Highlights
-
•
Knockdown of TGF-β1 gene expression by shRNA inhibited PRRSV replication in pig immune cells and increased the viability of infected cells.
-
•
Silencing TGF-β1 gene expression by shRNA enhanced the antiviral immunity and reduced PRRSV yield in the infected cells.
-
•
Silence of TGF-β1 gene expression by shRNA can facilitate the control of PRRSV infection in pigs.
Keywords: Tibetan pig, RNAi, TGF-β1 gene, PRRSV, Immune genes expression
Abstract
Transforming growth factor beta 1 (TGF-β1) was of importance in the pathogenesis of porcine reproductive and respiratory syndrome virus (PRRSV). To determine whether knockdown of TGF-β1 gene expression could facilitate the control of PRRSV infection, specific sequences for expressing shRNA targeted to porcine TGF-β1 gene were synthesized and cloned into pSilencer 3.1-H1 neovector. Then they were used to transfect peripheral blood mononuclear cells of Tibetan pig (Tp-PBMCs) followed by PRRSV inoculation. The positive recombinant plasmids were screened for inhibition of TGF-β1 gene expression by real-time quantitative RT-PCR. Conversely, the mRNA level of PRRSV in shRNA treated Tp-PBMCs dramatically decreased, and there were significant increases of the transcription of immune genes, such as interleukin-2 (IL-2), interleukin-4 (IL-4), interferon-alpha (IFN-α), interferon-gamma (IFN-γ), tumor necrosis factor-alpha (TNF-α), toll-like receptor 3 (TLR3), toll-like receptor 7 (TLR7), Myeloid differentiation primary response gene (88) (MyD88), and interleukin-27p28 (IL-27p28). However, the expressions of IL-8 and IL-10 genes significantly reduced in comparison to the control infected cells. In addition, transfection with the shRNA plasmids significantly elevated the viability of immune cells. Therefore the knockdown of TGF-β1 gene expression by shRNA not only inhibits the replication of PRRSV but also improves immune responsiveness following viral infection, suggesting a novel way to facilitate the control of PRRSV infection in pigs.
1. Introduction
Porcine reproductive and respiratory syndrome virus (PRRSV) is an enveloped, single-stranded positive-sense RNA virus, belonging to the family Arteriviridae, genus Rodartevirus (Kuhn et al., 2016). This highly variant virus can cause respiratory disease, abortions, and secondary viral and/or bacterial infection of all-aged pigs, resulting in long-term infection and widespread complex disease by inhibiting immune defense of host, and have been causing major economic lose worldwide (Li et al., 2016). Some viral proteins are multifunctional to not only maintain viral structure but also modulate immune response to facilitate viral survival by changing the numbers and functions of immune cells, including promoting the production of TGF-β and IL-10 to impair the equilibrium of pro-inflammatory cytokines and anti-inflammatory cytokines, and summoning non-neutralizing antibody instead of neutralizing antibody (Dwivedi et al., 2012; Gómezlaguna et al., 2012; Huang & Meng, 2010).
TGF-β contributes greatly to maintain immune homeostasis and tolerance through regulating the differentiation, proliferation and activity of multiple leukocyte lineages, and inhibiting the production and signaling of effector cytokine in Smad-dependent and -independent mechanisms (Zhang, 2009). Actually, both PRRSV-1 and PRRSV-2 have been demonstrated to induce over expression of TGF-β, in order to unbalance immune system, disarm host surveillance and finally benefit viral survival (Gómezlaguna et al., 2012; Renukaradhya, Alekseev, Jung, Fang, & &Saif, 2010; Silva-Campa et al., 2009). Among three TGF-β isoforms, TGF-β1 is predominant in immune system that has potent immunoregulatory properties like IL-10 (Gómezlaguna et al., 2012; Gorelik, 2000; Yoshimura, Wakabayashi, & Mori, 2010), and it is able to inhibit macrophage activation by inhibiting IFN-γ synthesis and promoting IL-10 production (Gómezlaguna et al., 2012). In contrast, TGF-β2 and TGF-β3 are mainly expressed in mesenchymal tissues and bones (Gorelik, 2000).
As a result, so we wonder whether knocking-down TGF-β gene expression can benefit immune cells to control PRRSV infection. So far, unfortunately, the effect of down-regulation of TGF-β1 on PRRSV infection is rarely observed. Therefore, in this experiment, RNAi was exploited to reduce TGF-β1 expression and subsequently evaluate its effect on PRRSV replication and anti-viral immune responses
2. Materials and methods
2.1. Preparations of peripheral blood mononuclear cells
Peripheral blood of healthy Tibetan pigs were collected from the superior vena cava in 5-mL tubes (Kangjian, Jiangsu) containing K2-EDTA as the anti-coagulant, and Tp-PBMCs were isolated by density gradient centrifugation (550 g, 20 min) in separation medium for mononuclear cells of pigs (HaoYang, Tianjin). After 2x washes in Hanks’ balanced salt solution without Ca2+/Mg2+ and 2% fetal bovine serum (FBS), cells were suspended at a concentration of no more than 6 × 106 cells/mL in RPMI 1640 medium, supplemented with 1% (vol/vol) penicillin/streptomycin mixture and 10% (vol/vol) heat-inactivated FBS (all from Hyclone, Beijing). The cells were incubated in Cell Repel plates (Eppendorf company, Germany) at 37 °C in 5% CO2 for 12 h before use. The ratio of monocytes in the cultured cells before transfection was checked by the flow cytometry with 0.5 ug/ml mouse anti-CD14 monoclonal anitbody following the recommended protocol (Abcam, ab186689, America).
2.2. Construction of shRNA expressing plasmid
Short interfering hairpin ODNs were designed based on porcine TGF-β1 mRNA (NM_214,015) using online siRNA design software (http://jura.wi.mit.edu/bioc/siRNA; http://www.ambion.com/techlib/misc/siRNA_finder.html). The four selected sequences were listed in Table 1. The sequences (Table 1) were synthesized by Invitrogen (Shanghai) and cloned into the vector pSilencer 3.1-H1 puro (Biovector Science Lab Inc.). Escherichia coli DH5α were transformed with the recombinant plasmids (shIL10Rα−1~4), which were then amplified in LB medium supplemented with 60 µg/mL ampicillin. The plasmids were then isolated using Plasmid Mini Kit I (Omega) and verified by restriction analysis with BamH I and Hind III (Takara, Dalian), and by nucleotide sequencing (BGI, Beijing). As the core sequence of the vector had no target in the Refseq mRNA of Sus scrofa (Taxid: 9823, NCBI), it was set as a negative control (pNeg). All plasmids for transfection contained <0.125 EU/mL endotoxin as assayed by Tachypleus Amebocyte Lysate test kit (A&C Biological Ltd, Zhanjiang).
Table 1.
Sequences of ODNs for generation of shTGFβ1-1~4.
| Designation | Location (bp) | Sequence (5′−3′) |
|---|---|---|
| shTGFβ1-1 | 1418~1436 | CCAGAAATACAGCAATGAT |
| shTGFβ1-2 | 1295~1312 | CTTATATATGCTGTTCAA |
| shTGFβ1-3 | 1256~1273 | CAACCAAATCTATGATAA |
| shTGFβ1-4 | 1586~1603 | CAAAGATAACACACTCCA |
2.3. Transfection of tp-pbmcs with shTGFβ1
The transfection mixtures were prepared according to the manufacturer's instructions. Briefly, 4 μg individual plasmid (shTGFβ1-1~4 and pNeg) or 10 μL cationic liposome transfection reagent DMRIE-C (Invitrogen, USA) was diluted in Opti-MEM I Reduced Serum Medium (Invitrogen, USA) to 500 μL. Following 5 min at ambient temperature, the plasmids were added to the diluted transfection reagent. Brief mixing at ambient temperature for 30 min formed the transfection complex completely. During this period, the Tp-PBMCs were prepared for transfection. Cells were centrifuged at 550 g for 15 min, and washed with serum-free RPMI 1640 without antibiotics. The Tp-PBMCs were re-suspended in serum-free RPMI 1640 without antibiotics at 1.5 × 107 cells per mL and 0.2 mL aliquots (3 × 106 cells) were added to each well of a 6-well culture plate. The transfection complex was added and mixed with cells, then incubated at 37 °C, 5% CO2 for 4.5 h, 2 mL pre-warmed RPMI 1640 containing 15% FBS and 1.5% penicillin/streptomycin mixture was added to the Tp-PBMCs with 10 μL PRRSV(JXA1 strain, gene type II, its infection dose was 107.5 TCID50/ml) per 1 mL medium. Cells were again incubated at 37 °C, 5% CO2, and Tp-PBMCs were collected daily for 3 days as followings: after centrifuge at 10,000 g for 30 s, the cell pellets were lysed by 1 mL RNAisoplus (Takara, Dalian) and frozen at −80 °C before RNA isolation. The negative control cells transfected with only 4 μg shTFGβ1-1 or pNeg, and blank control cells without plasmid and the virus were also cultured and processed in the same way.
The viability of PBMCs was assayed by 7-Sea CCK-8 (7-Sea, Shanghai), following the manufacturer's instructions. In brief, treated Tp-PBMCs were added at the concentration of 3 × 105 cells per 100 μL RPMI 1640 complete medium to each well with 100μL CCK8. The cells were oscillated for 30 s and incubated at 37 °C, 5% CO2 for 4 h, and its absorbance was read by the microplate reader Model 680 (BIO-RAD) at 480 nm. The viability was checked every 24 h until 72 hpi.
2.4. RNA isolation for reverse transcription pcr
RNA was isolated following the manufacturer's instructions of RNAisoplus (Takara, Dalian). The RNA pellet was washed with 1 mL 75% ethanol, followed by brief vortex, and then was centrifuged at 7500 g for 5 min at 4 °C. The RNA pellet was dried for 5~10 min, and dissolved with 20 μL RNase-free water. Absorbance at 260 nm and 280 nm was assayed to detect the concentration and 1.5% agarose gel electrophoresis was used to check its integrity.
2.5. Measurement of mRNA by rt-pcr and real-time pcr
After assay for RNA integrity and concentration, Reverse-transcription PCR was performed using Transcript One-Step gDNA Removal and cDNA synthesis SuperMix (Transgen, Beijing). Real-time PCR was conducted in a total reaction volume of 15 μL, consisting 7 μL cDNA, 7.5 μL SsoFast EvaGreen SuperMix (BioRad, Singapore), and 0.25 μL forward and reverse primers were used to detect the relative mRNA level of PRRSV in the RNA extracted from the cultured samples, which can amplify the conserved region of glycoprotein 5 of PRRSV RNA from 18 bp to 222 bp (GenBank: KY310602.1) . The PCR condition was 94 °C (3 mins), and 40 cycles of 94 °C (6 s), annealing temperature (6 s), 72 °C (10 s). At the end of the PCR cycle, melt curve analysis was performed at an increment of 0.5 °C per cycle from 55 °C to 95 °C. TATA box Binding Protein (TBP) and DNA topoisomerase 2-β (Top2-β) were used as reference genes for normalization of gene expression. All primer sequences, their annealing temperature and amplification efficiency were listed in Table 2, and the amplified fragments is 205 bp. The relative expression level of gene was calculated by 2-ΔΔCT.
Table 2.
Primers for Real-Time qPCR.
| Gene | GeneBank Accession Number | Sequence(5′−3′) | Annealing Temperature ( °C) | Product Length (bp) |
|---|---|---|---|---|
| PRRSV | — —1 | F2:TATCGTGCCGTTCTATCTT | 61.0 | 205 |
| R3:GAAATGGCTGGTGGTGAG | ||||
| TBP | DQ178129 | F:TACCCACCAACAGTTCAGTAGTTAT | 60.6 | 158 |
| R:TACCCACCAACAGTTCAGTAGTTAT | ||||
| Top2β | AF222921.1 | F: AACTGGATGATGCTAATGATGCT | 51 | 464 |
| R: TGGAAAAACTCCGTATCTGTCTC | ||||
| IL-10 | NM_214,041 | F: ATGGGCGACTTGTTGCTGAC | 60.6 | 215 |
| R: CAGGGCAGAAATTGATGACAG | ||||
| TGF-β1 | NM_214,015 | F: TCCAAGGACCCTTCTCGGAT | 60.0 | 110 |
| R: AAAAACCGAGATGGGCGAGA | ||||
| TGF-β3 | NM_214,198 | F: CCAGCCCGATGAGCACATA | 61.6 | 114 |
| R: AGCCATTCACGCACAGTGTC | ||||
| IL-2 | NM_213,861.1 | F: AGCTCTGGAGGGAGTGCTAA | 62.0 | 116 |
| R: TGTTTCAGATCCCTTTAGTTCCA | ||||
| IL-4 | NM_214,123 | F: GCTGCCCCAGAGAACACGAC | 61.0 | 119 |
| R: AGGTTCCTGTCAAGTCCGCTC | ||||
| IL-8 | NM_213,867 | F: TTCACAAGTCTTCTTGCCTCAAC | 61.0 | 86 |
| R: AAGGTAGGATGGGGGCTGAA | ||||
| TNF-α | NM_214,022 | F: CCCACGTTGTAGCCAATGTC | 61.5 | 131 |
| R: GAGGTACAGCCCATCTGTCG | ||||
| IFN-γ | NM_213,948 | F:GAAGAATTGGAAAGAGGAGAGTGAC | 61.5 | 114 |
| R: TCCATGCTCCTTTGAATGGC | ||||
| IFN-α | TQ839262.1 | F: ACTTCCACAGACTCACCCTCTATC | 54.5 | 79 |
| R: ATGACTTCTGCCCTGATGATCT | ||||
| IL-27p28 | NM_001007520 | F: CAGGAGTTGCAGAGGGAGTTCAAG | 61.3 | 102 |
| R: TGGCAGGTGTGATTCAGCAAAGT | ||||
| TLR3 | NM_001097444 | F: GCATTGCCTGGTTTGTTAGTTG | 56.0 | 122 |
| R: TGTATCAAAAAGAATCACTGGGAG | ||||
| TLR7 | NM_001097434.1 | F: TTTCCTCAAATGCCTAAACTTAT | 54.0 | 185 |
| R: AGTGGCTGTTACTACTTATATCT | ||||
| MyD88 | NM_001099923..1 | F: ATCTGCTACTGGCCCAGCGATAC | 61.6 | 101 |
| R: ACATCTCGGTCAGACACACATAACT |
1, the primer of PRRSV is designed based on conserved region of several different virus isolations.
2: forward primer;.
3: reverse primer;.
2.6. Statistical analysis
All the experiments were performed triplicate. Data were expressed as means±SD. Statistical analysis of data was performed by two way ANOVA and Sidak multiple comparison. Differences were considered significant if P<0.05.
3. Results
3.1. Knockdown TGF-β1 expression in tp-pbmcs by shTGFβ1-1
After 12 h culture in vitro and centrifuge washing, plenty of harvested leukocytes (10.2 ± 2.35%) were proved to be monocytes with mouse Anti-CD14 antibody (Phycoerythrin);Therefore, the harvested mononuclear cells are eligible for further PRRSV infection experiment.
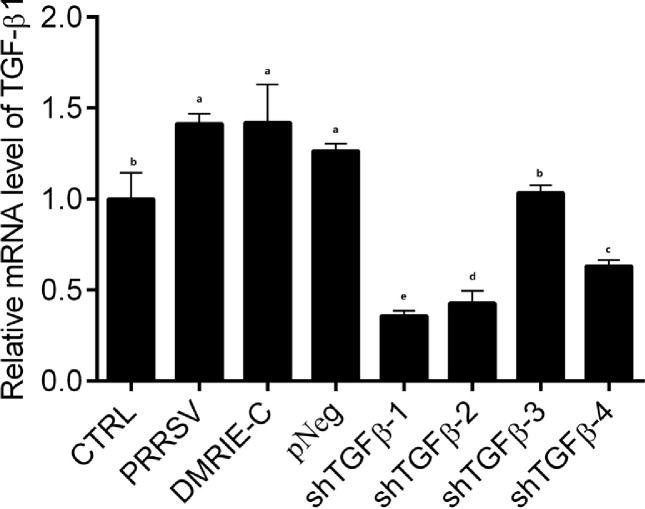
The four potential interfering candidates were detailed in Table 1. Before further study, their down regulatory efficiency was evaluated; shTFGβ1-1 was proved to be most potent in down-regulating the mRNA level of TFG-β1(P<0.05) (Fig. 1), so it was chosen for all following experiments.
Fig. 1.
Down-regulatory Efficiency of recombinant shRNA plasmids on TGF-β1 of the treated cells. The shTGFβ1-1~4 groups were transfected with the recombinant plasmid. The pS-PRRSV group was transfected with pNeg instead of recombinant interfering plasmid, while the DMRIE-C group was treated with the transfection reagent only. After incubation for 36 h, the mRNA level of TGF-β1 is determined. All experiments are performed in triplicate. All results were shown as means±SD. In all cases, different superscript letters indicate that there are statistically significant differences among groups (P<0.05), and vice versa (P>0.05). The followings are the same as here.
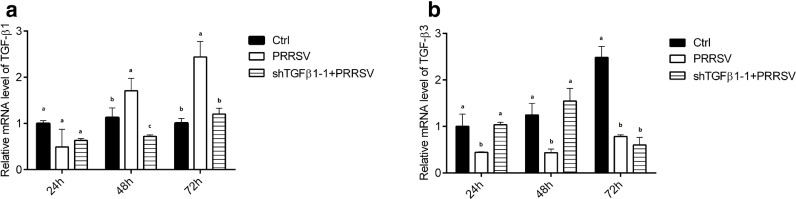
Further study was performed to see the persistent effect of shTFGβ1-1 on TFG-β1 expression. Apparently, shTFGβ1-1 inhibited the up-transcription of TFG-β1 gene caused by PRRSV for 72 h (P<0.05) (Fig. 3a).
Fig. 3.
mRNA levels of TGF-β1(a) and TGF-β3(b) gene in the treated cells. The shTGFβ1-1+PRRSV group was transfected with shTGFβ1-1 plasmid prior to PRRSV inoculation at the concentration of 10 μl per 1 mL.
In addition, the mRNA levels of immune-related genes were analyzed to observe the influence of shTFGβ1-1 and exclude the possible side effect of transfection reagent and pNeg. As listed in Table 3, 48 h culture after transfection, no significant changes of the expressions of most immune genes were observed among the three groups (P>0.05) except for TGF-β1 of shTFGβ1-1 group (P<0.05), indicating that the only shTFGβ1-1 plasmid itself is not stimulatory and just exerts negligible effect on the gene expression of leukocytes except for TGF-β1.
Table 3.
The relative mRNA levels of immune genes in Tp-PBMCs transfected with shTFGβ1-1 and pNeg plasmid and cultured for 48 h.
| Gene | Transfection media control | pNeg | shTFGβ1-1 |
|---|---|---|---|
| IL-2 | 1.00±0.11a | 0.91±0.02 a | 0.95±0.12 a |
| IL-4 | 1.00±0.11 a | 0.90±0.14 a | 0.97±0.11 a |
| IL-8 | 1.00±0.11 a | 1.13±0.24 a | 1.01±0.22 a |
| IFN-γ | 1.00±0.02 a | 0.87±0.26 a | 0.91±0.13 a |
| MyD88 | 1.00±0.04 a | 1.07±0.16 a | 1.02±0.18 a |
| TNF-α | 1.00±0.05 a | 1.03±0.15 a | 1.13±0.14 a |
| IFN-α | 1.00±0.04a | 1.40±0.44a | 1.29±0.32a |
| TLR3 | 1.00±0.02 a | 1.15±0.29 a | 1.09±0.21 a |
| IL-10 | 1.00±0.06 a | 1.07±0.07 a | 1.11±0.12 a |
| TGF-β1 | 1.00±0.02a | 0.94±0.14a | 0.31±0.15b |
| IL-12p28 | 1.00±0.06 a | 1.33±0.45 a | 1.28±0.20 a |
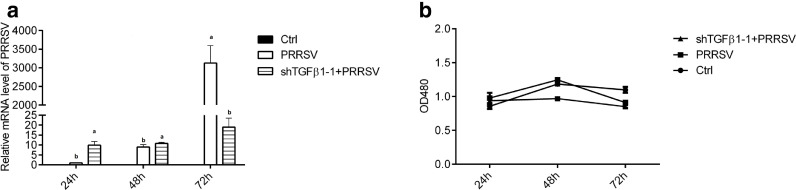
3.2. shTGFβ1-1 was capable to decrease prrsv load and improve cell viability
The mRNA level of PRRSV peaked at 72 h post infection (hpi) in Tp-PBMCs, while shTFGβ1-1 effectively inhibited the increase of PRRSV (Fig. 2a) (P<0.05).
Fig. 2.
Inhibition effect of shTGFβ1-1 on PRRSV replication (a) and its promotion of cell viability(b) of the treated cells.
Meanwhile, cell viability of Tp-PBMCs was analyzed (Fig. 2b), and PRRSV obviously reduced cell viability (P<0.05). However, the interfering plasmid evidently raised the cell viability (P<0.05).
3.3. Effects of shTGFβ1-1 on immune genes of infected leukocytes
The mRNA levels of several immune genes were determined to analyze the effect of shTFGβ1-1 on immune responses of Tp-PBMCs.
The shTFGβ1-1 obviously inverted the elevation of mRNA level of TGF-β1 gene that was provoked by PRRSV (P<0.05) (Fig. 3a). However, the expression of TFGβ3 gene was inhibited by PRRSV (P<0.05) (Fig. 3b), while the shTFGβ1-1 elevated its expression for the first 48 h (P<0.05), suggesting TGF-β3 could possibly compensate the absent function of TGF-β1 in vitro.
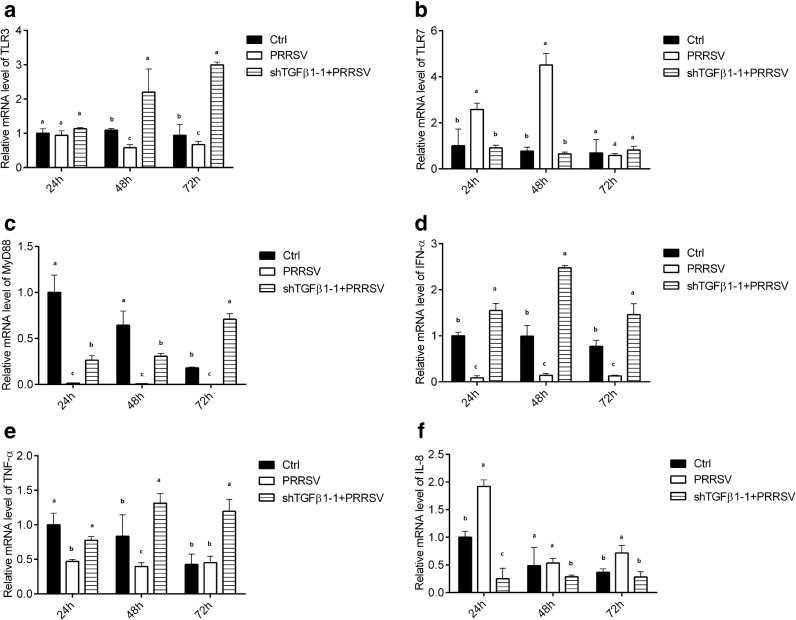
TLR3 mRNA level was not obviously modulated by PRRSV, while shTGFβ1-1 obviously increased its expression compared to the control (P<0.05) (Fig. 4a). Unlike TLR3, TLR7 gene was firstly activated by PRRSV at first 48 h, and its mRNA level rapidly decreased thereafter with shTGFβ1-1 incubation (Fig. 4b).
Fig. 4.
The changes of the mRNA levels of TLR3(a), TLR7(b), MyD88(c), IFN-α(d),TNF-α(e) and IL-8(f) genes in the treated cells.
The expression of MyD88 and IFN-α gene were significantly inhibited by PRRSV (P<0.05); in contrast, the shTGFβ1-1 dramatically elevated the mRNA level of both genes (P<0.05) (Fig. 4c and 4d).
Besides, the mRNA level of TNF-α was reduced by PRRSV infection at the first 48 h, and thereafter restored to the control level (P>0.05); whereas it was markedly increased by shTGFβ1-1(P<0.05) (Fig. 4e).
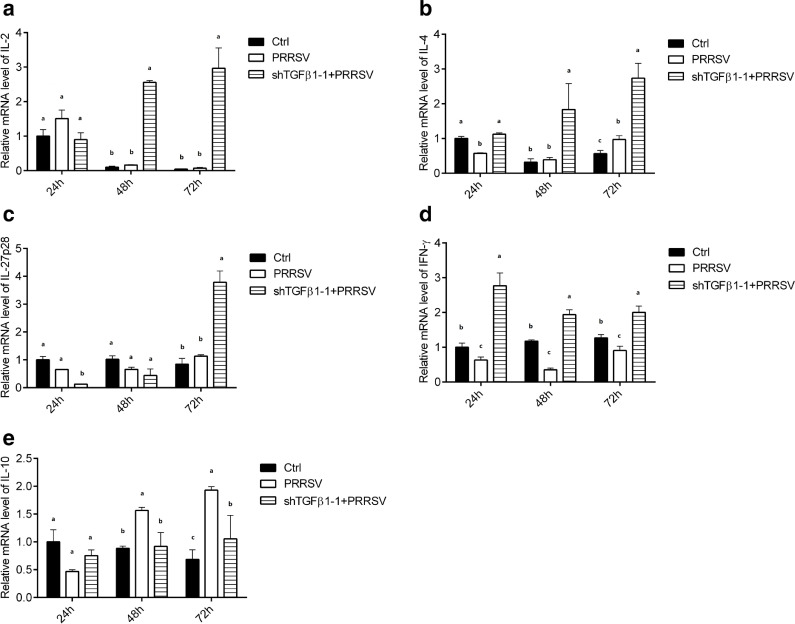
Similarly, the shTGFβ1-1plasmid also suppressed the increased expression of IL-8 gene, which was induced by PRRSV (P<0.05) (Fig. 4f). shTGFβ1-1 remarkably up-regulated the transcriptional level of IL-2, IL-4 and IL-27p28 gene to different extents (P<0.05), all of which were slightly modified by PRRSV (Fig. 5a, 5b and 5c).
Fig. 5.
The up-regulated transcriptional levels of IL-2(a), IL-4(b), IL-27(c) and IFN-γ(d) gene and down-regulation of IL-10(e) gene expression by shTGFβ1 in the treated cells.
In addition, PRRSV significantly reduced the expression of IFN-γ gene (P<0.05), while shTGFβ1-1 could obviously elevated its expression (Fig. 5d) (P<0.05).
Meanwhile, the IL-10 mRNA level was increased by PRRSV and peaked at 72hpi, and its transcriptional level was also down-regulated by shTGFβ1-1compared to PRRSV group (P<0.05) (Fig. 5e) .
4. Discussion
Normally, the porcine aveolar macrophages are very sensitive and suitable target cells for PRRSV. Herein, instead of high-cost and trouble washing lung to obtain macrophages, we just collected monocytes/macrophages from cultured PBMCs for PRRSV infection, in which target monocytes/macrophages was proved to be plenty of leukocytes after 12 h incubation in vitro and centrifuge in our experiment. To get rid of the possible loss of adherent monocytes/macrophages during our culture of PBMCs, we purposefully employed special cell culture plates, Cell Repel plates with ultra-low adherent surface from Eppendorf company. Also, we thoroughly washed the plates when we harvested the cultured cells for centrifuge, and carefully checked whether monocytes/macrophages still existed in the harvested cells by use of mouse anti-CD14 monoclonal anitbody (ab186689) from Abcam in FlowCyt. Therefore, we found that there were still plenty of monocytes/macrophages remained in the harvested cells before infection with PRRSV. Furthermore, we detected the burst mRNA increase of PRRSV during the culture of the infected cells, which was clearly manifested in the Fig. 2(a), confirming that PBMCs could support the replication of PRRSV in vitro and is qualified for further RNAi experiment.
It had been reported that the production of TGF-β could be induced by PRRSV infection (Gómezlaguna et al., 2012), and it was the main effector of PRRSV induced Tregs (also known as Th3 subset) (Silva-Campa et al., 2009; Yoshimura et al., 2010). Over expressed TGF-β, reduced IL-2, IFN-γ and TNF-α expression were found in the PRRSV infected group, which in turn dampened the host immune response during PRRSV infection (Han, Zhou, Ge, Guo, & Yang, 2017).
The antiviral capability of TLR3 could be impaired by PRRSV replication to facilitate virus evading host immune responses (Miller, Lager, & Kehrli, 2009), which was in accordance with the results in this study, TLR3 mRNA decreased to a half when the Tp-PBMCs were infected with PRRSV, and MyD88 was just beyond the detectable threshold of qPCR. The slightly inhibited IL-8 expression might hinder the recruitment of immune cells, and consequently slow down virus dissemination and infection, which was consistent with earlier report (Reeth, Gucht, & Pensaert, 2002). Besides, the mRNA level of IL-27 subunit was not changed obviously by PRRSV infection, implying that it was not critical factor utilized by PRRSV to thwart host immune system.
TGF-β1 was a multifunctional cytokine, dampening its expression might lead to severe damages to cells. Reports had demonstrated that TGF-β3, to some extent, could compensate the deficiency of TGF-β1 in vitro (Liu et al., 2008; Lucas, Kim, Melby, & Gress, 2000). The mRNA level of TGF-β3 was evidently increased in the early interfering plasmid transfection compared to the infected group. However, it is not clear whether this compensation could synergize the immune suppression of TGF-β1 or just maintain the essential viability or growth of treated cells, which need further research later.
Given the indispensable status of TGF-β, we exploited RNAi method to knockdown TGF-β1 to observe whether it could be feasible to inhibit PRRSV production and alleviate immune response to some extent. As expected, PRRSV replication could be markedly depressed in Tp-PBMCs to about 1.00%, and the cellular viability could be obviously prompted to 160~180% accompanied with minimal TGF-β1, indicating the essential role of TGF-β1 for PRRSV replication again, and also implying a promising strategy for PRRSV resistance. It was also confirmed that shTFGβ1-1 just specifically down-regulated the expression of TFGβ1-1 gene and did not provoke expressions of other immune genes during the transfection.
However, TLR7 was obviously induced by PRRSV in first 48 h PI, following swift decrease in shTFGβ1-1+ PRRSV group to the same level of Ctrl group. Because PRRSV was a positive ssRNA virus, TLR7 could recognize the viral genome prior to detection of dsRNA replicative intermediate by TLR3, and before PRRSV replication, some viral proteins which could inhibit TLR3 transcription might have been expressed. Nevertheless, the mRNA levels of these three genes were elevated after TGF-β1 expression was down-regulated, which suggested the suppressed innate immune responses were restored.
The levels of IL-1β and IFN-γ were linked to PRRSV resistance and clearance (Charerntantanakul, Yamkanchoo, & Kasinrerk, 2013; Darwich, Díaz, & Mateu, 2010). Increased IL-2, IFN-γ and TNF-α expression were observed following shTFGβ1-1 transfection, which could be indication of effective Th1 anti-PRRSV responses. In addition, the sharply increased mRNA levels of IL-4 also implied that Th2 response was activated.
Obvious repression of IL-10 expression was observed in the shRNA treated group, suggesting that inhibition of TGF-β1 expression could lead to the reduction of IL-10, which probably result from the evidently increased IL-2, IFN-γ, IFN-α and TNF-α expression and facilitate the enhancement of the antiviral immunity to clear the infected virus. We observed this promotion of immunity at least lasted 72 h in vitro and could maintain longer time in vivo until the shRNA could not be transcribed in the infected cells, which might be continuous form 7 to 14 days or so depending on doses.
Furthermore, we just analyzed the mRNA expression levels of the TLRs and cytokine genes by real time quantitative RT-PCR technique, though it is the most sensitive and economical method to analyze gene expression, our present observations could be consolidated through the detection of translation products of these cytokines and TLRs by ELISA and further utilization of shTFGβ1-1 in vivo later.
5. Conclusions
Our experiment firstly screened out effective specific shRNA targeted to pig TGF-β1 gene, it could significantly knock down the mRNA level of TGF-β1 gene and obviously increase the viability of PRRSV infected cells. The knockdown of TGF-β1 gene expression by shRNA could not only lead to significant inhibition of PRRSV replication in pig immune cells, but also enhance the antiviral immune responses and reduce the PRRSV yield in the infected cells. These results could inspire the development of novel promising way to prevent PRRSV infection of pig and promote the immunity of animal against viral disease.
Declaration of Competing Interest
The authors declare no competing financial interests.
Acknowledgments
Ethical Statement
The manuscript only contains experiments using pig blood, we assured that the care and use of experimental pigs completely complied with Chinese animal welfare laws, guidelines and policies.
Acknowledgments
This work was financially supported by key projects of Sichuan province (2016NYZ0042), National Natural Science Foundation of China (No. 30871855) and National International Cooperation Program (No.2011DFA10101103). We sincerely thanked Dr. Gang Wang (National Engineering Research Center for Biomaterials) for technical support.
References
- Charerntantanakul W., Yamkanchoo S., Kasinrerk W. Plasmids expressing porcine interferon gamma up-regulate pro-inflammatory cytokine and co-stimulatory molecule expression which are suppressed by porcine reproductive and respiratory syndrome virus. Veterinary Immunology & Immunopathology. 2013;153(1–2):107–117. doi: 10.1016/j.vetimm.2013.02.013. [DOI] [PubMed] [Google Scholar]
- Darwich L., Díaz I., Mateu E. Certainties, doubts and hypotheses in porcine reproductive and respiratory syndrome virus immunobiology. Virus Research. 2010;154(1):123–132. doi: 10.1016/j.virusres.2010.07.017. [DOI] [PubMed] [Google Scholar]
- Dwivedi V., Manickam C., Binjawadagi B., Linhares D., Murtaugh M.P., Renukaradhya G.J. Evaluation of immune responses to porcine reproductive and respiratory syndrome virus in pigs during early stage of infection under farm conditions. Virology Journal. 2012;9(1):45. doi: 10.1186/1743-422X-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómezlaguna J., Rodríguezgómez I.M., Barranco I., Pallarés F.J., Salguero F.J., Carrasco L. Enhanced expression of TGFβ protein in lymphoid organs and lung, but not in serum, of pigs infected with a european field isolate of porcine reproductive and respiratory syndrome virus. Veterinary Microbiology. 2012;158(1–2):187–193. doi: 10.1016/j.vetmic.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorelik L. Abrogation of TGFbeta signaling in t cells leads to spontaneous t cell differentiation and autoimmune disease. Immunity. 2000;12(2):171–181. doi: 10.1016/s1074-7613(00)80170-3. [DOI] [PubMed] [Google Scholar]
- Han J., Zhou L., Ge X., Guo X., Yang H. Pathogenesis and control of the chinese highly pathogenic porcine reproductive and respiratory syndrome virus. Veterinary Microbiology. 2017;209(9):30–47. doi: 10.1016/j.vetmic.2017.02.020. [DOI] [PubMed] [Google Scholar]
- Huang Y.W., Meng X.J. Novel strategies and approaches to develop the next generation of vaccines against porcine reproductive and respiratory syndrome virus (PRRSV) Virus Research. 2010;154(1):141–149. doi: 10.1016/j.virusres.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn, J.H., .Lauck, M., Bailey, A.L., .Shchetinin, A.M., .Vishnevskaya, T.V., .& Bao, Y.M. e.t al., (2016).Reorganization and expansion of the nidoviral family arteriviridae, archives of virology, 161(3), 755–768. [DOI] [PMC free article] [PubMed]
- Li Y.H., Shyu D.L., Shang P.C., Bai J.F., Ouyang K., Dhakal S. Mutations in a highly conserved motif of nsp1 beta protein attenuate the innate immune suppression function of porcine reproductive and respiratory syndrome virus. Journal of Immunology. 2016;90(7):3584–3599. doi: 10.1128/JVI.03069-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Zhang P., Li J., Kulkarni A.B., Perruche S., Chen W. A critical function for TGF-β signaling in the development of natural cd4cd25foxp3 regulatory t cells. Nature Immunology. 2008;9(6):632–640. doi: 10.1038/ni.1607. [DOI] [PubMed] [Google Scholar]
- Lucas P.J., Kim S.J., Melby S.J., Gress R.E. Disruption of t cell homeostasis in mice expressing a t cell–specific dominant negative transforming growth factor β ii receptor. The Journal of experimental medicine. 2000;191(7):1187–1196. doi: 10.1084/jem.191.7.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller L.C., Lager K.M., Kehrli M.E. Role of toll-like receptors in activation of porcine alveolar macrophages by porcine reproductive and respiratory syndrome virus. Clinical and Vaccine Immunology. 2009;16(3):360–365. doi: 10.1128/CVI.00269-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeth K.V., Gucht S.V., Pensaert M. In vivo studies on cytokine involvement during acute viral respiratory disease of swine: Troublesome but rewarding. Vet Immunol Immunopathol. 2002;87(3):161–168. doi: 10.1016/S0165-2427(02)00047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renukaradhya G.J., Alekseev K., Jung K., Fang Y., Saif L.J. Porcine reproductive and respiratory syndrome virus–induced immunosuppression exacerbates the inflammatory response to porcine respiratory coronavirus in pigs. Viral Immunology. 2010;23(5):457–466. doi: 10.1089/vim.2010.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva-Campa E., Flores-Mendoza L., Reséndiz M., Pinelli-Saavedra A., Mata-Haro V., Hernández J. Induction of t helper 3 regulatory cells by dendritic cells infected with porcine reproductive and respiratory syndrome virus. Virology. 2009;387(2):373–379. doi: 10.1016/j.virol.2009.02.033. [DOI] [PubMed] [Google Scholar]
- Yoshimura A., Wakabayashi Y., Mori T. Cellular and molecular basis for the regulation of inflammation by TGF-beta. Journal of Biochemistry. 2010;147(6):781–789. doi: 10.1093/jb/mvq043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Ying E. Non-Smad pathways in TGF-beta signaling. Cell Research. 2009;19(1):128–139. doi: 10.1038/cr.2008.328. [DOI] [PMC free article] [PubMed] [Google Scholar]