Abstract
Background:
The Portuguese mental health care plan emphasizes that health care professionals can be a source of stigma against people with mental illness enhancing self-stigma and leading to a decrease in the search for help and adherence to treatment.
Methods:
In this exploratory study, we surveyed 111 first and last year students from the Faculty of Medicine of the University of Porto, Portugal, using the Portuguese version of the Attribution Questionnaire AQ-27 to assess the attitudes toward mental illness.
Results:
The students showed a significant difference in the segregation dimension, and in some items related with pity and coercion in the end of the course. These results express a positive will to integrate people with mental illness in community, a decrease of pity and a valorization of the pharmacological treatment in this kind of disease. The previous personal experience of psychiatric problems decreases the level of segregation and psychological problems increase the motivation to help.
Conclusion:
Final-year students express more positive and less discriminatory attitudes toward people with severe mental illness than first-year students. This is likely due to education and contact opportunities promoted throughout the medical school, as well as due to the experience of having gone to a psychology or psychiatric consultation. Knowledge of stigma levels of future medical doctors is therefore crucial for the prevention of attitudes that could condition the provision of medical care.
Keywords: medical students, social stigma, mental illness
Introduction
Stigma is a global problem with severe implications in the lives of people who suffer from mental illness and those around them. It is a public health problem and it leads to loss of productivity and employability.1
Stigma can be defined in several ways. Some authors describe it as a feature that discredits and diminishes the person to a level where he is not considered suitable to live in society. The feature can be a physical dysfunction or deformity, a mental illness, a race, tribe, group, or ethnicity. It means the person is seen to be unable to have normal social interactions, or even being dangerous or unpredictable, being set apart and ignored by the group. Other authors propose 6 dimensions of the feature leading to stigmatization: whether it is easy to recognize by others; whether it is a short- or long-time situation; how it affects the social interaction; the subjective perception of the characteristic; its origin—whether it is caused by the individual; and whether it induces dangerous or threatening feelings.2
According to Corrigan et al3,4 and stigma can be divided in public stigma and self-stigma, and it is composed by 3 elements: stereotypes associated with misinformation or lack of information; prejudice as a problem of attitudes, experiencing negative feelings; and discrimination that comes from prejudice and is a problem of behavior toward himself or another person.
Public stigma consists in the way that a society faces the person with mental illness and is associated with stereotypes and the subsequent negative expectations, such as incompetence, lack of moral character, dangerousness, and blameworthiness.3,4 Society's beliefs often limit job opportunities, independent life with private housing or education to people with mental illness, which creates the biggest obstacles to their well-being, health, and quality of life.5,6,7
These attitudes also limit the rehabilitation and reinsertion in the community of those that were institutionalized and wish to return to a normal society life, directly affecting a satisfactory course of the disease.5
Self-stigma was described by Corrigan et al as the “why try” effect. It leads to depreciation with consequences like low self-esteem and giving up on personal goals in education, relationships or economic independence once they believe they are not able to correspond to the society's expectations.3,6,7 Self-stigma also discourages the person with mental illness from seeking and adhering to treatment, inhibiting the will to recover and overcome the challenges of the illness.1,7,8
Stigma is also one of the reasons indirectly appointed for the decreased life expectancy of people with mental illness disorders, adding to a complex number of factors such as higher risk factors for chronic diseases and some types of cancer, the iatrogenic effects of medications, and higher rates of suicide, accidental, and violent death. There is evidence that people with mental illness have poorer access to physical healthcare and receive worse treatment for physical disorders when compared with the general population, a phenomenon called, “diagnostic overshadowing.” Medical staff tend to treat physical illnesses of people with mental illness less thoroughly and less effectively. This may happen as a direct consequence of health professionals being poorly informed and misattributing physical symptoms to a mental disorder. It can also be an undeliberate act, guided by a negative stereotype.9
In this context, it is vital to consider how healthcare professionals handle stigma in their daily work, as they often present the same negative attitudes and stigma as the rest of the community.5,7,10,11
Some studies show that the close contact with people with mental illness is much more effective in promoting acceptance as changing attitudes in the general population and, particularly, specifically in high school and medical students. Moreover, interpersonal contact—either directly or indirectly (eg, by video call) produces greater improvements than just theoretical contents.4,5,10,12,13 Therefore, subjects such as medical psychology or psychiatry are essential in medical schools.
Several recent studies suggest that psychiatry clerkship training has a positive effect in reducing stigma toward mental illnesses.14,15,16,17,18,19,20 The impact of different populations and student-based interventions was also accessed, showing improvements in the attitudes in a short-term evaluation. In a long-term follow-up, results are, however, inconsistent, showing a decrease in the initial benefits of the intervention.10,11,21 Some authors argue that medical school education has little effect on nonstigmatized attitudes and long-term contact with people with mental illness does not necessarily modify negative attitudes.22,23,24 Also, interventions have been shown not to reach enough people to modify the public stigma associated with a population.4,12
Contact is also an important step against self-stigma because the more people with mental illness believe that they are going to be stigmatized and discriminated, the more they hide their disease and withdraw from contact, social interaction, and help and the more they avoid society.25 This is also true psychiatric problems of medical students and doctors. Despite possessing positive attitudes toward persons with mental illness, they delay seeking mental health services themselves, often only doing so in a crisis situation, for fear of exposure to stigmatization from peers.20,26
Negative views regarding psychiatry as a career and psychiatric illness have been found in studies from Nigeria, India, UK,27 China,22 Poland,23 and Iran.24 Conversely, students from Kenya and Pakistan,27 USA,17 Czech Republic,14 Greece,15 Canada,16 Taiwan,18 Singapore,24 and Australia27 reported more positive views regarding attitudes to psychiatry, and so psychiatric illness. These studies do not appear to show clear differences between developed and developing countries.
In Portugal, only one study was found looking at attitudes toward mental illness among medical students.21 Medical students from the University of Lisbon surveyed in this study showed better attitudes toward the patients with mental illness at the end of the course than in first year. The authors proposed that the positive effect found at the end of the third year were due to a very specific antistigma module, integrated in the third-year discipline “Introduction to Mental Health.”21
The present study aims to assess the differences of mental stigma attitudes and behaviors against people with mental illness, comparing students from different years in the Faculty of Medicine of the University of Porto, in Portugal.
Methods
Instruments
A 2-part questionnaire was used to obtain data for this study: the first part covering sociodemographic data and the second part consisting of the Attribution Questionnaire AQ-27 (preliminary version in Portuguese approved for use by the author of the original instrument). The sociodemographic part was used to evaluate sex, age, marital status, study year, place of birth, attendance in psychological or psychiatric consultations and its location, and contact with people with mental illness.
The AQ-27 questionnaire evaluates 9 dimensions of stigma: Responsibility (people with mental illness can control their symptoms and are responsible for having the illness); Pity (people with mental illness are overtaken by their own disorder and therefore deserve concern and pity); Anger (people with mental illness are blamed for having the illness and provoke wrath and rage); Dangerousness (people with mental illness are not safe); Fear (people with mental illness are dangerous); Help (people with mental illness need assistance); Coercion (people with mental illness have to participate in treatment management); Segregation (people with mental illness are sent to institutions separated from the community); and Avoidance (patients with mental illness do not live in society). Corrigan28 has associated some of these constructs with discriminative attitudes (responsibility, dangerousness, fear, anger, coercion, segregation, and avoidance) and others with attitudes of closeness and assistance (help and pity).29
The AQ-27 questionnaire has different vignettes with variations in the characteristics of the mental illness assessed, especially severity of the condition. In this case we decided to use schizophrenia, because it is easily identified as a serious mental illness by students. This vignette is followed by 27 questions intended to evaluate the students’ attitudes, behavioral intentions and affective responses in a score from 1 “no or nothing” to 9 “very much or completely.” Results are calculated considering the mean scores obtained for the items in each dimension. Questions in the avoidance dimension are reversely scored.
Procedure
The survey was undertaken online between May and June 2014. It was advertised to the students in the Faculty of Medicine of the University of Porto, who answered anonymously. Students were informed of the aims of the study and consented to the use of information. The survey was advertised to 490 students: 245 first-year and 245 sixth-year students.
As our research collects data on personal and socially sensitive topics, we also considered the impact of Socially Desirable Responding (SDR) bias on the validity of the questionnaire. SDR is the tendency for people to present a favorable image of themselves in questionnaires, which results in over-reporting of socially desirable responses and under-reporting of socially undesirable responses. The following methods were used to reduce SDR bias: anonymous responses, data collection through online surveys (instead of phone or face-to-face surveys), and informing respondents on the confidentially of their responses.
Our sample is not probabilistic by convenience and the results were analyzed using the PASW Statistics software version 21. Categorical variables are presented as frequencies and percentages, while continuous variables are presented as means and standard deviations, or medians and interquartile ranges for variables with skewed distributions. All reported P values are 2-tailed, with a P value of .05 indicating statistical significance. Normal distribution was checked using Shapiro-Wilk test of skewness and kurtosis and continuous variables were compared with the use of the Student t test.
Results
A total of 111 students answered the questionnaire, corresponding to a response rate of 25% amongst first-year students and 17% amongst sixth-year students. The majority of the students were female 79 (71.2%) and 32 (28.8%) were male. There were 61 first-year students (55%) and 50 sixth-year students (45%) who had already attended the psychiatry internship. They were all single and aged between 18 and 27 (mean = 21.1, standard deviation = 2.67).
With regard to the experience of having attended a psychology consultation, 65 (58.6%) students said they never went and 46 (41.4%) did, mostly in hospitals and private practices. In the case of psychiatric consultations, 89 (80.2%) never had a consultation, whereas 22 (19,8%) did, mostly in private practices.
The great majority of the respondents 102 (91.9%) did not report self-perception of mental illness. Concerning familiarity with mental illness, 60 (54.1%) respondents said they know someone with this kind of pathologies—37 (33.3%) a first-degree relative—whereas 46 (41.4%) did not know anyone with a mental illness.
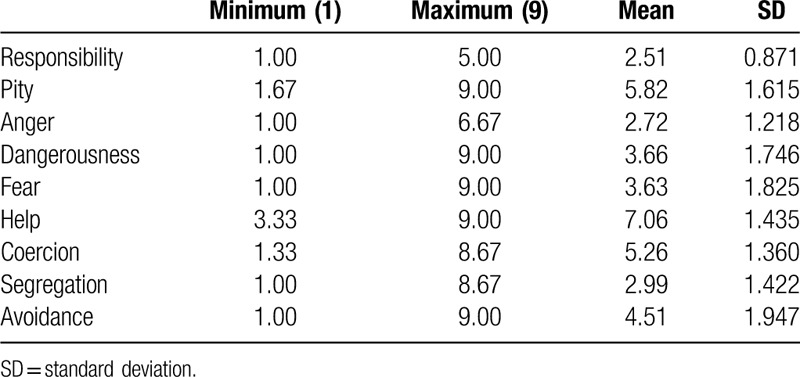
Table 1 shows the mean values for each dimension in the AQ-27 questionnaire. The item with the highest score was Help with a mean value of 7 and a minimum of 3. Responsibility had the lowest score, with a mean of 2.5 and a maximum of 5. Pity, Coercion, and Avoidance had also higher scores (means >4) than Dangerousness, Fear, Segregation, and Anger, in descending order.
Table 1.
Means obtained for each dimension in the AQ-27
The comparative parametric tests that revealed statistically significant differences will be analyzed in detail.
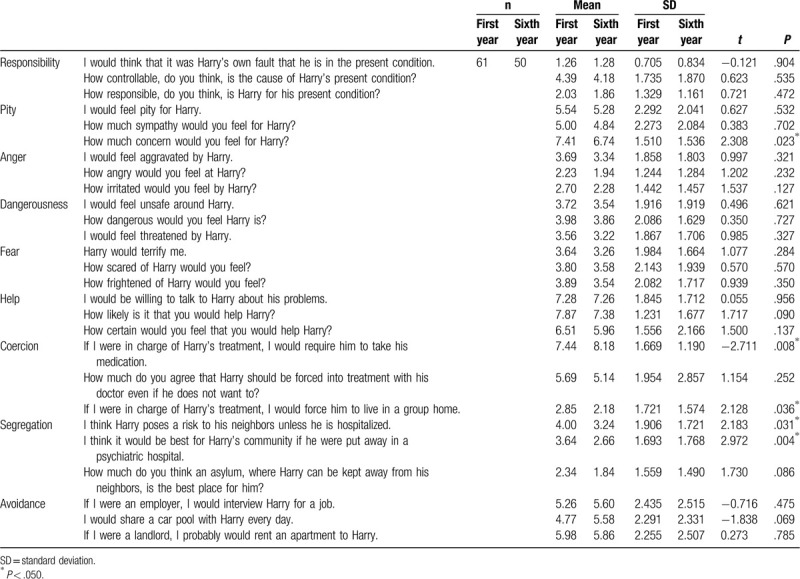
When comparing the first and sixth years across the different dimensions, although mean scores for the sixth year are always lower, only Segregation showed a statistically significant difference, with P = .005 (Table 2). Looking at each item of the AQ-27 questionnaire (Table 3) there is significant difference in 2 indicators of Segregation (lower mean in sixth-year students): “I think Harry poses a risk to his neighbors unless he is hospitalized” (P = .031) and “I think it would be best for Harry's community if he were put away in a psychiatric hospital” (P = .004). Two items of Coercion—“If I were in charge of Harry's treatment, I would require him to take his medication” (P = .008) and “If I were in charge of Harry's treatment, I would force him to live in a group home” (P = .036)—were also significant, with the former showing a bigger score in the sixth year and the latter showing a lower score in the first year. “How much concern would you feel for Harry?” as an indicator of Pity was significantly higher in the first year (P = .023).
Table 2.
Comparison of means according to the year
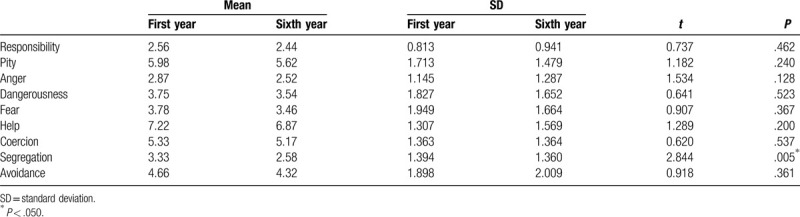
Table 3.
Comparison of means using T test accordingly to the year of studies related to each item of AQ-27
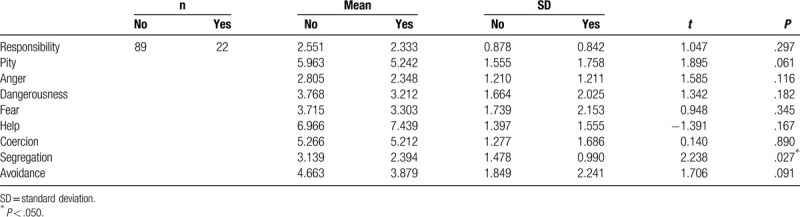
When analyzing the experience of having gone to a psychology consultation, there are several differences in the Help dimension, with significantly higher score (P = .018), as shown in Table 4. The students who had gone to a psychiatric consultation had a significantly lower segregation score with P = .027 (Table 5).
Table 4.
Comparison of means using T test accordingly to experience of having gone to a psychological consultation related to the dimensions of AQ-27
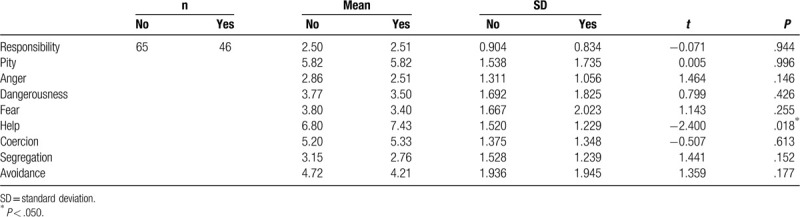
Table 5.
Comparison of means using T test accordingly to experience of having gone to a psychiatric consultation related to the dimensions of AQ-27
Discussion
This study aimed at understanding the differences in mental stigma attitudes and behaviors among medical students in the first and final years of their course. Stigma is still prevalent in health care professionals, who can promote self-stigma and, therefore, affect treatment and recover of patients with mental illness.
Our data comparing the 9 dimensions of the AQ-27 questionnaire demonstrates a significant decrease in Segregation throughout the course of the medical degree. This means that sixth-year students, who had already had the psychiatric internship, had a higher tendency to include people with mental illness in the community. Portugal was one of the countries that created policies to the deinstitutionalization of patients with mental illness toward rehabilitation in the society.30 Therefore, devaluing the need for institutionalization is consistent with the Portuguese mental health plan.
Sixth-year students demonstrated less Pity for people with mental illness, which can support the fact that those students have more information and education about mental illness.8 Education by itself can be an important strategy to decrease stigma, as referred in a review by Yamaguchi et al,31 through better understanding of the disease and the existence of treatment.31
The indicators of Coercion, specifically “If I were in charge of Harry's treatment, I would require him to take his medication” demonstrates the medical mentality acquired during the medical degree. Students learn how to help others, usually through medication. The importance of carrying on the prescription and attending appointments is deeply rooted, as well as the knowledge that patients frequently abandon their treatment, particularly when it is a chronic one, as they usually are in mental illness.
The other difference found was in the Help and Segregation dimensions in people with the experience of having gone to a psychology or psychiatric consultation. These results are also in accordance with the literature in that the familiarity with the situation diminishes the levels of stigma and discrimination.5,32 It is also stated that the contact with a close situation, in this case with the self, is intimately related to predisposition to help people with mental illness.33,34 This difference in Help was also showed in a Portuguese study with university students conducted by Barbosa.35
Results of this study are not directly comparable with previous research on medical students from the University of Lisbon carried out by Telles-Correia et al,21 due methodological differences.
A similar finding in both studies was, however, the small but significant improvement in scores after specific education interventions about psychiatry and antistigma psychiatric illnesses. The universities of Lisbon and Porto have different medical course structures, with the Porto degree offering contact with mental illness in 2 main moments, in the fifth and sixth years. If the first one is more theoretical and with more indirect contact (eg, observing appointments), the second moment offers closer contact with patients. Students interact directly with inpatient and ambulatory patients and have antistigma lectures.
These findings are in accordance with the literature, which established that both theoretical education and contact with people suffering from mental diseases are effective factors in changing attitudes and stigma during psychiatrics internships.4,10,11,12,14,15,17,18,19 Results reinforce the importance of a prolonged contact, in more than 1 moment, integrating the subjects in different years and multiple classes in each year.36,37
Furthermore, the absence of changes in the majority of our dimensions in the end of the course suggests medical education had little effect on globally reducing stigma. These findings are consistent with other studies that show stigma appears to be countered less with training and formal education than by personal experiences or preferences in medical students. It was also showed that, despite increasing the contact with people with mental illness during the psychiatric clerkship, the attitudes were not improved.
The main limitations of our study were the cross-sectional approach and a very small sample obtained that could have been augmented if more than one medical school was included in the study or if we had considered students from different academic years.
As previously mentioned, we implemented strategies to reduce SDR bias, but it is important to mention that our sample (medical students) is a population with high levels of Social Desirability, particularly in health-related topics. Expectations of community and of themselves may led them to distort their answers and “act the way a future doctor should act.” Another limitation associated with this investigation is that the increase in family error rate across the reported statistical analyses was not controlled.
One other problem to consider was the lack of specification to which kind of psychological consultation people where referring, since it is common to have appointments of vocational guidance in high school, and its frequency to understand if it was sporadic or a regular appointment. We also consider that would have been interesting to characterize our population regarding some other sociodemographic variables to better understand the previous contacts with mental health and anti-stigma interventions.
The data revealed a positive reduction in Segregation when the students finish their course as well as improvement in some indicators of Pity and Coercion. Familiarity with mental illness was also associated with less stigma. The absence of significant improvement in the other dimensions of stigma suggests that the medical course does not have the power to change attitudes and stigma as ideally would. With this in mind, it would be important to identify constraints that are limiting the change of in future doctors’ attitudes.
For the future, it would be interesting to transform the cross-sectional study in a follow-up study, analyzing the same students from the start until the end of the course. It could also be of value to complement our study through evaluation of stigma in the Portuguese medical community and in other health professionals.
Acknowledgements
Relating to this article.
Conflicts of interest
The authors declare no conflicts of interest.
References
- [1]. Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42:1741–1752. [DOI] [PubMed] [Google Scholar]
- [2]. Brohan E, Slade M, Clement S, Thornicroft G. Experiences of mental illness stigma, prejudice and discrimination: a review of measures. BMC Health Serv Res. 2010;10:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Corrigan PW, Shapiro JR. Measuring the impact of programs that challenge the public stigma of mental illness. Clin Psychol Rev. 2010;30:907–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr Serv. 2012;63:963–973. [DOI] [PubMed] [Google Scholar]
- [5]. Martinez-Zambrano F, Garcia-Morales E, Garcia-Franco M, et al. Intervention for reducing stigma: Assessing the influence of gender and knowledge. World J Psychiatry. 2013;3:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Crabtree JW, Haslam SA, Postmes T, Haslam C. Mental health support groups, stigma, and self-esteem: positive and negative implications of group identification. J Soc Issues. 2010;66:553–569. [Google Scholar]
- [7]. Michaels PJ, López M, Rüsch N, Corrigan P. Constructs and concepts comprising the stigma of mental illness. Psychol Soc Educ. 2012;4:183–194. [Google Scholar]
- [8]. Sousa SD, Marques A, Rosário C, Queirós C. Stigmatizing attitudes in relatives of people with schizophrenia: a study using the Attribution Questionnaire AQ-27. Trends Psychiatry Psychother. 2012;34:186–197. [DOI] [PubMed] [Google Scholar]
- [9]. Thornicroft G. Physical health disparities and mental illness: the scandal of premature mortality. Br J Psychiatry. 2011;199:441–442. [DOI] [PubMed] [Google Scholar]
- [10]. Friedrich B, Evans-Lacko S, London J, Rhydderch D, Henderson C, Thornicroft G. Anti-stigma training for medical students: the Education Not Discrimination project. Br J Psychiatry Suppl. 2013;55:s89–s94. [DOI] [PubMed] [Google Scholar]
- [11]. Kassam A, Glozier N, Leese M, Loughran J, Thornicroft G. A controlled trial of mental illness related stigma training for medical students. BMC Med Educ. 2011;11:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Corrigan PW. Research and the elimination of the stigma of mental illness. Br J Psychiatry. 2012;201:7–8. [DOI] [PubMed] [Google Scholar]
- [13]. Eksteen H-C, Becker PJ, Lippi G. Stigmatization towards the mentally ill: perceptions of psychiatrists, pre-clinical and post-clinical rotation medical students. Int J Soc Psychiatry. 2017;63:782–791. [DOI] [PubMed] [Google Scholar]
- [14]. Janousková M, Weissová A, Formánek T, Pasz J, Motlová LB. Mental illness stigma among medical students and teachers. Int J Soc Psychiatry. 2017;63:744–751. [DOI] [PubMed] [Google Scholar]
- [15]. Economou M, Kontoangelos K, Peppou LE, et al. Medical students’ attitudes to mental illnesses and to psychiatry before and after the psychiatric clerkship: training in a specialty and a general hospital. Psychiatry Res. 2017;258:108–115. [DOI] [PubMed] [Google Scholar]
- [16]. Sandhu HS, Arora A, Brasch J, Streiner DL. Mental Health Stigma: Explicit and Implicit Attitudes of Canadian Undergraduate Students, Medical School Students, and Psychiatrists. Can J Psychiatry. 2018;64:209–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. Chiles C, Stefanovics E, Rosenheck R. Attitudes of students at a US medical school toward mental illness and its causes. Acad Psychiatry. 2016;41:320–325. [DOI] [PubMed] [Google Scholar]
- [18]. Wang PW, Ko CH, Chen CS, et al. Changes of explicit and implicit stigma in medical students during psychiatric clerkship. Acad Psychiatry. 2016;40:224–228. [DOI] [PubMed] [Google Scholar]
- [19]. Shen Y, Dong H, Fan X, et al. What can the medical education do for eliminating stigma and discrimination associated with mental illness among future doctors? Effect of clerkship training on Chinese students’ attitudes. Int J Psychiatry Med. 2014;47:241–254. [DOI] [PubMed] [Google Scholar]
- [20]. Chang S, Ong HL, Seow E, et al. Stigma towards mental illness among medical and nursing students in Singapore: a cross-sectional study. BMJ Open. 2017;7:e018099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Telles-Correia D, Marques JG, Gramaça J, Sampaio D. Stigma and attitudes towards psychiatric patients in Portuguese medical students. Acta Med Port. 2015;28:715–719. [DOI] [PubMed] [Google Scholar]
- [22]. Zhu Y, Zhang H, Yang G, et al. Attitudes towards mental illness among medical students in China: Impact of medical education on stigma. Asia Pac Psychiatry. 2017;10:e12294. [DOI] [PubMed] [Google Scholar]
- [23]. Kopera M, Suszek H, Bonar E, et al. Evaluating explicit and implicit stigma of mental illness in mental health professionals and medical students. Community Ment Health J. 2015;51:628–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Amini H, Shoar S, Tabatabaee M, Arabzadeh S. The effect of clinical exposure to patients on medical students’ attitude towards mental illness. Iran J Psychiatry Behav Sci. 2016;10:e1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25]. Evans-Lacko S, London J, Japhet S, et al. Mass social contact interventions and their effect on mental health related stigma and intended discrimination. BMC public health. 2012;12:489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Hankie AK, Northall A, Zaman R. Stigma and mental health challenges in medical students. BMJ Case Report. 2014;bcr2014205226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Lyons Z, Laugharne J, Laugharne R, Appiah-Poku J. Stigma towards mental illness among medical students in Australia and Ghana. Acad Psychiatry. 2014;39:305–308. [DOI] [PubMed] [Google Scholar]
- [28]. Corrigan P. Attribution questionnaire (AQ-27). Available at: http://www.stigmaandempowerment.org/resources. Accessed October 2011. [Google Scholar]
- [29]. Sousa S, Queirós C, Marques A, Rocha N, Fernandes A. Versão preliminar portuguesa do AttributionQuestionnaire (AQ-27), adaptada com autorização de P. Corrigan. Porto: FPCEUP/ESTSPIPP; 2008. [Google Scholar]
- [30]. CNRSSM Proposta de Plano de Acção para a Reestruturação e Desenvolvimento dos Serviços de Saúde Mental em Portugal. Lisboa: Ministério da Saúde; 2007. [Google Scholar]
- [31]. Yamaguchi S, Mino Y, Uddin S. Strategies and future attempts to reduce stigmatization and increase awareness of mental health problems among young people: a narrative review of educational interventions. Psychiatry Clin Neurosci. 2011;65:405–415. [DOI] [PubMed] [Google Scholar]
- [32]. Mino Y, Yasuda N, Tsuda T, Shimodera S. Effects of a one-hour educational program on medical students’ attitudes to mental illness. Psychiatry Clin Neurosci. 2001;55:501–507. [DOI] [PubMed] [Google Scholar]
- [33]. Pinfold V, Toulmin H, Thornicroft G, Huxley P, Farmer P, Graham T. Reducing psychiatric stigma and discrimination: evaluation of educational interventions in UK secondary schools. Br J Psychiatry. 2003;182:342–346. [DOI] [PubMed] [Google Scholar]
- [34]. Corrigan P, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44:162–179. [PubMed] [Google Scholar]
- [35]. Barbosa T. Estigma Face à Doença Mental por Parte de Futuros Profissionais de Saúde Mental. Porto: F P C E U P; 2010. [Google Scholar]
- [36]. Corrigan PW, River PP, Lundin RK. Three strategies for changing attributions about severe mental illness. Schizophr Bull. 2001;27:187–195. [DOI] [PubMed] [Google Scholar]
- [37]. Martins V. Eficácia do Programa Anti-estigma “Porta Aberta à Saúde Mental” na Comunidade Escolar Juvenil: Estudo Exploratório. Porto: F P C E U P; 2014. [Google Scholar]


