Supplemental digital content is available in the text.
Key Words: human factors, second victim, mental health, adverse event, risk management
Objectives
Despite growing interest in the second-victim phenomenon and greater awareness of its consequences, there has not been a meta-analysis quantifying the negative impact of adverse events on providers involved in adverse events. This study systematically reviewed the types and prevalence of psychological and psychosomatic symptoms among second victims.
Methods
We conducted a systematic review of nine electronic databases up to February 2017, without restrictions to publication date or language, examining also additional sources (e.g., gray literature, volumes of journals). Two reviewers performed the search, selection process, quality assessment, data extraction, and synthesis. We resolved disagreements by consensus and/or involving a third reviewer. Quantitative studies on the prevalence of psychological and psychosomatic symptoms of second victims were eligible for inclusion. We used random effects modeling to calculate the overall prevalence rates and the I2 statistic.
Results
Of 7210 records retrieved, 98 potentially relevant studies were identified. Full-text evaluation led to a final selection of 18 studies, based on the reports of 11,649 healthcare providers involved in adverse events. The most prevalent symptoms were troubling memories (81%, 95% confidence interval [CI] = 46–95), anxiety/concern (76%, 95% CI = 33–95), anger toward themselves (75%, 95% CI = 59–86), regret/remorse (72%, 95% CI = 62–81), distress (70%, 95% CI = 60–79), fear of future errors (56%, 95% CI = 34–75), embarrassment (52%, 95% CI = 31–72), guilt (51%, 95% CI = 41–62), and sleeping difficulties (35%, 95% CI = 22–51).
Conclusions
Second victims report a high prevalence and wide range of psychological symptoms. More than two-thirds of providers reported troubling memories, anxiety, anger, remorse, and distress. Preventive and therapeutic programs should aim to decrease second victims’ emotional distress.
Recent decades have been characterized by improvements and innovations in medicine, as well as the progressively increasing use of health information technology as well as specialization and subspecialization of healthcare providers.1–3 Because in part of the rise of technology and fragmentation of care, the human aspects of clinical practice are undervalued for both patients and providers. Although patients’ emotions and individual needs as human beings have long been underappreciated,4,5 healthcare providers now face unprecedented time pressures and performance accountability in highly complex environments.6,7
There is a high expectation of perfection in medicine, and medical errors are often viewed as a personal failure of the healthcare providers involved.7,8 However, research has shown that unsafe acts are rarely isolated from their system context.9 Usually, it is a cluster of active failures and latent systemic conditions that causes a patient safety incident (i.e., adverse events harming or potentially harming a patient),10 as illustrated in Reason’s Swiss Cheese Model.9
Although patient safety incidents are common (i.e., between 4% and 17% of hospitals admissions are linked to adverse events),11 they are still stigmatized, with a strong negative impact for physicians.12,13 Historically, it has been overlooked that adverse events affect not only the patient as first victim but also are also highly stressful for the involved providers, thus commonly considered as second victims.8 Although there has been recent controversy over use of the term second victim, an alternative, more appropriate term has not been established.14,15 Second victims often feel responsible for the adverse event and may doubt their professional skills and knowledge,16 experience psychological and psychosomatic symptoms and may consider career changes,17 take sick leave,18 transition to a different department,19 or even leave their profession after.20 Quillivan et al.21 pointed out that the second-victim experience may incite a vicious cycle, leading to further medical errors and affecting patient safety.
There has been growing interest in the second-victim phenomenon,19 with more research on the topic, greater awareness of its negative impact on healthcare,15,22 and successful implementation of psychosocial support programs especially in the United States (e.g., RISE – Resilience in Stressful Events, Johns Hopkins Hospital, Maryland23; forYou, University of Missouri Health Care, Columbia, Missouri24; Medically Induced Trauma Support Services, Chestnut Hill, Massachusetts25). To gain further knowledge about second victims and to reduce the punitive culture still existing in many countries,26 several systematic reviews have been conducted.27–29 However, there has not been a meta-analysis quantifying the psychological impact of adverse events on second victims. To fill this gap, we aimed to provide a comprehensive synthesis and critical analysis of second victims’ emotional distress.
METHODS
The protocol of the study is registered in the International Prospective Register of Systematic Reviews (PROSPERO), Registration Number CRD42016053239.
Search and Selection Process
A systematic search of nine electronic databases (i.e., PubMed, Cochrane Library, Web of Science, Scopus, PsycINFO, EMBASE, ScienceDirect, MEDLINE, CINAHL) was conducted up to February 2017, without restrictions to publication date and language, using the following search strategy: (medical error OR patient safety incident OR adverse event OR near miss OR human error) AND (health personnel OR second victim OR health professional OR health care provider) AND (psychological impact OR experienc* OR psychological response OR psychological symptom OR feeling OR emotion* OR mental health OR cognit* OR psychosomatic symptom OR coping OR resilience OR peer support OR team building). A detailed record of the applied search strategy for each database is provided in Supplemental Data File 1, http://links.lww.com/JPS/A227.
To identify additional studies, we screened databases of gray literature (e.g., PsycEXTRA), volumes of journals, reference lists of books, book chapters, systematic reviews, and white papers (see Supplemental Data File 2, http://links.lww.com/JPS/A227 for a comprehensive overview of the additional searches). Furthermore, to detect newly published, potentially eligible articles, automatic, weekly e-mailed search alerts were set up for the databases Web of Science and PubMed for February 12, 2017, to April 15, 2018.
Studies were eligible for inclusion if (a) the participants were healthcare providers involved in adverse events/patient safety incidents (i.e., harmful incidents, near misses, and no-harm incidents), as defined by the Canadian Patient Safety Institute,10 and (b) the prevalence of psychological and psychosomatic symptoms in this population was reported. There were no restrictions on age, sex, healthcare profession, and setting (i.e., inpatient or outpatient care).
Editorials, general discussion papers, comments, letters, book chapters, systematic reviews, single case studies, case series, and qualitative studies were excluded because we did not expect original, quantitative findings (i.e., prevalence rates of psychological or psychosomatic symptoms of healthcare providers involved in adverse events) to be reported in these types of articles.
Two independent reviewers (I.M.B. and F.M.) screened titles and abstracts of the records using Rayyan, a Systematic Reviews Web application.30 The full texts of records considered as eligible by at least one of the two reviewers were then independently evaluated. In cases of dissent about the inclusion of the full texts, the appropriateness of the inclusion/exclusion was debated and a third reviewer (M.R.) was involved. As suggested in the Cochrane Handbook,31 all the excluded studies and the reasons for exclusion were recorded.
The entire search and selection process have been recorded according to the Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement by Moher et al.32
Quality Assessment
The quality of the included studies was assessed by two appraisers (I.M.B. and F.M.), independently and then by consensus, using the Joanna Briggs Institute Critical Appraisal Checklist for Studies Reporting Prevalence Data,33 a standardized tool based on nine quality criteria (i.e., appropriate sample frame to address target population, appropriate method of recruitment, adequate sample size, detailed description of study subjects and setting, data analysis with sufficient coverage of the identified sample, use of valid methods to identify the condition, measurement of condition in a standard and reliable way, appropriate statistical analysis, adequate response rate/appropriate management of low response rate) that can be scored as yes (i.e., met criterion), no (i.e., unmet criterion), unclear, and not applicable. Disagreements were discussed and resolved, involving a third appraiser (M.R.) to adjudicate.
Outcome Measure
The primary outcome measure was the prevalence of psychological (i.e., at the emotional and cognitive level, such as guilt and difficulty concentrating) and psychosomatic symptoms (e.g., sleep disturbance) among healthcare providers involved in an adverse event.
Data Extraction and Synthesis
Two investigators (I.M.B. and F.M.) independently collected study characteristics (e.g., publication year, country, study design, setting, sample size of the participants involved in an adverse event, type of adverse event, patient’s outcome) and outcome measures, using a data collection form.
Cases of dissent were discussed and, if necessary, a third investigator (M.R.) was involved to reach consensus. If missing data were identified, the authors of the primary study were contacted.
Aiming to synthesize the extracted findings, we applied the following rules:
If symptoms were expressed only as percentages, without any absolute frequency (required for the applied software Comprehensive Meta-Analysis V [Biostat Inc, Englewood, NJ]), we calculated frequency by converting the percentage to a decimal and then by multiplying the decimal by the sample size. If then the calculated absolute frequency included decimals, we rounded it according to standard rules.
To calculate the overall prevalence of psychological and psychosomatic symptoms, we grouped the variables of interest, retrieved from the primary studies, that corresponded in terms of content and wording. If variables of interest were similar thematically but differed from each other in terms of wording (e.g., fear of repeating the mistake,34 anxiety about the potential for future errors,35 anxious about potential for future errors),36 we considered them as a single group (see Supplemental Data File 3, http://links.lww.com/JPS/A227 for a comprehensive list of all groups of variables of interest included in the meta-analyses).
If more than one variable of interest, extracted from the same paper and thus based on the same sample, would have potentially fit into the same group, we selected—aiming to prevent overlap—the variable that was most appropriate in terms of content and wording (e.g., the variable of interest anxiety37 was considered more appropriate than panic/worries37 for the group “anxiety”).
Meta-analyses
Because we expected considerable heterogeneity across studies due to several factors, such as a variety of applied instruments, participants’ professions, and medical settings, we used random effects modeling for all analyses. We (M.P. and C.B.) calculated the overall prevalence (i.e., average effect size) of psychological and psychosomatic symptoms with 95% confidence interval (CI) by pooling the individual prevalence rates (i.e., individual effect sizes) of at least two primary studies. Regarding the investigation of statistical heterogeneity, we visually assessed forest plots, calculated and interpreted the I2 statistic as recommended in the Cochrane Handbook38: I2 estimates might not be important from 0% to 40%, may represent moderate heterogeneity from 30% to 60%, substantial heterogeneity from 50% to 90%, and considerable heterogeneity from 75% to 100%. The meta-analyses were performed using Comprehensive Meta-Analysis V3 (Biostat Inc, Englewood, NJ).
RESULTS
Selection and Inclusion of Studies
The search of the electronic databases (see Supplemental Data File 1, http://links.lww.com/JPS/A227) and additional sources (i.e., databases of gray literature, volumes of journals, reference lists of books, book chapters, systematic reviews, and white papers) (see Supplemental Data File 2, http://links.lww.com/JPS/A227) initially produced 7210 records (7195 and 15 records, respectively). After screening title and/or abstract, 98 full-text articles were assessed for eligibility. We contacted the authors of the primary study in six cases to request additional information. Eighty studies were then excluded for various reasons such as mismatch with the inclusion criteria, mixed population, wrong focus of the study, or insufficient information (see Supplemental Data File 4, http://links.lww.com/JPS/A227 for a comprehensive overview of the excluded studies). Finally, 18 studies, all meeting the inclusion criteria, were included (Fig. 1).
FIGURE 1.
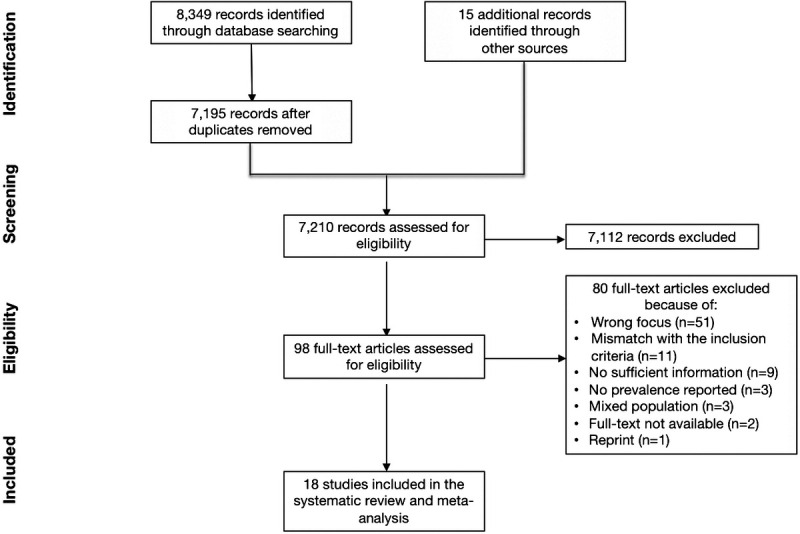
The PRISMA flow diagram.
Quality Assessment
All primary studies met more than half of the quality criteria (i.e., between 5 and 8) of the Joanna Briggs Institute Critical Appraisal Checklist for Prevalence Studies.33 All studies used an appropriate sample frame to address the target population, analyzed the data with sufficient coverage of the identified sample, and measured the conditions in a standard, reliable way. However, the adequacy of the sample size and the use of valid methods remained unclear for several studies; others did not recruit the participants appropriately or did not describe the characteristics of the participants and the setting in sufficient detail. In some articles, the statistical analyses were not entirely appropriate (e.g., prevalence rates expressed only by percentages). A detailed overview of appraisers’ judgments of each included primary study is given in Supplemental Data File 5, http://links.lww.com/JPS/A227.
Characteristics of the Included Studies
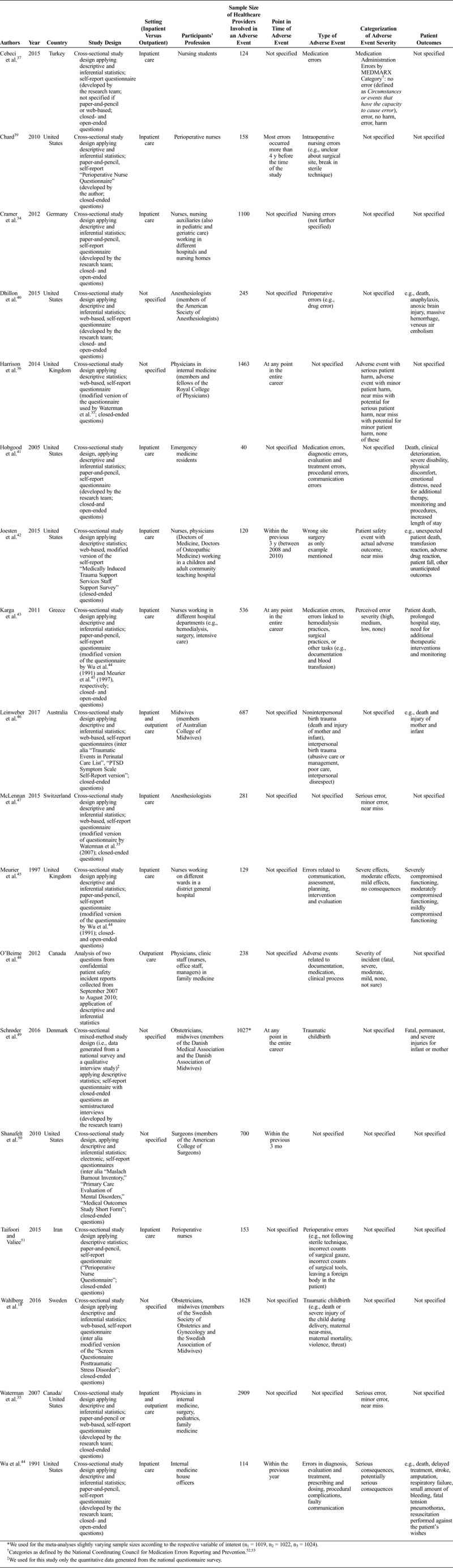
The 18 included primary studies (Table 1),18,34–37,39–51 all written in English except for one in German,34 were published between 1991 and 2016. Six were conducted in the United States, two in the United Kingdom, and one study each in Australia, Canada, Greece, Iran, Denmark, Sweden, Germany, Switzerland, and Turkey. One study35 was conducted both in Canada and in the United States. Aside from O’Beirne et al.48 who collected patient safety incident records for 3 years, all other studies applied a cross-sectional survey design. Although some authors calculated only descriptive statistics, others additionally applied inferential statistics (e.g., correlational or regression analyses). All authors used paper-and-pencil or web-based/electronic self-report questionnaires with predominantly closed-ended questions. Schrøder et al.49 additionally conducted semistructured interviews; however, we included only the quantitative data reported by Schrøder et al.49 in our study. Many authors created also own questionnaires or adapted already existing ones, such as the one developed and validated by Wu et al.44 or Waterman et al.35 Well-established clinical questionnaires, such as the PTSD Symptom Scale Self-Report version54 and the Primary Care Evaluation of Mental Disorders,55 were also used. The selected studies investigated participants with various occupational roles (e.g., nurses, midwives, physicians), working both in inpatient and outpatient care in different medical settings (e.g., surgery, obstetrics, internal medicine). The sample size of the respondents/healthcare providers involved in an adverse event ranged from 4041 to 2909,35 reaching a total of 11,649 participants. Seven studies provided information about the time of occurrence of the adverse event: some reported a long time frame (e.g., at any point in the entire career36), whereas others mentioned a narrow one (e.g., within the previous 3 months50). The adverse events, though heterogeneous, were mostly related to errors in diagnosis, evaluation, treatment, and communication. Categories describing the severity of the adverse events (e.g., serious error – minor error – near miss) were used in nine articles. In addition, eight studies gave examples of patient outcomes, ranging from physical discomfort through prolonged hospital stay to severe disability and death.
TABLE 1.
Characteristics of the Included Studies
Prevalence of Psychological and Psychosomatic Symptoms
Meta-analyses
We calculated the overall prevalence rates for 21 symptoms experienced by second victims in the aftermath of adverse events (Table 2). The most prevalent symptoms were troubling memories (81%, 95% CI = 46–95) (Fig. 2), anxiety/concern (76%, 95% CI = 33–95), anger toward themselves (75%, 95% CI = 59–86), regret/remorse (72%, 95% CI = 62–81), distress (70%, 95% CI = 60–79), fear of future errors (56%, 95% CI = 34–75), embarrassment (52%, 95% CI = 31–72), guilt (51%, 95% CI = 41–62), and sleeping difficulties (35%, 95% CI = 22–51), which was the only psychosomatic symptom we were able to pool (Fig. 3). All forest plots can be found in the Supplemental Data File 6, http://links.lww.com/JPS/A227. I2 estimates ranged between 0% and 53.1% indicating negligible to moderate heterogeneity across studies. We did not conduct subgroup analysis given the small amount of data available for this purpose.
TABLE 2.
Overall Prevalence Rates of Second Victims’ Psychological and Psychosomatic Symptoms
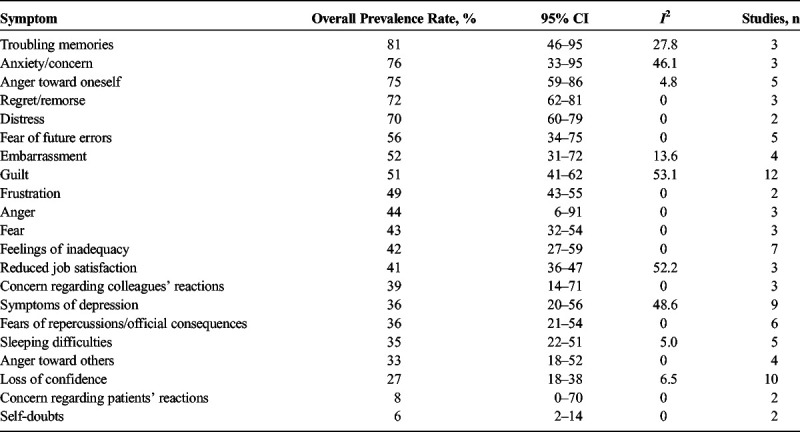
FIGURE 2.
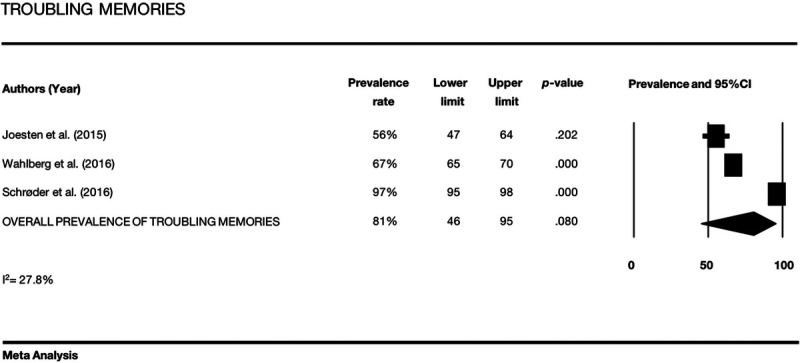
Forest plot showing the overall prevalence of troubling memories, the prevalence rates for the primary studies, the respective 95% CI, the P values, and the I2 statistic.
FIGURE 3.
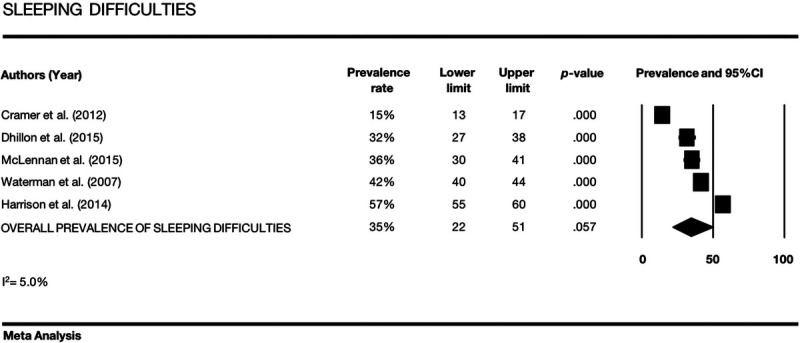
Forest plot showing the overall prevalence of sleeping difficulties, the prevalence rates for the primary studies, the respective 95% CI, the P values, and the I2 statistic.
Unpooled Prevalence rates
Because of a lack of sufficient data from different studies and/or too heterogeneous variables of interest, and to prevent overlaps, we did not pool all prevalence rates reported in the primary studies (see Supplemental Data File 7, http://links.lww.com/JPS/A227 for an overview of the ungrouped variables and their prevalence rates).
Two studies18,46 explicitly assessed the occurrence of posttraumatic stress disorder (PTSD), each using a different questionnaire. These showed 5% (95% CI = 4–7; 81/1628)18 and 17% (95% CI = 14–20; 102/601)46 prevalence rates of probable PTSD, respectively. Dhillon et al.40 evaluated the impact of adverse events on cognitive functioning, reporting difficulty concentrating (79% of the participants; 26/33) and that 9% (22/245) of the enrolled anesthesiologists experienced the psychosomatic symptom of change in appetite.
DISCUSSION
This study expands on previous research on the psychological impact of adverse events on healthcare providers by providing precise estimates of the prevalence of the symptoms affecting second victims. To our knowledge, this is the first systematic review and meta-analysis quantifying psychological and psychosomatic symptoms of these providers. Our results confirm that healthcare providers involved in adverse events are highly affected by a wide range of psychological symptoms. More than two-thirds of providers reported troubling memories, anxiety, anger, remorse, and distress. More than half reported fear of future errors, embarrassment, and guilt. A third reported difficulty sleeping.
Troubling memories had the highest overall prevalence with 81% reporting this symptom. It is well known that unwanted upsetting memories and flashbacks are common after traumatic experiences in general.56,57 Although we did not pool the results of the two primary studies specifically focusing on the prevalence of probable PTSD,18,46 the overall high prevalence of troubling memories, anxiety/concern, distress, symptoms of depression, sleeping difficulties, and loss of confidence suggests symptoms commonly associated with PTSD.58,59
Three quarters of providers studied experienced anxiety, and a similar number reported anger at themselves. The intensity, duration, and clinical relevance of these emotional reactions were not systematically explored in the primary studies, but these symptoms have been demonstrated to reduce professional performance. Anxiety can negatively influence cognitive functioning (e.g., working memory and concentration difficulties, attentional lapses, intrusive thoughts) in turn leading to difficulties in social and work settings.60 Moreover, anxiety and the fear of future errors may result in overcontrolling behaviors (e.g., excessive double-checking), which may undermine healthcare providers’ efficiency and actually increase error proneness.34 It is also well known that anger directed toward oneself or toward others is a feature of dysfunctional coping strategies61 and linked to the risk of burnout.62 Anger represents an emotion that, if not properly addressed, tends to reinforce defensive attitudes63 and to negatively affect interpersonal relationships64 as well as the quality of communication in the workplace.65 These may impede risk management66 and lead to medical errors.41,44,45
Consistent with Wu8 and Scott et al.,7 our results showed that healthcare providers often experience medical errors as a personal failure. Emotional reactions such as embarrassment, fear of future errors, frustration, and the feeling of inadequacy are often associated with adverse events. The occurrence of these symptoms might be the consequence of the common expectation for perfection, shaped by external punitive attitudes in the health care system or by internalized norms.8,21 It also demonstrates that effort is needed to reduce the distress caused by this culture of perfection8,67 and to promote instead the concept of “Just Culture.” Just Culture focuses on system failures to improve patient safety and recognizes at the same time individual behaviors as contributors to risk for which the involved healthcare provider should accept responsibility.68 Although there is growing agreement that it is important to shift healthcare away from the traditional approach of blame and judgment,26,69 these attitudes are persistent as it is shown by the high prevalence of concern regarding colleagues’ reactions. Interestingly, our results also suggested that this self-critical attitude did not take into account the role of the patient. Indeed, despite frequently described feelings of guilt, regret, and remorse by second victims, we found a relatively low overall prevalence (8%) of second victims’ concerns about patients’ reactions (i.e., anxiety about loss of patient’s trust37 and fear of having to speak to the patient and/or family42). This result seems to suggest that healthcare providers are much less concerned about patients as self-determining partners in the process of care70 and that they place a higher priority on the risk posed by the reactions of their colleagues. However, this finding needs to be interpreted with caution because second victims’ self-doubts were explored in only two studies, limiting generalizability. Future studies should further explore this provocative finding.
Implications for Clinical Practice and Policy
Our results highlight the importance of recognizing the significant distress experienced by second victims and addressing those needs in practice, education, and policy. The first priority is to support health care workers. As recently acknowledged by the Joint Commission in the United States, health care managers should provide easily accessed support programs tailored to the specific needs of the second victim, following already successful approaches, such as RISE at the Johns Hopkins Hospital.23,71 RISE provides peer-to-peer support to health care workers who have experienced a stressful patient-related incident or adverse event. The RISE team is composed of trained responders from different disciplines (e.g., physicians, nurses, chaplains, social workers) who deliver psychological first aid to peers in a confidential, nonjudgmental environment.
Broad education can provide a foundation for a more supportive health care environment. It will be important to raise awareness of work stress, the second victim phenomenon, and patient safety, through informational campaigns and educational programs for healthcare workers. Those individuals interested in playing a more active role can be trained to provide peer support and psychological first aid.72 Such programs should acknowledge the role of human factors in work and safety, as also recommended by Hollnagel et al.67 Policy makers should require health care organizations to make these programs available to staff and monitor their implementation and use. These preventive and supportive strategies are expected to reduce second victims’ psychological distress and to help create a Just Culture. Indeed, the humanity and fallibility of health care workers need to be acknowledged and accounted for in the design of the system while simultaneously maintaining the expectation that they deliver high-quality care.
Such a culture may also make it easier for the involved healthcare providers to initiate open, transparent discussions with the patients and their families about the adverse event, a step that has been shown to be highly appreciated.73
Limitations
Our study had some limitations. First, the primary studies included in our review were heterogeneous in terms of instruments used, participants’ profession, medical setting, and characterization of the adverse event (i.e., definition, point in time, type, severity, patient outcomes). In some cases, the articles differed from one another in reported prevalence, as reflected by the wide confidence intervals around overall estimates of prevalence. However, quantitative analyses did not indicate substantial heterogeneity across studies. Second, the study is subject to the limitations related to the included cross-sectional, self-report studies. Biases due to self-selection by respondents74 and recall75 may have affected the results of the primary studies, which were reflected in our meta-analyses. Third, the primary studies did not capture the intensity, duration, and clinical relevance of individual symptoms and if the healthcare providers had a history of mental disorders. These limitations could be overcome by future longitudinal studies of healthcare providers to record the incidence and the impact of adverse events and to clinically evaluate symptoms before and after an adverse event. To gain a better understanding about the predictors of psychological distress after adverse events,18,35,47 personality characteristics and contextual variables (e.g., existence of punitive culture at workplace, severity of adverse event) could be assessed in such longitudinal studies. Fourth, because of insufficient data and heterogeneous variables of interest, some prevalence rates of psychological and psychosomatic symptoms reported in the primary studies were not grouped and thus were excluded from the meta-analyses. Notably, we were only able to meta-analyze the prevalence rates of one psychosomatic symptom, namely, sleeping difficulties, because additional psychosomatic symptoms were examined in only one study.40 A recent qualitative study76 suggests that second victims experience a broad range of psychosomatic symptoms, such as extreme fatigue, increased respiratory rate and blood pressure, tachycardia, and muscle tension. Given the paucity of research on psychosomatic symptoms of second victims, future studies should explore this aspect further. In particular, quantitative methods, such as diagnostic tests or questionnaires, should be applied to thoroughly study the type and prevalence of psychosomatic symptoms experienced by second victims. Using quantitative instead of qualitative methodology would allow for greater objectivity and reliability of the results and would enhance their generalizability. Finally, this study focused only on the psychological impact of adverse events on second victims, without investigating the use of coping strategies in the aftermath of such an event. To overcome this limitation, we are planning to conduct an additional meta-analysis in the future.
CONCLUSIONS
Our meta-analysis, which included information from 11,649 healthcare providers involved in adverse events, provides an accurate overview of the severe psychological burden affecting second victims. These symptoms have serious repercussions for the well-being and fitness of the healthcare workforce. This evidence should be useful to develop and implement and evaluate support programs tailored to the specific needs of second victims. Such programs, in the long run, might have the potential to decrease the incidence of medical errors and increase patient safety, improving the overall quality of medical care.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Prof. Susan D. Scott, Prof. José Mira, and Prof. Reema Harrison for providing useful information for this study.
Footnotes
The authors disclose no conflict of interest.
Supplemental digital contents are available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.journalpatientsafety.com).
REFERENCES
- 1.Shekelle PG, Morton SC, Keeler EB. Costs and Benefits of Health Information Technology. Evidence Report/Technology Assessment No. 132. AHRQ Publication No.06-E006. Agency for Healthcare Research and Quality:Rockville, MD; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ball CG, Sutherland F, Kirkpatrick AW, et al. Dramatic innovations in modern surgical subspecialties. Can J Surg. 2010;53:335–341. [PMC free article] [PubMed] [Google Scholar]
- 3.Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009;7:100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Behruzi R, Hatem M, Goulet L, et al. Perception of humanization of birth in a highly specialized hospital: let’s think differently. Health Care Women Int. 2014;35:127–148. [DOI] [PubMed] [Google Scholar]
- 5.Grisales-Naranjo LV, Arias-Valencia MM. Humanized care; the case of patients subjected to chemotherapy. Invest Educ Enferm. 2013;31:364–376. [Google Scholar]
- 6.Rosenstein AH. Addressing physician stress, burnout, and compassion fatigue: the time has come. Isr J Health Policy Res. 2013;2:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott SD, Hirschinger LE, Cox KR, et al. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18:325–330. [DOI] [PubMed] [Google Scholar]
- 8.Wu AW. Medical error: the second victim. The doctor who makes mistakes needs help too. BMJ. 2000;320:726–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reason J. Human error: models and management. BMJ. 2000;320:768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Canadian Patient Safety Institute Patient Safety Incident. Available at: http://www.patientsafetyinstitute.ca/en/Topic/Pages/Patient-Safety-Incident.aspx. Accessed October 2, 2018.
- 11.Rafter N, Hickey A, Condell S, et al. Adverse events in healthcare: learning from mistakes. QJM. 2015;108:273–277. [DOI] [PubMed] [Google Scholar]
- 12.Edrees HH, Morlock L, Wu AW. Do hospitals support second victims? Collective insights from patient safety leaders in Maryland. Jt Comm J Qual Patient Saf. 2017;43:471–483. [DOI] [PubMed] [Google Scholar]
- 13.Van Gerven E, Deweer D, Scott SD, et al. Personal, situational and organizational aspects that influence the impact of patient safety incidents: a qualitative study. Rev Calid Asist. 2016;31(suppl 2):34–46. [DOI] [PubMed] [Google Scholar]
- 14.Tumelty ME. The second victim: a contested term? J Patient Saf. 2018. doi: 10.1097/PTS.0000000000000558Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Wu AW, Shapiro J, Harrison R, et al. The impact of adverse events on clinicians: what’s in a name? J Patient Saf. 2017. doi: 10.1097/PTS.0000000000000256Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 16.Harrison R, Lawton R, Perlo J, et al. Emotion and coping in the aftermath of medical error: a cross-country exploration. J Patient Saf. 2015;11:28–35. [DOI] [PubMed] [Google Scholar]
- 17.Gazoni FM, Amato PE, Malik ZM, et al. The impact of perioperative catastrophes on anesthesiologists: results of a national survey. Anesth Analg. 2012;114:596–603. [DOI] [PubMed] [Google Scholar]
- 18.Wahlberg A, Andreen Sachs M, Johannesson K, et al. Post-traumatic stress symptoms in Swedish obstetricians and midwives after severe obstetric events: a cross-sectional retrospective survey. BJOG. 2017;124:1264–1271. [DOI] [PubMed] [Google Scholar]
- 19.Rodriquez J, Scott SD. When clinicians drop out and start over after adverse events. Jt Comm J Qual Patient Saf. 2018;44:137–145. [DOI] [PubMed] [Google Scholar]
- 20.Martens J, Van Gerven E, Lannoy K, et al. Serious reportable events within the inpatient mental health care: impact on physicians and nurses. Rev Calid Asist. 2016;31(suppl 2):26–33. [DOI] [PubMed] [Google Scholar]
- 21.Quillivan RR, Burlison JD, Browne EK, et al. Patient safety culture and the second victim phenomenon: connecting culture to staff distress in nurses. Jt Comm J Qual Patient Saf. 2016;42:377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu AW, Steckelberg RC. Medical error, incident investigation and the second victim: doing better but feeling worse? BMJ Qual Saf. 2012;21:267–270. [DOI] [PubMed] [Google Scholar]
- 23.Edrees H, Connors C, Paine L, et al. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6:e011708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36:233–240. [DOI] [PubMed] [Google Scholar]
- 25.Medically Induced Trauma Support Services. Clinician support tool kit for healthcare workers 2010 Available at: http://mitss.org/wp-content/uploads/2017/11/Clinician-Support-Tool-Kit-for-Healthcare_05-07-2012.pdf. Accessed October 2, 2018.
- 26.Reis CT, Paiva SG, Sousa P. The patient safety culture: a systematic review by characteristics of hospital survey on patient safety culture dimensions. International J Qual Health Care. 2018;30:660–677. [DOI] [PubMed] [Google Scholar]
- 27.Chan ST, Khong PCB, Wang W. Psychological responses, coping and supporting needs of healthcare professionals as second victims. Int Nurs Rev. 2017;64:242–262. [DOI] [PubMed] [Google Scholar]
- 28.Seys D, Wu AW, Van Gerven E, et al. Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof. 2013;36:135–162. [DOI] [PubMed] [Google Scholar]
- 29.Sirriyeh R, Lawton R, Gardner P, et al. Coping with medical error: a systematic review of papers to assess the effects of involvement in medical errors on healthcare professionals’ psychological well-being. Qual Saf Health Care. 2010;19:e43. [DOI] [PubMed] [Google Scholar]
- 30.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan – a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JPT, Deeks JJ, eds. Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). : The Cochrane Collaboration, 2011.Available at: www.handbook.cochrane.org. Accessed October 2, 2018. [Google Scholar]
- 32.Moher D, Liberati A, Tezlaff J, et al. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269,W64. [DOI] [PubMed] [Google Scholar]
- 33.The Joanna Briggs Institute The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. Checklist for Prevalence Studies. 2017; Available at: http://joannabriggs.org/assets/docs/critical-appraisal-tools/JBI_Critical_Appraisal-Checklist_for_Prevalence_Studies2017.pdf. Accessed October 2, 2018. [Google Scholar]
- 34.Cramer H, Foraita R, Habermann M. Nursing errors and the consequences. Results of a survey of nurses from inpatient care institutions [in German]. Pflege. 2012;25:245–259. [DOI] [PubMed] [Google Scholar]
- 35.Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33:467–476. [DOI] [PubMed] [Google Scholar]
- 36.Harrison R, Lawton R, Stewart K. Doctors’ experiences of adverse events in secondary care: the professional and personal impact. Clin Med (Lond). 2014;14:585–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cebeci F, Karazeybek E, Sucu G, et al. Nursing students’ medication errors and their opinions on the reasons of errors: a cross-sectional survey. J Pak Med Assoc. 2015;65:457–462. [PubMed] [Google Scholar]
- 38.Deeks JJ, Higgins JPT, Altman DG, eds. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). : The Cochrane Collaboration, 2011.Available at: http://www.handbook.cochrane.org. Accessed October 2, 2018. [Google Scholar]
- 39.Chard R. How perioperative nurses define, attribute causes of, and react to intraoperative nursing errors. AORN J. 2010;91:132–145. [DOI] [PubMed] [Google Scholar]
- 40.Dhillon AK, Russel DL, Stiegler MP. Catastrophic events in the perioperative setting: a survey of U.S. anesthesiologists. Int J Emerg Ment Health. 2015;17:257. [Google Scholar]
- 41.Hobgood C, Hevia A, Tamayo-Sarver JH, et al. The influence of the causes and contexts of medical errors on emergency medicine residents’ responses to their errors: an exploration. Acad Med. 2005;80:758–764. [DOI] [PubMed] [Google Scholar]
- 42.Joesten L, Cipparrone N, Okuno-Jones S, et al. Assessing the perceived level of institutional support for the second victim after a patient safety event. J Patient Saf. 2015;11:73–78. [DOI] [PubMed] [Google Scholar]
- 43.Karga M, Kiekkas P, Aretha D, et al. Changes in nursing practice: associations with responses to and coping with errors. J Clin Nurs. 2011;20:3246–3255. [DOI] [PubMed] [Google Scholar]
- 44.Wu AW, Folkman S, McPhee S, et al. Do house officers learn from their mistakes? JAMA. 1991;265:2089–2094. [PubMed] [Google Scholar]
- 45.Meurier CE, Vincent CA, Parmar DG. Learning from errors in nursing practice. J Adv Nurs. 1997;26:111–119. [DOI] [PubMed] [Google Scholar]
- 46.Leinweber J, Creedy DK, Rowe H, et al. Responses to birth trauma and prevalence of posttraumatic stress among Australian midwives. Women Birth. 2017;30:40–45. [DOI] [PubMed] [Google Scholar]
- 47.McLennan SR, Engel-Glatter S, Meyer AH, et al. The impact of medical errors on Swiss anaesthesiologists: a cross-sectional survey. Acta Anaesthesiol Scand. 2015;59:990–998. [DOI] [PubMed] [Google Scholar]
- 48.O’Beirne M, Sterling P, Palacios-Derflingher L, et al. Emotional impact of patient safety incidents on family physicians and their office staff. J Am Board Fam Med. 2012;25:177–183. [DOI] [PubMed] [Google Scholar]
- 49.Schrøder K, Jørgensen JS, Lamont RF, et al. Blame and guilt – a mixed methods study of obstetricians’ and midwives’ experiences and existential considerations after involvement in traumatic childbirth. Acta Obstet Gynecol Scand. 2016;95:735–745. [DOI] [PubMed] [Google Scholar]
- 50.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. [DOI] [PubMed] [Google Scholar]
- 51.Taifoori L, Valiee S. Understanding or nurses’ reactions to errors and using this understanding to improve patient safety. ORNAC J. 2015;33:32–42. [PubMed] [Google Scholar]
- 52.Santell JP, Hicks RW, McMeekin J, et al. Medication errors: experience of the United States Pharmacopeia (USP) MEDMARX reporting system. J Clin Pharmacol. 2003;43:760–767. [PubMed] [Google Scholar]
- 53.Hicks RW, Cousins DD, Williams RL. Selected medication-error data from USP’s MEDMARX program for 2002. Am J Health Syst Pharm. 2004;61:993–1000. [DOI] [PubMed] [Google Scholar]
- 54.Foa E, Riggs D, Dancu C, et al. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- 55.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 56.Brewin CR. Re-experiencing traumatic events in PTSD: new avenues in research on intrusive memories and flashbacks. Eur J Psychotramatol. 2015;6:27180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ehlers A. Understanding and treating unwanted trauma memories in posttraumatic stress disorder. Z Psychol. 2010;218:141–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.World Health Organization The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Disgnostic Guidelines. Geneva, Switzerland: World Health Organisation; 1992. [Google Scholar]
- 59.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 60.Robinson OJ, Vytal K, Cornwell BR, et al. The impact of anxiety upon cognition: perspectives from human threat of shock studies. Front Hum Neurosci. 2013;7:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Laux L, Weber H. Presentation of self in coping with anger and anxiety: an intentional approach. Anxiety Res. 1991;3:4:233–255. [Google Scholar]
- 62.Muscatello MR, Bruno A, Carroccio C, et al. Association between burnout and anger in oncology versus ophthalmology health care professionals. Psychol Rep. 2006;99:641–650. [DOI] [PubMed] [Google Scholar]
- 63.Cramer P. Anger and the use of defensive mechanism in college students. J Pers. 1991;59:39–55. [DOI] [PubMed] [Google Scholar]
- 64.Han A, Won J, Kim O, et al. Anger expression types and interpersonal problems in nurses. Asian Nurs Res. 2015;9:146–151. [DOI] [PubMed] [Google Scholar]
- 65.Booth J, Ireland JL, Mann S, et al. Anger expression and suppression at work: causes, characteristics and predictors. Inter J Conflict Manag. 2017;28:3. [Google Scholar]
- 66.Gurses AP, Kim G, Martinez EA, et al. Identifying and categorising patient safety hazards in cardiovascular operating rooms using an interdisciplinary approach: a multisite study. BMJ Qual Saf. 2012;21:810–818. [DOI] [PubMed] [Google Scholar]
- 67.Hollnagel E, Wears RL, Braithwaite J. From Safety-I to Safety-II: A White Paper. The Resilient Health Care Net:Published simultaneously by the University of Southern Denmark, University of Florida, USA, and Macquarie University, Australia; 2015. [Google Scholar]
- 68.NHS Improvement A Just Culture Guide. National Health Service: London, UK; 2018. [Google Scholar]
- 69.Radhakrishna S. Culture of blame in the National Health Service; consequences and solutions. Br J Anaesth. 2015;115:653–655. [DOI] [PubMed] [Google Scholar]
- 70.European Health Parliament. Patient Empowerment and Centeredness 2015 Available at: http://www.healthparliament.eu/wp-content/uploads/2017/09/EHP-papers_Patients-empowerment.pdf. Accessed October 2, 2018.
- 71.The Joint Commission, Division of Healthcare Improvement Supporting second victims. Quick Saf. 2018;39:1–3. [Google Scholar]
- 72.Gispin F, Wu AW. Psychological first aid: CPR for mental health crises in health care. J Patient Saf Risk Manag. 2018;23:51–53. [Google Scholar]
- 73.National Patient Safety Foundation’s Lucian Leape Institute Shining a Light: Safer Health Care Through Transparency. Boston, MA: National Patient Safety Foundation; 2015. [Google Scholar]
- 74.Bethlehem J. Selection bias in web surveys. Int Stat Rev. 2010;78:161–188. [Google Scholar]
- 75.Last JM. A Dictionary of Epidemiology. Oxford, UK:Oxford University Press. [Google Scholar]
- 76.Rinaldi C, Leigheb F, Vanhaecht K, et al. Becoming a “second victim” in health care: pathway of recovery after adverse event. Rev Calid Asist. 2016;31(suppl 2):11–19. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


