Abstract
Background
Nationwide, unbiased, and unselected data of hospitalised patients with COVID-19 are scarce. Our aim was to provide a detailed account of case characteristics, resource use, and outcomes of hospitalised patients with COVID-19 in Germany, where the health-care system has not been overwhelmed by the pandemic.
Methods
In this observational study, adult patients with a confirmed COVID-19 diagnosis, who were admitted to hospital in Germany between Feb 26 and April 19, 2020, and for whom a complete hospital course was available (ie, the patient was discharged or died in hospital) were included in the study cohort. Claims data from the German Local Health Care Funds were analysed. The data set included detailed information on patient characteristics, duration of hospital stay, type and duration of ventilation, and survival status. Patients with adjacent completed hospital stays were grouped into one case. Patients were grouped according to whether or not they had received any form of mechanical ventilation. To account for comorbidities, we used the Charlson comorbidity index.
Findings
Of 10 021 hospitalised patients being treated in 920 different hospitals, 1727 (17%) received mechanical ventilation (of whom 422 [24%] were aged 18–59 years, 382 [22%] were aged 60–69 years, 535 [31%] were aged 70–79 years, and 388 [23%] were aged ≥80 years). The median age was 72 years (IQR 57–82). Men and women were equally represented in the non-ventilated group, whereas twice as many men than women were in the ventilated group. The likelihood of being ventilated was 12% for women (580 of 4822) and 22% for men (1147 of 5199). The most common comorbidities were hypertension (5575 [56%] of 10 021), diabetes (2791 [28%]), cardiac arrhythmia (2699 [27%]), renal failure (2287 [23%]), heart failure (1963 [20%]), and chronic pulmonary disease (1358 [14%]). Dialysis was required in 599 (6%) of all patients and in 469 (27%) of 1727 ventilated patients. The Charlson comorbidity index was 0 for 3237 (39%) of 8294 patients without ventilation, but only 374 (22%) of 1727 ventilated patients. The mean duration of ventilation was 13·5 days (SD 12·1). In-hospital mortality was 22% overall (2229 of 10 021), with wide variation between patients without ventilation (1323 [16%] of 8294) and with ventilation (906 [53%] of 1727; 65 [45%] of 145 for non-invasive ventilation only, 70 [50%] of 141 for non-invasive ventilation failure, and 696 [53%] of 1318 for invasive mechanical ventilation). In-hospital mortality in ventilated patients requiring dialysis was 73% (342 of 469). In-hospital mortality for patients with ventilation by age ranged from 28% (117 of 422) in patients aged 18–59 years to 72% (280 of 388) in patients aged 80 years or older.
Interpretation
In the German health-care system, in which hospital capacities have not been overwhelmed by the COVID-19 pandemic, mortality has been high for patients receiving mechanical ventilation, particularly for patients aged 80 years or older and those requiring dialysis, and has been considerably lower for patients younger than 60 years.
Funding
None.
Introduction
The COVID-19 pandemic has affected more than 13 million people worldwide. In Germany, the peak incidence of more than seven cases per 100 000 population per day was reached in March 31–April 3, 2020,1 after lockdown measures were introduced on March 21. As of July 15, 2020, 199 700 patients in Germany had tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 The number of COVID-19-related deaths is 10·9 per 100 000 population,1 which is low compared with other health-care systems that have, at least in part, been overburdened.
First reports from China indicated mild symptoms in 80% of all patients with SARS-CoV-2 infection; approximately 20% had to be admitted to hospital, of whom 25% needed to be treated in the intensive care unit (ICU).2, 3, 4, 5 However, the impact on the total population of patients with COVID-19 could vary considerably, as register data suggest. The cumulative proportion of patients who were hospitalised was 26% in Belgium, 30% in the Netherlands, 53% in Spain, and 69% in France,6, 7, 8, 9 whereas Germany reported 17% by July 2, 2020.1
Research in context.
Evidence before this study
The proportion of patients with COVID-19 requiring hospitalisation, internsive care unit (ICU) admission, and mechanical ventilation differs widely between countries affected by the pandemic. The in-hospital mortality of patients with COVID-19 is not well known because most studies report incomplete data, with a large group of patients still hospitalised or in the ICU. We searched PubMed on April 22, 2020, for articles using the search terms “SARS-CoV-2” OR “COVID-19” AND “critical care” OR “intensive care” OR “ICU” AND “mortality”. We included articles for which at least the abstract was available in English. Our search identified 44 studies that included original clinical outcome data from patients admitted to the ICU with COVID-19. We found no studies of large cohorts that reported only discharged patients.
Added value of this study
To our knowledge, this is the first large case series describing characteristics, resource use, and outcomes in patients with COVID-19 in an unselected and unbiased cohort of already discharged patients within a health-care system without major resource limitations. The study cohort included 10 021 patients, 1727 of whom were mechanically ventilated, in 920 hospitals across Germany, representing all treatment levels.
Implications of all the available evidence
In the German health-care system, in which capacities were not overwhelmed by the COVID-19 pandemic, mortality was high for patients receiving mechanical ventilation, reaching almost 75% in patients aged 80 years or older or in those requiring dialysis, but was considerably lower for patients younger than 60 years. From a European perspective, the study shows that the overall in-hospital mortality is similar to that in other countries, such as France. However, the age distribution of patients on mechanical ventilation differs between countries. The use of mechanical ventilation was comparatively high in Germany, particularly among older people.
In-hospital mortality of patients with COVID-19 varies widely between regions, ranging from 20% to more than 50%.10, 11, 12, 13, 14, 15 Because the duration of mechanical ventilation and recovery from COVID-19 often takes several weeks, recent publications include a substantial subset of patients who are still in the ICU, and little is known about outcomes of a nationwide cohort of patients discharged from hospital.16
Furthermore, differences in outcomes could be attributed to availability and access to health-care system resources. The number of ICU beds varies greatly in different health-care systems, with pre-COVID-19 levels within Europe ranging from 5·0 per 100 000 population in Ireland to 33·9 per 100 000 population in Germany, with intermediate capacities in countries such as the Netherlands (6·7), Spain (9·7), England (10·5), France (16·3), and Belgium (16·6).17 In the current pandemic, the availability of ICU beds might affect the long-term outcome for patients with COVID-19. To date, Germany has always had enough free ICU beds, as reported by the national registry.
The aim of this study was to identify detailed baseline characteristics and outcomes of a large, unselected, and unbiased cohort of hospitalised patients with COVID-19 with completed hospital treatments in one of the least resource-limited health-care systems, particularly focusing on patients requiring mechanical ventilation.
Methods
Study design
For this observational study, we used anonymised nationwide administrative claims data from the German Local Health Care Funds (Allgemeine Ortskrankenkassen [AOK]), the largest sickness fund group within Germany's statutory health insurance system. The study was approved by the Ethics Committee of the Witten/Herdecke University (research ethics board number 92/2020; May, 2020).
Participants and data collection
AOK provides statutory health insurance for around 32% of the German population.18 Membership is open to anyone regardless of factors such as professional affiliation, income, age, or comorbidities.19 Of note, almost every inhabitant of Germany has obligatory health-care insurance. According to the German accounting method for the health-care system, all diagnoses, outcomes, and procedures must be reported to the sickness funds, as required by law. Hence, the data set includes detailed information on patient characteristics, such as age, sex, length of hospital stay, diagnoses and procedure codes, and discharge type (survival status). Diagnoses were coded according to the tenth revision of the International Classification of Diseases and procedures were coded according to the International Classification of Procedures in Medicine, the Operationen- und Prozedurenschlüssel (2020 version).
For the analyses, we included only patients with a confirmed SARS-CoV-2 infection by RT-PCR (diagnosis code U07.1) who were at least 18 years old at admission and were admitted to hospital between Feb 26, 2020, and April 19, 2020, inclusive. We included only patients for whom the complete hospital course was available (ie, patients were discharged or died in hospital during the study period). Based on experiences from the first weeks of the pandemic, the total number of patients could increase by up to 2% because of subsequent completion of claims after patient discharge. For billing purposes, COVID-19 cannot be coded as a main diagnosis, which is defined as the main reason for hospitalisation. Hence, we could not distinguish between patients who were hospitalised for COVID-19 or for any other reason. Furthermore, because one insured person might have had several hospital stays during the observation period due to a transfer from one hospital to another, we grouped patients with adjacent completed hospital stays into one case.
Procedures
Patients were grouped according to whether or not they received any form of mechanical ventilation. Mechanical ventilation was defined as ventilation for more than 1 h. Patients who received mechanical ventilation for more than 6 h were grouped into three subgroups: patients with only non-invasive mechanical ventilation; patients with only invasive mechanical ventilation; and patients with non-invasive mechanical ventilation failure. If non-invasive ventilation and invasive ventilation occurred during the same day, patients were assigned to the invasive mechanical ventilation group, because non-invasive ventilation is often used for a short period to bridge patients to intubation. If non-invasive ventilation was coded at least 1 day before invasive ventilation, patients were assigned to the non-invasive mechanical ventilation failure group. We did not include patients with more than 6 h of ventilation for whom a procedure code for invasive or non-invasive ventilation was missing (n=58). Patients who were ventilated for 1–6 h were reported as a single group, regardless of the type of ventilation. Continuous positive airway pressure is not encoded in the German diagnosis-related group system in conjunction with ICU medicine (it is encoded only in sleep medicine), so it was not available for analysis. Moreover, in contrast to non-invasive ventilation or invasive mechanical ventilation, high-flow oxygen therapy is not reimbursed; therefore, the data quality is low, and patients could not be separately analysed. To account for comorbidities, we used the Charlson comorbidity index and Elixhauser comorbidities.20, 21
Statistical analysis
For continuous variables, we report means with SDs and medians with IQRs. For categorical variables, we report absolute numbers and percentages. All variables are reported for patients with and without mechanical ventilation and for the different ventilation groups. Additionally, we show descriptive statistics for patients with and without ventilation by age group (18–59 years, 60–69 years, 70–79 years, and ≥80 years) and sex. All analyses were done using Oracle Database (version 12c) and R (version 3.5.3).
Role of the funding source
There was no funding source for this study. All authors had full access to all the data in the study and had responsibility for the decision to submit for publication.
Results
The study cohort included 10 021 patients with confirmed COVID-19 diagnosis who were admitted as inpatients to 920 German hospitals between Feb 26, 2020, and April 19, 2020, and who had a closed hospital course. 563 (61%) hospitals treated patients with mechanical ventilation. 95·2% of AOK-insured patients with coded COVID-19 infection at admission were included in the analysis; 4·8% could not be reported because they were still in hospital (1·0%) or their claims were not yet completed (3·8%).
Baseline characteristics are presented in Table 1, Table 2 and in the appendix (p 4). 8294 (83%) patients were treated without ventilation and 1727 (17%) were treated with ventilation, of whom 145 received non-invasive ventilation only, 1318 received invasive mechanical ventilation only, and 141 had non-invasive ventilation failure.
Table 1.
Patient characteristics by type of ventilation
| All patients | Patients without ventilation |
Patients with ventilation |
||||||
|---|---|---|---|---|---|---|---|---|
| All types of ventilation | Non-invasive ventilation only | Invasive ventilation only | Non-invasive ventilation failure | Ventilation for 1–6 h | ||||
| Number of patients | 10 021 | 8294 | 1727 | 145 | 1318 | 141 | 65 | |
| Number of hospitals | 920 | 894 | 563 | 107 | 492 | 93 | 59 | |
| Age, years | ||||||||
| Mean (SD) | 68·3 (17·3) | 68·3 (18·0) | 68·4 (13·1) | 72·4 (12·2) | 67·9 (13·1) | 67·6 (12·9) | 74·0 (14·1) | |
| Median (IQR) | 72·0 (57·0–82·0) | 73·0 (56·0–83·0) | 71·0 (60·0–79·0) | 75·0 (64·0–82·0) | 70·0 (59·0–78·0) | 70·0 (59·0–78·0) | 77·0 (67·0–84·0) | |
| Age group, years | ||||||||
| 18–59 | 2896 (28·9%) | 2474 (29·8%) | 422 (24·4%) | 22 (15·2%) | 337 (25·6%) | 37 (26·2%) | 9 (13·8%) | |
| 60–69 | 1621 (16·2%) | 1239 (14·9%) | 382 (22·1%) | 23 (15·9%) | 305 (23·1%) | 32 (22·7%) | 9 (13·8%) | |
| 70–79 | 2158 (21·5%) | 1623 (19·6%) | 535 (31·0%) | 45 (31·0%) | 413 (31·3%) | 45 (31·9%) | 20 (30·8%) | |
| ≥80 | 3346 (33·4%) | 2958 (35·7%) | 388 (22·5%) | 55 (37·9%) | 263 (20·0%) | 27 (19·1%) | 27 (41·5%) | |
| Sex | ||||||||
| Female | 4822 (48·1%) | 4242 (51·1%) | 580 (33·6%) | 56 (38·6%) | 442 (33·5%) | 42 (29·8%) | 25 (38·5%) | |
| Male | 5199 (51·9%) | 4052 (48·9%) | 1147 (66·4%) | 89 (61·4%) | 876 (66·5%) | 99 (70·2%) | 40 (61·5%) | |
| Elixhauser comorbidities | ||||||||
| Hypertension | 5575 (55·6%) | 4498 (54·2%) | 1077 (62·4%) | 97 (66·9%) | 816 (61·9%) | 91 (64·5%) | 37 (56·9%) | |
| Diabetes | 2791 (27·9%) | 2120 (25·6%) | 671 (38·9%) | 56 (38·6%) | 520 (39·5%) | 60 (42·6%) | 15 (23·1%) | |
| Cardiac arrhythmia | 2699 (26·9%) | 1960 (23·6%) | 739 (42·8%) | 55 (37·9%) | 574 (43·6%) | 64 (45·4%) | 24 (36·9%) | |
| Renal failure | 2287 (22·8%) | 1870 (22·5%) | 417 (24·1%) | 45 (31·0%) | 306 (23·2%) | 28 (19·9%) | 21 (32·3%) | |
| Congestive heart failure | 1963 (19·6%) | 1436 (17·3%) | 527 (30·5%) | 58 (40·0%) | 385 (29·2%) | 45 (31·9%) | 21 (32·3%) | |
| Chronic pulmonary disease | 1358 (13·6%) | 1025 (12·4%) | 333 (19·3%) | 43 (29·7%) | 234 (17·8%) | 29 (20·6%) | 13 (20·0%) | |
| Obesity | 590 (5·9%) | 361 (4·4%) | 229 (13·3%) | 17 (11·7%) | 182 (13·8%) | 23 (16·3%) | .. | |
| Obesity category by BMI, kg/m2 | ||||||||
| ≥30 and <35 | 211 (2·1%) | 148 (1·8%) | 63 (3·6%) | .. | 52 (3·9%) | .. | .. | |
| ≥35 and <40 | 139 (1·4%) | 87 (1·0%) | 52 (3·0%) | .. | 39 (3·0%) | .. | .. | |
| ≥40 | 163 (1·6%) | 81 (1·0%) | 82 (4·7%) | .. | 64 (4·9%) | .. | .. | |
| Unknown | 77 (0·8%) | 45 (0·5%) | 32 (1·9%) | .. | 27 (2·0%) | .. | .. | |
| Patients transferred between hospitals | 1089 (10·9%) | 628 (7·6%) | 461 (26·7%) | 23 (15·9%) | 371 (28·1%) | 44 (31·2%) | 11 (16·9%) | |
| Length of hospital stay, days | ||||||||
| Mean (SD) | 14·3 (13·8) | 12·0 (11·3) | 25·2 (18·5) | 18·1 (13·3) | 26·5 (18·7) | 29·9 (19·7) | 11·9 (14·3) | |
| Median (IQR) | 10·0 (5·0–19·0) | 9·0 (5·0–15·0) | 21·0 (10·0–37·0) | 15·0 (8·0–25·0) | 23·0 (11·0–39·0) | 26·0 (14·0–44·0) | 6·0 (1·0–14·0) | |
| Ventilation, days | ||||||||
| Mean (SD) | 13·5 (12·1) | .. | 13·5 (12·1) | 3·6 (4·2) | 15·1 (12·1) | 17·1 (12·7) | 0·1 (0·1) | |
| Median (IQR) | 10·1 (4·3–19·3) | .. | 10·1 (4·3–19·3) | 2·2 (0·9–4·3) | 11·8 (5·9–21·5) | 13·0 (8·0–24·0) | 0·1 (0·1–0·2) | |
| Tracheostomy | 445 (4·4%) | .. | 445 (25·8%) | .. | 406 (30·8%) | 39 (27·7%) | .. | |
| Extracorporeal membrane oxygenation | 119 (1·2%) | .. | 119 (6·9%) | .. | 104 (7·9%) | 12 (8·5%) | .. | |
| Dialysis | 599 (6·0%) | 130 (1·6%) | 469 (27·2%) | 7 (4·8%) | 404 (30·7%) | 41 (29·1%) | .. | |
| Deaths | 2229 (22·2%) | 1323 (16·0%) | 906 (52·5%) | 65 (44·8%) | 696 (52·8%) | 70 (49·6%) | 42 (64·6%) | |
Data are n (%), unless otherwise indicated. Data are not shown in cells that contain fewer than five patients. BMI=body-mass index.
Table 2.
Patient characteristics by sex
|
Patients with ventilation |
Patients without ventilation |
||||
|---|---|---|---|---|---|
| Female | Male | Female | Male | ||
| Number of patients | 580 | 1147 | 4242 | 4052 | |
| Number of hospitals | 315 | 467 | 787 | 765 | |
| Age, years | |||||
| Mean (SD) | 70·7 (12·9) | 67·3 (13·1) | 69·6 (18·7) | 67·0 (17·2) | |
| Median (IQR) | 73·0 (63·0–80·0) | 69·0 (59·0–78·0) | 76·0 (57·0–84·0) | 70·0 (55·0–81·0) | |
| Age group, years | |||||
| 18–59 | 109 (18·8%) | 313 (27·3%) | 1192 (28·1%) | 1282 (31·6%) | |
| 60–69 | 107 (18·4%) | 275 (24·0%) | 554 (13·1%) | 685 (16·9%) | |
| 70–79 | 202 (34·8%) | 333 (29·0%) | 769 (18·1%) | 854 (21·1%) | |
| ≥80 | 162 (27·9%) | 226 (19·7%) | 1727 (40·7%) | 1231 (30·4%) | |
| Elixhauser comorbidities | |||||
| Hypertension | 379 (65·3%) | 698 (60·9%) | 2321 (54·7%) | 2177 (53·7%) | |
| Diabetes | 245 (42·2%) | 426 (37·1%) | 1,015 (23·9%) | 1105 (27·3%) | |
| Cardiac arrhythmia | 256 (44·1%) | 483 (42·1%) | 961 (22·7%) | 999 (24·7%) | |
| Renal failure | 157 (27·1%) | 260 (22·7%) | 985 (23·2%) | 885 (21·8%) | |
| Congestive heart failure | 193 (33·3%) | 334 (29·1%) | 739 (17·4%) | 697 (17·2%) | |
| Chronic pulmonary disease | 118 (20·3%) | 215 (18·7%) | 522 (12·3%) | 503 (12·4%) | |
| Obesity | 105 (18·1%) | 124 (10·8%) | 207 (4·9%) | 154 (3·8%) | |
| Obesity category by BMI, kg/m2 | |||||
| ≥30 and <35 | 32 (5·5%) | 31 (2·7%) | 82 (1·9%) | 66 (1·6%) | |
| ≥35 and <40 | 17 (2·9%) | 35 (3·1%) | 51 (1·2%) | 36 (0·9%) | |
| ≥40 | 42 (7·2%) | 40 (3·5%) | 49 (1·2%) | 32 (0·8%) | |
| Unknown | 14 (2·4%) | 18 (1·6%) | 25 (0·6%) | 20 (0·5%) | |
| Patients transferred between hospitals | 152 (26·2%) | 309 (26·9%) | 327 (7·7%) | 301 (7·4%) | |
| Length of hospital stay, days | |||||
| Mean (SD) | 26·4 (18·7) | 24·6 (18·4) | 12·3 (11·8) | 11·7 (10·8) | |
| Median (IQR) | 23·0 (11·0–39·0) | 20·0 (10·0–36·0) | 9·0 (4·0–16·0) | 8·0 (5·0–15·0) | |
| Ventilation (days) | |||||
| Mean (SD) | 13·0 (11·8) | 13·8 (12·3) | .. | .. | |
| Median (IQR) | 10·1 (4·3–18·3) | 10·0 (4·3–20·2) | .. | .. | |
| Tracheostomy | 132 (22·8%) | 313 (27·3%) | .. | .. | |
| Extracorporeal membrane oxygenation | 30 (5·2%) | 89 (7·8%) | .. | .. | |
| Dialysis | 115 (19·8%) | 354 (30·9%) | 57 (1·3%) | 73 (1·8%) | |
| Deaths | 289 (49·8%) | 617 (53·8%) | 644 (15·2%) | 679 (16·8%) | |
Data are n (%), unless otherwise indicated. BMI=body-mass index.
The median age was 72 years (IQR 57–82), with a similar median age for patients with and without ventilation (table 1). The proportion of patients who were ventilated was 15% (422 of 2896) of those aged 18–59 years, 24% (382 of 1621) of those aged 60–69 years, 25% (535 of 2158) of those aged 70–79 years, and 12% (388 of 3346) of those aged 80 years and older (figure 1A ).
Figure 1.
Age distribution (A) and Charlson comorbidity index (B)
Only adult patients aged 18 years or older were included in the analysis.
The proportion of men was 49% (4052 of 8294) among patients who did not receive ventilation and 66% (1147 of 1727) among patients who did receive ventilation (table 2). Thus, the probability of being ventilated was 12% (580 of 4822) for women and 22% (1147 of 5199) for men.
The most common comorbidities were hypertension (5575 [56%] of 10 021), diabetes (2791 [28%]), cardiac arrythmia (2699 [27%]), renal failure (2287 [23%]), heart failure (1963 [20%]), and chronic obstructive pulmonary disease (COPD; 1358 [14%]; table 1). 6% (590 of 10 021) of the patients were obese. Furthermore, 6% (599 of 10 021) of all patients received dialysis during hospitalisation. All comorbidities, as well as the number of patients receiving dialysis, were higher in the ventilated group compared with the non-ventilated group. 39% (3237 of 8294) of patients in the non-ventilated group and 22% (374 of 1727) of patients in the ventilated group had a Charlson comorbidity index of 0. In the ventilated group, more than 50% had an index of 2 or higher (figure 1B).
The mean length of hospital stay was 14·3 days (SD 13·8) overall, with a mean of 12·0 days (11·3) in the non-ventilated group and 25·2 days (18·5) in the ventilated group (table 1, appendix pp 2, 4). 27% (461 of 1727) of all ventilated patients were transferred between hospitals.
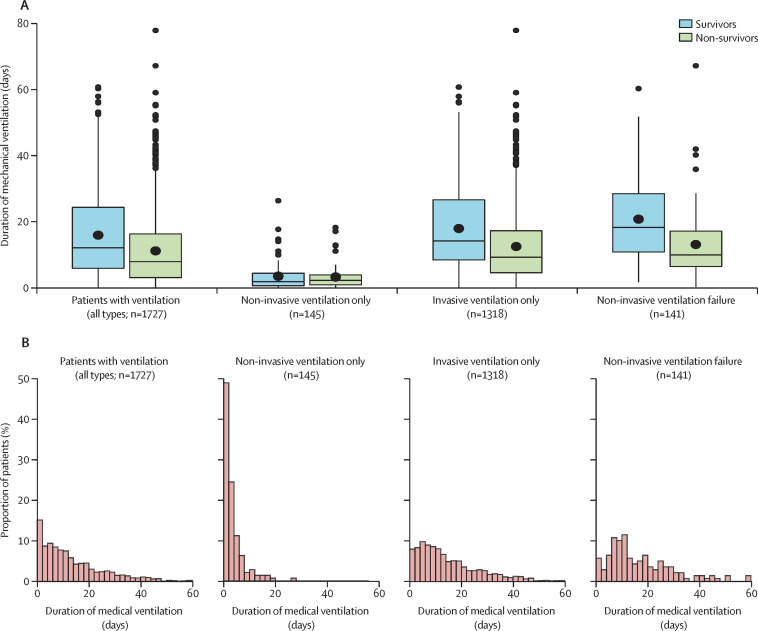
In the ventilated group, mean ventilation duration was 13·5 days (SD 12·1), ranging from 3·6 days (4·2) in patients receiving non-invasive ventilation only to 17·1 (12·7) in patients with non-invasive ventilation failure (table 1). The differences in duration of mechanical ventilation between patients who survived and those who did not were modest (figure 2A ). Additionally, figure 2B shows the distribution of mechanical ventilation duration by type of ventilation. 26% (445 of 1727) of all patients with ventilation were tracheostomised (table 1).
Figure 2.
Duration of mechanical ventilation by ventilation type
(A) Duration of mechanical ventilation by type of ventilation and survival status. Box plots show medians and IQRs. Means are shown with large circles. Outliers are shown with small circles. (B) Distribution of the duration of mechanical ventilation.
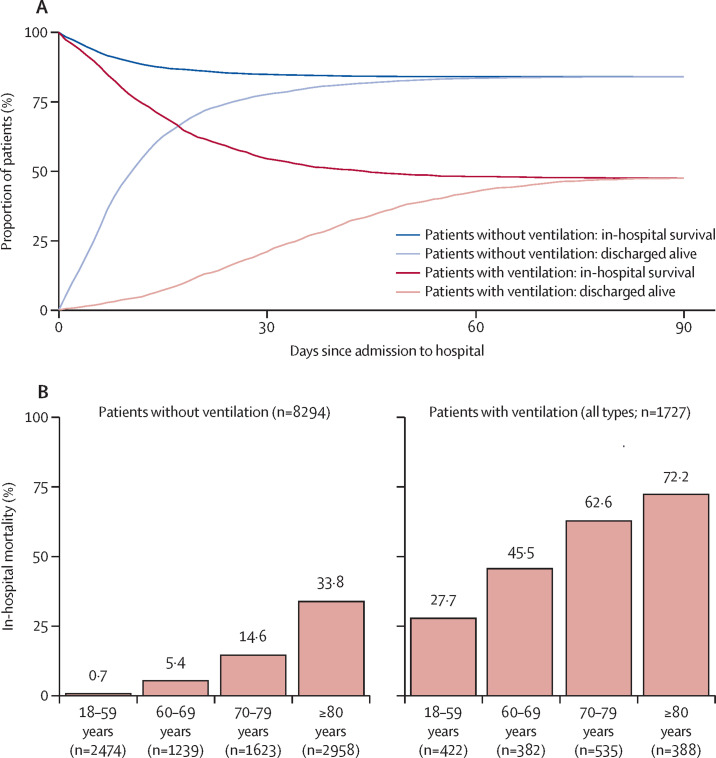
Overall, in-hospital mortality was 22% (2229 of 10 021), with wide variation between groups (table 1, figure 3A ). In-hospital mortality was 16% (1323 of 8294) for patients without mechanical ventilation, and 53% (906 of 1727) with mechanical ventilation (non-invasive ventilation 45% [65 of 145], non-invasive ventilation failure 50% [70 of 141], and invasive mechanical ventilation 53% [696 of 1318]; appendix p 3). Disaggregating by age, in-hospital mortality in the ventilated group was 28% (117 of 422) in patients aged 18–59 years, 46% (174 of 382) in patients aged 60–69 years, 63% (335 of 535) in patients aged 70–79 years, and 72% (280 of 388) in patients aged 80 years or older (figure 3B). In the same age groups, in-hospital mortality was lower in patients without mechanical ventilation: 1% (18 of 2474) in patients aged 18–59 years, 5% (67 of 1239) in patients aged 60–69 years, 15% (237 of 1623) in patients aged 70–79 years, and 34% (1001 of 2958) in patients aged 80 years or older (figure 3B, appendix p 4). In-hospital mortality in ventilated patients who were also treated with dialysis was particularly high at 73% (342 of 469), and 71% (84 of 119) of patients on extracorporeal membrane oxygenation died (appendix p 4). Furthermore, mortality did not change considerably over the study period (appendix p 5). Because most patients were not ventilated, in absolute terms, more patients died without ventilation (n=1323) than with ventilation (n=906).
Figure 3.
In-hospital mortality
(A) In-hospital survival with and without mechanical ventilation. (B) In-hospital mortality with and without mechanical ventilation by age.
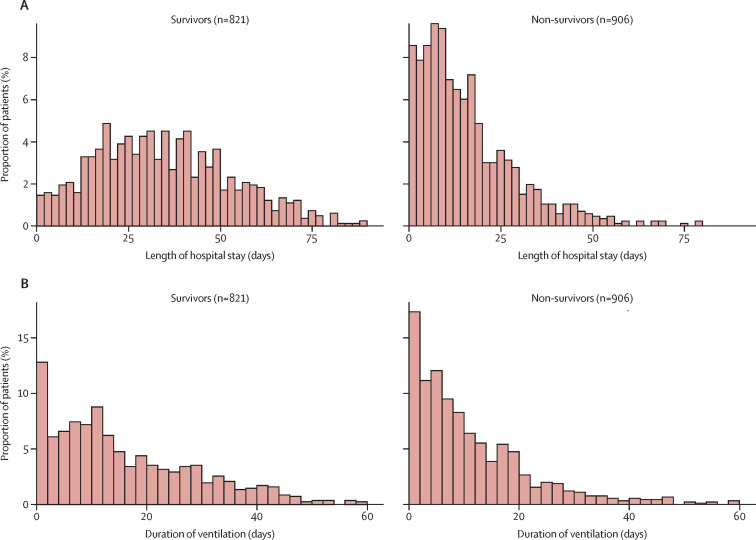
Stratifying the group of ventilated patients by length of hospital stay (figure 4A ) and duration of ventilation (figure 4B) shows that the probability of dying was particularly high in the first 10 days of hospitalisation. A length of stay of more than 18 days was associated with survival (figure 4A), whereas no such association was seen for duration of ventilation (figure 4B).
Figure 4.
Duration of hospital stay and mechanical ventilation by survival status in ventilated patients
Distribution of length of hospital stay (A) and duration of mechanical ventilation (B) in survivors and non-survivors.
Discussion
This study describes the characteristics of hospitalised patients with COVID-19 in a large, unselected, and unbiased nationwide cohort of 10 021 patients admitted to 920 hospitals in Germany, including during the peak of admissions at the end of March, 2020, and in the first half of April (ie, up to 2 weeks after the peak of new infections). To the best of our knowledge, this is the first report of in-hospital mortality in a large group of patients with COVID-19 in Germany. The main findings of our study were that most patients were aged 70 years or older, that patients on mechanical ventilation had more comorbidities than patients without mechanical ventilation, and that mortality was high, with a mortality of 53% in patients being mechanically ventilated and 73% in patients requiring both ventilation and dialysis. Overall, in-hospital mortality was 22%, which is similar to that reported in France,9 but considerably lower than in the UK where in-hospital mortality was reported to be 39%, if only patients who were discharged or died in hospital are taken into account.15 However, the age distribution of patients, particularly of patients admitted to hospital and of those on mechanical ventilation, generally differs between the European countries.
Mortality was particularly high for patients on mechanical ventilation (53%), reaching 63% in patients aged 70–79 years and 72% in patients aged 80 years and older. These mortality rates are higher than those for severe acute respiratory distress syndrome (ARDS).22 In the New York cohort reported by Richardson and colleagues,14 mortality was 24·5%, including patients remaining in the ICU. However, if only patients discharged from the ICU were included in the analysis, as done in our cohort, mortality among patients aged 18–65 years and those older than 65 years would be substantially higher. Of note, the smaller proportion of patients receiving mechanical ventilation and the higher in-hospital mortality in New York could reflect an overburdened health-care system. The Intensive Care National Audit & Research Centre23 reports an ICU mortality for England, Wales, and Northern Ireland of slightly less than 30% in patients younger than 60 years, consistent with our data, and of 60–80% in patients aged 60 years and older. In patients aged 60 years or older in particular, mortality is nearly 75% in those receiving renal replacement therapy.23
Our data indicate that half of all deaths among ventilated patients occurred in the first 12 days after hospital admission. Furthermore, patients requiring both ventilation and dialysis had the highest in-hospital mortality of 73%, possibly due to multiorgan failure or renal tropism of the virus.24
In general, our data show the high morbidity and mortality in older patients, with a considerably lower mortality for patients younger than 60 years. In particular, mortality is very high in patients older than 70 years, reaching 72% in patients aged 80 years or older with ventilation, which is in line with data reported from the UK23 and from patients undergoing surgery.25 Of note, mortality also reached 34% in patients aged 80 years and older without mechanical ventilation. These results provide new information relevant to patient allocation during the pandemic, especially in times of high ICU demand.26 Countries such as Italy,11 the UK, and France, which had limited ICU bed resources, high infection rates, and particularly high COVID-19-related deaths during the first wave of the pandemic, admitted fewer older patients to high-care ICU treatment, including invasive mechanical ventilation. In England, Wales, and Northern Ireland, only 20·3% of patients with COVID-19 being treated in ICUs were older than 70 years (and only 2·6% were older than 80 years),23 compared with 54% (and 23%) in our patient population. Data from the German ICU registry shows that there was sufficient ICU capacity throughout the study period, which could be a major explanation for the large number of older patients being mechanically ventilated in Germany.
Comorbidities are a major risk factor for requiring mechanical ventilation in COVID-19, with mortality of women and men on ventilation being equal. The high in-hospital mortality for ventilated patients is lower if patients can be treated with non-invasive ventilation alone, although 60% of such patients had a Charlson comorbidity index of 2 or more. Our data cannot distinguish whether the treatment or the severity of the disease accounts for this more preferential outcome. On the one hand, if patients can be treated with non-invasive ventilation alone, mortality is low, as has been shown for other diseases, such as acute exacerbated COPD.27 On the other hand, non-invasive ventilation failure is associated with mortality almost as high as invasive mechanical ventilation, highlighting that the indications and limits of non-invasive ventilation in COVID-19 need to be determined. Moreover, 27% of patients on mechanical ventilation required dialysis. In-hospital mortality in this group of patients was very high at 73%, indicating that acute renal failure must be prevented in patients with COVID-19 as far as possible.28 Extracorporeal membrane oxygenation was used in 7% of all patients on mechanical ventilation, with a high mortality of 71%. These data might show the heterogeneity of treatment and widespread use of extracorporeal membrane oxygenation in Germany because data from the EuroELSO show a more preferential outcome in dedicated centres.29
One key factor in containing the pandemic is access to and availability of ICU beds. Therefore, prognostic models have been established which could guide patient allocation and lockdown measures.26, 30 In this context, the duration of mechanical ventilation is an important factor; the mean duration in this cohort was 13·5 days (SD 12·1); median 10 days [IQR 5–19]). However, a substantial number of patients were on long-term invasive mechanical ventilation above the upper limit of the IQR, which has a considerable impact on accessible ICU beds in a severe phase of the pandemic. Therefore, long-term care facilities might have a substantial effect in generating free ICU capacity.
One limitation of our study is the data source, which includes only patients from the largest group of German sickness funds. However, they account for around a third of the total population, giving a large sample representative for the German population, even if the very old (≥80 years) are over-represented. Hospital data are of high quality because disease codes and procedure codes are relevant for the amount of remuneration and are therefore verified by hospitals and sickness funds. Nevertheless, codes can be missing if there is no impact on remuneration. Second, patient-specific data are limited to diagnoses, procedures, and initial characteristics. Third, with respect to mechanical ventilation, this observational study cannot distinguish between treatment effects and severity of the disease, particularly with regard to the use of non-invasive ventilation in COVID-19. Fourth, we stratified by mechanical ventilation but not by ICU treatment, which sometimes includes high-flow oxygen therapy without mechanical ventilation. Due to the absence of codes, the absence of incentives for coding, or both, continuous positive airway pressure and high-flow oxygen therapy could not be analysed. Fifth, we could not differentiate between patients who had been hospitalised for COVID-19 or for any other reason, or similarly for mortality, whether mortality was related to COVID-19 or an underlying medical condition. Sixth, we do not currently have outpatient data available, and therefore we cannot distinguish between acute and chronic comorbidities, particularly with regard to renal failure.
In the German health-care system, in which capacity limits were not reached during the first wave of COVID-19 cases, in-hospital mortality was 22%, similar to that in France where the hospitalisation rate was much higher.30 In-hospital mortality was considerably lower for patients younger than 60 years than those aged 80 years or older, and was even lower than expected for more severe forms of ARDS.22 Older patients and those requiring dialysis had the worst prognosis, with an in-hospital mortality of almost 75%. Furthermore, men had a higher severity of disease than women, but have similar outcomes when ventilated. With unrestrained resources, a small but considerable number of older patients and patients with comorbidities can survive severe forms of COVID-19, but in the event of a strong second wave of the pandemic, longer treatment times could limit hospital capacities.
Data sharing
The data used in this study cannot be made available in the manuscript, the supplemental files, or in a public repository due to German data protection laws (Bundesdatenschutzgesetz). Therefore, they are stored on a secure drive in the Wissenschaftliches Institut der AOK to facilitate replication of the results. Generally, access to data of statutory health insurance funds for research purposes is possible only under the conditions defined in German Social Law (SGB V § 287). Requests for data access can be sent as a formal proposal specifying the recipient and purpose of the data transfer to the appropriate data protection agency. Access to the data used in this study can only be provided to external parties under the conditions of the cooperation contract of this research project and after written approval by the AOK. For assistance in obtaining access to the data, please contact carina.mostert@wido.bv.aok.de.
Acknowledgments
Acknowledgments
Institutional support and physical resources were provided by the University Witten/Herdecke and Kliniken der Stadt Köln, the Federal Association of the Local Health Care Funds, and Technische Universität Berlin.
Contributors
CK, CM, and RB conceived the study and its design, had full access to the data, and take responsibility for the integrity of the data and accuracy of the analysis. CM, CH, JM, GS, and JK organised and entered data. CK, CM, CH, JM, GS, JK, and RB contributed to data analyses. CK, CM, CH, JM, GS, JK, and RB had access to the underlying data for verification. TV, JM, GS, JK, UJ, GM, SW-C, SK, MP, LG, and TW contributed to data interpretation. CK, CM, and RB wrote the main draft of the manuscript. All authors contributed to the final drafting of the manuscript.
Declaration of interests
CK received travel grants and lecture fees from Maquet, and travel grants and fees for advisory board meetings from Xenios and Bayer; he is the speaker of the German register of intensive care units; and he received grants from the German Ministry of Research and Education during the conduct of the study. UJ is the president of the German Society of Intensive Care Medicine. GM received consultant honorarium and research support from Biotest, B Braun, and Adrenomed. SW-C has an ongoing research cooperation with Dräger Medical. SK received research support from Ambu, ETView, Fisher & Paykel, Pfizer, and Xenios; lecture honorarium from ArjoHuntleigh, Astellas, Astra, Basilea, Bard, Baxter, Biotest, CSL Behring, Cytosorbents, Fresenius, Gilead, MSD, Orion, Pfizer, Philips, Sedana, Sorin, Xenios, and Zoll; and consultant honorarium from Amomed, Astellas, Baxter, Bayer, Fresenius, Gilead, MSD, Pfizer, and Xenios, during the conduct of the study. MP received lecture fees from Boehringer, AstraZeneca, Novartis, Roche, Chiesi, and GlaxoSmithKline; travel grants from Boehringer; and fees for advisory board meetings from Boehringer, Roche, Novartis, and Chiesi. TW received grants from the German Ministry of Research and Education, during the conduct of the study; grants from Roche, Novartis, Immunogenic, and GlaxoSmithKline, outside of the submitted work; and fees for advisory board participation and lectures from AstraZeneca, Bayer, Boehringer, GlaxoSmithKline, Novartis, and Roche, outside of the submitted work. RB is a member of the Federal Ministry of Health-appointed expert committee to evaluate the COVID-19 hospital exoneration measures; his department received grants from the German Ministry of Education and Research, WHO, and the Berlin University Alliance, outside of the submitted work. All other authors declare no competing interests.
Supplementary Material
References
- 1.Robert Koch Institut Coronavirus disease 2019 (COVID-19) daily situation report of the Robert Koch Institute. July 15, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-07-15-en.pdf?__blob=publicationFile
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xie J, Tong Z, Guan X, Du B, Qiu H. Clinical characteristics of patients who died of coronavirus disease 2019 in China. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.5619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nationale Intensive Care Evaluatie COVID-19 infecties op de verpleegafdeling. 2020. https://www.stichting-nice.nl/covid-19-op-de-zkh.jsp
- 7.Sante Publique France Point épidémiologique hebdomadaire du 21 mai 2020. May 21, 2020. https://www.santepubliquefrance.fr/content/download/254170/2609369
- 8.Centro Nacional de Epidemiología Situación de COVID-19 en España. 2020. https://cnecovid.isciii.es/covid19
- 9.Sciensano COVID-19—wekelijks epidemiologisch bulletin van 22 mei 2020. May 22, 2020. https://covid-19.sciensano.be/sites/default/files/Covid19/COVID-19_Weekly%20report_20200522%20-%20NL.pdf
- 10.Wadhera RK, Wadhera P, Gaba P. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grasselli G, Zangrillo A, Zanella A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu C, Chen X, Cai Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cao B, Wang Y, Wen D. A trial of lopinavir-ritonavir in adults hospitalised with severe COVID-19. N Engl J Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richardson S, Hirsch JS, Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Docherty AB, Harrison EM, Green CA. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369 doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wunsch H. Mechanical ventilation in COVID-19: interpreting the current epidemiology. Am J Respir Crit Care Med. 2020;202:1–4. doi: 10.1164/rccm.202004-1385ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.German Federal Ministry of Health Gesetzliche Krankenversicherung: Mitglieder, mitversicherte Angehörige und Krankenstand: Monatswerte Januar–April 2020. 2020. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/Statistiken/GKV/Mitglieder_Versicherte/KM1_Januar_bis_April_2020_bf.pdf
- 19.Busse R, Blümel M, Knieps F, Bärnighausen T. Statutory health insurance in Germany: a health system shaped by 135 years of solidarity, self-governance, and competition. Lancet. 2017;390:882–897. doi: 10.1016/S0140-6736(17)31280-1. [DOI] [PubMed] [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Ranieri VM, Rubenfeld GD, Thompson BT. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 23.Intensive Care National Audit & Research Centre ICNARC report on COVID-19 in critical care. May 22, 2020. https://www.icnarc.org/DataServices/Attachments/Download/593555ce-709c-ea11-9126-00505601089b
- 24.Puelles VG, Lütgehetmann M, Lindenmeyer MT. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. 2020 doi: 10.1056/NEJMc2011400. published online May 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Banerjee A, Pasea L, Harris S. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395:1715–1725. doi: 10.1016/S0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chandra D, Stamm JA, Taylor B. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med. 2012;185:152–159. doi: 10.1164/rccm.201106-1094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Institute for Health and Care Excellence Acute kidney injury: prevention, detection and management. Dec 18, 2019. https://www.nice.org.uk/guidance/ng148 [PubMed]
- 29.EuroELSO EuroELSO survey on ECMO use in adult COVID-19 patients in Europe. 2020. https://www.euroelso.net/covid-19/covid-19-survey
- 30.Salje H, Tran Kiem C, Lefrancq N. Estimating the burden of SARS-CoV-2 in France. Science. 2020 doi: 10.1126/science.abc3517. published online May 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Uncited References
- 17.Organisation for Economic Co-operation and Development Beyond containment: health systems responses to COVID-19 in the OECD. 2020. http://www.oecd.org/coronavirus/policy-responses/beyond-containment-health-systems-responses-to-covid-19-in-the-oecd-6ab740c0
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study cannot be made available in the manuscript, the supplemental files, or in a public repository due to German data protection laws (Bundesdatenschutzgesetz). Therefore, they are stored on a secure drive in the Wissenschaftliches Institut der AOK to facilitate replication of the results. Generally, access to data of statutory health insurance funds for research purposes is possible only under the conditions defined in German Social Law (SGB V § 287). Requests for data access can be sent as a formal proposal specifying the recipient and purpose of the data transfer to the appropriate data protection agency. Access to the data used in this study can only be provided to external parties under the conditions of the cooperation contract of this research project and after written approval by the AOK. For assistance in obtaining access to the data, please contact carina.mostert@wido.bv.aok.de.