Abstract
Introduction
Few cases of arterial thromboembolisms have been reported after novel coronavirus disease 2019 (COVID-19) in case of severe infection or in elderly patients. We report a case of femoral arterial thrombosis in a young patient after nonsevere infection.
Case description
A common femoral artery thrombosis extended in the first third of superficial and profunda femoral arteries associated with tibial posterior and popliteal artery thrombosis was diagnosed in a 24-year-old man complaining of right lower limb pain for one month. The evolution was good after anticoagulation and antiaggregant treatments and thrombectomy. Etiologic assessment was negative except for nonsevere COVID-19.
Discussion
COVID-19 accesses host cells via angiotensin-converting enzyme 2 protein, abundant in the lungs, which is also expressed by endothelial cells and is associated with important inflammatory syndrome and coagulopathy, leading to vascular lesions. Thrombosis prevalence is not fully established and seems to be higher in case of major inflammation and in the intensive care unit (ICU). Arterial thromboembolisms are described in many vascular territories, each time in elderly patients, or in case of severe infection. We described a femoral arterial thrombosis in a young patient with negative etiological assessment except nonsevere COVID-19. Treatment consists in anticoagulation and antiaggregant drugs and thrombectomy. Preventing venous thromboembolism treatment is recommended in case of severe infection or in the ICU, but there is no clear recommendation for arterial thromboembolism prevention. This case should lead us to be very careful of the arterial event risk even if the infection is nonsevere and the patient is young.
Since the beginning of novel coronavirus disease 2019 (COVID-19) in December 2019, many cases of venous thromboembolisms have been described. Arterial thromboembolisms have been reported more rarely, in case of severe infection or in elderly patients. We report a case of femoral arterial thrombosis in a 24-year-old patient after nonsevere COVID-19.
Case Report
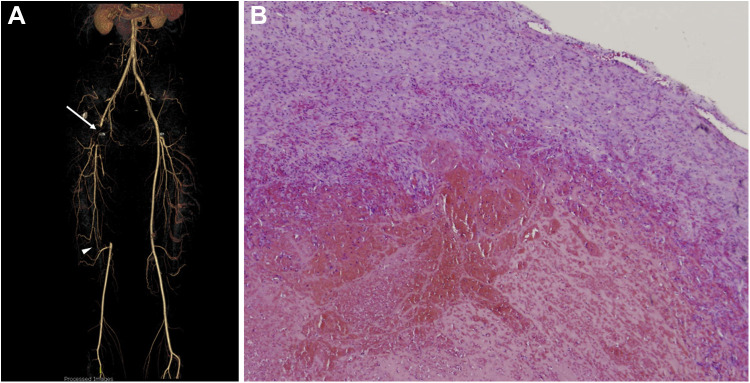
A 24-year-old Caucasian man complained of right lower limb pain for one month after flu-like syndrome evoking nonsevere COVID-19. He described initially grade III ischemia on Leriche classification with nocturnal decubitus pain and pain after walking a few meters. Symptoms gradually improved, but an intermittent claudication persisted after one month, leading him to consult his general practitioner. Echo-Doppler found right common femoral artery thrombosis, extended in the first third of superficial and profunda femoral arteries associated with tibial posterior and popliteal artery thrombosis. There was no deep venous thrombosis. AngioCT scan confirmed the right femoral and tibial posterior arterial thrombosis, found a millimetric thrombus in the peroneal artery, and showed superficial femoral artery recanalization by a muscular artery (Fig. 1 ). The patient was treated by using low-molecular-weight heparin (LMWH) and aspirin from the diagnosis. Thrombectomy was performed one week later because of the pandemic situation (reduced surgical activity, need for COVID-19 screening before hospitalization) and the absence of critical ischemia at diagnosis. It consisted in medium plan thromboendarterectomy and then superficial and profunda femoral artery thrombectomy with a Fogarty probe, finding the inflammatory and sclerotic inguinal area. Anatomopathological analysis found a fibrinocruoric thrombus without argument for septic etiology (Fig. 1). Evolution was uneventful without functional sequelae; the patient was discharged from the hospital after 3 days with apixaban and aspirin.
Fig. 1.
(A) Three-dimensional CT arterial reconstruction showing common, superficial, and profunda femoral artery thrombosis (arrow) and the muscular artery allowing superficial femoral artery recanalization (arrowhead). (B) The histologic aspect of the collateral artery showing a fibrinocruoric thrombus without argument for septic etiology.
Etiological assessment did not find cardiovascular risk factors (no active smoking, no dyslipidemia, no diabetes mellitus, no vascular family history) and no atherosclerosis of the contralateral lower limb and supra-aortic or visceral arteries. AngioCT scan showed a decreased caliber of the right external iliac artery compared with the left, but clinical presentation was not iliac artery endofibrosis (common femoral not external iliac thrombosis, no cycling, acute symptoms without previous exercise pain). He took no treatment (such as ergotamine, sildenafil) and no drug (cocaine, cannabis). There was no arrhythmia or endocarditis signs at transesophageal echocardiography. There was no biological argument for thrombophilia (normal rates of proteins C, S, antithrombin, and homocysteine; no mutation of factors V or II; no antiphospholipid) or systemic vasculitis. There was no clinical or biological argument for blood disease or solid cancer and no JAK2 mutation. The positron emission tomography scanner found lower limb vasculitis aspect. The patient described nonsevere COVID-19 few days before lower limb pain beginning, for which he received no specific treatment and stayed confined at home. Nasal RT-PCR at thrombosis diagnosis was negative, but the serologic test was positive (IgG and IgM positive–Biosynex, immunochromatography).
Discussion
Patients with COVID-19 most commonly present fever, cough, and dyspnea. Besides respiratory symptoms, several signs are described, among which some are related to vascular involvement (high blood pressure, thrombosis).1 , 2 The virus accesses host cells via angiotensin-converting enzyme 2 protein, abundant in the lungs, which is also expressed by endothelial cells.1, 2, 3 In an autopsy series, the lungs of a patient who died from COVID-19 showed severe endothelial injuries, intracellular virus, disrupted cell membranes, and widespread thrombosis with microangiopathy.2 , 3 This infection is associated with important inflammatory syndrome and coagulopathy, correlated with disease severity.1 , 4 , 5 Data from coagulation analysis on admission showed higher D-dimer levels and longer prothrombin time in nonsurvivor patients than in survivors.1 , 5 Moreover, Zhang et al.6 described antiphospholipid antibodies in 3 cases of arterial thromboembolism, in lower limb, and in cerebral arteries.
Prevalence of thrombosis among patients with COVID-19 is not fully established; most of the literature focuses on hospitalized patients.7 Most vascular events appear on the venous territory.5 , 8 Lodigiani et al.9 reported prevalence of venous thromboembolisms in 4.4%, ischemic strokes in 2.5%, acute coronary syndrome in 1.1%, in Milan Hospital, with a higher rate in patients in the intensive care unit (ICU). Thromboembolic risk seems to be higher in severe infections because of major inflammation and the need of an ICU.5 Thus, in the study by Klok et al.,10 the cumulative incidence of a composite outcome of vascular events (acute pulmonary embolism, deep-vein thrombosis, ischemic stroke, myocardial infarction, systemic arterial embolism) was 31%, the incidence of venous thromboembolisms was 27%, and the incidence of arterial events was 3.7%, among patients in the ICU.
Arterial complications take various forms. In children, COVID-19 is commonly asymptomatic but a Kawasaki-like syndrome is described.11 In adults, arterial thromboembolism has been described. Acute coronary syndrome and myocardial infarction have been reported in case of COVID-19 but seem to be infrequent.5 , 9 , 12 Vulliamy et al.13 detailed acute aortoiliac and mesenteric arterial thrombotic occlusions in a 60-year-old patient and a 75-year-old patient, respectively, while another case of acute aortic thrombosis was described in association with pulmonary embolism in a 71-year-old woman.14 Acute ischemic stroke secondary to common carotid artery thrombosis or in a prothrombotic state (leukemia) is reported.8 , 15 Finally, limb arteries can be affected in elderly patients and in pathological situations: upper limb ischemia in a 71-year-old diabetic man7 and lower limb ischemia complicated by distal cutaneous embolism in a 71-year-old aged patient with severe COVID-19.12 We present a femoral artery thrombosis in a 24 year-old adult without medical history and a negative etiological assessment except nonsevere COVID-19.
The treatment of this femoral artery thrombosis was standardized, using aspirin, LMWH, and thrombectomy. Using drugs to prevent thrombosis in COVID-19 context remains debated. To prevent venous events, prophylactic anticoagulation in high-risk situations is essential.5 Prevention of arterial complications is more difficult. Indeed, some antiviral drugs such as ritonavir interact with certain antithrombotic treatments, making their use complicated.5 Moreover, determining which patient is at high arterial thromboembolism risk seems uneasy because it could happen in nonpathological arteries, such as in the young patient with nonsevere COVID-19 reported here.
This case should lead us to be very careful of the arterial thromboembolic risk even if COVID-19 is nonsevere and the patient is young.
Conflict of interest
The authors have no conflict of interest to declare.
Acknowledgments
Authors’ contributions: F.V., C.P., and P.C. had the idea of the project and participated in the manuscript writing. C.P., A.E., N.M., J.L., and P.C. were involved in the clinical management. A.A. and P.C. reviewed the manuscript.
References
- 1.Sardu C., Gambardella J., Morelli M.B. Hypertension, thrombosis, Kidney failure, and diabetes: is COVID-19 an endothelial disease? A comprehensive evaluation of clinical and basic evidence. J Clin Med. 2020;9:1417. doi: 10.3390/jcm9051417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Varga Z., Flammer A.J., Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ackermann M., Verleden S.E., Kuehnel M. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fogarty H., Townsend L., Ni Cheallaigh C. COVID19 coagulopathy in Caucasian patients. Br J Haematol. 2020;189:1044–1049. doi: 10.1111/bjh.16749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bikdeli B., Madhavan M.V., Jimenez D. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y., Xiao M., Zhang S. Coagulopathy and antiphospholipid antibodies in patients with covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaur P., Qaqa F., Ramahi A. Acute upper limb ischemia in a patient with COVID-19. Hematol Oncol Stem Cell Ther. 2020 doi: 10.1016/j.hemonc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baldacini M., Pop R., Sattler L. Concomitant hemorrhagic syndrome and recurrent extensive arterial thrombosis in a patient with COVID-19 and acute promyelocytic leukemia. Br J Haematol. 2020;189:1054–1056. doi: 10.1111/bjh.16768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lodigiani C., Iapichino G., Carenzo L. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schroeder A.R., Wilson K.M., Ralston S.L. COVID-19 and Kawasaki Disease: Finding the Signal in the Noise. Hosp Pediatr. 2020 doi: 10.1542/hpeds.2020-000356. [DOI] [PubMed] [Google Scholar]
- 12.Mestres G., Puigmacià R., Blanco C. Risk of peripheral arterial thrombosis in COVID-19. J Vasc Surg. 2020;72:756–757. doi: 10.1016/j.jvs.2020.04.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vulliamy P., Jacob S., Davenport R.A. Acute aorto-iliac and mesenteric arterial thromboses as presenting features of COVID-19. Br J Haematol. 2020;189:1053–1054. doi: 10.1111/bjh.16760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Le Berre A., Marteau V., Emmerich J. Concomitant acute aortic thrombosis and pulmonary embolism complicating COVID-19 pneumonia. Diagn Interv Imaging. 2020;101:321–322. doi: 10.1016/j.diii.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Viguier A., Delamarre L., Duplantier J. Acute ischemic stroke complicating common carotid artery thrombosis during a severe COVID-19 infection. J Neuroradiol. 2020;47:393–394. doi: 10.1016/j.neurad.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]