Abstract
Background
The pandemic coronavirus disease 2019 (COVID-19) has taken a heavy toll on human life and has upended the medical system in many countries. The disease has created a system wide worsening shortage of N95, medical masks, and other personal protective equipment (PPE) that is regularly used by healthcare personnel and emergency service providers for their protection.
Aim
Considering the number of infected patients and the stressed supplies of PPE, reuse of PPE can serve as an efficient contingency plan. Multiple studies have investigated the effect of different decontamination methods.
Methods
We chose the most user-friendly, easily scalable viral decontamination methods, including ultraviolet irradiation and heat treatment. In this paper, we investigated a unique approach to reuse the mask by creating a hybrid model that efficiently sanitizes the infected mask.
Results
The advantages of the proposed hybrid model as compared to the respective single arms is its decontamination efficacy, operational speed, as well as the number of reuse cycles as verified by mathematical analysis and simulation. This model is mainly intended for medical PPE but can also be used for other domestic and personal sanitization during the COVID-19 pandemic. As per the situation, the hybrid system can be used as standalone systems also. This sanitization process is not only limited to the elimination of Severe acute respiratory syndrome coronavirus 2 but can be extended to any other infectious agents. Thus, our results indicate that the proposed hybrid system is more effective, meets disinfection criterion and time saving for the reuse of respirators and PPE.
Key Words: SARS-CoV-2, Mask, PPE, Sterilization, Reuse, UV, heat
Coronavirus disease 2019 (COVID-19) is a pandemic that has hit 217 countries and territories, with 3,759,967 confirmed cases and at least 259,474 deaths across the world as of May 8, 2020, according to the World Health Organization Situation Report-109. In December 2019, the first outbreak was reported in Wuhan City of China, followed by a rapid escalation of cases worldwide. COVID-19 is officially named as Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and characterized by severe infection of the respiratory system.1 In the last 2 decades, coronavirus outbreaks have become common and have affected global health. In 2002-03 SARS-CoV and again in 2011, the Middle East respiratory syndrome corona virus rattled the world.2 Coronaviruses are positive-strand RNA viruses and can be categorized into 4 genera, alpha, beta, delta, and gamma. The alpha and beta coronaviruses are known to infect humans. SARS-CoV-2 is a positive sense (+) single-stranded enveloped RNA ([+] ssRNA) virus and belongs to the beta coronavirus genus with a zoonotic origin.3 Current research suggests that bats are the viral reservoir, while pangolin may be the facilitating intermediate host causing the transmission to humans.4 The vital clinical symptoms include fever, dry cough and fatigue, while a small percentage of patients also exhibit gastrointestinal infection-related symptoms.5 High transmission rate, asymptomatic carriers, lack of testing, complex pathogenesis, and unavailability of medicine or vaccine attributed to the high infection rate of SARS-CoV-2.
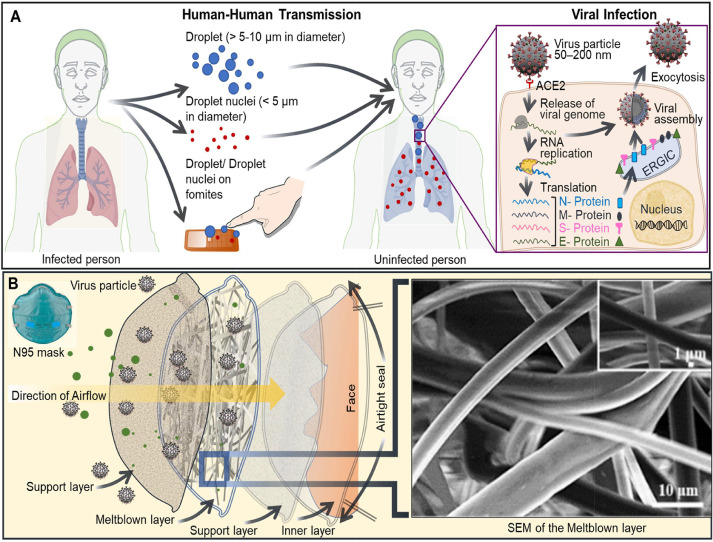
COVID-19 is a highly contagious disease, and dissemination of this virus is mainly through the transfer of virus-laden respiratory droplets. Once the virus gets deposited in the respiratory system of an uninfected person via droplets (>5-10 µm in diameter), aerosolized droplet nuclei (<5 µm in diameter) or by contact can lead to transmission.6 The virus upon replication gets transported to other organ systems like the kidney, intestine, liver, and heart.7 The droplet transmission of infection happens when the patient with respiratory symptoms comes in close proximity (under 1 m distance) or through fomites in the vicinity of a patient. Aerosolized droplet nuclei in certain circumstances can remain suspended for a longer period and also can travel distances greater than 1 m6 , 8 , 9 (Fig 1 A). The viral enters into the human cell by the interaction of the viral spike (S) glycoprotein with the human angiotensin-converting enzyme 2 receptor, followed by virus-human cell membrane fusion and subsequent internalization of the viral genome. The viral RNA induces the synthesis of more viral particles and eventually buds off from the infected cell to spread infection.10 The infection cycle is explained in Figure 1A. Epidemiological investigation suggests a median incubation period of 5.1 days and 97.5% of patients who will develop symptoms exhibit those symptoms within 14 days of infection and are also associated with viral shedding in the latency period.11
Fig 1.
SARS-CoV-2 transmission, infection, and the protective N95 mask.
(A) Human to human viral transmission and infection. Coronavirus is most commonly spread from an infected person by respiratory droplets (droplets and droplet nuclei) in the cough and sneeze. The respiratory droplets also can get deposited on fomites in close vicinity of the infected person. Touching a contaminated object or shaking compromised hands, followed by touching the mouth, nose, and eye can lead to the spread of viral infection. The larger droplets usually get deposited in the oral cavity, nasal passage and trachea, while the smaller droplet nuclei can also travel to the lower respiratory tract. Hence the concept of social distancing and wearing masks can help prevent human to human transmission. Once inside the respiratory tract, the virus infects the airway/ lung epithelial cells (Zoomed up view). The SARS-CoV-2 infections begin when the viral spike (S) protein binds to the cellular receptor angiotensin-converting enzyme 2 (ACE2). Receptor binding leads to a conformation change in the S protein that facilitates the fusion of the viral envelope with the cell membrane. Once internalized, the SARS-CoV-2 uncoats and releases RNA into the host cell and hijacks the host machinery to transcribe, replicate and translate. The positive-strand RNA gets translated into viral polymerase (RNA-dependent RNA polymerase), and subsequent RNA replication. By a mechanism of discontinuous transcription, the polymerase produces a series of sub-genomic mRNAs. The viral mRNAs then translate relevant viral proteins. Viral proteins and genomic RNA are assembled subsequently into virions in the Endoplasmic reticulum (ER) and ER-Golgi intermediate compartment (ERGIC). The virus particles undergo exocytosis and infect new cells. (B) Components of an N95 mask. Left top: An image of a typical N95 mask. Left: Diagram showing multiple layers of an N95 mask. Right: Scanning Electron micrograph of the meltblown fiber of a typical N95 mask (Lam et al., 2019). Smaller particles get trapped in the filter because of the electrostatic charge on the meltdown fiber.
Transmission control and personal protective equipment (PPE). The most effective mitigation plan is “social distancing,” isolation and self-quarantine and is practiced all over the world. As per the Centers for Disease Control and Prevention (CDC), USA, social distancing refers to maintaining a 6 feet space between yourself and other people outside of your home. An essential strategy for protecting healthcare workers, sick patients and emergency responders on the frontline of fighting with Covid19 requires the use of PPE, especially in the form of a face mask known as N95 respirator or N95 filtering facepiece respirators.12 , 13 The grade of N95 respirator is regulated by the National Institute of Occupational Safety and Health. It is meant to exhibit a minimum filtration efficiency of 95% for 0.3 µm (aerodynamic mass mean diameter) of sodium chloride aerosol.14 The SARS-CoV-2 virus is pleomorphic in form and the size ranges from 60 to 150 nm as per different investigating groups, like 70-90 nm15; ∼ 150 nm16; 60-140 nm17; 80-120. Balazy et al, 2006 showed that the N95 respirator could provide >95% protection from particles with a diameter of 80 nm.18 Therefore, the N95 mask can be highly effective in preventing airborne transmission in high-risk hospital conditions and CDC recommends its use for all healthcare professionals. However, there are some limitations to using a mask. Self-contamination may occur due to touching and reusing contaminated mask. Mainly in the health sector doctors are using a mask at random to treat infected patients and there is every chance of the mask getting infected. Therefore, after using any mask, it is essential to dispose of that mask or can be reused after disinfection. As per the CDC, surgical masks do not provide a reliable level of protection and are loose-fitting and disposable, but can protect from the exposure of large droplets, splashes or sprays of pathogenic fluids. N95 and the medical masks used in the healthcare setting is intended for 1-time use and not to be shared or reused.12 Most countries have recommended the use of single-use face masks and homemade masks for the general public.
Components of an N95 mask. There is an acute shortage of PPE, especially the N95 respirators in many countries. Health workers are facing a real challenge, forcing them to disregard the basic infection control protocols while serving corona infected patients19. Considering the cost and limited supplies, 1 option is to decontaminate the respirators and then reuse it. A recent study investigated the viability of SARS-CoV-2 on different surfaces, including plastic, and the viable virus was observed up to 72 hours (103.7 to 100.6 of the 50% tissue culture infectious dose or TCID50/ ml of media)20. Figure 1B shows the different component layers of a typical N95 mask. These layers are made of polypropylene nonwoven fabric. The most important layer (100-1000 µm) is then made by the melt-blown process in which melted polypropylene is extruded through a fine nozzle and combined with the heat-mediated self-adhesion leads to the formation of stacked, nonwoven microfibers (diameter ∼ 1-10 µm) as shown in Figure 1B.21 The microfibers are finally charged by the corona discharge method, creating the “electret” property that enhances the filtration efficacy of the mask. There are 2 options available, firstly, to dispose of the mask, which may not be a viable option due to its supply deficiency, cost-effectiveness, and biohazard disposal cost. The second option is reusing the mask after proper decontamination/sanitizing process.
Available methods for N95 mask sterilization. One sanitization option is to leave the contaminated mask for hours under the sun (direct heat) and wait for the virus on the surface of the mask to get inactivated. However, this method will be time-consuming and challenging on a large scale. Research suggests limited availability of decontaminating agents for SARS-CoV-2, including alcohol, soap solution, vaporous hydrogen peroxide (H2O2), moist heat and ultraviolet (UV) irradiation. Every method has its merits and demerits, but their effect on the SARS-CoV-2 viability needs to be strictly studied. The most common sanitizing agent ,that is, alcohol and soap, can effectively deactivate SARS-CoV-2 but significantly reduces the filtration efficacy of the N95 mask22 (Table 1 ). H2O2 vapor (HPV) and gas plasma are used for medical N95 mask decontamination recently.23 The key drawbacks of the use of H2O2 include residues left out due to insufficient off-gas time, which can pose serious respiratory and skin hazards. H2O2 is a strong oxidant, presents a combustion and explosion risk, and therefore, a skilled workforce is required to handle the decontamination system. Improper producing and limited decontamination cycles make a tricky choice. In the absence of better methods US Food and Drug Administration (FDA) has recently authorized some H2O2-based system. Electron-beam irradiation is costly and possess dangers to the user and hence not used.
Table 1.
Comparison of traditional methods
| Method | Mask condition after treatment | Degradation |
|---|---|---|
| Soap water | 78% | 21.9% |
| Alcohol | 62.9% | 37% |
| Sun (Direct heat) | 99% | Time is a constraint ( approx 5 hours) |
One of the common methods is warm moist heat (WMH), where the mask is subjected to a temperature of 65°C in a heat chamber.24, 25, 26 This affects the average log reduction of the viable virus without affecting the coating of the mask. Another method is microwave generated steam (MGS), where the contaminated mask can be loaded into a commercially available microwave oven with a small amount of water in a microwave approved pan to create steam. However, as most of the N95 and medical mask have metallic noseband so this process may not be useful. A very effective method is UV Germicidal Irradiation (UVGI), where 254 nm, UV-C lamp can be used.27 The infected mask can be exposed to a UV radiation ≥1 J/cm2 for 15 minutes for viral inactivation. However, in some types of mask penetration reachability of UV in their inner layers suffers and shadowing can cause major concerns.27 This is due to their design constraints, but this method does not harm the layering of the mask although the fitting elasticity can be hampered on repeated uses. Table 2 reflects the characteristics of all of these technical processes.
Table 2.
Comparison of the technical methods
| Method | Requirement | Virus average log reduction | Demerits |
|---|---|---|---|
| WMH | Heat chamber | 4.81 | Start-up time |
| MGS | Microwave oven | 5.06 | Not suitable for N95 |
| UVGI | UV-C lamp | 4.81 | Reaching to interior side/shadow |
| HPV | H2O2 vapour | 6 | Extra safety at the interior side |
From the above Table 2, it is clear that all the methods have a certain advantage and reach an appreciable and acceptable level of virus level reduction. However, every process has its demerits also and it can be found that hazards in the case of WMH are least and in UVGI, it is quite less. Different disinfection methods including chemical, radiation and thermal treatment, have been recommended by CDC.28 Though single agents are discussed and used by many but no hybrid systems have been tested. As a result of this, we propose a hybrid model to efficiently sanitize the compromised mask. The efficacy of this proposed model is its operational speed in achieving the high log decontamination, cheap, can be easily installed within a medical unit and ease of operation for people throughout the world.
Rationale and hypothesis. We concentrated on user-friendly, potentially scalable and time-saving decontamination methods for our study that will conserve the integrity, efficiency, and increase the number of reuse cycle of N95 and medical masks. The SARS-CoV viruses are constituted by different proteins, lipids and RNA as the genetic material and heat treatment is known to inactivate viral and bacterial pathogens.29 Heat treatment can denature proteins and affect lipid stability. Many researchers are currently trying to harness the power of UV radiation to disinfect SARS-CoV-2. Short wavelength UV also called UV-C, can inactivate the ARS-CoV at a fluence of ∼3.6 J/cm2.30 Liao et al, 2020 used moist heat (85°C, 30% RH) disinfection method and showed that in N95 can be used for 50 cycles without significant alteration in filtration efficiency. They also reported that UV irradiation could be used for 10 cycles without any alteration and with slight degradation by the 20th cycle.27 Heimbuch et al and Cadnum et al demonstrated decontamination methods like microwave-generated steam, low-temperature moist heat, and UV irradiation separately, provided >4-log reduction of viable H1N1 virus H5N1 influenza viruses without significantly affecting filtering facepiece respirators fit or function.24 As many UV-C is known to induce oxidation and RNA self-cleavage in single-stranded RNA viruses.31 We hypothesized that heat can inactivate viral protein and lipids, and UV disintegrates the genomic material (RNA), and therefore, a combination of both can be more effective in neutralizing the SARS-CoV-2 virus.
Proposed model
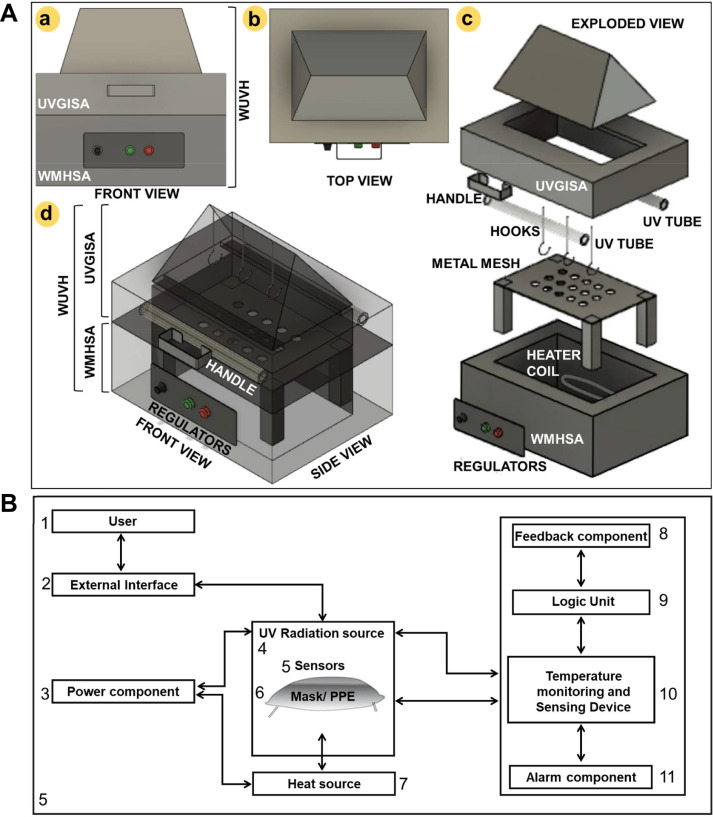
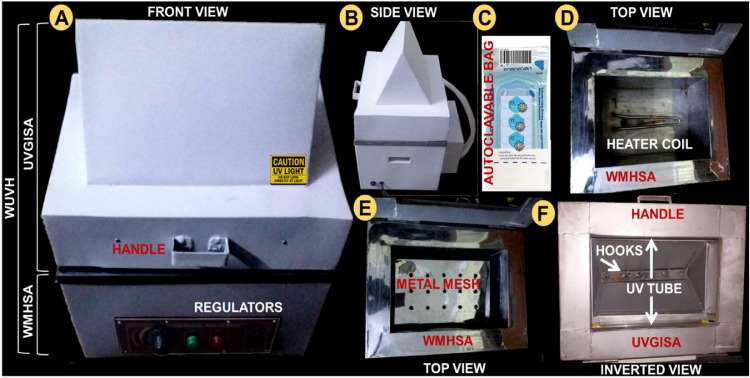
We proposed to combine 2 systems such as WMH standalone (WMHSA) and UVGI standalone (UVGISA) to harness the combined synergistic advantages into a hybrid model called Warm Ultra Violet Hybrid Model (WUVH). WUVH is designed to minimize mask degradation, maintain filtration efficiency, maximize recycle numbers, reduce price, and make it globally available. The hybrid model WUVH is developed mainly for medical PPE but can also be effectively used for industrial and domestic purposes. The standalone units WHMSA and UVGISA are shown in Figure 2 A. The process diagram is shown in Figure 2B. WHMSA consists of a sealable container with a heater coil and a mesh net at the top comprising of the physical components. Besides these, it also contains a temperature sensor, water inlet sensor and a relay as an electrical component, UV-C meter with datalogging card and alarm. The role of the temperature sensor is to maintain a constant temperature of 70°C so that the infected mask can be treated through the WMH coming through the mesh at the top of the WHMSA module. This process can be very easily scaled up and existing equipment can be modified to form a WUVH system . UVGISA consists of an evacuated chamber exposed with UV-C lamp of 254 nm and a dose of ≥ 1 J/cm 2 is supplied. Shadowing problem of UV exposure is taken care of by placing 2 UV sources positioned on opposite sides and equidistant from the position of the mask. Moreover, the walls of the WUVH has shiny UV-reflective surface making the UV-rays bounce back and forth from multiple angles. The hybrid system WUVH is shown in Figure 2 c and d, where the UVGISA is placed over the WMHSA. The arrangement of mask placement is kept within the UV chamber, where the mask can be hanged, and there is simultaneously exposed to the warm heat and the UV. UV-C photochromic card indicators may be placed in each run for confirming a dose of ≥ 1 J/cm 2 on the mask. Moreover, depending on the requirement or condition of the mask specific operation either warm heat or UV can also be applied using the same system. This hybrid model is designed with an aim to attain the average log reduction in much lesser time with less degradation in the mask surface layers.
Fig 2.
(A) 3D drawing of the proposed machine. Warm ultraviolet Hybrid model (WUVH) is a hybrid of 2 components Ultraviolet Germicidal Irradiation Standalone (UVGISA) and the Warm Moist Heat Standalone (WMHSA). (a) Front view of the WUVH. (b) Top view of the WUVH. (c) Exploded view of different components. (d) Assembled and translucent view of WUVH. (B) Process diagram of the proposed machine.
Methods
Analysis of WUVH
Considering the model of WUVH as a single input and single-output system, we effectively use an approach where the outputs can be forecasted. Model predictive control32 , 33 is used to forecast the system behavior. This is a feedback model and is used to predict the current values depending upon the difference between the actual and predicted values.x
The model is considered as a first-order time-delay model with transfer function
| (1) |
Where K is the steady-state gain, τ is the time constant and φ the delay time. These are the crucial parameters in determining the correct prediction. A stable dynamic process can be commonly defined and described by the first-order time-delay model. This model is used to obtain the initial controller tuning constant, easy to compute and have robust control. Taking a higher-order model unnecessarily will increase the system complexity with marginally better control over the first-order model but will potentially undermine the robustness of the system. The corrected predictions are made with step input at time t = 2 minutes by considering a step disturbance in the range of d = 0.15-0.20. For better operation, this step disturbance should be kept in the range of 0.15. This is because an increase in step disturbance may result in enhanced output but at the cost of shifting the process from the setpoint value. The sampling period Δt is considered to be 1 min. Moreover, for prediction, the samples are considered over a time span of 0 < t ≤ 80. Because and the step u begins at t = 2 minutes, the output y(t) starts responding and the start-up time is at t = 5 minutes. So before that, the output will be zero for the first cycle. This is because the time required for a standard heater to boil water is around 4.6 minutes. This implies that the start-up time for the disinfection cycle to start. The step input disturbance due to predicting the output, due to the past output starts at t = 8 minutes. Thus, the output step response of the system with delay can be written as
| (2a) |
| (2b) |
| (2c) |
The minimum infectious dose of SARS-CoV-2 is unknown so far, but researchers suspect it is low. Therefore, for purposes of analysis, we considered a >5 log 10 reduction of infectious agents on N95 respirators to be effective for the decontamination of respirators.
Results
This section provides the results of our scheme and its comparison by conducting 3 sets of experiments along with a statistical plot. In each set of experiments comparison of WUVH is done with UVGISA and WUVH. The performance of the proposed WUVH is done using MATLAB, and 20 independent runs have been taken while plotting the graphs.
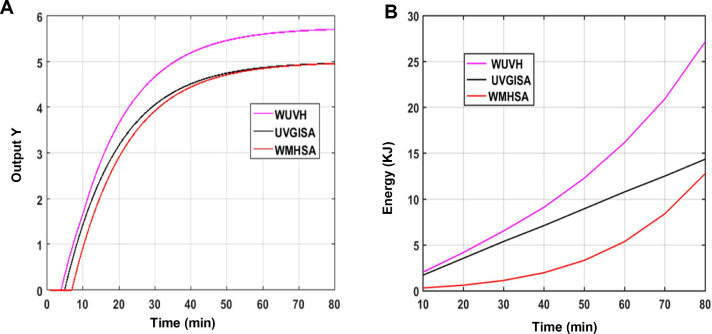
Experimental analysis
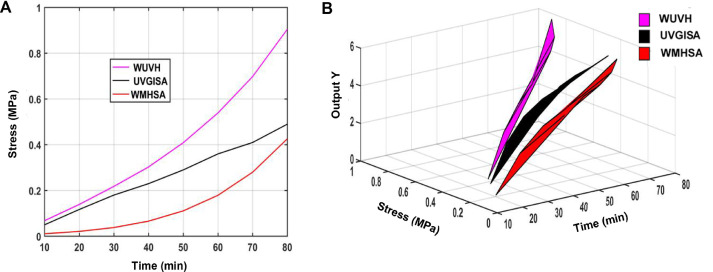
In the first set of the experiment (Fig 3 A), the output of the process in terms of achieving average log reduction after the treatment with respect to time is replicated. It can be seen from the graph that it requires a start-up time of 5 minutes. This is because the heater requires an initial start-up time for boiling the water for the first cycle. However, in a repeated cycle the initial conditions will reduce, and start-up time can be neglected in such cases implying lesser time for disinfection. After this temperature or start-up point is reached, there is an exponential rise of the output. It can be seen that at 16 min, the output reaches 3 log reductions (99.9%) sterilization with our hybrid WUVH model. Moreover, 4 log reductions (99.99 %), 5 log (99.999 %), and 6 log (99.9999 %) reduction with the WUVH model can be achieved within 23, 35 and ∼ 80 minutes respectively, and Maximum sterilization > 5.5 log reductions can be achieved at 52 minutes. It can also be noticed that to reach 3 log reductions other systems such as UVGISA and WMHSA requires a minimum of 19 minutes and 21 minutes respectively. While the standalone systems attain 3 log 10 reductions (UVGISA in ∼19 minutes) and (WMHSA in ∼ 21 minutes), while for 5 log reduction (UVGISA in >80 minutes) and (WMHSA in >80 minutes). The standalone UVGISA and WMHSA had plateaued ∼ 5 log 10 reduction at 80 minutes, and may not reach 6 log 10 reduction. Table 3 provides the relevant simulation parameter based on the model. This states the efficiency of the hybrid system in terms of quickly achieving the maximum target. Considering the biological aspect, the hybrid system may work even better because the hybrid system can launch a dual attack, where WMH destroys the protein and lipid of any virus, whereas UV destroys the genetic material of the virus. Gayan et al, 2013 showed synergistic 6 log reduction of the bacteria E. coli growth by the use of UV-C light and mild temperature.34 Moreover, moist heat is considered more effective than dry heat in killing microorganisms.35
Fig 3.
Graph depicting: (A) Average log reduction after the treatment with respect to time is replicated; (B) Energy emitted from the source is calculated.
Table 3.
Simulation parameters
| Simulation environment | Specification/value |
|---|---|
| Warm heat chamber | 1 |
| UV chamber | 1 |
| Moist heat | 65-70oC |
| UVC spec | 17 mW/cm2 at dose ∼1 J/cm2 |
| Mask placement | Centre |
There is no standard level of antiviral disinfection recommended for N95 respirators. FDA defines high-level disinfection for a short contact time to achieve a 6 log 10 (means 99.9999 %) reduction of an appropriate Mycobacterium species.36 Rutala et al have shown that disinfectants demonstrating a 3 log 10 (99.9 %) reduction on carriers are likely to be clinically effective on some surfaces.37 Considering the infectious nature of SARS-CoV-2, a minimum of >5 log 10 is considered safe. Oral et al used vapor H2O2 for 3 hours to reach 6 log 10 reductions of SARS-CoV-2.38 Battelle has launched a vapour hydrogen peroxide system that's FDA approved showed a 6 log 10 reduction in 3 hours with an extra 5 hours off-gassing time. Thus, our hybrid model with the combined effect of WMH and UV together can bring more efficiency and reliability to the decontamination process.
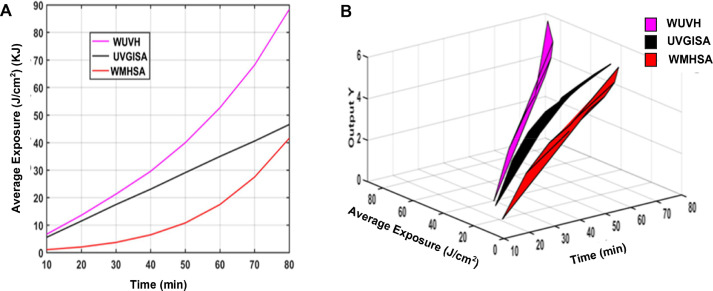
In the second set of experiments, energy, and average exposure/ cm2 emitted from the source is calculated. The energy emitted from the source is shown in Figure 3B. The energy due to UV is calculated using joules law of heating, whereby calculating kilowatt-hour the conversion of equivalent energy is estimated. The energy due to warm heat in a chamber is calculated using Clausius-clapayron relation.39 The calculated pressure with time from the stated relation is used to evaluate the energy of the warm heat chamber. The energy of the WUVH system is due to the combination of both UV and warm heat. It can be seen from Figure 3B that the average energy emitted by WUVH is much more than the other 2 systems. For example, at around 20 min WUVH emits 4.1 kJ whereas UVGISA and WMHSA emit 3.5 kJ and 0.63 kJ respectively. This justifies the efficacy of our system in terms of energy. Moreover, energy has a direct relation in terms of enhancement of average exposure per unit area. This average exposure40 is an important parameter in determining the actual emissive energy received by the target material during the decontamination process. Figure 4 represents the average exposure and is presented by plotting 2 plots. In the first plot (Fig 4A), average exposure is compared with the time and in the second plot (Fig 4B), a 3D plot is used to accommodate average exposure along with the output (average log reduction) with time. Considering the area of the masks under treatment, the average exposure per unit area is calculated for all the systems WUVH, UVGISA, and WMHSA. It is to be noticed from Figure 4A with time the average exposure is increased for all the processes. However, it is the highest in our proposed WUVH system. For example, in around 20 min, the average exposure/cm2 of WUVH is 13.6 J/cm2 while for UVGISA and WMHSA system, it is 11.5 J/cm2 and 2.05 J/cm2. These sets of results are validated using a 3D plot where it can be noticed that in a given time slot the average exposure is related with the performance of the system in terms of getting appreciable output. For example, in a steady state, within a time slot of 20 min the average exposure of 13.6 J/cm2 for the WUVH system provides an output of 3.5 log reduction. UVGISA and WMHSA system for an average exposure of 11.5 J/cm2 and 2.05 J/cm2 produces 3.1 and 2.7 average log reduction. This suggests that the more energy emitted by the source, the better will be the average exposure, which will result in speeding up the decontamination process. The results show that in the WUVH system, the state of 3 log reduction is reached in much less time with enhanced exposure as compared with other schemes. Moreover, 5 log reduction for WUVH is achieved at an exposure of 25.3 J/cm2 within 36 minutes and greater than 5-log reduction (5.5 log reduction) in 52 minutes with an average exposure of 41.2 J/cm2. Other systems such as UVGISA and WMHSA will reach a maximum of 5 log reductions at 80 minutes with an exposure of 46.6 J/cm2 and 41.6 J/cm2 respectively. This validates the enhances efficacy of our WUVH system as compared to the standalone.
Fig 4.
Graphs depicting: (A) Average exposure as a function of time. (B) 3D plot representing average exposure with log reduction and time.
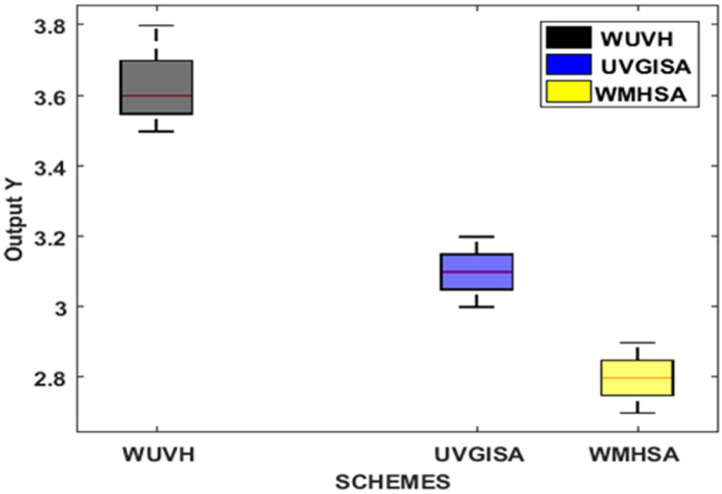
As the masks are subjected to an average exposure as already shown and described through Figure 4, the amount of increased exposure will produce stress (tensile or compressive) in the mask. This may reduce the functionality of the mask with a shrink in its reuse ratio.41 , 42 The relation between subjected stress and an appreciable output is described through the third set of experiments. Stress is calculated as the force per unit area. The force inducted on the mask is a property of energy and is calculated as energy per unit meter. Over a timespan, as the exposure is increased, the stress is also bound to be increased. A stress plot and a 3D plot of stress along with output representation are depicted in Figure 5 . Although Figure 4 and Figure 5 are structurally alike their functionality in terms of operation and description are different. It can be seen from Figure 5A that considering a time slot of 20 minutes, the stress attained by the mask under WUVH is 0.139 MPa, while for UVGISA and WMHSA, it is 0.117 MPa and 0.021 MPa. These values are suitably placed in a 3D plot (Figure 5B) to justify the role of stress along with output. It can be seen that in 20 minutes time WUVH system reaches 3.5 log reductions with the stress of 0.139 MPa. It is to be noted that this WUVH is a faster system where the standard 3 log reductions are achieved at 16 minutes under comparative less stress of 0.080MPa. Moreover, WUVH system also reaches 5 log reduction at a stress of 0.242 MPa in 36 minutes and greater than 5 log reduction at a stress of 0.422 MPa in about 52 minutes respectively. The other systems will reach the 3 log reductions at a minimum of 4 to 5 minutes later. Moreover, it can also be noticed that WUVH will reach 4 log reductions ensuring 99.99% decontamination in just 23 minutes with the stress of 0.14 MPa. The same output will be achieved by UVGISA at a 30-minute time with the stress of 0.18 MPa while WMSA requires 32 minutes with the stress of 0.040. However, to reach 5 log reduction UVGISA and WMHSA requires a stress of 0.49 MPa and 0.426 MPa at 80 minutes. This suggests that both UVGISA and WMSA are slower systems with more stress required to achieve the maximum. A detailed discussion with other comparison is shown through Table 4 to be discussed later in Section 4.3.
Fig 5.
Graphs depicting: (A) Stress as an important parameter with time. (B) 3D plot emphasizing the role of stress along with output.
Table 4.
Exhaustive analyses
| Process | Time required for log reduction (min) | Average exposure J/cm2 |
Stress N/m2 | Reuse | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Min | Max | ||||||||||
| WUVH | 16 | 23 | 36 | 52 | 6.7 | 88.4 | 0.080 | 0.3 | 187 | 50 | 36 |
| UVGISA | 19 | 30 | 80 | —- | 5.6 | 46.6 | 0.117 | 0.49 | 128 | 30 | — |
| WMHSA | 21 | 32 | 80 | —- | 1.08 | 41.6 | 0.022 | 0.42 | 681 | 36 | — |
Statistical analysis
Statistical analysis is done to validate the simulation results (Fig 6 ). This is done by using box plots with a varying number of runs. Although the WUVH process reaches 99.9% accuracy in terms of 3 log reduction in 16 minutes as a standard to accommodate and compare all the schemes, the simulation is carried on with a varying number of runs up to 20 minutes. It can be seen from the plot that the mean of WUVH is at 3.6 in 20 minutes duration with a maximum and minimum range variation from 3.7 to 3.5. Similarly, UVGISA and WMHSA also have a mean value of 3.1 and 2.8 for 20 minutes. These values are very much consistent with the plots of Figure 3A. Thus, the precision and accuracy of our scheme are justified with this box plot for the same set of parameters.
Fig 6.
Statistical analysis using box plot with number of runs.
Exhaustive analysis
An exhaustive data analysis is presented in Table 4. It is noticed from the table that the WUVH process requires the least time among all other processes to reach a standard reduction required for the decontamination of the masks. Moreover, the average exposure is also more in the case of WUVH than other processes.14 This enhanced exposure makes the WUVH system fast by reducing the time to perform decontamination. Stress is a function of exposure but if the target is achieved in lesser time, then stress for the same exposure will also reduce. This is because a targeted mask will be subjected to a lesser duration to achieve the target. To achieve 3 log reductions, it can be noticed that although in WUVH, the exposure is more than UVGISA, the tendency of WUVH to reach the target value in lesser time results in less stress. In this case, WMHSA overrides in terms of stress as exposure at this level is quite less. However, as the process proceeds towards better decontamination levels such as 5 log reductions, due to the inherent characteristics of WUVH, it requires very little time to reach the target. In such a scenario, WUVH has the least stress value compared with other schemes to achieve the target reduction.
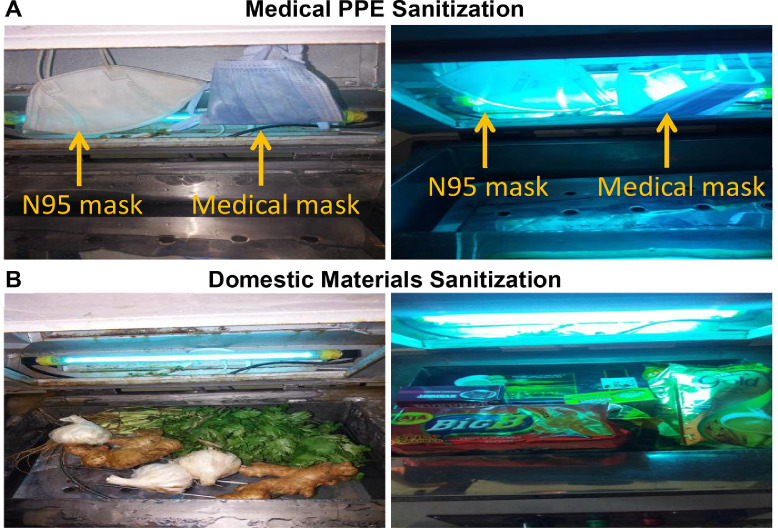
The material of the mask is made of Polypropylene having a maximum yield strength of 43 MPa with a tensile strength of 34 MPa, compressive strength 46.5MPa and Fatigue of 24 MPa. The nylon straps have a strength of 45 MPa. Now, considering the factors of filtration resistance and penetration in terms of mask property degradation during the decontamination process, the average strength of the mask can be considered as 15 MPa under the worst-case scenario. The reuse of the mask can be calculated by knowing the stress value to achieve a particular level of decontamination. For example, from Table 4, it is observed that for WUVH, the mask can be reused 50 times if 5 log reduction is to be achieved every time. This value is more than the competing schemes such as UVGISA and WMHSA. Similarly, for >5 log reduction, only mask under WUVH can be reused as other systems will not progress to that level of decontamination. This establishes the success of WUVH as despite having larger exposure, the stress level is always maintained at an appreciable level resulting in a good reuse ratio. Finally, the WUVH setup is designed and fabricated as shown in Figure 7 . Figure 8 is showing the sanitization process of medical PPE and domestic material using the WUVH-based instrument.
Fig 7.
Instrument design and components. (A) Warm ultraviolet Hybrid model (WUVH) is a hybrid of 2 components Ultraviolet Germicidal Irradiation Standalone (UVGISA) and the Warm Moist Heat Standalone (WMHSA). Front view of the WUVH. (B) Side view of the WUVH. (C) Masks and PPE can be put in autoclavable bags for WMHSA/ WUVH systems. (D) Top view of WMHSA unit without the metal mesh. (E) Top view of WMHSA unit with the metal mesh. (F) Inverted view of the UVGISA unit.
Figure 8.
Sanitization of materials using the warm ultra violet hybrid model-based Instrument. (A) Medical PPE sanitization. (B) Domestic materials sanitization.
Moreover, this hybrid system can be used as standalone systems also. The key benefit of this model is that it can be utilized for other domestic and personal sanitization purpose also. This sanitization process is specifically intended for medical masks decontamination and reuse purposes but can also be applied against any other viruses. A model is fabricated and its results are verified by mathematical analysis and simulation. The results show the supremacy of the proposed model in terms of its speed of sanitization and reuse. comprising of moist steam and UV radiation.
Conclusion and future directions
We have developed a hybrid disinfection model (WUVH) that concomitantly uses UV-C irradiation and heat for effective decontamination. Another feature of this model is that it can be customized to work in 3 modes, such as standalone warm heat, standalone UV or hybrid model. The analysis is supported by creating a mathematical model and by actual fabrication of the model. Simulated results show that the minimum accuracy of 3 log 10 (99.9%) reductions can be achieved within 16 minutes, while >5.5 log 10 reduction is reached in 52 minutes, far quicker than the standalone systems. As per our WUVH model, around 6 log 10 reduction may be reached in 80 minutes but not feasible with the other models. The average exposure is found to be more when compared with other schemes but on the contrary, the stress at the same level of exposure is quite less. The reduced decontamination time increases the reuse ratio of the mask under consideration. The advantage of this process is that the speed of sanitization in achieving efficiency is increased and both the membrane and DNA structure of the virus is damaged. Recent work by Cadnum et al, 2020 suggests that UV-C in a 30-minute cycle reduced contamination but did not meet the disinfection 6 log 10 reductions in 30 minutes. Similar data was also observed with dry heat at 70°C for 30 minutes. The authors suggest that wet heat may be more effective than dry heat, especially when disinfecting an N95 respirator.43 Our data is quite similar to that reported by Cadnum et al, 2020.
Our proposed hybrid model that relies on the concomitant use of heat and UV-irradiation can overcome the limitations of the existing single-arm based decontamination system both physically as well as biologically. Various reports suggest that synergistic effect can work better on bacteria.34 Yang et al, 2019 reported synergistic antimicrobial effect by the use of heat treatment and Lauric Arginate and also with Lauric Arginate and UVA (DOI 10.1128/AEM.01033-19). A dual attack on the viral envelope (heat inactivates viral protein and lipid), while UV causes damage to the genetic material. This aspect can make our proposed hybrid model even more efficacious while tested in vitro. Different brands of respirators and the straps are differentially susceptible to UV and/or high heat. Our model provides options to titrate the different agents accordingly for respective companies. We are in the process of evaluating the in vitro efficacy of our system. To reduce the warm up time and create a better coverage of the disinfecting area we have also integrate UV LED lights with controlled timer system in our model and needs further analysis. Dry heat can also be integrated in place of the moist heat system for certain PPE types. For extreme systems we can also use 30% H2O2 in the WMHSA unit to make a hybrid of UV and wet H2O2 vapor-based sanitation.
Application wise this hybrid model may be used for medical, industrial, domestic and personal sanitization purposes. Moreover, this model is not only restricted to SARS-CoV-2 (coronavirus) but can be used to treat any type of virus/ bacteria. Although the fabricated model is tested as a future extension of this work, the machine will be tested with the real random virus, and analysis to that respect will be made.
Acknowledgments
M.P. acknowledges Dr. Steven Dubinett and Dr. Brigitte Gomperts from UCLA for providing constant support and mentoring. R.B. acknowledges Dr. Sipra Das Bit of IIEST, Shibpur, Dr. Pijush Pal Roy, Dr. N. N. Pathak, Dr. C. K. Ghosh, and Mrs. Ruma Mitra of Dr. B. C. Roy Engineering College, India, for providing continuous support. R.B. acknowledges Dr. Susanta Dutta for helpful discussion.
Footnotes
Author contribution: M.P. and R.B. conceived of the presented idea, developed the theory, planned and designed the instrument, supervised the project, wrote and corrected the manuscript. R.B. and P.R. performed the computations and verified the analytical methods. M.P. and S.D. drew the 3D model diagram.
References
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paules CI, Marston HD, Fauci AS. Coronavirus infections-more than just the common cold. JAMA. 2020;323:707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 4.Singh Y, Gupta G, Satija S, Pabreja K, Chellappan DK, Dua K. COVID-19 transmission through host cell directed network of GPCR. Drug Dev Res.2020;81:647-649. [DOI] [PMC free article] [PubMed]
- 5.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu J, Liao X, Qian S, et al. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. 2020;26:1320–1323. doi: 10.3201/eid2606.200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Q, Zhang Y, Wu L, et al. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell. 2020;181:894–904. doi: 10.1016/j.cell.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Setti L, Passarini F, Gennaro GD, et al. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not be enough. Int J Environ Res Public Health. 2020;17:2932. [DOI] [PMC free article] [PubMed]
- 9.Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323:1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lukassen S, Chua RL, Trefzer T, et al. SARS‐CoV‐2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J. 2020;39:1–15. doi: 10.15252/embj.20105114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azap A, Erdinc FS. Medical mask or N95 respirator: when and how to use? Turk J Med Sci. 2020;50:633–637. doi: 10.3906/sag-2004-199. [DOI] [PubMed] [Google Scholar]
- 13.Wang X, Pan Z, Cheng Z. Association between 2019-nCoV transmission and N95 respirator use. J Hosp Infect. 2020;105:104–105. doi: 10.1016/j.jhin.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liao L, Xiao W, Zhao M, et al. Can N95 respirators be reused after disinfection? How many times? ACS Nano. 2020;14:6348–6356. doi: 10.1021/acsnano.0c03597. [DOI] [PubMed] [Google Scholar]
- 15.Kim JM, Chung YS, Jo HJ, et al. Identification of coronavirus isolated from a patient in Korea with COVID-19. Osong Public Health Res Perspect. 2020;11:3–7. doi: 10.24171/j.phrp.2020.11.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsuyama S, Nao N, Shirato K, et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proceed Natl Acad Sci. 2020;117:7001–7003. doi: 10.1073/pnas.2002589117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. StatPearls; Treasure Island (FL): 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) [PubMed] [Google Scholar]
- 18.Balazy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, Grinshpun SA. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control. 2006;34:51–57. doi: 10.1016/j.ajic.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 19.Nogee D, Tomassoni AJ. Covid-19 and the N95 respirator shortage: closing the gap. Infect Control Hosp Epidemiol. 2020;4:958. doi: 10.1017/ice.2020.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lam T-N, Wu C-H, Huang S-H, et al. Multi-scale microstructure investigation for a PM2.5 air-filter efficiency study of non-woven polypropylene. Quantum Beam Science. 2019;3:20. [Google Scholar]
- 22.Heimbuch BK, Kinney K, Lumley AE, Harnish DA, Bergman M, Wander JD. Cleaning of filtering facepiece respirators contaminated with mucin and Staphylococcus aureus. Am J Infect Control. 2014;42:265–270. doi: 10.1016/j.ajic.2013.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kenney P, Chan BK, Kortright K, et al., Hydrogen peroxide vapour sterilization for N95 respirators for reuse [e-pub ahead of print]. medrxiv. 10.1101/2020.03.24.20041087. Accessed August 28, 2020. [DOI]
- 24.Heimbuch BK, Wallace WH, Kinney K, et al. A pandemic influenza preparedness study: use of energetic methods to decontaminate filtering facepiece respirators contaminated with H1N1 aerosols and droplets. Am J Infect Control. 2011;39:e1–e9. doi: 10.1016/j.ajic.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Viscusi DJ, Bergman MS, Novak DA, et al. Impact of three biological decontamination methods on filtering facepiece respirator fit, odor, comfort, and donning ease. J Occup Environ Hyg. 2011;8:426–436. doi: 10.1080/15459624.2011.585927. [DOI] [PubMed] [Google Scholar]
- 26.de Man P, van Straten B, van den Dobbelsteen J, van der Eijk A, Horeman T, Koeleman H. Sterilization of disposable face masks by means of standardized dry and steam sterilization processes; an alternative in the fight against mask shortages due to COVID-19. J Hosp Infect. 2020;105:356–357. doi: 10.1016/j.jhin.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lindsley WG, Martin SB, Jr., Thewlis RE, et al. Effects of ultraviolet germicidal irradiation (UVGI) on N95 respirator filtration performance and structural integrity. J Occup Environ Hyg. 2015;12:509–517. doi: 10.1080/15459624.2015.1018518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WA Rutala, DJ Weber. Disinfection and sterilization: an overview Am J Infect Control. 2013;41:S2–S5. [DOI] [PubMed]
- 29.Rabenau HF, Cinatl J, Morgenstern B, Bauer G, Preiser W, Doerr HW. Stability and inactivation of SARS coronavirus. Med Microbiol Immunol. 2005;194:1–6. doi: 10.1007/s00430-004-0219-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Darnell ME, Subbarao K, Feinstone SM, Taylor DR. Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods. 2004;121:85–91. doi: 10.1016/j.jviromet.2004.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ariza-Mateos A, Prieto-Vega S, Diaz-Toledano R, et al. RNA self-cleavage activated by ultraviolet light-induced oxidation. Nucleic Acids Res. 2012;40:1748–1766. doi: 10.1093/nar/gkr822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Watkins NJ, Nowzari C, Pappas GJ. Robust economic model predictive control of continuous-time epidemic processes. IEEE Transact Automatic Control. 2020;65:1116–1131. [Google Scholar]
- 33.Lee JH. Model predictive control: review of the three decades of development. Int J Control Autom Syst. 2011;9:415–424. [Google Scholar]
- 34.Gayan E, Manas P, Alvarez I, Condon S. Mechanism of the synergistic inactivation of Escherichia coli by UV-C light at mild temperatures. Appl Environ Microbiol. 2013;79:4465–4473. doi: 10.1128/AEM.00623-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pathology for Surgeons in Training, 3Ed. 3rd Edition ed. London: CRC Press
- 36.Prevention CfDCa. Guideline for disinfection and sterilization in healthcare facilities, 2008. Available at: https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines-H.pdf. 2019. Accessed June 10, 2020.
- 37.Rutala WA, Kanamori H, Gergen MF, Sickbert-Bennett EE, Weber DJ. Susceptibility of Candida auris and Candida albicans to 21 germicides used in healthcare facilities. Infect Control Hosp Epidemiol. 2019;40:380–382. doi: 10.1017/ice.2019.1. [DOI] [PubMed] [Google Scholar]
- 38.Oral E, Wannomae KK, Connolly RL, et al. Vapour H2O2 sterilization as a decontamination method for the reuse of N95 respirators in the COVID-19 emergency [e-pub ahead of print]. medRxiv. 10.1101/2020.04.11.20062026. Accessed August 28, 2020. [DOI]
- 39.Koutsoyiannis D. Clausius–Clapeyron equation and saturation vapour pressure: simple theory reconciled with practice. Eur J Phys. 2012;33:295–305. [Google Scholar]
- 40.Lindsley WG, Martin SB, Thewlis RE, et al. Effects of ultraviolet germicidal irradiation (UVGI) on N95 respirator filtration performance and structural integrity. J Occup Environ Hyg. 2015;12:509–517. doi: 10.1080/15459624.2015.1018518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin TH, Chen CC, Huang SH, Kuo CW, Lai CY, Lin WY. Filter quality of electret masks in filtering 14.6-594 nm aerosol particles: effects of five decontamination methods. PLoS One. 2017;12 doi: 10.1371/journal.pone.0186217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rottach DR, Lei Z. Stockpiled N95 filtering facepiece respirator polyisoprene strap performance. J Int Soc Respir Prot. 2017;34:69–80. [PMC free article] [PubMed] [Google Scholar]
- 43.Cadnum JL, Li D, Redmond SN, John AR, Pearlmutter B, Donskey C. Effectiveness of ultraviolet-C light and a high-level disinfection cabinet for decontamination of N95 respirators. Pathog Immun. 2020;5:52–67. doi: 10.20411/pai.v5i1.372. [DOI] [PMC free article] [PubMed] [Google Scholar]