数(PSI)评分,CURB-65评分,C反应蛋白(CRP)及WBC[10]。本文拟通过临床回顾性研究,归纳出COVID-19普通型和危重型脏器功能变化的特点和NLR在临床分型、预后判断、主要脏器受损情况中的评估作用,为指导临床诊疗提供依据。
1. 资料和方法
1.1. 研究对象
1.1.1. 入组方法
收集2020年2~4月援鄂期间在鄂州市中心医院ICU和呼吸科病区被确诊为COVID-19患者资料共93例。包括ICU危重病例43例,这些患者研究期间已治愈或死亡,已剔除尚在治疗的11例患者;随机从同期在呼吸科住院治疗的162例COVID-19患者中选择普通型病例50例进行研究。随机方法:162例患者剔除研究截止日尚在治疗的49例患者,将剩余的113例患者的住院号及性别输入数据库,由计算机随机抽取50例患者进行对比研究,男女基本相等。
1.1.2. 纳入与排除标准
根据国家卫生与健康委员会办公厅《新型冠状病毒感染的肺炎诊疗方案》(试行第5版)诊断标准[11]纳入病例。诊断标准包括:临床表现符合发热或/和呼吸道症状,发病早期白细胞总数正常或降低,或者伴有淋巴细胞计数减少;胸部CT提示肺炎影像学表现;按照临床症状、血常规与胸部CT三项中符合两项,加上呼吸道标本RT-PCR检测新型冠状病毒核酸阳性作为确诊依据。本研究的普通型包括《新型冠状病毒肺炎诊疗方案》(试行第5版)中的普通型与重型,按照统一部署,轻型患者由鄂州市雷山医院收治,故无法获取相关资料;本研究中的普通型病例由呼吸科收治,其诊断标准为:符合新型冠状病毒肺炎的诊断标准并排除危重型的患者。危重型诊断标准:符合新型冠状病毒肺炎的诊断标准并具有下列任何一条:(1)动脉氧分压(PaO2)/吸氧浓度(FIO2)≤150 mmHg;(2)需要机械通气支持;(3)休克。危重型病例全部由ICU收治。排除标准如下:其他各种类型的细菌性肺炎、间质性肺炎、心力衰竭合并肺水肿、心源性休克、肺部肿瘤等患者;新型冠状病毒核酸检测阴性患者。
1.1.3. 临床治愈(出院)标准
对于临床治愈(出院)患者,执行国家卫生与健康委员会办公厅《新型冠状病毒感染的肺炎诊疗方案》(试行第5版)标准:(1)体温恢复正常3 d以上;(2)呼吸道症状明显好转;(3)肺部影像学显示急性渗出性病变明显吸收好转;(4)连续两次呼吸道标本核酸检测阴性(采样时间至少间隔1 d)。
1.2. 研究方法
收集所有患者入院时的基线资料、血常规与超敏C反应蛋白、生化指标(反应心、肝、肾功能的指标、电解质、凝血及血气分析指标)。计算NLR值,按照文献NLR四分类法[10]对所有患者进行COX生存分析以检验该分类法对COVID-19预后评估的有效性;根据患者转归(治愈,死亡)信息绘制NLR,WBC,NEUT,LY受试者工作曲线(ROC),计算NLR截断值,根据截断值将患者分为两类,与临床分类比较二者的各种指标,以评价截断值分类的科学性。根据患者转归、NLR截断值及临床分型(普通型和危重型)进行多重二元logistics回归,分析关键变量的影响原因,并探讨其在COVID-19中的意义。
1.3. 统计方法
所有计量资料采用均数±标准差表示,采用SPSS 19.0软件包进行统计处理,两组间计量资料比较采用t检验,多组资料比较采用单因素方差分析(ANOVA),先进行Leven方差齐性检验,方差齐则以Bonferroni结果判定;方差不齐则以Tamhane结果判定;计数资料采用χ2检验。按照患者生存时间进行COX生存分析;根据患者转归绘制受试者工作曲线(ROC),并计算截断值;根据患者转归、NLR截断值分类及临床分型进行多重二元logistics回归,获得关键变量。P < 0.05表示差异具有统计学意义。
2. 结果
2.1. 一般情况于转归分析
93例患者中,危重型患者年龄明显高于普通型,男性明显多于女性,死亡率明显高于普通型。普通型均治愈,部分危重型病例经治疗后治愈出院(表 1)。
1.
病例一般情况及转归
Baseline data and outcomes of the patients
| Type | Age (year) | Male | Female | Discharged | Death |
| There are significant differences between common type and critical type in age, gender, and outcome (P < 0.01). | |||||
| Common | 55.62±18.34 | 24 | 26 | 50 | 0 |
| Critical | 69.56±10.76 | 31 | 12 | 12 | 31 |
| t /χ2 | t=4.378 | χ2=5.532 | χ2=54.070 | ||
| P | P: 0.000 | P: 0.018 | P: 0.000 | ||
2.2. NLR四分类法对COVID-19的COX回归结果
根据Cataudella研究结果[10],将患者分为NLR1(NLR < 11.12)、NLR2(NLR:11.12~13.4)、NLR3(NLR:13.4~28.3)、NLR4(NLR > 28.3)4组。根据患者转归情况(死亡,好转)进行COX回归(图 1)。可见,NLR1组累积生存率明显高于NLR2,3,4组(P < 0.01)。后3组间无统计学差异,表明NLR四分类法对COVID-19患者预后判断无意义。
1.
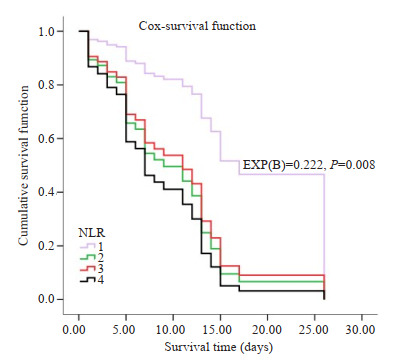
NLR四分类法对COVID-19的COX回归分析
COX regression analysis of the outcomes of COVID-19 patients by four parts of NLR.
2.3. NLR对COVID-19的预后分析
为找到简便易行的COVID-19的预后指标,我们采用NLR,WBC,NEUT,LY 4个指标对COVID-19患者进行预后分析,通过ROC曲线计算曲线下面积(AUC),筛选最佳指标,并根据Yuden Index获取最佳截断值、敏感性和特异性(图 2、表 2)。
2.
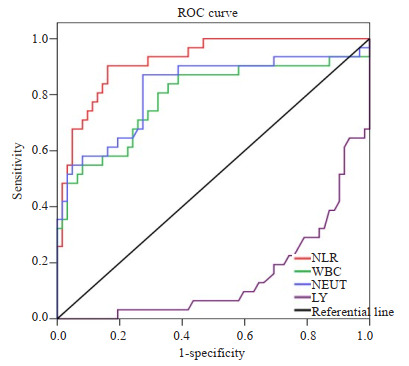
NLR,WBC,NEUT,LY预测患者转归的ROC
ROC predicting the outcomes.
2.
最佳截断值,敏感性,特异性
Cutoff value, sensitivity and specificity
| Variable | Cutoff value | Sensitivity | Specificity |
| The AUC of NLR, WBC, NEUT and LY are respectively 0.921 ± 0.028, 0.789±0.056, 0.821±0.052, 0.150±0.042. Obviously, NLR is the most advantageous index to predict the prognosis with high sensitivity and specificity(0.903, 0.839). | |||
| NLR | 11.26 | 0.90 | 0.84 |
| WBC | 7.54 | 0.84 | 0.65 |
| NEUT | 6.87 | 0.87 | 0.73 |
| LY | 0.95 | 0.16 | 0.31 |
从ROC及AUC可以看出,NLR在评价COVID-19预后方面优于WBC,NEUT,LY等指标(AUC: 0.921± 0.028,P=0.000,95%CI: 0.867~0.976),NLR预测患者死亡的最佳截断值为11.26,敏感性为0.903,特异性为0.839,均高于其他指标。
2.4. NLR对COVID-19病情与转归评估
将患者按照NLR截断值分为2组,NLR≥11.26组患者,其年龄明显高于NLR < 11.26组、男性高于女性、危重型患者明显多于普通型、死亡患者明显多于好转患者;NLR < 11.26时普通型患者明显多于危重型,好转患者明显多于死亡患者(表 3)。与临床分型比较,NLR截断值分类对于患者死亡预测价值优于临床分型(28/31 vs 31/43),对患者痊愈预测不及临床分型(52/62 vs 50/50)。
3.
按照NLR截断值对COVID-19评估与预后判断
Evaluation and prognosis according to the cutoff value of NLR
| NLR | Age (year) | Male | Female | Common | Critical | Discharged | Death |
| Patients with NLR≥11.26 were much older, more serious and easier to die. | |||||||
| < 11.26 | 56.98±17.57 | 28 | 27 | 46 | 9 | 52 | 10 |
| ≥11.26 | 68.87±12.42 | 27 | 11 | 4 | 34 | 3 | 28 |
| t/χ2 | t=-3.821, | χ2=3.774 | χ2=48.322 | χ2=47.078 | |||
| P | P: 0.000 | P: 0.052 | P: 0.000 | P: 0.000 | |||
在对患者器官功能评估方面,NLR < 11.26患者与普通型患者血常规,生化指标大致相近,无统计学差异;NLR≥11.26患者上述指标与危重型患者无统计学差异(表 4)。
4.
NLR截断值分型及临床分型患者血常规、生化与血气指标的比较
Comparison with NLR threshold classification and clinical classification (Mean±SD/Mediam)
| Variable | Common type | Critical type | t/z | P | NLR < 11.26 | NLR≥11.26 | t/z | P |
| There are almost no differences between clinic classification and NLR classification according to its cutoff value in the laboratory indicators. | ||||||||
| NLR | 5.2±4.3 | 33.8±29.3 | 6.2 | 0.000 | 4.8±2.9 | 37.8±29.4 | -6.9 | 0.000 |
| WBC | 6.2±2.8 | 13.2±6.5 | 6.4 | 0.000 | 6.6±3.2 | 13.7±7.1 | -5.8 | 0.000 |
| NEUT | 4.6±2.7 | 12.1±6.3 | 7.1 | 0.000 | 4.9±3.0 | 12.8±6.7 | -6.7 | 0.000 |
| LY | 1.2±0.6 | 0.6±0.4 | -5.8 | 0.000 | 1.2±0.6 | 0.4±0.3 | 8.6 | 0.000 |
| ALT | 41.6 | 53.2 | -2.1 | 0.039 | 42.1 | 54.1 | -2.1 | 0.034 |
| AST | 36.9 | 58.7 | -3.9 | 0.000 | 39.7 | 57.5 | -3.1 | 0.002 |
| TBIL | 42.0 | 52.8 | -1.9 | 0.056 | 43.0 | 52.8 | -1.7 | 0.086 |
| DBIL | 36.1 | 59.7 | -4.2 | 0.000 | 38.2 | 59.8 | -3.8 | 0.000 |
| Cr | 66.1±28.9 | 133.4±102.4 | 4.0 | 0.000 | 69.3±32.2 | 130.3±102.2 | -3.6 | 0.001 |
| BUN | 5.7±4.6 | 17.4 ±14.2 | 5.0 | 0.000 | 6.8±6.3 | 17.3±15.1 | -4.0 | 0.000 |
| UA | 269.5±117.6 | 298.6±179.5 | 0.7 | 0.510 | 263.0±121.2 | 302.3±174.2 | -1.2 | 0.233 |
| K | 4.0±0.5 | 4.4±1.1 | 2.2 | 0.034 | 3.9±0.5 | 4.5±1.1 | -2.6 | 0.012 |
| Na | 138.6±3.9 | 143.9±7.7 | 4.1 | 0.000 | 139.5±5.4 | 143.4±7.3 | -2.8 | 0.006 |
| CL | 102.9±4.3 | 115.0±87.1 | 1.0 | 0.303 | 102.3±5.6 | 119.5±99.6 | -1.1 | 0.293 |
| Ca | 2.1±0.2 | 2.0±0.4 | -1.5 | 0.051 | 2.1±0.2 | 1.9±0.4 | 2.4 | 0.020 |
| PT | 13.9±7.4 | 17.6±7.4 | 2.0 | 0.052 | 14.1±7.2 | 17.0±6.9 | -1.9 | 0.060 |
| APTT | 36.6±9.2 | 42.2±12.0 | 2.0 | 0.054 | 38.4±10.1 | 40.0±11.6 | -0.2 | 0.809 |
| FIB | 3.6±1.5 | 4.1±7. 8 | 0.7 | 0.487 | 3.6±1.5 | 4.4±8.8 | -0.6 | 0.000 |
| DD | 28.7 | 65.9 | -6.4 | 0.000 | 31.4 | 67.1 | -6.3 | 0.000 |
| TNI | 23.2 | 56.6 | -6.8 | 0.000 | 27.0 | 57.5 | -6.1 | 0.000 |
| PCT | 31.2 | 64.1 | -5.9 | 0.000 | 33.4 | 65.2 | -5.6 | 0.000 |
| hsCRP | 10.0±8.7 | 17.0±4.1 | 4.7 | 0.000 | 10.3±8.1 | 17.0±5.2 | -4.6 | 0.000 |
| LDH | 240.4±153.0 | 621.9±388.4 | 5.3 | 0.000 | 267.2±152.7 | 595.8±377.7 | -4.3 | 0.000 |
| BNP | 22.1 | 51.2 | -6.0 | 0.000 | 26.0 | 51.2 | -5.0 | 0.000 |
| pH | 7.4±0.1 | 7.3±0.2 | -3.6 | 0.001 | 7.4±0.1 | 7.3±0.2 | 2.2 | 0.038 |
| PO2 | 91.3±40.8 | 61.6±17.1 | -3.3 | 0.002 | 87.6±39.7 | 64.9±24.2 | 2.4 | 0.021 |
| PCO2 | 38.9±6.2 | 63.0±20.4 | 5.6 | 0.000 | 43.4±15.2 | 58.8±20.0 | -3.0 | 0.004 |
| Lac | 1.7±0.7 | 3.1±2.6 | 2.1 | 0.051 | 1.8±0.7 | 3.0±2.7 | -1.9 | 0.069 |
2.5. 生化指标对患者转归,临床分型及NLR截断值分类的影响
按照患者转归(死亡,治愈),NLR最佳截断值(11.26),临床分型(普通型,危重型)进行二元logistics回归,发现NLR,NEUT,DD,TNI,BNP,LDH对患者三种回归均有明显影响(P < 0.05);此外,WBC,Cr,BUN,Ca,PCT,PH,Lac对患者转归影响较大(P < 0.05);WBC,BUN,Na,PCT,PCO2对患者临床分型影响较大;LY,Ca,PCO2对于NLR截断值回归影响较大(P < 0.05,表 5)。
5.
二元logistics回归分析
Binary logistics regression analysis
| Variable | Outcome regression | Cut off regression | Clinic type regression | ||||
| Score | P | Score | P | Score | P | ||
| Age (year) | 0.2 | 0.7 | 3.6 | 0.1 | 2.7 | 0.1 | |
| NLR | 8.5 | 0.0 | 11.6 | 0.0 | 7.0 | 0.0 | |
| WBC | 11.0 | 0.0 | 3.1 | 0.1 | 10.2 | 0.0 | |
| NEUT | 12.2 | 0.0 | 5.0 | 0.0 | 11.2 | 0.0 | |
| LY | 0.8 | 0.4 | 8.8 | 0.0 | 0.3 | 0.6 | |
| ALT | 0.3 | 0.6 | 0.0 | 1.0 | 0.0 | 0.9 | |
| AST | 0.0 | 1.0 | 0.0 | 0.8 | 0.1 | 0.8 | |
| CR | 7.5 | 0.0 | 1.6 | 0.2 | 1.6 | 0.2 | |
| BUN | 8.4 | 0.0 | 3.6 | 0.1 | 5.8 | 0.0 | |
| K | 1.9 | 0.2 | 1.7 | 0.2 | 2.1 | 0.1 | |
| Na | 2.5 | 0.1 | 3.2 | 0.1 | 10.6 | 0.0 | |
| Ca | 4.4 | 0.0 | 8.4 | 0.0 | 0.5 | 0.5 | |
| DD | 22.0 | 0.0 | 10.2 | 0.0 | 8.1 | 0.0 | |
| TNI | 13.9 | 0.0 | 4.6 | 0.0 | 5.0 | 0.0 | |
| PCT | 8.6 | 0.0 | 2.7 | 0.1 | 3.9 | 0.0 | |
| hsCRP | 0.9 | 0.3 | 1.9 | 0.2 | 0.7 | 0.4 | |
| LDH | 16.0 | 0.0 | 8.6 | 0.0 | 10.3 | 0.0 | |
| BNP | 13.8 | 0.0 | 5.3 | 0.0 | 7.9 | 0.0 | |
| pH | 7.5 | 0.0 | 1.6 | 0.2 | 1.3 | 0.3 | |
| PO2 | 0.9 | 0.3 | 0.6 | 0.4 | 2.5 | 0.1 | |
| PCO2 | 1.6 | 0.2 | 4.8 | 0.0 | 9.5 | 0.0 | |
| Lac | 6.8 | 0.0 | 1.0 | 0.3 | 2.1 | 0.2 | |
3. 讨论
COVID-19表面的糖蛋白可与细胞毒性T细胞(CTL)和B细胞上有多个位点相结合,通过激活核转录因子-κB(NF-κB)信号通路、细胞外信号调节激酶(ERK)信号通路、磷脂酰肌醇-3-羟激酶(PI3K)/蛋白激酶B(Akt)信号通路等激活免疫反应[12-13]、诱导机体炎症、促进活性氧簇(ROS)的产生从而引起氧化应激、损伤组织细胞、通过损伤相关的分子模式(DAMPS)进一步诱导炎性因子,从而导致炎症风暴。炎症风暴激活凝血,诱导炎症性肺水肿与顽固低O2及CO2潴留,最终引起不同的多器官功能障碍的组合,是患者不同的预后和临床特征的病理基础。
本研究中,危重型患者年龄明显高于普通型,死亡率高达72.93%,普通型没有死亡病例。研究表明,65岁以上的老年人,接种流感疫苗产生的保护性抗体滴度只有正常成年人的50%[14]。因此,老年人对COVID-19的易感性明显增加;同时,老年人多合并心血管疾病(CVD)等基础疾病,免疫状态异常也易于诱发CVD[15-16],可能是高龄患者易于演变成危重型和预后差的原因。
人类的免疫体系包括固有免疫系统和适应性免疫系统,中性粒细胞主要执行固有免疫反应,淋巴细胞则与适应性免疫相关[17]。已证实,COVID-19患者淋巴细胞CD3、CD4、CD8细胞水平在危重症中明显降低;WBC、NEUT、CRP、PCT水平在危重症中明显升高[18],与本研究基本吻合,表明危重症患者免疫紊乱更为严重,固有免疫亢进而获得性免疫抑制,组织损伤严重而病毒清除能力不足,导致死亡率明显高于普通型。这种免疫表象在外周血象方面表现为NEUT升高,LY降低,而NLR明显升高,并与病情及预后密切相关。
为探索NLR在COVID-19中的意义,根据CAP的预后评估经验,我们首先按照NLR四分类法对COVID-19的转归进行COX回归分析,发现NLR < 11.12组转归明显好于其他三组,其他三组无显著性差异,提示四分类对COVID-19预后意义不大,一旦NLR≥11.12,患者死亡率就明显攀升;为此,对所有患者按照转归绘制NLR,WBC,NEUT,LY的ROC曲线,并计算AUC及临界值。发现NLR对患者转归的判断明显优于其他指标,11.26为NLR最佳截断值,敏感性为0.903、特异性为0.839,可以作为COVID-19转归的预警信号。为进一步明确NLR对患者病情的总体评估,我们将普通型和危重型患者的血常规、肝肾功能、电解质、凝血指标、超敏C反应蛋白、肌钙蛋白、脑钠肽、血气分析等指标进行统计分析,同时以NLR最佳截断值将患者分为NLR < 11.26和NLR≥11.26两组,进行上述分析,发现NLR < 11.26患者上述指标与普通型接近,NLR≥11.26与危重型接近。基于NLR可作为急慢性炎症的灵敏的指标,综合其他实验室指标可以看出:危重型患者较普通型更多地合并细菌感染、炎症反应更强烈、心肺肾功能损伤更重、DD,LDH明显升高。表明COVID-19系统性炎症是患者临床表现、生化与血气指标异常的根本原因,NLR可反应COVID-19总体病情,可作为临床分型的重要的参考。
免疫反应可以引起细胞代谢重新编程[19],通过分析免疫反应诱发的代谢方式改变,可以总结本病的发生发展规律,为临床诊疗及病情预后提供依据。为筛选对患者的临床转归和临床分型影响的关键指标,我们将血常规、生化、血气等指标以转归、NLR截断值和临床分型为依据,进行三重二元logistics回归分析,发现NLR,NEUT,DD,TNI,BNP,LDH对3个观察终点均有明显影响,表明COVID-19感染后,NEUT增多、NLR升高、凝血系统的激活、心肌损伤及心衰出现、LDH升高的患者容易发展成危重型,预后差;此外,WBC,Cr,BUN,Ca,PCT,PH,Lac对患者转归影响较大,表明COVID-19感染后,合并细菌感染、肾功能快速恶化、血钙低、酸中毒及微循环早期衰竭的患者预后也差;WBC,BUN,Na,PCT,PCO2对患者临床分型影响较大,表明COVID-19感染后,合并细菌性感染,基础肾功能不全的患者,CO2潴留或伴慢阻肺的患者易演变为危重型;LY,Ca,PCO2对于NLR截断值回归影响较大,表明COVID-19感染后,NLR比值高的患者更易伴有低钙、CO2潴留。
NLR升高是COVID-19院内死亡的独立的危险因素[20],一方面中性粒细胞被大量激活,产生大量的促炎因子和严重的氧化应激[21],后者损伤内皮细胞,激活凝血系统,进一步加剧炎症[22]。另一方面淋巴细胞降低,不利于调节炎症,保护组织器官,表明机体处于病理的应激状态[23]。此外,炎症-血栓相互激活[24],更易出现器官功能障碍,与预后不良相关。因此危重型和死亡组患者NLR、NEUT与DD均明显升高。严重的低氧,尤其伴有ARDS患者,可直接导致心肌损伤[25-26];危重患者常合并肾功能不全,TNI排泄障碍[27];此外,患者尸检证实:高的病毒载量可诱发的爆发性心肌炎[28-30],这些因素是危重患者TNI,LDH升高及死亡的重要原因。心肌的损伤势必导致心衰、危重型患者ARDS导致肺动脉高压及右心衰[31],均与BNP升高及预后差相关。
当患者合并细菌感染后,可迅速进展为Ⅱ型呼衰,进一步诱发心肾功能障碍及微循环功能障碍[32],导致严重的酸中毒,因此,危重型患者常表现为WBC,Cr,BUN,PCT,PCO2,Lac升高;危重型患者pH与血Ca降低。推测危重型患者虽然存在酸中毒,但交感神经兴奋导致儿茶酚胺毒性,可引起Ca离子通道障碍,可诱发细胞内Ca超载而引起低血Ca。NLR升高与血Ca低,CO2潴留相关,体现了炎症风暴激活交感及诱导炎症性肺水肿,从而导致严重的呼吸衰竭。
本研究中,LY在危重型组明显降低(P: 0.000),但在二元logistics回归分析中,其得分较低,并未对患者的转归变量和临床分型变量产生明显的影响;此外,以转归为变量绘制的ROC曲线,LY对预后的评估远不及NLR,WBC及NEUT。既往研究虽表明[33]LY是COVID-19较好的诊断指标,但本研究中LY对患者转归预测和临床分型的判断作用不大。虽然危重型患者年龄,hsCRP明显高于普通组(P: 0.000),但二者对转归变量和临床分型影响不大,表明心肾功能,微循环状态,血气指标,NLR等更能体现疾病的严重性和危险性。
当然,本研究属于回顾性分析,没有进行严格的随机对照设计,也没有考虑患者的基础健康状态,因此研究结果可能有一些偏差;同时,本研究属于单中心研究,研究层次比较浅,需要更深入的多中心研究,以更全面的把握本病的发展规律。
Biography
李红兵,博士,副主任医师,E-mail: mrbright789@sina.com
Funding Statement
贵州省科学技术基金资助项目(黔科合基础[2019]1005)
Contributor Information
李 红兵 (Hongbing LI), Email: mrbright789@sina.com.
赵 茂军 (Maojun ZHAO), Email: 1954483828@qq.com.
References
- 1.张 彦平, 王 岚. 新型冠状病毒肺炎流行病学特征分析. http://d.old.wanfangdata.com.cn/Periodical/zgrsghbzz202005006. 中华流行病学杂志. 2020;41(2):145–51. [张彦平, 王岚.新型冠状病毒肺炎流行病学特征分析[J].中华流行病学杂志, 2020, 41(2): 145-51.] [Google Scholar]
- 2.Huang CL, Wang YM, Li XW, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. http://cn.bing.com/academic/profile?id=e5e6e43ac9e6f8e9ccf742ff5ad1095b&encoded=0&v=paper_preview&mkt=zh-cn. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [Huang CL, Wang YM, Li XW, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China[J]. Lancet, 2020, 395(10223): 497-506.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen NS, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. http://cn.bing.com/academic/profile?id=426e7b324629c9565056d095b22b09a1&encoded=0&v=paper_preview&mkt=zh-cn. Lancet. 2020;395(10223):507–13. doi: 10.1016/S0140-6736(20)30211-7. [Chen NS, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study[J]. Lancet, 2020, 395(10223): 507-13.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang RR, Pan M, Zhang XM, et al. Epidemiological and clinical features of 125 Hospitalized Patients with COVID-19 in Fuyang, Anhui, China. https://www.ncbi.nlm.nih.gov/pubmed/32289565. Int J Infect Dis. 2020;95:421–8. doi: 10.1016/j.ijid.2020.03.070. [Wang RR, Pan M, Zhang XM, et al. Epidemiological and clinical features of 125 Hospitalized Patients with COVID-19 in Fuyang, Anhui, China[J]. Int J Infect Dis, 2020, 95: 421-8.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.丁 义, 黄 增发, 赵 胜超, et al. 新型冠状病毒肺炎(COVID-19)临床及影像学特征分析. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=fsxsj202003009. 放射学实践. 2020;35(3):281–5. [丁义, 黄增发, 赵胜超, 等.新型冠状病毒肺炎(COVID-19)临床及影像学特征分析[J].放射学实践, 2020, 35(3): 281-5.] [Google Scholar]
- 6.Corriere T, Di Marca S, Cataudella E, et al. Neutrophil-tolymphocyte ratio is a strong predictor of atherosclerotic carotid plaques in older adults. https://www.researchgate.net/publication/320874979_Neutrophil_To_Lymphocyte_Ratio_Is_A_Strong_Predictor_Of_Atherosclerotic_Carotid_Plaques_In_Older_Adults. Nutr Metab Cardiovasc Dis. 2018;28(1):23–7. doi: 10.1016/j.numecd.2017.10.022. [Corriere T, Di Marca S, Cataudella E, et al. Neutrophil-tolymphocyte ratio is a strong predictor of atherosclerotic carotid plaques in older adults[J]. Nutr Metab Cardiovasc Dis, 2018, 28(1): 23-7.] [DOI] [PubMed] [Google Scholar]
- 7.Nicoletis I, Pasco J, Maillot F, et al. High pre-treatment neutrophil-tolymphocyte ratio in patients with dermatomyositis/polymyositis predicts an increased risk of cancer. Eur J Dermatol. 2020 doi: 10.1684/ejd.2020.3756. [Nicoletis I, Pasco J, Maillot F, et al. High pre-treatment neutrophil-tolymphocyte ratio in patients with dermatomyositis/polymyositis predicts an increased risk of cancer[J]. Eur J Dermatol, 2020 DOI: 10.1684/ejd.2020.3756.] [DOI] [PubMed] [Google Scholar]
- 8.Hu J, Zhou W, Zhou ZM, et al. Elevated neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios predict post-stroke depression with acute ischemic stroke. http://cn.bing.com/academic/profile?id=6ac3ad0e98c05c0812a4ddc24139c10e&encoded=0&v=paper_preview&mkt=zh-cn. Exp Ther Med. 2020;19(4):2497–504. doi: 10.3892/etm.2020.8514. [Hu J, Zhou W, Zhou ZM, et al. Elevated neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios predict post-stroke depression with acute ischemic stroke[J]. Exp Ther Med, 2020, 19(4): 2497-504.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eren MA, Güneş AE, Kırhan İ, et al. The role of the platelet-tolymphocyte ratio and neutrophil-to-lymphocyte ratio in the prediction of length and cost of hospital stay in patients with infected diabetic foot ulcers: a retrospective comparative study. Acta Orthop Traumatol Turc. 2020;54(2):127–31. doi: 10.5152/j.aott.2020.02.518. [Eren MA, Güneş AE, Kırhan İ, et al. The role of the platelet-tolymphocyte ratio and neutrophil-to-lymphocyte ratio in the prediction of length and cost of hospital stay in patients with infected diabetic foot ulcers: a retrospective comparative study[J]. Acta Orthop Traumatol Turc, 2020, 54(2): 127-31.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cataudella E, Giraffa CM, Di Marca S, et al. Neutrophil-tolymphocyte ratio: an emerging marker predicting prognosis in elderly adults with community-acquired pneumonia. https://www.ncbi.nlm.nih.gov/pubmed/28407209. J Am Geriatr Soc. 2017;65(8):1796–801. doi: 10.1111/jgs.14894. [Cataudella E, Giraffa CM, Di Marca S, et al. Neutrophil-tolymphocyte ratio: an emerging marker predicting prognosis in elderly adults with community-acquired pneumonia[J]. J Am Geriatr Soc, 2017, 65(8): 1796-801.] [DOI] [PubMed] [Google Scholar]
- 11.新型冠状病毒感染的肺炎诊疗方案(试行第五版)[ J].江苏中医药, 2020, 52(2): 封3, 封4.
- 12.李 振, 俞 科贤. 苦参多路径抗冠状病毒的机制探究. http://d.old.wanfangdata.com.cn/Periodical/zcy202004010. 中草药. 2020;51(4):888–94. [李振, 俞科贤.苦参多路径抗冠状病毒的机制探究[J].中草药, 2020, 51(4): 888-94.] [Google Scholar]
- 13.Baruah V, Bose S. Immunoinformatics-aided identification of T cell and B cell epitopes in the surface glycoprotein of 2019-nCoV. http://cn.bing.com/academic/profile?id=aa52deca300c80b24ef8794ea83fdd6b&encoded=0&v=paper_preview&mkt=zh-cn. J MED VIROL. 2020;92(5):495–500. doi: 10.1002/jmv.25698. [Baruah V, Bose S. Immunoinformatics-aided identification of T cell and B cell epitopes in the surface glycoprotein of 2019-nCoV[J]. J MED VIROL, 2020, 92(5): 495-500] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu WM, Van d ZBAM, Boog CJP, et al. Aging and impaired immunity to influenza viruses: Implications for vaccine development. http://cn.bing.com/academic/profile?id=7ade0d21a3e909dee59c12ff4ba486e6&encoded=0&v=paper_preview&mkt=zh-cn. Hum Vaccines. 2011;7(sup1):94–8. doi: 10.4161/hv.7.0.14568. [Liu WM, Van d ZBAM, Boog CJP, et al. Aging and impaired immunity to influenza viruses: Implications for vaccine development [J]. Hum Vaccines, 2011, 7(sup1): 94-8.] [DOI] [PubMed] [Google Scholar]
- 15.Zidar DA, Al-Kindi SG, Liu YM, et al. Association of lymphopenia with risk of mortality among adults in the US general population. http://cn.bing.com/academic/profile?id=c3c6be6a8023cd2c30d39cd95b560896&encoded=0&v=paper_preview&mkt=zh-cn. JAMANetw Open. 2019;2(12):e1916526. doi: 10.1001/jamanetworkopen.2019.16526. [Zidar DA, Al-Kindi SG, Liu YM, et al. Association of lymphopenia with risk of mortality among adults in the US general population[J]. JAMANetw Open, 2019, 2(12): e1916526.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tall AR, Yvan-Charvet L. Cholesterol, inflammation and innate immunity. http://d.old.wanfangdata.com.cn/NSTLQK/NSTL_QKJJ0217558346/ Nat Rev Immunol. 2015;15(2):104–16. doi: 10.1038/nri3793. [Tall AR, Yvan-Charvet L. Cholesterol, inflammation and innate immunity[J]. Nat Rev Immunol, 2015, 15(2): 104-16.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.吴 田田, 姚 咏明. 脓毒症免疫紊乱及其临床意义. http://d.old.wanfangdata.com.cn/Periodical/jfjyxzz201702002. 解放军医学杂志. 2017;42(2):95–102. [吴田田, 姚咏明.脓毒症免疫紊乱及其临床意义[J].解放军医学杂志, 2017, 42(2): 95-102.] [Google Scholar]
- 18.李丹, 王梦龙, 何兵, 等. 62例新型冠状病毒肺炎患者的实验室指标分析[J/OL].武汉大学学报: 医学版, 2020, 1-5[2020-04-11].<a href="https://doi.org/10.14188/j.1671-8852.2020.0220" target="_blank">https://doi.org/10.14188/j.1671-8852.2020.0220</a>.
- 19.战祥毅, 李嘉鑫, 张薛建, 等.由代谢免疫及氧化应激角度探寻新型冠状病毒肺炎治疗方向及有效药物[J/OL].中华中医药学刊: 1-17[2020-11]. <a href="http://kns.cnki.net/kcms/detail/21.1546.R.20200331.0958.002.html" target="_blank">http://kns.cnki.net/kcms/detail/21.1546.R.20200331.0958.002.html</a>.
- 20.Liu YW, Du XB, Chen J, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. https://www.sciencedirect.com/science/article/abs/pii/S0163445320302085. J Infect. 2020:S0163-S4453(20)30208-5. doi: 10.1016/j.jinf.2020.04.002. [Liu YW, Du XB, Chen J, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19[J]. J Infect, 2020: S0163-S4453(20)30208-5.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasama T, Miwa Y, Isozaki T, et al. Neutrophil-derived cytokines: potential therapeutic targets in inflammation. http://cn.bing.com/academic/profile?id=b84c4872a4fb61b25c3d7498c61cbd6c&encoded=0&v=paper_preview&mkt=zh-cn. Curr Drug Targets InflammAllergy. 2005;4(3):273–9. doi: 10.2174/1568010054022114. [Kasama T, Miwa Y, Isozaki T, et al. Neutrophil-derived cytokines: potential therapeutic targets in inflammation[J]. Curr Drug Targets InflammAllergy, 2005, 4(3): 273-9.] [DOI] [PubMed] [Google Scholar]
- 22.Celikbilek A, Ismailogullari S, Zararsiz G. Neutrophil to lymphocyte ratio predicts poor prognosis in ischemic cerebrovascular disease. http://cn.bing.com/academic/profile?id=00894feb13be507c357b4031ac95b3bf&encoded=0&v=paper_preview&mkt=zh-cn. J Clin LabAnal. 2014;28(1):27–31. doi: 10.1002/jcla.21639. [Celikbilek A, Ismailogullari S, Zararsiz G. Neutrophil to lymphocyte ratio predicts poor prognosis in ischemic cerebrovascular disease[J]. J Clin LabAnal, 2014, 28(1): 27-31.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gibson PH, Cuthbertson BH, Croal BL, et al. Usefulness of neutrophil/lymphocyte ratio as predictor of new-onset atrial fibrillation after coronary artery bypass grafting. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=c62e47e9b74674e05cf1c3383ec88291. Am J Cardiol. 2010;105(2):186–91. doi: 10.1016/j.amjcard.2009.09.007. [Gibson PH, Cuthbertson BH, Croal BL, et al. Usefulness of neutrophil/lymphocyte ratio as predictor of new-onset atrial fibrillation after coronary artery bypass grafting[J]. Am J Cardiol, 2010, 105(2): 186-91.] [DOI] [PubMed] [Google Scholar]
- 24.Dietrich-Muszalska A, Wachowicz B. Platelet haemostatic function in psychiatric disorders: Effects of antidepressants and antipsychotic drugs. http://cn.bing.com/academic/profile?id=1ca9644727a7400c78b938ee30c702a2&encoded=0&v=paper_preview&mkt=zh-cn. World J Biol Psychiatry. 2017;18(8):564–74. doi: 10.3109/15622975.2016.1155748. [Dietrich-Muszalska A, Wachowicz B. Platelet haemostatic function in psychiatric disorders: Effects of antidepressants and antipsychotic drugs[J]. World J Biol Psychiatry, 2017, 18(8): 564-74.] [DOI] [PubMed] [Google Scholar]
- 25.Yang XB, Yu Y, Xu JQ, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. http://cn.bing.com/academic/profile?id=9bc42445132ecc7a78c8de9dda009710&encoded=0&v=paper_preview&mkt=zh-cn. Lancet Respir Med. 2020;8(5):475–81. doi: 10.1016/S2213-2600(20)30079-5. [Yang XB, Yu Y, Xu JQ, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study[J]. Lancet Respir Med, 2020, 8(5): 475-81.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruan QR, Yang K, Wang WX, et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. http://cn.bing.com/academic/profile?id=0100fe4ab997f979be7b58e762480e68&encoded=0&v=paper_preview&mkt=zh-cn. Intensive Care Med. 2020;46(5):846–8. doi: 10.1007/s00134-020-05991-x. [Ruan QR, Yang K, Wang WX, et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China[J]. Intensive Care Med, 2020, 46(5): 846-8.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang DW, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. http://cn.bing.com/academic/profile?id=b82b6e9c439b1b1758277e389146f86e&encoded=0&v=paper_preview&mkt=zh-cn. JAMA. 2020;323(11):1061–9. doi: 10.1001/jama.2020.1585. [Wang DW, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China[J]. JAMA, 2020, 323(11): 1061-9.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. http://d.old.wanfangdata.com.cn/Periodical/zhcmj202009004. Chin Med J. 2020;133(9):1025–31. doi: 10.1097/CM9.0000000000000744. [Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province[J]. Chin Med J, 2020, 133(9): 1025-31.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu Z, Shi L, Wang YJ, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. http://cn.bing.com/academic/profile?id=a6351596c7e1294322bbfc8985f05912&encoded=0&v=paper_preview&mkt=zh-cn. Lancet Respir Med. 2020;8(4):420–2. doi: 10.1016/S2213-2600(20)30076-X. [Xu Z, Shi L, Wang YJ, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome[J]. Lancet Respir Med, 2020, 8(4): 420-2.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu YX, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgkx-ec202003004. Sci China Life Sci. 2020;63(3):364–74. doi: 10.1007/s11427-020-1643-8. [Liu YX, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury[J]. Sci China Life Sci, 2020, 63(3): 364-74.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=10.1097/CRD.0000000000000317. J Am Coll Cardiol. 2020;75(18):2352–71. doi: 10.1016/j.jacc.2020.03.031. [Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic[J]. J Am Coll Cardiol, 2020, 75 (18): 2352-71.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou F, Yu T, Du RH, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. http://cn.bing.com/academic/profile?id=688eb0e3d0393e1369176af6687fd74f&encoded=0&v=paper_preview&mkt=zh-cn. Lancet. 2020;395(10229):1054–62. doi: 10.1016/S0140-6736(20)30566-3. [Zhou F, Yu T, Du RH, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study[J]. Lancet, 2020, 395(10229): 1054-62.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.于 恪, 黄 河, 邓 海燕, et al. 淋巴细胞计数对新型冠状病毒肺炎的诊断价值. http://d.old.wanfangdata.com.cn/Periodical/gdyx202008005. 广东医学. 2020;41(8):776–80. [于恪, 黄河, 邓海燕, 等.淋巴细胞计数对新型冠状病毒肺炎的诊断价值[J].广东医学, 2020, 41(8): 776-80.] [Google Scholar]


