Abstract
Rising emissions of greenhouse gases in the atmosphere have warmed the planet substantially and are also accompanied by poor air quality. The increased prevalence of allergic airway disease worldwide can be partially attributed to those global environmental changes. Climate change and air pollution pose adverse impacts on respiratory allergies, and that the mechanisms are complex and interactive. Adverse weather conditions, such as extreme temperatures, can act directly on the respiratory tract to induce allergic respiratory illnesses. Thunderstorms and floods can alter the production and distribution of aeroallergens while wildfires and dust storms increase air pollution, and therefore indirectly enhance health risks. Concentrations of particulate matter and ozone in the air have been projected to increase with climate warming and air stagnation, and the rising temperatures and CO2 increase pollen, molds, and spores, which escalate the risk of allergic respiratory diseases. The synergistic effects of extreme heat and aeroallergens intensify the toxic effect of air pollutants, which in turn augment the allergenicity of aeroallergens. With the Earth's climate change, migration of humans and plants shift the living environments and allergens of susceptible people. Urban residents are exposed to multiple factors while children are sensitive to environmental exposure. Since climate change may pose many unexpected and persistent effects on allergic respiratory diseases, health professionals should advocate for effective mitigation and adaptation strategies to minimize its respiratory health effects.
Keywords: Respiratory allergy, Climate change, Air pollution, Extreme weather events, Aeroallergen
Introduction
Allergic respiratory diseases are common chronic conditions caused by immune system disorders; asthma, rhinitis, and hay fever are the most common. Indoor and outdoor allergens, tobacco smoke, air pollution, cold air, and even rapid urbanization are considered environmental risk factors for these diseases.[1] Respiratory allergies can occur in both high and low-income countries. More than 272 million people currently suffer from asthma and millions have allergic rhinitis. In China, it is estimated that the overall prevalence of asthma for those over 20 years old was 4.2%,[2] with the southeastern regions having a higher prevalence than northwestern regions.[3] Worldwide, asthma prevalence has been rising over the past decades, increasing by 19.3% from 2007 to 2017, compared to 8.0% from 1997 to 2007.[4]
It is suggested that the global asthma prevalence increase may have been an early signal of anthropogenic climate change.[5] Air pollution and climate change are potential drivers for the increased prevalence of respiratory allergy because of the body's immune response to temperature, allergens, and other environmental factors.[6] The Intergovernmental Panel on Climate Change has concluded that warming of the climate is unequivocal, attributed to the growing emission of greenhouse gases (GHGs). Increases in warm temperatures, heavy precipitation events, and high sea levels have been observed since the last century.[7] These changes result in more intense and frequent heat waves, storms, floods, wildfires, and dust storms. In addition, enhanced GHG emissions, atmospheric stagnations, and more frequent heat waves are likely to increase the risk of severe air pollution events by modifying the generation, dispersion, and elimination of air pollutants.[8] Climate change is also anticipated to affect the production and release of allergenic pollens and warmer winter may increase mite growth and spore formation.[9] These elevated factors have quantifiable negative impacts on the morbidity and mortality of allergic respiratory diseases, especially asthma.
The relationships among climate change, air pollution, aeroallergens, and allergic respiratory diseases are very complex and elusive [Figure 1]. Previous literature on this topic, however, has only explained the individual effect of ambient temperature, air pollution, mold, or pollen on the morbidity and prevalence of allergic respiratory diseases. A more holistic review accounting of how climate change and other environmental factors related to allergic respiratory diseases may help to understand the underlying mechanisms of airway disease and inform better prevention strategies. In this paper, we attempt to draw a comprehensive picture of the interactions between meteorological factors, aeroallergens, air pollution, and allergic respiratory diseases in the context of global climate change.
Figure 1.
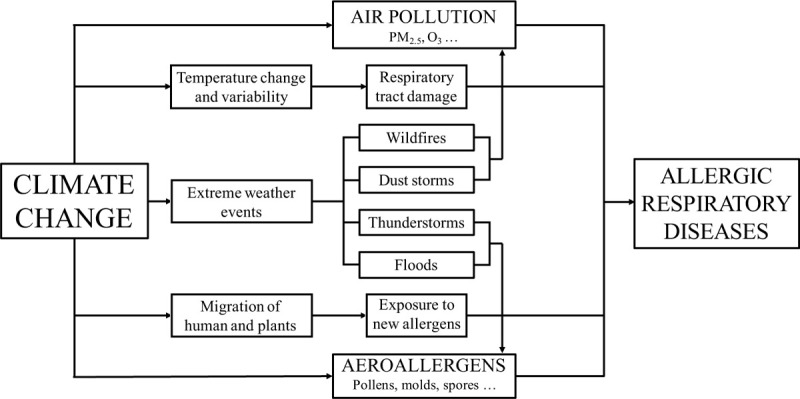
Comprehensive pathways of climate change, air pollution, aeroallergens, and allergic respiratory diseases. PM2.5: Particulate matter with an aerodynamic diameter less than or equal to 2.5 μm.
Climate Change
The global mean temperature is projected to rise over the 21st century under all assessed GHG emission scenarios and will cause long-lasting changes in the pattern of precipitation and increases in extreme weather events.[10] Projected climate change is expected to strengthen the burden of a variety of climate-sensitive health outcomes,[11] including critical respiratory diseases. Even if anthropogenic emissions are stopped now, many aspects of climate change and associated impacts will continue for many decades.[7]
Temperature extremes and variation
Extreme heat can increase airway resistance rapidly and trigger asthma symptoms by stimulating thermosensitive bronchopulmonary C-fiber nerves.[12] A study in Kentucky, USA, demonstrated a 112% increase in airway resistance after hyperventilation of warmed air vs. a 38% increase after hyperventilation of room temperature air in patients with asthma.[13] High temperature may cause an increased number of hospitalizations and emergency department visits of asthma. A time-series study in Hong Kong, China, showed that relative risk for asthma hospitalizations increased when the daily mean temperature rose over 27°C in the hot season.[14] Another study in Brisbane, Australia, found the hot temperature was associated with increases in emergency department visits for childhood asthma and the effect appeared to be acute.[15]
Although the global average temperature is increasing, climate change may also lead to occasional cold extremes.[7] Cold temperature can induce bronchial hyper-reactivity, contraction of the tracheal smooth muscle and decrease of the pulmonary circulation and lung perfusion.[16] A study of women athletes in Canada found that exercise in cold air was associated with an increased prevalence of airway hyper-responsiveness and bronchoconstriction, which is the main characteristic of asthma.[17] Other studies have shown the effects of cold air on asthma, such as increased asthma admissions in Hong Kong, China[14] and pediatric outpatient visits for asthma in Shanghai, China[18] during the cold season. Cold weather increased respiratory symptoms among patients with asthma and allergic rhinitis in Finland.[19]
Temperature variation also increases the risk of asthma and the aggravation of asthmatic symptoms.[20] Qiu et al[21] found that an increase of 1°C in diurnal temperature range was correlated with a 2.5% increase in daily emergency asthma hospitalizations in Hong Kong, China, and the effect was greater in the cold season than in the warm season. A rise in temperature variation between neighboring days increased hospital visits for childhood asthma in Hefei, China,[22] possibly related to more outdoor activity when the weather became warmer and more exposure to more pollen and mold spores. However, a meta-analysis reported that temperature drop had a stronger association than temperature rise in asthma risk.[23]
The increasing use of air conditioners because of the heat waves has become a new risk factor for allergic respiratory diseases. When people entering an air-conditioned room, the sudden drop in temperature, even as small as 2 to 3°C without a gradual adaptation may have negative consequences on the respiratory system. Cold air hyperpnea quickly provokes bronchoconstriction in asthmatic subjects.[24] Besides, reduced ventilation in closed environments may cause an increased concentration of air pollutants and infectious agents, which can potentiate the pathogenic activity of the cold and dry air.[25]
Extreme weather events
Thunderstorms
Thunderstorms have become more intense and frequent over most mid-latitude land masses and wet tropical regions as global temperature increases.[7] Many locations around the world have witnessed asthma outbreaks following thunderstorms; the term “thunderstorm asthma” has been used to describe this phenomenon.[26] One of the first observations of thunderstorm asthma was at the East Birmingham Hospital in the UK in 1983.[27] Since then, asthma outbreaks during thunderstorms had been reported in many countries, including Australia,[28] USA,[29] Italy,[30] and Iran.[31]
A close temporal association can be observed between the arrival of a thunderstorm and the onset of asthma epidemics. Thien et al[32] described a catastrophic epidemic of thunderstorm asthma crossing Melbourne Australia in 2016, with ten deaths and about 9000 persons hospitalized, an unprecedented scale of intensity in comparison with previous events. Within 30 h, there were 3365 excess respiratory-related emergency presentations, 476 excess asthma-related hospital admissions, and 35 patients admitted to the intensive care unit. A telephone questionnaire found that susceptibility factors for severe thunderstorm asthma were pre-existing asthma, pollen sensitization, allergic rhinitis, and outdoor location during the storm.[33]
Epidemiological evidence has shown that thunderstorm asthma is limited to pollen seasons. The causal link between thunderstorm asthma and pollen exposure has been supported by consistent epidemiological evidence, and temporal and dose-response relationships, but experimental data and specificity criterion are still limited.[34] It is assumed that storms can concentrate pollen grains at ground level and provoke the release of allergenic particles in respirable size after their absorption of water[35] and rupture by osmotic shock. Thus, high atmospheric concentrations of inhalable allergen-carrying fine particles can easily penetrate the lower respiratory tract and cause an inflammatory response.[36] This hypothesis was supported in a work that showed that in a condition of higher humidity, more allergens are available in ambient air.[37] Thunderstorms co-expose individuals to high electric charges, heavy rainfall, outflows, increases of humidity, and drops in temperature; the impact of these factors on pollens remains unclear or inconsistent.[28,29,38]
Floods
The frequency and intensity of floods are projected to increase under climate change scenarios resulting from rising sea levels and extreme precipitation events.[7] Increased levels of microbes and mold growth in houses as well as mold spores in the atmosphere are usually observed following a severe flood. A study from the USA showed that floods following a hurricane may contribute to increased concentrations of atmospheric fungal spores.[39] Increased moisture levels and consequent enhanced fungal growth in flooded houses have been also shown in the months following hurricanes.[40–42]
Compared to pollens, molds have been less studied but are also associated with increased severity of allergic respiratory diseases. Several studies among children and adults have revealed that increases in atmospheric fungal spore counts were linked to significant increases in asthma admissions and emergency department visits.[43] Moreover, respiratory allergies have been associated with exposure to fungal contamination in homes. A meta-analysis of 33 epidemiological studies showed an increase of 30% to 50% in respiratory diseases in occupants of the home with dampness and mold exposure.[44] However, since few studies have evaluated the effect of flooding on mold spores and then respiratory symptoms, the evidence is insufficient to evaluate the magnitude of the health effect.
Wildfires
Wildfires have increased in number and magnitude over the past decades and this trend will continue in response to further climate warming.[45] Wildfire smoke contains a variety of chemical components, generating various pollutants including particulate matter (PM), ozone (O3), and organic compounds. Current evidence consistently demonstrates that respiratory symptoms, particularly those related to asthma, are associated with exposure to wildfire smoke.[46,47] An analysis in rural North Carolina showed a significant increase of 65% in emergency department visits for asthma during the peat bog wildfire in 2008.[48]
Monitoring stations and satellite information are used to assess exposure to PM with an aerodynamic diameter less than or equal to 2.5 μm (PM2.5) from wildfires in recent years, but there are still difficulties in distinguishing wildfire emissions from other sources of air pollution and estimating personal exposure to wildfire emission. Recent studies have statistically “blended” data from multiple sources, such as ground monitors, satellites, land-use models, atmospheric models, and meteorology.[49] Although most of the evidence of wildfire and asthma focused on PM2.5, a recent study found that effect estimates of O3 during a wildfire in California in 2008 were significant for emergency department visits for asthma and suggested that the combined effect of O3 and PM2.5 during wildfires should be investigated in the future.[50]
Dust storms
More dust storms can be anticipated as a result of increasing drought and desertification. Although coarse particles of dust storms have been thought to be less toxic than fine particles, they have a stronger effect in inducing inflammatory mediators that play essential roles in allergic attacks.[51] Sand particles carry a vast number of allergens on their surface or within their matrix, ranging from dust mites, pollen, gaseous and mineral contaminants, to fungal spores,[52] which enhance allergic reactions within atopic asthmatics. Emergency presentations of asthma in dust storm areas were higher than non-dust storm areas in the 2009 dust storm in Sydney, Australia.[53]
Areas with a high occurrence of dust storms, like Middle Eastern countries, have a larger burden of respiratory allergies. A survey questionnaire involving 1000 asthmatic patients in five Gulf Cooperation Council countries revealed that the dust storms posed persistent adverse effects on the psychosocial and productive life of patients.[54] Children with immature immune systems are most vulnerable to dust storm exposure. In Kuwait, an age-stratified time-series analysis of dust storms and asthma admissions found that the children 0 to 14 years old were the only group with a significant risk.[55]
Climate-driven human and plants migration
Rising sea levels and water degradation resulting from climate change can contribute to human migration, which affects health. Migration involves exposure to a different set of allergens as well as changes in socio-economic background, housing conditions, diet, indoor and outdoor contamination, all of which may increase the possibility of developing atopic diseases.[56] A study of the Melbourne epidemic thunderstorm asthma event in 2016 found that 39% of the emergency department visits and that six out of the ten patients who died were of Asian ethnicity.[32] Hew et al observed that odds ratio for asthmatic hospitalization in the same event was 0.6 in Asian patients born overseas but 5.4 in those born locally possibly because of the earlier age when immigrated and longer time of immigration.[33]
With global warming, migrations also involve plants moving to regions where such species did not exist previously, posing new challenges in the future. Maps of the U.S. Department of Agriculture showed that plant hardiness zones have moved northward from 1960 to 2018.[57] The changing patterns of plant habitat suggest that sensitive individuals may be exposed to new plant types and new aeroallergens, which could aggravate respiratory symptoms and potentially concomitant anaphylaxis. A study in New Zealand argued that vegetation diversity had a protective effect on childhood asthma, but it also showed that exotic types were associated with an increase in asthma risk and would attenuate the protective effect of vegetation diversity.[58] The effect of plant migrations on allergic respiratory diseases remains controversial and needs to be understood better.
Air Pollution
Concentrations of PM and secondary pollutants (eg, O3) in the air have been projected to increase with climate warming and changing patterns of atmospheric circulation.[59] It is well documented that both PM and O3 are linked to allergic respiratory diseases.[60]
Altered patterns of air pollution in a changing climate
Climate change acts to enhance the severity and frequency of air pollution episodes and thereby indirectly affects allergic respiratory diseases.[61] Global changes to atmospheric circulation will increase air stagnation, which weakens the transport and diffusion of air pollutants and enhances pollution haze.[62] Elevated temperatures and solar irradiation enhance photochemical reactions to generate O3 at ground level.[63] Wildfires and dust storms increase natural emissions of PM while rising energy demands to adapt to extreme heat and cold for cooling or heating increase anthropogenic emissions.[43] The representative concentration pathway 4.5, a GHG modeling trajectory based on global CO2 reaching a peak around 2040, predicts that conditions such as atmospheric stagnation and heat waves will contribute 68% to the climate-driven increase in PM2.5 and 14% to O3 in China.[8]
Those excess PM and O3 could induce epidemics of asthma and exacerbations of asthmatic symptoms. Exposure to high levels of O3 had a negative effect on lung function, with increased airway inflammation and hyper-reactivity to bronchoconstrictor agents.[64] A time-stratified case-crossover study showed that ambient O3 exposure caused excess risks for emergency department visits for asthma in California.[65] Diesel exhaust contains fine (PM2.5) and ultrafine particles (PM0.1) that strongly stimulate oxidation and inflammation in the airways[66]. A large study conducted in 5443 Korean children, aged 6 to 14 years, in ten cities in 2005 to 2006 revealed that residential distance to traffic-related pollutants had an inverse association with increased risk of asthma and allergic sensitization.[67]
Interaction effect of extreme heat and air pollution
The respiratory health effect of air pollution not only depends on the concentrations and components of the pollutants but also on climatic factors. It is well established that extreme heat and air pollution act synergistically to exacerbate physiologic dysfunction and respiratory symptoms in patients suffering from chronic lung disease.[68] Fluid loss, disrupting pulmonary perfusion, increasing ventilation and lung volumes in heat exposure may worsen the respiratory health effect of air pollutants, and decrease the threshold for bronchoconstriction.[69] In a study by McCormack et al, heat stress in combination with air pollutants showed a positive interaction resulting in worsening breathlessness.[70] This synergy causes excess mortality and hospital admissions for respiratory conditions.[71] Malig et al[65] reported that the association between short-term O3 exposures and emergency department visits for asthma was larger and more consistent during the warm season.
Aeroallergens
The increase in pollen, molds, and spores occurring in many countries as climate change will result in a greater likelihood of asthma development.[9] Those aeroallergens in combination with exposure to air pollutants act synergistically to intensify the allergic response [Figure 2].
Figure 2.
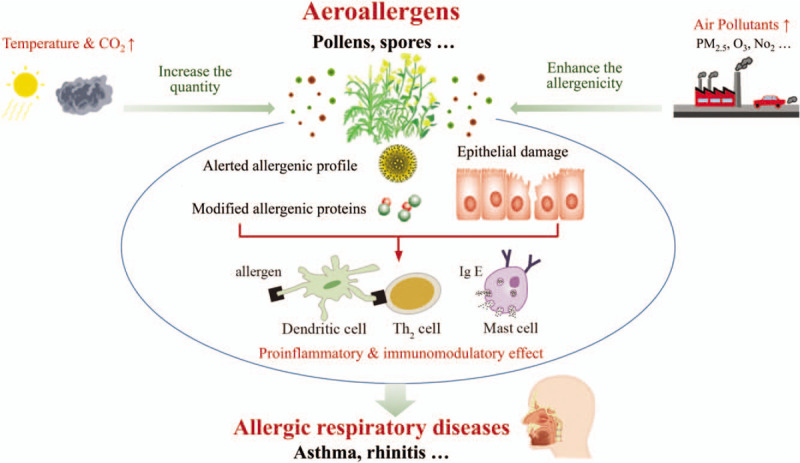
The mechanism by which aeroallergens increase risk of allergic respiratory diseases.
Intensive pollen season and greater aeroallergens
Increased temperature and CO2 levels have been shown to affect the onset and duration of pollen season as well as the concentration of aeroallergens including spores. Pollen seasons have increased in duration in North America in association with increased temperatures and lengthening frost-free periods.[72] Experimental data show that doubling of CO2 increased ragweed plant pollen production by 30% to 90% because of enhanced photosynthesis and reproductive effects.[73] Elevated CO2 levels and temperatures appear to increase the major allergenic peptide content in ragweed pollen and thus increase its allergenicity.[74]
Enhanced allergenicity due to increasing air pollutant emission
With the advancement of global urbanization and warming, increasing emissions and longer stagnation of air pollutants may generate more pollens with increased allergenicity.[75] By attaching to the surface of plant-derived particles, air pollutants could alter their allergenic profiles and modify their immune-modulatory potential.[76] Beck and associates found that high levels of O3 enhanced allergenicity of birch pollen in susceptible individuals.[77] Traffic-related air pollution increases allergenicity of ragweed pollen compared to pollen sampled in areas with less traffic-related air pollution.[43] Also, air pollutants, particularly O3, PM, and diesel exhaust, have been shown to increase the permeability of allergens in the respiratory mucous membranes and strengthen the allergen-induced inflammatory effect on airways.[6] It has been speculated that air pollutants make allergic-atopic patients more susceptible to the antigen they are already sensitized.[76] Carlsten et al[78] observed that inhalation of diesel exhaust augmented allergen-induced inflammation in the lower airways of atopic individuals.
Vulnerable Groups
The risk factors of asthma include genetics and external triggers. People who have asthma or have a family history of asthma are more likely to be susceptible to environmental insults. However, urban residents and children are among the groups most vulnerable to climate change.
Urban residents
City dwellers have a greater risk of allergic respiratory diseases because of synergistic exposures of air pollutants, high temperature, and allergens. Keet et al[79] reported that urban residence was independently associated with increased risk of asthma-related emergency department visits and hospitalizations in the US. Migration from rural regions to urban centers is accompanied by increased prevalence rates of asthma.[43] The increased use of fossil fuels in cities contributes to the World Health Organization (WHO) statistic that over 90% of the urban population of the world breathe air that exceeds WHO's air quality guidelines.[80] The urban population will likely be disproportionately affected because of the urban heat island effect since excess heat causes direct impairment on airway and increase the formation of O3.[81] A study from Southern Spain showed that the pollen season in urban areas was twice as long as that of rural environments.[82]
Children
Children have higher asthma prevalence than adults and are more sensitive to environmental exposures. During the critical phase of lung development, exposure of the airway epithelium to environmental insults may lead to persistent and life-long changes in lung structure and metabolism.[83,84] A birth cohort study reported that exposure to allergens in the first 3 years of life impaired lung function at school age and affected the development of asthma in adulthood.[85] Prenatal and perinatal exposure to air pollutants has been linked to increase respiratory symptoms and the risk of developing childhood asthma.[86] Both heat exposure and air pollution to pregnant women are associated with pre-term birth[87–90]; younger gestational age and prematurity are risk factors for the incidence of pre-school wheezing and asthma.[91]
A Call to Action for Health Professionals
Climate change is the largest crisis the human civilization has faced in its modern history.[92] Mediated through a variety of pathways, climate change interacts with and affects air pollution and aeroallergens, having serious consequences for allergic respiratory diseases. There is an urgent need to transform our societies to achieve 45% reduced emissions of GHGs by 2030 and near-zero-emissions by 2050 to limit warming to below 1.5°C relative to pre-industrial levels.[10] Health professionals should communicate with policymakers to advocate for GHG mitigation as well as air pollution and allergen reduction.[93] They should also consider clinical interventions to minimize climate change-related risk in allergic respiratory diseases.[94,95]
Reducing atmospheric allergens
Reduction of air pollutants and allergens exposure should be considered into public approaches and urban planning to avoid synergy effect and protect urban residents. For air pollution, simple buffer zones of 200 to 300 m should be applied between high-traffic areas and spaces for residents to work, learn, and live, which can remarkably decrease those toxic exposures. For aeroallergens, the “Allergy Safe Tree Decalogue” model carried out some simple solutions, including non-allergenic plants in public and private green areas, pruning hedges before flowering or pollen emission, consulting maps of pollen levels before planning public events.[81] This project has been evaluated and showed a significant reduction of pollen in the atmosphere and a decrease in hospital admissions due to respiratory crises.[96]
Building climate-resilient health systems
Consistent monitoring and early warning systems of weather-related events should be part of the health information systems. With this information, health departments can mitigate air pollution and aeroallergen health effects. For instance, pollen allergic individuals should be alerted to the risk of being outdoors during thunderstorms in the pollen season. Identifying and addressing individuals with risk factors combined with tailored prescriptions would help patients better adapt real-world multiple exposures of heatwaves, pollutants, and pollens.[68]
Conclusions
This review draws a comprehensive picture of the direct and indirect impact of climate change on allergic respiratory diseases and illustrates the synergistic effects of heat, air pollution, and aeroallergens that cause excess mortality and hospital admissions for allergic respiratory diseases. Health professionals should play an important role in promoting effective strategies to cope with the health effect of global environmental changes, undertaking research on climate change and respiratory health and applying the methods to diseases prevention and control.
Acknowledgement
The authors thank Prof. Dean E. Schraufnagel (University of Illinois, USA) for his generous effort in editing this manuscript and assembling the special issue.
Funding
This work was supported by the grant from the National Key Research and Development Program of China (No. 2018YFA0606200).
Conflicts of interest
None.
Footnotes
How to cite this article: Deng SZ, Jalaludin BB, Antó JM, Hess JJ, Huang CR. Climate change, air pollution, and allergic respiratory diseases: a call to action for health professionals. Chin Med J 2020;133:1552–1560. doi: 10.1097/CM9.0000000000000861
References
- 1. Bousquet J. Global Surveillance, Prevention and Control of Chronic Respiratory Diseases: A Comprehensive Approach. Kaltaev N, ed. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 2.Huang K, Yang T, Xu J, Yang L, Zhao J, Zhang X, et al. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet 2019; 394:407–418. doi: 10.1016/s0140-6736(19)31147-x. [DOI] [PubMed] [Google Scholar]
- 3.Guo X, Li Z, Ling W, Long J, Su C, Li J, et al. Epidemiology of childhood asthma in mainland China (1988-2014): a meta-analysis. Allergy Asthma Proc 2018; 39:15–29. doi: 10.2500/aap.2018.39.4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392:1789–1858. doi: 10.1016/s0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beggs PJ, Bambrick HJ. Is the global rise of asthma an early impact of anthropogenic climate change? Environ Health Perspect 2005; 113:915–919. doi: 10.1289/ehp.7724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reinmuth-Selzle K, Kampf CJ, Lucas K, Lang-Yona N, Frohlich-Nowoisky J, Shiraiwa M, et al. Air pollution and climate change effects on allergies in the anthropocene: abundance, interaction, and modification of allergens and adjuvants. Environ Sci Technol 2017; 51:4119–4141. doi: 10.1021/acs.est.6b04908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Climate Change 2014: Synthesis Report. Pachauri RK and Meyer LA, eds. Geneva, Switzerland: IPCC; 2014. [Google Scholar]
- 8.Hong C, Zhang Q, Zhang Y, Davis SJ, Tong D, Zheng Y, et al. Impacts of climate change on future air quality and human health in China. Proc Natl Acad Sci U S A 2019; 116:17193–17200. doi: 10.1073/pnas.1812881116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergmann KC. Weather conditions and climate change have an effect on allergies. Allergo J 2016; 25:33–39. doi: 10.1007/s40629-016-0119-z. [Google Scholar]
- 10.IPCC Special Report: Global Warming of 1.5°C: Summary for Policymakers. Geneva:World Meteorological Organization; 2018. [Google Scholar]
- 11.Haines A, Ebi K. The imperative for climate action to protect health. N Engl J Med 2019; 380:263–273. doi: 10.1056/NEJMra1807873. [DOI] [PubMed] [Google Scholar]
- 12.Li S, Baker PJ, Jalaludin BB, Marks GB, Denison LS, Williams GM. Ambient temperature and lung function in children with asthma in Australia. Eur Respir J 2014; 43:1059–1066. doi: 10.1183/09031936.00079313. [DOI] [PubMed] [Google Scholar]
- 13.Hayes D, Jr, Collins PB, Khosravi M, Lin RL, Lee LY. Bronchoconstriction triggered by breathing hot humid air in patients with asthma: role of cholinergic reflex. Am J Respir Crit Care Med 2012; 185:1190–1196. doi: 10.1164/rccm.201201-0088OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lam HCY, Li AM, Chan EYY, Goggins WB. The short-term association between asthma hospitalisations, ambient temperature, other meteorological factors and air pollutants in Hong Kong: a time-series study. Thorax 2016; 71:1097–1109. doi: 10.1136/thoraxjnl-2015-208054. [DOI] [PubMed] [Google Scholar]
- 15.Xu Z, Huang C, Hu W, Turner LR, Su H, Tong S. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occup Environ Med 2013; 70:730–735. doi: 10.1136/oemed-2013-101538. [DOI] [PubMed] [Google Scholar]
- 16.Cruz AA, Togias A. Upper airways reactions to cold air. Curr Allergy Asthma Rep 2008; 8:111–117. doi: 10.1007/s11882-008-0020-z. [DOI] [PubMed] [Google Scholar]
- 17.Kennedy MD, Faulhaber M. Respiratory function and symptoms post cold air exercise in female high and low ventilation sport athletes. Allergy Asthma Immunol Res 2018; 10:43–51. doi: 10.4168/aair.2018.10.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo Y, Jiang F, Peng L, Zhang J, Geng F, Xu J, et al. The association between cold spells and pediatric outpatient visits for asthma in Shanghai, China. PLoS One 2012; 7:e42232.doi: 10.1371/journal.pone.0042232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hyrkas-Palmu H, Ikaheimo TM, Laatikainen T, Jousilahti P, Jaakkola MS, Jaakkola JJK. Cold weather increases respiratory symptoms and functional disability especially among patients with asthma and allergic rhinitis. Sci Rep 2018; 8:10131.doi: 10.1038/s41598-018-28466-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim J, Lim Y, Kim H. Outdoor temperature changes and emergency department visits for asthma in Seoul, Korea: a time-series study. Environ Res 2014; 135:15–20. doi: 10.1016/j.envres.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 21.Qiu H, Yu IT, Tse LA, Chan EY, Wong TW, Tian L. Greater temperature variation within a day associated with increased emergency hospital admissions for asthma. Sci Total Environ 2015; 505:508–513. doi: 10.1016/j.scitotenv.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Li K, Ni H, Yang Z, Wang Y, Ding S, Wen L, et al. Effects of temperature variation between neighbouring days on daily hospital visits for childhood asthma: a time-series analysis. Public Health 2016; 136:133–140. doi: 10.1016/j.puhe.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Cong X, Xu X, Zhang Y, Wang Q, Xu L, Huo X. Temperature drop and the risk of asthma: a systematic review and meta-analysis. Environ Sci Pollut Res Int 2017; 24:22535–22546. doi: 10.1007/s11356-017-9914-4. [DOI] [PubMed] [Google Scholar]
- 24.Koskela HO. Cold air-provoked respiratory symptoms: the mechanisms and management. Int J Circumpolar Health 2007; 66:91–100. doi: 10.3402/ijch.v66i2.18237. [DOI] [PubMed] [Google Scholar]
- 25.D’Amato M, Molino A, Calabrese G, Cecchi L, Annesi-Maesano I, D’Amato G. The impact of cold on the respiratory tract and its consequences to respiratory health. Clin Transl Allergy 2018; 8:20.doi: 10.1186/s13601-018-0208-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.D’Amato G, Annesi-Maesano I, Vaghi A, Cecchi L, D’Amato M. How do storms affect asthma? Curr Allergy Asthma Rep 2018; 18:24.doi: 10.1007/s11882-018-0775-9. [DOI] [PubMed] [Google Scholar]
- 27.Packe GE, Ayres JG. Asthma outbreak during a thunderstorm. Lancet 1985; 2:199–204. doi: 10.1016/s0140-6736(85)91510-7. [DOI] [PubMed] [Google Scholar]
- 28.Marks GB, Colquhoun JR, Girgis ST, Koski MH, Treloar ABA, Hansen P, et al. Thunderstorm outflows preceding epidemics of asthma during spring and summer. Thorax 2001; 56:468–471. doi: 10.1136/thorax.56.6.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grundstein A, Sarnat SE, Klein M, Shepherd M, Naeher L, Mote T, et al. Thunderstorm associated asthma in Atlanta, Georgia. Thorax 2008; 63:659–660. doi: 10.1136/thx.2007.092882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Losappio L, Heffler E, Contento F, Cannito C, Rolla G. Thunderstorm-related asthma epidemic owing to Olea Europaea pollen sensitization. Allergy 2011; 66:1510–1511. doi: 10.1111/j.1398-9995.2011.02699.x. [DOI] [PubMed] [Google Scholar]
- 31.Forouzan A, Masoumi K, Haddadzadeh Shoushtari M, Idani E, Tirandaz F, Feli M, et al. An overview of thunderstorm-associated asthma outbreak in southwest of Iran. J Environ Public Health 2014; 2014:504017.doi: 10.1155/2014/504017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thien F, Beggs PJ, Csutoros D, Darvall J, Hew M, Davies JM, et al. The Melbourne epidemic thunderstorm asthma event 2016: an investigation of environmental triggers, effect on health services, and patient risk factors. Lancet Planet Health 2018; 2:e255–e263. doi: 10.1016/s2542-5196(18)30120-7. [DOI] [PubMed] [Google Scholar]
- 33.Hew M, Lee J, Susanto NH, Prasad S, Bardin PG, Barnes S, et al. The 2016 Melbourne thunderstorm asthma epidemic: risk factors for severe attacks requiring hospital admission. Allergy 2019; 74:122–130. doi: 10.1111/all.13609. [DOI] [PubMed] [Google Scholar]
- 34.D’Amato G, Vitale C, D’Amato M, Cecchi L, Liccardi G, Molino A, et al. Thunderstorm-related asthma: what happens and why. Clin Exp Allergy 2016; 46:390–396. doi: 10.1111/cea.12709. [DOI] [PubMed] [Google Scholar]
- 35.Suphioglu C, Singh MB, Taylor P, Bellomo R, Holmes P, Puy R, et al. Mechanism of grass-pollen-induced asthma. Lancet 1992; 339:569–572. doi: 10.1016/0140-6736(92)90864-y. [DOI] [PubMed] [Google Scholar]
- 36.Cockcroft DW. Epidemic thunderstorm asthma. Lancet Planet Health 2018; 2:e236–e237. doi: 10.1016/s2542-5196(18)30123-2. [DOI] [PubMed] [Google Scholar]
- 37.Buters J, Prank M, Sofiev M, Pusch G, Albertini R, Annesi-Maesano I, et al. Variation of the group 5 grass pollen allergen content of airborne pollen in relation to geographic location and time in season. J Allergy Clin Immunol 2015; 136:87–95.e6. doi: 10.1016/j.jaci.2015.01.049. [DOI] [PubMed] [Google Scholar]
- 38.Antó JM, Sunyer J. Thunderstorms: a risk factor for asthma attacks. Thorax 1997; 52:669–670. doi: 10.1136/thx.52.8.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freye HB, King J, Litwin CM. Variations of pollen and mold concentrations in 1998 during the strong El Nino event of 1997-1998 and their impact on clinical exacerbations of allergic rhinitis, asthma and sinusitis. Allergy Asthma Proc 2001; 22:239–247. [PubMed] [Google Scholar]
- 40.Solomon GM, Hjelmroos-Koski M, Rotkin-Ellman M, Hammond SK. Airborne mold and endotoxin concentrations in New Orleans, Louisiana, after flooding, October through November 2005. Environ Health Perspect 2006; 114:1381–1386. doi: 10.1289/ehp.9198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schwab KJ, Gibson KE, Williams DL, Kulbicki KM, Lo CP, Mihalic JN, et al. Microbial and chemical assessment of regions within New Orleans, LA impacted by Hurricane Katrina. Environ Sci Technol 2007; 41:2401–2406. doi: 10.1021/es062916x. [DOI] [PubMed] [Google Scholar]
- 42.Riggs MA, Rao CY, Brown CM, Van Sickle D, Cummings KJ, Dunn KH, et al. Resident cleanup activities, characteristics of flood-damaged homes and airborne microbial concentrations in New Orleans, Louisiana, October 2005. Environ Res 2008; 106:401–409. doi: 10.1016/j.envres.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 43.D’Amato G, Holgate ST, Pawankar R, Ledford DK, Cecchi L, Al-Ahmad M, et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J 2015; 8:25.doi: 10.1186/s40413-015-0073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fisk WJ, Lei-Gomez Q, Mendell MJ. Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air 2007; 17:284–296. doi: 10.1111/j.1600-0668.2007.00475.x. [DOI] [PubMed] [Google Scholar]
- 45.Schoennagel T, Balch JK, Brenkert-Smith H, Dennison PE, Harvey BJ, Krawchuk MA, et al. Adapt to more wildfire in western North American forests as climate changes. Proc Natl Acad Sci U S A 2017; 114:4582–4590. doi: 10.1073/pnas.1617464114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reid CE, Jerrett M, Tager IB, Petersen ML, Mann JK, Balmes JR. Differential respiratory health effects from the 2008 northern California wildfires: a spatiotemporal approach. Environ Res 2016; 150:227–235. doi: 10.1016/j.envres.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 47.Hutchinson JA, Vargo J, Milet M, French NHF, Billmire M, Johnson J, et al. The San Diego 2007 wildfires and Medi-Cal emergency department presentations, inpatient hospitalizations, and outpatient visits: an observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med 2018; 15:e1002601.doi: 10.1371/journal.pmed.1002601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rappold AG, Stone SL, Cascio WE, Neas LM, Kilaru VJ, Carraway MS, et al. Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ Health Perspect 2011; 119:1415–1420. doi: 10.1289/ehp.1003206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reid CE, Maestas MM. Wildfire smoke exposure under climate change: impact on respiratory health of affected communities. Curr Opin Pulm Med 2019; 25:179–187. doi: 10.1097/MCP.0000000000000552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reid CE, Considine EM, Watson GL, Telesca D, Pfister GG, Jerrett M. Associations between respiratory health and ozone and fine particulate matter during a wildfire event. Environ Int 2019; 129:291–298. doi: 10.1016/j.envint.2019.04.033. [DOI] [PubMed] [Google Scholar]
- 51.Baldasano J, Valera E, Jimenez P. Air quality data from large cities. Sci Total Environ 2003; 307:141–165. doi: 10.1016/s0048-9697(02)00537-5. [DOI] [PubMed] [Google Scholar]
- 52.Shabankarehfard E, Ostovar A, Farrokhi S, Naeimi B, Zaeri S, Nazmara S, et al. Air- and dust-borne fungi in indoor and outdoor home of allergic patients in a dust-storm-affected area. Immunol Invest 2017; 46:577–589. doi: 10.1080/08820139.2017.1322102. [DOI] [PubMed] [Google Scholar]
- 53.Merrifield A, Schindeler S, Jalaludin B, Smith W. Health effects of the September 2009 dust storm in Sydney, Australia: did emergency department visits and hospital admissions increase? Environ Health 2013; 12:32.doi: 10.1186/1476-069X-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khadadah M, Mahboub B, Al-Busaidi NH, Sliman N, Soriano JB, Bahous J. Asthma insights and reality in the Gulf and the near East. Int J Tuberc Lung Dis 2009; 13:1015–1022. [PubMed] [Google Scholar]
- 55.Thalib L, Al-Taiar A. Dust storms and the risk of asthma admissions to hospitals in Kuwait. Sci Total Environ 2012; 433:347–351. doi: 10.1016/j.scitotenv.2012.06.082. [DOI] [PubMed] [Google Scholar]
- 56.D’Amato G, Rottem M, Dahl R, Blaiss M, Ridolo E, Cecchi L, et al. Climate change, migration, and allergic respiratory diseases: an update for the allergist. World Allergy Organ J 2011; 4:120–125. doi: 10.1097/WOX.0b013e3182260a57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barnes CS. Impact of climate change on pollen and respiratory disease. Curr Allergy Asthma Rep 2018; 18:59.doi: 10.1007/s11882-018-0813-7. [DOI] [PubMed] [Google Scholar]
- 58.Donovan GH, Gatziolis D, Longley I, Douwes J. Vegetation diversity protects against childhood asthma: results from a large New Zealand birth cohort. Nat Plants 2018; 4:358–364. doi: 10.1038/s41477-018-0151-8. [DOI] [PubMed] [Google Scholar]
- 59.Madaniyazi L, Guo Y, Yu W, Tong S. Projecting future air pollution-related mortality under a changing climate: progress, uncertainties and research needs. Environ Int 2015; 75:21–32. doi: 10.1016/j.envint.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 60.Faizan MA, Thakur R. Measuring the impact of household energy consumption on respiratory diseases in India. Glob Health Res Policy 2019; 4:10.doi: 10.1186/s41256-019-0101-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.D’Amato G, Vitale C, Lanza M, Molino A, D’Amato M. Climate change, air pollution, and allergic respiratory diseases: an update. Curr Opin Allergy Clin Immunol 2016; 16:434–440. doi: 10.1097/ACI.0000000000000301. [DOI] [PubMed] [Google Scholar]
- 62.Horton DE, Skinner CB, Singh D, Diffenbaugh NS. Occurrence and persistence of future atmospheric stagnation events. Nat Clim Chang 2014; 4:698–703. doi: 10.1038/nclimate2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Demain JG. Climate change and the impact on respiratory and allergic disease: 2018. Curr Allergy Asthma Rep 2018; 18:22.doi: 10.1007/s11882-018-0777-7. [DOI] [PubMed] [Google Scholar]
- 64.D’Amato G, Pawankar R, Vitale C, Lanza M, Molino A, Stanziola A, et al. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res 2016; 8:391–395. doi: 10.4168/aair.2016.8.5.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Malig BJ, Pearson DL, Chang YB, Broadwin R, Basu R, Green RS, et al. A time-stratified case-crossover study of ambient ozone exposure and emergency department visits for specific respiratory diagnoses in California (2005-2008). Environ Health Perspect 2016; 124:745–753. doi: 10.1289/ehp.1409495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhao Y-X, Zhang H-R, Yang X-N, Zhang Y-H, Feng S, Yu F-X, et al. Fine particulate matter-induced exacerbation of allergic asthma via activation of T-cell immunoglobulin and mucin domain 1. Chin Med J 2018; 131:2461–2473. doi: 10.4103/0366-6999.243551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jung DY, Leem JH, Kim HC, Kim JH, Hwang SS, Lee JY, et al. Effect of traffic-related air pollution on allergic disease: results of the children's health and environmental research. Allergy Asthma Immunol Res 2015; 7:359–366. doi: 10.4168/aair.2015.7.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carlsten C. Synergistic environmental exposures and the airways capturing complexity in humans: an underappreciated world of complex exposures. Chest 2018; 154:918–924. doi: 10.1016/j.chest.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 69.Witt C, Schubert AJ, Jehn M, Holzgreve A, Liebers U, Endlicher W, et al. The effects of climate change on patients with chronic lung disease. A systematic literature review. Dtsch Arztebl Int 2015; 112:878–883. doi: 10.3238/arztebl.2015.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McCormack MC, Belli AJ, Waugh D, Matsui EC, Peng RD, Williams DL, et al. Respiratory effects of indoor heat and the interaction with air pollution in chronic obstructive pulmonary disease. Ann Am Thorac Soc 2016; 13:2125–2131. doi: 10.1513/AnnalsATS.201605-329OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bernstein AS, Rice MB. Lungs in a warming world: climate change and respiratory health. Chest 2013; 143:1455–1459. doi: 10.1378/chest.12-2384. [DOI] [PubMed] [Google Scholar]
- 72.Ziska L, Knowlton K, Rogers C, Dalan D, Tierney N, Elder MA, et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci U S A 2011; 108:4248–4251. doi: 10.1073/pnas.1014107108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rogers CA, Wayne PM, Macklin EA, Muilenberg ML, Wagner CJ, Epstein PR, et al. Interaction of the onset of spring and elevated atmospheric CO2 on ragweed (Ambrosia artemisiifolia L.) pollen production. Environ Health Perspect 2006; 114:865–869. doi: 10.1289/ehp.8549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Singer BD, Straka JG, Ziska LH, Frenz DA, Gebhard DE. Increasing Amb a 1 content in common ragweed (Ambrosia artemisiifolia) pollen as a function of rising atmospheric CO2 concentration. Functional Plant Biol 2005; 32:667–670. doi: 10.1071/FP05039. [DOI] [PubMed] [Google Scholar]
- 75.Aina R, Asero R, Ghiani A, Marconi G, Albertini E, Citterio S. Exposure to cadmium-contaminated soils increases allergenicity of Poa annua L. pollen. Allergy 2010; 65:1313–1321. doi: 10.1111/j.1398-9995.2010.02364.x. [DOI] [PubMed] [Google Scholar]
- 76.D’Amato M, Cecchi L, Annesi-Maesano I, D’Amato G. News on climate change, air pollution, and allergic triggers of asthma. J Investig Allergol Clin Immunol 2018; 28:91–97. doi: 10.18176/jiaci.0228. [DOI] [PubMed] [Google Scholar]
- 77.Beck I, Jochner S, Gilles S, McIntyre M, Buters JT, Schmidt-Weber C, et al. High environmental ozone levels lead to enhanced allergenicity of birch pollen. PLoS One 2013; 8:e80147.doi: 10.1371/journal.pone.0080147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Carlsten C, Blomberg A, Pui M, Sandstrom T, Wong SW, Alexis N, et al. Diesel exhaust augments allergen-induced lower airway inflammation in allergic individuals: a controlled human exposure study. Thorax 2016; 71:35–44. doi: 10.1136/thoraxjnl-2015-207399. [DOI] [PubMed] [Google Scholar]
- 79.Keet CA, Matsui EC, McCormack MC, Peng RD. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol 2017; 140:822–827. doi: 10.1016/j.jaci.2017.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. World Health Organization, COP24 Special report: Health & Climate Change. Geneva, Switzerland: World Health Organization; 2018. [Google Scholar]
- 81.Patella V, Florio G, Magliacane D, Giuliano A, Crivellaro MA, Di Bartolomeo D, et al. Urban air pollution and climate change: “The Decalogue: Allergy Safe Tree” for allergic and respiratory diseases care. Clin Mol Allergy 2018; 16:20.doi: 10.1186/s12948-018-0098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hernandez-Ceballos MA, Garcia-Mozo H, Galan C. Cluster analysis of intradiurnal holm oak pollen cycles at peri-urban and rural sampling sites in southwestern Spain. Int J Biometeorol 2015; 59:971–982. doi: 10.1007/s00484-014-0910-9. [DOI] [PubMed] [Google Scholar]
- 83.Carraro S, Scheltema N, Bont L, Baraldi E. Early-life origins of chronic respiratory diseases: understanding and promoting healthy ageing. Eur Respir J 2014; 44:1682–1696. doi: 10.1183/09031936.00084114. [DOI] [PubMed] [Google Scholar]
- 84.Spann K, Snape N, Baturcam E, Fantino E. The impact of early-life exposure to air-borne environmental insults on the function of the airway epithelium in asthma. Ann Global Health 2016; 82:28–40. doi: 10.1016/j.aogh.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 85.Illi S, von Mutius E, Lau S, Niggemann B, Grüber C, Wahn U. Perennial allergen sensitisation early in life and chronic asthma in children: a birth cohort study. Lancet 2006; 368:763–770. doi: 10.1016/s0140-6736(06)69286-6. [DOI] [PubMed] [Google Scholar]
- 86.Korten I, Ramsey K, Latzin P. Air pollution during pregnancy and lung development in the child. Paediatr Respir Rev 2017; 21:38–46. doi: 10.1016/j.prrv.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 87.Kuehn L, McCormick S. Heat exposure and maternal health in the face of climate change. Int J Environ Res Public Health 2017; 14:E853.doi: 10.3390/ijerph14080853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang Q, Benmarhnia T, Zhang H, Knibbs LD, Sheridan P, Li C, et al. Identifying windows of susceptibility for maternal exposure to ambient air pollution and preterm birth. Environ Int 2018; 121:317–324. doi: 10.1016/j.envint.2018.09.021. [DOI] [PubMed] [Google Scholar]
- 89.Kim JJ, Axelrad DA, Dockins C. Preterm birth and economic benefits of reduced maternal exposure to fine particulate matter. Environ Res 2019; 170:178–186. doi: 10.1016/j.envres.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang Q, Benmarhnia T, Li C, Knibbs LD, Bao J, Ren M, et al. Seasonal analyses of the association between prenatal ambient air pollution exposure and birth weight for gestational age in Guangzhou, China. Sci Total Environ 2019; 649:526–534. doi: 10.1016/j.scitotenv.2018.08.303. [DOI] [PubMed] [Google Scholar]
- 91.Sonnenschein-van der Voort AM, Arends LR, de Jongste JC, Annesi-Maesano I, Arshad SH, Barros H, et al. Preterm birth, infant weight gain, and childhood asthma risk: a meta-analysis of 147,000 European children. J Allergy Clin Immunol 2014; 133:1317–1329. doi: 10.1016/j.jaci.2013.12.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhong S, Huang C. Climate change and human health: risks and responses. Chin Sci Bull Chin 2019; 64:2002–2010. doi: 10.1360/N972018-00898. [Google Scholar]
- 93.Zeng YQ, Au DH, Cai S, Carey E, Jiang F, Chen Y, et al. Effect of a patient education intervention on asthma control and patient-doctor relationship. Chin Med J 2018; 131:1110–1112. doi: 10.4103/0366-6999.230736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yang L, Liao W, Liu C, Zhang N, Zhong S, Huang C. Associations between knowledge of the causes and perceived impacts of climate change: a cross-sectional survey of medical, public health and nursing students in universities in China. Int J Environ Res Public Health 2018; 15:E2650.doi: 10.3390/ijerph15122650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liao W, Yang L, Zhong S, Hess JJ, Wang Q, Bao J, et al. Preparing the next generation of health professionals to tackle climate change: are China's medical students ready? Environ Res 2019; 168:270–277. doi: 10.1016/j.envres.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 96.Patella V, Florio G, Magliacane D, Giuliano A, Russo LF, D’Amato V, et al. Public prevention plans to manage climate change and respiratory allergic diseases. innovative models used in Campania region (Italy): the twinning aria implementation and the allergy safe tree decalogue. Transl Med UniSa 2019; 19:95–102. [PMC free article] [PubMed] [Google Scholar]


