Abstract
A cross-sectional study was conducted to estimate the sero-prevalence, potential risk factors for transmission and spread of brucellosis in livestock and human in Jigjiga and Gursum Woredas of Fafan Zone in Ethiopian-Somali. Two Kebeles were purposively selected from each Worada based on accessibility and willingness of livestock owners. For serology, a total of 268 cattle, 108 sheep, 172 goats, 183 camels, 211 humans were included. For questionnaire, 99 volunteers were recruited. Blood samples were collected from livestock and human. The serum was subjected to Rose Bengal Plate Test (RBPT) and Complement Fixation Test (CFT) to detect Brucella antibody. Out of the total 731 livestock examined, 3.0% were positive for Brucella antibodies using RBPT. Highest sero-prevalence was recorded in camels (4.9%) followed by goat (2.9%), cattle (2.6%), and sheep (0.9%). Using CFT, 0.4% of animals were found positive for brucellosis. A sero-prevalence of 1.7% was recorded in goats using CFT but no in other animal species. From the 211 human serum samples, 5 (2.4%) were positive for Brucella infection using RBPT. One (0.4%) was confirmed by CFT. Questioner survey revealed, almost all respondents (98%) were not aware about zoonotic risks of brucellosis. Cattle and camel milking were mainly performed by housewives. Although 97-99% of respondent had habits of cooked meat consumption, the majorities (99%) consume raw milk. In the pastoral community, the observed sero-prevalence of human brucellosis along with the practices of animal husbandry and animal food consumption habits, might give an insight that brucellosis could pose a public health hazard.
Keywords: Camel, CFT, Husbandry practices, Pastoral community, RBPT, Ruminants
1. Introduction
Brucellosis is a contagious infectious bacterial disease affecting domestic animals (OIE, 2008), maintained in wildlife population (Dwight & Yuan, 1999) and with risk of zoonosis in human (Mantur, Amarnath and Shinde, 2007, OIE 2008). In livestock it results reproductive losses due to abortion, placentitis, stillbirth, birth of weak offspring, epididymitis, and orchitis (Dwight and Yuan, 1999, OIE 2008, Radostits, Gay, Hinchcliff and Constable, 2007). Cattle are a major reservoir of B. abortus. Sheep, goats, pigs, equines and camels are occasionally infected but rarely act as a source of infection for cattle (Radostits et al., 2007).
Many developing countries with limited resources, including Ethiopia, are facing other priority diseases that are more spectacular and have not yet fully launched programs featuring any aspects of brucellosis intervention. The epidemiology of the disease in livestock and humans as well as cost-effective prevention measures is not well understood (McDermott & Arimi, 2002). Hence, brucellosis remains challenging widespread in domesticated and wildlife animal population and presents enormous economic and public health problems in developing countries (Acha and Szyfres, 2001, Memish and Mah, 2001). The true incidence of human brucellosis is unknown and the estimated burden of the disease varies widely, from < 0.03 to > 160 per 100,000 population (Pappas, Papadimitriou, Akritidis, Christou, & Tsianos, 2006). Occupationally, 11% among animal health workers and 7% among hospital patients (Franc, Krecek, Häsler and Arenas-Gamboa, 2018, McDermott, Grace and Zinsstag, 2013) are at risk of acquiring Brucella infection.
Franc et al. (2018) reported an average prevalence ranging from 0 to 88.8%, 0 to 68.8%, 0.4–20% and 0–12.9% in sheep and goats, cattle, camels and other species (pigs and dogs), respectively in Africa and Asia. An overall true Brucella sero-prevalence of 5.3% in goats, 2.7% in sheep, and 2.9% in each of camels and cattle were reported in Ethiopia (Tadesse, 2016). Bekele, Mohammed, Tefera, and Tolosa (2011) reported brucellosis in sheep and goats at Jigjiga district. A huge and diverse livestock species of Ethiopia are maintained under different agro- ecological zones, predominately extensive animal husbandry practices. These provide ample opportunities for inter-mixing of different animal species at communal grazing areas and water points nearly in of 80% the rural community (Samui, Oloya, Munyeme, & Skjerve, 2007), which are mainly characterized by poor sanitary condition. Such species composition and mixing could attributed to risk of widespread host for the establishment and transmission of pathogen owning to high stock density and multi-species composition under lack of controlling measures in Ethiopian livestock industry (Benkirane, 2006, Megersa et al., 2011, Samui, Oloya, Munyeme and Skjerve, 2007).
Thus, the economic and public health impact of brucellosis remains of particular concern in developing countries mainly among the vulnerable sector in rural pastoral populations. The risk is presumed to be high in nomadic pastoral societies, where close and frequent contact between man and animals is unavoidable part of ecology (Hamdy & Amin, 2002). However, little information is available on the prevalence of brucellosis at the livestock and human interface in such kind of society. Therefore, the objectives of this study were to estimate the sero-prevalence of livestock and human brucellosis and to assess the community awareness on the risks of zoonotic brucellosis in selected districts of Fafan Zone, Ethiopia.
2. Materials and methods
2.1. Ethical considerations and clearance
Ethical clearance was obtained from the Ethiopian Somali Regional State Health Research Ethical Review Committee. Additionally, verbal consent was obtained from the owner of the animal. Full cooperation and voluntary participation of all participants was obtained by assuring them the confidentiality of their involvement.
2.2. Description of the study areas
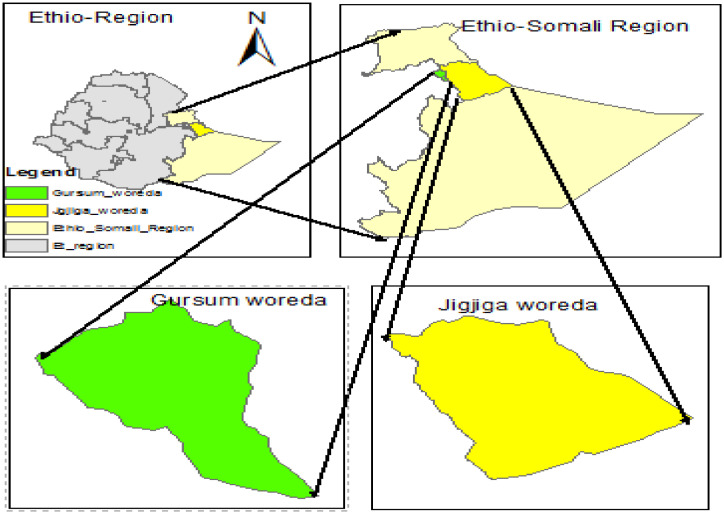
The study was conducted in two districts namely Jigjiga and Gursum that are found in Fafan administrative Zone of Somali Regional State at about 600 km east of Addis Ababa, Ethiopia. The altitude of the zone ranges from 500 to 1650 m above sea level and lies between approximately 9020′ North e and 45,056′ East (Fig. 1). The climate is semi-arid type which is characterized by high temperature. The mean annual rainfall in the area ranges from 600 to 700 mm. Agro-pastoralism is the dominant production system in Fafan Zone. The Zone is estimated to have human population of 430,634. The livestock population of the zone is 503,871 cattle, 1134,856 sheep, 1365,265 goats, and 290,649 camels (CSA, 2015).
Fig. 1.
Map of the study area.
2.3. Study population
The study populations were apparently healthy livestock species (cattle, sheep, goats, and camels) and human found in selected rural Kebeles of the study districts. Animal included were local breeds (indigenous), both sexes, age groups of greater than six months, and with no previous vaccination history against brucellosis. In the study districts, livestock were managed under typical pastoral community characterized by clan-based segregation with often mixing of animals from different houses within a clan. Human that has close contact with sampled animals were considered for the study.
2.4. Study design
A cross-sectional study type was employed to estimate the sero-prevalence of brucellosis in target population and to assess awareness of community on risks associated with brucellosis.
2.5. Sampling methods
From the seven Woredas of Fafan Zone, two were randomly selected based up on lottery system. Similarly, two Kebeles were selected from each Woredas. The selected Kebeles were Hadew and Shebele from Jigjiga, while Fafan and Bombas from Gursum districts. Households keeping livestock in and around the study area were sampled based on accessibility, population of the study livestock and willingness of the owners to be involved in the study. From each household, 50-70% of the herd was randomly selected for sampling. Individuals for questioner interview were recruited based on their willingness and participation in animal management practices related with risk of brucellosis.
2.6. Sample size determination and distribution
The sample size was determined based on the formula recommended by Thrusfield (2005) using 95% confidence interval and desired precision of 0.05 (5%) considering an expected prevalence of 3% (Hunduma & Regassa, 2009), 1.2% and 1.9 % (Bekele et al., 2011) and 4.2% (Teshome, Molla, & Tibbo, 2003) for cattle, sheep, goat and camel. Using the same formula, sample size for human was calculated with expected prevalence of 16.5% (Ahmed, Ali, Mesfin, Deressa, & Girmaye, 2008). Accordingly, the sample size was 45 cattle, 18 sheep, 29 goats, 62 camels, and 211 human. However, to increase precision, the sample size was increased by 6 fold for cattle, sheep, and goat and by 3 fold for camel. Thus, a total of 731 animals (268 cattle, 108 sheep, 172 goats, and 183 camels) were included for the study based on proportional allocations of the sample size for each Kebele (Table 1).
Table 1.
Livestock and human sample distribution in the selected study areas.
| Study population | Jigjiga Woreda №. | Gursum Woreda № | Total № | |||
|---|---|---|---|---|---|---|
| Hadew kebele | Shebele kebele | Fafan kebele | Bombas kebele | |||
| Animal | Cattle | 50 | 60 | 90 | 68 | 268 |
| Sheep | 30 | 16 | 38 | 24 | 108 | |
| Goat | 44 | 38 | 56 | 34 | 172 | |
| Camel | 50 | 35 | 52 | 46 | 183 | |
| Total | 174 | 149 | 236 | 172 | 731 | |
| Huma | Human* | 58 | 55 | 45 | 53 | 211 |
| Human⁎⁎ | 25 | 25 | 24 | 25 | 99 | |
studied for sero-prevalence of brucellosis.
studied for knowledge of zoonotic diseases and zoonotic brucellosis as well as livestock management and product utilization.
For questionnaire survey sample size was calculated using the formula given by Arsham (2002); N = 0.25/SE2, where: N = sample size, SE (standard error) = 5%. Thus, the required sample size for the questionnaire survey was 100. However, only 99 volunteers were included.
2.7. Sample collection and laboratory analysis
2.7.1. Blood sample collection
Before withdrawal of blood from the jugular vein, the site was disinfected using 70% alcohol. Blood volume of 7 ml to 10 ml from cattle and camel; and 4 ml to 5 ml from sheep and goats was collected. Each sample was labeled with specific identification number and transported to Jigjiga Regional Veterinary Diagnostic and Research Laboratory in an ice box for processing and RBPT. The serum was separated by allowing the blood to clot overnight at room temperature and the purified serum was harvested into sterile screw capped cryovials.
In the case of sample collection from human, 4 ml to 5 ml of blood was withdrawn from the radial vein by health professionals at nearby health center using plain vacationer tube and needle. The serum was then separated by allowing the blood to clot for one hour and the serum was collected into sterilized screw caped cryovials.
2.7.2. Serological test
Primary screening of serum samples for Brucella antibody was performed using RBPT at Jigjiga Regional Veterinary Diagnostic and Research Laboratory according to the standard procedure described by Nielsen (2002). The results were read by examining the degree of agglutination in good light source and when necessary using magnifying glass. Any visible agglutination was considered positive. For interpretation of the results, both positive and negative control sera were used as recommended by OIE (2004). Due to the absence of reagents required for CFT at the regional laboratory, the RBPT positive samples were stored at −20⁰C until transported to National Veterinary Institute (NVI), Bishoftu, Ethiopia for confirmatory test using CFT. The serum from human blood was subjected to RBPT at respective health centre. The CFT was preformed and interpreted according to OIE (2004).
2.8. Questionnaire survey
Questionnaire interview format was prepared and administered to gather information from randomly selected households’ individuals using local language. The questionnaire format was focused on the knowledge and awareness related with the transmission of brucellosis from livestock to human. Factors like livestock management practices, milk source and milking practices, milk consumption practices, meat sources and meat consumption practices of community were considered. In addition, the presences of reproductive disorders in livestock were considered.
2.9. Data management and analysis
The data from the field and laboratory were entered into Microsoft Excel 2013© and analyzed using SPSS version 20 software program. Categorical variables (species, sex, age, and Kebeles) and data on management system were expressed in frequency and proportions. Brucellosis prevalence was calculated based on results from RBPT positive per sampled animal or human. Similar, calculation was made from CFT positive animal or human.
3. Results
3.1. Seroprevalence of livestock brucellosis
Out of the 731 animals examined, 22 (3.0%) were positive for brucellosis upon screening using RBPT, while 3 (0.4%) were confirmed using CFT (Table 2). Based on RBPT, the highest prevalence was recorded in camels (4.9%). The study also showed that brucellosis was higher in females (3.9%). Regarding the Kebeles, the highest prevalence was observed in Bombas (4.1%). Based on CFT, the prevalence was similar in most of variable categories but it was higher in goats (1.7%) than other livestock species (0%).
Table 2.
Sero-prevalence of brucellosis in livestock animals in the study area.
| Variables of study | № of examined animals | № (%) sero-positive with: | ||
|---|---|---|---|---|
| RBPT | CFT | |||
| Sex | Male | 245 | 3 (1.2) | 1 (0.4) |
| Female | 486 | 19 (3.9) | 2 (0.4) | |
| Age | Young | 322 | 9 (2.8) | 2 (0.6) |
| Adult | 409 | 13 (3.2) | 1 (0.2) | |
| Species | Cattle | 268 | 7 (2.6) | 0 (0.0) |
| Camel | 183 | 9 (4.9) | 0 (0.0) | |
| Sheep | 108 | 1 (0.9) | 0 (0.0) | |
| Goat | 172 | 5 (2.9) | 3 (1.7) | |
| Kebele | Hadew | 174 | 4 (2.3) | 1 (0.6) |
| Shebele | 149 | 4 (2.7) | 0 (0.0) | |
| Fafan | 236 | 7 (3.0) | 2 (0.8) | |
| Bombas | 172 | 7 (4.1) | 0 (0.0) | |
| Total | 731 | 22 (3.0) | 3 (0.4) | |
3.2. Seroprevalence of human brucellosis
Out of the 211 serum samples, 5 (2.4%) and 1 (0.4%) were found positive for Brucella antibody by RBPT and CFT, respectively (Table 3). The RBPT revealed that Fafan and Bombas were the Kebeles with relatively higher prevalence of human brucellosis with a proportion of 4 and 3.8%, respectively. Meanwhile, the prevalence was higher in female (4.4%) and in adult (3.9%).
Table 3.
Sero-prevalence of humans brucellosis in the study area.
| Variables of study | №. of tested individuals | № (%) sero-positive with: | ||
|---|---|---|---|---|
| RBPT | CFT | |||
| Gender | Male | 98 | 0 (0.0) | 0(0.0) |
| Female | 113 | 5 (4.4) | 1(0.9) | |
| Age | Young | 106 | 1(0.9) | 0(0.0) |
| Adult | 105 | 4(3.8) | 1(1.0) | |
| Kebele | Hadew | 58 | 1(1.7) | 0(0.0) |
| Shebele | 75 | 1(1.3) | 0(0.0) | |
| Fafan | 25 | 1(4.0) | 1(0.4) | |
| Bombas | 53 | 2(3.8) | 0(0.0) | |
| Total | 211 | 5 (2.4) | 1 (0.4) | |
3.3. Questionnaire survey
Of the 99 respondents, 13 (13.1%) were knowledgeable on the presence of zoonotic diseases but only 2 (2.0%) were aware of zoonotic risks related to animal brucellosis (Table 4). Large proportion of respondents from Fafan (25%) and Bombas (16%) Kebeles were aware of zoonotic diseases. However, very low proportion (4 - 4.2%) were aware of the zoonotic risks brucellosis.
Table 4.
Knowledge status of community on the presence of zoonotic diseases and zoonotic brucellosis by studied demography/parameters.
| Demography/parameters of studied community | Total № interviewed | № (%) individuals knowledgeable on: | ||
|---|---|---|---|---|
| Presence of zoonotic diseases | Zoonotic risk of brucellosis | |||
| Gender | Male | 91 | 11 (12.1) | 2 (2.2) |
| Female | 8 | 2 (25.0) | 0 (0) | |
| Age | Young | 52 | 6 (11.5) | 1 (1.9) |
| Adult | 47 | 7 (14.9) | 1 (2.1) | |
| Kebele | Hadew | 25 | 2 (8.0) | 0 (0) |
| Shebele | 25 | 1 (4.0) | 0 (0) | |
| Fafan | 24 | 6 (25.0) | 1 (4.2) | |
| Bombas | 25 | 4 (16.0) | 1 (4.0) | |
| Total | 99 | 13 (13.1) | 2 (2.0) | |
With regard to livestock management, almost all (99-100%) of studied community keep animals at day and night time separately, while high proportion (57.6%) practiced mixing of their livestock during grazing. Milking of camel and cattle was mainly performed by house wives, while only low (5.1-6.1%) proportion of husband was involved. The majority (91-98%) of respondents use all studied animals as sources of milk and nearly all (97-99%) of interviewed individuals had habit of raw milk consumption as well as used cooked meat as a source of food. Only 3% of respondents indicated the presence of abortion/ stillbirth in the herd (Table 5).
Table 5.
Livestock management and product utilization associated with risk of brucellosis transmission in animal and human.
| Livestock management and product utilization | Parameters of the study | № | Risk of brucellosis acquiring (%)* | ||
|---|---|---|---|---|---|
| Livestock management | Keeping animal at day time | Mixed | 1 | 1.0* | |
| Separate | 98 | 99.0 | |||
| Keeping animal at night time | Mixed | 0 | 0* | ||
| Separate | 99 | 100 | |||
| Mixed grazing with other animal | Present | 57 | 57.6* | ||
| Absent | 42 | 42.4 | |||
| Milk source and milking practices | Animals used for milk source | Cattle | Yes | 97 | 98.0* |
| No | 2 | 2.0 | |||
| Sheep | Yes | 92 | 92.9* | ||
| No | 7 | 7.1 | |||
| Goats | Yes | 91 | 91.9* | ||
| No | 8 | 8.1 | |||
| Camel | Yes | 89 | 89.9* | ||
| No | 10 | 10.1 | |||
| Responsible personnel for milking* | Sheep | Wife | 27 | 27.3 | |
| Others⁎⁎ | 72 | 72.7 | |||
| Goats | Wife | 29 | 29.3 | ||
| Others⁎⁎ | 70 | 70.7 | |||
| Cattle | Wife | 92 | 92.9 | ||
| Husband | 6 | 6.1 | |||
| Camel | Wife | 91 | 91.9 | ||
| Husband | 5 | 5.1 | |||
| Milk consumption practice | Raw milk consumption | Yes | 98 | 99.0* | |
| No | 1 | 1.0 | |||
| Milk treatment method | Boiled | 1 | 1.0 | ||
| Raw | 98 | 99.0* | |||
| Meat source and consumption practices | Meat consumption method | Cattle | Cooked | 98 | 99.0 |
| Raw | 1 | 1.0* | |||
| Sheep | Cooked | 98 | 99.0 | ||
| Raw | 1 | 1.0* | |||
| Goats | Cooked | 98 | 99.0 | ||
| Raw | 1 | 1.0* | |||
| Camel | Cooked | 96 | 97.0 | ||
| Raw | 3 | 3.0* | |||
| Reproductive disorders in the herd | Abortion/ stillbirth | Present | 3 | 3.0* | |
| Absent | 96 | 97.0 | |||
Suspected risk of Brucella transmission, acquiring, infection;
Husband, children and neighbors.
4. Discussion
4.1. Livestock brucellosis
Brucellosis creates a serious economic problem for both the intensive and extensive livestock production system in the tropics and is considered a threat to public health. This is particularly important in the pastoral community where the livelihood is closely linked with the livestock population. In the present study, RBPT revealed that the overall prevalence of livestock brucellosis in studied districts of Ethiopian-Somali was 3.0%. Our study revealed that brucellosis was observed in both sexes with estimated prevalence of 1.2 and 3.9% in male and female, respectively. The similarity in the prevalence of brucellosis among sex category is not in line with the reports of Tesfaye (2003) and Tolosa (2004) who reported only female positive reactors in Tigray region and Jimma Zone of the country, respectively. In addition, the similarity in the prevalence of brucellosis in young's (2.8%) and adults (3.2%) using RBPT is not in line with the expected high occurrences in sexually mature than immature animals of either sex (Radostits et al., 2007). The variations in sero-prevalence of brucellosis might occur due to agro ecological differences of study areas, sample size, animal management, the diagnostic test used and production systems. The similarity in the proportion of infection between male and female animals indicates similar exposure risk of both sexes. This is supported by the present finding where no sex based segregation of livestock during grazing in the field. Radostits et al. (2007) suggested that herd size and management condition determine the rate of transmission of Brucella infection among susceptible hosts.
The present study revealed that sero-prevalence of cattle brucellosis was 2.6% using RBPT which concurs with the proportion reported by previous studies in the country. Thus, Adugna, Agga and Zewde, 2013, Asmare, Asfaw, Gelaye and Ayelet, 2010, Gumi et al., 2013, Hailu, Mohamed, Mussie and Moti, 2011, and Asmare et al. (2007) reported prevalence of 1.4%, 0.9%, 1%, 1.7%, and 2.5%, respectively. However, a relatively high prevalence (4.63%) was reported by Hailemelekot, Kassa, and Assfaw (2007) in the country.
The proportion of RBPT based Brucella positive goats (2.9%) and sheep (0.9%) recorded in this study are relatively lower than prevalence reports of 5.8% (in goats) and 3.2% (in sheep) by Ashenafi, Teshale, Ejeta, Fikru, and Laikemariam (2007) in Afar region. In agreement with the present finding, Mengistu (2007) reported a prevalence of 3.2% in goats in southern region of the country.
The current finding on the prevalence of camel brucellosis (4.9 %) is higher than the previous reports of 0.4-2.5% (Bekele et al., 2011), 0.9% (Gumi et al., 2013), 0.53% (Gessese, Mulate, Nazir, & Asmare, 2014), and 2.8% (Teshome et al., 2003) using RBPT in different parts of the country. However, the present finding is similar with previous reports from Kenya (Njeru et al., 2016) and Somalia (Ghanem et al., 2009) at a proportion of 3.9% (by RBPT) and 3.1% (by I-ELISA), respectively.
Using CFT, the overall 0.4% Brucella antibody positive livestock indicates the public health risk of pastoral communities in study area. Corbel (2006) also suggested possible cross transmission of the diseases among susceptible hosts sharing common environment. Similarly, Njeru et al. (2016) from Kenya and Ghanem et al. (2009) from Somalia reported the risk of brucellosis transmission in human and animal who share similar environment. The prevalence was the same in male (0.4%) and female (0.4%), indicating similar risk of infection for both sexes in the pastoral community settings. The prevalence was also similar in young's (0.6%) and adults (0.2%) indicating again similar risk of infection of both age categories. Agreeably, Asfaw, Molla, Zessin, and Azage (1998) reported CFT based confirmation in males at proportion of 0.1% in bovine species. On the other hand, Hailemelekot et al. (2007) reported relatively higher proportion in males (2.1%) under extensive management system. Complement fixation test confirmed the presence of Brucella infection only in goats with proportion of 1.7%. This finding in goats is closely related with the 9%, 1.3%, 1.7%, and 1.6% report of Bekele, Mohammed, Tefera and Tolosa, 2011, Muhie, 2005 and Sori, 2006, Tekeleye and Kasali, 1990, respectively in Ethiopia.
4.2. Human brucellosis
The overall prevalence of human brucellosis in studied districts of Ethiopian-Somali revealed 2.4% using RBPT but 0.4% using CFT for Brucella antibody indicating public health importance the disease among pastoral communities in the area. Corbel (2006) suggested possible cross transmission of the diseases among susceptible hosts including humans who's sharing common environment with infected animals. Similarly, Njeru et al. (2016) from Kenya and Ghanem et al. (2009) from Somalia reported prevalence of brucellosis in human and animal who share similar environment. This is also supported by the observed exposure risks related to animal husbandry, occurrence of reproductive disorders, and consumption of raw milk in this finding.
The sero-prevalence obtained by CFT is lower than the 2.2%, 1.2%, 3.4%, and 3.8% reported by Mekonnen et al., 2011, Tibesso, Ibrahim and Tolosa, 2014, Tolosa, 2004, and Hailemelekot et al. (2007), respectively in different parts of the Ethiopia. It was also lower than the 4.6% reported in Eritrea (Omer, Asfaw, Skjerve, Teklegiorgis, & Woldehiwot, 2002). Based on RBPT, our study showed that only females were reactive to brucellosis. This may be linked with the observed disparity in the role of gender with regard to milking of livestock risking for exposure. In accordance to this, 91-93% house wives were responsible for milking of cattle and camel cows. The present RBPT sero-reaction to brucellosis among theses livestock was higher in the area. This is also true for the higher prevalence in adults (3.8%) than young (0.9%).
Although, 99-100% of studied community keeps animal at day and night time in a separate, 57.6% use communal grazing. Moreover, abortion/ stillbirth was reported in 3% of the herd which have risk of transmission while contact (Hamdy and Amin, 2002, Radostits, Gay, Hinchcliff and Constable, 2007). Surprisingly, almost all (99%) of interviewed individuals consume raw milk which is one of the sources of human infection from animals shedding the pathogen (Mantur, Amarnath and Shinde, 2007, OIE 2008, Radostits, Gay, Hinchcliff and Constable, 2007). However, the majorities (97-99%) practiced consumption of cooked meat, which reduces the risk of getting infected with Brucella. Overall, the lack of community awareness about brucellosis; and the habit of raw milk consumption among others might greatly contribute for further spread of brucellosis (Njeru et al., 2016).
5. Conclusion
The present study revealed the occurrence of brucellosis in both livestock and human at a low proportion in Ethiopian-Somali pastoral communities. This could be due to the clan-based segregation of animals as a mitigation measure of the risk of brucellosis transmission amongst animals and humans. Although the causes of abortion and stillbirth in herd are multi-factorial, the low presences of such cases found concomitant with that of prevalence of brucellosis in the area. However, the risk of acquiring Brucella infection is very high, particularly due to the consumption of raw milk and involvement of family members as well as neighbors on milking. Thus, public awareness among pastoralists on the transmission and health hazard of brucellosis needs to be addressed through community trainings. Further epidemiological studies with isolation and identifications of Brucella biotypes involved at the interface of livestock and human might give a clear picture on the role of livestock in zoonotic brucellosis.
Conflict of interests
None of the authors has any financial or personal relationships that could inappropriately influence or bias the content of the paper.
Acknowledgements
The Authors would like to acknowledge Ministry of Livestock and Fishery for the financial support, Haramaya University for facilitating Budget use, Somali Regional State of Ethiopia Livestock and Pastoralist Development Bureau, Jigjiga Regional Veterinary Research and Diagnostic Laboratory Office for allowing access to laboratory facilities, National Veterinary Institute (NVI) for allowing access to laboratory facilities, Somali Regional State Health Bureau and Research and Diagnostic Laboratory Office for processing of human samples, and Dire Dawa Plant and Live Animal Export Quarantine Staffs for the kind help and facilitation during the field work.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.vas.2019.100047.
Appendix. Supplementary materials
References
- Acha P.N., Szyfres B. 3rd edition. Vol. 1. Pan American Health organization; Washington D.C.: 2001. pp. 233–246. (Zoonoses and communicable diseases common to man and animals; Bacteriosis and Mycoses). [Google Scholar]
- Adugna K.E., Agga G.E., Zewde G. Sero-epidemiological survey of bovine brucellosis in cattle under a traditional production system in western Ethiopia. Revue Scientifique et Technique (Office International des Epizooties) 2013;32(3):1–20. doi: 10.20506/rst.32.2.2218. [DOI] [PubMed] [Google Scholar]
- Ahmed E.Y., Ali A., Mesfin A., Deressa A., Girmaye T. Brucellosis as a zoonosis in Chifra district, Afar Regional State, Ethiopia. Bulletin of Animal Health and Production in Africa. 2008;56:357–361. [Google Scholar]
- Arsham H. Descriptive Sampling Data Analysis. 2002. http://ubmail.ubalt.edu/harsham/Business-stat/opre504.htm#rwhyrssm Statistical Thinking for Managerial Decision Making. Retrieved October 03, 2017, from.
- Asfaw Y., Molla B., Zessin K., Azage T. A cross sectional study on bovine brucellosis and test performance in intra and peri-urban dairy production system in and around Addis Ababa. Bulletin of Animal Health and Production in Africa. 1998;46:217–224. [Google Scholar]
- Ashenafi F., Teshale S., Ejeta G., Fikru R., Laikemariam Y. Distribution of brucellosis among small ruminants in the pastoral region of Afar, eastern Ethiopia. Revue Scientifique et Technique (Office International des Epizooties) 2007;26:731–739. doi: 10.20506/rst.26.3.1781. [DOI] [PubMed] [Google Scholar]
- Asmare K., Asfaw Y., Gelaye E., Ayelet G. Brucellosis in extensive management system of Zebu cattle in Sidama Zone, Southern Ethiopia. African Journal of Agricultural research. 2010;5:257–263. [Google Scholar]
- Asmare K., Shiv P., Asfaw Y., Esayas G., Gelagaye A., Aschalew Z. Seroprevalence of brucellosis in cattle and high risk professionals in Sidama Zone, Southern Ethiopia. Ethiopian Veterinary Journal. 2007;11(1):69–84. [Google Scholar]
- Bekele M., Mohammed H., Tefera M., Tolosa T. Small ruminant brucellosis and community perception in Jijiga District, Somali Regional State, Eastern Ethiopia. Tropical Animal Health and Production. 2011;43:893–898. doi: 10.1007/s11250-011-9781-9. [DOI] [PubMed] [Google Scholar]
- Benkirane A. Ovine and caprine brucellosis: World distribution and control/eradication strategies in West Asia/North Africa region. Small Ruminant Research. 2006;62:19–25. [Google Scholar]
- Corbel, M. J, ( 2006). Food and Agriculture Organization of the United Nations, World Health Organization & World Organization for Animal Health. Brucellosis in humans and animals. Geneva: World Health Organization. http://www.who.int/iris/handle/10665/43597.
- CSA (2015). Central Statistical Agency, Agricultural sample survey (2014/15). Statistical Bulletin 578, Addis Ababa, Ethiopia.
- Dwight C.H., Yuan C.Z. Veterinary Microbiology. 1st edition. Blackwell science Ltd. Blackwell publishing company; Tokyo 104, Japan: 1999. pp. 196–203. [Google Scholar]
- Franc K.A., Krecek R.C., Häsler B.N., Arenas-Gamboa A.M. Brucellosis remains a neglected disease in the developing world: A call for interdisciplinary action. BMC Public Health. 2018;18:125. doi: 10.1186/s12889-017-5016-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gessese A.T., Mulate B., Nazir S., Asmare A. Seroprevalence of brucellosis in camels (Camelus dromedaries) in South East Ethiopia. Journal of Veterinary Science & Medical Diagnosis. 2014;3(1):1–10. [Google Scholar]
- Ghanem Y.M., El-Khodery S.A., Saad A.A., Abdelkader A.H., Heybe A., Musse Y.A. Seroprevalence of camel brucellosis (Camelus dromedarius) in Somaliland. Tropical Animal Health and Production. 2009;41(8):1779–1786. doi: 10.1007/s11250-009-9377-9. [DOI] [PubMed] [Google Scholar]
- Gumi B., Firdessa R., Yamuah L., Sori T., Tolosa T., Aseffa A., Zinsstag J., Schelling E. Seroprevalence of brucellosis and Q-fever in southeast Ethiopian pastoral livestock. Journal of Veterinary Science & Medical Diagnosis. 2013;2(1):1–5. doi: 10.4172/2325-9590.1000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hailemelekot M., Kassa T., Assfaw Y. Seroprevalence study of bovine brucellosis in Bahir Dar milk shed, Northwestern Amhara Region. Ethiopian Veterinary Journal. 2007;11(1):49–65. [Google Scholar]
- Hailu D., Mohamed M., Mussie H., Moti Y. Seroprevalence of bovine brucellosis in agro pastoral areas of Jijjiga zone of Somali National Regional State, Eastern Ethiopia. Ethiopian Veterinary Journal. 2011;15(1):37–47. [Google Scholar]
- Hamdy M.E.R., Amin A.S. Detection of Brucella species in the milk of infected cattle, sheep, goats and camels by PCR. The Veterinary Journal. 2002;163:299–305. doi: 10.1053/tvjl.2001.0681. [DOI] [PubMed] [Google Scholar]
- Hunduma D., Regassa C. Seroprevalence study of Bovine brucellosis in pastoral and Agro-Pastoral areas of East Showa Zone, Oromia Regional State, Ethiopia. American-Eurasian Journal Of Agricultural & Environmental Sciences. 2009;6:508–512. [Google Scholar]
- Mantur B.G., Amarnath S.K., Shinde R.S. Review of clinical and laboratory features of human Brucellosis. Indian Journal of Medical Microbiology. 2007;25:188–202. doi: 10.4103/0255-0857.34758. [DOI] [PubMed] [Google Scholar]
- McDermott J., Grace D., Zinsstag J. Economics of brucellosis impact and control in low-income countries. Revue Scientifique et Technique (Office International des Epizooties) 2013;32(1):249–261. doi: 10.20506/rst.32.1.2197. [DOI] [PubMed] [Google Scholar]
- McDermott J.J., Arimi S.M. Brucellosis in Sub-Saharan Africa: epidemiology, control and impact. Veterinary Microbiology. 2002;90:111–134. doi: 10.1016/s0378-1135(02)00249-3. [DOI] [PubMed] [Google Scholar]
- Megersa M., Biffa D., Niguse F., Rufael T., Asmare K., Skjerve E. Cattle brucellosis in traditional livestock husbandry practice in Southern and Eastern Ethiopia, and its zoonotic implication. Acta veterinaria Scandinavica. 2011;53:24. doi: 10.1186/1751-0147-53-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekonnen H., Shewit K., Moses K., Mekonnen A., Belihu K. Effect of Brucella infection on reproduction conditions of female breeding cattle and its public health significance in western Tigray, northern Ethiopia. Veterinary Medicine International. 2011;7:1–7. doi: 10.4061/2011/354943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memish Z.A., Mah M.W. Brucellosis in laboratory workers at a Saudi Arabian hospital. American Journal of Infection Control. 2001;29(1):48–52. doi: 10.1067/mic.2001.111374. [DOI] [PubMed] [Google Scholar]
- Mengistu M. Thesis, Addis Ababa University, Faculty of Veterinary Medicine; Debre Zeit, Ethiopia: 2007. Seroepidemiology of brucellosis in small ruminants in Southern Ethiopia, MSc. [Google Scholar]
- Nielsen K. Diagnosis of brucellosis by serology. Veterinary Microbiology. 2002;90:447–459. doi: 10.1016/s0378-1135(02)00229-8. [DOI] [PubMed] [Google Scholar]
- Njeru J., Wareth G., Melzer F., Henning K., Pletz M.W., Heller R., Neubauer H. Systematic review of brucellosis in Kenya: Disease frequency in humans and animals and risk factors for human infection. BMC Public Health. 2016;16(1):853. doi: 10.1186/s12889-016-3532-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OIE . 5th edition. Office international des Epizootics-World Organization for Animal Health; Paris: 2004. Bovine brucellosis. In: Manual of standard for diagnostic tests and vaccines; pp. 246–262. [Google Scholar]
- OIE . 6th edition. Office international des Epizootics; Paris: 2008. Bovine brucellosis. In: OIE manual of diagnostic tests and vaccines for terrestrial animals; pp. 624–659. [Google Scholar]
- Omer M.K., Asfaw T., Skjerve E., Teklegiorgis T., Woldehiwot Z. Prevalence of antibodies to Brucella spp. and risk factors related to high risk occupational group in Eritrea. Epidemiology & Infection. 2002;129:85–91. doi: 10.1017/s0950268802007215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappas G.S., Papadimitriou P., Akritidis N., Christou L., Tsianos E.V. The new global map of human brucellosis. The Lancet Infectious Diseases. 2006;6:91–99. doi: 10.1016/S1473-3099(06)70382-6. [DOI] [PubMed] [Google Scholar]
- Radostits O.M., Gay C.C., Hinchcliff W., Constable D. 10th edition. Saunders Elsevier; EdinburghLondon, New York, Oxford, Philadelphia, St Louis, Sydney, Toronto: 2007. Veterinary medicine: A text book of the disease of cattle, sheep, goats, pigs and horse; pp. 966–984. [Google Scholar]
- Samui K.L., Oloya J., Munyeme M., Skjerve E. Risk factors for brucellosis in indigenous cattle reared in livestock-wildlife interface areas of Zambia. Preventive Veterinary Medicine. 2007;80:306–317. doi: 10.1016/j.prevetmed.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Sori T. Seroprevalence of small ruminant brucellosis in selected districts of Afar and Somali pastoral areas of Eastern Ethiopia: The impact of husbandry practice. Revue de Médecine Vétérinaire. 2006;157:557–563. [Google Scholar]
- Tadesse G. Correction: Brucellosis Seropositivity in animals and humans in Ethiopia: a meta-analysis. PLOS Neglected Tropical Diseases. 2016;10(12) doi: 10.1371/journal.pntd.0005006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tekeleye B., Kasali O.B. Brucellosis in sheep and goats in Central Ethiopia. Bulletin of Animal Health and Production in Africa. 1990;38:23–25. [Google Scholar]
- Tesfaye A. Faculty of Veterinary Medicine, Addis Ababa University; Debre-Zeit, Ethiopia: 2003. DVM Thesis. [Google Scholar]
- Teshome H., Molla B., Tibbo M. A seroprevalence study of camel brucellosis in three camel rearing regions of Ethiopia. Tropical Animal Health and Production. 2003;35:381–389. doi: 10.1023/a:1025874310261. [DOI] [PubMed] [Google Scholar]
- Thrusfield M.V. 3rd edition. Published by Black Well science Ltd.; Edinburgh, UK: 2005. Veterinary epidemiology; pp. 229–250. [Google Scholar]
- Tibesso G., Ibrahim N., Tolosa T. Seroprevalence of bovine and human brucellosis in Adami Tulu, Central Ethiopia. World Applied Sciences Journal. 2014;31(5):776–780. [Google Scholar]
- Tolosa T. Faculty of Veterinary Medicine, Addis Ababa University; Debre-Zeit, Ethiopia: 2004. MSc Thesis. [Google Scholar]
- Muhie M. Faculty of Veterinary Medicine, Addis Ababa University; Debre- Zeit, Ethiopia: 2005. DVM Thesis. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.