Court-involved youth are at particular risk for Human Immunodeficiency Virus (HIV) and other sexually transmitted infections (STIs) due to high rates of engagement in risky sexual behaviors (Teplin, Mericle, McClelland, & Abram, 2003). Compared to the general adolescent population, court-involved youth engage in significantly more risky sex behaviors (Elkington et al., 2015), including earlier onset of sexual activity (Moser, 2011), infrequent condom use, and sex with multiple partners (Teplin et al.,, 2005). Parenting practices during adolescence can significantly buffer against youth engagement in sexual risk behaviors (Teitelman, Ratcliff, & Cederbaum, 2008). For court-involved youth, however, parenting practices may be compromised due to factors such as the youth’s delinquency (Gault-Sherman, 2012), parent substance use and mental health problems (Brown et al., under review), and poorer family functioning (Elkington et al., 2015). However, the pathways through which such factors diminish parenting practices for court-involved youth are not clearly defined. Studying these pathways is vital to strengthening parenting practices that can protect against adolescent sexual risk behavior and HIV/STI risk, particularly within families of court-involved youth (Elkington et al., 2015).
Parenting practices have been shown to significantly impact adolescent sexual attitudes and behaviors. For example, parent-adolescent communication, especially about using condoms, has been linked to increased condom use among sexually active adolescents as well as adolescents feeling more open to discussing sex with their parents (Hadley, et al., 2009). Additionally, close parental monitoring of general adolescent activities and peer associations has been associated with delayed onset of sexual activity, safer sex practices, and improved adolescent-intimate partner communication (for a review, see Perrino, Gonzalez-Soldevilla, Pantin, & Szapocznik, 2000). Conversely, inadequate parental support is a documented risk factor for youth engagement in risky sexual behaviors, including early onset of sexual activity (Conduct Problems Prevention Research Group, 2014; Price & Shibley Hyde, 2009) and multiple sexual partners (Gordon Simons, Sutton, Simons, Gibbons, McBride Murry, 2016).
There exist many barriers to engaging in effective parental monitoring and communication about sex, especially for parents with court-involved youth. Parent mental health consistently emerges as a family-based factor that impairs these parenting practices. Compared to parents without mental health problems, those with mental health issues have been shown to demonstrate poorer parental monitoring, less positive parent-child interactions, and more negative behaviors towards their children (Van Loon, Van de Ven, Van Doesum, Witteman, & Hosman, 2014). Mental illness may diminish available faculties a parent needs to monitor their child or be emotionally available and nurturing (Goodyear et al., 2015; Van Loon et al., 2014). Few studies have examined parent mental health among parents of court-involved youth; however, existing literature indicates heightened rates of parent alcohol abuse (Barylnik, 2003; Dembo, et al., 2000; Lederman, Dakof, Larrea, & Li, 2004), other problematic substance use (Dembo et al., 2000; Lederman et al., 2004), and mental health symptoms (Brown et al., under review). One recent report found that nearly one-third of parents of court-involved youth met criteria for clinically significant mental health problems and that these parents, compared to parents without clinically significant mental health symptoms, also reported higher levels of parenting stress (Brown et al., under review). Adolescent legal involvement may significantly burden parents who are not adequately prepared to manage the additional strain of complying with court orders to reduce their youth’s likelihood of recidivating (Brown et al., under review)—potentially placing strain on parents’ psychological well-being, parent-child relationships, and the family.
Family functioning may help to explain the effect of parent mental health on specific parenting practices that are instrumental in reducing adolescent risky sex behaviors. Parenting practices, specifically communication and monitoring, are components of family functioning (Sheidow, Henry, Tolan, & Strachan, 2014). However, family functioning is a multifaceted construct, beyond just parenting practices, and concerns the overall health and pathology of the family environment. Specifically, family functioning refers to the structural and organizational properties of the family environment, such as fulfilment and management of roles and daily responsibilities, as well as interactions between family members, including how members communicate and emotionally connect (Epstein, Baldwin, & Bishop, 1983; Rhee, 2008). Recent research calls for a broader examination of family functioning that not only studies parenting practices, but includes additional factors comprising the construct, such as cohesiveness, beliefs, and structure (Sheidow et al., 2014). A parent’s mental illness not only impacts parent-child interactions and relationships, but also influences other family members’ interactions and relationships. Parent psychopathology and distress can have different effects on several family factors (Van Loon et al., 2014). Adolescents are more likely to experience externalizing and internalizing behaviors, demonstrate deviant behavior, and be at higher risk for developing a substance use disorder if they have a parent with a mental illness or substance use disorder (Finan, Schulz, Gordon, & McCauley Ohannessian, 2015; Nijjar, Ellenbogen, & Hodgins, 2016; Tandon, Tillman, Spitznagel, & Luby, 2014; Van Loon et al., 2014). Families with a mentally ill parent also show lower levels of family expressiveness and report greater family conflict compared to those without a mentally ill parent (Horwitz, Briggs-Gowan, Storfer-Isser, & Carter, 2007; Van Loon et al., 2014). Taken together, studies suggest that parent mental illness weakens certain facets of family functioning (Van Loon et al., 2014) that have been shown to be effective in reducing risky sex behaviors among high-risk adolescent populations (Diiorio et al., 2006; Elkington et al., 2015; Prado, et al., 2007; Stanton et al., 2004).
Studies have not clearly identified pathways through which parent mental illness and family functioning impair parenting practices, specifically parent-child communication and parental monitoring, known to be protective against adolescent sexual risk behaviors. Thus, the primary aim of this study was to investigate whether associations exist among parent mental health symptoms, family functioning, and parenting practices, specifically parent-child sex communication and parental monitoring, within families of court-involved youth. We hypothesized that parents of court-involved youth who reported heightened mental health symptoms and poorer family functioning would report poorer parenting practices, including less parent-child sex communication and less parental monitoring. We also explored whether there exists an indirect effect of family functioning on the hypothesized association between parental mental health and parenting practices. See Figure 1 for a visual depiction of the primary models analyzed in this study.
Figure 1. Direct and Indirect Effects of Parent Mental Health Symptoms on Parenting Practices through Family Functioning.
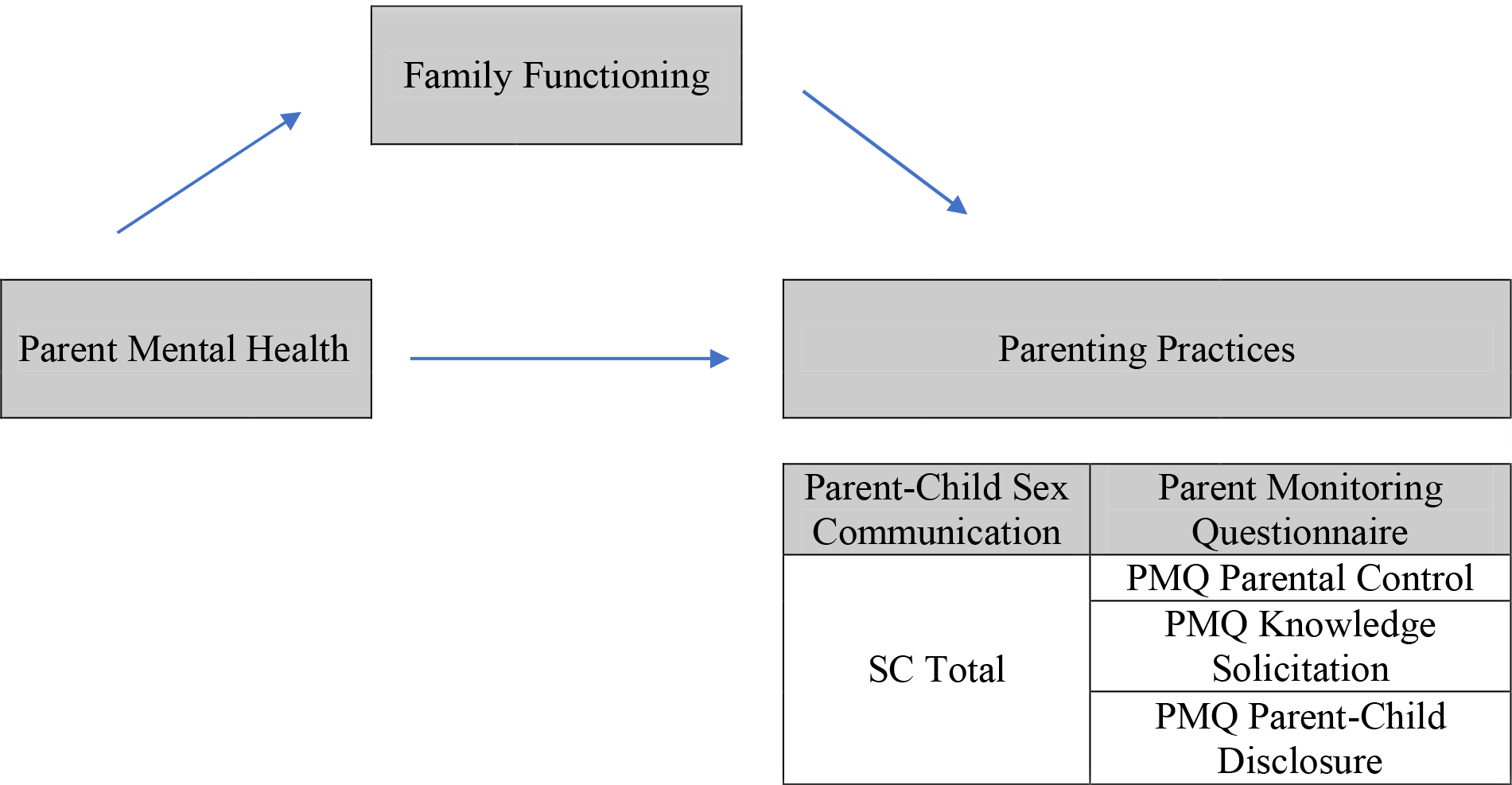
Note. SC = Parent Child Sexual Communication questionnaire; PMQ = Parental Monitoring Questionnaire.
Methods
Procedures
All study protocols were approved by the Institutional Review Boards (IRBs) of the two sites conducting research for this study. Participants were recruited to participate in a longitudinal randomized controlled trial comparing a new integrated mental health treatment and HIV prevention program to standard mental health counseling received in the community. Research participation was completely separate and voluntary from a youth’s court involvement. Prior to and throughout study enrollment, research staff assured that the court understood it could not mandate youth and families into the experimental intervention and prevention program. If the court ordered the youth to participate in therapy, families were allowed to choose between participation in the integrated mental health intervention and HIV prevention program or any other community-or clinic-based mental health treatment. Adolescent assent and parental consent were obtained for the study. Parent and adolescent participants completed assessment measures on laptop computers using an audio computer-assisted self-interview (ACASI) program. Approximately 78% of parent-adolescent dyads completed the assessment in their home (n = 121), 12% at the court (n = 18), 5% at the hospital clinic (n = 8), and another 5% in the community (n = 8). All parent-adolescent dyads completed the intervention within the hospital or court clinic setting. Current research questions were analyzed using baseline parent self-report data.
Participants
Participants were parent and adolescent dyads recruited in two eastern U.S. cities. Parental eligibility to participate was based upon the adolescent being referred by the court for mental health treatment. Inclusion criteria for adolescents included: 1) being between the ages of 11 and 17 at the time of the consent; 2) ability to speak and read English (adolescent and parents) or Spanish (parents only); 3) currently residing with a legal guardian able to attend weekly therapy sessions; and 4) having an open petition with the partnering Family Court at the time of referral. Adolescents were excluded if they: 1) were diagnosed with obsessive-compulsive disorder (OCD) or pervasive developmental disorders; 2) were already engaged in outpatient mental health treatment; 3) had a history of psychotic symptoms requiring specialized or intensive treatment; or 4) were charged with a sexual offense. Adolescents were excluded if they were diagnosed with OCD or other pervasive development disorders as the experimental treatment under evaluation did not offer the evidence-based interventions (e.g., cognitive-behavior therapy with exposure and response prevention for OCD; Rojas, 2016; Applied Behavior Analysis for autism spectrum disorders; Leaf et al., 2016) to address the symptoms of these types of psychiatric diagnoses. Additionally, youth with sexual offenses were excluded as the intervention under evaluation did not support the evidence-based treatment models found to be effective in working with juvenile sex offenders [e.g., Multisystemic Therapy for Problem Sexual Behavior (MST-PSB); Borduin, Letourneau, Henggeler, & Swenson, 2005]. Court officials (i.e., intake worker, probation officer, magistrate, judge) referred adolescents to the study when mental health services were thought to be appropriate for the case. Participants were then screened by research assistants to determine eligibility. Inclusion criteria required that parents lived in the same household with the adolescent for at least six months prior to consent in order to sufficiently complete family-based questionnaires and engage in family-based intervention. Parents were excluded if they were not the legal guardian of the adolescent as such adults could not provide study consent for their adolescent. Court officials referred a total of 598 adolescents and parents to the study from November 2011 to April 2015. Of the 598 referrals received, 53% (n = 317) were eligible to participate based upon the screening. The primary reasons for exclusion were the parent being unable to attend the weekly sessions (38%, n = 107), the adolescent needing a higher level of care (22%, n = 62), or the adolescent already being engaged in treatment (14%, n = 40). Of those eligible, 54% (n = 170) consented to participate in the study. The sample for this study includes data from 157 parents who have valid baseline data for the variables under investigation.
Adolescents were, on average, 15.19 years old (SD = 1.35 years) and 41% identified as female. Parents were mostly female (80%) with average age of 43.78 years (SD = 8.38). Parents identified their race as White (73.8%), Native Hawaiian or Pacific Islander (9.2%), Black/African American/Haitian (8.5%), Asian (6.4%), and American Indian/Alaska Native (2.1%). Sixteen percent of parents ethnically identified as Hispanic/Latino. Almost half of parents reported an annual household income of $30,000 or less (45.7%) and roughly one-third endorsed having obtained at least a college degree (30.9%). Of parent participants, 80% were female (n = 130) and 19.8% were male (n = 32). The majority of female parents (93.5%) identified as the adolescent participant’s natural birth mother with 3.2% identifying as a grandmother, 1.6% as an aunt, 0.8% as an adoptive mother, or 0.8% as a step-mother. The majority of male parents (90.3%) identified as the adolescent participant’s natural birth father with 3.2% identifying as a grandfather, 3.2% as an adoptive father, and 3.2% as a step-father. Of the 40 parents (24.3% of total sample) who endorsed being diagnosed with a psychiatric disorder, 32.5% reported an anxiety disorder, 22.5% depressive disorder, 7.5% substance use disorder, 2.5% personality disorder, 27.5% reported multiple diagnoses, and 7.5% were unable to identify a specific psychiatric diagnosis. Approximately one-third (38%) of parents’ GSI scores (see Measures section for description of GSI) surpassed the GSI clinical cut-off (T scores ≥ 70), indicating potentially clinically significant mental health symptoms. Table 1 provides means, standard deviations, and ranges for primary study variables.
Table 1.
Descriptives for Main Study Variables
| M (SD) | Range | |
|---|---|---|
| 1. GSI | 0.75 (0.68) | 0 to 3.76 |
| 2. FAD General Functioning | 26.62 (6.26) | 12 to 41 |
| 3. SC Total | 32.51 (6.40) | 14 to 42 |
| 4. PMQ Parental Control | 6.99 (3.58) | 5 to 25 |
| 5. PMQ Parental Knowledge Solicitation | 12.26 (4.60) | 5 to 23 |
| 6. PMQ Parent-Child Disclosure | 12.58 (4.53) | 5 to 23 |
Note. GSI = Global Severity Index of the SCL-90-R; FAD = Family Assessment Device; SC = Parent Child Sexual Communication questionnaire; PMQ = Parental Monitoring Questionnaire. Higher scores on SC Total scale indicate more overall parent-child sex communication. Lower scores on PMQ correspond to more parent control over adolescent behavior, more favorable parent impressions of being able to solicit information from their adolescent, and more favorable parent impressions of their adolescent’s willingness to disclose information about their behavior to them.
Measures
Sociodemographics included parent self-report of: parent gender (male/female), race (White/Other/Native Hawaiian or Pacific Islander/African American or Black/Asian/Alaskan Native or American Indian), ethnicity (Hispanic/Latino: yes/no), psychiatric diagnosis (anxiety/depression/substance use/personality/multiple diagnoses) and household annual income (≤ or > $30,000). For the purposes of this study, adolescent self-reported gender (male/female) and age were included as covariates (see Data Analytic Strategy below).
Parent Mental Health
Psychiatric diagnosis.
Parents were asked to report if a physician had ever diagnosed them with a psychiatric disorder and, if so, indicated which disorder(s) (i.e., depressive disorder, bipolar disorder, anxiety disorder, psychosis, substance abuse, personality disorder). Parent psychiatric diagnosis is reported to provide more specific context regarding symptoms endorsed as part of the overall parent GSI score used in this study’s analyses.
Symptom Checklist-90-Revised (SCL-90-R).
The SCL-90-R (Derogatis, 1975) is a 90-item measure that assesses mental health symptom severity experienced over the past week (e.g., “How much were you distressed by nervousness and shakiness inside?”). The SCL-90-R measures nine dimensions of psychopathology (e.g., obsessive-compulsive, depression, anxiety) and has three supplementary global indices of symptom severity. The Global Severity Index (GSI) is the overall index of general psychological symptomatology on the SCL-90-R and is the sum of the nine symptom dimensions and any additional items divided by the total number of responses on the SCL-90-R (Derogatis & Melisaratos, 1983; Hardt, Gerbershagen, & Franke, 2000; Lam, Naar-King, & Wright, 2007). For the purposes of this study, we used the GSI as an index of overall parent mental health symptomatology. Responses for the SCL-90-R range from 0 (not at all) to 4 (extremely) on a 5-point Likert-scale. Higher scores represent higher levels of psychological distress and greater mental health symptomatology. Those parents with scores above the GSI clinical cut-off (T score ≥ 70) were considered to have “clinically significant” mental health symptoms as establishing a diagnosis is beyond the scope of any screening instrument (Brown et al., 2015). The reliability and construct validity of this measure have been repeatedly demonstrated since the development of the scale (Derogatis and Unger, 2010). The internal consistency of the GSI for the current sample was adequate (α = .98).
Family Functioning
Family Assessment Device (FAD).
The FAD (Epstein, Baldwin, & Bishop, 1983) includes 60 items that assess parent perception of family functioning. The FAD consists of six scales that assess the six dimensions of the McMaster Model of Family Functioning (affective involvement, affective responsiveness, behavioral control, communication, problem solving, and roles). The present study used the general family functioning scale, which consists of 12 statements about family communication and support (e.g., “We don’t get along well together.”). Parents rate how well statements describe their family using a 4-point Likert-scale (responses range from 1 = strongly disagree to 4 = strongly agree). Higher scores on this scale represent lower levels of family functioning (i.e., more family dysfunction). Adequate reliability (α =.72 – 92; r =.66 – .76) and validity have been established (Epstein, Baldwin, & Bishop, 1983). For the current sample, internal consistency for the FAD General Functioning scale was α = .88.
Parental Monitoring Questionnaire (PMQ).
The PMQ (Stattin & Kerr, 2000) is a 24-item questionnaire designed to assess parental monitoring and sources of parental knowledge. Parents responded to questions regarding parent-child disclosure (e.g., “Does your child keep a lot of secrets from you about what they do during their free time?”), parental knowledge solicitation (e.g., “During the past month, how often have you started a conversation with your child about their free time?”), and parental control (e.g., “Does your child need to have permission to stay out late on a weekday evening?”). Responses for the measure range from 1 (almost always) to 4 (never) on a 4-point Likert-scale, with higher scores representing lower levels of parental monitoring. The monitoring subscale has demonstrated good reliability (α = .82 for parents) and correlates with adolescent internalizing and externalizing maladjustment, deviant peer relationships, and family discord (Stattin & Kerr, 2000). For this sample, internal consistencies were α = .71 for the PMQ Parent-Child disclosure, α = .72 for the Parental Knowledge Solicitation scale, and α = .78 for the PMQ Parental Control scale.
Parent Child Sexual Communication (SC).
The SC questionnaire (Baker, Thalberg, & Morrison, 1988) includes 48 items that assess parents’ general communication regarding adolescents’ sexual behavior (e.g., “I know how to talk to my teen about topics regarding sex; responses range from 1 = not true to 7 = very true), how helpful parents perceive conversations about sex with their adolescent (e.g., “How helpful do you think your discussions about when it is appropriate to start having sex were? ”; responses range from 1 = not at all helpful to 7 = very helpful), parent and teen comfort during conversations with adolescents about sex (e.g., “How comfortable did you feel when you discussed this topic of condoms with your teen?”; responses range from 1 = not at all comfortable to 7 = very comfortable), and conversations about adolescent sexual activity and history (e.g., “Have you ever talked to your teen about how to handle sexual peer pressures by his/her friends, or potential sex partners?”; yes/no). For the purposes of analyses, SC Total scale scores were utilized. Higher scores on this scale represent greater frequency of positive communication about sexual behaviors. Internal reliability estimates range from .73 to .93 (Baker et al., 1988). This sample produced an internal consistency of α = .68 on the SC Total scale.
Data Analytic Strategy
Preliminary analyses consisted of descriptive statistics and bivariate correlations between all study variables. Although data from adolescent participants were available for analysis, this study focused solely on parent participants’ data as study findings are intended to inform parent-specific interventions addressing parent mental health and parenting practices within samples of court-involved youth and their families. To examine the direct effect of parent mental health on parenting practices and the indirect effect of parent mental health on parenting practices through family functioning, multiple linear regression analyses were conducted in SPSS 24 (IBM, 2016) using the computational tool PROCESS (Hayes, 2013). Parent gender (male/female) and race (White vs. non-White), annual household income, and adolescent gender (male/female) and age were simultaneously entered into the regression models as covariates.
We followed procedures recommended by Hayes (2013), using the PROCESS macro for SPSS 24 (IBM, 2016), to test the significance of indirect effects. PROCESS implements bootstrapping—a nonparametric method that takes large resamples of the original sample—from which is calculated a standardized indirect effect statistic and 95% biased-corrected confidence intervals (MacKinnon, Lockwood, & Williams, 2004; Williams & MacKinnon, 2008). Parameter estimates and confidence intervals of the total and indirect effects were generated from 1,000 random samples. Significant indirect effects are said to have occurred if the 95% bias-corrected confidence interval for the parameter estimate, representing the indirect effect, does not contain zero (Hayes, 2013). As recommended by Preacher and Kelley (2011), we used κ2 to measure the effect size of indirect effects with small, medium, and large effect sizes interpreted as 0.01, 0.09, and 0.25.
A missing data variable was created and correlated with all study variables to determine if parent characteristics were associated with the probability of being excluded from analyses due to listwise deletion. No parent characteristics [i.e., parent gender, household income (i.e., ≤ $30,000 or > $30,000, race (i.e., White vs. non-White)] were significantly associated with being excluded from analyses. Approximately 15% (n = 23) of cases were excluded from the final models due to missing data resulting in a total analyzed sample size of N = 134.
Preliminary analyses were conducted to test the assumptions of the planned analyses. Correlations between predictor variables (i.e., GSI and FAD General Family Functioning scores) did not exceed .7, and tolerance statistics were within acceptable ranges for all variables, indicating no significant multicollinearity. Visual inspection of the data (i.e., histograms and Q-Q plots) and descriptive statistics (skewness and kurtosis) indicated that PMQ Control scores were positively skewed. To correct for non-normal distribution of the dependent variable, several transformations [i.e., logarithmic (log10), square root, inverse] were performed on PMQ Control scores. The inverse transformation reduced the greatest amount of PMQ Control scores’ positive skew. However, non-transformed PMQ Control scores were retained in the final model as inclusion of the transformed PMQ Control scores did not lead to significantly different findings.
Results
Associations among Parent Mental Health Symptoms, Family Functioning, and Parenting Practices (See Table 2)
Table 2.
Correlations among Main Study Variables
| 2 | 3 | 4 | 5 | 6 | ||
|---|---|---|---|---|---|---|
| 1. | GSI | .24** | .16 | .18* | .06 | .06 |
| 2. | FAD General Functioning | - | −.18* | .13 | .22** | .39** |
| 3. | SC Total | - | −.07 | −.43** | −.47** | |
| 4. | PMQ Parental Control | - | .27** | .13 | ||
| 5. | PMQ Parental Knowledge Solicitation | - | .46** | |||
| 6. | PMQ Parent-Child Disclosure | - |
Note. GSI = Global Severity Index of the SCL-90-R; FAD = Family Assessment Device; SC = Parent Child Sexual Communication questionnaire; PMQ = Parental Monitoring Questionnaire.
p < .05.
p < .01.
Parent mental health symptoms were significantly associated with family functioning, such that more parent mental health symptoms were associated with more family dysfunction (r = .24, p = .002). Parent mental health symptoms were significantly associated with only one parenting practice, such that greater mental health symptoms were associated with parents’ perception of lesser control of or influence on their adolescent’s behavior (r = .18, p = .03). Family functioning was associated with two parenting practices. Greater family dysfunction was significantly associated with lower frequency of parent-child sex communication (SC Total: r = − .18, p = .02), less favorable parent impressions of how well they can solicit information from their adolescent (PMQ Parental Knowledge Solicitation: r = .22, p = .01), and less favorable parent impressions of their adolescent’s disclosure of information to them (PMQ Parent-Child Disclosure: r = .39, p < .001). For further interpretation of negative and positive correlations, see the Measures section for descriptions of scoring for the PMQ and SC questionnaire.
Indirect Effect of Parent Mental Health Symptoms on Parent-Child Sex Communication through Family Functioning
Results did not confirm a significant indirect effect of parent mental health symptoms on overall parent-child sex communication through family functioning, SC Total: β = −0.56, p = .08, CI (−1.27, −0.13), κ2 = 0.06. Greater parent mental health symptoms were significantly related to greater family dysfunction, β = 2.80, t(127) = 3.30, p = .001, and greater family dysfunction was significantly related to lower frequency of parent-child sex communication, SC Total; β = −0.20, t(126) = −2.18, p = .03. Table 3 provides unstandardized direct and indirect estimates for all study models.
Table 3.
Unstandardized Direct and Indirect Effect Estimates of Parent Mental Health on Parenting Practices through Family Functioning
| b | 95% CI | P | κ2 | |
|---|---|---|---|---|
| Direct Effects | ||||
| GSI - SC Total | 0.97 | −0.85 to 2.80 | .29 | - |
| GSI - PMQ Parental Control | 0.54 | −0.47 to 1.55 | .29 | - |
| GSI - PMQ Parental Knowledge Solicitation | 0.00 | −1.33 to 1.33 | 1.00 | - |
| GSI - Parent-Child Disclosure | 0.07 | −1.13 to 1.28 | .90 | - |
| Indirect Effects | ||||
| GSI - Family Functioning - SC Total | −0.56 | −1.27 to −0.13 | .08 | 0.06 |
| GSI - Family Functioning - PMQ Parental Control | 0.12 | −0.12 to 0.42 | .44 | 0.02 |
| GSI - Family Functioning - PMQ Parental Knowledge Solicitation | 0.48 | 0.13 to 1.11 | .05 | 0.07 |
| GSI - Family Functioning - PMQ Parent-Child Disclosure | 0.85 | 0.36 to 1.57 | .01 | 0.13 |
Note. GSI = Global Severity Index of the SCL-90-R; SC = Parent Child Sexual Communication questionnaire; PMQ = Parental Monitoring Questionnaire.
Indirect Effect of Parent Mental Health Symptoms on Parental Monitoring through Family Functioning
Results confirmed significant indirect effects of parent mental health symptoms on parental monitoring through family functioning. This was evident for parent impressions of their adolescent’s disclosure of information to them, PMQ Parent-Child Disclosure: β = 0.85, p = .01, CI (0.36, 1.57), κ2 = 0.13. The indirect effect of parent mental health symptoms on parents’ solicitation of information from their adolescent through family functioning neared significance, PMQ Parental Knowledge Solicitation: β = 0.48, p = .05, CI (0.12, 1.11), κ2 = 0.07. For the PMQ Parent-Child Disclosure scale, greater parent mental health symptoms were significantly related to more family dysfunction, β = 2.80, t(127) = 3.30, p = .001, and greater family dysfunction was significantly associated with less favorable parent impressions of their adolescent’s disclosure of information to them, PMQ Parent-Child Disclosure: β = 0.31, t(126) = 5.00, p < .001. For the PMQ Parental Knowledge Solicitation scale, greater parent mental health symptoms were significantly related to more family dysfunction, β = 2.80, t(127) = 3.30, p = .001, and greater family dysfunction was significantly associated with less parent solicitation of information from their adolescent about their behaviors, PMQ Parental Knowledge Solicitation: β = 0.17, t(126) = 2.56, p = .01. Table 3 provides unstandardized direct and indirect estimates for all study models.
Discussion
Improving parenting practices is critical for court-involved youth and families. To date, no studies have examined the impact of parent mental health status and family functioning on parent-child communication and parental monitoring—two parenting practices that are known to protect youth from adverse sexual outcomes (Perrino et al., 2000). Consistent with study hypotheses and existing literature that have revealed significant associations between poorer family functioning and parent internalizing symptoms (Krug, Wittchen, Lieb, Beesdo-Baum, & Knappe, 2016) as well as parent substance abuse (Finan et al., 2015), the present study also found that greater parent mental health symptoms were associated with worse family functioning. Dysfunctional family environments can disrupt normative adolescent developmental processes and lead to negative adolescent physical and mental health outcomes, such as increased depressive symptoms (Kim, Viner-Brown, & Garcia, 2007) and lower cognitive functioning (Ybarra, Wilkens, & Lieberman, 2007). Family functioning also appears to serve a vital role in the association between parent and child psychological problems, with some studies finding that family dysfunction mediates the relation between parent psychopathology and youth internalizing and externalizing disorders (Brennan, Hammen, Katz, & Le Brocque, 2002; Burstein, Stanger, & Dumenci, 2012; Grekin, Brennan, & Hammen, 2005). Thus, the family serves an integral role in adolescent development—both maladaptive and healthy. Identifying and addressing factors that contribute to difficulties in the family environment, such as parent mental health symptoms in this study, is key to designing and implementing effective family-based behavioral health interventions.
Notably, parent mental health was weakly or not at all directly associated with the parenting practices examined in this study—a finding that is inconsistent with study hypotheses and previous research establishing direct associations between parent mental illness and poorer parenting practices (for a review, see Van Loon et al., 2014). However, parents with more mental health symptoms endorsed more family dysfunction. Subsequently, more family dysfunction was associated with perceived less disclosure from their child, whether through being less adept at soliciting the information (as parent) or their child being less willing to disclose. These study findings may suggest that family functioning serves as one mechanism through which parent mental health compromises positive parenting practices. Parents with psychiatric impairments tend to have difficulty communicating, interacting, and monitoring their children and experience greater family conflict (Van Loon et al., 2014). Most existing family-based treatments currently used in the juvenile justice system bring the family, as a whole, into treatment, but do not directly treat parents’ emotional and/or mental health distress (National Institute of Justice, 2011). As an exception, Multisystemic Therapy (MST) directly addresses parents’ substance abuse or untreated mental illness because these are theoretically conceptualized as potential barriers to effective parenting (MST Services, Inc., 2007). MST recommends evidence-based treatments to parents for their specific illness, such as Community Reinforcement Approaches for substance abusing parents (Meyers, Roozen, & Smith, 2011), as well as collaborates with parents on devising and implementing strategies for managing high levels of stress that compromise parental monitoring and supervision (e.g., enlisting additional supports to watch elderly relatives or engaging youth in extracurricular activities; MST Services, Inc., 2007). Family-based adolescent sexual risk reduction interventions used with court-involved youth and families that directly address parent mental health problems may be more effective in reducing youth sexual risk behaviors. Providing appropriate services and support to parents in psychiatric distress may enable parents to more actively participate in their child’s treatment, thereby facilitating use of parenting skills learned in treatment that mitigate youth sexual risk-taking. Additionally, directly targeting parental mental health in family-based adolescent sexual risk reduction interventions may strengthen family processes that promote communication and trust between youth and parents.
There remain few family-based mental health and substance use interventions targeting co-occurring HIV/STI risk behaviors for court-involved youth (Letourneau, McCart, Sheidow, & Mauro, 2017; Tolou-Shams et al., 2017). Those that do have demonstrated reductions in adolescent STIs, sexual risk behaviors, and other risk factors (e.g., substance use) (Liddle, Rowe, Dakof, Henderson, & Greenbaum, 2009; Tolou-Shams et al., 2017). Our findings suggest that family-based HIV/STI prevention interventions for court-involved youth should consider parent emotional and mental wellbeing when attempting to modify existing parenting practices (e.g., parent-child communication) and improve family functioning, as both are instrumental for adolescent sexual risk reduction.
Limitations
Theoretical and empirical work guided the direction of our proposed models; however, use of cross-sectional data limits our ability to infer directionality and causality in this model. Additionally, the 54% of parent-youth dyads who consented to participate in the study may have been characteristically distinct from the 46% who declined study participation due to various factors that made them more willing to volunteer for study participation (e.g., higher education levels; younger, female, and non-authoritarian parents; religious affiliation; or maladjusted family life; Rosenthal & Rosnow, 2008). However, no data were collected on those who declined study participation, which limits our ability to statistically identify and further explore the factors separating those who consented in this study from those who declined participation. In addition, our court-involved sample was recruited from only two courts in two states in the Northeastern region of the United States; thus, results may not be as generalizable to other regions in the United States and/or patterns may not be similar to those observed in other court-involved youth and parent samples. English was a requirement for both adolescents and parents as this was the first evaluation of the intervention’s effectiveness and is not yet available in other languages. This too may limit intervention generalizability to other court-involved youth and family samples given that nearly one-fifth of cases handled by juvenile courts in 2014 involved Hispanic youth (Sickmund, Sladky, & Kang, 2017) who may have had monolingual Spanish-speaking parents. Lack of strong, direct associations between parent mental health and parenting practices may reflect variations in methodology and measures of parent psychiatric status used across studies as well as unique study population differences. For example, justice-involved families, compared to families without justice system involvement, may experience multiple social and structural adversities, such as single-parent homes, involvement in the child welfare system, interruption in public financial assistance, and parental incarceration (Akesson et al., 2012; Perkins-Dock, 2001), that may influence the magnitude of the direct association between parent mental health and parenting practices. Differences in our findings relative to prior studies may also be related to the fact that GSI score was used as our index of mental health symptoms. It is possible that other subscales of the SCL-90 may show significant and direct associations with parenting practices. The absence of a clearer and stronger direct relationship between parent mental health and parenting practices may be accounted for by the high percentage of parents in this sample who endorsed enrollment in mental health treatment. In another study using this sample of court-involved youth and parents, Brown and colleagues (under review) found that 35% of parents endorsed clinically significant psychological distress of which nearly one-half also reported receiving mental health or substance use treatment. Given that we used parent self-report data, self-report bias of parenting practices may have influenced findings (e.g., inflated ratings of their own parenting practices). For example, parents tended to positively rate (i.e., reported a higher frequency) the degree to which they appropriately communicated with their youth about sex and monitored their youth’s activities. However, given that the goal of this study was to inform parent-based intervention, it was most relevant to analyze data using the parent’s self-perception of parenting practices and family functioning.
Conclusions
The efficacy of family-based mental health and/or substance use treatment for court-involved youth may be compromised if parent mental health is not directly addressed. Our findings suggest that the development and testing of more holistic approaches to sexual health programming for court-involved youth may be warranted, such as family-based interventions that simultaneously and directly treat parents’ mental health needs. Directly addressing parent mental health needs may improve parent-child relationships vital to preventing adolescent sexual risk-taking by strengthening family processes (e.g., cohesion, affective expression and responsiveness, and roles) that contribute to family environments supportive of adolescent sexual safety (Perrino et al., 2000; Tolou-Shams et al., 2017). Although greater clinical resources for the testing and implementation of such models may be needed relative to traditional family-based treatment models, the one empirically supported model that has addressed parent mental health in some way (e.g., MST) has demonstrated greater long-term improvements in youth outcomes as well as cost-effectiveness (MST Services, Inc., 2015).
Acknowledgements
This work was supported by National Institutes of Health grant R01 MH087520 (PI: Brown); Providence Boston Center for AIDS Research P30 AI 042853 (PI: Cu-Uvin); Health Services Research Administration grant G02HP27926 (PI: McQuaid). The funding organizations are public institutions and had no role in the conduct and design of the study; the collection, analysis and interpretation of the data; preparation or approval of the report; or the decision to submit the article for publication. The authors of this manuscript report no potential conflicts of interest. The views expressed herein are those of the authors and not necessarily those of the National Institutes of Health, Providence Boston Center for AIDS Research, or Health Services Research Administration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akesson B, Smyth JM, Mandell DJ, Doan T, Donia K, & Hoven CW (2012). Parental involvement with the criminal justice system and the effects on their children: A collaborative model for researching vulnerable families. Social Work in Public Health, 27, 148–164. doi: 10.1080/19371918.2012.629898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker SA, Thalberg SP, & Morrison DM (1988). Parents’ behavioral norms as predictors of adolescent sexual activity and contraceptive use. Adolescence, 23, 265–282. [PubMed] [Google Scholar]
- Barylnik J (2003). Psychopathology, psychosocial characteristics and family environment in juvenile delinquents. German Journal of Psychiatry, 6, 30–32. [Google Scholar]
- Borduin CM, Letourneau EJ, Henggeler SW, & Swenson C (2005). Treatment manual for Multisytemic Therapy with juvenile sexual offenders and their families (2nd edition). Unpublished manual, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina. [Google Scholar]
- Brennan PA, Hammen C, Katz AR, & Le Brocque RM (2002). Maternal depression, parental psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Clinical Psychology, 70, 1075–1085. doi: 10.1037/0022-006X.70.5.1075 [DOI] [PubMed] [Google Scholar]
- Brown LK, Tarantino N, Tolou-Shams M, Healy MG, Craker L, & Esposito-Smythers C (under review). Mental health symptoms and parenting stress of parents court-involved youth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Whiteley L, Harper GW, Nichols S, Nieves A, & The ATN 086 Protocol Team for the Adolescent Medicine Trials Network for HIV/AIDS Interventions. (2015). Psychological symptoms among 2032 youth living with HIV: A multisite study. AIDS Patient Care and STDS, 29, 212–219. doi: 10.1089/apc.2014.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burstein M, Stanger C, & Dumenci L (2012). Relations between parent psychopathology, family functioning, and adolescent problems in substance-abusing families: Disaggregating the effects of parent gender. Child Psychiatry and Human Development, 43, 631–647. doi: 10.1007/s10578-012-0288-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conduct Problems Prevention Research Group (2014). Trajectories of risk for early sexual activity and early substance use in the fast track prevention program. Prevention Science, 15 (Supplement 1), S33–S46. doi: 10.1007/s11121-012-0328-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Wothke W, Seeberger W, Shemwell M, Pacheco K, Rollie M, …Livingston S (2000). Family problem factors on high-risk youths’ troubled behavior: A three-wave longitudinal study. Journal of Psychoative Drugs, 32, 55–65. [DOI] [PubMed] [Google Scholar]
- Derogatis L (1975). SCL-90-R (Symptom Checklist-90-Revised): Administration, scoring, and procedures manual. Minnetonka, MN: National Computer Systems. [Google Scholar]
- Derogatis LR & Melisaratos N (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13, 595–605. doi: 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Unger R (2010). Symptom Checklist-90-Revised. Corsini Encyclopedia of Psychology: 1–2. doi: 10.1002/9780470479216.corpsy0970 [DOI] [Google Scholar]
- Diiorio C, Resnicow K, McCarty F, De AK, Dudley WN, Wang DT, & Denzmore P (2006). Keepin’ it R.E.A.L.!: Results of a mother-adolescent HIV prevention program. Nursing Research, 55, 43–51. doi: 10.1097/00006199-200601000-00006 [DOI] [PubMed] [Google Scholar]
- Elkington KS, Belmonte K, Latack JA, Mellins CA, & Wasserman GA (2015). An exploration of family and juvenile justice systems to reduce youth HIV/STI risk. Journal of Research on Adolescence, 25, 700–716. doi: 10.1111/jora.12163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, & Bishop DS (1983). The McMaster Family Assessment Device. Journal of Marital and Family Therapy, 9, 171–180. doi: 10.1111/j.1752-0606.1983.tb01497.x [DOI] [Google Scholar]
- Finan LJ, Schulz J, Gordon MS, & McCauley Ohannessian C (2015). Parental problem drinking and adolescent externalizing behaviors: The mediating role of family functioning. Journal of Adolescence, 43, 100–110. doi: 10.1016/j.adolescence.2015.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gault-Sherman M (2012). It’s a two-way street: The bidirectional relationship between parenting and delinquency. Journal of Youth and Adolescence, 41, 121–145. doi: 10.1007/s10964-011-9656-4 [DOI] [PubMed] [Google Scholar]
- Goodyear M, Hill T-L, Allchin B, McCormick F, Hine R, Cuff R, & O’Hanlon B (2015). Standards of practice for the adult mental health workforce: Meeting the needs of families where a parent has a mental illness. International Journal of Mental Health Nursing, 24, 169–180. doi: 10.1111/inm.12120 [DOI] [PubMed] [Google Scholar]
- Gordon Simons L, Sutton TE, Simons RL, Gibbons FX, & McBride Murry V (2016). Mechanisms that link parenting practices to adolescents’ risky sexual behavior: A test of six competing theories. Journal of Youth and Adolescence, 45, 255–270. doi: 10.1007/s10964-015-0409-7 [DOI] [PubMed] [Google Scholar]
- Grekin ER, Brennan PA, & Hammen C (2005). Parental alcohol use disorders and child delinquency: The mediating effects of executive functioning and chronic family stress. Journal of Studies on Alcohol, 66, 14–22. [DOI] [PubMed] [Google Scholar]
- Hadley W, Brown LK, Lescano CM, Harrison K, Spalding K, DiClemente R,…Project STYLE Study Group (2009). Parent-adolescent sexual communication: Associations of condom use with condom discussions. AIDS Behaviors, 13, 997–1004. doi: 10.1007/s10461-008-9468-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt J, Gerbershagen HU, & Franke P (2000). The Symptom Check-list, SCL-90-R: Its use and characteristics in chronic pain patients. European Journal of Pain, 4, 137–148, 10.1053/eujp.2000.0162. [DOI] [PubMed] [Google Scholar]
- Hayes A (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: The Guildford Press. [Google Scholar]
- Horwitz SM, Briggs-Gowan MJ, Storfer-Isser A, & Carter AS (2007). Prevalence, correlates, and persistence of maternal depression. Journal of Women’s Health, 16, 678–691. doi: 10.1089/jwh.2006.0185 [DOI] [PubMed] [Google Scholar]
- IBM, Corporation. (2016). IBM Statistics for Windows, Version 24.0. Armonk, NY: IBM Corporation. [Google Scholar]
- Kim HH, Viner-Brown SI, & Garcia J (2007). Children’s mental health and family functioning in Rhode Island. Pediatrics, 119, S22–S28. doi: 10.1542/peds.2006-2089E [DOI] [PubMed] [Google Scholar]
- Krug S, Wittchen H-U, Lieb R, Beesdo-Baum K, & Knappe S (2016). Family functioning mediates the association between parental depression and low self-esteem in adolescents. Journal of Affective Disorders, 203, 184–18. doi: 10.1016/j.jad.2016.06.008 [DOI] [PubMed] [Google Scholar]
- Lam PK, Naar-King S, Wright K (2007). Social support and disclosure as predictors of mental health in HIV-positive youth. AIDS Patient Care, 21, 20–29. doi: 10.1089/apc.2006.005 [DOI] [PubMed] [Google Scholar]
- Leaf JB, Leaf R, McEachin J, Taubman M, Ala’i-Rosales S, Ross RK,…Weiss MJ (2016). Applied Behavior Analysis is a science and, therefore, progressive. Journal of Autism and Developmental Disorders, 46, 720–731, doi: 10.1007/s10803-015-2591-6 [DOI] [PubMed] [Google Scholar]
- Lederman CS, Dakof GA, Larrea M, & Li H (2004). Characteristics of adolescent females in juvenile detention. International Journal of Law and Psychiatry, 27, 321–337. doi: 10.1016/j.ijlp.2004.03.009 [DOI] [PubMed] [Google Scholar]
- Letourneau EJ, McCart MR, Sheidow AJ, & Mauro PM (2017). First evaluation of a contingency management intervention addressing adolescent substance use and sexual risk behaviors: Risk reduction therapy for adolescents. Journal of Substance Abuse Treatment, 72, 56–65. doi: 10.1016/j.jsat.2016.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle H, Rowe C, Dakof G, Henderson C, & Greenbaum P (2009). Multidimensional family therapy for young adolescent substance abuse: Twelve-month outcomes of a randomized controlled trial. Journal of Consulting and Clinical Psychology, 77, 12–25. doi: 10.1037/a0014160 [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. doi: 10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers RJ, Roozen HG, & Smith JE (2011). The Community Reinforcement Approach. Alcohol Research & Health, 33, 380–388. [PMC free article] [PubMed] [Google Scholar]
- Moser C (2011). The sexual health of adolescents involved in corrections In Gowen LK& Aue N(Eds.), Sexual health disparities among disenfranchised youth. Portland, OR: Public Health Division, Oregon Health Authority and Research and Training Center for Pathways to Positive Futures, Portland State University. [Google Scholar]
- MST Services, Inc. (2007). MST Treatment Model. Retrieved from: http://mstservices.com/mst_treatment_model.
- MST Services, Inc. (2015). Multisystemic Therapy. Retrieved from: http://mstservices.com/what-is-mst/what-is-mst.
- National Institute of Justice (2011, June 17). All programs and practices. Retrieved from: https://www.crimesolutions.gov/Programs.aspx#programs
- Nijjar R, Ellenbogen MA, Hodgins S (2016). Sexual risk behaviors in the adolescent offspring of parents with Bipolar Disorder: Prospective associations with parents’ personality and externalizing behavior in childhood. Journal of Abnormal Child Psychology, 44, 1347–1359. doi: 10.1007/s10802-015-0112-x [DOI] [PubMed] [Google Scholar]
- Perkins-Dock RE (2001). Family interventions with incarcerated youth: A review of the literature. International Journal of Offender Therapy and Comparative Criminology, 45, 606–625. doi: 10.1177/0306624X01455006 [DOI] [Google Scholar]
- Perrino T, Gonzalez-Soldevilla A, Pantin H, & Szapocznik J (2000). The role of families in adolescent HIV prevention: A review. Clinical Child and Family Psychology Review, 3, 81–96. doi: 10.1023/A:1009571518900 [DOI] [PubMed] [Google Scholar]
- Prado G, Pantin H, Briones E, Schwartz SJ, Feaster D, Huang S,…Szapocznik J, (2007). A randomized controlled trial of a parent-centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. Journal of Consulting and Clinical Psychology, 75, 914–926. doi: 10.1037/0022-006X.75.6.914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Kelley K (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16, 93–115. doi: 10.1037/a0022658.supp [DOI] [PubMed] [Google Scholar]
- Price MN, & Shibley Hyde J (2009). When two isn’t better than one: Predictors of early sexual activity in adolescence using a cumulative risk model. Journal of Youth and Adolescence, 38, 1059–1071. doi: 10.1007/s10964-008-9351-2 [DOI] [PubMed] [Google Scholar]
- Rhee K (2008). Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. The Annals of the American Academy of Political and Social Science, 615, 11–37. [Google Scholar]
- Rojas A (2016). Cognitive-behavioral interventions for Obsessive-Compulsive Disorder and Tourette’s Disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 55(10), S60. doi: 10.1016/j.jaac.2016.07.671 [DOI] [Google Scholar]
- Rosenthal R, & Rosnow RL (2008). Randomly and nonrandomly selected sampling units In Authors (Eds.) Essentials of behavioral research: Methods and data analysis (3rd ed., pp. 260–289). New York, NY: McGraw Hill. [Google Scholar]
- Sheidow AJ, Henry DB, Tolan PH, & Strachan MK (2014). The role of stress exposure and family functioning in internalizing outcomes of urban families. Journal of Child and Family Studies, 23, 1351–1365. doi: 10.1007/s10826-013-9793-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sickmund M, Sladky A, & Kang W (2017). Easy access to juvenile court statistics: 1984–2014. Retrieved from http://www.ojjdp.gov/ojstatbb/ezajcs/
- Stanton B, Cole M, Galbraith J, Li X, Penleton S, Cottrel L,…Kaljee L (2004). Randomized trial of a parent intervention: Parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Archives of Pediatrics and Adolescent Medicine, 158, 947–955. doi: 10.1001/archpedi.158.10.947 [DOI] [PubMed] [Google Scholar]
- Stattin H & Kerr M (2000). Parental monitoring: A reinterpretation. Child Development, 71, 1072–1085. doi: 10.1111/1467-8624.00210 [DOI] [PubMed] [Google Scholar]
- Tandon M, Tillman R, Spitznagel E, & Luby J (2014). Parental warmth and risks of substance use in children with Attention-Deficit/Hyperactivity Disorder: Findings from a 10–12 year longitudinal investigation. Addiction Research and Theory, 22, 239–250. doi: 10.3109/16066359.2013.830713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teitelman AM, Ratcliffe SJ, & Cederbaum JA (2008). Parent-adolescent communication about sexual pressure, maternal norms about relationship power, and STI/HIV protective behaviors of minority urban girls. Journal of the American Psychiatric Nurses Association, 14, 50–60. doi: 10.1177/1078390307311770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, & Washburn JJ (2005). Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatric Services, 56, 823–828. doi: 10.1176/appi.ps.56.7.823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin L, Mericle A, McClelland G, & Abram K (2003). HIV and AIDS risk behaviors in juvenile detainees: Implications for public health policy. American Journal of Public Health, 93, 906–912. doi: 10.2105/AJPH.93.6.906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolou-Shams M, Dauria E, Conrad SM, Kemp K, Johnson S, & Brown LK (2017). Outcomes of a family-based HIV prevention for substance using juvenile offenders. Journal of Substance Abuse Treatment, 77, 115–125. doi: 10.1016/j.jsat.2017.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Loon LMA, Van de Ven MOM, Van Doesum KTM, Witteman CLM, & Hosman CMH (2014). The role between parental mental illness and adolescent mental health: The role of family factors. Journal of Child and Family Studies, 23, 1201–1214. doi: 10.1007/s10826-013-9781-7 [DOI] [Google Scholar]
- Williams J, & MacKinnon D (2008). Resampling and distribution of the product methods for testing indirect effects in complex models. Structural Equation Modeling, 15, 23–51. doi: 10.1080/10705510701758166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra GJ, Wilkens SL, & Lieberman AF (2007). The influence of domestic violence on preschooler behavior and functioning. Journal of Family Violence, 22, 33–42. doi: 10.1007/s10896-006-9054-y [DOI] [Google Scholar]


