Background:
The goal of this study was to investigate the association between preoperative radiographic severity of knee osteoarthritis (OA) and patient-reported outcomes following total knee replacement.
Methods:
We used data from a prospective cohort study of individuals who underwent total knee replacement at a high-volume medical center. Patient-reported outcomes included the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score and the Knee injury and Osteoarthritis Outcome Score (KOOS) activities of daily living (ADL) subscore, assessed preoperatively and 2 years postoperatively. We measured preoperative radiographic OA severity using the Osteoarthritis Research Society International (OARSI) Atlas score, dichotomized at the median. We assessed the association between radiographic OA severity and postoperative patient-reported outcomes in bivariate analyses and in multivariable linear regression, with adjustment for age, sex, body mass index, and comorbidity score.
Results:
The analytic cohort included 240 patients with a mean age at surgery of 66.6 years (standard deviation, 8 years); 61% were female. The median total OARSI radiographic severity score was 10 (range, 3 to 17). The cohort improved substantially at 2 years following total knee replacement, with WOMAC pain and KOOS ADL score improvements on the order of 30 points. We did not observe significant or clinically important differences in pain relief or functional improvement between patients with milder and more severe radiographic OA. Sensitivity analyses using other radiographic assessment measures yielded similar findings.
Conclusions:
Total knee replacement offers substantial symptomatic relief and functional improvement regardless of preoperative radiographic OA severity.
Level of Evidence:
Prognostic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Millions of primary total knee replacement procedures have been performed worldwide, and >80% have been performed for a primary diagnosis of osteoarthritis (OA)1-3. As of 2010, approximately 4.7 million adults were living with a knee replacement in the United States4. Although total knee replacement has a high success rate, is cost-effective, and improves quality of life for millions of individuals5,6, up to 20% of patients experience suboptimal outcomes7. The number of total knee replacement procedures performed annually continues to rise8, highlighting the importance of continued attention to optimizing outcomes for patients following total knee replacement.
Knee radiographs are the mainstay of OA diagnosis9. Understanding implications of preoperative radiographic findings for total knee replacement surgical outcomes may help guide the preoperative planning process and help set expectations prior to total knee replacement surgery. Previous investigations of the association between preoperative radiographic OA severity and postoperative patient-reported outcomes following total knee replacement have not reached definitive conclusions10-16. Some studies have demonstrated better outcomes among individuals with radiographically severe OA compared with milder OA10-14, while other studies have shown no difference in outcomes between the 2 groups15,16. Most of these investigations utilized the Kellgren-Lawrence (KL) system, or a variant of this method, to grade radiographic OA severity. However, the KL system does not provide granular assessments of radiographic findings, such as osteophytes or joint-space narrowing, does not differentiate between medial and lateral tibiofemoral disease, and gives substantial weight to joint-space narrowing in the final score17.
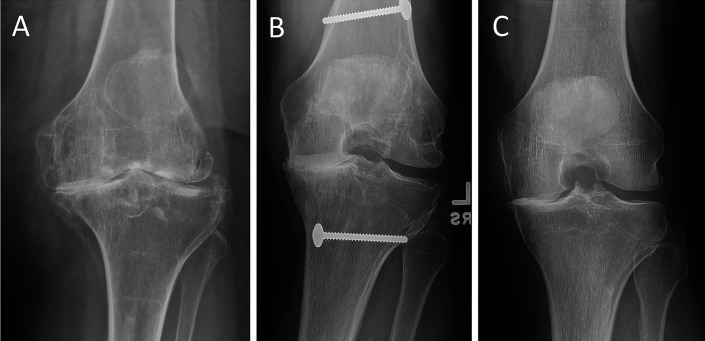
The Osteoarthritis Research Society International (OARSI) Atlas is a widely accepted and standardized radiographic assessment tool that takes into account osteophyte formation and joint-space narrowing in the medial and lateral tibiofemoral compartments9. Distinct contributions of each osteophyte size and location and each joint-space width are graded and added together for a final, total OARSI score. Each radiographic element’s contribution is weighted equally, thus providing a more standardized and more granular assessment than the KL grade (Fig. 1).
Fig. 1.
Figs. 1-A, 1-B, and 1-C The Osteoarthritis Research Society International (OARSI) score offers a more standardized and granular radiographic assessment than does Kellgren-Lawrence (KL) grade. All 3 knee radiographs demonstrate KL grade-4 osteoarthritis (OA) given definite osteophyte formation and severe joint-space narrowing. However, the OARSI score is different for each radiograph, demonstrating differences in the presence of osteophytes and differences in medial and lateral involvement. Fig. 1-A Advanced knee OA: KL grade 4, OARSI score of 17. Fig. 1-B Advanced knee OA: KL grade 4, OARSI score of 9. Fig. 1-C Advanced knee OA: KL grade 4, OARSI score of 8.
The goal of this study was to investigate the association between preoperative radiographic OA severity, as measured by the OARSI score, and patient-reported outcomes following total knee replacement.
Materials and Methods
Sample
The Adding Value in Knee Arthroplasty (AViKA) Postoperative Care Navigation Trial is a 2-arm randomized controlled trial that evaluated motivational interviewing to enhance rehabilitation following total knee replacement17. Three hundred and eight consecutive patients undergoing primary unilateral total knee replacement at a tertiary medical center were enrolled. Eligible patients were community-dwelling adults ≥40 years of age who had a primary diagnosis of OA and spoke English. Excluded were patients with an underlying diagnosis other than OA (e.g., inflammatory arthritis), psychological issues precluding participation, or dementia, non-English speakers, nursing home residents, and patients with plans for additional elective surgery within 6 months. The primary outcome variable investigated in that study17 was improvement in function as measured by the change in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) function score from preoperatively to 6 months postoperatively. Our final analysis included patients who had radiographs available at baseline as well as outcomes available at both baseline and 2 years.
Data Elements
Radiographic Assessments
The large majority of preoperative radiographs were posteroanterior (PA) flexed weight-bearing views. We assessed anteroposterior weight-bearing views when PA flexed views were not available. If multiple radiographs were available, the radiograph demonstrating maximum joint-space narrowing was utilized. The radiographs were scored according to the OARSI method, as previously described18, with 0 representing the least severe findings and 18 representing the most severe possible. The radiographs were assessed by 2 reviewers who were blinded to patient outcome scores. The reliability of these readings has been established previously19. The OARSI score was dichotomized at the median based on the distribution within the cohort, producing a “milder OA” group (OARSI score of <10) and a “more severe OA” group (OARSI score of ≥10). Other radiographic assessments performed for sensitivity analyses included KL grade, compartment-specific OARSI scores, and compartment-specific joint-space-narrowing (JSN) scores. KL grade was calculated on the basis of the method described by Kellgren and Lawrence19, with 0 representing no abnormalities and 4 representing the most severe arthritis possible. The compartment-specific OARSI score was calculated according to the OARSI method18, but only included the score from a single tibiofemoral compartment, with 0 representing the least severe findings possible and 9 representing the most severe possible. The compartment-specific JSN score was calculated for individual compartments alone according to the OARSI method of calculating joint-space narrowing18, with 0 representing no joint-space narrowing and 3 representing the most joint-space narrowing possible.
Data Collection and Outcomes
Participants completed a baseline questionnaire within 6 weeks prior to surgery and were asked to complete another questionnaire 2 years following total knee replacement. Primary outcomes were the WOMAC pain score and the Knee injury and Osteoarthritis Outcome Score (KOOS) activities of daily living (ADL) subscore20,21. WOMAC pain scores were converted to a 0-to-100 scale, with 100 indicating the worst pain possible, per convention. KOOS ADL subscores were converted to a 0-to-100 scale, with 0 indicating the greatest knee dysfunction possible, per convention.
Covariates
We assessed demographics and preoperative clinical characteristics of the cohort at baseline, including age, race, sex, body mass index (BMI), and Charlson Comorbidity Index (Table I). BMI was calculated from self-reported height and weight. We stratified BMI into 5 groups22: <25.0, 25 to 29.9, 30 to 34.9, 35 to 39.9, and ≥40.0 kg/m2. Charlson Comorbidity Index scores were grouped as follows23: 0, 1, 2, and ≥3.
TABLE I.
Baseline Characteristics*
| Overall (N = 304) | Missing Follow-up (N = 64) | Final Analytic Cohort | |||
| Complete Cases (N = 240) | OARSI Score <10 (N = 102) | OARSI Score ≥10 (N = 138) | |||
| Age at surgery (yr) | 66.5 (8.2) | 66.1 (8.7) | 66.6 (8.0) | 66.8 (8.5) | 66.4 (7.7) |
| Age group | |||||
| <65 yr | 129 (42.4%) | 32 (50.0%) | 97 (40.4%) | 35 (34.3%) | 62 (44.9%) |
| ≥65 yr | 175 (57.6%) | 32 (50.0%) | 143 (59.6%) | 67 (65.7%) | 76 (55.1%) |
| White vs. non-white | |||||
| Non-white | 26 (8.8%) | 7 (11.5%) | 19 (8.1%) | 4 (4.0%) | 15 (11.1%) |
| White | 270 (91.2%) | 54 (88.5%) | 216 (91.9%) | 96 (96.0%) | 120 (88.9%) |
| Sex | |||||
| Male | 121 (39.8%) | 28 (43.8%) | 93 (38.8%) | 36 (35.3%) | 57 (41.3%) |
| Female | 183 (60.2%) | 36 (56.3%) | 147 (61.3%) | 66 (64.7%) | 81 (58.7%) |
| BMI (kg/m2) | 30.75 (6.08) | 31.76 (6.58) | 30.48 (5.93) | 30.17 (6.14) | 30.72 (5.78) |
| BMI group | |||||
| <25.0 kg/m2 | 49 (16.6%) | 8 (12.9%) | 41 (17.5%) | 24 (23.8%) | 17 (12.8%) |
| 25-29.9 | 99 (33.4%) | 19 (30.6%) | 80 (34.2%) | 27 (26.7%) | 53 (39.9%) |
| 30-34.9 | 84 (28.4%) | 22 (35.5%) | 62 (26.5%) | 29 (28.7%) | 33 (24.8%) |
| 35-39.9 | 40 (13.5%) | 5 (8.1%) | 35 (15.0%) | 14 (13.9%) | 21 (15.8%) |
| ≥40.0 | 24 (8.1%) | 8 (12.9%) | 16 (6.8%) | 7 (6.9%) | 9 (6.8%) |
| Comorbidity score | 1.3 (1.6) | 1.6 (1.7) | 1.2 (1.5) | 1.40 (1.71) | 1.09 (1.33) |
| Comorbidity score group | |||||
| 0 | 129 (43.7%) | 22 (35.5%) | 107 (45.9%) | 44 (44.0%) | 63 (47.4%) |
| 1 | 54 (18.3%) | 10 (16.1%) | 44 (18.9%) | 16 (16.0%) | 28 (21.1%) |
| 2 | 56 (19.0%) | 15 (24.2%) | 41 (17.6%) | 20 (20.0%) | 21 (15.8%) |
| ≥3 | 56 (19.0%) | 15 (24.2%) | 41 (17.6%) | 20 (20.0%) | 21 (15.8%) |
| WOMAC pain at baseline | 40.6 (17.6) | 47.2 (17.9) | 39.1 (17.2) | 39.0 (16.9) | 39.1 (17.5) |
| KOOS ADL at baseline | 58.7 (17.4) | 52.3 (19.5) | 60.4 (16.5) | 60.1 (15.8) | 60.6 (17.0) |
| SF-36 MHI-5 at baseline | 76.7 (17.4) | 73.9 (18.2) | 77.5 (17.1) | 75.5 (18.4) | 78.9 (16.0) |
| Index knee OARSI Atlas score | 10.0 (2.7) | 10.2 (2.9) | 10.0 (2.7) | 7.5 (1.5) | 11.8 (1.6) |
| OARSI Atlas category | |||||
| Score of <10 | 129 (42.4%) | 27 (42.2%) | 102 (42.5%) | NA | NA |
| Score of ≥10 | 175 (57.6%) | 37 (57.8%) | 138 (57.5%) | NA | NA |
| KL category | |||||
| Grade 1 | 6 (2.0%) | 0 (0%) | 6 (2.5%) | NA | NA |
| Grade 2 | 27 (8.9%) | 4 (6.3%) | 23 (9.6%) | NA | NA |
| Grade 3 | 75 (24.7%) | 18 (28.1%) | 57 (23.8%) | NA | NA |
| Grade 4 | 196 (64.5%) | 42 (65.6%) | 154 (64.2%) | NA | NA |
Demographic characteristics are reported for all subjects with available radiographic data (“Overall” column) and separately for individuals with complete self-reported outcome data and with incomplete self-reported outcome data. Osteoarthritis Research Society International (OARSI) score categories represent subgroups of the analytic cohort only (i.e., subgroups of Complete Cases only). Continuous variables are given as the mean, with the standard deviation in parentheses. Categorical variables are given as the number, with the percentage in parentheses. BMI = body mass index, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index, KOOS ADL = Knee injury and Osteoarthritis Outcome Score activities of daily living, SF-36 = Short Form-36, MHI = Mental Health Inventory, NA = not applicable, and KL = Kellgren-Lawrence.
Statistical Analysis
Initially, we assessed the relationship between preoperative OARSI score and patient-reported outcomes with scatterplots. We assessed the association between OARSI score and patient-reported outcomes using Pearson (baseline and 2-year change) or Spearman (2-year outcomes, which were skewed) correlation coefficients and linear regression. We assessed the unadjusted association between the binary radiographic OA severity measure and postoperative patient-reported outcomes by a t test or Wilcoxon rank-sum test, as appropriate. We used multivariable linear regression to adjust for age, sex, BMI, and comorbidity score. For baseline and change in patient-reported outcomes, we used the untransformed outcome measure; due to the skewed nature of the 2-year outcome scores, we used the cube root transformation for statistical testing24.
We performed sensitivity analyses to examine the association between outcomes and alternate measures of baseline OA severity. These included (1) KL grade (<4 versus 4), (2) compartment-specific (i.e., medial and lateral) OARSI scores, (3) compartment-specific (medial and lateral) JSN scores, and (4) 4-level OARSI score based on quartiles. We investigated KL grade because of its wide use in previous studies. We investigated compartment-specific OARSI scores because total knee replacement may be performed for unicompartmental disease. We investigated compartment-specific joint-space narrowing because it is one major driver of clinical indication for total knee replacement. For compartment-specific JSN scores, we performed an unadjusted analysis of variance (ANOVA) or Kruskal-Wallis test, as appropriate.
KL grade and compartment-specific JSN score subcategories indicating radiographically milder or more severe OA were created on the basis of the distribution of KL grades or compartment-specific JSN scores, respectively, within the cohort. Compartment-specific OARSI score subcategories of low (“milder OA”) and high (“more severe OA”) were created by dichotomizing compartment-specific OARSI scores within the cohort at the median for medial (median = 6) and lateral (median = 4) compartments individually. A 4-level compartment-specific OARSI score metric was created by describing each combination of subcategories as a separate entity: (1) low medial, low lateral; (2) low medial, high lateral; (3) high medial, low lateral; and (4) high medial, high lateral.
We compared the radiographic features between those who completed the 2-year survey and those who missed 2-year follow-up in order to assess the impact of missing data.
All analyses were conducted in SAS version 9.4. (SAS Institute).
Results
Of the 308 enrolled subjects, 304 had radiographs available for analysis (see “Radiographic Assessments” above). Of these 304 subjects, 240 (78.95%) completed baseline and 2-year outcome surveys (see “Data Collection and Outcomes” above). These 240 subjects represent our final analytic cohort.
The mean age at surgery was 66.6 years (standard deviation [SD], 8 years), and 61% of the subjects were female. The median preoperative OARSI radiographic severity score was 10 (range, 3 to 17); 102 (42.5%) of the subjects had an OARSI score of <10. Of note, OARSI scores were similar between subjects in the analytic cohort and those excluded because of missing questionnaire data (Table I). Prior to total knee replacement, study participants reported a mean WOMAC pain score of 39.1 (SD, 17). We did not observe a significant or clinically relevant association between preoperative OARSI score and preoperative patient-reported pain and functional limitation (Table II). Scatterplots of the 2-year change in scores for WOMAC pain and KOOS ADL provide a clear depiction of the lack of linear association with OARSI score (Appendix Figure 1). The correlation between patient-reported outcomes and OARSI score ranged from −0.036 (95% confidence interval [CI], −0.162 to 0.091) for the WOMAC pain score at 2 years to 0.079 (95% CI, −0.048 to 0.204) for the KOOS ADL subscore at 2 years (Table II).
TABLE II.
Association Between Patient-Reported Outcome Scores at Baseline and 2 Years Postoperatively and Continuous Preoperative Osteoarthritis Research Society International (OARSI) Score*
| Patient-Reported Outcome | Unadjusted | Adjusted | |
| Correlation Coefficient (95% CI) | Parameter Estimate (95% CI) | Parameter Estimate (95% CI) | |
| WOMAC pain | |||
| Baseline | 0.012 (−0.114, 0.139) | 0.08 (−0.74, 0.90) | −0.23 (−1.06, 0.59) |
| 2 yr | −0.036 (−0.162, 0.091) | −0.17 (−0.79, 0.44) | −0.37 (−1.00, 0.27) |
| Change from baseline to 2 yr | −0.041 (−0.166, 0.087) | −0.25 (−1.06, 0.55) | −0.13 (−0.98, 0.72) |
| KOOS ADL | |||
| Baseline | −0.004 (−0.131, 0.122) | −0.03 (−0.81, 0.76) | 0.23 (−0.57, 1.03) |
| 2 yr | 0.079 (−0.048, 0.204) | 0.41 (−0.25, 1.08) | 0.63 (−0.06, 1.32) |
| Change from baseline to 2 yr | 0.067 (−0.06, 0.192) | 0.44 (−0.39, 1.27) | 0.4 (−0.48, 1.29) |
Unadjusted correlations are from Pearson (baseline, 2-year change) or Spearman (2-year outcome) correlation. Unadjusted parameter estimates are from linear regression, and adjusted estimates are from multivariable linear regression, adjusting for age, sex, body mass index, and comorbidity score. The parameter estimate is interpreted as the increase in patient-reported outcome associated with a 1-unit increase in baseline OARSI score. WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain is scaled 0 to 100, with 100 being the worst pain. KOOS ADL (Knee injury and Osteoarthritis Outcome Score activities of daily living) is scaled 0 to 100, with 100 being the best function. CI = confidence interval.
Demographic characteristics and radiographic OA severity scores were similar between subjects in the analytic cohort and those who were excluded from our analysis; however, those with complete data exhibited superior self-reported baseline pain, function, and mental health (Table I).
The cohort improved substantially over 2 years following total knee replacement, with improvements in WOMAC pain and KOOS ADL scores on the order of 30 points (0-to-100 scale) (Table III). Low postoperative WOMAC pain scores among the majority of the cohort were indicative of excellent outcomes. We did not observe a significant or clinically important difference in pain relief between subjects with milder and more severe radiographic OA (change in WOMAC pain score, −30.7 for those with an OARSI score of <10 versus −32.6 for those with an OARSI score of ≥10; difference, 1.9 [95% CI, −2.4 to 6.2]) (Table III). The results were confirmed in multivariable analyses that adjusted for age, sex, BMI, and comorbidity. Similarly, we did not observe a significant or clinically important difference in functional improvement, as assessed by change in KOOS ADL subscores, between subjects with radiographically milder and more severe OA (28.6 for those with milder OA versus 31.2 for those with more severe OA; difference, −2.6 [95% CI, −7.1 to 1.9]) (Table III). Results were similar in multivariable models adjusted for age, sex, BMI, and comorbidity score.
TABLE III.
Patient-Reported Outcome Scores at Baseline and 2 Years Postoperatively, Stratified by Preoperative Osteoarthritis Research Society International (OARSI) Score*
| Patient-Reported Outcomes | OARSI Score <10 | OARSI Score ≥10 | Unadjusted Difference Between Groups (95% CI) | Adjusted Difference Between Groups (95% CI) |
| WOMAC pain | ||||
| Baseline | 39.0 (16.9) | 39.1 (17.5) | 0.0 (−4.5, 4.4) | 0.68 (−3.75, 5.1) |
| 2 yr | 8.3 (14.8) | 6.5 (11.2) | 1.8 (−1.5, 5.2) | 0.18 (−0.15, 0.5) |
| Change from baseline to 2 yr | −30.7 (17.8) | −32.6 (16.1) | 1.9 (−2.4, 6.2) | 1.62 (−2.92, 6.17) |
| KOOS ADL | ||||
| Baseline | 60.1 (15.8) | 60.6 (17.0) | −0.5 (−4.8, 3.7) | −1.11 (−5.4, 3.17) |
| 2 yr | 88.7 (16.7) | 91.8 (11.4) | −3.1 (−6.7, 0.5) | −0.1 (−0.2, 0.01) |
| Change from baseline to 2 yr | 28.6 (18.3) | 31.2 (17.0) | −2.6 (−7.1, 1.9) | −2.53 (−7.3, 2.24) |
Patient-reported outcome scores are reported separately for individuals with radiographically milder osteoarthritis (OARSI score of <10) and more severe osteoarthritis (OARSI score of ≥10). Continuous variables are given as the mean, with the standard deviation in parentheses. “Difference between groups” indicates the difference in mean outcome scores between OARSI score categories as assessed by t test or Wilcoxon rank-sum test, as appropriate, for unadjusted analyses and linear regression for adjusted analyses. WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain is scaled 0 to 100, with 100 being the worst pain. KOOS ADL (Knee injury and Osteoarthritis Outcome Score activities of daily living) is scaled 0 to 100, with 100 being the best function. CI = confidence interval. No significant associations were found.
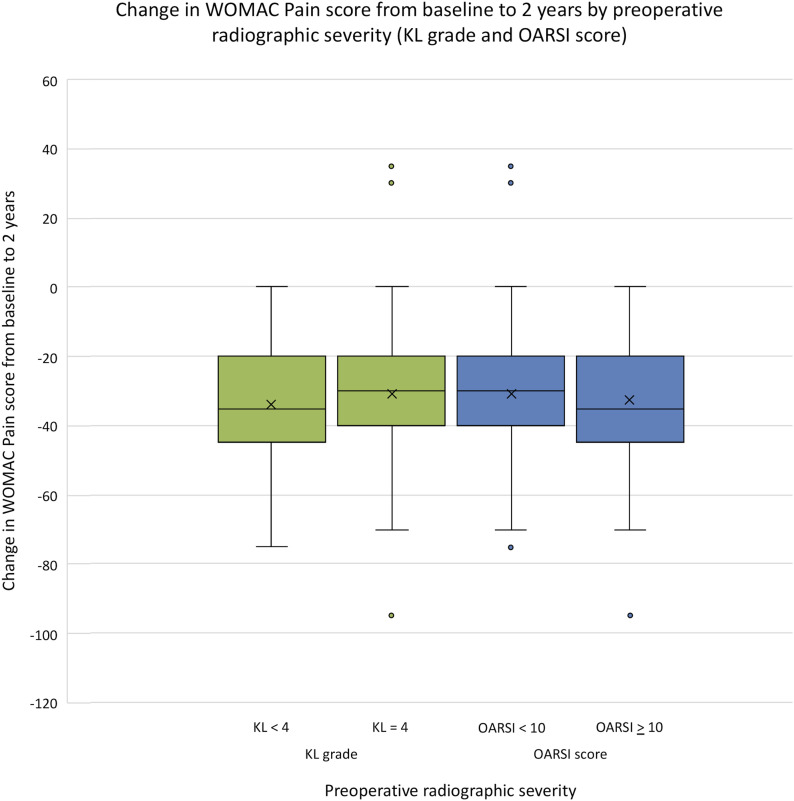
In sensitivity analyses, we compared pain relief and functional improvement between subjects with milder and more severe radiographic findings utilizing 4 other radiographic assessments: KL grade (Fig. 2, Table IV), compartment-specific OARSI scores (Table V), compartment-specific JSN scores (Appendix Tables 1 and 2), and 4-level OARSI score category (Appendix Table 3). In each case, we did not observe clinically important differences in pain or function scores between subjects with radiographically milder and more severe OA.
Fig. 2.
Change in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain score from baseline to 2 years by preoperative radiographic osteoarthritis (OA) severity. Individuals with mild and severe radiographic arthritis, as defined by both Kellgren-Lawrence (KL) and Osteoarthritis Research Society International (OARSI) criteria preoperatively, experienced meaningful pain relief at 2 years postoperatively with no significant differences between the groups. The top and bottom of the boxes = the 25th and 75th percentile, the horizontal line within the boxes = the median, the “x” within the boxes = the mean, the circles = outliers, and the whiskers = the minimum and maximum excluding outliers.
TABLE IV.
Patient-Reported Outcome Scores at Baseline and 2 Years Postoperatively, Stratified by Preoperative Kellgren-Lawrence (KL) Score*
| Patient-Reported Outcome | KL <4 | KL = 4 | Difference Between Groups (95% CI) |
| WOMAC pain | |||
| Baseline | 43.0 (18.0) | 36.9 (16.4) | 6.1 (1.6, 10.6) |
| 2 yr | 9.2 (15.5) | 6.2 (11.1) | 3.0 (−0.5, 6.4) |
| Change from baseline to 2 yr | −33.8 (16.2) | −30.7 (17.1) | −3.1 (−7.6, 1.3) |
| KOOS ADL | |||
| Baseline | 57.8 (16.8) | 61.8 (16.2) | −4.0 (−8.4, 0.3) |
| 2 yr | 88.5 (17.4) | 91.6 (11.6) | −3.1 (−6.8, 0.6) |
| Change from baseline to 2 yr | 30.7 (16.9) | 29.8 (17.9) | 0.9 (−3.7, 5.6) |
Patient-reported outcome scores are reported separately for individuals with milder radiographic arthritis (KL <4) and more severe radiographic arthritis (KL = 4). Continuous variables are given as the mean, with the standard deviation in parentheses. “Difference between groups” indicates the difference in mean outcome scores between KL categories as assessed by t test or Wilcoxon rank-sum test, as appropriate. WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain is scaled 0 to 100, with 100 being the worst pain. KOOS ADL (Knee injury and Osteoarthritis Outcome Score activities of daily living) is scaled 0 to 100, with 100 being the best function. CI = confidence interval. Bold indicates a significant association.
TABLE V.
Patient-Reported Outcome Scores at Baseline and 2 Years Postoperatively, Stratified by Preoperative Compartment-Specific Osteoarthritis Research Society International (OARSI) Score*
| Patient-Reported Outcome | Low Medial, Low Lateral | Low Medial, High Lateral | High Medial, Low Lateral | High Medial, High Lateral | P Value |
| WOMAC pain | |||||
| Baseline | 43.5 (17.1) | 38.4 (17.5) | 36.5 (16.4) | 41.1 (17.9) | 0.57 |
| 2 yr | 10.1 (20.2) | 7.4 (11.6) | 5.7 (10.6) | 7.8 (12.2) | 0.47 |
| Change from baseline to 2 yr | −33.4 (15.6) | −31.0 (15.4) | −30.7 (19.2) | −33.4 (15.3) | 0.69 |
| KOOS ADL at baseline | 55.0 (16.3) | 61.8 (16.3) | 62.6 (15.7) | 58.6 (17.4) | 0.73 |
| KOOS ADL at 2 years | 86.7 (19.5) | 89.5 (16.2) | 92.6 (10.6) | 90.7 (12.0) | 0.26 |
| Change in KOOS ADL from baseline to 2 years | 31.8 (16.1) | 27.7 (16.3) | 29.9 (19.1) | 32.0 (17.3) | 0.35 |
Patient-reported outcome scores are reported separately for 4 preoperative compartment-specific OARSI score combinations: low medial, low lateral (milder osteoarthritis of the medial and lateral compartments); low medial, high lateral (milder osteoarthritis of the medial compartment, more severe arthritis of the lateral compartment); high medial, low lateral (more severe osteoarthritis of the medial compartment, milder osteoarthritis of the lateral compartment); and high medial, high lateral (more severe arthritis of the medial and lateral compartments). Continuous variables are given as the mean, with the standard deviation in parentheses. P values represent comparison across all compartment-specific OARSI score combinations, as assessed by the Kruskal-Wallis test. WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain is scaled 0 to 100, with 100 being the worst pain. KOOS ADL (Knee injury and Osteoarthritis Outcome Score activities of daily living) is scaled 0 to 100, with 100 being the best function.
Discussion
We did not observe a clinically important association between preoperative radiographic severity of OA and patient-reported outcomes 2 years following total knee replacement. Subjects with milder and more severe radiographic OA severity demonstrated meaningful and similar pain relief and functional improvement after total knee replacement. Additional sensitivity analyses supported this finding: KL grade, compartment-specific OARSI score, and compartment-specific JSN score were not associated with meaningful differences in pain relief or functional improvement.
Our study elucidates the distinct contributions of joint-space narrowing and compartment-specific tibiofemoral disease, providing a more granular analysis than previous studies. These findings may help clinicians in counseling patients that radiographic OA severity is not predictive of total knee replacement outcome. One should not infer from our findings, however, that evidence of radiographic OA alone is an indication for total knee replacement. Rather, our findings suggest that if total knee replacement is indicated for an individual patient on the basis of multiple clinical criteria, his or her outcome following total knee replacement will not be predicted by preoperative radiographic OA severity.
Our findings are consistent with those of prior literature. In an investigation that included 1,888 patients who underwent total knee replacement, Meding et al. utilized a modified KL grading system that dichotomized radiographic findings as “severe” or “mild,” with severe defined as at least 1 compartment with severe osteophytosis or bone-on-bone changes13. The authors did not find clinically important differences in post-total knee replacement pain and functional improvement between individuals with severe versus mild radiographic arthritis despite identifying some small statistically significant differences.
In a study including 478 patients who underwent total knee replacement, Dowsey et al. utilized a modified KL grading system for radiographic OA assessment10. The key findings of that report were that pain relief was unsatisfactory in about 30% of the cohort and functional improvement was suboptimal in about 50% of the cohort. The authors showed that, at 12 months, the likelihood of having suboptimal pain outcomes was substantially higher among those with less OA radiographic severity. The differences in findings described by Dowsey et al. and those in the current analysis could be explained mainly by the difference in outcomes. Compared with our cohort, the cohort described by Dowsey et al. had much worse outcomes. In addition, we used different pain scales (IKKS [International Knee Society score] in that study versus WOMAC in ours), which may have contributed to the difference in findings.
Other studies have reported on the association between radiographic severity of OA and outcomes of total knee replacement. Kahn et al. reported on outcomes among Osteoarthritis Initiative subjects, demonstrating a very weak correlation between radiographic OA severity and post-total knee replacement patient-reported outcomes11. Keurentjes et al. reported on the association between generic quality-of-life measures and radiographic severity of knee OA12. While the authors showed that higher radiographic severity was associated with better quality of life 2 to 5 years post-total knee replacement, the response rate for the study was <50%, raising questions regarding the generalizability of the findings.
Of note, the presence of joint-space narrowing is typically required to reach higher KL grades, while the OARSI score weights joint-space narrowing, tibial osteophyte presence, and femoral osteophyte presence equally in contribution to the final score. Thus, joint-space narrowing may be given more weight in determining radiographic arthritis severity when KL-based methods are employed than when OARSI-based methods are employed. On the basis of our results and the results of others, it appears that differences in preoperative joint-space narrowing alone may be associated with small differences in patient-reported outcomes after total knee replacement. However, our data and others’ suggest that these differences do not appear to be clinically important.
Some reports did not demonstrate an association between preoperative radiographic OA severity and patient-reported outcomes following total knee replacement. Perry et al. investigated the results of 62 total knee replacements at 2 to 10-year follow-up, finding no difference in Knee Society scores between individuals with milder and more severe preoperative radiographic arthritis as determined by KL grade16. Similarly, Chang et al. reported on the outcomes of 383 total knee replacement procedures at minimum of 1 year of follow-up, observing no association between radiographic OA grade and patient-reported outcomes15. Importantly, the authors noted that all patients in their study had evidence of at least 75% joint-space narrowing, which implies that all patients would likely be classified as KL grade 4 in our study. In addition, the authors utilized the modified Ahlbäck radiographic scoring system, a semiquantitative radiographic assessment that considers a different complement of radiographic findings than does the KL grading system. These studies align with the overall message of our study and others that there do not appear to be clinically important differences in postoperative outcomes between those subjects with milder versus more severe preoperative radiographic arthritis.
Our study had several limitations. First, we did not evaluate all sources of intra-articular damage, especially focal cartilage defects, which may not be apparent on radiographs. Second, tibiofemoral alignment was not assessed, and this is known to be a possible contributor to differential outcome following total knee replacement25,26. However, we assessed the role of compartment-specific OA severity, which may be a proxy for preoperative alignment. Third, this report represents total knee replacements performed at a single high-volume joint replacement center, and the surgeon and patient populations may not be representative of other surgeon and patient populations. Fourth, the decision-making process for undergoing total knee replacement was not assessed in these cases, including the utilization of advanced imaging, which may have illuminated why patients with relatively mild radiographic OA fared as well as those with severe radiographic OA after total knee replacement. Finally, we assessed the severity of baseline radiographic damage in several ways, and assessed several patient-reported outcomes, and we did not adjust for multiple testing. However, we did not find significant associations between OARSI score and patient-reported outcome in any of the primary analyses, so adjustment for multiple testing is not pertinent.
In our cohort, regardless of preoperative radiographic OA severity, subjects experienced clinically meaningful postoperative pain relief and functional improvement. We did not observe a clinically meaningful association between preoperative radiographic OA severity and patient-reported outcomes following total knee replacement. We emphasize that these findings reflect the outcomes of individuals already indicated for total knee replacement surgery, and that radiographic OA assessment should not be utilized alone to indicate a patient for total knee replacement.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A191).
Footnotes
Investigation performed at Brigham and Women’s Hospital, Boston, Massachusetts
Disclosure: This work was supported by grants from the National Institutes of Health (NIH) (grants K24AR057827, P30AR072577, and P60AR047782). On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work and “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJSOA/A190).
References
- 1.American Academy of Orthopaedic Surgeons. AJRR registry annual report 2017. Accessed 2020 Apr 30. http://connect.ajrr.net/2017-annual-report-download [Google Scholar]
- 2.Australian Orthopaedic Association National Joint Replacement Registry. AOANJRR annual report. 2018. Accessed 2020 Apr 30. https://aoanjrr.sahmri.com/annual-reports-2018 [Google Scholar]
- 3.National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 15th annual report. 2018. Accessed 2020 Apr 30. https://www.hqip.org.uk/resource/national-joint-registry-15th-annual-report-2018/#.XqsnqKhKg2w [Google Scholar]
- 4.Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015. September 2;97(17):1386-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009. June 22;169(12):1113-21; discussion 1121-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shan L, Shan B, Suzuki A, Nouh F, Saxena A. Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Am. 2015. January 21;97(2):156-68. [DOI] [PubMed] [Google Scholar]
- 7.Choi YJ, Ra HJ. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res. 2016. March;28(1):1-15. Epub 2016 Feb 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018. September 5;100(17):1455-60. [DOI] [PubMed] [Google Scholar]
- 9.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15 Suppl A:A1-56. [DOI] [PubMed] [Google Scholar]
- 10.Dowsey MM, Nikpour M, Dieppe P, Choong PF. Associations between pre-operative radiographic changes and outcomes after total knee joint replacement for osteoarthritis. Osteoarthritis Cartilage. 2012. October;20(10):1095-102. Epub 2012 Jul 16. [DOI] [PubMed] [Google Scholar]
- 11.Kahn TL, Soheili A, Schwarzkopf R. Outcomes of total knee arthroplasty in relation to preoperative patient-reported and radiographic measures: data from the Osteoarthritis Initiative. Geriatr Orthop Surg Rehabil. 2013. December;4(4):117-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keurentjes JC, Fiocco M, So-Osman C, Onstenk R, Koopman-Van Gemert AW, Pöll RG, Kroon HM, Vliet Vlieland TP, Nelissen RG. Patients with severe radiographic osteoarthritis have a better prognosis in physical functioning after hip and knee replacement: a cohort-study. PLoS One. 2013;8(4):e59500. Epub 2013 Apr 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meding JB, Ritter MA, Faris PM, Keating EM, Harris W. Does the preoperative radiographic degree of osteoarthritis correlate to results in primary total knee arthroplasty? J Arthroplasty. 2001. January;16(1):13-6. [DOI] [PubMed] [Google Scholar]
- 14.Peck CN, Childs J, McLauchlan GJ. Inferior outcomes of total knee replacement in early radiological stages of osteoarthritis. Knee. 2014. December;21(6):1229-32. Epub 2014 Sep 6. [DOI] [PubMed] [Google Scholar]
- 15.Chang CB, Yoo JH, Koh IJ, Kang YG, Seong SC, Kim TK. Key factors in determining surgical timing of total knee arthroplasty in osteoarthritic patients: age, radiographic severity, and symptomatic severity. J Orthop Traumatol. 2010. March;11(1):21-7. Epub 2010 Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perry KI, Strasser NL, Harmsen WS, Pagnano MW, Trousdale RT. Minimal preoperative degenerative arthritis may not predict poor TKA outcome. Orthopedics. 2015. August;38(8):e681-4. [DOI] [PubMed] [Google Scholar]
- 17.Losina E, Collins JE, Wright J, Daigle ME, Donnell-Fink LA, Strnad D, Usiskin IM, Yang HY, Lerner V, Katz JN. Postoperative care navigation for total knee arthroplasty patients: a randomized controlled trial. Arthritis Care Res (Hoboken). 2016. September;68(9):1252-9. Epub 2016 Jul 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klara K, Collins JE, Gurary E, Elman SA, Stenquist DS, Losina E, Katz JN. Reliability and accuracy of cross-sectional radiographic assessment of severe knee osteoarthritis: role of training and experience. J Rheumatol. 2016. July;43(7):1421-6. Epub 2016 Apr 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957. December;16(4):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988. December;15(12):1833-40. [PubMed] [Google Scholar]
- 21.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003. May 25;1:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Defining adult overweight and obesity. 2017. Accessed 2020 Apr 30. https://www.cdc.gov/obesity/adult/defining.html [Google Scholar]
- 23.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan LM. Essentials of biostatistics in public health. Jones & Bartlett Learning; 2017. [Google Scholar]
- 25.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009. September;24(6)(Suppl):39-43. Epub 2009 Jun 24. [DOI] [PubMed] [Google Scholar]
- 26.Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, Meding JB. Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am. 2013. January 16;95(2):126-31. [DOI] [PubMed] [Google Scholar]