Abstract
Killing someone directly is never morally right, but sometimes, choosing someone to save and leaving another to die is. The moral philosophy, law, and medical ethics have all wrestled with the problem of distinguishing between saving someone and leaving another to die. While this distinction might seem intuitively straightforward, it becomes far more complex when applied in treating patients of novel Coronavirus Disease pandemic (COVID-19). The World Health Organization reports more than eight million and half cases of infection and more than 450,000 deaths, 26% in USA. However, with the exponential rise in number of COVID-19 victims and the shortage of life-saving ventilators, the pandemic has imposed to health professionals an ethical medical triage decision-making based on the utilitarian theory to maximize total benefits and life expectancy. Moreover, the decision to put restrictions on treatment beneficence is not discretionary, but an indispensable response to the overwhelming impacts of COVID-19 pandemic. The main concern is not whether to underline priorities, but how to do so systematically and ethically, instead of building decisions on individualized institutional aspirations or health professionals’ intuition. The serious glaring disequilibrium, in healthcare market, between supply and demand for scarce medical resources in several developed nations (including the USA, UK, France, Italy, Spain, etc.) imposes a fundamental question: which COVID-19 patient to save when facing scarce resources?
Keywords: COV-19, Ethics, Justice, Moral, Triage decision-making
Résumé
Tuer quelqu’un directement n’est jamais moralement correct, mais parfois, choisir quelqu’un à sauver et en laisser un autre mourir l’est. La philosophie morale, le droit et l’éthique médicale ont tous été confrontés au problème de la distinction entre sauver quelqu’un et en laisser mourir un autre. Si cette distinction peut sembler intuitive, elle devient beaucoup plus complexe lorsqu’elle est appliquée au traitement des patients atteints d’une nouvelle pandémie de maladie à coronavirus (COVID-19). L’Organisation mondiale de la santé signale plus de huit millions et demi de cas d’infection et plus de 450 000 décès, dont 26 % aux États-Unis. Cependant, avec l’augmentation exponentielle du nombre de victimes de COVID-19 et la pénurie de respirateurs vitaux, la pandémie a imposé aux professionnels de la santé une prise de décision éthique de tri médical basée sur la théorie utilitariste pour maximiser les bénéfices totaux et l’espérance de vie. En outre, la décision de restreindre la prise en charge des patients n’est pas discrétionnaire, mais constitue une réponse indispensable aux conséquences considérables de la pandémie de COVID-19. La principale préoccupation n’est pas de savoir s’il faut souligner les priorités, mais comment le faire de manière systématique et éthique, au lieu de fonder les décisions sur des aspirations institutionnelles individualisées ou sur l’intuition des professionnels de la santé. Le grave déséquilibre flagrant, sur le marché des soins de santé, entre l’offre et la demande de ressources médicales rares dans plusieurs pays développés (dont les États-Unis, le Royaume-Uni, la France, l’Italie, l’Espagne, etc.) pose une question fondamentale : quel patient COVID-19 faut-il sauver face à la rareté des ressources ?
Mots clés: COV-19, Éthique, Justice, Morale, Décision de tri
Introduction
In December 2019, a novel virus from the coronavirus family appeared in central China, which quickly took drastic measures of containment and disinfection for nearly 60 million people. However, The COVID-19 pandemic is spreading all over the world and affecting nearly 213 countries1 , causing psychosis and plunging the world into an unprecedented situation [1], [2]. Thenceforth, the pandemic spread worldwide killing more than 450,000 out of 8.5 million confirmed cases till the end of June 2020.
In the beginning the outbreak was concentrated in China where the peak for all cases occurred on February 1, 2020 and then, the epidemiological curve has declined [3]. Currently the pandemic is spreading across the world. The highest confirmed cases and deaths was registered in the USA of 120,721 until now as per the date mentioned above. The maximum number of recovered patients is in USA about 931,310. After the USA, we find Brazil with the second largest number of COVID-19 positive cases (929,149), but Italy has registered the highest case-fatality rate till the end of March 2020 [4]. According to the United Nations, Italy has the second oldest population in the world after Japan. These people are the most vulnerable group to suffer from the novel coronavirus disease once they are infected.
Facing the increasing number of COVID-19 deaths in the world and the scarcity of medical resources especially life-saving ventilators, clinicians in Italy, France, Spain, USA and UK are obliged to make an ethical triage decisions using guidelines [5]. The imposed question in this case is: which COVID-19 patient to save? Elderly or young adult subjects?
Healthcare professionals are confronted by medical and ethical decisions concerning allocation of scarce medical resources, mainly ventilators. Consequently, the principle of “first come, first served” is no longer applied. If there is only one artificial respirator left, assigning it to the first patient brought into respiratory distress, if his chances of benefiting from it are low, would mean an unfair condemnation for all those who could come behind with a less bad life expectancy. Without forgetting, all other patients who are not affected by the pandemic, but the congestion of hospitals would put them in a danger situation.
According to healthcare economists, since medical resources are scarce, it is imperative to rationalize them by targeting treatment to those most in need, as they stand to benefit the most from it [6]. Several useful medical devices become wasteful if used to include low-risk individuals [7]. Rationing the utilization of rare medical resources is inevitable while needs are unlimited and resources are not. Rationalization is necessary because it not only affects individual lives but also reveal the foremost values of the whole society.
This paper will scrutinize ethical principles and approaches for fair medical resource allocation. We examine if the orientation of intensive care units (ICU) to COVID-19 elderly patient who are near the end of life would maximize the overall Quality-Adjusted Life Years (QALYs). To do so, we first focus on ethical ICU bed triage decision to optimize resource allocation during the COVID-19 patients’ treatment.
This paper begins with an overview of statistical considerations about the severity of COVID-19 pandemic in the world. Besides, it examines the concept of medical triage and rationing in times of pandemic. Then discusses specifically both moral and ethical considerations of COVID-19 patient triage regarding principles of justice theories. Finally, we suggest recommendations to consider how to apply ethical principles in triage decision-making in case of scarce medical resources.
Statistical considerations about COVID-19 severity in the World
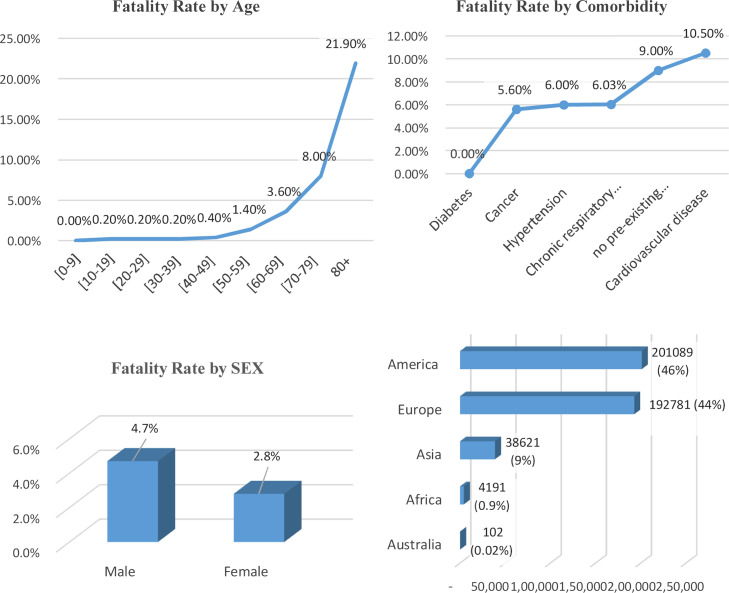
The World Health Organization stated that 1 among 7 COVID-19 patients reported breathing problem with additional severe complications. These patients suffer from both respiratory and other vital systems failure. COVID-19 pandemic can lead to viral pneumonia affecting further extrapulmonary problems with acute respiratory distress syndrome (ARDS), which has a fatality rate fluctuating from 27 to 45% [8]. Moreover, novel coronavirus disease is deadlier for patients with pre-existing health conditions [9]. According to world Health Organization, there are three factors related to fatality include (1) gender especially male patient about 4.7%, (2) old age patient over 80 years around 21.9%, and (3) the presence of comorbidities including diabetes, hypertension (6%), cancer (5.6%), cardiovascular diseases (10.5%), and chronic respiratory diseases (6.03%). Moreover, Chiappelli et al. [10] argued that from pre-existing conditions, the elderly are the most high-risk group of vulnerability to COVID-19 fatality. They argued that noncommunicable diseases (NCDs) affect the older people who are more likely to be at higher risk of severe COVID-19 infection.
Fig. 1 shows summarize all factors (age, sex, comorbidity) associated with fatality and the distribution of total death rate per continent in the wide world.
Figure 1.
COVID-19 Fatality rate by age, sex, comorbidity and by continent. Source: Authors’ analysis of data from WTO.
COVID-19 Taux de mortalité par âge, sexe, comorbidité et par continent.
COVID-19 pandemic has reached nearly all continents [11]. America is deemed as the most affected with COVID-19 in terms of confirmed cases in the world (50.24%) and deaths (46%), followed by the Europe with roughly 30.27% of total confirmed cases all over the world and 44% of fatality, then Asia with 17.55% of total confirmed cases and 9% of the world total fatality. While the very lowest impact of CIVID-19 pandemic is on Australia and Africa, which is respectively about 0.2‱ and 9‰.
At continent-level, the highest death impact in Europe is respectively in United Kingdom (42,153), Italy (34,514), France (29,547), Spain (27,136) and Belgium (9675), at the end of June 2020. While in the Americas the largest number of deaths occurred respectively in USA (120,721), Brazil (45,467), Mexico (6860) and Ecuador (3970).
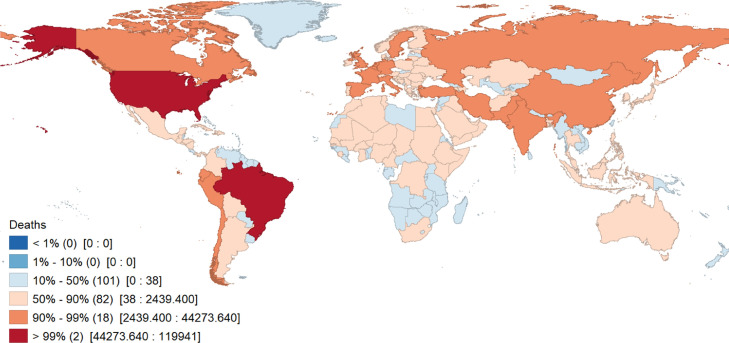
The percentile map of COVID-19 fatalities in the world (Fig. 2 ) summarizes total deaths distribution in all continents (457,267 deaths). Consequently, 50% of infected countries (101) have the lowest total deaths between 0 and 38 fatalities and are in the majority developing countries. While, 18 developed countries have an important range of total fatality between 2439 and 44,273 deaths, there are only two countries, namely USA and Brazil, which have the highest total deaths representing nearly 38% of total fatality in the world.
Figure 2.
Percentile Map of COVID-19 Deaths in the world. Source: Authors’ elaboration using data from WTO (Geoda software output).
Carte des percentiles de décès de COVID-19 dans le monde.
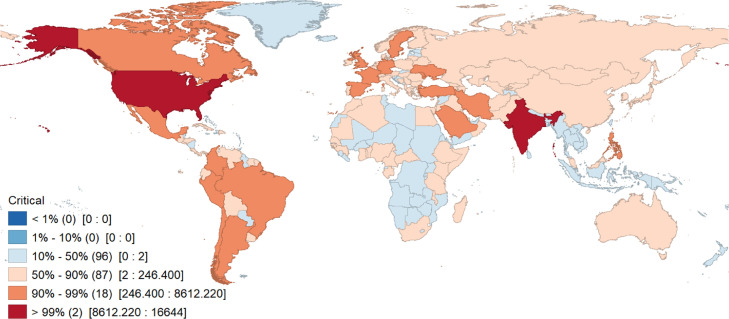
As World Health Organization (WHO) statistics show, the proportion of reported severe and critical COVID-19 cases and those in serious condition such as admitted to ICU is steadily increasing. Statically, the critical case rate was calculated by dividing the number of serious or critical cases by the number of COVID-19 infected cases. Moreover, Liang et al. [12] found, in their study carried on 78 infected countries, that the number of severe and critical cases has a positive effect on COVID-19 fatality rate. They argued that the mean of COVID-19 mortality rate was 3.42% and the mean critical case rate was 2.41%.
At continent-level, the highest critical cases number in America is respectively in USA (16,644), Brazil (8318) and Canada (1982), at the end of June 2020. While the most severe cases in Asia, are registered respectively in India (8944), Iran (2789) and Saudi Arabia (1859), in Europe the number of critical cases, is generally considered as lower than in America or Asia, and has registered respectively in France (772), Spain (617) and Italy (163).
The percentile map of COVID-19 critical cases in the world (Fig. 3 ) shows that total severe and critical cases distribution in all the world is about 54,726. Furthermore, 40% of infected countries (96) have the lower number of severe cases between 0 and 2 patients and are in the majority developing countries. While, 18 developed countries have total serious cases between 246 and 8612, there are only two countries, namely USA and Brazil, which have the highest number of critical cases representing nearly 22% of total severe cases in the world.
Figure 3.
Percentile Map of COVID-19 Critical Cases in the world. Source: Authors’ elaboration using data from WTO (Geoda software output).
Carte des percentiles de cas critiques de COVID-19 dans le monde.
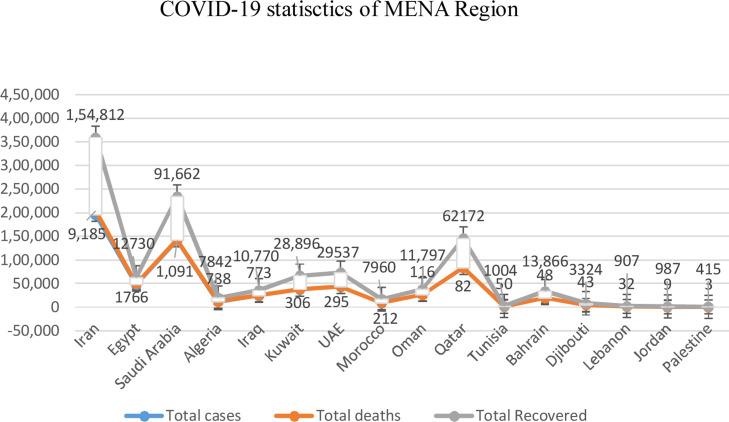
The COVID-19 pandemic has reached and expanded in all countries of the Middle East and North Africa (MENA) region [13], [14]. The first recorded COVID-19 deaths in the MENA region occurred in the Iranian holey city Qom [15]. Rapidly, all cities across Iran was affected [16]. When Tehran does not opt for lockdown on its population in February 2020, this has permitted the spread of the virus into other countries, including Bahrain, Saudi Arabia, Kuwait and Lebanon [17]. At the end of June 2020, the highest total deaths in MENA region was reported respectively in Iran (9185), Egypt (1766) and Saudi Arabia (1091), while the lowest fatalities are registered respectively in Lebanon (32), Jordan (9), and Palestine (3) (Fig. 4 ).
Figure 4.
COVID-19 statistics of MENA Region. Source: Authors’ analysis of data from WTO.
Statistiques COVID-19 de la région Moyen-Orient-Afrique-du-nord.
According to these statistics, it seems that the largest number of infected cases as well as the number of severe and critical patients, needing intensive care triage, exist in high-income countries. Consequently, it seems to be necessary to analyze the practical and ethical issues involved in medical triage and rationing during COVID-19 pandemic.
Medical triage and rationing in COVID-19 pandemic
In their article entitled “Triage in Medicine: Concept, History, and Types”, Kenneth et al. [18] have distinguished between three concepts: “Triage”, “rationing” and “allocation” frequently used in medicine to refer to the distribution and utilization of medical resources to patients. While these three concepts are occasionally used to explain the same reality, there is a strong distinction between them. Firstly, the concept of allocation defines the distribution of all medical facilities, devices and resources disregarding the principle of scarcity. Secondly, the concept of rationing deals with the distribution of medical resources while taking into account the availability and sufficiency of resources to satisfy patients’ needs. Thirdly, the concept of “triage” has a limited scope. It is used in healthcare field to focus on decision-making about distribution and utilization of scarce medical resources.
The use of the triage concept must fulfill three conditions. Firstly, the omnipresence of scarce medical resources. The level of rarity or scarcity can vary significantly. It could be low when a patient coming for care to emergency department (ED) and not served immediately. Scarcity also could be very high, as after COVID-19 pandemic when hundreds of patient coming to hospital and couldn’t be treated owing to the shortage of life-saving ventilators or absence of a bed in the Intensive Care Units (ICU). Consequently, if medical resources are sufficient, there will be no triage, but if these resources are unavailable, triage becomes inevitable. As, Italy is considered the first European country overwhelmed by COVID-19 pandemic, physicians were faced with an ethical triage dilemma as about 10% of COVID-19 patients need respiratory assistance [5].
When dealing with the concept of medical triage the cruel question of selection criteria arises. In fact, the principle of “First come, first served” is not applicable. Thenceforth, the question to be asked is: should we give priority to the oldest or youngest COVID-19 patients? The privilege has to be given to patient having the highest “life expectancy”. Regrettably, owing to the large number of COVID-19 patients necessitating respiratory support, healthcare professionals are facing a decision dilemma at higher occurrence and at a quicker speed. Some criteria are considered as determinant factors for patients’ admission such as age and comorbidities [5]. In 2009, at the peak of the influenza H1N1 pandemic, the Institute of Medicine [19] had developed a national guidance for use by pubic healthcare professionals in order to establish and implement Crisis standards of Care (CSC) that have to be applied in disaster situations under conditions of scarce resources. The IOM's 2009 letter report describes ethical values and rules of justice and responsibility of care.
The need to resort to the rationing in medicine has not usually an ethical justification [6]. Moreover, a justifiable rationing decision in a specific situation, like COVID-19 pandemic, may be unjustifiable in another. This decisional situation imposes the question; which COVID-19 patient to treat/to save? Is it for the economic “value” of the patients? for their “social utility”? for their fragility index? for their age?
To deal with valuable treatments is very important because nearly no treatment in medicine provides certain benefit for a COVID-19 patient and due to a crucial point of divergence is whether the profit have a very high probability to happen in order to justify costs. Furthermore, medical triage is deemed as inevitable. Unavoidably, it is hard to make choices to distribute scarce resources in a way that attains a rational equilibrium across the variety of essential social goods. Consequently, some degree of medical triage is essential for the overall well-being of citizens.
Triage of ICU admission in a COVID-19 pandemic
Medical triage decisions is considered as a regular practice in ICUs [20], [21]. Moreover, ICUs become overwhelmed by COVID-19 patient and critical triage is necessary to prioritize young patients for intensive care in the face of limited number of ICU beds [22], [23], [24], [25], [26]. As a result, it is common to transfer out of an ICU an elderly COVID-19 patient when he receive a small benefit and life expectancy. Regularly doctors in ICUs to optimize their time [27]. They have to decide which COVID-19 patients to treat first and to save. Physicians should change the wants of patients in contradiction of their nonprofessional duties, such as accountabilities to their families. Certainly, doctors cannot provide all probable benefit to each critically COVID-19 patient. Practically, through implicit ICUs triage decisions made by doctors COVID-19 patients are systematically deprived of a potential benefit even if it is small.
The control of the COVID-19 outbreak in societies is hard but remain largely possible [28] and is very important to optimize ICUs capacity. The modelling of intensive care requirements is essential [24], [25]. Many countries suffer from a lack of ICU beds and isolation rooms. In lower-middle-income countries the median of ICU beds was 2–3 beds per 100,000 population, and about 4.6 beds in upper-middle-income countries, while, this median is 12.3 beds in high-income countries [29]. Therefore, both ICU professionals, health administrators and public health policy makers have to plan to rise ICU bed capacity [24], [25], [30]. A significant rise in ICU capacity encompasses rises in beds, respirators, pharmaceuticals, and technicians [23], [31].
In order to maximize the total benefit and life expectancy in a COVID-19 pandemic context, we think that depriving a critical elderly patients from an ICU ventilator to provide it to younger ones in need is ethically justifiable and elderlies must be informed in advance of this option at admission [32], [33], [34]. Certainly, removing ICU ventilators from elderly COVID-19 patients arriving earlier to save younger ones with better prognosis is tremendously psychologically traumatic for health professionals while some of them could possibly refuse to do so [35]. Nevertheless, many rules approve that the decision to remove medical scarce resources to save a patient instead of another is not considered as a killing act and does not necessitate the formal consent of patient [36], [37]. Moreover, distributing ICU scarce resources (beds, ventilators, etc.) in order to maximize the value of total benefits and life expectancy might contribute to decrease the need for removal.
Empiric data related to ICU rationing in COVID-19 pandemic
In USA, the number of COVID-19 patient admitted to the ICU is 960,000 of moderate cases and 3,840,000 of severe cases [35]. Moreover, in the USA, there are almost 62,000 specific ICU ventilators dedicated to treat severe cases of COVID-19 [38] while the average ICU length of stay is about 8 days [39].
ICUs rationing in COVID-19 pandemic showed that approximately more than 10% of patients were rejected intensive care admission in triage decisions due to lack of beds especially in Italy, Spain, Belgium [29], [40], [41]. Moreover, during COVID-19 pandemic with the lack of ICU bed, less patients were admitted for monitoring, which recommends that some patients were deprived of treatment [39]. Some healthcare centers have tried to decrease the usage of ICU by opting for mechanical ventilation installed on the wards [26], [42]. This represents rationing since ICU care is related to lower probability of unfortunate occurrence and fatality rate compared with delivering mechanical ventilation outside of intensive care units. Moreover, the absence of awareness about irrevocability of critical care rationing is problematic, since it proposes that lots of ICU professionals are not well placed to make the hard decisions concerning competing social goods.
Meyfroidt et al. [40] argued that the Belgian Society of Intensive Care Medicine (BSICM), has outlined the different ethical values and rules regarding proportionality of care in the time of COVID-19 pandemic. Consequently, an ethical guideline was proposed for medical triage of COVID-19 patients. The BSICM suggested that every healthcare center have to put its own ethical guidelines during the pandemic, to avoid taking unethical random decisions by healthcare professionals without [40].
Elderly are classified as the most critically COVID-19 patients especially those having comorbidities [27], [43]. Consequently, the inevitability of medical triage does not justify the ethical dimension of rationing, and a reasonable medical rationing decision could not be justifiable in other case.
Ethical values in COVID-19 pandemic
Despite conflicting aspects, each of the moral theories described here addresses the following four components: (1) consideration of abstract moral principles, (2) a systematic portrayal of the fundamentals of ethics, (3) moral principles presented as an interrelated whole, and (4) a coherent, cogent argument in defense of these principles. Among the major approaches to moral theory are: Utilitarianism, Kantianism, Rights Theory, and Communitarianism.
Utilitarianism, found by Bentham [44], also known as consequentialism, implies that all human actions are right or wrong, depending on whether the balance of their consequences are good or bad. Consequently, among multiple courses of action, the right one leads to the best overall outcome in terms of a relevant hierarchy of values. Regarding the assessment of medical triage protocols, Persad et al. [45] recognized four rules used in treating patients equally: (1) first come, first served models; (2) choosing the worst case based on the “rule of recuse”; (3) the utilitarian approach of maximizing total benefits and life expectancy; (4) recompensing social utility that privilege crucial professions but is stressed with latent biases. In the case of COVID-19 pandemic, Ezekiel et al. [35] outlined the ethical values to control the rationing of rare resources. According to the utilitarian approach of maximizing benefits, the supremacy of treatment have to be given to patient having a highest chance of survival. Clinicians must be given preference to develop and recompense usefulness. Consequently, healthcare have not to be provided based on the model of first come, first served but somewhat, arbitrary selection must be done, if all patients have the same prognosis.
In contrast, Kantianism, fundamentally a theory of duty, argues that the rightness of actions depends on features aside from their positive or negative consequences. In this theory, founded by Immanuel Kant and also known as deontological or non-consequentialist, moral obligation is the foundation of moral theory. Through his three works on ethics, Kant's goal was to divorce human knowing from empirical or post-hoc considerations, leaving solely it a priori elements.
A third approach, Rights Theory features the rights of the individual as equally important to that of moral obligation, in that they are vital protections for human life and liberty. In many fields, various professionals hold the protection of such right to be the primary goal of morality. Beauchamp and Childress [46] assert distinct legal and moral rights, in both positive and negative forms. A positive right guarantees that the individual receives something, obligating another to provide it. As a result, a COVID-19 patient have to receive a compulsory treatment from health professionals at any case. A negative right, on the other hand, guarantees one freedom from some eventuality and entails an obligation on the part of others to refrain from causing that thing. In the case of COVID-19 pandemic the clinicians should not denied treatment to an elderly COVID-19 patient.
What ethical values could guide triage of COVID-19 patient?
Methodically triage system distributes the benefits of healthcare among COVID-19 patients. Therefore, triage is considered as a typical issue in the field of distributive justice and ethical theory. The concept of social justice encompasses the field of medicine and healthcare, raising issues that incite controversy over the role of the society, government, and the family of humanity in reducing or eliminating the unequal access to, quality of, and affordability of healthcare. Some go so far as to argue that there is a societal obligation to guarantee universal access, quality, and affordability for all COVID-19 patients. This section of the paper will discuss the concept and principles of justice and distributive justice. The discussion also considers several theories of justice, including Utilitarian theories, Libertarian theories, Communitarian theories, and Egalitarian theories.
Moral Philosophers have attempted to define justice in terms of what is fair to an individual, what that person deserves, or what that person is entitled to expect. The existence of benefits, which COVID-19 patients have coming to them, as well as hardships for which they are owed redress, is a fundamental assumption in society. The existence of these situations creates the need for standards to ensure that justice is afforded to all. Beauchamp & Childress [46] assert that the term distributive justice refers to the fairness, equity, and suitability of distribution determined by societal norms, which in turn derive their justification in the structure social cooperation which holds sway in the given community.
To understand the medial triage of COVID-19 patients, we refer to the two principles of justice: the principle of formal justice and the material principle of justice. Firstly, the principle of formal justice, or principle of formal equality, does not delineate particular circumstances or situations, specifying when patients have to be treated in the same manner; furthermore, it offers no guidelines that can be used to judge whether COVID-19 patients hold status as equals. Secondly, the material principle of justice identifies the substantive properties to be considered in determining distribution.
According to Beauchamp and Childress [46], there are various theories of justice, namely (1) Utilitarian theories, (2) Libertarian theories, (3) Communitarian theories, and (4) Egalitarian theories. The first group of these, utilitarian theories, focus on combining criteria from a variety of sources in order to achieve the greatest form of public utility. This approach considers distributive justice to be one of a number of impediments to attaining a maximum value and insists on placing optimal social welfare near or at the top of the hierarchy of priorities. By contrast, the second category, libertarian theories give first priority to individual rights of social and economic liberty, resulting in the demand that the fairness of procedures take precedence over any assessment of substantive outcomes, paying only limited attention to issues of public utility or to adequately addressing the health needs of the population. Like the libertarian approach, the third group, communitarian theories, base their approach on an agent larger than the individual; however, what distinguishes this group is its reliance on the traditions and practices of a community developed throughout its history. The fourth approach among theories of justice, egalitarian theories, emphasizes equal access to all the benefits of life, both material and intangible, which are universally valued by rational individuals. This approach often highlights material aspects, defining the most important criteria for achieving justice in terms of need and equality. In relation to this paper's discussion of healthcare ethics, egalitarian theories would prioritize the claim that all COVID-19 patients ought to receive an equal distribution of health care, as the latter would be seen as analogous to goods or services [46].
A main obstacle to choose the best approach to healthcare triage is the problem to determine the right principle(s) to be used to make allocation of scarce resources. Several principles contribute to medical triage decision-making, each principle have its own explanation of distributive justice. Beauchamp and Childress [46] suggested the following principles of distributive justice to be used: (1) to every patient an equal share, (2) to everyone in accordance with need, (3) to everyone in accordance with effort, (4) to everyone in accordance with free market conditions, (5) to everyone to maximize total utility. Many scholars have deeply elucidated these principles and their mutual use with other allocation strategies—can be found elsewhere [45], [47].
The main issue of distributive justice, in the COVID-19 pandemic context, is how to pilot the discordance in order to maximize efficiency (decision-making to optimize the use of medical devices excluding low-risk individuals), equity (treating patient similarly), and the approach of justice priority (choosing the worst-off patient). Consequently, we will discuss three principles of distributing scarce medical resources related to the concept of distributive justice: utilitarianism, egalitarianism and prioritarianism.
Maximizing quality-adjusted life years: the utilitarianism approach
The main choice to be made in COVID-19 pandemic is how to distribute equitably scarce medical resources, total benefit and life expectancy between COVID-19 patients. Therefore, both policy makers and public healthcare specialists must outline what mechanisms to use and at what cost. The utilitarianism approach tries to maximize total benefits and life expectancy. There are different approaches to quantifying benefits related to health care. Many healthcare economists refer to the approach of the quality-adjusted life years (QALYs) as a metric to calculate the value of preventing deaths [48]. In fact, QALYs calculates the value of preventing COVID-19 deaths by assessing the cost-viability of clinical medication. The use of QALYs in rationing includes two stages: choosing outcome metrics that adjust life-years for quality, and then distributing so as to maximize QALYs. Moreover, the use of QALYs approach permits effectiveness’ evaluation between diseases and healthcare services that is otherwise hard to compare. For instance, the intensive care unit treatment of COVID-19 patient costs nearly $700 per QALY and the intensive care unit treatment of acute kidney failure costs around $40 per QALY.
Henceforth, many questions have to be asked and answered in the case of heath policy recession due to COVID-19 pandemic especially: What resources could be distributed fairly? What is the predictable gain in QALY? Does it merely extend the unavoidable mortalities or does it decrease them by providing more ICUs ventilators and perhaps new vaccine at the end of 2020?
In their study in the Canadian context, Vaillancourt [49] elucidated the distribution of COVID-19 fatalities and total gained quality-adjusted life years by age group as regard the driven health policy. According to the projected effect of the public intervention plan in Canada, the distribution of COVID-19 fatalities by age and the QALYs related to different age group show that the recession of health policy produces 1850 million QALYs when redistributing health resources intervention.
Commonly, health policies have to opt for optimizing the utilization of the mobilized COVID-19 support resources. From the healthcare economic viewpoint, one must equalize the gain in QALYs of resources distributed among novel coronavirus disease and other ones. Consequently, one should not excessively present scarce medical resources such as ICUs and clinicians to risks to save a few patients in a short period [49]. One should distribute medical resources equitably between different sorts of patients and between different age group. There is no way to evaluate inversely the QALYs related to COVID-19 than those related to other diseases.
Despite limitations of rationing by maximizing QALYs, public uncertainty of general policies including cost strategies has made the usage of QALYs and cost-effectiveness analysis an ethical dilemma [6].
The treatment equity and the egalitarianism approach
In the COVID-19 pandemic, egalitarianism is an ethical approach to face medical resource scarcity. Egalitarianism highlights the moral equality between patients by delivering equal chance for equal need of healthcare beneficence [46]. As a result, physicians have to be presumably egalitarian, and they are obliged to treat each COVID-19 patient according to their clinical need. However, sometimes lottery seems to be as a forthright example to determine medical priority as an application of the egalitarianism approach to scarce resource rationing [50]. Many COVID-19 patients have strong moral sensitivities regarding equal distribution strategies, even if they maximize their utility. For instance, facing shortage of ICUs beds due to the large number of COVID-19 patients in need, egalitarianism approach lead to medical triage to choose which patients would be treated and saved. Medical triage needs some information about COVID-19 patients. Moreover, lotteries as a practical rule of egalitarianism and distributive justice are unresponsive to reasons that are instinctively interesting to patients’ wants of care beneficence.
The principle of “first come, first served” in distributing medical scarce resources seems to be egalitarian, but in the COVID-19 pandemic is not [51]. Ethically, ICU triage is a complex practice and can be warmly challenging. It must preferably be organized at all healthcare systems in all countries by providing clear COVID-19 admission guidelines [52]. Health professionals have to instigate a triage policy using healthcare decision support systems, this, could categorize COVID-19 patients having a small chance of survival who are ineligible to benefit from intensive care unit [22].
Choosing the worst-off COVID-19 patient: the prioritarianism approach
The prioritarian moral theory tries to give medical support to the worst-off COVID-19 patients by providing them priority in difficult circumstances in which not all patients can obtain a specific medical resource [53]. For example, in COVID-19 pandemic prioritarianism approach could specially distribute scarce medical resources to young rather than elderly because young patients have the highest life expectancy. Healthcare professionals as decision-makers require to be fair and transparent in distributing scarce resource during COVID-19 pandemic. A fair decision-making process must respect a special ethical view [54]. Daniels [55] suggested four criterions of fair distribution process: to be supervised by a legal institution, to make transparent decision, to be reasonable using relevant information, and to revise personal decision using adequate procedures. A fifth facet of fair allocation process is the significant community commitment [56].
The prioritization guidance of COVID-19 patients, must be contingent and should change regarding to the scientific evidence. Therefore, young patients must be unprivileged for novel coronavirus vaccine, if found effective, because it precludes COVID-19 disease instead of cure it. COVID-19 have severe consequences on elderly and those having chronic morbidities. The optimization of life saving value justifies the priority to give vaccine to elderly COVID-19 patients [32], [35], [44].
Utilitarian theories applied to scarce resource distribution have been largely criticized for unfair guidelines that could be used in detriment of vulnerable patients [57], [58]. Faced with the large COVID-19 patient flow and scarcity of ICU beds, emerged an ethical justification of ICU triage decision to maximize benefit for the most vulnerable patients [30], [46], [59], [60], [61], [62]. Azoulay et al. [62] argued that the ethical principle of distributive justice requires taking into account patient vulnerability to construct ICU admission guidelines for handling critical COVID-19 cases. Consequently, guidelines must be outlined to guarantee equity, avoid irrational inflexibility and confirm transparency [63]. Table 1 summarize the three ethical values managing medical triage in COVID-19 pandemic especially: utilitarianism, egalitarianism and prioritarianism.
Table 1.
Ethical values guiding triage of COVID-19 patients.
Valeurs éthiques guidant le tri des patients COVID-19.
| Ethical approaches and principles | Application in the Time of COVID-19 |
|---|---|
| Utilitarianism | |
| Save the maximum of lives | Give the uppermost priority |
| Save the maximum of life-years and maximize the prognosis | Give the highest priority |
| Egalitarianism | |
| “First come, first serve” principle | This principle must be banned |
| Choosing patients randomly using lottery principle | This principle is used for choosing patients having the same prognosis |
| Prioritarianism | |
| Treat firstly the worst-off | Should be used if it supports total benefit maximization |
| Treat firstly young patient Treat the most vulnerable patients |
Should be used if it supports total benefit maximization such as avoiding the virus expansion Should be used if it supports total benefit maximization |
Conclusions and recommendations
It is widely recognized that rationing of healthcare is indispensable, inevitable and have a complex ethical considerations. In COVID-19 pandemic, the attention given to a balanced use of many ethical values for different involvements and in various situations leads probably to conflicting decisions about how much preeminence should be assigned to each value in specific circumstances during the pandemic. This emphasizes the necessity for equal chance and regular resource distribution rules including the affected protagonists: physicians, technicians, patients, etc. Triage guidelines should be transparent to ensure public confidence in their integrity.
The consequences of these fair distribution rules, based on ethical values and outlined recommendations, must be the deployment of an explicit guidelines of prioritization to avoid improvising judgments about which patient to save. Nevertheless, even well-conceived guidelines may reveal serious problems in immediate decision making. To support healthcare professionals navigate these problems, healthcare organizations should implement a multidisciplinary triage committee including qualified doctors, technicians, administrators and ethicists, to help rationing decisions.
Policy makers in healthcare systems should do their best to avoid the shortage of medical resources. Nevertheless, if there is a lack of resources, we outline the following recommendations to develop guidelines that have to be applied equitably and regularly across cases in times of pandemic. These guidelines may guarantee that physicians are never confused in choosing which patients to save and which ones to let die. The following recommendations might outline the implementation of these guidelines.
Key recommendations.
To overcome the ethical dilemma associated with the distribution of scarce medical resources in the COVID-19 Pandemic, we suggest some recommendations:
-
•maximization of total benefit and life expectancy:
-
∘highlights the optimization of managing scarce resources such as ICUs beds and ventilators,
-
∘saves the maximum of lives and years of life expectancy among inhabitants,
-
∘gives priority to patient who might be recovered when they are treated,
-
∘gives priority to worst-off patients with a high risk of death at young age and deprived of a full life,
-
∘gives priority the most vulnerable patients;
-
∘
-
•prioritization of health professionals:
-
∘the treatment priority should be given to healthcare professionals who are indispensable in time of pandemic. They must obtain firstly the critical care as a recognition to their commitment in saving the community while taking the high-risk of infection,
-
∘the priority of treatment should not be given to rich or well-known people or to the politicians;
-
∘
-
•do not apply “first-come, first served” principle:
-
∘for patients having same prognoses, equal chance should be given using random distribution such as lottery,
-
∘the principle of “first-come, first-served” is used for longtime rare resources that patients may stay alive without them;
-
∘
-
•reactivity to contingency:
-
∘prioritize elderly for preventive vaccination, of course after serious cases of healthcare professionals,
-
∘prioritize the vaccination of younger COVID-19 patients only when this decision contribute in decreasing the spreading out of contamination risk to others,
-
∘regarding prognosis and scarce resource, prioritize younger severe COVID-19 patients in beneficiating from the ICU beds and ventilators to maximize total benefits,
-
∘distribution of trial treatments to positive symptomatic COVID-19 cases but not seriously ill, would maximize benefits;
-
∘
-
•practice the same ethical principles to all patients even those non COVID-19:
-
∘resource scarcity effects all types of patients (Stroke, cancer); equal distribution of ICU ventilators that gives priority to the maximization of total benefit and life expectancy.
-
∘
Disclosure of interest
The authors declare that they have no competing interest.
Footnotes
The number of countries and their geographical clustering is based on the United Nations Geoscheme. The latest statistical updates about COVID-19 data: https://www.worldometers.info/coronavirus/.
References
- 1.Everett J., Colombatto C., Chituc V., Brady W.J., Crockett M.J. 2020. The effectiveness of moral messages on public health behavioral intentions during the COVID-19 pandemic Jim A.C.https://www.psyarxiv.com/9yqs8/ [Google Scholar]
- 2.Bhattacharyaa S., Islam M., Alokkumar D.E. medRxiv; 2020. Search for trends of Covid-19 infection in India, China, Denmark, Brazil, France. Germany and the USA on the basis of power law scaling. [DOI] [Google Scholar]
- 3.Zhang H. The epidemiological characteristics of an outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China, 2020. China CDC Weekly. 2020;2:113–122. [PMC free article] [PubMed] [Google Scholar]
- 4.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. https://www.sfndt.org/sites/www.sfndt.org/files/medias/documents/Onder%20et%20al.%2C%20JAMA%20Mars%202020.pdf [DOI] [PubMed] [Google Scholar]
- 5.Solnica A., Barski L., Jotkowitz A. Allocation of scarce resources during the COVID-19 pandemic: a Jewish ethical perspective. J Med Ethics. 2020 doi: 10.1136/medethics-2020-106242. [DOI] [PubMed] [Google Scholar]
- 6.Scheunemann L.-P., White D.-B. The ethics and reality of rationing in medicine. Chest. 2011;140:1625–1632. doi: 10.1378/chest.11-0622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Getzen T. 5th ed. John Wiley & Sons; Hoboken, NJ: 2012. Health economics and financing. [Google Scholar]
- 8.Wu X., Nethery R.-C., Sabath M.-B., Braun D., Dominici F. medRxiv; 2020. Exposure to air pollution and COVID-19 mortality in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO . World Health Organization; 2020. Coronavirus Disease 2019 (Covid-19) Situation Report–51.https://www.who.int/docs/default-source/coronaviruse/situationreports/20200311-sitrep-51-Covid-19.pdf?sfvrsn=1ba62e57_8 [Google Scholar]
- 10.Chiappelli F., Khakshooy A., Greenberg G. Covid-19 immunopathology and immunotherapy. Bioinformation. 2020;16:219–222. doi: 10.6026/97320630016219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koubaa A. 2020. Understanding the COVID19 Outbreak: a comparative data analytics and study.https://www.arxiv.org/pdf/2003.14150.pdf [Google Scholar]
- 12.Liang L.L., Tseng C.H., Ho H.J., Wu C.Y. Covid-19 mortality is associated with test number and government effectiveness. Research Square. 2020 doi: 10.1038/s41598-020-68862-x. https://www.researchsquare.com/article/rs-28218/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arezki R., Nguyen H. World Bank; 2020. The corona virus’ potential effects on the Middle East and North Africa.https://www.worldbank.org/arabvoices/coronavirus-potential-effects-middle-east-and-north-africa [accessed: 31 March 2020] [Google Scholar]
- 14.Bianco C., Infected: European Council on Foreign Relations; 2020. The impact of the coronavirus on the Middle East and North Africa.https://www.ecfr.eu/commentary-infected-the-impact-of-the-corona-virus-on-the-middle-east-and-no [Date accessed: 31 March 2020] [Google Scholar]
- 15.Riboua Z. Atlantic Council; 2020. Coronavirus experiences on the ground in the Middle East.https://www.atlanticcouncil.org/blogs/menasources/coronavirus-experiences-on-the-ground-in-the-middle-east [Date accessed: 30 March 2020] [Google Scholar]
- 16.Gambill G.C. Middle East Forum; 2020. Roman on the Arab Gulf States’ Reaction to the Coronavirus Pandemic.https://www.meforum/org/60613/roman-on-arab-gulf-states-reaction-to-coronavirus [Date accessed 28 March 2020] [Google Scholar]
- 17.Frantzman S. Middle East Forum; 2020. COVID-19 widens the divide in the fractured Middle East.https://www.meforum.org/60653-Covid-19-widens-the-divide-in-middle-east [Date accessed: 3 April 2020] [Google Scholar]
- 18.Kenneth V., Iserson M.D., Moskop J.C. Triage in medicine, part I: concept, history, and types. Ann Emerg Med. 2007;9:275–281. doi: 10.1016/j.annemergmed.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 19.Institute of Medicine IOM . Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations. In: Altevogt B.M., Stroud C., Hanson S.L., editors. Guidance for establishing crisis standards of care for use in disaster situations: a letter report. National Academies Press (Us); Washington (DC): 2009. https://www.ncbi.nlm.nih.gov/books/NBK219958/ [PubMed] [Google Scholar]
- 20.Strech D., Synofzik M., Marckmann G. How physicians allocate scarce resources at the bedside: a systematic review of qualitative studies. J Med Philos. 2008;33:80–99. doi: 10.1093/jmp/jhm007. [DOI] [PubMed] [Google Scholar]
- 21.Truog R.D., Brock D.W., Cook D.J. Rationing in the intensive care unit. Crit Care Med. 2006;34:958–963. doi: 10.1097/01.CCM.0000206116.10417.D9. [DOI] [PubMed] [Google Scholar]
- 22.Xie J., Tong Z., Guan X., Du B., Qiu H., Slutsky A.S. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qiu H., Tong Z., Ma P. Intensive care during the coronavirus epidemic. Intensive Care Med. 2020;46:576–578. doi: 10.1007/s00134-020-05966-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020 doi: 10.1001/jama.2020.4031. [published online March 13] [DOI] [PubMed] [Google Scholar]
- 25.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020 doi: 10.1016/S0140-6736(20)30627-9. [S0140-6736 (published online March 13)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [published online Feb 28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fisher D., Wilder-Smith A. The global community needs to swiftly ramp up the response to contain COVID-19. Lancet. 2020 doi: 10.1016/S0140-6736(20)30679-6. [published online March 18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phua J., Weng L., Ling L., Egi M., Lim C.-M. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Einav S., Hick J.L., Hanfling D. Surge capacity logistics: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146 doi: 10.1378/chest.14-0734. [e17S–43S] [DOI] [PubMed] [Google Scholar]
- 31.Phua J., Faruq M.O., Kulkarni A.P. Critical care bed capacity in Asian countries and regions. Crit Care Med. 2020 doi: 10.1097/CCM.0000000000004222. [published online Jan 9] [DOI] [PubMed] [Google Scholar]
- 32.Rosenbaum S.J., Bayer R., Bernheim R.G. Centers for Disease Control and Prevention; Atlanta: 2011. Ethical considerations for decision making regarding allocation of mechanical ventilators during a severe influenza pandemic or other public health emergency.https://www.cdc.gov/od/science/integrity/phethics/docs/Vent_Document_Final_Version.pdf [Google Scholar]
- 33.Zucker H., Adler K., Berens D. New York State Department of Health Task Force on Life and the Law; Albany: 2015. Ventilator allocation guidelines.https://www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf [Google Scholar]
- 34.Toner E., Waldhorn R. Johns Hopkins University Center for Health Security; Baltimore: 2020. What US hospitals should do now to prepare for a COVID-19 pandemic.http://www.centerforhealthsecurity.org/cbn/2020/cbnreport-02272020html [Google Scholar]
- 35.Ezekiel J., Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 36.Biddison L.D., Berkowitz K.A., Courtney B. Ethical considerations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146 doi: 10.1378/chest.14-0742. [e145S–55S] [DOI] [PubMed] [Google Scholar]
- 37.Hick J.L., Hanfling D., Wynia M.K., Pavia A.T. Duty to plan: health care, crisis standards of care, and novel coronavirus SARS-CoV-2. NAM Perspectives. 2020 doi: 10.31478/202003b. https://www.nam.edu/duty-to-plan-health-care-crisis-standards-of-care-and-novel-coronavirus-sars-cov-2/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cohn J. Huffington Post; 2020. How to get more ventilators and what to do if we can’t.https://www.huffpost.com/entry/coronavirus-ventilators-supply-manufacture_n_5e6dc4f7c5b6747ef11e8134 [Google Scholar]
- 39.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meyfroidt E., Vlieghe E., Biston P. Ethical principles concerning proportionality of critical care during the 2020 COVID-19 pandemic in Belgium: advice by the Belgian Society of Intensive care medicine Geert. Belgian Soc Intensive Care Med. 2020 https://www.hartcentrumhasselt.be/professioneel/nieuws-professioneel/ethical-principles-concerning-proportionality-of-critical-care-during-the-Covid-19-pandemic-advice-by-the-belgian-society-of-ic-medicine [Google Scholar]
- 41.Arango A. Lessons learned from the coronavirus health crisis in Madrid, Spain: how Covid-19 has changed our lives in the last 2 weeks. Biol Psychiatry. 2020 doi: 10.1016/j.biopsych.2020.04.003. https://www.biologicalpsychiatryjournal.com/article/S0006-3223(20)31493-1/pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ñamendys-Silva S.A. Respiratory support for patients with COVID-19 infection. Lancet Respir Med. 2020;8:E18. doi: 10.1016/S2213-2600(20)30110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [published online Feb 7] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bentham J. Oxford University Press; England: 1983. Deontology; together with a table of the springs of action; and the article on utilitarianism. [Google Scholar]
- 45.Persad G., Wertheimer A., Emanuel E.J. Principles for allocation of scarce medical, interventions. Lancet. 2009;373:423–431. doi: 10.1016/S0140-6736(09)60137-9. [DOI] [PubMed] [Google Scholar]
- 46.Beauchamp T.L., Childress J.F. 6th ed. Oxford University Press; Oxford: 2009. Principles of biomedical ethics. [Google Scholar]
- 47.White D.B., Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323:1773–1774. doi: 10.1001/jama.2020.5046. [DOI] [PubMed] [Google Scholar]
- 48.Luce J.M., Rubenfeld G.D. Can health care costs be reduced by limiting intensive care at the end of life? Am J Respir Crit Care Med. 2002;165:750–754. doi: 10.1164/ajrccm.165.6.2109045. [DOI] [PubMed] [Google Scholar]
- 49.Vaillancourt F. COVID-19 and the health policy recession: whatever it takes, grandma or the economy or what makes sense? Cirano. 2020 https://www.cirano.qc.ca/files/publications/2020PE-01.pdf [Google Scholar]
- 50.Savulescu J., Cameron J., Wilkinson D. Equality or utility? Ethics and law of rationing ventilators. Br J Anaesthesia. 2020 doi: 10.1016/j.bja.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Geldsetzer P. Knowledge and perceptions of COVID-19 among the general public in the United States and the United Kingdom: a cross-sectional online survey. Ann Internal Med. 2020 doi: 10.7326/M20-0912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vergano M., Bertolini G., Giannini A. Italian Society of Anesthesia, Analgesia, Resuscitation, and Intensive Care (SIAARTI); 2020. Clinical ethics recommendations for the allocation of intensive care treatments, in exceptional, resource-limited circumstances.http://www.siaarti.it/SiteAssets/News/COVID19%20-%20documenti%20SIAARTI/SIAARTI%20-%20Covid-19%20-%20Clinical%20Ethics%20Reccomendations.pdf [Google Scholar]
- 53.Kate H.-D., Nicholson M. 2020. Rationing and disability in a state of crisis, working papers University of Virginia School of Law, Public Law and Legal Theory Paper Series 2020-33.https://www.papers.ssrn.com/sol3/papers.cfm?abstract_id=3570088 [Google Scholar]
- 54.Daniels N., Sabin J. Limits to health care: fair procedures, democratic deliberation, and the legitimacy problem for insurers. Philos Public Aff. 1997;26:303–350. doi: 10.1111/j.1088-4963.1997.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 55.Daniels N. Accountability for reasonableness. BMJ. 2000;3(21):1300–1301. doi: 10.1136/bmj.321.7272.1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Baum N.M., Jacobson P.D., Goold S.D. Listen to the people: public deliberation about social distancing measures in a pandemic. Am J Bioeth. 2009;9:4–14. doi: 10.1080/15265160903197531. [DOI] [PubMed] [Google Scholar]
- 57.Silva D.S., Gibson J.L., Robertson A. Priority setting of ICU resources in an influenza pandemic: a qualitative study of the Canadian public's perspectives. BMC Public Health. 2012;26:241. doi: 10.1186/1471-2458-12-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bourgois P., Holmes S.-M., Sue K., Quesada J. Structural vulnerability: operationalizing the concept to address health disparities in clinical care. Acad Med. 2017;92:299–307. doi: 10.1097/ACM.0000000000001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Maves R.C., Downar J., Dichter J.R. Triage of scarce critical care resources in COVID-19 an implementation guide for regional allocation. Chest. 2020 doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 61.Mohile S., Dumontier C., Mian H. Perspectives from the Cancer and Aging Research Group: caring for the vulnerable older patient with cancer and their caregivers during the COVID-19 crisis in the United States. J Geriatric Oncol. 2020;11:753–760. doi: 10.1016/j.jgo.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Azoulay É., Beloucif S., Guidet B. Admission decisions to intensive care units in the context of the major COVID-19 outbreak: local guidance from the COVID-19 Paris-region area. Crit Care. 2020;24:293. doi: 10.1186/s13054-020-03021-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Truog R.D., Campbell M.L., Curtis J.R. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med. 2008;36:953–963. doi: 10.1097/CCM.0B013E3181659096. [DOI] [PubMed] [Google Scholar]